Abstract
The way in which health care is delivered has rapidly changed since the onset of the COVID-19 pandemic, with a rapid increase in virtual delivery of clinical care. As a result, the learning environment (LE) in health professions education, which has traditionally been situated in the bricks-and-mortar clinical context, now also requires attention to the virtual space. As a frequently examined topic in the health professions literature, the LE is a critical component in the development and training of future healthcare professionals. Based on a published conceptual framework for the LE from Gruppen et al. in 2019, a conceptual framework for how the LE can manifest through virtual care space is presented here. The four components of personal, social, organizational, physical/virtual spaces are explored, with a discussion of how they can be integrated into virtual care. The authors provide suggestions that health professions educators can consider when adapting their LE to the virtual environment and highlight aspects of its integration that require further research and investigation.
Abstract
La prestation des soins de santé a connu un changement fulgurant depuis le début de la pandémie de la COVID-19, notamment en raison de la virtualisation des soins cliniques. Par conséquent, l’environnement d’apprentissage (EA) qui, dans l’enseignement traditionnel des professions de la santé, se situait dans un cadre clinique physique, doit désormais inclure l’espace virtuel. Sujet souvent exploré dans la littérature en sciences de la santé, l’environnement d’apprentissage est un élément essentiel de la formation des futurs professionnels de la santé. Nous proposons un cadre conceptuel, inspiré du cadre de l’EA élaboré par Gruppen et al. en 2019, sur la façon de définir un EA dans l’espace de soins virtuel. Après avoir exploré les quatre dimensions de l’espace, à savoir personnelle, sociale, organisationnelle et physique/virtuelle, les auteurs analysent la façon de les intégrer dans les soins virtuels. Ils formulent des suggestions à l’intention des enseignants des professions de la santé concernant l’adaptation de leur environnement d’apprentissage à l’environnement virtuel, tout en soulignant les aspects d’une telle intégration qui nécessitent des recherches plus approfondies.
Introduction
Virtual Care
Physical distancing measures due to COVID-19 around the world have necessitated a rapid shift of unprecedented magnitude to virtual delivery of clinical care.1,2 One recent report suggests that in the United States, due to physical distancing requirements of the pandemic, 46% of patients are now using virtual care, up from 11% in 2019. Clinicians have also seen a large uptake of virtual care, with estimates showing that providers are seeing 50 to 175 times the number of patients virtually now compared to before the pandemic.3
The terms ‘virtual care’ and ‘telehealth’ are often found together. While some sources use them interchangeably,4,5 others highlight some small differences between them.6 For the purposes of this paper, we use the term ‘virtual care’ as an umbrella term, which we define as using technology (e.g. live video, audio, and instant messaging) to provide clinical care to patients.
Virtual care has slowly been making its way into clinical education.7 Although virtual care has existed for many years, the recent increase due to COVID-19 is expected to continue even after physical distancing protocols have relaxed.8,9 This may be due to the increased convenience of virtual care for patients and the fact that some patients may not feel entirely safe or confident about in person care even after COVID-19 starts to resolve. Additionally, virtual care provides improved efficiency in healthcare delivery leading to better health outcomes and the ability to provide access to rural or underserved areas.7,10,3 The integration of learners into this environment is therefore essential to ensure the continuity of their clinical experiences as well as to prepare them to be providers of virtual care in the future; health professional education programs have therefore begun more rapidly to integrate learners into virtual care modalities.11
In Canada, various changes to medical education have been implemented, including a call for continuing advances in virtual care.12 One published example from a surgical post-graduate education program in the United States demonstrates how trainees can be engaged in the provision of virtual care as well as conferencing encounters with the attending physician and the patient through a variety of interactions and platforms in a triangulated manner.13 These strategies create meaningful ways for learners to continue their clinical education despite physical distancing requirements of COVID-19 while simultaneously providing medical learners necessary skills in virtual care for their future careers.
Both medical students and employees of a medical university felt a lack of familiarity with the concept of virtual care, and were not sufficiently informed.14 While a transition to virtual care learning may be intimidating to the uninitiated stakeholders, some virtual care curricula have shown promise.15 The successful implementation of virtual care into the LE is crucial to position virtual care as an emerging public health service and therefore needs to continue. As virtual care becomes a more accepted mode of care, it is imperative that graduating students are competent practicing in this environment.
