Abstract
We report delayed intravitreal pigment dispersion following Iodine-125 plaque brachytherapy, without evidence of tumor recurrence, in 4 patients treated for choroidal melanoma. These patients were treated with Iodine-125 plaque brachytherapy, with or without transpupillary thermotherapy, and were followed clinically and using ancillary investigations for signs of tumor recurrence. All 4 patients were noted to develop pigment dispersion − it was detected on the surface of the retina (2 patients), diffusely in the vitreous (1 patient), or both (1 patient). Follow-up ranged from 70 to 343 months (mean 165 months; median 124 months) post-treatment with plaque brachytherapy, throughout which the location and amount of pigment remained grossly unchanged. None of the patients developed tumor recurrence or metastasis. We conclude that post-brachytherapy pigment dispersion is an unusual but known complication in the treatment of uveal melanoma. Close surveillance to rule out tumor recurrence and metastasis may be a reasonable line of management.
Keywords: Intraocular tumors, Ocular oncology, Pigment dispersion, Retina and vitreous, Uveal melanoma
Established Facts
Uveal melanoma tumor recurrence can present as intraocular pigment dispersion due to seeding of viable melanoma cells.
Novel Insights
Post-plaque brachytherapy-delayed pigment dispersion can mimic tumor recurrence.
Close surveillance is required to detect proliferation of the pigment or seeding of the retina.
Introduction
Uveal melanoma is the most common primary intraocular malignancy in adults [1]. Treatment of choroidal melanoma with Iodine-125 (I-125) plaque brachytherapy has been well established for effective local tumor control [2]. A rare presentation of tumor recurrence can manifest as intravitreal seeding of viable melanoma cells. These are difficult to distinguish from pigment-laden macrophages which are benign and only warrant observation. Here, we report a series of 4 patients with medium-sized choroidal melanomas who developed delayed pigment dispersion following plaque brachytherapy.
Patients and Methods
This is a retrospective case series. HIPAA compliance was ensured, and we adhered to the declaration of Tenets of Helsinki. Institutional Review Board approval was obtained. Four patients with a diagnosis of uveal melanoma who underwent I-125 plaque brachytherapy who were found to have dispersion of pigment following treatment were included. Diagnosis was based on clinical examination and ancillary testing by an experienced ocular oncologist (BPM). None of the patients underwent fine-needle aspiration biopsy for cytology and/or cytogenetics. Charts, ocular imaging studies, ultrasonography, and systemic screening imaging were reviewed.
Four patients were found to have pigment dispersion into the vitreous and/or on to the retina. All patients opted for conservative management with observation. None of the patients showed metastatic disease or local recurrence during their follow-up period. Demographics and tumor characteristics are listed in Table 1.
Table 1.
Tumor characteristics and patient demographics
| Characteristics | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Age | 56 | 48 | 44 | 75 |
| Sex | Female | Female | Male | Female |
| Basal dimension, mm | 11.5X9 | 10X12 | 14X10 | 10×8 |
| Thickness, mm | 5 | 6 | 4.4 | Not known |
| Retinal invasion | No | No | No | No |
| Vitreous/subretinal pigment prior to plaque brachytherapy | No | No | No | No |
| Tumor biopsy | No | No | No | No |
| Treatment | I-125 plaque | I-125 plaque | I-125 plaque | I-125 plaque |
| brachytherapy + TTT | brachytherapy + TTT | brachytherapy | brachytherapy | |
| Duration from treatment to appearance of pigment dispersion, months | 120 | 44 | 24 | 36 |
| Location of pigment dispersion | Subretinal + intravitreal | Subretinal + intravitreal | Intravitreal | Overlying retina |
| Diagnostic vitrectomy | No | No | Yes | No |
| Follow-up since primary treatment, months | 144 | 70 | 104 | 343 |
| Follow-up since pigment dispersion, months | 26 | 26 | 80 | 307 |
