Abstract
Purpose
Evaluation and management of voice and upper airway disorders in adults and children, by speech-language pathologists worldwide, have been significantly altered by the COVID-19 pandemic. Secondary to the pathogenic nature of the virus in the respiratory tract and upper airway, it is essential that speech-language pathologists who specialize in these disorders are knowledgeable of current practices to provide evidence-based care while minimizing viral transmission. Understanding how and when SARS-CoV-2 spreads is critical to the development of effective infection prevention within clinical practices.
Method
We established an evidence-based clinical practice guide for clinicians working with voice and upper airway through a comprehensive evaluation of peer-reviewed journals, non–peer-reviewed manuscripts on preprint servers, national health guidelines, and published and online consensus statements and emerging data. Emphasis was placed on risk mitigation for viral transmission via safe clinical practices, including evaluative procedures, therapy including telehealth, personal protective equipment, room, staffing, and distancing considerations.
Results/Conclusions
While knowledge relevant to viral transmission of SARS-CoV-2 is rapidly evolving, there is a paucity of literature specific to the evaluation and treatment of voice and upper airway disorders. Within these confines and given the potentially significant high risk of infection secondary to the nature of COVID-19, we summarize current considerations and recommend best practices that maximize risk mitigation whereby ensuring patient and provider safety.
SARS-CoV-2 is a highly pathogenic human coronavirus that was first identified in late 2019. This single-strand positive-sense RNA virus is highly pathogenic and causes the disease known as COVID-19 (Fung & Liu, 2019). COVID-19 can cause mild-to-severe respiratory disease and can be characterized by fever, cough, headaches, pneumonia, and loss of taste and smell (Guan & Zhong, 2020; Holshue et al., 2020). Moreover, the precipitous spread of SARS-CoV-2 has been complicated by persons who are asymptomatic, also known as silent spreaders (Byambasuren et al., 2020); the rate of truly asymptomatic infection is unknown. This virus has rapidly spread worldwide in less than 12 months, with over 60 million infected and 1.5 million deaths (Johns Hopkins Coronavirus Resource Center, 2020). The zoonotic transmission, precipitous emergence, and spread of SARS-CoV-2 have dramatically affected medical and health care practices. Speech-language pathologists (SLPs) who specialize in the treatment of voice and upper airway disorders have had to quickly pivot in providing care to their patients secondary to the pathogenic nature of the virus in the respiratory tract and upper airway—areas of the body that these SLPs are exposed to daily. In this clinical focus article, it is our intention to present considerations that are specific to SLPs who work with patients who have disorders of the voice and upper airway. Now, because of its recent rapid emergence, research specific to SARS-CoV-2 and its complementary disease, COVID-19, is limited. Specific evidence-based research in the area of voice and upper airway is present to even a lesser extent.
COVID-19 typically presents as illness of the lungs and upper respiratory tract (Guan & Zhong, 2020). High viral loads and successful isolation from nasal and throat swabs suggest viral replication in tissues of the upper respiratory tract (Wölfel et al., 2020). Active independent pharyngeal virus replication (rather than passive shedding from the lung) has been measured to be very high (1,000 times higher than SARS) during the first week of symptoms (first 5 days; Wölfel et al., 2020). Furthermore, shedding of viral RNA from the sputum has been shown to outlast the end of symptoms (Wölfel et al., 2020). Viral transmission of SARS-CoV-2 is thought to be possible through contact and droplet transmission and/or airborne transmission. Direct contact is defined as exposure to infected secretions (5–10 μm) or particles (< 5 μm) that may spread during talking, coughing, singing, or sneezing or aerosol-generating procedures (AGPs; < 1 μm; World Health Organization [WHO], 2014). Airborne transmission of SARS-CoV-2 occurs through dissemination of aerosols that remain infectious when suspended in air over long distances and time (WHO, 2014). It should be noted that there is high variability in droplet and/or aerosol generation between persons and in those who have SARS-CoV-2 versus healthy individuals (WHO, 2020). Airborne transmission of SARS-CoV-2 can occur during AGPs, and most recently, it has been determined that the virus can be found airborne, particularly in indoor settings that have poor ventilation (Somsen et al., 2020). Lastly, indirect contact transmission involving contact with contaminated objects or surfaces has been reported (Matson et al., 2020). Fomites form on contaminated surfaces and have been reported to last hours to days, depending on the ambient environment (including temperature and humidity) and the type of surface (median half-life of 5.6 hr on stainless steel and 6 hr on plastic; Guo et al., 2020; Ma et al., 2020). Indirect transmission is possible by exposure to surfaces or objects contaminated with the virus, followed by touching one's face, mouth, nose, and so forth. Despite evidence as to SARS-CoV-2 contamination of surfaces and the survival of the virus, there are no reports that have confirmed direct fomite transmission (WHO, 2020).
Current evidence and experience suggest that SARS-CoV-2 is predominantly spread person-to-person (WHO, 2020). It has been hypothesized that normal breathing and talking produces small exhaled aerosols and if inhaled by another person, they could get COVID-19 if there is sufficient virus in the aerosols to cause infection. Unfortunately, this hypothesis is complicated by the fact that the proportion of exhaled droplet nuclei or of respiratory droplets that evaporate to generate aerosols and the infectious dose of viable SARS-CoV-2 required to cause infection in another person are not known. The most recent research has quantified the amount of droplets of various sizes that remain airborne during normal speech (Anfinrud et al., 2020) and the aerosols that healthy individuals can produce through coughing and talking (Somsen et al., 2020). There is high variability between individuals in terms of particle emission rates during speech, with increased rates correlated with increased amplitude of vocalization (Asadi et al., 2019). It is also known that certain persons, known as super emitters, release more aerosol particles during speech than do their peers (Asadi et al., 2019). Whether or not SARS-CoV-2 can be found in air after breathing, talking, or coughing has had limited investigation. Multiple studies have reported SARS-CoV-2 RNA in air samples taken from rooms where symptomatic COVID-19 patients were cared for but where AGPs were not performed (Chia et al., 2020; Ma et al., 2020; Liu et al., 2020), whereas similar studies in health care found no SARS-CoV-2 RNA in room air (Cheng et al., 2020; Faridi et al., 2020). When SARS-CoV-2 RNA was found, the quantity of RNA was low with no viable virus identified (Santarpia et al., 2020). It should be further noted that detection of RNA is not indicative of the presence of a viable virus that could spread and cause infection. Further research is warranted to elucidate the potential for talking to be a route of viral transmission of SARS-CoV-2 and if this potential changes in indoor/outdoor settings, with and without good ventilation.
Support of viral transmission of SARS-CoV-2 from coughing and sneezing comes from controlled laboratory experiments using high-powered jet nebulizers that generated aerosols of infectious samples, not human studies. Virus was present in aerosol for 3 hr (van Doremalen et al., 2020) to 16 hr (Matson et al., 2020). Lastly, while there have been reports of COVID-19 spread between members of choirs (Hamner et al., 2020), there is a paucity of data regarding viral transmission of this disease specifically during singing, as other activities such as sitting close to one another, sharing snacks, and stacking chairs at the end of the practice occur. The act of singing, itself, might have contributed to transmission through emission of aerosols, which is affected by loudness of vocalization; however, opportunities for droplet and fomite transmission were also present (Hamner et al., 2020).