Learning environment
The Learning Environment (LE) is a critical component in education that aims to optimize the ability of students to learn. When students view the LE as positive and supportive, it allows them to learn better.16 Ideally, these are environments in which students trust others, tackle challenges, ask questions, feel a sense of belonging, and grow and develop their professional identities.17
Several frameworks conceptualize the LE using various components and dimensions. These frameworks are useful for clinicians, health professions educators, patients, and learners to identify and analyze problems in the LE, and then improve ways the LE functions.18 The construction of traditional clinical LEs (e.g. patient bedside, outpatient clinic encounters, and surgical encounters) are generally intuitive for clinician educators as they are the same LEs in which the clinicians themselves trained and practice. However, the LE in virtual care may be novel to practicing clinicians, and many existing frameworks do not consider the emerging presence of virtual care in medical education. As a result, there has been a call for a swifter transition toward virtual care in medical education, which will help future doctors prepare for the present challenges with COVID-19 and future pandemics.19 Virtual LEs may be challenging or intimidating to many practicing clinicians involved in education, as they may be a new medium both for clinical care and for clinical teaching. Practical tips and guidance have begun to emerge to help physicians to succeed in this environment.20 We suggest that medical schools may need to add new elements to the construct of the virtual LE for the benefit of all – patients, clinicians, and learners.
Purpose
Our purpose is to discuss the application of an existing clinical LE framework18 to the virtual clinical learning space, and to describe how educators can use this framework to enhance the LE within which virtual care education takes place. Additionally, we will discuss issues that clinicians should consider in the design of their virtual LE and gaps that exist in understanding how the virtual LE affects health professional education that might provide opportunities for further scholarship. This study was exempt from research ethics board review.
Framework
A recent review conducted for a Josiah Macy Jr. Foundation consensus conference18 identified four overlapping and interactive core components: personal, social, organizational, and physical and virtual spaces.18 We will discuss these four components below along with considerations for expansion of the learning environment to include virtual care. Figure 1 shows the adapted framework.
Figure 1.
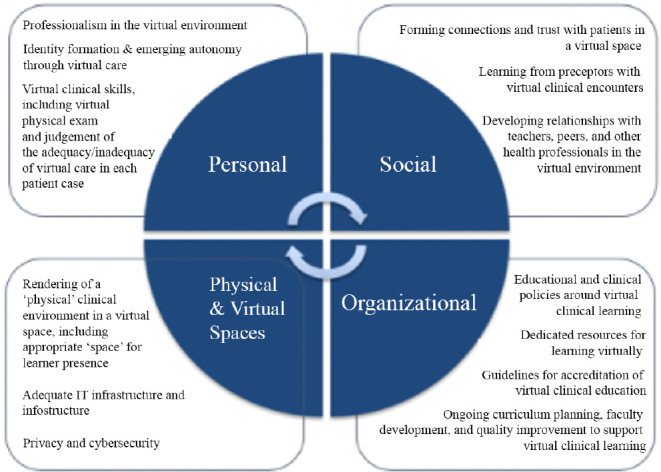
Learning environment framework for virtual care Adapted from Gruppen et al. 201818
Personal component
The personal component of the LE describes how the individual learner interacts with the LE through activity, develops perceptions of the LE, and engages in personal growth through clarity about goals and selection of relevant and meaningful learning, and through this process develops a professional identity and increasing autonomy.18 The virtual space can still allow for these processes; therefore, learner growth, professional identity formation, and autonomy can continue to be viewed as a meaningful adjunct to the traditional LE. Aspects of the personal component may not significantly change when transitioning to a virtual space given that it is focused primarily on the individual’s own growth and mindset. However, this personal growth is inseparably linked to other components such as the social and organizational aspects of the virtual LE that also enable identity formation and autonomy. As a result, specific care and attention needs to be directed to how the personal component could change in this environment–specifically, how growth/development and professional identity development occur differentially compared to the traditional LE’s. For instance, the virtual LE also allows learners to develop a sense of the limitations to virtual care and understanding when clinical diagnoses require an in-person physical examination. Learning how to navigate this clinical gap when treating and advising patients on a virtual platform is an important aspect of personal development within the virtual LE.
