Abstract
Purpose
Our aim was to critically review recent literature on the use of telehealth for dysphagia during the COVID-19 pandemic and enhance this information in order to provide evidence- and practice-based clinical guidance during and after the pandemic.
Method
We conducted a rapid systematized review to identify telehealth adaptations during COVID-19, according to peer-reviewed articles published from January to August 2020. Of the 40 articles identified, 11 met the inclusion criteria. Full-text reviews were completed by three raters, followed by qualitative synthesis of the results and description of practical recommendations for the use of telehealth for dysphagia.
Results
Seven articles were guidelines articles, three were editorials, and one was a narrative review. One article focused on telehealth and dysphagia during COVID-19. The remaining 10 mentioned telehealth in varying degrees while focusing on dysphagia management during the pandemic. No articles discussed pediatrics in depth. The most common procedure for which telehealth was recommended was the clinical swallowing assessment (8/11), followed by therapy (7/11). Six articles characterized telehealth as a second-tier service delivery option. Only one article included brief guidance on telehealth-specific factors, such as legal safeguards, safety, privacy, infrastructure, and facilitators.
Conclusions
Literature published during the pandemic on telehealth for dysphagia is extremely limited and guarded in endorsing telehealth as an equivalent service delivery model. We have presented prepandemic and emerging current evidence for the safety and reliability of dysphagia telemanagement, in combination with practical guidelines to facilitate the safe adoption of telehealth during and after the pandemic.
The COVID-19 pandemic has challenged our ability to manage dysphagia. Both swallowing evaluation and treatment sessions typically involve close physical proximity between the patient and the clinician, as well as several aerosol-generating actions or tasks, such as production of reflexive or voluntary cough, tracheostomy care, and more (Bolton et al., 2020; Brodsky & Gilbert, 2020; Miles et al., 2020). As a result, during the pandemic, patients with suspected or confirmed dysphagia have often been triaged; evaluation and treatment procedures have been canceled, postponed, or conducted with substantial personal protective equipment (PPE); and/or clinicians have started using telehealth (Brodsky & Gilbert, 2020; Ku et al., 2020; Miles et al., 2020). Telehealth is a broad term that includes the use of a variety of telecommunication technologies (including but not limited to videoconferencing, phone, e-mail) to provide care from a distance (Health Resources & Services Administration, 2019) and has been around for more than 100 years (Cipolat & Geiges, 2003). This service delivery model has been implemented regularly in some settings (e.g., the Veterans Affairs system) and countries (e.g., Australia) even prior to the COVID-19 pandemic and has also been shown to be beneficial in earlier public health emergencies and disasters (American Occupational Therapy Association, 2020; Lurie & Carr, 2018; Thomas et al., 2020). Since the early 1990s and with the ever-increasing advances in health care technology and infrastructure, the research interest in telehealth has grown exponentially.
A similar trend of increased interest has also been evident in dysphagia telehealth research. Specifically, since the 1990s, there has been a gradual increase in investigations on the feasibility, validity, and reliability of dysphagia telemanagement. The majority of these studies has examined dysphagia tele-assessments (both clinical and tele–videofluoroscopic swallowing study [tele-VFSS]) and has repeatedly demonstrated that these assessments are safe, valid, and reliable when compared to traditional in-person dysphagia evaluations (Burns et al., 2019, 2016; Kantarcigil & Malandraki, 2017; Kantarcigil et al., 2016; Malandraki et al., 2011; Morrell et al., 2017; Perlman & Witthawaskul, 2002; Ward et al., 2013, 2009, 2012a, 2012b). In the last few years, evidence for the use of teleconsultation and teletreatment sessions for dysphagia has also emerged with equally positive preliminary results (e.g., Burns et al., 2017; Burns, Wishart et al., 2020; Malandraki et al., 2013, 2014; Wall et al., 2016). Additional documented benefits of this service delivery model for dysphagia management include service efficiency (Burns et al., 2017; Burns, Wishart et al., 2020), cost savings (Burns et al., 2019), clinician and patient/caregiver satisfaction (Burns et al., 2019; Kantarcigil & Malandraki, 2017; Malandraki et al., 2014; Ward et al., 2012b), and increased access to specialists leading to improved quality of care (Burns et al., 2017; Malandraki et al., 2013).
Despite these positive developments and benefits, it was not until the COVID-19 pandemic that our field and other rehabilitative professions saw a dramatic increase in the use of telehealth in clinical practice as safety and mitigation of the virus became highest priorities for health care systems worldwide (American Occupational Therapy Association, 2020; Thomas et al., 2020). Indeed, the COVID-19 pandemic has enabled several prior restrictions (e.g., privacy, licensure, reimbursement) to be lifted—albeit temporarily—in some countries such as the United States and has resulted in rapid expansion of the use of telehealth across medical disciplines (Mann et al., 2020), including speech-language pathology and, in part, dysphagia care.
These steps have been a silver lining for the expansion and acceptance of telehealth in our field. However, for dysphagia clinicians, this transition has not been easy. In April and May 2020, the first author participated as a speaker in two webinars for the American Speech-Language-Hearing Association (ASHA) and the American Board of Swallowing and Swallowing Disorders, respectively (Burns, Malandraki, & Ward, 2020; Malandraki, 2020b). During the webinars—attended by > 500 clinicians across the globe (with > 12,000 views of the recorded sessions)—clinicians repeatedly expressed feeling underprepared for the adaptation to telehealth given the lack of resources, training, and guidance and were baffled by the limited reimbursement coverage (particularly in the United States) during the pandemic. This sentiment has been further validated by the hundreds of e-mails we have received as a team to provide support to clinicians on this topic from March 2020 to August 2020.
During this time, several organizations and clinical teams have attempted to help guide clinical practice by publishing narrative reviews, clinical recommendations, or experiential commentaries (e.g., Frajkova et al., 2020; Ku et al., 2020; Miles et al., 2020; Soldatova et al., 2020). In much of this recent literature, telehealth is mentioned briefly as a potential service delivery option for select dysphagia management procedures. Furthermore, for many of these organizations and teams, telehealth has been a brand new venture, and therefore, their recommendations have been based on very novel experiences during the pandemic and/or on scientific evidence largely produced prior to this public health emergency, in which some models are yet to be translated into mainstream clinical practice.
Given the rapid increase of the use of telehealth for dysphagia management globally and the precipitous dissemination of information during the pandemic, we believe it is essential to critically review the recent literature and enhance this information using the prepandemic evidence and our expertise and practice-based knowledge in this area in order to provide evidence- and practice-based recommendations for clinicians. Therefore, the purpose of this clinical focus article is twofold.
First, we aim to provide a rapid systematized review of the telehealth adaptations clinicians made across settings during COVID-19 according to peer-reviewed guidelines, research, and reviews published from January 2020 to August 2020.
Second, using the growing evidence published in the area of dysphagia telehealth, along with our 15 years of clinical and research experience, we aim to enhance the information obtained in Aim 1 and offer evidence-based practice guidelines to assist clinicians to adopt telehealth for dysphagia management both during and critically after the pandemic as well.
Method
Rapid Systematized Review of Telehealth for Dysphagia During COVID-19
Search Strategy
Literature searches were conducted from July 2020 through August 2020 in the following databases: MEDLINE (via PubMed), CINAHL, and Web of Science, including a hand search using Google Scholar. Searches included a combination of controlled vocabulary terms, when applicable, and free-text keywords. The only filter used during the search process was a year filter, limiting the search to 2020, per inclusion criteria. Although COVID-19 was officially declared a pandemic on March 11, 2020, the World Health Organization identified the first cases in late December 2019. Thus, we chose to begin our search in January 2020 to ensure that early 2020 reports or studies (if available) would not be missed. A two-step search was completed. First, the literature was searched using combinations of terms including the following: “COVID,” “pandemic,” “coronavirus,” AND “dysphagia,” “deglutition,” “deglutition disorders,” “swallowing,” AND “telepractice,” “telehealth,” “telemedicine,” “telerehabilitation,” “mobile health units,” “remote consultation.” Terms were nominated by the first author and were further discussed and agreed upon with all authors. However, this first search revealed only five unique results from all databases combined. As part of their regular literature readings, all authors had already identified additional relevant articles; therefore, a second broader search was deemed necessary. The second search was broadened by removing the keywords specific to telehealth in order to capture all COVID-19-related articles on dysphagia and screen each of them for inclusion of telehealth/telepractice considerations and also included a back-chained search of the reference lists of all identified articles. The final search was executed on August 14, 2020, just before manuscript submission, to capture new publications.
Rapid Systematized Review Protocol
Our rapid systematized search followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) protocol (Moher et al., 2009), with the exception of not including a standard risk of bias assessment. Since we identified mostly narrative guideline/review papers and expert opinions, it was not feasible to formally assess risk of bias. Furthermore, this review was constrained by a rapid time frame and did not include an evaluation of the full breadth of literature across time. Therefore, this review is considered a systematized review (Grant & Booth, 2009).
Inclusion and Exclusion Criteria
Studies were included in this systematized review if they met the following criteria: (a) included (or included reference to) human subjects of all ages, (b) were peer-reviewed published articles of any type (including research articles, guideline papers, reviews, case studies, etc.), (c) were written in the English language, (d) included information on both telehealth and dysphagia/swallowing management, and (e) directly referred to the COVID-19 pandemic. Consequently, studies were excluded if they (a) included only animals and (b) were not in English.
Data Extraction and Qualitative Synthesis
The first three authors (G. A. M., R. A., and S. S. M.) independently extracted data from all included articles. Data extracted from all articles included article type (i.e., guideline paper, research study, editorial/commentary), population and setting characteristics, and telehealth specifications. Data extracted specifically on telehealth specifications from all articles included legal and privacy considerations, telehealth safety precautions, patient candidacy criteria, information on Internet connectivity/bandwidth and technology/equipment used, procedure type for which telehealth was used/recommended, and facilitator role. Finally, for each article, the three raters also rated the level of endorsement of telehealth for dysphagia management. Levels of endorsement were arbitrarily defined as the following: negative for articles not endorsing telehealth for dysphagia management, neutral for articles not taking a clear negative or positive stance for dysphagia telehealth, positive—guarded for articles endorsing dysphagia telehealth but expressing reservations about the effectiveness/appropriateness of certain procedures, and positive for articles endorsing use of telehealth for dysphagia management without reservations. During the review, an additional level of endorsement was identified that could not be fully captured by the aforementioned categories; this fifth level (positive—extra guarded) represented articles that, while acknowledging the utility of telehealth for dysphagia, described it as a last resort solution.
Furthermore, for experimental research articles, we planned to extract information on study design, methods, statistical and sample size information, and results; however, no peer-reviewed experimental research studies were identified at this time. The three researchers extracted data with 95% exact agreement on extracted items and reached consensus on the remaining items. Due to the lack of experimental research studies available in the recent literature, quantitative synthesis was not possible; however, a brief qualitative synthesis of findings was completed.