Timing of spread of SARS-CoV-2 is an important factor in determining clinical practice guidelines. The incubation period (time between exposure of virus and symptom onset) of COVID-19 is, on average, 5–6 days but has been reported as long as 14 days (WHO, 2020). Data suggest that SARS-CoV-2 can be detected 1–3 days before symptom onset, with highest viral loads, measured close to symptom onset, followed by a measured decline over time (Pan et al., 2020). Positive RNA presence has been reported to be 1–2 weeks for asymptomatic persons and up to 3 weeks or more for patients with mild-to-moderate disease (Pan et al., 2020; Wölfel et al., 2020; Xu et al., 2020), and for those with severe COVID-19, it was considerably prolonged (Pan et al., 2020). To provide interpretation, detection of viral RNA is not necessarily suggestive of a person being infectious or able to transmit the virus to another person (WHO, 2020).
AGPs
AGPs are defined as medical procedures with the potential to generate infectious respiratory particles at higher concentrations than breathing, coughing, sneezing, or talking or procedures that create uncontrolled respiratory secretions (Lammers et al., 2020). This increase is secondary to active viral shedding in the lungs and upper airway. The diagnosis and treatment of voice and upper airways disorders by SLPs frequently require procedures that can cause AGP (see Table 1) including endoscopy (rigid and flexible, oral and nasal). Please refer to Zaga et al. (2020) for guidelines and recommendations for AGP management for SLPs who manage tracheostomy care and work in intensive care units (Zaga et al., 2020). To date, it is unknown if other assessments, that is, acoustic, aerodynamic, and nasal function studies, commonly completed in voice and upper airway evaluations, create higher concentrations of infectious particles. If it is necessary to complete AGPs, the level of personal protective equipment (PPE) recommended is dependent upon COVID-19 status (see Table 2).
Table 1.
Infection control recommendations for voice and upper airway common equipment.
| Variable | Rigid endoscopy/stroboscopy | Flexible endoscopy/stroboscopy | Aerodynamics | Acoustics | Nasal function studies | Voice therapy |
|---|---|---|---|---|---|---|
| CPT code | 31579 | 31575, 31579 | 92520 | 92520 | 92512 | 92507 |
| AGP | Yes | Yes | Unknown | Unknown | Unknown | Unknown |
| Infection control | Standard reprocessing of endoscopes | Standard reprocessing of endoscopes | Airflow head, coupler, pneumotachograph and microphone: disinfect per manufacturer instructions Intra-oral pressure tubes, pressure port tubes, flow head tubes, and pressure screening tubes: dispose after each patient Mask, Luer cap, and O-rings: replace with each patient if disposable; disinfect per manufacturer instructions if reusable |
Microphone: cannot be submerged—disinfect per manufacturer instructions Consider microphone cover a |
Microphone: wipe with disinfection solution Baffle: wipe with disinfection solution |
Use disposable materials |
Note. Please check with your facility's infection control department for their recommendations for all equipment and those not listed above.
Effect of microphone cover on acoustic results is unknown at this time.
Table 2.
Recommendations for personal protective equipment (PPE), distancing, and room considerations based upon COVID-19 status.
| COVID-19 status | PPE for providers | Room density | Room type and turnover time | Other considerations |
|---|---|---|---|---|
| Aerosol-generating procedures | ||||
| COVID-19 positive within last 10 days | N95 or PAPR, gloves, gown, eye protection, or face shield | Institution specific Minimum occupancy |
Negative pressure room Institution-specific turnover time |
Postpone if nonessential |
| COVID-19 positive 11–30 days from procedure and asymptomatic | N-95 or PAPR, gloves, gown, eye protection, or face shield | Institution specific Minimum occupancy |
Negative pressure room Institution specific turnover time |
Postpone if nonessential Screen for COVID-19 symptoms |
| COVID-19 positive ≥ 30 days from procedure and asymptomatic | Barrier mask, gloves, eye protection, or face shield | 6-ft distancing | Standard cleaning and turnover time | Screen for COVID-19 symptoms |
| Patient under investigation | N95 or PAPR, gloves, gown, eye protection, or face shield | Institution specific Minimum occupancy |
Negative pressure room Institution-specific turnover time |
Postpone if nonessential Screen for COVID-19 symptoms |
| COVID-19 negative (within 3 days of procedure and no positive history of COVID-19 within past 30 days) | Barrier mask, gloves, eye protection, or face shield | 6-ft distancing | Standard room and turnover times | Screen for COVID-19 symptoms that may have begun since testing |
| Non–aerosol-generating procedures | ||||
| COVID-19 positive within last 10 days and symptomatic | N95 or PAPR, face shield, gown, gloves | Institution specific Minimum occupancy |
Negative pressure room Institution-specific turnover times |
Consider postponing if nonessential |
| COVID-19 positive within last 10 days and asymptomatic | Barrier mask, gloves, eye protection, or face shield | Institution specific Minimum occupancy |
HEPA filter Institution-specific turnover time |
Consider postponing if nonessential Screen for COVID-19 symptoms |
| COVID-19 positive 11–30 days from visit and asymptomatic | Barrier mask, gloves, eye protection, or face shield | Institution specific Minimum occupancy |
HEPA filter Institution-specific turnover time |
Consider postponing if nonessential Screen for COVID-19 symptoms |
| COVID-19 positive ≥ 30 days from visit and asymptomatic | Barrier mask, gloves, eye protection, or face shield | 6-ft distancing | Standard room and turnover time | Screen for COVID-19 symptoms |
| Patient under investigation | N95 or PAPR, face shield, gown, gloves | Institution specific Minimum occupancy |
Negative pressure room Institution-specific turnover times |
Consider postponing if nonessential Screen for COVID-19 symptoms |
| Asymptomatic Unknown status |
Barrier mask, gloves, eye protection, or face shield | 6-ft distancing | Standard room and turnover time | Screen for COVID-19 symptoms |
| COVID-19 negative (within 3 days of visit and no positive history of COVID-19 within past 30 days) | Barrier mask, gloves, eye protection, or face shield | 6-ft distancing | Standard room and cleaning | Screen for COVID-19 symptoms that may have begun since testing |
Note. Table information was tailored from the following sources: ASHA (2020a), CDC (2020b, 2020c), Givi et al. (2020), Kramer et al. (2015), Lammers et al. (2020), and OSHA (2020a).
Relevant precautionary statements and PPE recommendations have been published by various national associations, which include, but are not limited to, the American Speech-Language-Hearing Association (ASHA, 2020a), Speech Pathology Australia (2020), the Royal College of Speech-Language Therapy (2020), the Speech-Language & Audiology Canada (2020), The Irish Association of Speech & Language Therapists (2020), and the New Zealand Speech-Language Therapists' Association (2020).
