Abstract
Background
Osteoarthritis (OA) of the hip is a progressive condition that has no cure and often requires a total hip arthroplasty (THA). The principal methods for THA are the posterior and direct lateral approaches. The posterior approach is considered to be easy to perform, however, increased rates of dislocation have been reported. The direct lateral approach facilitates cup positioning which may decrease rates of hip dislocation and diminishes the risk of injury to the sciatic nerve. However, there is an increased risk of limp. Dislocation of a hip prosthesis is a clinically important complication after THA, in terms of morbidity implications and costs.
Objectives
To determine the risks of prosthesis dislocation, postoperative Trendelenburg gait and sciatic nerve palsy after a posterior approach, compared to a direct lateral approach, for adult patients undergoing THA for primary OA and to update the previous review made in 2003.
Search methods
MEDLINE, EMBASE, CINAHL and Cochrane databases were searched and updated, from the previous search of 2002, to Oct 13, 2005. No language restrictions were applied.
Selection criteria
Published trials comparing posterior and direct lateral surgical approaches to THA in participants 18 years and older with a diagnosis of primary hip OA.
Data collection and analysis
Retrieved articles were assessed independently by the two reviewers for their methodological quality.
Main results
Four prospective cohort studies involving 241 participants met the inclusion criteria. The primary outcome, dislocation, was reported in two studies. No significant difference between posterior and direct lateral surgical approach was found [1/77 (1.3%) versus 3/72 (4.2%); relative risk (RR) 0.35; 95% confidence intervals (CI) 0.04 to 3.22]. The presence of postoperative Trendelenburg gait was not significantly different between these surgical approaches. The risk of nerve palsy or injury (all nerves taken together) was significantly higher among the direct lateral approaches [1/43 (2%) versus 10/49 (20%); RR 0.16, 95% CI 0.03 to 0.83]. However, there were no significant differences when comparing this risk nerve by nerve for both approaches, in particular for the sciatic nerve. Of the other outcomes considered only the average range of internal rotation in extension of the hip was significantly higher (weighted mean difference 16 degrees, 95% CI 8 to 23) in the posterior approach group (mean 35°, standard deviation 13°) compared to the direct lateral approach (mean 19°, standard deviation 13°).
Authors' conclusions
The quality and quantity of information extracted from the trials performed to date are insufficient to make any firm conclusion on the optimum choice of surgical approach in adult patients undergoing primary THA for OA.
Plain language summary
Total hip arthroplasty for osteoarthritis
This summary of a Cochrane review presents what we know from research about the effects of a posterior or lateral approach in total hip replacement surgery for osteoarthritis. The review shows that:
In people with osteoarthritis of the hip, there is not enough evidence to be certain about whether the posterior (back) or the lateral (side) approach to total hip replacement surgery is better.
What is osteoarthritis of the hip and what types of total hip replacement surgery are there? Osteoarthritis (OA) is the most common form of arthritis that can affect the hips. In some people, the damage and pain in the hip may be severe enough for surgery. In these people, the whole hip joint can be replaced by an artificial joint with total hip replacement surgery.
In total hip replacement surgery, the surgeon can make the cut from the posterior (back) or lateral (side) of the hip. Some surgeons believe that the posterior approach is better because people may have less problems walking after surgery. Other surgeons believe that the lateral approach is better because people may have less chance of nerve damage and less chance of dislocating their hip after surgery. Dislocating a hip causes pain and people may need to go to hospital to put the hip back in place.
What are the results of this review? People in the studies had total hip replacement surgery that was either done from the posterior (back of the hip) or from the lateral (side of the hip).
Benefits of posterior and lateral approach In people who had total hip replacement surgery:
the posterior approach may improve range of motion more than the lateral approach the posterior and lateral approaches may improve function about the same
But there is not enough evidence to be certain about these benefits. Harms of posterior and lateral approach In people who had total hip replacement surgery:
the chance of dislocating the hip after surgery may be about the same with either the posterior or lateral approach the chance of having difficulty walking may be about the same with either the posterior or lateral approach the posterior approach may cause less nerve damage than the lateral approach
But there is not enough evidence to be certain about these harms.
Background
Osteoarthritis affects 10% of the population, and mainly weight‐bearing joints such as the hips (5%) (Hoaglund 2001; Arthritis Soc. 2005). Osteoarthritis of the hip is characterized by loss of articular cartilage of the hip joint. It may be primary, i.e. idiopathic, or secondary i.e. following hip diseases during childhood, trauma, osteonecrosis, previous joint infection or other conditions (Greene 2001). Osteoarthritis of the hip is a progressive condition that has no cure. The usual clinical course is deteriorating gait, increasing pain and stiffness that will ultimately require a total hip arthroplasty (THA) (2.5% of people 40 years to 84 years of age) (Oishi 1998). A THA refers to replacement of both parts of the hip joint (acetabulum and femoral head) with prosthetic implants (cup, head and stem).
Many different surgical approaches to the hip have been described. Currently, the principal methods for THA are the posterior and direct lateral approaches (Brown 1995; Byström 2003). The posterior approach entails a curved incision centered on the posterior aspect of the greater trochanter. The fascia lata is incised in line of the incision and the fibers of the gluteus maximus split by blunt dissection. The short external rotators are then detached close to their femoral insertion and reflected exposing the posterior aspect of the hip joint capsule. The capsule can be either incised or excised, although most surgeons are preserving it (Moore 1959). The direct lateral approach entails a longitudinal skin incision centered over the greater trochanter. The gluteal fascia and iliotibial band are exposed and divided in the line of the incision. The insertion of the gluteus medius is incised down to the bone, prolonged distally through the vastus lateralis and medially with the insertion of the anterior portion of the gluteus minimus. The capsule of the hip comes into view and can be either incised or excised (Hardinge 1982).
The posterior approach is generally considered to be easy to perform, using less extensive tissue dissection which gives shorter operation times and less blood loss. It allows a good exposure of the femur that may reduce the risk of femoral fracture during the procedure. It is considered to be associated with less problems with gait since the abductor muscles are not dissected. However, it is often more difficult to see the acetabulum and increased rates of dislocation have been reported (Woo 1982; Paterno 1997; Li 1999).
The advantages proposed for the direct lateral approach are that it allows good exposure of the acetabulum, facilitating cup positioning which may decrease rates of hip dislocation. It also diminishes the risk of injury to the sciatic nerve which is not close to the operative field. However, there is an increased risk of damage to the superior gluteal nerve as well as to the gluteus medius muscle resulting in trouble with limp (Baker 1989; Downing 2001). Insertion of long stems or further revision by the same approach is also more difficult. Increased heterotopic ossifications have been reported (Mulliken 1998).