Specific recommendations to enhance the personal component of the LE may include incorporating journaling and reflection into virtual care visits, which will encourage students to reflect on the limitations of virtual care and engage in continuous quality improvement. Students and clinicians can co-create specific checklists of physical exam maneuvers that can be performed virtually (e.g. in the context of a specific patient), which would also assist in furthering their understanding of both the opportunities and limitations of virtual care. Additionally, virtual care can easily allow for the video recording of a clinical encounter, which can become a teaching tool for students in reviewing and identifying specific feedback points for themselves, assisting with personal growth. Medical students resonate strongly with timely and constructive feedback, which they feel is one of the most useful tools to improve their learning of clinical history taking.21
Social component
The original review paper defined the social component as learners engaging with others and navigating multiple relationships, shaping their perceptions of and experiences with the LE.18 This can arise from peer-to-peer relationships via competition, cooperation, shared values and learner culture, learner-to-faculty/staff relationships via trust, feedback, communication, instructional strategies, mentoring, and finally learner-to-patient relationship via responsibility, acceptance, and trust. These social relationships all affect the manner in which students learn in their LE.18
In transitioning this to a virtual care space, the LE needs to continue to allow space for learners to meaningfully form relationships, although the nature of these relationships may be different. Learner-patient relationships can be built when learners actively participate in a virtual clinic (e.g. with activities such as taking a history that build rapport with patients). Further, particularly if acting as a first point of contact, learners would have the opportunity to cultivate empathy for patients who also may not be as familiar with virtual environments in health care. Learner-preceptor relationships might also be built through activities such as pre-encounter discussions of learning goals, or post-encounter review and feedback conversations that can also occur virtually. Through these, learners can further their understanding of how to work within a team of healthcare professionals to prioritize patient centered care in a virtual environment.13
Peer relationships might take form through dedicated online platforms for peer-to-peer communication. For example, a post-graduate surgical education program created a closed Facebook group specific for residents in response to changes from the COVID-19 pandemic to discuss practice questions and surgical topics online; a survey of the participants found that 100% reported that the platform was helpful and 95% were likely to use it in the future as preparation for their surgery board examinations.13 These types of platforms and interventions can be used to foster and maintain the peer-to-peer relationships that would have formed in an in-person LE.
Specific recommendations to enhance the social component of the LE could include allowing educators to actively identify and foster opportunities for social interaction within the virtual space (including peer-to-peer, learner-to-faculty, learner-to-patient), and ensuring that ample and equal opportunities to foster these relationships are created throughout the learner’s educational experience. Actively including the learner in a virtual care visit has been identified as a useful tip in teaching within the virtual space.22 Program evaluation focusing on these various relationships would help identify deficiencies and create avenues to allow for these relationships to form.
Further inquiry into the nature and impact of virtual relationships requires additional investigation. For example, a pre-existing relationship (e.g. between student and patient, or student and clinician) prior to providing virtual care may provide a very different dynamic compared to a relationship formed solely in the virtual space. Continued understanding of how relationships can be supported/nurtured is needed to better understand the social component of the virtual care LE.