Results of Systematized Review
Study Selection
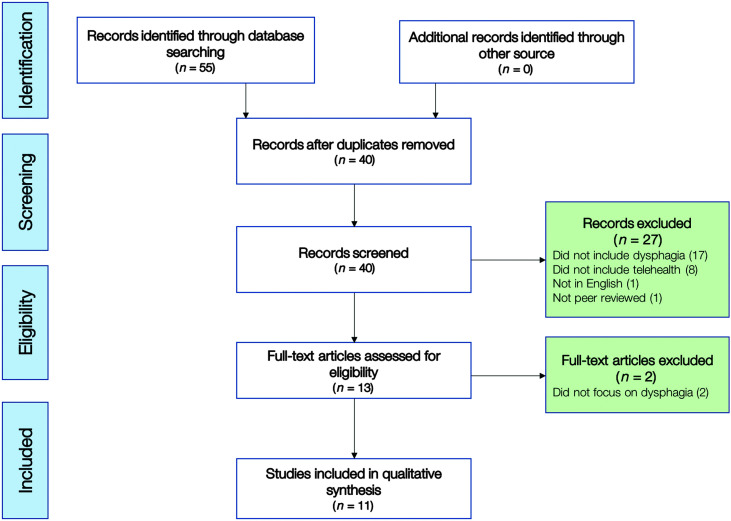
The initial search of three databases (MEDLINE [via PubMed], CINAHL, and Web of Science) in July 2020 retrieved a total of 55 articles, with zero additional unique articles identified via hand search of Google Scholar. Of these 55 articles, 40 were unique (nonduplicates). Two authors (R. A. and S. S. M.) screened the titles and abstracts of the 40 articles for keywords related to dysphagia and COVID-19 (see Figure 1). Then, three authors (G. A. M., R. A., and S. S. M.) independently screened the full text of the remaining 13 articles for eligibility, which resulted in 11 articles meeting the inclusion criteria. Any disagreements were planned to be resolved through consensus, though no disagreements occurred. A final search on August 14 revealed no new articles; therefore, 11 articles were included in the qualitative synthesis.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of the search process used in this systematized review.
Study Types and Demographics
The most common study type identified was “guidelines” (7/11; see Table 1). Of the seven guidelines articles, five were proposed by clinical teams (Fritz et al., 2020; Ku et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Nilsen et al., 2020; Zaga et al., 2020), and two were developed by committees or task forces of global or national associations, that is, the Dysphagia Research Society (Miles et al., 2020) and the French Society of Phoniatrics and Laryngology (Mattei et al., 2020). Three articles (3/11) were editorials or commentaries (Brodsky & Gilbert, 2020; Freitas et al., 2020; Soldatova et al., 2020). The final article was classified as a review article and included a narrative review of prior and contemporary literature (Frajkova et al., 2020). Importantly, only one article was specifically centered on telehealth and dysphagia management during COVID-19 (Soldatova et al., 2020). All other articles mentioned telehealth to varying degrees while primarily focusing on the more general topic of dysphagia management during COVID-19.
Table 1.
Summary of characteristics and specifications of included studies.
| Study | Study type and demographics |
Telehealth specifications |
Strength of endorsement for telehealth | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study type | Population and/or diagnosis | Setting | Age | Legal and privacy | Safety | Patient candidacy | Internet connectivity | Technology and equipment | Procedure type | Facilitator role | Limitations of telehealth | ||
| Brodsky & Gilbert (2020) | Editorial | — | — | — | — | — | — | — | Technical insufficiencies, training, billing reimbursement | Positive (guarded) | |||
| Frajkova et al. (2020) | Narrative review | Post-extubated COVID-19 patients | Acute | Adults | — | — | — | — | — | Case history, clinical eval | — | None | Positive |
| Freitas et al. (2020) | Editorial | COVID-19 patients | Acute, outpatient rehab | Adults | — | — | — | — | — | Rehabilitation only | — | None | Positive (guarded) |
| Fritz et al. (2020) | Guideline (team) | Dysphagia | Acute, outpatient, ambulatory, LTC | Adults | — | — | P | — | — | Clinical eval | — | Medicare coverage | Positive (guarded) |
| Ku et al. (2020) | Guideline (team) | Dysphagia in HNC | Unspecified (mostly outpatient) | Adults | — | — | + | — | — | Clinical eval, therapy | + | Cannot capture all elements of clinical swallow, need advanced prep, specialized tools, limited research on telehealth | Positive (guarded) |
| Mattei et al. (2020) | Guideline (association) | Dysphagia and dysphonia | Unspecified | Adults | P | — | — | — | — | Clinical eval, therapy | — | Not always “technically possible” or “allowed by current regulations” | Positive (guarded) |
| Namasivayam-MacDonald & Riquelme (2020) | Guideline (team) | COVID-19 patients | Acute care | Adults | — | — | — | — | — | Clinical eval, therapy | + | Not the typical form of service delivery | Positive (extra guarded) |
| Miles et al. (2020) | Guideline (association) | Dysphagia | Inpatient and outpatient | All | + | + | + | + | + | Clinical eval, VFSS, therapy | + | Needs more research under current conditions Misdiagnosis is possible |
Positive |
| Nilsen et al. (2020) | Guideline (team) | HNC | Outpatient | Adults | P | — | — | — | — | Therapy, clinical reevals | — | Internet connectivity, regulations, time, lack of interest | Positive |
| Soldatova et al. (2020) | Editorial | Dysphagia | Unspecified (mostly outpatient) | Adults | P | — | P | — | — | Clinical eval, therapy | + | Cannot complete all elements of clinical swallow | Positive |
| Zaga et al. (2020) | Guideline (team) | Tracheostomy and HNC | Acute and LTC | Adults | — | — | P | — | — | Unspecified | — | None | Positive |
Note. P = partial coverage; em dash = not reported; + = adequate coverage; LTC = long-term care; HNC = head and neck cancer; VFSS = videofluoroscopic swallowing study.
Information on demographics (i.e., age groups and specific diagnosis/population) is also included in Table 1. Nine of the 11 articles specified that they were referring to adult populations, one did not specify an age group (but an adult focus could be inferred; Brodsky & Gilbert, 2020), and one stated their focus spanned across the life span; however, pediatric information was only mentioned in two short sections of this article (Miles et al., 2020). No articles discussed pediatric patients in any depth.
In regard to specific diagnoses/populations, four articles discussed dysphagia generally without identifying a specific cause or population (Fritz et al., 2020; Mattei et al., 2020; Miles et al., 2020; Soldatova et al., 2020), three articles discussed dysphagia in COVID-19 patients (Frajkova et al., 2020; Freitas et al., 2020; Namasivayam-MacDonald & Riquelme, 2020), and three articles discussed head and neck cancer (HNC) patients (Ku et al., 2020; Nilsen et al., 2020; Zaga et al., 2020). Of the three articles focused on HNC patients, one specifically included guidance on tracheostomy care (Zaga et al., 2020).
Settings and Procedure
The one article that focused on telehealth and dysphagia during COVID-19 did not specify the settings (e.g., inpatient, outpatient) for which telehealth was being recommended (Soldatova et al., 2020); however, a focus on the outpatient setting could be inferred. Most of the remaining articles with references (of varying levels) to telehealth (7/10) offered information for general dysphagia management adaptations during COVID-19 in specific settings. The most frequent setting explicitly referenced was acute care, which was discussed in five articles (Frajkova et al., 2020; Freitas et al., 2020; Fritz et al., 2020; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020). Four discussed outpatient settings (Freitas et al., 2020; Fritz et al., 2020; Miles et al., 2020; Nilsen et al., 2020), and two made reference to long-term care settings (Fritz et al., 2020; Zaga et al., 2020). Two articles did not specify setting (Ku et al., 2020; Mattei et al., 2020), but one of these articles appeared to be focusing on the outpatient setting based on the populations discussed (Ku et al., 2020). Of the seven articles that reported the setting, six articles further detailed setting recommendations specifically for telehealth. Three discussed the use of telehealth in outpatient settings (Freitas et al., 2020; Miles et al., 2020; Nilsen et al., 2020), and three made reference to telehealth in acute care (Frajkova et al., 2020; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020).
In terms of specific dysphagia procedures for which telehealth was recommended/used, the most frequently reported procedure (8/11 articles) was the clinical swallowing evaluation (CSE; Frajkova et al., 2020; Fritz et al., 2020; Ku et al., 2020; Mattei et al., 2020; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Nilsen et al., 2020; Soldatova et al., 2020). Seven of these eight articles recommended the use of telehealth for initial CSEs or parts of these assessments (Frajkova et al., 2020; Fritz et al., 2020; Ku et al., 2020; Mattei et al., 2020; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Soldatova et al., 2020), and one reported that the initial evaluation in their setting is always conducted in person, but a clinical reevaluation via telehealth is appropriate (Nilsen et al., 2020). Seven articles further mentioned the use of teletherapy for dysphagia (Freitas et al., 2020; Ku et al., 2020; Mattei et al., 2020; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Nilsen et al., 2020; Soldatova et al., 2020), and one article reported the evidence on the use of tele-instrumental evaluations (i.e., televideofluoroscopy) prior to the pandemic (Miles et al., 2020). Finally, one article also supported the use of telehealth for gathering case history information (Frajkova et al., 2020).
Telehealth-Specific Factors
Although all 11 identified articles referenced the use of telehealth for dysphagia management, the lack of detailed specifications or guidelines on factors critical for the implementation of telehealth was glaring. These factors include parameters such as privacy and legal safeguards, safety precautions, patient candidacy criteria, Internet and technology specifications and infrastructure, and facilitator's role (Gough et al., 2015; Richmond et al., 2017). As shown in Table 1, only one article included brief specifications on all six of these parameters (Miles et al., 2020).
Seven articles did not discuss legal safeguards or privacy issues at all (Brodsky & Gilbert, 2020; Frajkova et al., 2020; Freitas et al., 2020; Fritz et al., 2020; Ku et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Zaga et al., 2020), while three articles reported that legal and/or privacy factors are important but did not provide details (Mattei et al., 2020; Nilsen et al., 2020; Soldatova et al., 2020). Two articles discussed some patient candidacy considerations for telehealth (Ku et al., 2020; Miles et al., 2020), three additional articles briefly touched upon this topic (Fritz et al., 2020; Soldatova et al., 2020; Zaga et al., 2020), and six had no reference to patient candidacy considerations (Brodsky & Gilbert, 2020; Frajkova et al., 2020; Freitas et al., 2020; Mattei et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Nilsen et al., 2020). The role of the facilitator (nurse/caregiver) was referenced briefly in four articles (Ku et al., 2020; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Soldatova et al., 2020). Critically, only the guidelines article by the Dysphagia Research Society (Miles et al., 2020) remarked on patient safety and Internet connectivity and technology considerations.
Strength of Endorsement for Telehealth
All 11 articles conveyed some level of support/endorsement for the use of telehealth for dysphagia management during COVID-19; however, the level of support varied. Five conveyed a positive endorsement (Frajkova et al., 2020; Miles et al., 2020; Nilsen et al., 2020; Soldatova et al., 2020; Zaga et al., 2020), and two of these articles emphasized the need for specific recommendations and guidelines to be followed (Miles et al., 2020; Nilsen et al., 2020). Five articles also conveyed positive support for the use of telehealth but were guarded in their recommendations due to reservations about its effectiveness or appropriateness for certain aspects of procedures (Brodsky & Gilbert, 2020; Freitas et al., 2020; Fritz et al., 2020; Ku et al., 2020; Mattei et al., 2020). Lastly, one article recommended telehealth only as a last resort approach, specifically reporting: “In the absence of adequate PPE… this [telepractice] may offer a temporary option in the rare event that the need arises” (Namasivayam-MacDonald & Riquelme, 2020).