Dislocation of a hip prosthesis is a clinically important complication after THA, in terms of morbidity implications and costs. It implies a new hospitalisation for the patient who is not able to move his/her hip anymore until the head of the prosthesis is moved back in its socket, usually under a short general anaesthesia. Dislocation has been reported in 0.5% to 6% of participants undergoing primary THA and 6% to 10% for revision THA. This does not seem to decrease with increasing experience. The influence of the surgical approach of the hip on the dislocation rate has often been debated but no clear consensus has been established and no systematic review has previously been published ( McCollum 1990; Morrey 1992; Turner 1994; Huten 1999; Jolles 2002) with the exception of the first publication of this Cochrane review (Jolles 2004).
Objectives
Primary objective: To determine, based on evidence from randomised trials, the risk of prosthesis dislocation after a posterior approach, compared to a direct lateral approach, for adult participants undergoing total hip arthroplasty (THA) for primary osteoarthritis.
Secondary objectives: To determine, based on evidence from randomised trials, the risk of postoperative Trendelenburg gait after a posterior approach, compared to a direct lateral approach, for adult patients undergoing THA for primary osteoarthritis. To determine, based on evidence from randomised trials, the risk of sciatic nerve palsy after a posterior approach, compared to a direct lateral approach, for adult patients undergoing THA for primary osteoarthritis.
Methods
Criteria for considering studies for this review
Types of studies
All published randomised controlled trials comparing total hip arthroplasty (THA) by posterior and direct lateral surgical approaches. Quasi‐randomised trials (for example, allocation by alternation or date of birth) and inadequately concealed prospective comparative studies were considered for inclusion.
Types of participants
Any patient 18 years old or older having a THA with a diagnosis of primary hip osteoarthritis .
Types of interventions
Posterior or direct lateral surgical approaches for THA.
Types of outcome measures
Adverse outcomes 1) Prosthesis dislocation rate. Only true dislocations, documented by X‐rays, were considered. 2) Rate of Trendelenburg gait, as defined by Hardcastle (Hardcastle 1985). 3) Rate of nerve palsy or injury, as documented by an electromyographic study (EMG). 4) Rate of sciatic nerve palsy or injury, as documented by an electromyographic study (EMG). 5) Pain, as documented by a visual analogue scale (VAS).
Functional outcomes 1) Harris Hip Score (Harris 1969) 2) WOMAC Score (Western Ontario and McMaster Universities Osteoarthritis Index, Bellamy 1988) 3) Range of motion 4) Leg length discrepancy
Data for the following outcomes were sought: 1) Operative details a. Length of incision (in millimetres) b. Operative time (in minutes) c. Operative blood loss (in millilitres) d. Post‐operative blood transfusion (in units)
2) Perioperative complications a. Intra‐operative fracture at the time of surgery (acetabulum or femur) b. Periprosthetic fracture after surgery c. Superior gluteal nerve palsy d. Obturator nerve palsy e. Femoral nerve palsy f. Damage to other anatomical structures g. Other surgical complications (as detailed in each study).
3) Post‐operative complications a. Superficial wound infection. b. Deep wound infection (infection around the implant) c. Superficial hematoma d. Deep hematoma e. Thromboembolic complications (deep thrombosis or pulmonary embolism) f. Heterotopic ossification g. Pneumonia h. Bladder infection i. Any medical complication (as detailed in each individual study)
4) Post‐operative care outcomes a. Days to mobilisation b. Length of hospital stay (days) c. Length of rehabilitation centre stay (days)
5) Complications related to the implant a. Cup loosening b. Stem loosening c. Polyethylene wear d. Head fracture e. Other complications (as detailed in each study).
6) Final outcome measures a. Days to dislocation b. Reoperation rate c. Survival rate of prosthesis d. Mortality e. Residence at final follow‐up (return to living at home, discharge location) f. Mobility (use of walking aids, return of mobility) g. Other functional outcomes as listed in each study h. Health related quality of life measures
Search methods for identification of studies
Relevant randomised controlled trials were selected from those identified by application of the general search strategy developed by the Musculoskeletal Review Group (update from the end of 2002 to Oct 13, 2005). The latter included:
a) computer aided searching of various computer databases, MEDLINE (1982‐2005), EMBASE (1982‐2005), CINAHL (1982‐2005), as well as the Cochrane Musculoskeletal Group Trials Register, the Cochrane Controlled Trials Register (CENTRAL/CCTR), the Health Technology Assessment database (HTA) and the Database of Abstracts of Reviews of Effectiveness (DARE) (2005). A trained medical librarian was consulted to develop an optimal search strategy.
Search terms that were used are shown in Appendix 1.
b. investigation of the bibliographies of retrieved studies,
c. entering identified trials into Science Citation Index to identify articles that quoted the original study.
Unpublished data were not sought, but authors of published trials were contacted to clarify or provide additional information.
No language restriction were applied. The search covered the period from January 1982 to October, 2005. Studies before 1982 were not included in order to have articles dealing with the Hardinge approach (published in 1982) and describing results of modern implantation techniques and modern types of prostheses.
Data collection and analysis
STUDY SELECTION Two reviewers (BMJ, ERB) independently assessed all potential abstracts and published reports that were identified by the literature search. Consensus was reached through discussion of any disagreements. Reasons for excluded studies were noted. The two reviewers were not blinded to authors, institution or journal of the publication.
QUALITY ASSESSMENT Quality of included trials was evaluated independently by the reviewers, using the following 18 criteria adapted from Verhagen (Verhagen 1998) and Van Tulder (Van Tulder 1997). There are 3 potential answers to the following questions: Yes (score of 1), Can't Tell (score of 0) and No (score of 0). A maximum score of 17 can be achieved.
Patient Selection a. Were the eligibility criteria specified? b1. Was a method of randomization performed? b2. Was the treatment allocation concealed? c. Were the groups similar at baseline regarding the most important prognostic indicators?
Interventions d. Were the index and control interventions explicitly described? e. Were the surgeons experienced in both operations prior to the trial? f. Were co‐interventions avoided or comparable? g. Was the compliance acceptable in all groups?
Outcome Measurement h. Was the outcome assessor blinded to the intervention? i. Were the outcome measures relevant? j. Was the timing of follow‐up appropriate? k. Was a long‐term follow‐up performed? l. Was the timing of the outcome assessment in both groups comparable? m. Were other complications described? n. Was the withdrawal/drop‐out rate described and acceptable?
Statistics o. Was the sample size for each group described? p. Did the analysis include an intention‐to‐treat analysis? q. Were point estimates and measures of variability presented for the primary outcome measures?
