Abstract
Background/purpose
Graft bone maturation and remodeling in the maxillary sinus require adequate angiogenesis and osteoprogenitor cells migration from the surrounding bony walls and Schneiderian membrane. This study aimed to evaluate the influence of anatomical factors related to maxillary sinus on the outcomes of transcrestal sinus floor elevation using cone-beam computed tomography (CBCT).
Materials and methods
Forty-five patients (63 elevated sites) were included in this study. CBCT were obtained preoperatively, immediately and 6 months after surgery. The anatomical features of residual bone height, maxillary sinus width, maxillary sinus angle and Schneiderian membrane thickness were measured on preoperative CBCT. Descriptive statistics and correlation analysis were conducted to evaluate the influence of anatomical factors on outcome parameters, including sinus lift height, graft bone resorption and marginal bone loss.
Results
The results showed that there was a positive correlation between sinus width and graft bone resorption. A significantly positive correlation between sinus angle and graft bone resorption was also found.
Conclusion
Our findings indicate that the anatomical factors of maxillary sinus (sinus width and sinus angle) have influence on the linear change of bone grafts after transcrestal sinus floor elevation.
Keywords: Transcrestal sinus floor elevation, Maxillary sinus width, Maxillary sinus angle, Residual bone height, Schneiderian membrane thickness
1. Introduction
Insufficient alveolar bone height resulting from alveolar bone resorption and an increase of sinus pneumatization after tooth loss often limits the placement of dental implants in the posterior maxilla. Maxillary sinus floor elevation is a reliable technique to overcome this problem.
Two approaches have been described for maxillary sinus floor lift: the lateral window approach and the transcrestal technique. Maxillary sinus floor elevation by lateral window approach was proposed by Tatum in 1976 and first published in 1980 by Boyne and James.1 The technique of transcrestal sinus floor elevation (tSFE) was first suggested by Tatum 2 and then developed by Summers.3 Compared with the lateral window approach, tSFE has many advantages, such as minimally invasive, mild postoperative reaction and preservation of bone walls integrity.
No matter which surgical procedure is performed, the aim of maxillary sinus floor elevation is to obtain the vertical height for placing dental implant. Usually, bone grafts were used to maintain the newly formed space below the elevated sinus membrane. The long-term stability of graft bone remains an important factor affecting the success rate of dental implant.4,5
The anatomic features of the maxillary sinus were frequently considered to affect the ease of operation and risk of perforation, thus relating to success rate of augmentation surgery. The presence of maxillary sinus septa increased the risk of membrane perforation during sinus floor augmentation.6 Quite a high risk of membrane perforation occurred in a narrow sinus with an angle less than 30°.7 Recently, some scholars pointed out that anatomical factors also influence the bone remodeling of graft bone in the elevated sinus. The mediolateral distance of the maxillary sinus was negatively associated with the total percentage of vital bone after sinus lift through lateral window technique.8 Our previous study revealed that sinus width also has influence on the resorption of graft bone after tSFE.9 To our knowledge, there are no research with respect to the effect of other anatomical factors on the outcomes of tSFE.
Dental cone-beam computed tomography (CBCT) provides a 3D view on jaw bones and teeth with relatively low radiation dose and high diagnostic information.10 CBCT could be justified for presurgical diagnosis and preoperative planning for dental implant rehabilitation.11 It is suggested that CBCT should be considered the gold standard when evaluating the maxillary sinus.12 In this article, the following anatomical features were evaluated by CBCT:1 residual bone height (RBH);2 maxillary sinus width (SW);3 maxillary sinus angle (SA);4 Schneiderian membrane thickness (MT). The aim of this research is to evaluate the influence of anatomical factors on the outcomes of tSFE.
2. Materials and methods
2.1. Study sample
From March 2015 to December 2018, 45 patients (63 elevated sites) who had undergone tSFE with simultaneous implant placement were included in this study. The inclusion criteria were as follows.