Limitations of Telehealth for Dysphagia Management
Most of the articles reported some limitations of telehealth for dysphagia management (8/11). Specifically, four articles reported limitations related to technological and/or logistical insufficiencies (i.e., lack of training, specialized tools, Internet specifications; Brodsky & Gilbert, 2020; Ku et al., 2020; Mattei et al., 2020; Nilsen et al., 2020). Billing and reimbursement difficulties were also discussed briefly in two articles (Brodsky & Gilbert, 2020; Fritz et al., 2020), and federal and state regulations or restrictions were mentioned as potential limitations in two articles as well (Mattei et al., 2020; Nilsen et al., 2020). Two articles reported that not all elements of the CSE could be captured via telehealth (Ku et al., 2020; Soldatova et al., 2020). Lastly, the need for additional research, especially under current pandemic conditions, was highlighted in two articles (Ku et al., 2020; Miles et al., 2020).
Discussion and How to Enhance Current Guidance
The first aim of this clinical focus article was to critically review the recent literature on the area of telehealth for dysphagia management. It is clear from the results of this rapid systematized review that the literature published during the pandemic on this topic is extremely limited. Characteristically, of the 11 articles reviewed, only one specifically focused on telehealth and dysphagia during COVID-19 (Soldatova et al., 2020), and a second included brief guidance on telehealth-specific factors (Miles et al., 2020) that are essential for the safe and effective use of telehealth services. The remaining nine articles mentioned telehealth to varying degrees while primarily focusing on dysphagia management during the pandemic. Many of these articles referred to telehealth as a second-tier service delivery option and not as equivalent to in-person services. Specifically, six of 11 articles (rated as positive—guarded or positive—extra guarded; see Table 1) recommended the use of telehealth for dysphagia management but expressed several reservations (Brodsky & Gilbert, 2020; Mattei et al., 2020) and suggested it only for specific situations or parts of procedures (Freitas et al., 2020; Fritz et al., 2020; Ku et al., 2020) or even as a last resort approach when in-person care would not be feasible (Namasivayam-MacDonald & Riquelme, 2020).
This “better than nothing” approach, in part, parallels the sentiment expressed by several clinicians during our webinars (Burns, Malandraki, & Ward, 2020; Malandraki, 2020b). However, while this sentiment is understandable at this challenging time, it is also alarming and stands in contrast to existing research evidence on the telemanagement of dysphagia. It appears that the lack of resources, infrastructure, and training, in addition to continued reimbursement hurdles, make it so that telehealth for dysphagia care is not perceived as a fully equivalent approach by many clinical teams at this time. However, several organizations, such as the U.S. Center for Connected Health Policy, ASHA, and Speech Pathology Australia, emphasize that services delivered via telehealth should be equivalent to the quality of services offered in-person and that there should be no regulatory distinction between these two types of services (ASHA, n.d.; Burns & Hill, 2014; Telehealth Resource Centers, 2018). It is evident that work needs to be done for these statements to be fully realized for dysphagia telemanagement. This is especially essential if, as a field, we want to embrace the many documented benefits of telehealth for dysphagia care (e.g., Burns et al., 2019, 2017; Malandraki et al., 2013) and aspire toward the goal of telehealth becoming a sustainable and supported service delivery model beyond the pandemic.
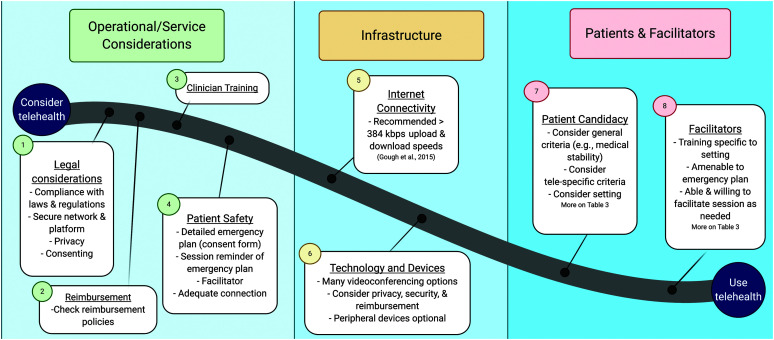
In an effort to help in this direction, the second aim of this clinical focus article is to enhance the contemporary evidence by synthesizing prepandemic and recent evidence with our expertise and practice-based knowledge in this area. Therefore, this last section offers evidence- and practice-based clinical guidance on telehealth considerations as a road map (see Figure 2) that clinicians can use to guide their clinical decision making.
Figure 2.
Road map of considerations for establishing telehealth services. This figure was created with biorender.com.
Legal Considerations and Privacy—Informed Consent
Four of the 11 reviewed articles included some information, and one of them included short but specific guidance, on legal considerations and the topic of privacy when using telehealth. This could be because several legal and privacy restrictions have been temporarily lifted due to the public health emergency (Office for Civil Rights, 2020). Nevertheless, ensuring legal safeguards are in place in order to protect our licensure and the privacy of our patients is a critical endeavor. For telehealth usage specifically, in acute care, subacute rehab, and long-term care settings (henceforth referred to as inpatient settings), risk management and IT teams are typically available to provide consultation and support on this topic (Miles et al., 2020). These teams need to work collaboratively with clinicians so that they can (a) help ensure compliance with all relevant facility and state/country regulations and laws and (b) provide access to a secure network, storage space, and platform that will ensure privacy during the tele-encounters (Gough et al., 2015; Richmond et al., 2017; Turvey et al., 2013). In outpatient clinics, university clinics, and home health settings (henceforth referred to as outpatient settings), this is typically achieved through consultation with legal counsel and IT support, when available.
The risk management or legal counsel teams should also help with the development of facility-specific forms/processes of achieving and documenting informed consent and offer advice or referrals for inquiries related to liability insurance coverage for teleservices. This is important for both inpatient and outpatient settings. The importance of a consent form/process (written or verbal) for provision of teleservices in dysphagia cannot be overstated. According to guidelines by the American Telemedicine Association (ATA) and ASHA, it is advisable that all patients participating in telehealth provide informed consent (ASHA, n.d.; ATA, 2014). This consent should be worded in simple language and should explicitly state the risks and benefits of teleservices, the steps and technical safeguards in place to mitigate any risks, the credentials of the providers, and a detailed emergency/safety plan (Gough et al., 2015; Malandraki & Kantarcigil, 2017; Turvey et al., 2013). In addition, it is of note that, in the United States, several states require informed consent for telehealth services covered by Medicaid programs or as a requirement of the state law.
Patient Safety
The issue of patient safety during tele-encounters was addressed only in one reviewed article (Miles et al., 2020). This was surprising because some of the most frequently asked questions during the webinars (Burns, Malandraki, & Ward, 2020; Malandraki, 2020b) and our communications with clinicians have been: “Can we provide telehealth for dysphagia services safely?,” “What if someone aspirates/chokes during the tele-session?,” and “What happens if the connection is slow or interrupted?” Regarding the first question, the safety of our patients is paramount irrespective of how the service is delivered (in-person or via telehealth). For in-person services across care settings, patients are routinely required to sign waivers or to provide consent for stated risks for various procedures, as well as what they may agree to in unforeseen or emergency situations. Similarly, all clinicians working in health care settings are required to carry current certification in Basic Life Support/Cardiopulmonary Resuscitation and have proficiency in accessing and using an automated external defibrillator in order to quickly address any emergent situation. Luckily, the safety process is similar for telehealth. That is, once a facilitator is secured, an emergency/safety plan needs to be outlined (ideally in the consent form) and agreed upon by the patient/family before the services are initiated (Burns et al., 2019; Gough et al., 2015; Raatz et al., 2019; Turvey et al., 2013).
In inpatient settings, this is relatively simple. Regardless of the physical location of the clinician when providing services (office, outside the room, or home), the patient is located within a medical setting, and therefore, a facilitator (nurse/aide) is typically present in the room with them. Even if an emergency occurs, it can be dealt with rapidly and efficiently. The concern is higher in adult and pediatric outpatient settings where the clinician may be in their clinic and the patient/family at their home, or where both clinician and patient/family are in their respective homes. In this case, a detailed emergency/safety plan needs to be devised, clearly communicated to the patient/family, and included in the consent form that will be signed/agreed upon (Gough et al., 2015; Turvey et al., 2013). At a minimum, this emergency/safety plan should include information about the person who will call 911 in case of an emergency; the contact information of local (at the site of the patient) emergency services; the address for where the patient is located; and the cell phone numbers of the patient, clinician, and facilitator (Gough et al., 2015; Malandraki, 2020a). In addition, the clinician is advised to review the emergency plan in the beginning of each session with the patient and facilitator (Turvey et al., 2013). It is important to highlight that such an emergency/safety plan is recommended for all telehealth encounters across disciplines (Gough et al., 2015; Richmond et al., 2017) and is not specific to dysphagia telecare. Finally, one of the reasons why a facilitator is needed for dysphagia telehealth encounters is for safety (Burns et al., 2017; Malandraki et al., 2011, 2014; Sharma et al., 2012). The facilitator must be capable and agreeable to follow an emergency plan, if needed.
Regarding the second common safety question (“aspiration/choking risk during tele-session”), it must be understood that any person has the potential to aspirate while eating/drinking. It is also true that this risk is higher in those with oropharyngeal dysphagia. Therefore, it is possible that an aspiration or choking event may occur during a dysphagia telesession, particularly during liquid or food trials. However, the same level of risk is present each time the patient eats or drinks. To our knowledge, there is no evidence to suggest that the risk of aspiration/choking is higher during a swallowing evaluation or treatment session versus during any other time a patient is eating or drinking. To the contrary, we argue that speech-language pathologists who treat dysphagia, regardless of service delivery model, are experts trained to reduce this risk. In telehealth settings, this still includes carefully selecting the consistencies and volumes to be trialed, asking the patient/facilitator to stop a specific trial if deemed necessary, and ensuring the patient has performed oral care before oral trials are introduced. The establishment of an emergency plan and the presence of trained facilitators should provide further safeguards against this risk.
Lastly, regarding the question “What happens if the connection is slow or interrupted?,” this issue should also be addressed in the emergency/safety plan. Although it does not always constitute a typical emergency, it is understandable that such a disruption can be concerning, especially in the context of a dysphagia telesession. For that reason, it is recommended that clinicians have an alternative plan in place in the event of a poor connection or technical issues (Gough et al., 2015). This alternative plan may include using phones to reestablish communication right away once connection is lost, using a different videoconferencing platform, having an extra computer or tablet available, or having IT support to deal with such issues (Gough et al., 2015; Turvey et al., 2013). From our recent experiences during the pandemic, at times, small technological tips have made a substantial difference when the patient's or clinician's connection has been slow. These have included disconnecting and reconnecting to the same or a different videoconferencing platform, ensuring all other members in the family/household are not using the Internet during the session to preserve bandwidth, asking the patient/clinician to move closer to the router, plugging in an Ethernet cord instead of using wireless connections, or purchasing wireless extenders or boosters.