Organizational component
The original review paper proffered that the organizational component of the LE emphasizes how individuals interact with policies and navigate organizations that provide performance measures, structural/learning changes, or rules and resources. Specifically, this involves guidance and support for learning, curriculum resources, geographic placements, accreditation rules, as well as organizational practices (such as duty hours, teacher control, placements, and technology infrastructure).18 The Clinical Learning Environment Review (CLER) adopted by the Accreditation Council for Graduate Medical Education (ACGME) is an example of a policy within the organizational component.23 The CLER program is designed to guide and improve how clinical sites engage with resident and fellow physicians to provide safe, high quality patient care.23 Another example involves the Canadian transition to Competency-Based Medical Education (CBME), which reforms postgraduate training to ensure physicians graduate with defined competencies.24
Any of these policies that govern overall healthcare processes and healthcare education will require adaptation to the virtual space. For instance, initiatives such as CBME could require the addition of a ‘virtual care’ competency, or the recognition that certain competencies should be also taught in a virtual capacity. Health professional practice policies placed by state medical boards in the United States or provincial medical regulatory authorities in Canada may provide practice recommendations on virtual care, which may be relevant to learners starting to transition to solo practice. Finally, health system enabling policies that are informed by clinical care such as government health professional acts or national online privacy acts (building off of acts such as the Health Insurance Portability and Accountability Act, or HIPAA)25 will need to be introduced into the virtual LE to ensure early understanding and adoption of appropriate practices as learners develop their professional culture within virtual healthcare. This introduction will require thoughtful curriculum planning (including assessment tools/strategies) as well as faculty development for implementation. Finally, additional resources would have to be created for technology-troubleshooting, as training to interact in a virtual space may result in ongoing technical difficulties that could hinder healthcare team function and therefore learning.
Significant resources have started to become available to help provide clinicians practical insights into involving learners in virtual care, including a Virtual Care Playbook from the Canadian Medical Association10, among others from various medical and academic institutions.8,9,26,27,28,29 However, there is minimal published literature on the principles of these curricula, how to adapt assessment tools/strategies, and how to include patient perspectives in these interventions. Faculty development strategies will also be required to both gather perspectives and provide support to clinicians practicing in the virtual care arena. Administrative policies will also be necessary to establish clear expectations of teachers and learners within virtual care and endorse the contribution of virtual care to clinical education, similar to how this is established with in-person clinical placements.
Specific recommendations within the organizational realm might include advocacy from educators addressing how administrative policies can adapt to and support the shift to virtual care. Dedicating administrative efforts to specifically ensure a smooth transition to virtual care would be an effective way to ensure nothing is overlooked within organizational policies. Additionally, engaging with all relevant stakeholders (educators, learners, patients, and senior administrative staff) could help to better inform the best way in which organizational practices can be shifted to a virtual setting for all participants.
Physical and virtual spaces
The final component of the LE framework includes the space that health professional learners are placed in; traditionally, health professional learners are placed in a specific physical environment to promote learning, of which the virtual space often involved mostly informational infrastructure and digital resources (such as electronic health records or other online educational resources). However, since the recent boom in virtual care, the design of the ‘physical environment’ of the virtual care platform/encounter must be given deliberate attention to maximize learning.
The physical and virtual set-up of the virtual encounter environment is important and with its many permutations, it may affect the relationships between parties, the role of each participant, the clinical teaching/learning, etc. There are many possible permutations of the physical set-up in virtual care (e.g. learner/preceptor in the same physical room with a ‘virtual’ patient; preceptor, learner, and patient all ‘virtual’; etc.).10 In addition, the geographic location of each party may also vary: learners/preceptors/patients may be in a hospital, a clinic, another designated location, or even in their own home. With regards to the virtual logistics of the learner’s role in the visit, there are equally many possibilities: the learner may play a more passive role (e.g. as an observer in the virtual ‘room’), or a more active role (e.g. the learner is given time to interview/examine the patient before the preceptor ‘arrives’, or the preceptor is a silent observer ‘in the room’). How the physical and virtual space is organized will ostensibly also have a significant impact on the clinical learning that ensues.
The virtual space is clearly the most transformed component of the original framework. Previously, the material aspect simply considered the adequacy of a virtual space for online learning, not patient care. However, with this expansion of scope, there are many other attributes of the virtual space that may need further exploration – e.g. the adequacy of Information Technology (IT) infrastructure (e.g. health record access for learners, various virtual care IT platforms), the layout of the virtual space during a patient encounter (e.g. can all participants in a virtual encounter see each other at the same time? Who else is permitted ‘in the room’?) Many of these important dimensions of virtual spaces have yet to be discussed and researched. Involving the views of all stakeholders (including patients) will be integral to achieving a positive LE for all of these groups.
