Abstract
Background/purpose
People who suffer with chronic illness, functional impairment, or cognitive impairment are not easily to visit dental clinics. Domiciliary dental care (DDC) can provide the feasible alternative for these clients. In this study, we first reported the DDC services from a university hospital in central Taiwan from 2010 to 2020.
Materials and methods
This retrospective study collected the DDC data from Department of Dentistry, Chung Shan Medical University Hospital, Taichung, Taiwan. The data including age, sex, geographic locations, place of residence, grade of disability, and type of dental treatment for the patients were obtained and analyzed.
Results
A total of 419 patients (168 females and 251 males) who received dental treatment were included in the study. The average age was 57.4 years old. The total DDC services were up to 2444 visits. The top of place of residence for DDC is patient's home (231/419; 55.13%). Scaling was the most common type of dental treatment for DDC (317/419; 75.67%). The male patients whose age <60 years old had received more DDC (p = 0.002). The profound grade of disability had higher DDC in age <60 years old group (p < 0.001).
Conclusion
Taken together, this study demonstrates the demographic data of DDC in central Taiwan. The results may be valuable for governmental policy to improve the availability of DDC and in turn to facilitate oral health in this specific group of dental patients.
Keywords: Domiciliary dental care, Central Taiwan, Retrospective study
Introduction
People who suffer with chronic illness, functional impairment, or cognitive impairment are not easily to visit dental clinics. In Taiwan, the cases of dental treatment for the disabled are gradually increasing.1,2 In addition to people with disabilities, the dependent elder people also have the same problem. This will be resulted in the reduced access to oral health services. Oral diseases are crucial health concerns for people. Poor oral conditions and periodontal diseases are well-known linked to many systemic diseases.3 This observation presents the considerable challenges for the current dental care system.
Domiciliary dental care (DDC), the so-called home dental care, is characterized by the patient receiving dental healthcare or treatment at home.4 The dentist and oral health professional team travel to see patients in their place of residence such as their house or nursing home to prevent or treat oral health problems. Studies on the survey of DDC in elder population have been conducted in Scotland,4 Finland,5 Japan,6 Australia,7 and Malaysia.8 The education of DDC was not implemented in the of 6-year post-secondary dental curriculum. The dental care of these vulnerable patients poses a challenge for the dentist.
In Taiwan, DDC was first carried out by Chung Shan Medical University Hospital (CSMUH) in March, 2010. At the beginning of 2011, July, DDC has been partly included in Taiwanese National Health Insurance system. However, little is known about the survey of DDC in Taiwan. Therefore, we conducted this retrospective analysis of the demographics and the trends of DDC service from CSMUH.
Materials and methods
Data collection
This retrospective study reviewed and analyzed the data from treatment records of DDC services at the Department of Dentistry, CSMUH, Taichung, between March 2010 and December 2020. Patients with incomplete registered data were excluded from this study. This study received approval from the institutional review board at CSMUH (CS18217). All sensitive patient information was removed before analysis, written informed consent from each of the patients involved was not required according to the institutional review board. The demographic data including annual trends, age, sex, geographic locations, place of residence, grade of disability, and type of treatment for the patients were obtained and analyzed.
Statistical analysis
SPSS version 18 (SPSS, Chicago, IL, USA) was used for all data processing and statistical analyses. Chi-square and Fisher's exact tests were used for categorical variables such as sex, age, place of residence, type of treatment, and grade of disability. Probability levels of <0.05 were considered significant.