DATA EXTRACTION Each reviewer extracted data independently using pre‐designed standardized data abstraction forms. One reviewer entered data into RevMan and the other cross‐checked the printout against his own data abstraction forms. Discrepancies were resolved by a consensus of the two reviewers. Information from the primary author was obtained when published article provided inadequate information to the review.
DATA SYNTHESIS AND ANALYSIS For each study, relative risks and 95% confidence limits were calculated for dichotomous outcomes, and weighted mean differences and 95% confidence limits calculated for continuous outcomes. Meta‐analyses were conducted with a fixed effects model. Where there was statistical evidence of heterogeneity a random effects model was used.
GRADING THE STRENGTH OF THE EVIDENCE The common system of grading the strength of scientific evidence for a therapeutic agent that is described in the CMSG module scope and in the Evidence‐based Rheumatology BMJ book (Tugwell 2003) was used to rank the evidence included in this systematic review. Four categories are used to rank the evidence from research studies from highest to lowest quality: Platinum, Gold, Silver, and Bronze. The ranking is included in the synopsis of this review.
Results
Description of studies
In total, 44 studies were identified (from the literature search). Only 11 studies were found relevant and 4 met the eligibility criteria and were included. The 4 included studies were prospective cohort studies.
Baker 1989 evaluated 79 hips in a trial involving 69 participants, grouped according to the operative approach used by their surgeon: 21 total hip arthroplasties (THA) were done by the posterior approach, 29 by the direct lateral approach and 29 by the Dall's modified direct lateral approach. Only data related to the posterior and direct lateral approaches (evidence of Trendelenburg gait, denervation and trochanteric pain) were extracted .
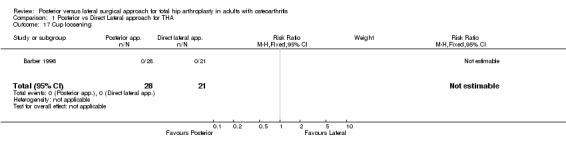
Barber 1996 compared the clinical outcome of the direct lateral and posterior surgical approaches, in terms of Trendelenburg gait and dislocation in particular, in a consecutive series of 49 participants who had a primary THA for osteoarthritis.
Weale 1996 evaluated 42 participants undergoing primary total hip replacement. According to the surgeon's normal practice, 22 participants were operated on by the posterior approach and 20 participants by the direct lateral approach. The sciatic, obturator and femoral nerves were assessed clinically and electrophysiologically four weeks after surgery.
Downing 2001 evaluated 100 participants undergoing primary THA for osteoarthritis. The first consecutive suitable people, who were willing to participate, were separated in two groups according to their surgeon's usual surgical approach. All the 49 posterior approaches received Exeter stems and Charnley stems were used for all the 51 lateral Hardinge approaches. Trendelenburg gait and dislocation were recorded.
A summary of the details of these trials is given in the Characteristics of Included Studies Table.
Characteristics of the excluded studies are reported in the Table of Characteristics of Excluded Studies.
Risk of bias in included studies
The methodology of the identified studies was generally poor. All four of the included studies scored less than 12 out of a possible maximum quality score of 17 (70%).
None used an appropriate method of randomisation. All groups of participants were formed according to the usual practice of the surgeon who was performing the posterior or the direct lateral approach and therefore inadequately concealed.
For studies comparing different approaches, ideally, implants used and rehabilitation programs should be well described. No provided sufficient details on these important factors. Only one study (Downing 2001) had the outcome assessor blinded to the intervention. None of the studies described the justification and calculations for the sample size.
Table 1. Assessment of methodology.
a b c d e f g h i j k l m n o p q Internal validity Descriptive Criteria Statistical criteria Total Study name _____________________________________________________________________________________
0 0 0 1 1 0 1 0 1 1 0 1 0 1 0 1 0 6 2 0 8 Baker 1989 1 0 0 1 1 0 1 0 1 1 1 1 1 1 0 1 1 6 5 1 12 Barber 1996 1 0 0 1 1 0 1 0 1 1 0 1 1 1 0 0 0 5 4 0 9 Weale 1996 1 0 0 1 1 0 0 1 1 1 0 1 1 0 0 0 1 4 4 1 9 Downing 2001 ______________________________________________________________________________________ Maximum of points 10 5 2 17
Effects of interventions
Posterior and direct lateral approaches were compared in all four studies. The outcome measures reported by each study are listed in the Characteristics of Included Studies table.
ADVERSE OUTCOMES DISLOCATION The primary outcome, dislocation, was studied only by Barber 1996 and Downing 2001. Summation of the data available from these studies is given in the analysis tables. These indicate no significant difference between posterior versus direct lateral surgical approach [1/77 (1.3%) versus 3/72 (4.2%); relative risk (RR) 0.35; 95% confidence intervals (CI) 0.04 to 3.22].
TRENDELENBURG GAIT The presence of a postoperative Trendelenburg gait was studied by Baker 1989, Barber 1996 and Downing 2001. Summation of the data available from these studies is given in the analysis tables. These indicate no significant difference between posterior versus direct lateral surgical approach [7/88 (8.0%) versus 13/78 (16.7%); RR 0.52; 95% CI 0.21 to 1.27]. This outcome measure seems to favour slightly the posterior surgical approach as having less participants with postoperative Trendelenburg gait. However, the pooled results should be taken with care as all the studies did not compare the patient gait at the same follow‐up times.
NERVE PALSY OR INJURY Nerve palsy or injury was studied by Baker 1989 and Weale 1996. Weale observed sciatic, femoral and obturator nerve palsies. Baker observed only superior gluteal nerve palsies. A significant difference between posterior versus direct lateral surgical approach was found in favour of less nerve injuries with the posterior approach [1/43 (2%) versus 10/49 (20%); RR 0.16; 95% CI 0.03 to 0.83]. However, when looking at each type of nerve palsy separately, no significant difference was found between each type of surgical approach.
PAIN The last adverse outcome selected, pain, was studied only by Baker 1989. No significant difference was observed between the posterior and direct lateral surgical approaches [3/21 (14%) versus 7/29 (24%); RR 0.59; 95% CI 0.17 to 2.03].
FUNCTIONAL OUTCOMES HARRIS HIP SCORE and WOMAC SCORE Harris hip scores were recorded only by Barber 1996. Patients of both groups improved their score to obtain the same mean score of 94 two years after surgery. WOMAC scores were not computed in any of the studies
RANGE OF MOTION Only the mobility in internal rotation while the hip joint lies in extension was recorded by Barber 1996. A significant difference was observed between posterior and direct lateral surgical approach in favour of the posterior approach [35° (SD 13) versus 19° (SD 13); WMD 16; 95% CI 8.64 to 23.36].