Room Considerations
Voice care typically occurs in relatively small rooms. Room size, ventilation, and turnaround times for cleaning and ventilation are significant considerations (see Table 2). Please refer to the Centers for Disease Control and Prevention (CDC) recommendations for Employers Information for Office Buildings (CDC, 2020b) for a comprehensive review of these topics. The CDC recommends maintaining 6-ft distance between individuals whenever possible; this is supported by research on SARS-CoV-2 and other viruses. Chu and colleagues completed a systematic review of 172 observational studies, which included studies of SARS, MERS, and COVID-19 and found that physical distancing of 1 m or more and the use of barrier masks or respirators were associated with much lower risk of infection (Chu et al., 2020). They further concluded that a distance of 2 m would mitigate risk to a greater degree. Unfortunately, there is not a universal recommendation for physical distancing at this time and appears to be institution specific.
Because of the potential for aerosolization of COVID-19 and its transmission through particles suspended in the air, the Occupational Safety and Health Administration (OSHA) recommends use of airborne infection isolation rooms for COVID-19–positive patients and recommends that AGPs be performed on patients with suspected COVID-19 only in these rooms. Requirements for an airborne infection isolation room are that they are single-patient rooms with negative pressure with a minimum of six air exchanges per hour (OSHA, 2020a). While specific recommendations for patients with unknown COVID-19 status have not been provided, many institutions are considering those without a recent negative test to be a person under investigation due to high rate of asymptomatic spread in many communities. Regardless of COVID-19 status, it has been recommended that buildings increase ventilation rate, use natural ventilation, and avoid air recirculation (Morawska & Cao, 2020). This also includes delayed use of an exam room between patients to allow total room air turnover, such that potentially infectious particles are removed through ventilation. Outdoor activities allow for greater physical distancing and dispersal of droplets and aerosolized particles than indoor activities. While it is atypical practice pattern, SLP therapy could be conducted out of doors, if privacy considerations can be maintained. For example, respiratory retraining for exercise paradoxical vocal fold motion could easily be performed outdoors, with the patient running on a soccer field or sidewalk. In this sort of a situation, the clinician could easily maintain 6 ft of distance, and the athlete could exercise without a mask. Depending on the facility, singing or loud voice use could also be done outdoors to mitigate the risk of aerosols in a small room.
Telemedicine Considerations
Currently, the Centers for Medicare & Medicaid Services strongly advises maximum use of all telehealth modalities. During the COVID-19 pandemic, health care systems around the world have been challenged to be innovative to maintain effective treatment in outpatient care. An expedited review of telemedical practices revealed that utilization of telemedicine may reduce the number of emergency room visits, preserve health care resources, and reduce the spread of COVID-19 by decreasing in-person visits during and following the pandemic (Bokolo, 2020). Mayo Clinic reviewed 150 speech pathology telemedicine evaluations between 1987 and 1994, stating that 82 of those patients were diagnosed with a voice disorder, including spasmodic dysphonia, voice tremor, psychogenic dysphonia, and musculoskeletal tension dysphonia, with 50 of those being recommended for otolaryngologic intervention for spasmodic dysphonia (Duffy et al., 1997). They concluded that telemedicine evaluations were found to be an appropriate alternative to in-person speech-language pathology evaluations when distance prevents in-person evaluations and when specialists are unavailable to diagnosis and manage difficult speech and language disorders or, in our current case, a pandemic. During the current 2020 COVID-19 pandemic, 87% of patients who received telemedicine ENT consultation reported beingly highly satisfied with the telemedicine appointment; however, no significant factors associated with satisfaction were found (Fieux et al., 2020). Telemedicine assessment for those with Parkinson's disease (PD) and hypokinetic dysarthria were shown to have comparable levels of agreement between in-person and telemedicine assessments, suggesting telemedicine assessment is both reliable and valid for hypokinetic dysarthria in those with PD (Constantinescu et al., 2010). Telemedicine provides voice evaluation access and voice therapy in the safety of a patient's own home (Duffy et al., 1997). If telemedicine is appropriate for the patient, including availability of resources such as access to technology and appropriate support secondary to age and cognitive/behavioral/mental status, telemedicine can be utilized for both evaluations and therapy (Duffy et al., 1997). Telemedicine platforms need to be encrypted and in compliance with HIPAA standards. To implement telemedicine, payment and coverage issues, state laws and regulations, and licensure policies, including professional liability insurance, billing, coding, and appropriate reporting of documentation, need to be considered. If able and appropriate, telemedicine should be used in lieu of in-person appointments to continue to limit nonessential in-person care for patients and to maintain social distancing recommendations during the COVID-19 pandemic (Bokolo, 2020; Castilles-Allendes et al., 2020).
Triage Considerations
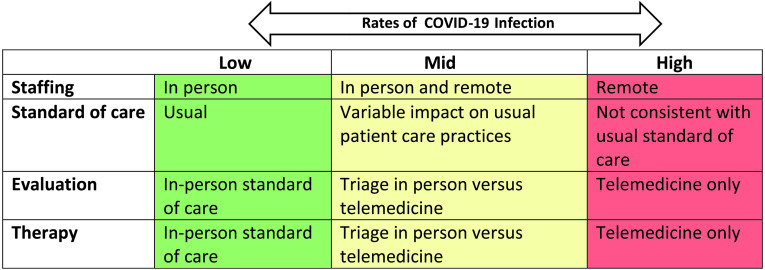
When rates of COVID-19 are increased, health care facilities drastically reduce the number of ambulatory and inpatients, resulting in the majority of patients' care being postponed or provided remotely via telehealth with variable deviations in care provided (see Figure 1). To follow physical distancing restrictions, federal guidelines permitted the temporary utilization of telemedicine appointments, allowing health care facilities to care for both essential and nonessential patients from afar (Murphy, 2020). ASHA has provided excellent documentation of State Law and Regulations for Telepractice and Licensure During COVID-19 https://www.asha.org/uploadedFiles/State-Telepractice-Policy-COVID-Tracking.pdf(ASHA, 2020c). Furthermore, eligibility of State Medicaid Telemedicine Policies and Emergency Telepractice Orders should be consulted to determine care coverage for each state.
Figure 1.
Continuum considerations in practice patterns.
To determine essential versus nonessential patients, an interdisciplinary triaging team has been suggested, consisting of a laryngologist and an SLP to review patients' medical records for those needing care in voice and upper airway (Mattei et al., 2020). Review of patients' medical records should include assessment of the number and severity of risk factors in order to determine the appropriate modality of care. Risk factors include, but are not limited to, age, gender, tobacco or alcohol use, unintentional weight loss, race, head and neck trauma, comorbidities, and initial onset and type of symptoms (Tikka et al., 2020). Further considerations should be given for those patients who may be at an increased risk for complications associated with COVID-19 and may want to avoid an in-person appointment to reduce their risk of contracting the coronavirus. In a recent study that reviewed 17,278,393 electronic medical records, 10,926 COVID-19–related deaths were recorded. Deaths were greater among those patients who were older, male, and with various medical conditions, including diabetes and severe asthma, and people who were of Black or South Asian ethnicity (Williamson et al., 2020).