| Visual acuity at last visit | 20/40 | 20/80 | 20/60 | No LP |
| Tumor recurrence at last visit | None | None | None | None |
| Systemic status at last visit | None | None | None | None |
Patient 1
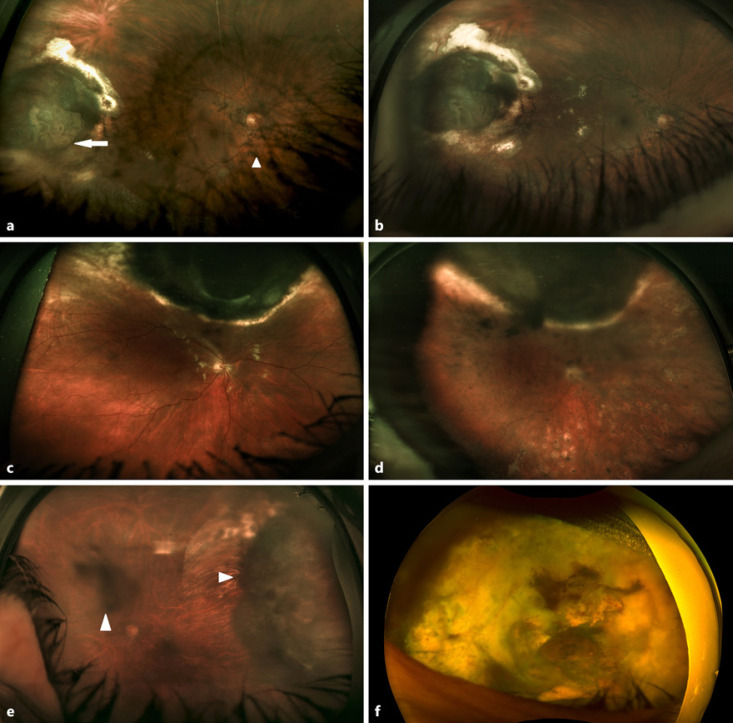
A 56-year-old woman was found to have a moderately pigmented choroidal melanoma in the right eye, measuring 11.5 mm × 9 mm basal dimensions, with a height of 5 mm. At baseline, there was no evidence of retinal invasion, break in Bruch's membrane, or pigment dispersion in the fundus. She was treated with I-125 plaque brachytherapy and adjuvant transpupillary thermotherapy (TTT). Following treatment, tumor regression was noted and the patient was followed up at 6-month intervals. Approximately 10 years post-plaque treatment, she developed sudden-onset deterioration of vision along with increased light sensitivity in the right eye. Best-corrected visual acuity was 20/40 OD. Anterior segment examination was significant showing +4 pigmented cells in anterior vitreous with no anterior chamber inflammation. Fundus examination of the right eye revealed a brownish black blob of pigment over the tumor with retinal pigment dispersion along the vascular arcade and optic disc (Fig. 1a). The tumor appeared regressed with thickness similar to prior ultrasonography and OCT. The patient was followed closely to look for any signs of tumor activity. At 2.5 years following pigment dispersion, the tumor remained regressed with minimal change in the size of vitreous as well as subretinal pigmentation and maintained a visual acuity of 20/40 OD with no evidence of systemic metastasis (Fig. 1b).
Fig. 1.
a Fundus photograph 10 years following plaque brachytherapy showing pigment dispersion over the tumor (arrow) and along the vascular arcades and optic disc (arrowhead). b Fundus photograph showing nearly unchanged pigment dispersion 2.5 years later. c Fundus photograph post-brachytherapy and adjuvant TTT with no evidence of pigment dispersion. d Fundus photograph 31 months following treatment with plaque brachytherapy showing intravitreal and retinal pigment dispersion which remained unchanged. e Fundus photograph post-vitrectomy showing regressed tumor with residual vitreous debris (arrowheads). f Fundus photograph showing regressed tumor in the temporal quadrant with multiple areas of pigment dispersion overlying the retina and chronic atrophic retinal detachment 28 years following the initial plaque treatment.
Patient 2
A 48-year-old woman was diagnosed with a pigmented choroidal melanoma in the right eye, measuring 12 mm × 10 mm wide and 6 mm in height. She was treated with I-125 plaque brachytherapy along with 3 sessions of adjuvant TTT. Seventeen months post-treatment, she showed marked tumor regression with residual apical bulge along with early radiation retinopathy. She was treated with 3 additional cycles of TTT at 3-month intervals to ensure no recurrence (Fig. 1c). She received anti-VEGF injections for progressive radiation retinopathy. On follow-up examinations, she maintained a best-corrected visual acuity of 20/100 OD. Ultrasound showed continued decrease in thickness of the overall tumor by 30% with no intrinsic vascular pulsations or any signs of extraocular extension. Forty-four months following the initial treatment, the patient developed sudden-onset floaters in the right eye. VA dropped from 20/50 to 20/400 OD. Intraocular pressure and anterior chamber were normal. Fundus examination showed an area of necrosis over the tumor apex with small clumps of brownish pigments dispersed retinally and throughout the vitreous cavity. The tumor itself appeared regressed. Ultrasound showed low reflectivity but was otherwise unchanged from prior. Pigment dispersion in her case was presumably from the necrotic cap, secondary to treatment from brachytherapy and multiple TTT treatments. The patient was reassured, and at 26 months following pigment dispersion, there was no change in the pigment location or density, with stable vision, regressed tumor, and no evidence of metastatic disease (Fig. 1d).