Internet Connectivity/Bandwidth and Technology/Equipment
Internet connectivity and technology requirements were also only explicitly discussed in the Dysphagia Research Society guidelines article (Miles et al., 2020). In regard to Internet connectivity, the authors cited the ATA recommendations that suggest bandwidth should be at a minimum of 384 kbps for both upload and download speeds in order to provide a minimum of 640 × 360 resolution at 30 frames per second (Gough et al., 2015). Such a solid connection enables good quality transmission of video and audio data, which is critical for any synchronous (live interaction) telehealth session. However, in prepandemic dysphagia research, synchronous telesessions were conducted safely and effectively even with lower bandwidth levels (as low as 128 kbps), with infrequent issues with video or audio quality (e.g., Ward et al., 2013).
In general, with the increasing availability of broadband Internet in many areas and the recent effort of governments across the globe to further expand its availability, Internet connectivity is significantly improving. In inpatient settings, there is a typically solid and secure Internet connection, whereas in outpatient settings, connectivity may be variable, especially at the patient's end (Collins et al., 2017; Raatz et al., 2019). In a recent study completed during the pandemic, outpatient tele-assessments were conducted successfully even with variable Internet speeds available across both different clinicians and patients (Borders et al., 2020), suggesting the feasibility of this approach under current conditions. In terms of technology and equipment needed, Miles et al. (2020) briefly mentioned that proper hardware, software, and peripheral devices are recommended in order for clinicians to visualize and hear all the information they need. However, no further specifics were provided. In dysphagia telehealth research published prior to the pandemic, both custom-designed (business class) technologies and more widespread but secure (software based) technologies had been used to provide synchronous services (e.g., Burns et al., 2017; Malandraki et al., 2011, 2014; Ward et al., 2013). Currently, there is an abundance of commercial videoconferencing hardware and software from which clinicians can choose. However, in choosing a specific videoconferencing platform for synchronous teleservices, one needs to ensure privacy; security; and, in some cases, even reimbursement considerations have been carefully reviewed for each setting (Malandraki, 2020a).
In inpatient settings, some clinicians reported that, during the pandemic, they were provided with tablets in order to evaluate and treat patients remotely (from outside the room or their office; Burns, Malandraki, & Ward, 2020; Malandraki, 2020b). In outpatient settings, including our own university clinic, various devices (computers, tablets, or phones) have been available at the patient's end during this time. While audiovisual quality may be variable, recent advancements in technology have been remarkable, with most smart devices (phones/tablets) having high-definition cameras and high-quality microphones that allow for excellent audio and video transmission (Collins et al., 2017; Raatz et al., 2019). Indeed, the recently completed preliminary study where patients used their own devices (ranging from smartphones to tablets) to connect with clinicians, who also used variable devices due to the requirement to be at home when providing services, provided the first evidence that clinical tele-assessments are reliable with a variety of devices at both the patient's and the clinician's end (Borders et al., 2020). Based on this prior work and our clinical experiences during the pandemic, it appears that, as long as Internet connectivity is solid and fast, security and privacy safeguards are in place through the use of a secure platform and network, and the clinician can visualize and hear the information needed, a variety of devices can be used (Borders et al., 2020; Collins et al., 2017; Raatz et al., 2019).
Patient Candidacy
Patient candidacy for telehealth was explicitly addressed by two guidelines articles in this review (Ku et al., 2020; Miles et al., 2020). In the Miles et al. (2020) study, it is emphasized that not all patients are appropriate candidates for dysphagia telemanagement, and specific criteria are listed. These include adequate vision and hearing, ability to be positioned in front of a camera, availability and ability of facilitator to intervene if needed, adequate Internet connection, and medical stability (Miles et al., 2020). The authors note that medical stability is a criterion for in-person sessions as well and should be examined similarly for a telehealth encounter. Furthermore, some guidance is provided about candidacy across different settings. In acute care, issues of alertness may inhibit ability to participate; in subacute/long-term care, cognitive status is reported as a potential barrier; and in outpatient settings, availability of facilitators may be an issue (Miles et al., 2020). However, it should be highlighted that prior telehealth research in the area of dysphagia has shown that tele-encounters can be safe and reliable even when patients have mild cognitive decline, as well as physical and/or sensory issues with appropriate session planning and facilitator support (Kantarcigil et al., 2016; Ward et al., 2012a, 2012b). Specifically, facilitators can reduce communication breakdowns between the clinician and patient by adjusting the audio and/or by clarifying/repeating directions, questions, and comments (Ward et al., 2012a).
Ku et al. (2020) also list patient selection criteria in one of their tables. These include willingness of patients and caregivers/facilitators to participate in telehealth and addressing problems that can be tackled by indirect training, consultation, and education. This last criterion appears to reflect the belief that direct intervention (i.e., involving oral trials) is not appropriate via telehealth. Although this belief is understandable in a pandemic era, a plethora of prior evidence suggests that direct approaches for the evaluation and management of dysphagia are safe, feasible, and reliable via telehealth (e.g., Burns et al., 2019, 2016; Collins et al., 2017; Malandraki et al., 2011; Raatz et al., 2019; Ward et al., 2013, 2012b). Importantly, emerging evidence with data collected during the pandemic in an outpatient setting also supports the safety and reliability of clinical swallowing tele-assessments, including the administration of oral trials at this time (Borders et al., 2020). Table 2 summarizes patient candidacy considerations across settings.
Table 2.
Dysphagia telehealth patient candidacy and facilitator characteristics with special considerations across settings/age.
| Variable | General (across settings/age) | Inpatient care (acute, subacute rehab, long-term care) | Outpatient care (clinics, home health) | Pediatrics |
|---|---|---|---|---|
| Patient candidacy | • Adequate hearing and vision • Medical stability • Ability to be positioned in front of device • Adequate Internet connection • Alertness • Cognitive status • Availability and willingness of a facilitator |
• Alertness of patient may be a barrier • Cognitive status may be a barrier • Facilitator critical for safety and helping with session tasks |
• Cognitive status may be a barrier • Facilitator critical for safety and helping with tasks (less frequent) |
• Child's ability to pay attention and engage in activities • Willingness of parent to be involved in the session • Willingness of parent to help with behavior management, as needed |
| Facilitator characteristics | • Ability and willingness to follow emergency plan • Ability to help with environmental and technological adaptations • Ability and willingness to help with specific session tasks, if needed • Ability to support patient's engagement, if cognitive and/or sensory issues are present |
• Typically readily available (e.g., nurse) • Training on direct facilitation/help with session tasks • Typically directly involved in session tasks |
• Caregiver, family member, or trained health care worker • Training for emergency plan and session facilitation • Direct involvement in session may or may not be needed |
• Typically a parent • Training for emergency plan and session facilitation • Always directly involved in the session |
Note. Primary resources: ASHA (n.d.), ATA (2014), Malandraki (2020a), and Queensland Health e-Learning Program (2020).
Telehealth for Specific Dysphagia Procedures
Clinical Swallowing Tele-Evaluations
During the pandemic and due to the many postponements or cancellations of instrumental swallowing assessments, clinicians have been often forced to rely solely on CSEs (Fritz et al., 2020; Ku et al., 2020; Soldatova et al., 2020). The majority of articles included in this systematized review (7/11) overall supported the use of telehealth for initial CSEs or parts of this assessment (Frajkova et al., 2020; Fritz et al., 2020; Ku et al., 2020; Mattei et al., 2020; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Soldatova et al., 2020).
This is logical since most prior research in the area of telehealth and dysphagia has provided positive evidence for the reliability and validity of tele-CSEs (e.g., Burns et al., 2019; Kantarcigil et al., 2016; Ward et al., 2012b). This prepandemic evidence is based primarily on studies conducted in outpatient settings, with some studies including inpatient or mixed inpatient and outpatient samples as well (Burns et al., 2019; Ward et al., 2014, 2012b). During the pandemic, preliminary evidence for the feasibility and reliability of tele-CSEs in outpatient settings is starting to emerge (Borders et al., 2020). Despite that, two reviewed articles supported that only portions of a CSE can be completed via telehealth without specifying these portions (Ku et al., 2020; Soldatova et al., 2020), and one of the reviewed articles took a more conservative approach and suggested telehealth usage only for clinical reevaluations (Nilsen et al., 2020).
In inpatient settings, research on the feasibility and utility of tele-CSEs is documented by few studies prior to the pandemic, and studies reporting on services conducted during the pandemic are beginning to emerge. Anecdotal reports and a gray literature article published in the August/September 2020 issue of The ASHA Leader have provided initial support for the feasibility of this approach. Specifically, Kurtz (2020) described adaptations that were made in their acute care hospital in order to be able to continue conducting CSEs for their intensive care unit (ICU) patients. They took advantage of a high-definition ICU camera system typically used by nurses and MDs to monitor patients' vital signs and provide consultation and used it successfully to perform tele-CSEs. They report getting training in the system by nurses, establishing specific candidacy criteria for patients, and using the nurse as a facilitator for the sessions (Kurtz, 2020). Further studies reporting on the use of telehealth for dysphagia services with a range of inpatient populations, including patients in the ICU, are needed, and during the pandemic, it is critical that speech-language pathologists continue to provide their services to these patients safely and effectively, by using either appropriate PPE or telehealth.
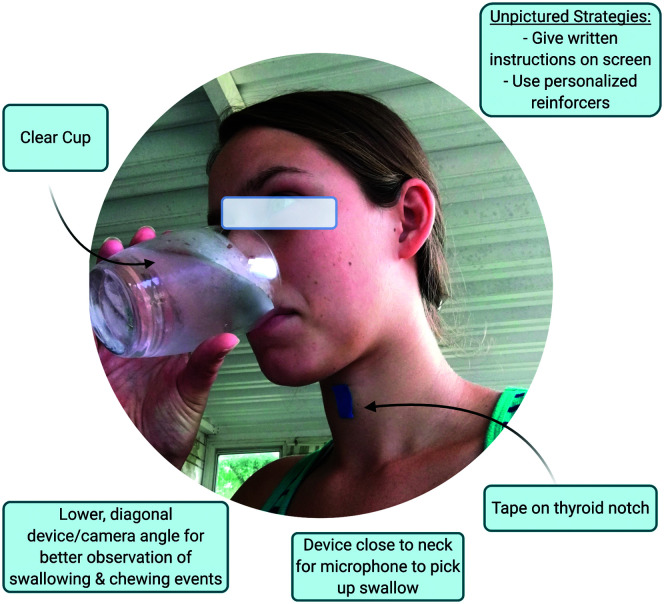
Irrespective of the exact setting (inpatient or outpatient), a few parameters have been recognized, by both existing and more recent research, as useful during these assessments. Clinical swallowing assessments typically include case history interviews; a cranial nerve and oropharyngeal mechanism assessment; and, at times, trials of foods and liquids. For the cranial nerve assessment conducted via telehealth, positioning of the camera/device at the patient's end may need to be adjusted for the best views of areas that need to be visualized for each component of the examination. In our clinical practice, this has, at times, included the addition of another video device, such as a peripheral camera, if available, or the facilitator connecting to the session with their own phone/tablet to provide an easily manipulated/repositioned video source. Clinicians need to provide clear instructions to the patient/facilitator for guidance on the exact positioning and visualization needed. For oral trials, use of clear cups/glasses and utensils has been recommended to help visualize amounts of liquids/foods consumed by the patient (Borders et al., 2020; Malandraki et al., 2014; Ward et al., 2014, 2012a, 2012b). In addition, lateral or diagonal positioning of the patient toward the camera, closer views to clearly see the face and neck and allow for better audio acquisition, and use of colored tape on the thyroid notch (Borders et al., 2020; Malandraki et al., 2014; Ward et al., 2014) are simple tips that can improve observation of swallows and signs of difficulty during oral trials (see Figure 3). Finally, when synchronous tele-assessment does not allow for acquisition of all data points needed to complete our assessment, the use of asynchronous methods (store and forward) can significantly complement the synchronous procedure. For instance, parents can send videos of their child consuming a meal/snack in their home environment (Kantarcigil et al., 2016) or a photograph of the seating to the clinician (Raatz et al., 2019) prior to the session in order to help guide the assessment.