LEG LENGTH DISCREPANCY The last functional outcome selected was studied only by Weale 1996. Limb length discrepancies of more than 1cm were recorded and no significant difference was found between posterior and direct lateral surgical approaches [4/22 (18%) versus 6/20 (30%); RR 0.61; 95% CI 0.20 to 1.84].
Baker 1989 compared 21 participants operated on by the posterior approach to 29 operated on by the direct lateral one. There were no loss to follow‐up. However, the type of implants used as well as the rehabilitation procedure were not stated. Trendelenburg gait was reported 3 months after surgery with a trend of less positive tests among the posterior approach group but no significant difference between groups [2/20 (10.0%) versus 9/24 (37.5%); RR 0.27; 95% CI 0.06 to 1.10]. Evidence of superior gluteal nerve denervation was reported at 2 weeks and 3 months without significant difference between groups. Trochanteric pain was assessed on a visual analogue scale (number of participants who had a score of 3 or greater, out of ten), without significant difference between groups.
Barber 1996 compared 28 total hip prostheses operated on using the posterior approach versus 21 hips using the direct lateral approach. Cemented and un cemented implants were used in both approaches in different proportions. The rehabilitation program included protected weight bearing, starting on postoperative day 2 for both approaches. At 2‐years follow‐up, no dislocations were recorded in either group. The risk difference (RD) was 0.00 with a 95% CI ‐0.08 to 0.08 (RR not estimable). A Trendelenburg test score as well as a limp score and an abductor power score were recorded without significant differences between groups. There were no significant difference in postoperative heterotopic ossifications and no evidence of implant loosening in either group. The average range of internal rotation in extension of the hip was significantly higher in the posterior approach group [mean (m) 35°, standard deviation (sd) 13°] compared to the direct lateral approach [m 19°, sd 13°; mean weighted difference 16.0; 95% CI 8.64 to 23.36]. The average Harris hip scores were the same at 1‐year follow‐up for both groups.
Weale 1996 compared 22 participants operated on by the posterior approach to 20 operated on by the direct lateral one. There were no loss to follow‐up. However, the type of implants used as well as the rehabilitation procedure were not stated. Mean operative time and operative blood loss were evaluated without mention of standard deviation, making difficult any meaningful comparison (78 min and 599 ml for posterior approach vs 107 min and 768 ml for direct lateral approach). Incidence of nerve injury (sciatic, obturator, femoral nerves) was reported at 4 weeks from operation with no difference between groups. Post‐operative limb‐length discrepancy of more than 1 cm was reported also with no difference between groups.
Downing 2001 compared 49 total hip arthroplasties done by the posterior approach versus 51 hips by the direct lateral approach for 100 participants. All participants had cemented stems, but the type was different in each group; Exeter prostheses for the posterior approach and Charnley ones for the direct lateral approach. Follow‐up was done at 3 and 12 months. Twenty seven participants were lost to follow‐up, but the number of lost to follow‐up per group was not stated. Four participants had a hip dislocation, 1/49 (2.0%) in the posterior approach group versus 3/51 (5.9%) in the direct lateral approach group. The difference was not statistically significant between the groups (RR 0.35; 95% CI 0.04 to 3.22). Trendelenburg tests were reported at 12 months from surgery without difference between groups [2/40 (5.0%) versus 2/33 (6.1%); RR 0.82; 95% CI 0.12 to 5.54]. Hip abductor strength of the operated leg improved in both groups at 3 months and 12 months without any difference between groups. Two complications were noted: one periprosthetic fracture and one death (approach used for these 2 participants was not stated).
Discussion
Many of the trial reports indicated a poor level of methodological rigour, in particular regarding concealment of allocation and assessor blinding. Furthermore, many of the studies involved small numbers of participants with limited reporting of outcome measures. The low methodology scoring for these studies may reflect firstly poor reporting and secondly poor trial methodology.
The four identified studies investigating the comparison between posterior and direct lateral surgical approach involved a total of 241 participants. All studies were inadequately concealed: groups were made up according to surgeon's approach and usual referral practice to get consecutive participants.
The largest study, Downing 2001 with 100 participants, was of poor methodological quality, with limited reporting of baseline groups characteristics and outcomes, inadequate follow‐up of participants and 27% of participants lost to follow‐up without knowing to which group they belonged. There were less than 30 participants in each groups of the other included studies. The limited number of participants in these trials prevents firm conclusions being made. This is especially true for low rate events as hip dislocation, currently reported in the literature to be often less than 5%.
Details of surgery and rehabilitation were not well described in any of the included studies. This might prevent meaningful pooling of results. In a recent review of more than 50'000 primary total hip arthroplasty, Furnes 2001 reported that the type of implant and fixation were major confounding factors in the study of hip replacement. Pellicci 1998 showed in 2 series of 395 total hip replacement that capsular repair in a posterior approach reduced the dislocation rate (from 4% to 0% in his study) enhancing the need for a detailed description of the surgical technique. As well, early mobilisation is recognized as mandatory for a good functional recovery after total hip arthroplasty, and should be part of the details given in the method section of a study, separated from any other rehabilitation interventions for which the value is not yet proven as recently mentioned by Roos 2003. Baker 1989 and Weale 1996 did not report which type of implants and rehabilitation programs were used and if they were the same for all participants in both groups. Barber 1996 described the type of prostheses that were used for participants in both groups, but the proportion of each type were different between approaches: 86% fully cemented for the posterior approach group and 91% hybrid procedure for the direct lateral approach group. Downing 2001 used Exeter cemented stems for the posterior approach group and Charnley cemented stems for the direct lateral approach group, without mention of the type of cups that were used. Co‐interventions should be well described and similar between groups. Surgeon experience in both procedures should also be well described. Hedlundh 1996 observed twice the number of dislocations among inexperienced surgeons, with an important change as soon as the surgeon has done 30 primary total hip arthroplasty and at least 10 times a year. In these trials, neither is done, therefore preventing meaningful conclusions to be made.