-
1.
RBH ranging from 2 mm to 8 mm.
-
2.
The use of composite graft material consisting of Bio-Oss particles and autogenous bone.
-
3.
No lack of teeth in the opposing jaw so that the same location of the recipient site could be identified on the preoperative and postoperative CBCT images.
-
4.
Healthy maxillary sinus without infection or cyst, no bony septa in the elevated site.
-
5.
Patients have completed the permanent restoration and were followed for at least 1-year after loading.
The present study was conducted in accordance with the fundamental principles of the Helsinki Declaration and approved by the Ethical Committee of our institution for studies involving human subjects. All the selected patients provided informed consent to participate in this study.
2.2. Surgical procedure
All the surgeries were performed by one experienced operator. The surgical processes are briefly described here. Prior to the surgery, patients rinsed with 0.12% chlorhexidine mouthwash for 3 min, and then were performed perioral disinfection with 1% iodophor. After local anesthesia, full-thickness flaps were reflected following a crestal incision. A pilot drill was used to drill to the depth of 1 mm away from the sinus floor, then a series of osteotomes was performed to fracture and elevate the sinus floor. The incidence of membrane perforation was evaluated by the Valsalva maneuver. After filling the composite graft materials consisting of Bio-Oss particles (Geistlich Pharma AG, Wolhusen, Switzerland) and autogenous bone in a 2:1 ratio, implants were placed simultaneously. The mucoperiosteal flap was repositioned and sutured.
All patients received antibiotics including amoxicillin and ornidazole, as well as analgesics. If allergic to amoxicillin, azithromycin can be used instead. Oral hygiene instruction was provided for patients. Sutures were removed 10 days after surgery. After a healing period of 6 months, second-stage surgery was performed.
2.3. Complications recording and implant survival rates
Complications such as infection and implant failure during the healing period were recorded. Biological complications (peri-implant mucositis and peri-implantitis), implant loosening and prosthetic complications after loading were also recorded.
2.4. Radiographic evaluation
For each patient, CBCT examination was performed preoperatively, immediately after surgery, and 6 months after surgery. A CBCT machine (Morita, Tokyo, Japan) was used in the mode at 80 kV and 4.5 mA. The slice thickness was 0.125 mm and the scan time was set at 23.0 s. The following parameters were measured.
-
1.
RBH: the vertical distance from the alveolar crest to the sinus floor.
-
2.
SW: the distance between the lateral and medial wall of maxillary sinus. SW was measured at 5 mm above the sinus floor.
-
3.
SA: the angle between the lateral and medial wall of maxillary sinus. To measure SA, a horizontal line was drawn 10 mm from the sinus floor.
-
4.
MT: the distance from the initial sinus floor to the upper margin of the Schneiderian membrane.
-
5.
Implant protrusion length (IPL): the length of implant protruded into the sinus.
-
6.
Graft height (GH): the height of graft bone between the implant apex and the new sinus floor.
-
7.
Sinus lift height (SLH): the distance between the initial sinus floor to the elevated sinus floor calculated as the sum of IPL and GH.
-
8.
Marginal bone height (MBH): the mean distance from the implant shoulder to the alveolar crest.
-
9.
Graft bone resorption (GR): the difference of GH measured on the day of surgery (GH0) and 6 months after surgery (GH1), calculated as GH0-GH1.
-
10.
Marginal bone loss (MBL): the difference of MBH measured immediately after surgery (MBH0) and 6 months after surgery (MBH1), calculated as MBH0- MBH1.
The precision of the measuring system is 0.01 mm. All parameters were measured on the coronal plane. Preoperative and postoperative scans were adjusted to the same view according to the opposing and adjacent teeth of implant site. The anatomical parameters (RBH, SW, SA, MT) were measured on preoperative CBCT at implant site (Fig. 1). The rest parameters were obtained from the postoperative CBCT scans. Radiographic measurement and analysis were executed by one single trained researcher.