Figure 3.
Patient positioning and adaptations to support tele-assessment during oral trials. Sources: Borders et al. (2020), Malandraki et al. (2014), and Ward et al. (2014, 2012b). This figure was created with biorender.com.
It should be noted that some of the reviewed articles recommended the use of specific validated clinical evaluation tools, screenings, or patient-reported outcome measures via telehealth (Fritz et al., 2020; Ku et al., 2020). In general, supplementing the CSE with the use of validated tools and patient-reported outcome measures is highly recommended in order to further standardize the assessment and enhance validity. However, most of these tools have not been tested/validated for online use. For tests including only swallow observations or completion of survey questions, it is possible that such testing/validation may not be fully necessary, as validations of similar tools have been demonstrated. For example, online case history completion by outpatients with suspected dysphagia has been shown to be an effective alternative to in-person case history completion (Kantarcigil & Malandraki, 2017). For added fidelity, we recommend clinicians take the following steps when planning to use such tools as part of their tele-CSE. First, we recommend reaching out to the individuals who developed the tool to inquire about online options, as well as gain first-hand insight into the translatability of the tool from an in-person to an online format, and obtain any necessary permissions. Second, it would also be important to disclose the usage of all tools, their validation status for online use, and their potential limitations in their clinical documentation.
Instrumental Swallowing Tele-Evaluations
Upon completion of the CSE, clinicians are required to weigh the benefits and risks of completing an instrumental assessment with each patient. During this pandemic, in an attempt to lower exposure risks, only patients identified as high risk for silent aspiration and dysphagia have been referred for instrumental assessments, and for many other patients, these procedures have been postponed or canceled (Fritz et al., 2020; Ku et al., 2020; Mattei et al., 2020; Soldatova et al., 2020). The use of telehealth for instrumental assessments could offer a valuable alternative; however, its use in clinical practice is currently minimal (with rare exceptions outside the United States).
Only one article in this review reported the evidence on the use of tele-instrumental evaluations (i.e., tele-VFSS) prior to the pandemic (Miles et al., 2020). These pre–COVID-19 studies have supported the reliability and validity of tele-VFSS assessments (Burns et al., 2016; Malandraki et al., 2011; Perlman & Witthawaskul, 2002). At the time of this clinical focus article's submission, there were no published data on the use of instrumental swallowing tele-assessments during the pandemic. The gray literature article by Kurtz supported the use of a videofluoroscopic c-arm at the bedside to conduct VFSS evaluations in their ICU; however, the clinician or nurse was in the room with the patient during this assessment (Kurtz, 2020). This further highlights the urgent need to conduct research in this area under and despite current conditions in order to offer guidance for clinicians to be able to continue providing standard of care procedures to their patients. In addition, research efforts on the development and validation of tools that will allow noninvasive and remote measurement of swallowing need to be accelerated (Brodsky & Gilbert 2020).
Swallowing Telerehabilitation
Seven reviewed articles further mentioned the use of telehealth for the rehabilitation of dysphagia without providing explicit guidance on the topic. Three reviewed articles focused on dysphagia management in patients with tracheostomies and HNC (Ku et al., 2020; Nilsen et al., 2020; Zaga et al., 2020) and emphasized that both populations require long-term care and follow-up appointments, which could not cease during the pandemic. Therefore, teletherapy was strongly proposed as an effective approach to continue care for these populations while maintaining appropriate physical distancing. However, the article by Ku et al. (2020) took a more conservative stance and suggested the use of telehealth for indirect treatment approaches (e.g., for patient education, home program delivery, and monitoring) during this time.
Pre-COVID-19 evidence for the feasibility and effectiveness of synchronous dysphagia telerehabilitation is also positive, but emerging (Burns et al., 2017; Malandraki et al., 2013, 2014). Based on our experiences before and during the pandemic, several of the adaptations discussed in the Clinical Swallowing Tele-Evaluations subsection earlier (e.g., positioning of patient and cameras, ideal views for oral trials observations, clear cups and utensils) are applicable to swallowing teletherapy as well. Based on emerging evidence and our clinical practice, two additional strategies have been useful for swallowing teletherapy. First, developing typed scripts and visual aids, including step-by-step instructions of treatment approaches/exercises, has been helpful (Burns, Malandraki, & Ward, 2020; Collins et al., 2017; Malandraki, 2020a). This enhances standardization of our approaches and has proven beneficial for patients who cannot easily understand verbal instructions, especially virtually. Second, particularly for some pediatric patients and/or patients with intellectual and developmental disabilities, using personalized reinforcements, such as personalized online cards/videos, or favorite items has also been effective to engage the patients in therapy (e.g., Malandraki et al., 2014).
Furthermore, two reviewed articles conveyed support for the use of mobile applications and wearable devices for provision of telerehabilitation for dysphagia (Brodsky & Gilbert, 2020; Soldatova et al., 2020). Indeed, there are now several apps or devices that allow for remote tracking/monitoring of the patient's performance on rehabilitative exercises, allowing for clinicians to be able to keep data, track progress, and provide feedback to patients (e.g., Burns, Wishart, et al., 2020; Constantinescu et al., 2017; Kim et al., 2019; Starmer et al., 2018; Wall et al., 2016). It is our hope that the development and validation of such technologies will be accelerated during this time and advanced research and commercialization efforts will help establish their role in the care of our patients.
Patient Facilitator/Helper
The role of the facilitator (nurse/caregiver/parent) was referenced briefly in four articles of this review (Ku et al., 2020; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Soldatova et al., 2020). The use of trained facilitators has been repeatedly supported in prior dysphagia telehealth research (e.g., Burns et al., 2017; Malandraki et al., 2011, 2014; Raatz et al., 2019; Sharma et al., 2012; Ward et al., 2013). It is important to clarify that the role of facilitators is to help patients in the use of technology, connecting with the clinician, and environmental adaptations (Alvares, 2013; Queensland Health e-Learning Program, 2020) and to be available to address safety/emergency issues if needed. In addition and upon training, they can help with completing tasks in order to facilitate the evaluation or treatment (e.g., help with sensory testing during a cranial nerve assessment; Malandraki et al., 2014; Sharma et al., 2012). As stated in Miles et al. (2020), facilitators are critical for all the aforementioned reasons but should not be used as substitutes or proxies for the dysphagia specialist. Both pre-COVID-19 evidence and current published guidance support the use of trained facilitators (Ku et al., 2020; Malandraki et al., 2014; Miles et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Sharma et al., 2012; Soldatova et al., 2020) and suggest taking the time to train the facilitators and ensuring they feel comfortable and able to address any safety issues that may arise (Miles et al., 2020; Queensland Health e-Learning Program, 2020).
In inpatient settings, facilitators are readily available (e.g., nurses or aides), and they are generally accustomed to addressing safety issues when those occur. In telehealth service delivery, their role can be rather critical and direct, given that many of these patients may have reduced alertness and/or impaired cognition (Miles et al., 2020). Facilitators in inpatient settings are needed to facilitate patient engagement and participation in telehealth sessions, as well as to ensure all tasks are completed safely. In outpatient settings, facilitators can also be caregivers or family members/parents and will require variable levels of training and support, depending on their comfort level with technology and their overall caregivers' experiences (see Table 2; Malandraki et al., 2014; Sharma et al., 2012). Our recent clinical experiences have further shown that online facilitator training is feasible and can be effective.
Clinician Training for Telehealth
Importantly, only two of the reviewed articles made a brief mention to the need for clinical training in telehealth service delivery (Brodsky & Gilbert, 2020; Miles et al., 2020). In a survey conducted prior to the pandemic, clinicians expressed positive interest in providing pediatric dysphagia services via telehealth, but relatively few of them reported access to telehealth training opportunities (Raatz, Ward, & Marshall, 2020). This is consistent with our anecdotal conversations with clinicians during the pandemic, who expressed feeling unprepared for the rapid transition to telehealth (Burns, Malandraki, & Ward, 2020; Malandraki, 2020b). Although during this time, based on clinical reports, several clinicians have transitioned to telehealth methods without formal training, it needs to be emphasized that formal training is imperative, as has been shown in prior research (Burns et al., 2019, 2017), and should be established. To that end, several clinical/research teams and professional federal and state (in the United States) associations have already developed training modules for telehealth services in general (California Telehealth Resource Center, 2020) and for dysphagia or speech pathology specifically (Queensland Health e-Learning Program, 2020; University of Maine, 2020), and more specialized ones are being developed.
Proximity—Fear of Being Away From the Patient
In addition to safety concerns, another frequently expressed fear of clinicians for the use of telehealth for dysphagia management has been the lack of proximity (Burns, Malandraki, & Ward, 2020; Malandraki, 2020b; Miles et al., 2020). Many clinicians state that their effectiveness may be reduced when the clinician is providing care remotely (Burns, Malandraki, & Ward, 2020; Malandraki, 2020b; Miles et al., 2020). During in-person care, clinicians can themselves perform hands-on activities (such as strength and sensory testing), can see and hear the patient and their responses clearly, and can directly respond to an emergency situation. Although these are all legitimate reasons to prefer in-person care, both pre-COVID-19 and emerging current evidence suggest that most of these components can be safely and reliably addressed via telehealth as well (Borders et al., 2020; Burns et al., 2019, 2016; Malandraki et al., 2011; Perlman & Witthawaskul, 2002; Ward et al., 2014, 2012b). Furthermore, as stated by Miles et al. (2020), “it can be argued that providing services with heavy PPE, the use of face shields or with a plexiglass separating patient and clinician pose many of the same challenges as telehealth.” With increased knowledge of the research and proper training on how to engage in dysphagia telecare, these fears should be assuaged.
What About Pediatrics?
Perhaps one of the most disheartening findings of our systematized review was that no articles discussed the use of telehealth during the pandemic for pediatric patients. Pediatricians report that the needs of developmental pediatric patients need to be addressed now, not after the pandemic, and highly recommend the use of telemedicine as a tool to continue to provide essential care to pediatric patients (Fung & Ricci, 2020). Early childhood is a time of immense growth and learning in relation to feeding and swallowing, and it could be particularly disruptive if children do not receive necessary intervention for dysphagia during these critical periods (Delaney & Arvedson, 2008). Although we found no data on how pediatric dysphagia services have been affected during the COVID-19 crisis, it has been documented that many young children have missed well-child visits and vaccinations (Santoli et al., 2020). Thus, it is likely that some children may have also missed care more directly related to feeding and swallowing.