Two studies reported the dislocation rate (Barber 1996; Downing 2001), three studies reported postoperative Trendelenburg gait (Baker 1989; Barber 1996; Downing 2001), and two reported postoperative nerve palsy (Weale 1996). No significant differences were found between the posterior and direct lateral approaches dislocation rate and the postoperative Trendelenburg gait, in each study or in the meta‐analysis. A significant difference was found for the presence of a nerve palsy or injury when using the direct lateral approach. However, when looking at each nerve injury separately (sciatic, gluteal, obturator, or femoral), no significant difference was found with the posterior approach. In addition, this result should be taken cautiously as it represents only the situation in a collective of less than 100 patients, which is small for hip arthroplasty surgery, and in which the details of surgery and rehabilitation procedure were not stated by the authors. Among the other outcomes, the only significant result found was an increased range of motion in internal rotation of the hip in extension for participants operated on by posterior approach (Barber 1996). However, the limited number of studies found as well as the limited reporting of their outcome measures prevent definite conclusions being drawn.
Finally, only one study had a blinded outcome assessor (Downing 2001). It is clear that blinding of the surgeon is impossible. Patient blinding is almost impossible because of the obvious scar on the upper thigh. But the outcome assessor should have been blinded in all studies in order to decrease the number of possible study biases.
Authors' conclusions
Implications for practice.
The quality of the information extracted from the trials performed to date is poor, which prevents any firm conclusion on the optimum choice of surgical approach in adult patients undergoing primary total hip arthroplasty for osteoarthritis to be drawn.
Implications for research.
Further well conducted randomised trials with full reporting of outcomes, blinding of outcome assessors and correct methodology are required to determine the optimum surgical approach for the insertion of a total hip arthroplasty. Reporting should conform to the CONSORT statement (Moher 2001).
A sample size calculation revealed that about 1500 participants will be required in each arm of the study (alpha = 0.05, power = 0.80, probability of event among controls = 1.5%, RR = 2, case sample size = 1534, PS software version 2.1.30, February, 2003) to determine if there is an increased or decreased risk of dislocation with one or the other surgical approach. A multi‐centre prospective randomised controlled study is recommended.
This Cochrane review should be updated as further studies become available. The authors of this review will be pleased to receive information about any other prospective studies or RCT comparing the lateral and posterior approaches in primary total hip arthroplasty.
What's new
| Date | Event | Description |
|---|---|---|
| 9 November 2008 | Amended | Converted to new review format. CMSG ID: C069‐R |
Acknowledgements
The authors would like to thank Dr. Arne Ohlsson for his helpful comments, Jessie McGowan and Louise Falzon for help with literature search as well as Maria Judd and Lara Maxwell for help with preparation of the review. We would also like to thank the following for useful feedback at editorial review Ann Scott and Jason Werle.
Appendices
Appendix 1. Full search strategy
1 arthroplasty, replacement, hip/ (6632) 2 Hip Prosthesis/ (14867) 3 or/1‐2 (18638) 4 arthroplasty/ or arthroplasty, replacement/ (6923) 5 Joint Prosthesis/ (7466) 6 "Prostheses and Implants"/ (27329) 7 (arthroplasty or replacement or prosthes#s).tw. (151653) 8 or/4‐7 (177019) 9 hip/ or hip joint/ or hip.tw. (59269) 10 8 and 9 (19395) 11 3 or 10 (25121) 12 (moore or austin‐moore).tw. (1569) 13 posterior.tw. (113463) 14 12 or 13 (115004) 15 3 and 14 (542) 16 hardinge.tw. (27) 17 lateral.tw. (121370) 18 16 or 17 (121386) 19 3 and 18 (616) 20 15 and 19 (102) 21 (mt or su).fs. (2162624) 22 11 and 21 (13337) 23 clinical trial.pt. (431542) 24 randomized controlled trial.pt. (206880) 25 random$.tw. (352004) 26 meta‐analysis.pt,sh. (21089) 27 (meta‐anal: or metaanal:).tw. (16560) 28 (quantitativ: review: or quantitativ: overview:).tw. (336) 29 (methodologic: review: or methodologic: overview:).tw. (181) 30 (systematic: review: or systematic: overview).tw. (13159) 31 review.pt. and medline.tw. (12662) 32 or/23‐31 (651784) 33 22 and 32 (1007) 34 33 not 20 (1004) 35 limit 20 to all adult <19 plus years> (63) 36 limit 33 to all adult <19 plus years> (798) 37 from 35 keep 1‐63 (63) 38 limit 37 to yr="2002‐2005" (16) (update from the end of 2002 to Oct 13, 2005)
Data and analyses
Comparison 1. Posterior vs Direct Lateral approach for THA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Dislocation | 2 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.04, 3.22] |
| 2 Trendelenburg gait | 3 | 166 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.21, 1.27] |
| 3 Nerve palsy or injury | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.03, 0.83] |
| 4 Pain | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.17, 2.03] |
| 4.1 Trochanteric pain (>3/10) | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.17, 2.03] |
| 5 Trendelenburg score [0‐2] | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.25, 0.31] |
| 6 Limp score [0‐4] | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.61, 0.33] |
| 7 Abductor power score [0‐5] | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.24, 0.64] |
| 8 Sciatic nerve palsy | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 3.59] |
| 9 Sup. gluteal nerve palsy | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.03, 2.19] |
| 10 Obturator nerve palsy | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 3.59] |
| 11 Femoral nerve palsy | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.01, 7.07] |
| 12 Harris hip score | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Pre‐operative | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Postoperative | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 Change post‐preop at folllow‐up | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 WOMAC score | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Range of motion | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 14.1 Internal rotation | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | 16.0 [8.64, 23.36] |
| 15 Limb‐length discrepancy | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.20, 1.84] |
| 15.1 LLD > 1cm | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.20, 1.84] |
| 16 Stem loosening | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Cup loosening | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Reoperation | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Periprosthetic fracture | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Heterotopic ossification [Brooker 1‐4] | 1 | 245 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.30, 1.09] |
| 20.1 Brooker I | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.16, 1.55] |
| 20.2 Brooker II | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.15, 15.46] |
| 20.3 Brooker III | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.01, 5.91] |
| 20.4 Brooker IV | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20.5 Total | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.23, 1.38] |
1.1. Analysis.
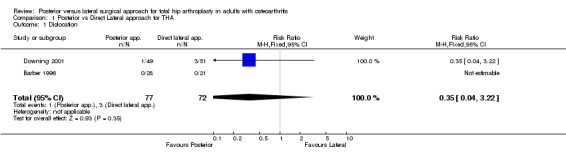
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 1 Dislocation.
1.2. Analysis.
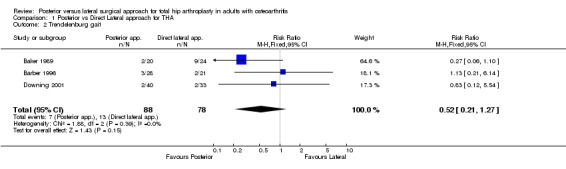
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 2 Trendelenburg gait.