Additionally, each of the four components of the LE are interdependent with one another. The virtual space, as the platform through which every other LE component is translated, is affected by each of the other components. For instance, in the personal component, increasing autonomy will need to be negotiated with the clinician-teacher and will impact the setup of the virtual care space and the flow of communication between patient/clinician/learner. In turn, this change in virtual care space and communication flow will also affect the relationship formation between both learner/clinician and learner/patient. Specific attention will thus need to be directed towards understanding how these relationships form in order to support meaningful development.
Further, given the emerging concept of virtual care, many IT platforms are often focused primarily on delivering care and service to patients from a single clinician; affordances that allow a space for learners need consideration and planning as well. For instance, making use of existing infrastructure within a platform to allow for a three-way call would permit a learner and supervising clinician to be simultaneously present during a virtual patient encounter.
Specific recommendations to enhance the physical and virtual spaces component of the LE could involve setting clear expectations between supervisors and students in terms of who is “present” and in what role; having students intentionally experience a variety of different setups may also provide learning in different ways (e.g. watching the ‘expert’ take a focused history versus having the space to do it oneself). Additionally, educator advocacy to increase the use of existing technology infrastructure (e.g. breakout rooms to debrief, virtual whiteboards for patient education, or allowing multiple callers at once to facilitate team care) will be very important to maximize the efficiency of available technology for both patient care and learning.
Conclusion
As health practices must adapt to the COVID-19 pandemic, so must the health professional LE pivot to prepare the current and future workforce to this changing landscape. It is essential to appropriately structure and develop an optimized LE that is tailored to a virtual clinical setting for patients, learners, and educators.
The adapted framework we presented in this paper starts this important conversation by presenting considerations involved with the integration of virtual care into the health professional LE, while also providing recommendations on ways to enhance the LE in transitioning to a virtual environment. Catapulted forward by the COVID-19 pandemic, virtual care is growing increasingly popular throughout the world and is likely here to stay; this framework not only serves as a useful guide to begin shaping the LE in virtual care, but also illuminates the important scholarship and research opportunities that can further help optimize the virtual learning environment.
Conflicts of Interest
None
Funding
None
References
- 1.Codispoti CD, Bandi S, Moy JN, Mahdavinia M. Running a virtual allergy division and training program in the time of COVID-19 pandemic. J. Allergy Clin. Immunol. 2020;145(5):1357-1359. 10.1016/j.jaci.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kohan L, Sobey C, Wahezi S, et al. Maintaining high quality multidisciplinary pain medicine fellowship programs: Part II: Innovations in clinical care workflow, clinical supervision, job satisfaction and postgraduation mentorship for pain fellows during the Covid-19 pandemic. Pain Med. May 7, 2020:pnaa176. 10.1093/pm/pnaa176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bestsennyy O, Gilbert G, Harris A, Rost J. Telehealth: a quarter-trillion-dollar post-COVID-19 reality? McKinsey & Company. May 29, 2020.https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality [Accessed on Nov 30, 2020]
- 4.Medisys. 6 things you need to know about telemedicine and telehealth companies Canada. https://blog.medisys.ca/things-you-need-to-know-about-telemedicine-telehealth-companies-canada [Accessed on July 11, 2020].
- 5.Sharrat A. What are telemedicine and virtual care? Lumino Health. https://luminohealth.sunlife.ca/s/article/What-are-telemedicine-and-virtual-care?language=en_US [Accessed on July 11, 2020].
- 6.Riopel L. What is virtual care and how to apply it in your practice? PositivePsychology.com. Oct 28, 2019. https://positivepsychology.com/virtual-care/ [Accessed on July 11, 2020].
- 7.Hersh W. The telemedicine curriculum. J Telemed Telecare. 2003;9(6):353-354. 10.1258/135763303771005298 [DOI] [PubMed] [Google Scholar]
- 8.Affleck E, Hedden D, Osler G. Virtual care: recommendations for scaling up virtual medical services. Canadian Medical Association; 2020. [Google Scholar]
- 9.Doctors of BC . The Doctor Is In: recommendations for expanding in-person care in physician practices. https://www.doctorsofbc.ca/sites/default/files/recommendations_for_expanding_in-person_care_in_community_practice.pdf [Accessed on Nov 30, 2020] [Google Scholar]
- 10.Mark D. Virtual Care Playbook. Canadian Medical Association; 2020.