Results
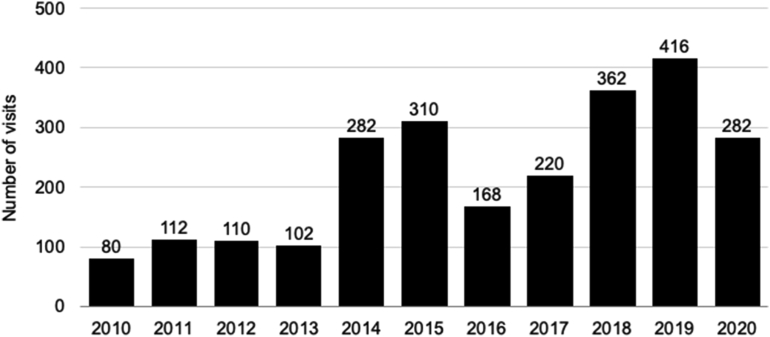
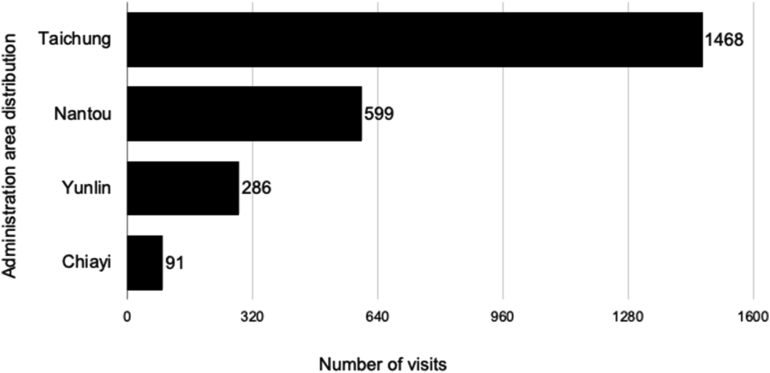
Fig. 1 demonstrates the number of DDC service from 2010 to 2020. The total DDC services were up to 2444 visits. The peak of DDC service number was 416 in 2019. The service number of DDC analyzed by geographic locations is shown in Fig. 2. The population dwelling in Taichung city received the most DDC services with a ratio of approximately 60.07%.
Figure 1.
Annual trend in the number of patients receiving domiciliary dental care.
Figure 2.
The geographic location of domiciliary dental care in Central Taiwan.
The age, sex, place of residence, type of dental treatment, and grade of disability for DDC patients are shown in Table 1. A total of 419 DDC patients (168 females and 251 males) were recruited in the study. The average age was 57.4 ± 21.2 years old. Patient's home was the most common place of DDC (231/419; 55.1%). Scaling was the most common dental treatment for domiciliary dental care (317/419; 75.7%). The grade of profound was the most disability seeking for DDC (291/419: 69.5%).
Table 1.
The demographic characteristics of DDC patients.
| n | % | |
|---|---|---|
| Age | ||
| <60 | 211 | 50.4 |
| ≥60 | 208 | 49.6 |
| Mean ± SD | 57.4 ± 21.2 | |
| Sex | ||
| Female | 168 | 40.1 |
| Male | 251 | 59.9 |
| Place of residence | ||
| Patients home | 231 | 55.1 |
| Vegetative care home | 173 | 41.3 |
| Local hospital | 15 | 3.6 |
| Type of treatment | ||
| Scaling | 317 | 75.7 |
| Extraction | 21 | 5.0 |
| Filling | 2 | 0.5 |
| Others | 79 | 18.9 |
| Grade of disability | ||
| Profound | 291 | 69.5 |
| Moderate/severe | 126 | 30.1 |
| Others | 2 | 0.5 |
The association between age and epidemiology of DDC is shown in Table 2. The male patients age <60 years old had received more DDC (p = 0.002). The place of residence in age <60 years group and age ≥60 years group was vegetative care home and patients home, respectively. For the DDC treatments, the age <60 years group received more scaling treatment and the age ≥60 years group received more tooth extraction treatment (p < 0.001). The patients with profound grade of disability received higher DDC treatments in age <60 years group (p < 0.001).
Table 2.
The association between age and the epidemiology of DDC.
| Age <60 n % | Age ≥60 n % | p value | |
|---|---|---|---|
| Sex | 0.002a | ||
| Female | 69 (32.7) | 99 (46.9) | |
| Male | 142 (67.3) | 109 (51.7) | |
| Place of residence | <0.001a | ||
| Patients home | 81 (38.4) | 150 (72.1) | |
| Vegetative care home | 129 (61.1) | 44 (21.2) | |
| Local hospital | 1 (0.5) | 14 (6.7) | |
| Type of treatment | <0.001b | ||
| Scaling | 183 (86.7) | 134 (63.5) | |
| Extraction | 2 (0.9) | 19 (9.0) | |
| Filling | 2 (0.9) | 0 (0.0) | |
| Others | 24 (11.4) | 55 (26.1) | |
| Grade of disability | <0.001b | ||
| Profound | 179 (84.8) | 112 (53.1) | |
| Moderate/severe | 32 (15.2) | 94 (44.5) | |
| Others | 0 (0.0) | 2 (0.9) | |
Chi-square test.