1.3. Analysis.
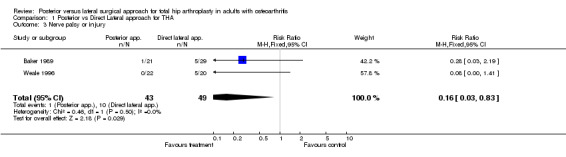
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 3 Nerve palsy or injury.
1.4. Analysis.
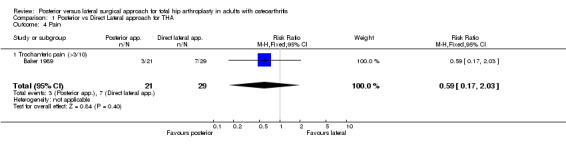
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 4 Pain.
1.5. Analysis.

Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 5 Trendelenburg score [0‐2].
1.6. Analysis.
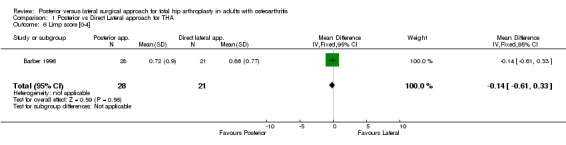
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 6 Limp score [0‐4].
1.7. Analysis.
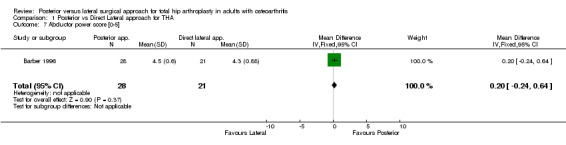
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 7 Abductor power score [0‐5].
1.8. Analysis.
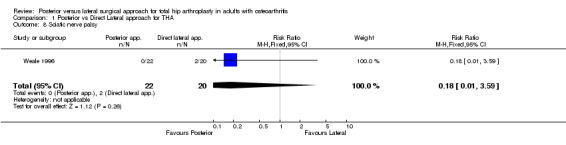
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 8 Sciatic nerve palsy.
1.9. Analysis.

Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 9 Sup. gluteal nerve palsy.
1.10. Analysis.
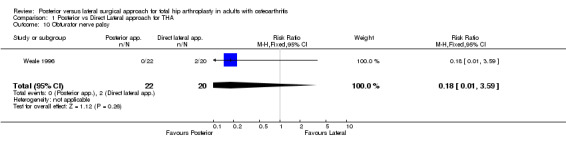
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 10 Obturator nerve palsy.
1.11. Analysis.
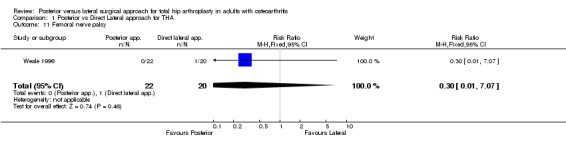
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 11 Femoral nerve palsy.
1.12. Analysis.

Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 12 Harris hip score.
1.14. Analysis.
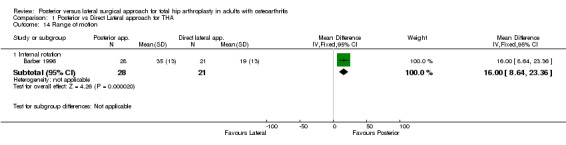
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 14 Range of motion.
1.15. Analysis.
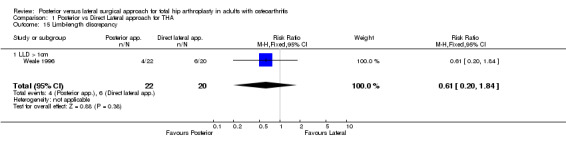
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 15 Limb‐length discrepancy.
1.16. Analysis.
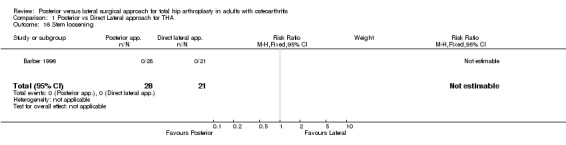
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 16 Stem loosening.
1.17. Analysis.
Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 17 Cup loosening.
1.18. Analysis.

Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 18 Reoperation.
1.20. Analysis.

Comparison 1 Posterior vs Direct Lateral approach for THA, Outcome 20 Heterotopic ossification [Brooker 1‐4].
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Baker 1989.
| Methods | Trial: groups according to surgeon's approach ‐ prospective cohort study | |
| Participants | 50 patients 21 posterior approach 29 direct lateral approach Bristol Royal Infirmary, Bristol, UK Mean age not stated Male/Female repartition not stated Follow‐up: all patients 3 months post surgery. None lost to follow‐up | |
| Interventions | Implants used not stated Rehabilitation procedure not stated | |
| Outcomes | ‐ Trendelenburg gait ‐ Gluteal denervation ‐ Trochanteric pain | |
| Notes | Quality score: Internal validity 6/10, descriptive criteria 2/5, statistical criteria 0/2, total 8/17 Pre‐operative diagnosis not well stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Barber 1996.
| Methods | Trial: consecutive patients grouped according to surgeon's approach ‐ prospective cohort study | |
| Participants | 49 patients 28 posterior approach 21 direct lateral approach Division of Orthopaedic Surgery, Standford, CA, USA Mean age 70 y (post) 72 y (lat) 50% female (post) 72% female (lat) Follow‐up of at least 2 years None lost to follow‐up | |
| Interventions | Mixed cemented and uncemented implants for both approaches Rehabilitation with protected weight bearing started on day 2 for both approaches | |
| Outcomes | ‐ Trendelenburg gait ‐ Abductor power ‐ Limp ‐ Dislocations ‐ Harris hip scores ‐ Range of motion ‐ Heterotopic ossification ‐ Loosening | |
| Notes | Quality score: Internal validity 6/10, descriptive criteria 5/5, statistical criteria 1/2, total 12/17 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Downing 2001.
| Methods | Trial: consecutive patients grouped according to surgeon's approach (usual referral practice) ‐ prospective cohort study | |
| Participants | 100 patients 49 posterior approach 51 direct lateral approach Queen's Medical Centre, University Hospital, Nottingham, UK Mean age 67y [41‐83] (post), 65y [42‐83] (lat) 51% female (post) 59% female (lat) Follow‐up at 3 and 12 months Losses to follow‐up not described per group (27 lost/100) | |
| Interventions | Cemented stems: Exeter (post) Charnley (lat). Cup used not stated. Standard rehabilitation program for both approaches but not described | |
| Outcomes | ‐ Trendelenburg gait ‐ Abductor strength ‐ Dislocation ‐ Periprosthetic fracture ‐ Mortality | |
| Notes | Quality score: Internal validity 4/10, descriptive criteria 4/5, statistical criteria 1/2, total 9/17 Benefits from commercial part | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Weale 1996.