Figure 1.
The investigated anatomical parameters measured on preoperative CBCT. A, residual bone height; B, the width of maxillary sinus; C, the angle of maxillary sinus; D, the thickness of Schneiderian membrane.
2.5. Statistical analysis
All data were analyzed by statistical SPSS software (version 21; SPSS Inc., Chicago, IL, USA). Descriptive statistics (means ± SD) were calculated. The associations of anatomical parameters (RBH, SW, SA, MT) with the outcome parameters (GR, SLH, MBL) were analyzed by Pearson's correlation test. If there is statistical significance, correlation analysis was performed again with grouping according to: 1 implant system; 2 RBH (2 mm ≤ RBH<5 mm, 5 mm ≤ RBH<8 mm). Statistical significance was set at P < 0.05.
3. Results
3.1. Study patients
A total of 63 elevated sites in 45 patients (27 males and 18 females) were included in this study. The average age was 49 years old (ranging from 37 to 63). Among the 63 implants, 9 implants were placed in premolar region, 54 in molar region. The distribution of implants according to their location in the jaw is displayed in Supplementary Fig. 1. Two types of implants (Bicon and ITI) were used in this study. Implant characteristics were displayed in supplementary data.
3.2. Complications and implant condition
No membrane perforation occurred. Patients complained of only slight postoperative swelling and minor discomfort. During 6 months of healing period, no infection or implant failure was recorded. No severe resorption of peri-implant bone was revealed by CBCT. All the implants were successfully in function during 12–37 months follow-up, with a survival rate of 100%.
3.3. Radiographic analysis
RBH ranged from 2.11 mm to 7.64 mm, with a mean value of 4.54 ± 1.56 mm. The mean value of SW was 14.05 ± 2.73 mm, ranging from 7.62 mm to 21.5 mm. SA was 79.15 ± 10.09°, range from 50.05° to 105.3°. The mean value of MT was 1.60 ± 1.13 mm, ranging from 0.31 mm to 4.76 mm.
The mean value of IPL was 3.01 ± 1.24 mm and GH was 2.87 ± 1.11 mm immediately after surgery. SLH amounted to 5.89 ± 1.49 mm immediately after surgery and decreased to 4.41 ± 1.66 mm 6 months after surgery. The mean value of GR was 1.48 ± 0.66 mm. During the 6-month follow-up period, MBL was calculated as 0.49 ± 0.29 mm.
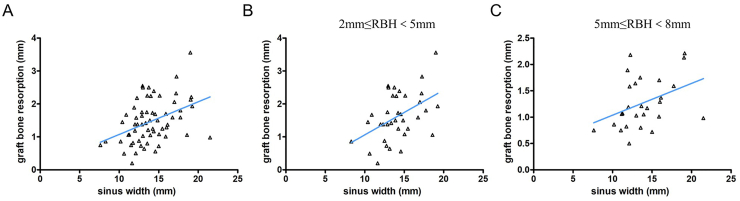
Analysis of the relationship using the Pearson's correlation analysis revealed that there was a positive correlation between SW and GR (r = 0.376, P = 0.001) (Fig. 2). Similarly, a positive correlation exited between SA and GR (r = 0.376, P = 0.002) (Fig. 3). No correlation between RBH and GR was found, neither between MT and GR (Table 1). There was no correlation between anatomical factors and SLH, neither between anatomical factors and MBL.
Figure 2.
Scatter diagrams illustrating the distribution of graft bone resorption relative to sinus width. A, The general distribution without grouping; B, The distribution in the group of 2 mm ≤ RBH<5 mm; C, The distribution in the group of 5 mm ≤ RBH<8 mm.
Figure 3.
Scatter diagrams illustrating the distribution of graft bone resorption relative to sinus angle. A, The general distribution without grouping; B, The distribution in the group of 2 mm ≤ RBH<5 mm; C, The distribution in the group of 5 mm ≤ RBH<8 mm.