Considerations for Voice and Upper Airway Care in Children
Clinical and research evidence to date indicate that children appear to be less severely impacted by SARS-CoV-2 than adults (Lanari et al., 2020; Ludvigsson, 2020; Wang et al., 2020). While there are many hypotheses behind why this might be, there has been no conclusive evidence to explain this phenomenon (Lanari et al., 2020). In the Weekly Morbidity and Mortality Report February 14–April 2, only 1.7% of diagnosed cases of COVID-19 were in individuals 0–18 years of age, and a third of those were 15- to 18-year-olds (CDC, 2020a). However, since that time, rates of infection has increased in children. According to a report issued by the American Academy of Pediatrics and the Children's Hospital Association, summarizing state-reported data from 49 states, Puerto Rico, Guam, and Washington, DC, as of September 3, 2020, there had been 513,415 cases in children, making up 9.8% of all U.S. cases (American Academy of Pediatrics and Children's Hospital Association, 2020). Schools have been closed throughout most of the United States since March, greatly reducing the number of people children interact with on a daily basis, which may have reduced the spread to children. As schools in some communities open, impacts on infection rates among children will be closely scrutinized.
Several systematic reviews have found that, of those children who do contract the virus, their symptoms are usually milder. A systematic review completed by Wang et al. (2020) found that, of 1,667 pediatric patients, 94% had mild cases, and only 3% had severe cases. In a second review of 1,065 pediatric participants, only one died and one developed pneumonia (Castagnoli et al., 2020). Children who are symptomatic seem to have a different distribution of symptoms from adults. For example, children may present with vomiting or diarrhea rather than respiratory symptoms (Tian et al., 2020). Multisystem inflammatory syndrome has also been linked to COVID-19 in children (Riollano-Cruz et al., 2020). With these differences in symptoms and severity, it is possible that standard screening questions may not adequately capture children with COVID-19.
Further complicating is the unknown risk that children may have in children transmitting the virus to adults, especially older adults, who are at higher risk of more severe illness. One study looked at spread from children to adults via contact tracing in South Korea and found that younger children (ages 0–9 years) spread SARS-CoV-2 to household and nonhousehold contacts at a lower rate than older children (ages 10–19 years), but spread did occur (Park et al., 2020). There have not been conclusive studies to determine whether lower symptom severity is associated with lower transmission risk, and in fact, if children are minimally symptomatic or asymptomatic, they may be more likely to attend school, activities, or voice therapy appointments when sick. As these factors are still unclear, it is advisable to consider that children may be infectious even if asymptomatic and take precautions accordingly.
Voice and Upper Airway Evaluations
In Person
If a voice evaluation is deemed essential or time sensitive, an in-person comprehensive voice evaluation consisting of a thorough case history, laryngeal imaging, acoustic measures, aerodynamic measures, auditory–perceptual evaluation, and patient self-report measures is recommended, depending upon COVID-19 status (Patel et al., 2018). Maximizing safety requires considerations of flexible PPE use and availablity, room density, and room turn over times (see Table 2). It has been recommended that COVID-19 testing be completed prior to performing any AGP, such as endoscopy (Rameau et al., 2020). If a COVID-19 test is available, it has been suggested that COVID-19 testing be completed within 24–72 hr of visit (Castilles-Allendes et al., 2020; Reddy et al., 2020), followed by self-quarantine until their appointment.
If a patient's COVID-19 test is negative and they continue to screen negative for COVID-19 symptoms at the time of their appointment, AGPs such as endoscopy, with or without stroboscopy, may be completed. The use of nasal anesthetic spray is considered an AGP (Rameau et al., 2020; Tan et al., 2020); therefore, consideration to replace nasal anesthetic spray with viscous anesthetic gel is advised (Rameau et al., 2020) . Always confirm your facility, local, state, and professional guidelines/recommendations when considering the minimum PPE for AGPs and ensure appropriate donning and doffing for all PPE. If local, state, and/or national recommendations for 6-ft distancing and barrier masks are still advised, even with a negative-tested patient, providers should continue to practice physical distancing by maintaining at least a 6-ft distance whenever possible. Even if the patient has tested negative for COVID-19, it is possible for an SLP to be an asymptomatic carrier themselves.
In locations where COVID-19 testing is not attainable when an AGP is performed and the patient has screened negative for COVID-19 symptoms, the patient may still be an asymptomatic carrier and therefore should be treated as having an unknown status. ASHA's guidance in this case is to use CDC-recommended PPE for all AGPs, which would include maintaining 6-ft distance whenever possible, full protective PPE such as an N95 or a powered air purifying respirator (PAPR), protective eye wear, gown, and gloves (Givi et al., 2020; Lammers et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Rameau et al., 2020; Reddy et al., 2020), as well as consideration for performing the AGP in a negative pressure room (Givi et al., 2020; Lammers et al., 2020; Namasivayam-MacDonald & Riquelme, 2020; Rameau et al., 2020; Reddy et al., 2020) if available and/or leave the room unoccupied for a time. To reduce potential exposure and to conserve PPE, AGPs should be performed by the most experienced provider without any observers (Givi et al., 2020; Rameau et al., 2020). Furthermore, if possible, patients should maintain their face mask over their mouth during flexible endoscopy, in case the patient sneezes and/or coughs (Tan et al., 2020). Consider having the patient remove their face mask during vocal function testing in order to maintain validity with normative data. There is a paucity of data in the literature that inform changes that the presence of a face mask or microphone cover may have on acoustic and aerodynamic measures. A consensus of a panel of 11 experts in voice and swallowing disorders from five different countries suggest avoiding the use of headsets (Castilles-Allendes et al., 2020). Lastly, use of an AKG headset mic may be possible if using approved COVID-19 equipment precautions such as wiping down the headset plastic portion of the mic, headset, and cord and using disposable foam balls, as per local infection control requirements.
If a patient tests positive for COVID-19 or screens positive for COVID-19 symptoms, the urgency of the evaluation should be considered. If essential, patient should be evaluated, full protective PPE should be donned (Givi et al., 2020; Rameau et al., 2020; Reddy et al., 2020), and if available, a negative pressure room should be used (Namasivayam-MacDonald & Riquelme, 2020; Lammers et al., 2020; Rameau et al., 2020; Reddy et al., 2020). Additionally, as determined by the institution, if an AGP was performed, the room used should remain unoccupied for a time to allow for full room ventilation between patients. To further reduce potential exposure and to conserve PPE, the AGP should be performed by the most experienced provider without any observers (Castilles-Allendes et al., 2020; Rameau et al., 2020). A patient that has tested positive for COVID-19 within 30 days of an AGP should follow the above described full protective PPE recommendations. If the evaluation can be postponed for a COVID-19–positive patient or for someone that has screened positive for COVID-19 symptoms, the patient should return for their evauation following appropriate quarantine and/or the patient has a negative COVID-19 test (Rameau et al., 2020) and continues to remain asymptomatic. When considering appropriate PPE for a patient who has a past history of a positive COVID-19 test at least more than 30 days ago, has a recent negative COVID-19 test, and remains asymptomatic of COVID-19 symptoms, the patient can be treated as a negative COVID-19 test for their AGP.