Providing dysphagia services to pediatric patients both during and after the pandemic is vitally important. Delivering these services via telehealth is possible and may be particularly advantageous for certain pediatric patients. One study surveyed parents to identify factors limiting participation in outpatient pediatric feeding services (Raatz, Ward, Marshall, Afoakwah, & Byrnes, 2020). They found three main barriers: distance and travel, impact on daily activities (i.e., work, school), and parent perception that in-clinic sessions were an inaccurate representation of the child's feeding skills. Telehealth can address all of these issues effectively, as it eliminates travel; minimizes impact on daily activities; and, if done from home, provides a more naturalistic view of a child's eating environment and functional skills (Malandraki et al., 2014). Additionally, if a child is having difficulty generalizing feeding behaviors from the clinic to their home, telehealth may be a unique solution to encourage generalization (Clark et al., 2019).
Prior to the pandemic, a small number of studies had demonstrated the feasibility of implementing telehealth for children with dysphagia. One of the first studies was a case report presenting the preliminary effectiveness of a 4-week pediatric swallowing telepractice program in improving oral acceptance of foods and other swallowing parameters in a pediatric patient with complex medical history and dysphagia (Malandraki et al., 2014). A later study by Kantarcigil et al. (2016) including school-age children with cerebral palsy showed that asynchronous CSEs including a validated tool (i.e., the Dysphagia Disorder Survey) were reliable when compared to in-person administration of the same tool. More recently, Raatz et al. (2019) described the development of system architecture for conducting pediatric feeding assessments of infants and children via telehealth. Additionally, an interdisciplinary feeding team described using telehealth to deliver outpatient feeding therapy to children between the ages of 4 and 10 years. They reported cost savings, enhanced flexibility of service provision, and improved generalization in several of their cases (Clark et al., 2019).
This early preliminary evidence shows that the use of telehealth for pediatric dysphagia is promising; however, no data are yet available for the COVID-19 period. We know that general pediatric medicine systems have rapidly shifted care by limiting in-person visits, increasing precautions when in-person care is necessary, and increasing use of telehealth across all pediatric disciplines (Patel et al., 2020). From our communications with pediatric clinicians, we also know that many have adapted to the use of telehealth for pediatric feeding and swallowing services (Burns, Malandraki, & Ward, 2020; Malandraki, 2020b). Similar to their colleagues focusing on adults, feelings of unpreparedness and apprehension have been expressed. In addition, in the survey study by Raatz, Ward, Marshall, Afoakwah, and Byrnes (2020), it was evident that many pediatric clinicians have a high interest in providing these services via telehealth but report minimal experience. Based on the existing evidence, along with our clinical experience and evidence on adaptations made in other pediatric fields during the pandemic, the following recommendations are provided.
First, all telehealth-specific considerations discussed earlier (e.g., legal safeguards and privacy, safety, technology and connectivity, facilitator's role; see Figure 2) are directly relevant and need to be carefully considered for pediatric patients as well. However, working with pediatric patients via telehealth presents some additional unique challenges and requires special considerations. In regard to legal and procedural adaptations, complexities related to parentage documentation, identity verification, and adolescent assent need to be considered (Patel et al., 2020). Legal counsel will be critical as clinicians need to investigate these topics in local laws and policies that may differ by state and setting.
Furthermore, one of the most important telehealth considerations to highlight is the required presence of a trained facilitator when working with children (see Table 2). Typically, the child's parent or caregiver is the facilitator, and in addition to their standard facilitator roles discussed previously, they will now need to directly assist with feeding (in most situations), as well as with behavior management and reinforcement, as needed. In fact, in pediatric feeding therapy, many times the parent is the direct recipient of our services, as we are coaching them on how to help their little ones improve their feeding and swallowing skills. Providing the parent or caregiver with written instructions and/or factsheets can be beneficial to support their training and knowledge of tasks during telehealth sessions (Malandraki et al., 2014; Raatz et al., 2019). One pediatric study required at least one in-person session to provide family training and establish rapport (Clark et al., 2019); however, we have also conducted these trainings remotely with success (Malandraki et al., 2014).
In addition to parental facilitation, maximizing child attention and engagement is an essential consideration to providing high-quality pediatric services via telehealth. Studies have reported slightly reduced child attention for early intervention and speech therapy delivered via telehealth (Wales et al., 2017; Yang et al., 2020). Therefore, clinicians must carefully consider strategies to maximize engagement, such as the intentional use of reinforcements. We have found that creating personalized images/videos with topics of high interest to the child and presenting them on screen as rewards can be an effective reinforcement strategy (Malandraki et al., 2014). Additionally, many clinicians report use of video backgrounds (green screens) or online games as successful reinforcing activities. However, it is clear that some children may not prefer virtual reinforcements or virtual therapy. Strategies that can be helpful in such cases include using “screenless” teletherapy, where the clinician does not appear on the screen but coaches the parent via headphones on specific strategies and can still observe and hear the child's responses (Nicolet, 2020) or using real-life objects and foods that both the clinician and child have available to play “show and tell” and engage in feeding activities or food “science experiments.” We have further found that using music and movement/dance type activities may be an effective reinforcement via telehealth.
Additional considerations are related to seating and hands-on equipment. In clinical settings, many pediatric clinicians report use of specialized seating, utensils, or equipment to promote positive feeding experiences (Mitchell & Paluszak, 2018). If sessions are occurring within the child's home, it is unlikely that specialized options will be available. This may pose a level of difficulty for the treating clinicians but will provide a more accurate representation of how the child is supported during eating in their natural environment. Particularly for pediatrics, using an external camera or an additional device to connect to the session (in order to use it as an added video source) may be rather beneficial. This external or additional video source can provide closer/clearer or added views of the child or parts of their anatomy (e.g., oral cavity), which can offer critical information to the clinician. This external camera is particularly imperative if clinicians are evaluating breastfeeding (Raatz et al., 2019). Finally, as mentioned earlier, the use of asynchronous methods (e.g., parents video-recording and sending videos of their child eating a meal/snack in their home [Kantarcigil et al., 2016] or videos of their child's oral cavity [Raatz et al., 2019] to the clinician in advance of the session) can offer important insight into the child's real-life feeding and swallowing behaviors and provide information difficult to capture during a synchronous session.
Limitations of Telehealth for Dysphagia Management
Telehealth is not a cure-all. The need to integrate technology, determine patient appropriateness, and adapt the clinical tasks means that telehealth is not appropriate for all patients or for all services (ASHA, n.d.; Malandraki, 2020a). Evidence to date supports its use as an equivalent alternative to in-person dysphagia care for adults in outpatient and some inpatient settings, with growing evidence in the area of pediatrics. Evidence from inpatient settings and in pediatrics has also started to emerge but is limited (Burns et al., 2019; Kantarcigil et al., 2016; Raatz et al., 2019). The good news is that new evidence further suggests that this approach is feasible and reliable even under current pandemic conditions (i.e., conditions with great variability in technology/infrastructure, rapid and remote clinician and facilitator training, rapid adoption of telehealth, variable Internet connectivity, and limited resources; Borders et al., 2020). However, there is a need to accumulate more evidence for the use of telehealth for dysphagia services in more populations (inpatients, pediatrics, etc.) and across types of services (e.g., treatment) and settings. Additional limitations listed by the reviewed articles included limitations related to technological and/or logistical insufficiencies (i.e., lack of training, specialized tools, Internet connectivity), limited information obtained, regulatory restrictions, and reimbursement issues. We have provided evidence- and practice-based solutions that address some of these limitations (e.g., technology and clinical adaptations to enhance information acquired via telehealth) in our discussion. In addition, recently, organizations and clinical research teams have provided free online resources providing education and guidance regarding telehealth for dysphagia (Malandraki, 2020a; Queensland Health e-Learning Program, 2020), and further specialized trainings and continuing education unit events are constantly becoming available. Regulatory and reimbursement restrictions are harder to address and require significant advocacy at the national and state levels to change, in addition to further research efforts to build the evidence base in more settings, in more populations, and across dysphagia procedures. Finally, the need for experimental research under pandemic conditions, as well as for interdisciplinary and clinic–industry collaborations to enable more rapid clinical translation of technological innovations, is urgent and cannot be overemphasized.
Conclusions
Our aim in this clinical focus article was to critically review the recent literature on the use of telehealth for dysphagia management and enhance this information using our expertise in order to provide evidence- and practice-based guidance for clinicians during the pandemic and beyond. The literature published during the pandemic on this topic is extremely limited, and it appears that the lack of infrastructure and training, in addition to reimbursement restrictions, has contributed to telehealth being perceived as a second-tier service delivery option for dysphagia at this time. However, it is universally reflected in professional guidelines that services delivered via telehealth should be equivalent to the quality of services offered in-person (ASHA, n.d.). In the second part of this clinical focus article, we have offered prepandemic and emerging contemporary evidence for the safety, feasibility, and reliability of dysphagia telemanagement, in combination with practice-based experiences to facilitate the inroads of our field in adopting telehealth as it should be, an equivalent service delivery approach. More work in terms of experimental research under current conditions, development of specialized trainings, and advocacy is needed to further help in this direction. This pandemic provided extraordinary clinical challenges but also offered unique opportunities for our field to grow and adapt in order to continue to serve our patients. We believe that telehealth has the potential to be a twofold solution. In the short term, it can clearly be an important response to challenges created by the COVID-19 pandemic, and in the long term, it can be a solution to several long-standing barriers to service provision in feeding and swallowing.
Acknowledgments
The first author was partially supported by the National Institute of Biomedical Imaging and Bioengineering R21 Trailblazer Grant 1R21EB026099-01A1 (Georgia A. Malandraki and Chi Hwan Lee, equal PIs) for this work.
Funding Statement
The first author was partially supported by the National Institute of Biomedical Imaging and Bioengineering R21 Trailblazer Grant 1R21EB026099-01A1 (Georgia A. Malandraki and Chi Hwan Lee, equal PIs) for this work.