| Methods | Trial: consecutive patients grouped according to surgeon's practice (usual referral practice) ‐ prospective cohort study | |
| Participants | 42 patients 22 posterior approach 20 direct lateral approach Southmead Hospital, Bristol, UK Mean age 69.4y (post) 68.5y (lat) 68% female (post) 45% female (lat) Follow‐up: all patients 4 weeks post surgery. None lost to follow‐up | |
| Interventions | Implants used not stated Rehabilitation procedure not stated | |
| Outcomes | ‐ Sciatic nerve injury ‐ Obturator nerve injury ‐ Femoral nerve injury ‐ Operative time ‐ Operative blood loss ‐ Limb length discrepancy | |
| Notes | Quality score: Internal validity 5/10, descriptive criteria 4/5, statistical criteria 0/2, total 9/17 Pre‐operative diagnosis not well stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Byström 2003 | This study analyzed the Norwegian Arthroplasty Register to find risk factors for prosthesis dislocation leading to revision. Seven prosthesis brand combinations were used in 42897 primary hip arthroplasty in 68 hospitals. The study was excluded because we had no idea if groups of surgical approach are similar as for age, comorbidities, and types of prosthesis (shape, fixation,head sizes). In addition, the lateral approach included a mixed of Hardinge, antero‐lateral and trochanterotomy approaches. |
| Grossmann 1994 | This study compared 45 dislocations in 1734 patients with a randomized control group of 61 patients. Factors causing an increasing number of dislocation as surgical approaches were analysed. The study was excluded as it was retrospective and without mention of the clinical diagnosis before total hip replacement. |
| Kohn 1997 | This study reviewed 1238 primary total hip arthroplasties for arthritis. The influence of surgical approaches on dislocation was studied. The study was excluded as it was retrospective. |
| Moreschini 1996 | This study reviewed 19 patients operated on for osteoarthritis (primary and secondary) or femoral neck fractures with clinical and electromyographic assessments. This study was excluded as it was retrospective and without specific data for primary osteoarthritis and adults results. |
| Moroni 2000 | This study reviewed intraoperative femoral fractures after 3566 total hip replacements. Potential risk factors as surgical approaches were reviewed. The study was excluded as it was retrospective and there was not a comparison per surgical approaches. |
| Pascarel 1989 | This randomized study compared 63 hip prostheses implanted with the direct lateral approach with 63 total hip arthroplasties implanted with the posterior approach to assess the functional impact. The study was excluded as the hip replacements were not done for osteoarthritis only (fractures, osteonecrosis, dysplasia,...) and no specific data were available for patients with osteoarthritis. |
| Zimmerman 2002 | The study reviewed 271 patients aged 65 years and older, operated on for osteoarthritis, from numerous surgeons in different hospitals. The study was excluded as lateral and antero‐lateral approaches were mixed in one group, as well as posterior and postero‐lateral approaches in the other group. In addition, it was unrandomized and the groups were different in terms of age and comorbidities. |
Contributions of authors
Brigitte M. Jolles: developing and writing the text of this review Earl R. Bogoch: developing and writing the text of this review
Sources of support
Internal sources
Hôpital Orthopédique de la Suisse Romande, University of Lausanne, Lausanne, Switzerland.
St. Michael's Hospital, University of Toronto, Toronto, Canada.
External sources
No sources of support supplied
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Baker 1989 {published data only}
- Baker AS, Bitounis VC. Abductor function after total hip replacement ‐ An electromyographic and clinical review. J Bone Joint Surg 1989;71‐B:47‐50. [DOI] [PubMed] [Google Scholar]
Barber 1996 {published data only}
- Barber TC, Roger DJ, Goodman SB, Schurman DJ. Early outcome of total hip arthroplasty using the direct lateral vs the posterior surgical approach. Orthopedics 1996;19:873‐5. [DOI] [PubMed] [Google Scholar]
Downing 2001 {published data only}
- Downing ND, Clark DI, Hutchinson JW, Colclough K, Howard PW. Hip abductor strength following total hip arthroplasty ‐ A prospective comparison of the posterior and lateral approach in 100 patients. Acta Orthop Scand 2001;72:215‐20. [DOI] [PubMed] [Google Scholar]
Weale 1996 {published data only}
- Weale AE, Newman P, Ferguson IT, Bannister GC. Nerve injury after posterior and direct lateral approaches for hip replacement. A clinical and electrophysiological study. J Bone Joint Surg 1996;78‐B:899‐902. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Byström 2003 {published and unpublished data}
- Byström S, Espehaug B, Furnes O, Havelin LI. Femoral head size is a risk factor for total hip luxation. A study of 42'897 primary hip arthroplasties from the Norwegian Arthroplasty Register. Acta Orthopedica Scandinavica 2003;74(5):514‐24. [DOI] [PubMed] [Google Scholar]
Grossmann 1994 {published data only}
- Grossmann P, Braun M, Becker W. Dislocation following total hip arthroplasties. Association with surgical approach and other factors [Luxationen nach Huft‐TEP‐Implantationen: Abhangigkeit vom operativen Zugang und anderen Faktoren]. Z Orthop 1994;132:521‐6. [DOI] [PubMed] [Google Scholar]
Kohn 1997 {published data only}
- Kohn D, Ruhmann O, Wirth CJ. Influence of surgical approach on dislocation of total hip replacements [Die Verrenkung der Hufttotalenendoprothese unter besonderer Beachtung verschiedener Zugangswege]. Z Orthop 1997;135:40‐4. [DOI] [PubMed] [Google Scholar]
Moreschini 1996 {published data only}
- Moreschini O, Giordano MC, Margheritini F, Chiatti R. A clinical and electromyographic review of the lateral and postero‐lateral approaches to the hip after prosthetic replacement. Hip international 1996;6:40‐7. [Google Scholar]
Moroni 2000 {published data only}
- Moroni A, Faldini C, Piras F, Giannini S. Risk factors for intraoperative femoral fractures during total hip replacement. Ann Chir Gyn 2000;89:113‐8. [PubMed] [Google Scholar]
Pascarel 1989 {published data only}
- Pascarel X, Dumont D, Nehme B, Dubreuilh JP, Honton JL. Total hip arthroplasty using Hardinge's approach. Clinical results of 63 cases [Arthroplastie totale de hanche par voie de Hardinge. Résultat clinique de 63 cas]. Rev Chir Orthop 1989;75:98‐103. [PubMed] [Google Scholar]
Zimmerman 2002 {published data only}
- Zimmerman S, Hawkes Wg, Hudson JI, Magaziner J, Hebel JR, Towheed T, Gardner J, Provenzano G, Kenzora JE. Outcomes of surgical management of total hip replacement in patients aged 65 years and older: cemented versus cementless femoral components and lateral or anterolateral versus posterior anatomical approach. J Orthop Res 2002;20:182‐191. [DOI] [PubMed] [Google Scholar]
Additional references
Arthritis Soc. 2005
- The Arthritis Society. How common is osteoarthritis?. www.arthritis.ca 2005.