- 11.Mian A, Khan S. Medical education during pandemics: a UK perspective. BMC Med. 2020;18(1):100. 10.1186/s12916-020-01577-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehta N, Sayed C, Sharma R, Do V. Medical education advances and innovations: a silver lining during the COVID-19 pandemic. Can Med Ed J. Oct 10, 2020. 10.36834/cmej.70926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chick RC, Clifton GT, Peace KM, et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. Apr 2020:S1931720420300842. 10.1016/j.jsurg.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wernhart A, Gahbauer S, Haluza D. eHealth and telemedicine: practices and beliefs among healthcare professionals and medical students at a medical university. Helve O, ed. PLoS ONE. 2019;14(2):e213067. 10.1371/journal.pone.0213067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afshari M, Witek NP, Galifianakis NB. Education research: an experiential outpatient teleneurology curriculum for residents. Neurology. 2019;93(4):170-175. 10.1212/WNL.0000000000007848 [DOI] [PubMed] [Google Scholar]
- 16.Dorman JP, Aldridge JM, Fraser BJ. Using students’ assessment of classroom environment to develop a typology of secondary school classrooms. Intern Educ J. 2006;7(7). [Google Scholar]
- 17.Bucholz JL, Sheffler JL. Creating a warm and inclusive classroom environment: planning for all children to feel welcome. Electronic Journal for Inclusive Education. 2009; 2(4). [Google Scholar]
- 18.Gruppen LD, Irby DM, Durning SJ, Maggio LA. Conceptualizing learning environments in the health professions: Acad Med. 2019;94(7):969-974. 10.1097/ACM.0000000000002702 [DOI] [PubMed] [Google Scholar]
- 19.Jumreornvong O, Yang E, Race J, Appel J. Telemedicine and Medical Education in the Age of COVID-19. Acad Med. 2020;95(12):1838-1843. 10.1097/ACM.0000000000003711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rashid M, Foulds J, Forgie S. Practical tips on incorporating learners into virtual clinical care. MedEdPublish. 2020;9(1). 10.15694/mep.2020.000167.1 [DOI] [Google Scholar]
- 21.Ellard OB, Whiteman E, Brandstatter E, Cleere R. Medical students’ opinion on tips for telemedicine teaching. Med Teach. May 13, 2021:1-1. 10.1080/0142159X.2021.1923683 [DOI] [PubMed] [Google Scholar]
- 22.Hovaguimian A, Joshi A, Onorato S, Schwartz AW, Frankl S. Twelve tips for clinical teaching with telemedicine visits. Med Teach. Feb 8, 2021:1-7. 10.1080/0142159X.2021.1880558 [DOI] [PubMed] [Google Scholar]
- 23.Accreditation Council for Graduate Medical Education . Clinical Learning Environment Review (CLER). https://www.acgme.org/What-We-Do/Initiatives/Clinical-Learning-Environment-Review-CLER [Accessed July 11, 2020].
- 24.Royal College of Physicians and Surgeons of Canada . Competency by Design. 2020. http://www.royalcollege.ca/rcsite/cbd/competence-by-design-cbd-e [Accessed on Nov 30, 2020].
- 25.HHS.gov . Health information privacy. Aug 26, 2015. https://www.hhs.gov/hipaa/index.html [Accessed May 16, 2021].
- 26.Oandasan I, Cavett T, Singer A, Wolfrom B. Tips for supervising family medicine learners providing virtual care. College of Family Physicians of Canada; 2020.
- 27.Academy of Communication in Healthcare . COVID-19 telehealth relationship-centered communication skills. 2020. https://www.achonline.org/COVID-19/Telemedicine
- 28.University of British Columbia Department of Family Practice . UBC family practice: teaching in turbulent times. 2020. [Google Scholar]
- 29.University of Saskatchewan Faculty Development . Virtual visit guidelines. 2020. https://medicine.usask.ca/facultydev/clinical_resources/virtual-care.php#VirtualVisitGuidelines [Accessed on Nov 30, 2020].