References
- Alvares, R. (2013). Working with facilitators to provide school-based speech and language intervention via telepractice. SIG 18 Perspectives on Telepractice, 3(2), 44–48. https://doi.org/10.1044/teles3.2.44 [Google Scholar]
- American Occupational Therapy Association. (2020). COVID-19 occupational therapy service delivery guide. https://www.aota.org/-/media/Corporate/Files/Practice/Health/COVID-19-OT-Service-Delivery-Guide.pdf
- American Speech-Language-Hearing Association. (n.d.). Telepractice. https://www.asha.org/Practice-Portal/Professional-Issues/Telepractice/
- American Telemedicine Association. (2014). Core operational guidelines for telehealth services involving provider-patient interactions. https://www.uwyo.edu/wind/_files/docs/wytn-doc/toolkit-docs/ata_core_provider.pdf
- Bolton, L. , Mills, C. , Wallace, S. , Brady, M. C. , & Royal College of Speech and Language Therapists COVID-19 Advisory Group. (2020). Aerosol generating procedures, dysphagia assessment and COVID-19: A rapid review. International Journal of Language & Communication Disorders, 55(4), 629–636. https://doi.org/10.1111/1460-6984.12544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borders, J. C. , Sevitz, J. S. , Bauer Malandraki, J. , Malandraki, G. A. , & Troche, M. S. (2020). Objective and subjective clinical swallowing outcomes via telehealth during COVID-19: A reliability study [Manuscript submitted for publication]. [DOI] [PubMed]
- Brodsky, M. B. , & Gilbert, R. J. (2020). The long-term effects of COVID-19 on dysphagia evaluation and treatment. Archives of Physical Medicine and Rehabilitation, 101(9), 1662–1664. https://doi.org/10.1016/j.apmr.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns, C. L. , & Hill, A. (2014). Speech Pathology Australia position statement: Telepractice in speech pathology. Speech Pathology Australia. https://www.speechpathologyaustralia.org.au/SPAweb/Members/Position_Statements/spaweb/Members/Position_Statements/Position_Statements.aspx?hkey=dedc1a49-75de-474a-8bcb-bfbd2ac078b7 [Google Scholar]
- Burns, C. L. , Malandraki, G. A. , & Ward, E. C. (2020, May 4). Dysphagia and telepractice during COVID-19 and beyond [Webinar] . American Speech-Language-Hearing Association. https://asha.zoom.us/rec/play/vJEuJO_5rDg3S9ec4wSDV6QsW9S0f62s1CAW-vULxBzgAHEKZ1GlN-AbNuOOGI30Oniav1gTt7wfWIBl?continueMode=true&_x_zm_rtaid=4qQCe6H-Qt-Ufzb1y0JCfQ.1588697367989.6382bb7268e0784f548fddbc69930027&_x_zm_rhtaid=330 [Google Scholar]
- Burns, C. L. , Ward, E. C. , Gray, A. , Baker, L. , Cowie, B. , Winter, N. , Rusch, R. , Saxon, R. , Barnes, S. , & Turvey, J. (2019). Implementation of speech pathology telepractice services for clinical swallowing assessment: An evaluation of service outcomes, costs and consumer satisfaction. Journal of Telemedicine and Telecare, 25(9), 545–551. https://doi.org/10.1177/1357633X19873248 [DOI] [PubMed] [Google Scholar]
- Burns, C. L. , Ward, E. C. , Hill, A. J. , Kularatna, S. , Byrnes, J. , & Kenny, L. M. (2017). Randomized controlled trial of a multisite speech pathology telepractice service providing swallowing and communication intervention to patients with head and neck cancer: Evaluation of service outcomes. Head & Neck, 39(5), 932–939. https://doi.org/10.1002/hed.24706 [DOI] [PubMed] [Google Scholar]
- Burns, C. L. , Ward, E. C. , Hill, A. J. , Phillips, N. , & Porter, L. (2016). Conducting real-time videofluoroscopic swallow study via telepractice: A preliminary feasibility and reliability study. Dysphagia, 31(3), 473–483. https://doi.org/10.1007/s00455-016-9701-2 [DOI] [PubMed] [Google Scholar]
- Burns, C. L. , Wishart, L. R. , Kularatna, S. , & Ward, E. C. (2020). Knowing the costs of change: An introduction to health economic analyses and considerations for their use in implementation research. Speech, Language and Hearing, 23(1), 30–36. https://doi.org/10.1080/2050571X.2019.1693750 [Google Scholar]
- California Telehealth Resource Center. (2020). Training [online] . https://www.caltrc.org/knowledge-center/training/ [Google Scholar]
- Cipolat, C. , & Geiges, M. (2003). The history of telemedicine. Current Problems in Dermatology, 32, 6–11. https://doi.org/10.1159/000067346 [DOI] [PubMed] [Google Scholar]
- Clark, R. R. , Fischer, A. J. , Lehman, E. L. , & Bloomfield, B. S. (2019). Developing and implementing a telehealth enhanced interdisciplinary pediatric feeding disorders clinic: A program description and evaluation. Journal of Developmental and Physical Disabilities, 31(2), 171–188. https://doi.org/10.1007/s10882-018-9652-7 [Google Scholar]
- Collins, A. , Burns, C. L. , Ward, E. C. , Comans, T. , Blake, C. , Kenny, L. , Greenup, P. , & Best, D. (2017). Home-based telehealth service for swallowing and nutrition management following head and neck cancer treatment. Journal of Telemedicine and Telecare, 23(10), 866–872. https://doi.org/10.1177/1357633X17733020 [DOI] [PubMed] [Google Scholar]
- Constantinescu, G. , Loewen, I. , King, B. , Brodt, C. , Hodgetts, W. , & Rieger, J. (2017). Designing a mobile health app for patients with dysphagia following head and neck cancer: A qualitative study. JMIR Rehabilitation and Assistive Technologies, 4(1), Article e3. https://doi.org/10.2196/rehab.6319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delaney, A. L. , & Arvedson, J. C. (2008). Development of swallowing and feeding: Prenatal through first year of life. Developmental Disabilities Research Reviews, 14(2), 105–117. https://doi.org/10.1002/ddrr.16 [DOI] [PubMed] [Google Scholar]
- Frajkova, Z. , Tedla, M. , Tedlova, E. , Suchankova, M. , & Geneid, A. (2020). Postintubation dysphagia during COVID-19 outbreak—Contemporary review. Dysphagia, 35(4), 549–557. https://doi.org/10.1007/s00455-020-10139-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freitas, A. S. , Zica, G. M. , & de Albuquerque, C. L. (2020). Coronavirus pandemic (COVID-19): What speech therapists should know. CoDAS, 32(3), Article e20200073. https://doi.org/10.1590/2317-1782/20192020073 [DOI] [PubMed] [Google Scholar]
- Fritz, M. A. , Howell, R. J. , Brodsky, M. B. , Suiter, D. M. , Dhar, S. I. , Rameau, A. , Richard, T. , Skelley, M. , Ashford, J. R. , O'Rourke, A. K. , & Kuhn, M. A. (2020). Moving forward with dysphagia care: Implementing strategies during the COVID-19 pandemic and beyond. Dysphagia. Advance online publication. https://doi.org/10.1007/s00455-020-10144-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung, A. , & Ricci, M. F. (2020). Rethinking ‘essential’ and ‘nonessential’: The developmental paediatrician's COVID-19 response. Paediatrics & Child Health, 25(5), 265–267. https://doi.org/10.1093/pch/pxaa077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gough, F. , Budhrani, S. , Cohn, E. , Dappen, A. , Leenknecht, C. , Lewis, B. , Mulligan, D. A. , Randall, D. , Rheuban, K. , Roberts, L. , Shanahan, T. J. , Webster, K. , Krupinski, E. A. , Bashshur, R. , & Bernard, J. (2015). ATA practice guidelines for live, on-demand primary and urgent care. Telemedicine and e-Health, 21(3), 233–241. https://doi.org/10.1089/tmj.2015.0008 [DOI] [PubMed] [Google Scholar]
- Grant, M. J. , & Booth, A. (2009). A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information and Libraries Journal, 26(2), 91–108. https://doi.org/10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- Health Resources & Services Administration. (2019, August). Official website of the U.S. Department of Health Resources & Services Administration: Telehealth programs. https://www.hrsa.gov/rural-health/telehealth
- Kantarcigil, C. , & Malandraki, G. A. (2017). First step in telehealth assessment: A randomized controlled trial to investigate the effectiveness of an electronic case history form for dysphagia. Dysphagia, 32(4), 548–558. https://doi.org/10.1007/s00455-017-9798-y [DOI] [PubMed] [Google Scholar]
- Kantarcigil, C. , Sheppard, J. J. , Gordon, A. M. , Friel, K. M. , & Malandraki, G. A. (2016). A telehealth approach to conducting clinical swallowing evaluations in children with cerebral palsy. Research in Developmental Disabilities, 55, 207–217. https://doi.org/10.1016/j.ridd.2016.04.008 [DOI] [PubMed] [Google Scholar]
- Kim, M. K. , Kantarcigil, C. , Kim, B. , Baruah, R. K. , Maity, S. , Park, Y. , Kim, K. , Lee, S. , Malandraki, J. B. , Avlani, S. , Smith, A. , Sen, S. , Alam, M. A. , Malandraki, G. A. , & Lee, C. H. (2019). Flexible submental sensor patch with remote monitoring controls for management of oropharyngeal swallowing disorders. Science Advances, 5(12), Article eaay3210. https://doi.org/10.1126/sciadv.aay3210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku, P. K. M. , Holsinger, F. C. , Chan, J. Y. K. , Yeung, Z. W. C. , Chan, B. Y. T. , Tong, M. C. F. , & Starmer, H. M. (2020). Management of dysphagia in the patient with head and neck cancer during COVID-19 pandemic: Practical strategy. Head & Neck, 42(7), 1491–1496. https://doi.org/10.1002/hed.26224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz, M. (2020). Making instrumental assessments work in a COVID-19 world. Leader Live.
- Lurie, N. , & Carr, B. G. (2018). The role of telehealth in the medical response to disasters. JAMA Internal Medicine, 178(6), 745–746. https://doi.org/10.1001/jamainternmed.2018.1314 [DOI] [PubMed] [Google Scholar]
- Malandraki, G. A. (2020a, April 24). Telehealth recommendations for dysphagia management during COVID-19. Purdue I-EaT Research Lab. [Google Scholar]
- Malandraki, G. A. (2020b). Telehealth resources for dysphagia management during COVID-19 [Webinar] . American Board of Swallowing and Swallowing Disorders. https://www.facebook.com/watch/?v=627125277871497
- Malandraki, G. A. , & Kantarcigil, C. (2017). Telehealth for dysphagia rehabilitation: The present and the future. Perspectives of the ASHA Special Interest Groups, 2(18), 42–48. https://doi.org/10.1044/persp2.SIG18.42 [Google Scholar]
- Malandraki, G. A. , Markaki, V. , Georgopoulos, V. C. , Bauer, J. L. , Kalogeropoulos, I. , & Nanas, S. (2013). An international pilot study of asynchronous teleconsultation for oropharyngeal dysphagia. Journal of Telemedicine and Telecare, 19(2), 75–79. https://doi.org/10.1177/1357633x12474963 [DOI] [PubMed] [Google Scholar]
- Malandraki, G. A. , McCullough, G. , He, X. , McWeeny, E. , & Perlman, A. L. (2011). Teledynamic evaluation of oropharyngeal swallowing. Journal of Speech, Language, and Hearing Research, 54(6), 1497–1505. https://doi.org/10.1044/1092-4388(2011/10-0284) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malandraki, G. A. , Roth, M. , & Sheppard, J. J. (2014). Telepractice for pediatric dysphagia: A case study. International Journal of Telerehabilitation, 6(1), 3–16. https://doi.org/10.5195/ijt.2014.6135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann, D. M. , Chen, J. , Chunara, R. , Testa, P. A. , & Nov, O. (2020). COVID-19 transforms health care through telemedicine: Evidence from the field. Journal of the American Medical Informatics Association, 27(7), 1132–1135. https://doi.org/10.1093/jamia/ocaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattei, A. , Amy de la Bretèque, B. , Crestani, S. , Crevier-Buchman, L. , Galant, C. , Hans, S. , Julien-Laferrière, A. , Lagier, A. , Lobryeau, C. , Marmouset, F. , Robert, D. , Woisard, V. , & Giovanni, A. (2020). Guidelines of clinical practice for the management of swallowing disorders and recent dysphonia in the context of the COVID-19 pandemic. European Annals of Otorhinolaryngology, Head and Neck Diseases, 137(3), 173–175. https://doi.org/10.1016/j.anorl.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles, A. , Connor, N. P. , Desai, R. V. , Jadcherla, S. , Allen, J. , Brodsky, M. , Garand, K. L. , Malandraki, G. A. , McCulloch, T. M. , Moss, M. , Murray, J. , Pulia, M. , Riquelme, L. F. , & Langmore, S. E. (2020). Dysphagia care across the continuum: A multidisciplinary dysphagia research society taskforce report of service-delivery during the COVID-19 global pandemic. Dysphagia. Advance online publication. https://doi.org/10.1007/s00455-020-10153-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell, C. , & Paluszak, S. L. (2018). Adaptive feeding techniques and positioning: An occupational therapist's perspective. In Ongkasuwan J. & Chiou E. H. (Eds.), Pediatric dysphagia: Challenges and controversies. Springer. https://doi.org/10.1007/978-3-319-97025-7 [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , & PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ, 339, b2535. https://doi.org/10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrell, K. , Hyers, M. , Stuchiner, T. , Lucas, L. , Schwartz, K. , Mako, J. , Spinelli, K. J. , & Yanase, L. (2017). Telehealth stroke dysphagia evaluation is safe and effective. Cerebrovascular Diseases (Basel, Switzerland), 44(3–4), 225–231. https://doi.org/10.1159/000478107 [DOI] [PubMed] [Google Scholar]
- Namasivayam-MacDonald, A. M. , & Riquelme, L. F. (2020). Speech-language pathology management for adults with COVID-19 in the acute hospital setting: Initial recommendations to guide clinical practice. American Journal of Speech-Language Pathology, 29(4), 1850–1865. https://doi.org/10.1044/2020_AJSLP-20-00096 [DOI] [PubMed] [Google Scholar]
- Nicolet, G. (2020). ‘Screenless’ telepractice for toddlers. Leader Live. https://leader.pubs.asha.org/do/10.1044/2020-0812-screenless-telepractice/full/ [Google Scholar]
- Nilsen, M. L. , Clump, D. A. , Kubik, M. , Losego, K. , Mrozek, A. , Pawlowicz, E. , Pickford, D. , Sridharan, S. , Traylor, K. , Wasserman-Wincko, T. , Young, K. , Zandberg, D. , & Johnson, J. T. (2020). Prevision of multidisciplinary head and neck cancer survivorship care during the 2019 novel coronavirus pandemic. Head & Neck, 42(7), 1668–1673. https://doi.org/10.1002/hed.26256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office for Civil Rights. (2020). Notification of enforcement discretion for telehealth.