Bellamy 1988
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of the WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. Journal of Rheumatology 1988;15:1833‐40. [PubMed] [Google Scholar]
Brown 1995
- Brown DE, Neumann RD. Orthopedic secrets. Philadelphia, PA, USA: Hanley & Belfus, Inc, 1995. [Google Scholar]
Furnes 2001
- Furnes O, Lie SA, Espehaug B, Vollset SE, Engesaeter LB, Havelin LI. Hip disease and the prognosis of total hip replacements. A review of 53698 primary total hip replacements reported to the Norwegian arthroplasty register 1987‐99. Journal of Bone and Joint Surgery. British Volume 2001;83‐B:579‐86. [DOI] [PubMed] [Google Scholar]
Greene 2001
- Berry DJ, Garvin KL. In: Greene WB, Lieberman JR editor(s). Essentials of musculoskeletal care. 2nd Edition. Rosemont, Illinois, USA: American Academy of Orthopaedic Surgeons, 2001. [Google Scholar]
Hardcastle 1985
- Hardcastle P, Nade S. The significance of the Trendelenburg test. Journal of Bone and Joint Surgery 1985;67‐B:741‐6. [DOI] [PubMed] [Google Scholar]
Hardinge 1982
- Hardinge K. The direct lateral approach to the hip. Journal of Bone and Joint Surgery. British Volume 1982;64‐B:17‐9. [DOI] [PubMed] [Google Scholar]
Harris 1969
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by Mold arthroplasty. An end‐result study using a new method of result evaluation. Journal of Bone and Joint Surgery 1969;51‐A:737‐55. [PubMed] [Google Scholar]
Hedlundh 1996
- Hedlundh U, Ahnfelt L, Hybbinette CH, Weckström J, Fredin H. Surgical experience related to dislocations after total hip arthroplasty. Journal of Bone and Joint Surgery. British Volume 1996;78‐B:206‐9. [PubMed] [Google Scholar]
Hoaglund 2001
- Hoaglund FT, Steinbach LS. Primary osteoarthritis of the hip: etiology and epidemiology. Journal of the American Academy of Orthopaedic Surgeons 2001;9:320‐7. [DOI] [PubMed] [Google Scholar]
Huten 1999
- Huten D. [Luxations et subluxations des protheses totale de hanche]. In: Duparc J editor(s). Pathologie de la hanche adulte ‐ Une selection des conferences d'enseignement de la SOFCOT. Vol. 2, Paris, France: Expansion Scientifique Publications, 1999:81‐108. [Google Scholar]
Jolles 2002
- Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: A multivariate analysis. Journal of Arthroplasty 2002;17(3):282‐8. [DOI] [PubMed] [Google Scholar]
Li 1999
- Li E, Meding JB, Ritter MA, Keating EM, Faris PM. The natural history of a posteriorly dislocated total hip replacement. Journal of Arthroplasty 1999;14:964‐8. [DOI] [PubMed] [Google Scholar]
McCollum 1990
- McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clinical Orthopaedics and Related Research 1990;261:159‐70. [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DC, for the CONSORT group. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357:1191‐4. [PubMed] [Google Scholar]
Moore 1959
- Moore AT. The Moore self‐locking vitallium prosthesis in fresh femoral neck fractures: a new low posterior approach (the southern exposure). In: American Academy of Orthopaedic Surgeons editor(s). Instructional Course Lectures. Vol. 16, St Louis: CV Mosby, 1959. [Google Scholar]
Morrey 1992
- Morrey BF. Instability after total hip arthroplasty. Orthopedic Clinics of North America 1992;23:237‐48. [PubMed] [Google Scholar]
Mulliken 1998
- Mulliken BD, Rorabeck CH, Bourne RB, et al. A modified direct lateral approach in total hip arthroplasty: a comprehensive review. Journal of Arthroplasty 1998;13:737‐47. [DOI] [PubMed] [Google Scholar]
Oishi 1998
- Oishi CS, Hoaglund FT, Gordon L, Ross PD. Total hip replacement rates are higher among Caucasians than Asians in Hawaii. Clinical Orthopaedics and Related Research 1998;353:166‐74. [DOI] [PubMed] [Google Scholar]
Paterno 1997
- Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient‐related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. Journal of Bone and Joint Surgery 1997;79‐A:1202‐10. [DOI] [PubMed] [Google Scholar]
Pellicci 1998
- Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clinical Orthopaedics and Related Research 1998;355:224‐8. [DOI] [PubMed] [Google Scholar]
Roos 2003
- Ross EM. Effectiveness and practice variation of rehabilitation after joint replacement. Current Opinion in Rheumatology 2003;15:160‐2. [DOI] [PubMed] [Google Scholar]
Tugwell 2003
- Tugwell P, Shea B, Boers M, Simons L, Strand V, Wells G. Evidence‐based Rheumatology. BMJ Books, 2003. [Google Scholar]
Turner 1994
- Turner RS. Postoperative total hip prosthetic femoral head dislocations: incidence, etiologic factors, and management. Clinical Orthopaedics and Related Research 1994;301:196‐204. [PubMed] [Google Scholar]
Van Tulder 1997
- Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group for Spinal Disorders. Spine 1997;22:2323‐30. [DOI] [PubMed] [Google Scholar]
Verhagen 1998
- Verhagen AP, Vet HC, Bie RA, Kessels AG, Boers M, Knipschild PG. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of Clinical Epidemiology 1998;51:1235‐41. [DOI] [PubMed] [Google Scholar]
Woo 1982
- Woo RYG, Morrey BF. Dislocations after total hip arthroplasty. Journal of Bone and Joint Surgery 1982;64‐A:1295‐306. [PubMed] [Google Scholar]
References to other published versions of this review
Jolles 2004
- Jolles BM, Bogoch ER. Surgical approach for total hip arthroplasty: direct lateral or posterior?. Journal of Rheumatology 2004;31(9):1790‐6. [PubMed] [Google Scholar]