Telemedicine Voice Evaluations
If a patient is low risk, elective, and/or not time sensitive, an in-person comprehensive evaluation may be postponed; the patient may be a candidate for a telemedicine evaluation. Evaluating a patient with telemedicine can mitigate the negative impact that a voice and/or an upper airway disorder can have on an individual in lieu of postponing an evaluation and/or treatment.
During a telemedicine evaluation, the SLP should perform behavioral and qualitative analysis of voice and resonance (CPT Code 92524), with considerations for low-tech maximum phonation time and voice range profile (Castilles-Allendes et al., 2020; Zughni et al., 2020). Voice samples could be obtained via various recordings and audio clips, that is, phone and voicemail, and placed in the electronic medical record for perceptual postevaluation and/or therapy comparisons (Castilles-Allendes et al., 2020). It is impossible to complete laryngeal imaging via telemedicine. Recently, ASHA's Special Interest Group Coordinating Committee of Voice and Upper Airway Disorders provided a statement of consideration for telemedicine voice evaluation in the absence of a laryngeal evaluation endorsing that making recommendations for voice therapy should be determined from history, acoustic measures if available, and therapeutic stimulability tasks (ASHA, 2020b). Should therapy be recommended, the risks and benefits associated with receiving treatment without laryngeal evaluation must be conveyed to the patient, and the patient should be advised to return for a full evaluation, including laryngeal evaluation, when appropriate (Castilles-Allendes et al., 2020) . If there is concern for underlying high-risk pathology following history, voice evaluation, and extensive therapy stimulability (Gillespie & Gartner-Schmidt, 2016) by the interdisciplinary team of otolaryngologists/laryngologists and SLPs, a patient should be strongly considered for an in-person evaluation consisting of laryngeal visualization. Should a patient not improve during telemedicine voice therapy at the rate that is expected and/or other red flags are raised during therapy, the patient should be advised to have an in-person evaluation with laryngeal evaluation to assess vocal structure and function to determine the etiology for halted vocal improvement.
Pediatric Considerations
Children are accompanied by parents, and even if children have undergone COVID-19 testing prior to evaluation, their parents have not. Symptoms screening of parents is necessary, and parents should be required to wear a barrier mask throughout the evaluation. In our experience, young children often require more assistance, practice, and training to perform tasks during a voice evaluation. This may lead the clinician to be in closer proximity to the child for a longer time than they might to an adult. Most older children participate well with rigid or flexible stroboscopy, but younger children can have more difficulty with the procedure. Success often requires comfort positioning, including sitting in a parent's lap and having another adult steady the child's head. This puts three adults well within 6 ft of each other. Young children may also yell, cry, or cough during the procedure, increasing the volume of droplets and possible aerosolization. All of these factors should be considered in the use of PPE, and all staff involved should wear appropriate PPE for the procedure, COVID-19 status of the patient, and the room. Lastly, if a child has had a recent experience of having a nasal swab for COVID-19 testing, this may negatively influence their willingness to participate in endoscopy. It may be even more beneficial than usual to enroll Child Life experts if available, in order to increase participation and have a more positive experience.
Voice and Upper Airway Therapy
In Person
When considering in-person voice therapy appointments, it is necessary to evaluate COVID-19 status (see Table 2). There is paucity of research into the potential airborne transmission of SARS-CoV-2 during voice therapy, and as such, guidelines below are based upon best evidence and experience with other viral illnesses. In-person voice therapy should be postponed for those who are COVID-19 positive within the past 30 days, are symptomatic, or are persons under investigation. Patients who have tested negative for COVID-19 (within 3 days of visit) or who are asymptomatic may be appropriate for voice therapy with appropriate PPE. If local, state, and/or national recommendations for a 6-ft distancing and barrier masks are still advised, these practices should be maintained for in-person voice therapy and for any non-AGP (Lammers et al., 2020), which may or may not include voice therapy. PPE considerations may include a medical-grade mask, an N95, or a PAPR for the SLP, gown, and protector eyewear (Lammers et al., 2020), as well as a barrier mask for the patient. If clear masks are accessible, they may be a consideration to aid in visualization of the articulators but have the disadvantage of fogging. The effectiveness of a clear mask as barrier protection has not been closely studied and likely varies by type and brand. There is also a concern that a plastic mask alters the sound quality and may make it more difficult to hear speech and changes in voice quality. Vocal tasks such as increased loudness, such as with Lee Silverman Voice Treatment, have been shown to produce increased droplets (Asadi et al., 2019) and velocities, as well as with whispered voices (Giovanni et al., 2020). However, loud phonation and semi-occluded vocal tract exercises, such as straw phonation and flow phonation of sustained /v/ and /ʒ/, did not demonstrate a higher risk of droplet spread as compared to standard speech (Giovanni et al., 2020). Sustained voiceless consonants such as /s/ and /ʃ/ or blowing through a straw produces faster air velocity as compared to loud phonation, but the initial high-velocity flow quickly decreases during sustained tasks (Giovanni et al., 2020). Further considerations should be given for the length of time of the therapy session and the room size. Air circulation may play a pivotal role when considering having the room unoccupied for any given amount of time following a therapy session to maintain safety for both the SLP and the patient.
Telemedicine Therapy
Literature reviews assessing available research utilizing telemedicine and voice therapy suggest that in-person therapy and therapy received via telemedicine have comparable outcomes (Kelchner, 2013; Mashima et al., 2003; Mashima & Brown, 2011; Rangarathnam et al., 2016). Telemedicine voice therapy revealed comparable outcomes as compared to in-person therapy for those with vocal fold nodules, vocal fold edema, unilateral vocal fold paralysis, and vocal hyperfunction (Mashima et al., 2003). Those with muscle tension dysphonia were found to have significant improvements post–telemedicine therapy and were statistically comparable with those who received in-person therapy (Rangarathnam et al., 2015). An intensive voice therapy model for 10 women diagnosed with vocal fold nodules received one therapy session in person and the remaining eight therapy sessions via telemedicine 3 times a week for 3 weeks (Fu et al., 2015). Post–telemedicine treatment comparisons revealed significant improvements in perceptual ratings, mean fundamental frequency, perturbation, mean airflow rate, voice handicap index total score and physical score, and stroboscopy ratings, including mucosal wave, vocal fold edge, glottal closure, and reduced edema posttreatment (Fu et al., 2015). Patients with PD were found to have comparable improvement via telemedicine therapy as compared to those who received therapy face-to-face (Howell et al., 2009). Telemedicine for seven female patients diagnosed with paradoxical vocal fold motion during a restrospective review was found to have symptom resolution via telemedicine by an SLP, as well as reduced medical costs as compared to in-person therapy (Towery, 2012).
Additional advantages of telemedicine therapy compared to in-person therapy are subspecialized services accessibility, provider and patient convenience, and reduced travel burdens (Kelchner, 2013). During the COVID-19 era, telemedicine continues to allow therapeutic services to be delivered in the safety of the patient's home without the restrictions of face masks and to maintain physical distancing recommendations (Bokolo, 2020). Disadvantages continue to be technology accessibility, sound quality, poor or low Internet bandwidth, out-of-state service restrictions, inability to perform digital laryngeal manipulation and/or manual circumlaryngeal techniques, and lack of insurance coverage (Bokolo, 2020).