- Patel, P. D. , Cobb, J. , Wright, D. , Turer, R. W. , Jordan, T. , Humphrey, A. , Kepner, A. L. , Smith, G. , & Rosenbloom, S. T. (2020). Rapid development of telehealth capabilities within pediatric patient portal infrastructure for COVID-19 care: Barriers, solutions, results. Journal of the American Medical Informatics Association, 27(7), 1116–1120. https://doi.org/10.1093/jamia/ocaa065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman, A. L. , & Witthawaskul, W. (2002). Real-time remote telefluoroscopic assessment of patients with dysphagia. Dysphagia, 17(2), 162–167. https://doi.org/10.1007/s00455-001-0116-2 [DOI] [PubMed] [Google Scholar]
- Queensland Health e-Learning Program. (2020). Conducting clinical swallowing examinations via telepractice.
- Raatz, M. K. , Ward, E. C. , & Marshall, J. (2020). Telepractice for the delivery of pediatric feeding services: A survey of practice investigating clinician perceptions and current service models in Australia. Dysphagia, 35(2), 378–388. https://doi.org/10.1007/s00455-019-10042-9 [DOI] [PubMed] [Google Scholar]
- Raatz, M. K. , Ward, E. C. , Marshall, J. , Afoakwah, C. , & Byrnes, J. (2020). “It takes a whole day, even though it's a one-hour appointment!” Factors impacting access to pediatric feeding services. Dysphagia. Advance online publication. https://doi.org/10.1007/s00455-020-10152-9 [DOI] [PubMed] [Google Scholar]
- Raatz, M. K. , Ward, E. C. , Marshall, J. , & Burns, C. L. (2019). Developing the system architecture for conducting synchronous paediatric feeding assessments via telepractice. Journal of Telemedicine and Telecare, 25(9), 552–558. https://doi.org/10.1177/1357633X19872091 [DOI] [PubMed] [Google Scholar]
- Richmond, T. , Peterson, C. , Cason, J. , Billings, M. , Terrell, E. A. , Lee, A. C. W. , Towey, M. , Parmanto, B. , Saptano, A. , Cohn, E. R. , & Brennan, D. (2017). American Telemedicine Association's principles for delivering telerehabilitation services. International Journal of Telerehabilitation, 9(2), 63–68. https://doi.org/10.5195/ijt.2017.6232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoli, J. M. , Lindley, M. C. , DeSilva, M. B. , Kharbanda, E. O. , Daley, M. F. , Galloway, L. , Gee, J. , Glover, M. , Herring, B. , Kang, Y. , Lucas, P. , Noblit, C. , Tropper, J. , Vogt, T. , & Weintraub, E. (2020). Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration—United States, 2020. Morbidity and Mortality Weekly Report, 69(19), 591–593. https://doi.org/10.15585/mmwr.mm6919e2 [DOI] [PubMed] [Google Scholar]
- Sharma, S. , Ward, E. C. , Burns, C. , Theodoros, D. , & Russell, T. (2012). Training the allied health assistant for the telerehabilitation assessment of dysphagia. Journal of Telemedicine and Telecare, 18(5), 287–291. https://doi.org/10.1258/jtt.2012.111202 [DOI] [PubMed] [Google Scholar]
- Soldatova, L. , Williams, C. , Postma, G. N. , Falk, G. W. , & Mirza, N. (2020). Virtual dysphagia evaluation: Practical guidelines for dysphagia management in the context of the COVID-19 pandemic. Otolaryngology—Head & Neck Surgery, 163(3), 455–458. https://doi.org/10.1177/0194599820931791 [DOI] [PubMed] [Google Scholar]
- Starmer, H. M. , Abrams, R. , Webster, K. , Kizner, J. , Beadle, B. , Holsinger, F. C. , Quon, H. , & Richmon, J. (2018). Feasibility of a mobile application to enhance swallowing therapy for patients undergoing radiation-based treatment for head and neck cancer. Dysphagia, 33(2), 227–233. https://doi.org/10.1007/s00455-017-9850-y [DOI] [PubMed] [Google Scholar]
- Telehealth Resource Centers. (2018). A framework for defining telehealth.
- Thomas, P. , Baldwin, C. , Bissett, B. , Boden, I. , Gosselink, R. , Granger, C. L. , Hodgson, C. , Jones, A. Y. , Kho, M. E. , Moses, R. , Ntoumenopoulos, G. , Parry, S. M. , Patman, S. , & van der Lee, L. (2020). Physiotherapy management for COVID-19 in the acute hospital setting: Clinical practice recommendations. Journal of Physiotherapy, 66(2), 73–82. https://doi.org/10.1016/j.jphys.2020.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turvey, C. , Coleman, M. , Dennison, O. , Drude, K. , Goldenson, M. , Hirsch, P. , Jueneman, R. , Kramer, G. M. , Luxton, D. D. , Maheu, M. M. , Malik, T. S. , Mishkind, M. C. , Rabinowitz, T. , Roberts, L. J. , Sheeran, T. , Shore, J. H. , Shore, P. , van Heeswyk, F. , Wregglesworth, B. , … Bernard, J. (2013). ATA practice guidelines for video-based online mental health services. Telemedicine and e-Health, 19(9), 722–730. https://doi.org/10.1089/tmj.2013.9989 [DOI] [PubMed] [Google Scholar]
- University of Maine. (2020). Training program [online] . Speech Therapy Telepractice Program. https://umaine.edu/telespeech/training-program/
- Wales, D. , Skinner, L. , & Hayman, M. (2017). The efficacy of telehealth-delivered speech and language intervention for primary school-age children: A systematic review. International Journal of Telerehabilitation, 9(1), 55–70. https://doi.org/10.5195/IJT.2017.6219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall, L. R. , Cartmill, B. , Ward, E. C. , Hill, A. J. , Isenring, E. , Byrnes, J. , Chambers, S. , Dunn, J. , Nixon, J. , Whelan, J. , & Porceddu, S. V. (2016). “ScreenIT”: Computerized screening of swallowing, nutrition and distress in head and neck cancer patients during (chemo)radiotherapy. Oral Oncology, 54, 47–53. https://doi.org/10.1016/j.oraloncology.2016.01.004 [DOI] [PubMed] [Google Scholar]
- Ward, E. C. , Burns, C. L. , Theodoros, D. G. , & Russell, T. G. (2013). Evaluation of a clinical service model for dysphagia assessment via telerehabilitation. International Journal of Telemedicine and Applications, 2013, Article 918526. https://doi.org/10.1155/2013/918526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, E. C. , Burns, C. L. , Theodoros, D. G. , & Russell, T. G. (2014). Impact of dysphagia severity on clinical decision making via telerehabilitation. Telemedicine and e-Health, 20(4), 296–303. https://doi.org/10.1089/tmj.2013.0198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, E. C. , Crombie, J. , Trickey, M. , Hill, A. , Theodoros, D. , & Russell, T. (2009). Assessment of communication and swallowing post-laryngectomy: A telerehabilitation trial. Journal of Telemedicine and Telecare, 15(5), 232–237. https://doi.org/10.1258/jtt.2009.081204 [DOI] [PubMed] [Google Scholar]
- Ward, E. C. , Sharma, S. , Burns, C. , Theodoros, D. , & Russell, T. (2012a). Managing patient factors in the assessment of swallowing via telerehabilitation. International Journal of Telemedicine and Applications, 2012, Article 132719. https://doi.org/10.1155/2012/132719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, E. C. , Sharma, S. , Burns, C. , Theodoros, D. , & Russell, T. (2012b). Validity of conducting clinical dysphagia assessments for patients with normal to mild cognitive impairment via telerehabilitation. Dysphagia, 27(4), 460–472. https://doi.org/10.1007/s00455-011-9390-9 [DOI] [PubMed] [Google Scholar]
- Yang, H. W. , Burke, M. , Isaacs, S. , Rios, K. , Schraml-Block, K. , Aleman-Tovar, J. , Tompkins, J. , & Swartz, R. (2020). Family perspectives toward using telehealth in early intervention. Journal of Developmental and Physical Disabilities. Advance online publication. https://doi.org/10.1007/s10882-020-09744-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaga, C. J. , Pandian, V. , Brodsky, M. B. , Wallace, S. , Cameron, T. S. , Chao, C. , Orloff, L. A. , Atkins, N. E. , McGrath, B. A. , Lazarus, C. L. , Vogel, A. P. , & Brenner, M. J. (2020). Speech-language pathology guidance for tracheostomy during the COVID-19 pandemic: An international multidisciplinary perspective. American Journal of Speech-Language Pathology, 29(3), 1320–1334. https://doi.org/10.1044/2020_AJSLP-20-00089 [DOI] [PubMed] [Google Scholar]