Fisher's exact test.
Discussion
To the best of our knowledge, this is the first longitudinal study for the DDC survey in Taiwan. A total of 419 patients who received DDC at CSMUH were included in this retrospective study. From the literature review, most DDC studies were focused on the elder group.4,5,7,8 Our findings were in agreement with a survey in Tokyo that the people who received DDC predominantly was the males and age >50 years old.6 The most place of visit was the patients' own house.9,10 However, the most type of DDC service provided in Scotland was the replacement of dentures.4 In Japan, the most common DDC services were removable prosthetic treatment and oral care, followed by dysphagia rehabilitation.10 It is quite different as compared with this study. The reasons might be due to the unique influences of the geographic, cultural, and disability status of the study region.
With an aging population, Taiwan is going to step into the superaged society in 2026.11 The need for care support for dependent older adults is supposed to increase for the general public. DDC may improve the access to dental care for older adults of the community who may find it difficult attending the dental clinic. A well-planned oral health care provision can be adapted to improve access to these individuals who experience poorer oral health and unmet treatment need.
However, the DDC services seem not be expanding. In Japan, DDC provided in Tokyo was demonstrated a relatively low rate: 36.6% in 2006 and 29.2% in 2011.6 In Malaysia, only 36.1% dentists had the experience in providing DDC for elderly people.8 A recent report also demonstrated that more than half of the dental clinics surveyed did not provide DDC in Japan.12 The reasons might be due to complex medical history of this population and dentist's unfavorable working condition. The unfriendly environment leads few dentists to engage in DDC service. From the lesson of these barriers, the service provision models and workforce in Taiwan needs to be considered in the promotion of DDC service.
The implementation of DDC education into dental curriculum is important. In Taiwan, the first author Dr. Yu seems the pioneer to conduct DDC service from 2010. Initiating DDC into dental education was launched in School of Dentistry, Chung Shan Medical University from 2017 in the class of year 102 students. In addition to the traditional clinical skill-oriented competency-based dental education and training,13 the concept of “narrative dentistry” is also conducted into the class of DDC. The narrative dentistry competency can facilitate patient-dentist discourse, structured communication skills, and medical ethics.14,15 Students learn not only delivery DDC service, but also heal patient holistically. Encouraging younger dentist is willing to provide DDC and be a full-time worker in this specialty.
The model of DDC with oral professional team work have been successfully conducted.6,7,16 The results demonstrated that the assistance for maintaining oral hygiene with nursing staff can provide a good level among DDC. Recently, the guideline of DDC in Taiwan also needs two dental professional together either two dentists or dentist with nurse. With the alliance of “team resource management” for patient, it is believed to provide the good quality of DDC.
However, there are some limitations in the present study. Data analysis was based on retrospectively extracted data from patient files. The more detailed data such as beneficiary's medical conditions and social economic status are required to further analysis. The present study might have underestimated the proportion of DDC. Multiple centers or even the nationwide survey are necessary to reflect the whole perspective of DDC in Taiwan. In the opinion of the authors, a risk-benefit assessment should be taken into account before the DDC visit who occur more often with aged and disability population.
In conclusion, within the limitations of this study, we analyzed patients who received DDC in the last 11 years. This data may assist the medical center that performs dental treatments for DDC, as well as help to plan future directions for DDC treatments and establish new policies for DDC.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
This work is supported by a joint grant from Ministry of Education and Chung Shan Medical University. The authors would like to thank all the staffs of CSMUH for participating domiciliary dental care.