Pediatric Considerations
As with adults, voice therapy with children often involves tasks that can potentially increase droplets. SLPs should wear necessary PPE; however, the patient cannot see the clinician's mouth. Creative ways of getting around this include using a clear mask and creating videos for the child to watch. Play with children often occurs in proximity, as it can be hard to engage in a board game or card game, or imaginative play with toys from 6 ft away. Additionally, for most therapy tasks, it is possible for the patient to wear a mask, but children may have more difficulty than adults keeping a mask on. It can be helpful to get buy-in from parents so that they are wearing a mask and encouraging their child to do the same. If tasks cannot be done with a mask on or if the child has difficulty wearing the mask, increasing distance or considering telemedicine is recommended.
Plexiglas shields have been suggested as a potential alternative to masks. The CDC and OSHA have both recommended the use of Plexiglas shields to reduce distribution of droplets in settings, including pharmacies and retail locations, but do not recommend it as a substitute from use of PPE in medical settings (CDC, 2020b, 2020c; OSHA, 2020b). At this time, the evidence indicates that the shield could protect against droplets, but smaller droplets or aerosolized particles could hang in the air or disperse around the shield, and it is not a substitute for a mask. In a very small room, it is questionable how much benefit would be derived from the Plexiglas shield, but it could be more helpful in a larger one. To date, no studies have been done on the use of Plexiglas in speech therapy or similar activities. Another solution suggested has been for therapy participants to wear a clear face shield for tasks that cannot be done in a mask.
Telemedicine can be a service delivery model for children as well. The same advantages and disadvantages listed above apply for children, with some notable differences. Parents do not have to find care for siblings or bring them to appointments, potentially increasing risk for COVID-19 exposure. Children may benefit more from being able to see the clinician's face during therapy tasks. Challenges include children having difficulty remaining engaged in front of a screen for the full session, maintaining a position where the clinician can see them on the screen, and maintaining consistent distance from the microphone. For patients with exercise-induced laryngeal obstruction, they are able to engage in their typical exercise routine with the clinician supporting them, as long as Internet is available and privacy can be maintained. To date, outcomes of telemedicine in pediatric voice therapy have not been studied, but the use of a web-based telehealth platform to provide supported home practice for weekly voice therapy was found to be feasible and effective in children aged 10–14 years of age (Doarn et al., 2019).
Video therapy was found to be as effective as in-person therapy in the treatment of articulation disorders (Grogan-Johnson et al., 2010). More research is needed to evaluate the effectiveness of telehealth voice therapy in children compared to traditional in-person care, but especially during the pandemic, telehealth should be considered as a viable option.
Equipment Considerations
SLP care for voice and upper airway requires utilization of medical equipment that are placed in or are in proximity to the mouth, nose, and pharynx (see Table 1). Pre–COVID-19, disinfection and sterilization procedures should have already been in place to prevent the spread of virus or bacteria from one patient to another; however, it is prudent to revisit these processes. Standard disinfection procedures should continue to be followed (Kramer et al., 2015), as per recommendations made by each institution. Instructions for use manuals should be consulted for endoscopes. In addition, the use of disposables (i.e., tubing) has been introduced by manufacturers to mitigate cumbersome cleaning (i.e., intra-oral pressure tubes, pressure port tubes, flow head tubes). Microphones may catch droplets in the mesh and can be more difficult to disinfect. Procedures are dependent on the type of microphone used, and we would recommend seeking guidance from the manufacturer and your infection control department to determine the best way to clean between patients.
Conclusions
For SLPs who specialize in the care and management of voice and upper airway disorders, it is essential that there is comprehensive understanding of SARS-CoV-2, its viral transmission, the disease COVID-19, and their daily practices to ensure mitigation of risk for their patients and themselves. As future progress is made and we understand the viral transmission of SARS-CoV-2 to a greater degree, it is likely that our abovementioned recommendations will change. It will therefore be worthwhile to evaluate progress and reassess directions as scientific advances are made and the field further matures. Given the current level of community spread in the United States and beyond, precautions related to COVID-19 are likely to be a part of our practice for some time. Lastly, the applicability of these considerations to future pandemics, viral illnesses, and outbreaks cannot be overstated.
Acknowledgments
This work was completed with support of monies from the Diane M. Bless Endowed Chair and by National Institute on Deafness and Other Communication Disorders Grants R01DC012773 and DC012773 (awarded to Thibeault).
Funding Statement
This work was completed with support of monies from the Diane M. Bless Endowed Chair and by National Institute on Deafness and Other Communication Disorders Grants R01DC012773 and DC012773 (awarded to Thibeault).
References
- American Academy of Pediatrics and the Children's Hospital Association. (2020). Children and COVID-19: State data report. Summary of publicly reported data from 49 states, NYC, DC, PR, and GU. https://downloads.aap.org/AAP/PDF/AAP%20and%20CHA%20-%20Children%20and%20COVID-19%20State%20Data%20Report%209.3.20%20FINAL.pdf
- American Speech-Language-Hearing Association. (2020a). ASHA guidance to SLPs regarding aerosol generating procedures. https://www.asha.org/slp/healthcare/asha-guidance-to-slps-regarding-aerosol-generating-procedures/
- American Speech-Language-Hearing Association. (2020b). Considerations when providing voice services in the absence of endoscopic evaluation during COVID-19. https://www.asha.org/slp/healthcare/considerations-when-providing-voice-services-in-the-absence-of-endoscopic-evaluation-during-covid-19/
- American Speech-Language-Hearing Association. (2020c). COVID-19: Tracking of state laws and regulations for telepractice and licensure policy. https://www.asha.org/uploadedfiles/state-telepractice-policy-covid-tracking.pdf