Table 1.
Pearson's correlation test of residual bone height, sinus width, sinus angle, Schneiderian membrane thickness and graft bone resorption (n = 63).
| Correlation analysis | GR | |
|---|---|---|
| RBH | r | −0.229 |
| P value | 0.071 | |
| SW | r | 0.413 |
| P value | 0.001∗∗ | |
| SA | r | 0.376 |
| P value | 0.002∗∗ | |
| MT | r | −0.024 |
| P value | 0.855 | |
RBH = residual bone height; SW = sinus width; SA = sinus angle; MT = Schneiderian membrane thickness; GR = graft bone resorption.
∗∗Correlation is significant at level 0.01 (two-tailed).
Categorical analysis of correlation was performed after stratification by RBH (2 mm ≤ RBH<5 mm and 5 mm ≤ RBH<8 mm) and implant system (Bicon and ITI). The results revealed that a positive correlation between SW and GR, as well as between SA and GR in the different groups divided by RBH (Table 2). Categorical analysis of correlation after stratification by implant system showed that a positive correlation between SW and GR, as well as between SA and GR (Table 3).
Table 2.
Pearson's correlation test of sinus width, sinus angle and graft bone resorption based on the classification of residual bone height.
| Anatomical factor | RBH | GR |
||
|---|---|---|---|---|
| n | r | P value | ||
| SW | 2 mm ≤ RBH<5 mm | 36 | 0.465 | 0.004∗∗ |
| 5 mm ≤ RBH<8 mm | 27 | 0.385 | 0.047∗ | |
| SA | 2 mm ≤ RBH<5 mm | 36 | 0.390 | 0.019∗ |
| 5 mm ≤ RBH<8 mm | 27 | 0.438 | 0.022b | |
SW = sinus width; SA = sinus angle; GR = graft bone resorption.
∗∗Correlation is significant at level 0.01 (two-tailed).
∗Correlation is significant at level 0.05 (two-tailed).
Table 3.
Pearson's correlation test of sinus width, sinus angle and graft bone resorption based on the classification of implant system.
| Anatomical factor | Implant system | GR |
||
|---|---|---|---|---|
| n | r | P value | ||
| SW | Bicon | 32 | 0.500 | 0.004∗∗ |
| ITI | 31 | 0.432 | 0.014∗ | |
| SA | Bicon | 32 | 0.423 | 0.018∗ |
| ITI | 31 | 0.386 | 0.032∗ | |
SW = sinus width; SA = sinus angle; GR = graft bone resorption.
∗∗Correlation is significant at level 0.01 (two-tailed).
∗Correlation is significant at level 0.05 (two-tailed).
4. Discussion
The technique of tSFE is considered safe and reliable to gain the vertical bone height for dental implant placement with less complication and discomfort. The maintenance of the space for bone formation is particularly important for the long-term outcome of dental implants placed in the elevated maxillary sinus. Though some clinical trials have reported successful outcomes when performing tSFE without grafting material,13, 14, 15 it was demonstrated that simultaneous placement of an osteoconductive filler at the time of tSFE approach led to improved radiographic outcomes.16 Moreover, grafting materials could play the role of scaffold to maintain the space below the sinus membrane and to promote the endosinus bone gain.17
The maturation of graft materials is a process of osteogenesis and angiogenesis. Blood supply and osteogenic cells coming from the natural bone or mucosa are vital for the formation and remodeling of bone grafts. The bony walls and Schneiderian membrane are important source of blood supply and osteogenic cells.18,19 These are the biological basis for new bone formation in the elevated sinus.
The medial and lateral wall are two important walls for the operation process and healing effect of maxillary sinus lift. In our previous study, it was indicated that SW has a positive correlation with GR in a transcrestal sinus lift.18, 19 A statistically significant correlation of intra-sinus bone loss with wall distance was identified in wide sinuses than in narrow sinuses,20 consistent with our findings. Other scholars also reported that a negative correlation between SW and new bone formation.18,21 The results suggest that the closer between the sinus walls are, the more blood supply to accelerate graft integration with less graft resorption.