Patient 3
A 44-year-old man with a history of moderate-sized pigmented ciliochoroidal melanoma of the left eye was treated with I-125 plaque brachytherapy. His ocular history was significant for postradiation cataract and multiple aflibercept injections for radiation retinopathy. Subsequent cataract removal was complicated by exuberant postoperative panuveitis which was managed with steroids. Two years after brachytherapy, the patient developed sudden-onset reduction in vision in the left eye, accompanied with floaters. Vision was 20/200 OS, and intraocular pressure was normal. Slit-lamp examination showed +3 cells and pigment in anterior chamber with +3 cells and pigments in the anterior vitreous. Fundus examination showed vitreous opacification, and pigmented debris obscured the view of the tumor. Ultrasound showed measurements comparable to the previously recorded regressed tumor. Pars plana vitrectomy was performed to clear the pigmented cells and improve acuity. Vitreous specimens sent for cytology were negative for viable tumor cells. After vitrectomy, visual acuity improved but a low-grade vitritis persisted, managed with topical and intravitreal steroids as well as anti-VEGF injections. Clearer fundus view confirmed regressed choroidal tumor with minimal pigmented debris in the vitreous and overlying the tumor. Follow-up examination 8.5 years after the initial plaque showed continued regression of the tumor with minimal change in the pigmented debris over the tumor as well as in the vitreous debris, without any evidence of systemic metastasis (Fig. 1e).
Patient 4
A 75-year-old woman with a long-standing history of left eye choroidal melanoma was treated with I-125 plaque brachytherapy at an outside institution approximately 28 years prior to evaluation. She was referred to our institute for continued follow-up. She had known retinal and vitreous pigment dispersion which was being observed without any treatment since approximately 24 years. Vision in the right eye was 20/25 with no light perception in the left eye. The left cornea had band-shaped keratopathy with sectoral iridial nevus. There was inferior dislocation of the lens. Fundus examination showed a regressed tumor in the temporal quadrant. There were multiple areas of brownish pigment dispersion overlying the retina with chronic atrophic retinal detachment (Fig. 1f). Ultrasound was consistent with a choroidal melanoma scar with no intrinsic vascular pulsations. There was no evidence of extraocular extension. She remains stable with no evidence of systemic metastasis 24 years after the discovery of pigment dispersion.
Discussion
Uveal melanoma is the most common primary intraocular malignancy in adults [1]. The Collaborative Ocular Melanoma Study, a large multicenter trial, established that treatment with I-125 plaque brachytherapy compared to enucleation offered similar 5-year mortality rates for medium-sized choroidal melanomas (between 2.5 and 10 mm in height and <16 mm basal diameter), thus shifting the treatment preference to plaque brachytherapy, to better preserve vision [2]. Recurrence rates were 10% in this group and required enucleation [2]. Now that the majority of lesions are treated with globe sparing techniques, the detection and treatment of recurrences are crucial. The normal patterns for local recurrences are marginal growth, increase in thickness, extraocular extension, and rarely intraocular seeding [3]. Distinguishing between dispersed recurrent viable tumor and melanophagic debris is difficult both clinically and histopathologically. In this series, we focus on the clinical significance of pigment dispersion following brachytherapy.
All of our patients were treated with episcleral I-125 plaque brachytherapy with a median dose of 85 Gy to the tumor apex. Patients 1 and 2 were also treated with adjuvant TTT at the time of treatment. Post-treatment intraocular pigment dispersion can occur due to one of several mechanisms. One of the commonly reported mechanisms is brachytherapy-induced shrinkage of the tumor body after a break in Bruch's membrane, with invasion of the overlying retina and dispersion into the vitreous [4]. Kiratli et al. [5, 6] hypothesized that the heat produced during TTT results in ischemic necrosis and chronic inflammatory cell infiltration, resulting in thinning of overlying neurosensory retina. Additionally, TTT is a diode laser and can cause chorioretinal adhesion [7]. As the former shrinks, traction on areas of chorioretinal adhesion may liberate pigment in areas of thinned retina that stretch or break over the tumor and gain entry into the vitreous.