- Anfinrud, P. , Stadnytskyi, V. , Bax, C. E. , & Bax, A. (2020). Visualizing speech-generated oral fluid droplets with laser light scattering. New England Journal of Medicine, 382(21), 2061–2063. https://www.nejm.org/doi/10.1056/NEJMc2007800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asadi, S. , Wexler, A. , Cappa, C. , Barreda, S. , Bouvier, N. , & Ristenpart, W. D. (2019). Aerosol emission and superemission during human speech increase with voice loudness. Scientific Reports, 9(1), 2348. https://doi.org/10.1038/s41598-019-38808-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokolo, A. (2020). Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Irish Journal of Medical Science, 1–10. https://doi.org/10.1007/s11845-020-02299-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byambasuren, O. , Cardona, M. , Bell, K. , Clark, J. , Mclaws, M. , & Glasziou, P. (2020). Estimating the extent of true asymptomatic COVID-19 and its potential for community transmission: Systematic review and meta-analysis. MedRxiv. https://doi.org/10.1101/2020.05.10.20097543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castagnoli, R. , Votto, M. , Licari, A. , Brambilla, I. , Bruno, R. , Perlini, S. , Rovida, F. , Baldanti, F. , & Marseglia, G. L. (2020). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: A systematic review. Journal of the American Medical Association of Pediatrics. https://doi.org/10.1001/jamapediatrics.2020.1467 [DOI] [PubMed] [Google Scholar]
- Castilles-Allendes, A. , Contreras-Ruston, F. , Cantor-Cutiva, L. , Codino, J. , Guzman, M. , Malebran, C. , Manzano, C. , Pavez, A. , Vaiano, T. , Wilder, F. , & Behlau, M. (2020). Voice therapy in the context of the COVID-19 pandemic: Guidelines for clinical practice. Journal of Voice. https://doi.org/10.1016/j.jvoice.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020a). Coronavirus disease 2019 in children—United States. Morbidity and Mortality Weekly Report, 69(14), 422–426. https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e4.htm?s_cid=mm6914e4_w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020b). Employer information for office buildings. https://www.cdc.gov/coronavirus/2019-ncov/community/office-buildings.html
- Centers for Disease Control and Prevention. (2020c). Guidance for pharmacists and pharmacy technicians in community pharmacies during the COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/pharmacies.html
- Cheng, V. C. , Wong, S. C. , Chan, V. W. , So, S. Y. , Chen, J. H. , Yip, C. C. , Chan, K. , Chu, H. , Chung, T. W. , Sridhar, S. K. , To, K. K. , Chan, J. F. , Hung, I. F. , Ho, P. , & Yuen, K. Y. (2020). Air and environmental sampling for SARS-CoV-2 around hospitalized patients with coronavirus disease 2019 (COVID-19). Infectection Control & Hospital Epidemiology, 41(11), 1258–1265. https://doi.org/10.1017/ice.2020.282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia, P. Y. , Coleman, K. K. , Tan, Y. K. , Ong, S. W. X. , Gum, M. , Lau, S. K. , Lim, X. F. , Lim, A. S. , Sutjipto, S. , Lee, P. H. , Son, T. T. , Young, B. E. , Milton, D. K. , Gray, G. C. , Schuster, S. , Barkham, T. , De, P. P. , Vasoo, S. , Chan, M. , …. Singapore 2019 Novel Coroavirus Outbreak Research Team. (2020). Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nature Communications, 11(1), 2800. https://doi.org/10.1038/s41467-020-16670-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu, D. K. , Akl, E. A. , Duda, S. , Solo, K. , Yaacoub, S. , & Schünemann, H. J. (2020). Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet, 395(10242), 1973–1987. https://doi.org/10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantinescu, G. , Theodoros, D. , Russell, T. , Ward, E. , Wilson, S. , & Wootton, R. (2010). Assessing disordered speech and voice in Parkinson's disease: A telerehabilitation application. International Journal of Language & Communication Disorders, 45(6), 630–644. https://doi.org/10.3109/13682820903470569 [DOI] [PubMed] [Google Scholar]
- Doarn, C. R. , Zacharias, S. , Keck, C. S. , Tabangin, M. , DeAlarcon, A. , & Kelchner, L. (2019). Design and implementation of an interactive website for pediatric voice therapy—The concept of in-between care: A telehealth model. Telemed Journal and EHealth, 25(5), 415–422. https://doi.org/10.1089/tmj.2018.0108 [DOI] [PubMed] [Google Scholar]
- Duffy, J. R. , Werven, G. W. , & Aronson, A. E. (1997). Telemedicine and the diagnosis of speech and language disorders. Mayo Clinic Proceedings, 72(12), 1116–1122. https://www.sciencedirect.com/science/article/pii/S0025619611636732?via%3Dihub [DOI] [PubMed] [Google Scholar]
- Faridi, S. , Niazi, S. , Sadeghi, K. , Naddafi, K. , Yavarian, J. , Shamsipour, M. , Jandaghi, N. Z. S. , Sadeghniiat, K. , Navizadeh, R. , Yunesian, M. , Momeniha, F. , Mokamel, A. , Hassanvand, M. S. , & MokhtariAzad, T. (2020). A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Science of the Total Environment, 725. https://doi.org/10.1016/j.scitotenv.2020.138401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fieux, M. , Duret, S. , Bawazeer, N. , Denoix, L. , Zaouche, S. , & Tringali, S. (2020). Telemedicine for ENT: Effect on quality of care during COVID-19 pandemic. European Annals of Otorhinolaryngology, Head and Neck Diseases, 137(4), 257–261. https://doi.org/10.1016/j.anorl.2020.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu, S. , Theodoros, D. , & Ward, E. (2015). Delivery of intensive voice therapy for vocal fold nodules via telepractice: A pilot feasibility and efficacy study. Journal of Voice, 29(6), 697–706. https://doi.org/10.1016/j.jvoice.2014.12.003 [DOI] [PubMed] [Google Scholar]
- Fung, T. S. , & Liu, D. X. (2019). Human xoronavirus: Host–pathogen interaction. Annual Reviews of Microbiology, 8(73), 529–557. https://doi.org/10.1146/annurev-micro-020518-115759 [DOI] [PubMed] [Google Scholar]
- Gillespie, A. , & Gartner-Schmidt, J. (2016). Immediate effect of stimulability assessment on acoustic, aerodynamic and patient-perceptual measures of voice. Journal of Voice, 30(4), 507.e9–507.e14. https://doi.org/10.1016/j.jvoice.2015.06.004 [DOI] [PubMed] [Google Scholar]
- Giovanni, A. , Radulesco, T. , Bouchet, G. , Mattei, A. , Révis, J. , Bogdanski, E. , & Michel, J. (2020). Transmission of droplet-conveyed infectious agents such as SARS-CoV-2 by speech and vocal exercises during speech therapy: Preliminary experiment concerning airflow velocity. European Archives of Otorhinolaryngology, 16, 1–6. https://doi.org/10.1007/s00405-020-06200-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Givi, B. , Schiff, B. A. , Chinn, S. B. , Clayburgh, D. , Iyer, N. G. , Jalisi, S. , Moore, M. G. , Nathan, C. , Orloff, L. A. , O'Neill, J. P. , Paker, N. , Zender, C. , Morris, L. G. T. , & Davies, L. (2020). Safety recommendations for evaulation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngology—Head & Neck Surgery, 146(6), 579–558. https://doi.org/10.1001/jamaoto.2020.0780 [DOI] [PubMed] [Google Scholar]
- Grogan-Johnson, S. , Alvares, R. , Rowan, L. , & Creaghead, N. (2010). A pilot study comparing the effectiveness of speech language therapy provided by telemedicine with conventional on-site therapy. Journal of Telemediciine Telecare, 16(3), 134–139. https://doi.org/10.1258/jtt.2009.090608 [DOI] [PubMed] [Google Scholar]