The angle between the medial and lateral wall was associated with the incidence of membrane perforation.18, 21 The sites with sharper angles are at a higher risk of membrane perforation.22 To our knowledge, no literature concerned about SA on tSFE outcome was available. In this research, a positive correlation between SA and GR was found, suggesting that more graft bone resorption occurred in a sinus with sharper sinus angle. This can be explained by that a large sinus angle between mesial and lateral sinus wall means a long distance for blood supply transported to the graft bone, leading to a lack of blood supply. The close contact of bony walls with the graft provides fast and predictable colonization of osteogenic cells, as well as ample blood supply, into bone grafts.
RBH is the first included anatomical factor to be considered when planning a maxillary sinus lift. RBH not only determines the primary stability of dental implant, but also influences the choice of surgery treatment. Traditionally, a minimum RBH of 5 mm was required for achieving predictable outcome when performing tSFE. However, recent studies reported that the procedure of tSFE could be reliable and predictable even in the case of RBH less than 5 mm 23, 24, 25 Moreover, RBH is considered to be a factor influencing the bone formation of sinus lift. It was reported that RBH is significantly correlated with graft bone resorption.26 Nevertheless, other study indicated that RBH has no influence on consolidation and maturation of bone graft with a lateral window approach.27 In this study, the mean value of RBH was 4.54 mm, and all cases achieved successful outcome without implant failure. The correlation analysis revealed that there was no significant correlation between RBH and GR.
Schneiderian membrane is one of the most important anatomical factors in maxillary sinus process. Previous studies indicated that Schneiderian membrane contains stem cells with the functional capacity for bone regeneration and can form heterotopic bone.19,28,29 Considering the innate osteogenic potential of Schneiderian membrane and its possible contribution to successful sinus augmentation, we evaluated the influence of Schneiderian membrane thickness on graft bone remodeling in this study. The results showed that there was no significant correlation between MT and GR.
In conclusion, this study revealed a strong correlation between SW and GR, as well as between SA and GR. The results suggest that more bone graft resorption occurred in a sinus with a wide distance and large angle between medial and lateral wall. These findings can provide clinicians with guidance basis for the selection and dosage of bone graft materials when performing tSFE.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
This work was supported by grants from Health Commission Joint Project of Henan Province (LHGJ20200291) and Medical Science and Technology Youth Project of Henan Province (SBGJ202003039).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jds.2021.07.023.
Contributor Information
Anchun Mo, Email: dentistzzu@163.com.
Juanfang Zhu, Email: 805493768@qq.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Supplementary Figure 1.

References
- 1.Boyne P.J., James R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613–616. [PubMed] [Google Scholar]
- 2.Tatum H., Jr. Maxillary and sinus implant reconstructions. Dent Clin. 1986;30:207–229. [PubMed] [Google Scholar]
- 3.Summers R.B. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15(152):154–156. 158 passim; quiz 162. [PubMed] [Google Scholar]