With the advent of diagnostic vitrectomy, clinical management of intravitreal pigment dispersion evolved from enucleation to more novel techniques involving pars plana vitrectomy and intravitreal chemotherapy. In their study, Metz and colleagues found that diagnostic vitrectomy post-brachytherapy showed equal number of melanophagic debris as well as viable melanoma cells [8]. Moreover, in a small subset, while cytology showed melanoma cells, the enucleated specimen revealed only necrotic tumor debris, thus questioning the necessity for enucleation especially when there is no increased risk of systemic metastasis. In recent times, progressive pigment dispersion is managed with early 23–25 gauge pars plana vitrectomy to surgically debulk the pigment cells followed by intravitreal chemotherapy in the form of methotrexate (400 μg in 0.1 mL) or melphalan (32 μg in 0.075 mL) [9, 10].
Metz and colleagues had found metastatic disease in 1 of 23 (4.3%) of their patients of uveal melanoma with pigment dispersion, while Harbour and other authors found no evidence of metastatic disease in their patients they had reported [4, 6, 8]. Our patients with pigment dispersion had a much longer duration of follow-up. They had stable pigment dispersion, and none of them developed metastatic disease, even in the absence of treatment.
Conclusion
Based on this information, one may surmise that the presence of uveal melanoma with pigment dispersion requires close surveillance. New proliferation of the pigment or seeding of the retina should be closely monitored. Diagnostic vitrectomy is recommended in patients with increased pigment proliferation to detect tumor recurrence. Close observation in patients with stable pigment may be a reasonable approach for detection of tumor progression.
Statement of Ethics
The study was approved by Institutional Review Board: IRB-AAAS7259. Written informed consents were obtained from the patients for publication of this case series and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive any funding sources for this study.
Author Contributions
Arpita Maniar performed data collection and analysis and drafted the manuscript. Brian P. Marr designed and conceptualized the study and revised the manuscript for intellectual content.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
- 1.Singh AD, Turell ME, Topham AK. Uveal melanoma: trends in incidence, treatment, and survival. Ophthalmology. 2011 Sep;118((9)):1881–5. doi: 10.1016/j.ophtha.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 2.Collaborative Ocular Melanoma Study Group The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: V. Twelve-year mortality rates and prognostic factors: COMS report no. 28. Arch Ophthalmol. 2006;124:1684–93. doi: 10.1001/archopht.124.12.1684. [DOI] [PubMed] [Google Scholar]
- 3.Shields CL, Cater J, Shields JA, Chao A, Krema H, Materin M, et al. Combined plaque radiotherapy and transpupillary thermotherapy for choroidal melanoma: tumor control and treatment complications in 270 consecutive patients. Arch Ophthalmol. 2002;120((7)):933–40. doi: 10.1001/archopht.120.7.933. [DOI] [PubMed] [Google Scholar]
- 4.Paez-Escamilla M, Walter SD, Mohsenin A, Decatur CL, Harocopos GJ, Dubovy S, et al. Intraocular dissemination of uveal melanoma cells following radiotherapy: evolving management over the past decade. Ophthalmic Surg Lasers Imaging Retina. 2019 Sep 1;50((9)):573–9. doi: 10.3928/23258160-20190905-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiratli H, Bilgiç S, Söylemezoglu F, Alaçal S. Peripheral subretinal pigment accumulation following transpupillary thermotherapy for choroidal melanoma. Ophthalmic Surg Lasers Imaging. 2008 Jan-Feb;39((1)):60–2. doi: 10.3928/15428877-20080101-06. [DOI] [PubMed] [Google Scholar]
- 6.Kiratli H, Bilgiç S, Cal P. Intravitreal pigment dispersion as a complication of transpupillary thermotherapy of choroidal melanoma. Retina. 2000;20((4)):408–9. doi: 10.1097/00006982-200004000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Eagle RC, Jr, Shields JA. Pseudoretinitis pigmentosa secondary to preretinal malignant melanoma cells. Retina. 1982;2((1)):51–5. doi: 10.1097/00006982-198200210-00006. [DOI] [PubMed] [Google Scholar]
- 8.Metz CH, Bornfeld N, Metz KA, Gök M. Suspected vitreous seeding of uveal melanoma: relevance of diagnostic vitrectomy. Br J Ophthalmol. 2016 May;100((5)):660–4. doi: 10.1136/bjophthalmol-2014-306443. [DOI] [PubMed] [Google Scholar]
- 9.Masoomian B, Mashayekhi A, Malik K, Shields CL. Intravitreal melphalan for treatment of vitreous seeding from choroidal melanoma. Retin Cases Brief Rep. 2021 Mar 1;15((2)):97–100. doi: 10.1097/ICB.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 10.Hardwig PW, Pulido JS, Erie JC, Baratz KH, Buettner H. Intraocular methotrexate in ocular diseases other than primary central nervous system lymphoma. Am J Ophthalmol. 2006;142((5)):883–5. doi: 10.1016/j.ajo.2006.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.