References
- 1.Jeng W.L., Wang T.M., Cher T.L., Lin C.P., Jeng J.H. Strategies for oral health care for people with disabilities in Taiwan. J Dent Sci. 2009;4:165–172. [Google Scholar]
- 2.Lin P.Y., Wang K.W., Tu Y.K., Chen H.M., Chi L.Y., Lin C.P. Dental service use among patients with specific disabilities: a nationwide population-based study. J Formos Med Assoc. 2016;115:867–875. doi: 10.1016/j.jfma.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Yang L.C., Yu H.C., Chang Y.C. The recent new findings of periodontal-systemic connection from Taiwan's National Health Insurance Research Database. J Dent Sci. 2021;16:789–790. doi: 10.1016/j.jds.2021.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bedi R., Devlin H., McCord J.F., Schoolbread J.W. Provision of domiciliary dental care for the older person by general dental practitioners in Scotland. J Dent. 1992;20:167–170. doi: 10.1016/0300-5712(92)90131-u. [DOI] [PubMed] [Google Scholar]
- 5.Komulainen K., Ylöstalo P., Syrjälä A.M., et al. Preference for dentist's home visits among older people. Community Dent Oral Epidemiol. 2012;40:89–95. doi: 10.1111/j.1600-0528.2011.00631.x. [DOI] [PubMed] [Google Scholar]
- 6.Hirata S., Sakayori T., Maki Y., Takano N., Ishii T. Factor analysis on implementation of domiciliary dental care in Metropolitan Tokyo. Bull Tokyo Dent Coll. 2013;54:67–72. doi: 10.2209/tdcpublication.54.67. [DOI] [PubMed] [Google Scholar]
- 7.Wright F.A.C., Law G., Chu S.K.Y., Cullen J.S., Le Couteur D.G. Residential age care and domiciliary oral health services: reach-OHT-The development of a metropolitan oral health programme in Sydney, Australia. Gerodontol. 2017;34:420–426. doi: 10.1111/ger.12282. [DOI] [PubMed] [Google Scholar]
- 8.Othman A.A., Yusof Z., Saub R. Malaysian government dentists' experience, willingness and barriers in providing domiciliary care for elderly people. Gerodontol. 2014;31:136–144. doi: 10.1111/ger.12023. [DOI] [PubMed] [Google Scholar]
- 9.Ishimaru M., Ono S., Morita K., Matsui H., Yasunaga H. Domiciliary dental care among homebound older adults: a nested case–control study in Japan. Geriatr Gerontol Int. 2019;19:679–683. doi: 10.1111/ggi.13676. [DOI] [PubMed] [Google Scholar]
- 10.Kamijo S., Sugimoto K., Oki M., Tsuchida Y., Suzuki T. Trends in domiciliary dental care including the need for oral appliances and dental technicians in Japan. J Oral Sci. 2018;60:626–633. doi: 10.2334/josnusd.18-0053. [DOI] [PubMed] [Google Scholar]
- 11.National Development Council . National Development Council; Taiwan: 2016. Population projections for Republic of China (Taiwan): 2016-2060.https://www.mohw.gov.tw/cp-115-33347-2.html Ministry of Health and Welfare. Available online: [Google Scholar]
- 12.Nomura Y., Okada A., Kakuta E., et al. Workforce and contents of home dental care in Japanese insurance system. Int J Dent. 2020;2020:7316796. doi: 10.1155/2020/7316796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu C.M., Huang P.S., Chang Y.C. Perspectives on the challenge and change of COVID-19 crisis on dental education. J Dent Sci. 2021;16:1039–1040. doi: 10.1016/j.jds.2021.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang Y.K., Chang Y.C. Narrative medicine as a good tool for patient-dentist discourse. J Dent Sci. 2021;17:612. doi: 10.1016/j.jds.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang Y.K., Chen Y.T., Chang Y.C. Initiating narrative medicine into dental education: opportunity, change, and challenge. J Formos Med Assoc. 2021 doi: 10.1016/j.jfma.2021.06.008. (In press) [DOI] [PubMed] [Google Scholar]
- 16.Salmi R., Tolvanen M., Suhonen R., Lahti S., Närhi T. Knowledge, perceived skills and activities of nursing staff to support oral home care among older domiciliary care clients. Scand J Caring Sci. 2019;32:1–6. doi: 10.1111/scs.12579. [DOI] [PubMed] [Google Scholar]