- 4.Hong J.Y., Baek W.S., Cha J.K., Lim H.C., Lee J.S., Jung U.W. Long-term evaluation of sinus floor elevation using a modified lateral approach in the posterior maxilla. Clin Oral Implants Res. 2017;28:946–953. doi: 10.1111/clr.12901. [DOI] [PubMed] [Google Scholar]
- 5.Hatano N., Shimizu Y., Ooya K. A clinical long-term radiographic evaluation of graft height changes after maxillary sinus floor augmentation with a 2:1 autogenous bone/xenograft mixture and simultaneous placement of dental implants. Clin Oral Implants Res. 2004;15:339–345. doi: 10.1111/j.1600-0501.2004.00996.x. [DOI] [PubMed] [Google Scholar]
- 6.Danesh-Sani S.A., Loomer P.M., Wallace S.S. A comprehensive clinical review of maxillary sinus floor elevation: anatomy, techniques, biomaterials and complications. Br J Oral Maxillofac Surg. 2016;54:724–730. doi: 10.1016/j.bjoms.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Cho S.C., Wallace S.S., Froum S.J., Tarnow D.P. Influence of anatomy on Schneiderian membrane perforations during sinus elevation surgery: three-dimensional analysis. Pract Proced Aesthetic Dent PPAD. 2001;13:160–163. [PubMed] [Google Scholar]
- 8.Avila G., Wang H.L., Galindo-Moreno P., et al. The influence of the bucco-palatal distance on sinus augmentation outcomes. J Periodontol. 2010;81:1041–1050. doi: 10.1902/jop.2010.090686. [DOI] [PubMed] [Google Scholar]
- 9.Zheng X., Teng M., Zhou F., Ye J., Li G., Mo A. Influence of maxillary sinus width on transcrestal sinus augmentation outcomes: radiographic evaluation based on cone beam CT. Clin Implant Dent Relat Res. 2016;18:292–300. doi: 10.1111/cid.12298. [DOI] [PubMed] [Google Scholar]
- 10.Yoshimine S., Nishihara K., Nozoe E., Yoshimine M., Nakamura N. Topographic analysis of maxillary premolars and molars and maxillary sinus using cone beam computed tomography. Implant Dent. 2012;21:528–535. doi: 10.1097/ID.0b013e31827464fc. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs R., Salmon B., Codari M., Hassan B., Bornstein M.M. Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Health. 2018;18:88. doi: 10.1186/s12903-018-0523-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lozano-Carrascal N., Salomó-Coll O., Gehrke S.A., Calvo-Guirado J.L., Hernández-Alfaro F., Gargallo-Albiol J. Radiological evaluation of maxillary sinus anatomy: a cross-sectional study of 300 patients. Ann Anat. 2017;214:1–8. doi: 10.1016/j.aanat.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Abi Najm S., Nurdin N., El Hage M., Bischof M., Nedir R. Osteotome sinus floor elevation without grafting: a 10-year clinical and cone-beam sinus assessment. Implant Dent. 2018;27:439–444. doi: 10.1097/ID.0000000000000793. [DOI] [PubMed] [Google Scholar]
- 14.Fermergård R., Åstrand P. Osteotome sinus floor elevation without bone grafts--a 3-year retrospective study with Astra Tech implants. Clin Implant Dent Relat Res. 2012;14:198–205. doi: 10.1111/j.1708-8208.2009.00254.x. [DOI] [PubMed] [Google Scholar]
- 15.Nedir R., Nurdin N., Vazquez L., Abi Najm S., Bischof M. Osteotome sinus floor elevation without grafting: a 10-year prospective study. Clin Implant Dent Relat Res. 2016;18:609–617. doi: 10.1111/cid.12331. [DOI] [PubMed] [Google Scholar]
- 16.Pjetursson B.E., Ignjatovic D., Matuliene G., Brägger U., Schmidlin K., Lang N.P. Transalveolar maxillary sinus floor elevation using osteotomes with or without grafting material. Part II: radiographic tissue remodeling. Clin Oral Implants Res. 2009;20:677–683. doi: 10.1111/j.1600-0501.2009.01721.x. [DOI] [PubMed] [Google Scholar]
- 17.de Melo W.M., de Oliveira F.S., Marcantonio E., Jr., Beloti M.M., de Oliveira P.T., Rosa A.L. Autogenous bone combined with anorganic bovine bone for maxillary sinus augmentation: analysis of the osteogenic potential of cells derived from the donor and the grafted sites. Clin Oral Implants Res. 2014;25:603–609. doi: 10.1111/clr.12100. [DOI] [PubMed] [Google Scholar]
- 18.Lombardi T., Stacchi C., Berton F., Traini T., Torelli L., Di Lenarda R. Influence of maxillary sinus width on new bone formation after transcrestal sinus floor elevation: a proof-of-concept prospective cohort study. Implant Dent. 2017;26:209–216. doi: 10.1097/ID.0000000000000554. [DOI] [PubMed] [Google Scholar]
- 19.Srouji S., Ben-David D., Lotan R., Riminucci M., Livne E., Bianco P. The innate osteogenic potential of the maxillary sinus (Schneiderian) membrane: an ectopic tissue transplant model simulating sinus lifting. Int J Oral Maxillofac Surg. 2010;39:793–801. doi: 10.1016/j.ijom.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 20.Spinato S., Bernardello F., Galindo-Moreno P., Zaffe D. Maxillary sinus augmentation by crestal access: a retrospective study on cavity size and outcome correlation. Clin Oral Implants Res. 2015;26:1375–1382. doi: 10.1111/clr.12477. [DOI] [PubMed] [Google Scholar]
- 21.Cheng X., Hu X., Wan S., Li X., Li Y., Deng F. Influence of lateral-medial sinus width on No-grafting inlay osteotome sinus augmentation outcomes. J Oral Maxillofac Surg. 2017;75:1644–1655. doi: 10.1016/j.joms.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 22.Velloso G.R., Vidigal G.M., Jr., de Freitas M.M., Garcia de Brito O.F., Manso M.C., Groisman M. Tridimensional analysis of maxillary sinus anatomy related to sinus lift procedure. Implant Dent. 2006;15:192–196. doi: 10.1097/01.id.0000223233.29454.77. [DOI] [PubMed] [Google Scholar]
- 23.Teng M., Liang X., Yuan Q., et al. The inlay osteotome sinus augmentation technique for placing short implants simultaneously with reduced crestal bone height. A short-term follow-up. Clin Implant Dent Relat Res. 2013;15:918–926. doi: 10.1111/cid.12088. [DOI] [PubMed] [Google Scholar]
- 24.Gonzalez S., Tuan M.C., Ahn K.M., Nowzari H. Crestal approach for maxillary sinus augmentation in patients with ≤ 4 mm of residual alveolar bone. Clin Implant Dent Relat Res. 2014;16:827–835. doi: 10.1111/cid.12067. [DOI] [PubMed] [Google Scholar]
- 25.Gu Y.X., Shi J.Y., Zhuang L.F., Qian S.J., Mo J.J., Lai H.C. Transalveolar sinus floor elevation using osteotomes without grafting in severely atrophic maxilla: a 5-year prospective study. Clin Oral Implants Res. 2016;27:120–125. doi: 10.1111/clr.12547. [DOI] [PubMed] [Google Scholar]
- 26.Galindo-Moreno P., Fernández-Jiménez A., O'Valle F., et al. Marginal bone loss in implants placed in grafted maxillary sinus. Clin Implant Dent Relat Res. 2015;17:373–383. doi: 10.1111/cid.12092. [DOI] [PubMed] [Google Scholar]
- 27.Avila-Ortiz G., Neiva R., Galindo-Moreno P., Rudek I., Benavides E., Wang H.L. Analysis of the influence of residual alveolar bone height on sinus augmentation outcomes. Clin Oral Implants Res. 2012;23:1082–1088. doi: 10.1111/j.1600-0501.2011.02270.x. [DOI] [PubMed] [Google Scholar]
- 28.Graziano A., Benedetti L., Massei G., Cusella de Angelis M.G., Ferrarotti F., Aimetti M. Bone production by human maxillary sinus mucosa cells. J Cell Physiol. 2012;227:3278. doi: 10.1002/jcp.24022. 81. [DOI] [PubMed] [Google Scholar]
- 29.Guo J., Weng J., Rong Q., et al. Investigation of multipotent postnatal stem cells from human maxillary sinus membrane. Sci Rep. 2015;5:11660. doi: 10.1038/srep11660. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.