- Guan, W. J. , & Zhong, N. S. (2020). Clinical characteristics of COVID-19 in China. Reply. The New England Journal of Medicine, 382(19), 1861–1862. https://doi.org/10.1056/nejmc2005203 [DOI] [PubMed] [Google Scholar]
- Guo, Z. D. , Wang, Z. Y. , Zhang, S. F. , Li, X. , Li, L. , Li, C. , Dong, X.-Y. , Chi, M.-Y. , Cao, Z. C. , Zhang, K. , Gao, Y.-W. , & Chen, W. (2020). Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerging Infectious Disease, 26(7), 1583–1591. https://doi.org/10.3201/eid2607.200885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamner, L. , Dubbel, P. , Capron, I. , Ross, A. , Jordan, A. , Lee, J. , Lynn, J. , Ball, A. , Narwal, S. , Russell, S. , Patrick, D. , & Leibrand, H. (2020). High SARS-CoV-2 attack rate following exposure at a choir practice—Skagit County, Washington, March 2020. Morbidity and Mortality Weekly Report, 69(19), 606–610. https://doi.org/10.15585/mmwr.mm6919e6 [DOI] [PubMed] [Google Scholar]
- Holshue, M. L. , DeBolt, C. , Lindquist, S. , Lofy, K. H. , Wiesman, J. , Bruce, H. , Spitters, C. , Ericson, K. , Wilkerson, S. , Patel, A. , Pharm, D. , Gerber, S. I. , Kim, L. , Tong, S. , Lu, X. , Lindstrom, S. , …. Washington State 2019-nCoV Case Investigation. (2020). First case of 2019 novel coronavirus in the United States. The New England Journal of Medicine, 382(10), 929–936. https://doi.org/10.1056/nejmoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell, S. , Tripoliti, E. , & Pring, T. (2009). Delivering the Lee Silverman Voice Treatment (LSVT) by web camera a feasibility study. International Journal of Language & Communication Disorders, 44(3), 287–300. https://doi.org/10.1080/13682820802033968 [DOI] [PubMed] [Google Scholar]
- Johns Hopkins Coronavirus Resource Center. (2020). COVID-19 dashboard by the Center for Systems Science and Engineering at Johns Hopkins University. https://coronavirus.jhu.edu/map.html
- Kelchner, L. (2013). Telehealth and the treatment of voice sisorders: A discussion regarding evidence. SIG 3 Perspectives on Voice and Voice Disorders, 23(3), 88–94. https://doi.org/10.1044/vvd23.3.88 [Google Scholar]
- Kramer, A. , Kohnen, W. , Israel, S. , Ryll, S. , Hübner, N. O. , Luckhaupt, H. , & Hosemann, W. (2015). Principles of infection prevention and reprocessing in ENT endoscopy. GMS Current Topics in Otorhinolaryngology—Head and Neck Surgery, 14, Doc10. https://doi.org/10.3205/cto000125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lammers, M. , Lea, J. , Lea, J. , & Westerberg, B. (2020). Guidance for otolaryngology health care workers performing aerosol generating medical procedures during the COVID-19 pandemic. Journal of Otolaryngology—Head & Neck Surgery, 49(1), 36. https://doi.org/10.1186/s40463-020-00429-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanari, M. , Chiereghin, A. , Biserni, G. B. , Rocca, A. , Re, M. C. , & Lazzarotto, T. (2020). Children and SARS-CoV-2 infection: Innocent bystanders until proven otherwise. Clinical Microbiology and Infection, 26(9), 1130–1132. https://doi.org/10.1016/j.cmi.2020.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Y. , Ning, Z. , Chen, Y. , Guo, M. , Gali, N. K. , Sun, L. , Duan, Y. , Cai, J. , Westerdahl, D. , Liu, X. , Xu, K. , Ho, K. , Kan, H. , Fu, Q. , & Lan, K. (2020). Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature, 582(7813), 557–560. https://doi.org/10.1038/s41586-020-2271-3 [DOI] [PubMed] [Google Scholar]
- Ludvigsson, J. F. (2020). Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica, 109(6), 1088–1095. https://doi.org/10.1111/apa.15270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, J. , Qi, X. , Chen, H. , Li, X. , Zhan, Z. , Wang, H. , Sun, L. , Zhang, L. , Guo, J. , Morawska, S. , Grinshpun, S. A. , Biswas, P. , Flagan, R. C. , & Yao, M. (2020). Exhaled breath is a significant source of SARS-CoV-2 emission (Preprint). MedRxiv. https://doi.org/10.1101/2020.05.31.20115154 [Google Scholar]
- Mashima, P. , Birkmire-Peters, D. , Syms, M. , Holtel, M. , Burgess, L. P. , & Peters, L. (2003). Telehealth: Voice therapy using telecommunications technology. American Journal of Speech-Language Pathology, 12(4), 432–439. https://doi.org/10.1044/1058-0360(2003/089) [DOI] [PubMed] [Google Scholar]
- Mashima, P. , & Brown, J. (2011). Remote management of voice and swallowing disorders. Otolaryngologic Clinics of North America, 44(6), 1305–1316. https://doi.org/10.1016/j.otc.2011.08.007 [DOI] [PubMed] [Google Scholar]
- Matson, M. J. , Yinda, C. K. , Seifert, S. N. , Bushmaker, T. , Fischer, R. J. , van, Doremalen, N. , Lloys-Smith, J. O. , & Munster, V. J. (2020). Effect of environmental conditions on SARS-CoV-2 stability in human nasal mucus and sputum. Emerging Infectious Disease, 26(9), 2276–2278. https://doi.org/10.3201/eid2609.202267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattei, A. , Amy de la Bretèque, B. , Crestani, S. , Crevier-Buchman, L. , Galant, C. , Hans, S. , Julien-Laferriere Giovanni, A. , French Society of Otorhinolaryngology, Head, Neck Surgery, & French Society of Phoniatrics, Laryngology. (2020). Guidelines of clinical practice for the management of swallowing disorders and recent dysphonia in the context of the COVID-19 pandemic. European Annals of Otorhinolaryngology, Head and Neck Diseases, 137(3), 173–175. https://doi.org/10.1016/j.anorl.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska, L. , & Cao, J. (2020). Airborne transmission of SARS-CoV-2: The world should face the reality. Environment International, 139, 105730. https://doi.org/10.1016/j.envint.2020.105730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, J. (2020). Planning for reactivation of ambulatory care settings post–COVID-19 pandemic restrictions. Journal of Ambulatory Care Management, 43(4), 286–289. https://doi.org/10.1097/jac.0000000000000341 [DOI] [PubMed] [Google Scholar]
- Namasivayam-MacDonald, A. M. , & Riquelme, L. F. (2020). Speech-language pathology management for adults with COVID-19 in the acute hospital setting: Initial recommendations to guide clinicians. American Journal of Speech-Language Pathology. https://doi.org/10.1044/2020_AJSLP-20-00096 [DOI] [PubMed] [Google Scholar]
- New Zealand Speech-Language Therapists' Association. (2020). COVID-19 guidance for DHB SLTs. https://speechtherapy.org.nz/wp-content/uploads/2020/05/NZSTACOVID-19Level3forDHBs_final.pdf
- Occupational Safety and Health Administration. (2020a). COVID-19—Control and prevention. Healthcare workers and employers. https://www.osha.gov/SLTC/covid-19/healthcare-workers.html
- Occupational Safety and Health Administration. (2020b). COVID-19 guidance for retail pharmacies. https://www.osha.gov/pls/publications/publication.searchresults?pSearch=Coronavirus%3A+COVID-19+Guidance+for+Retail+Pharmacies%3A+OSHA+Alert
- Pan, Y. , Zhang, D. , Yang, P. , Poon, L. L. M. , & Wang, Q. (2020). Viral load of SARS-CoV-2 in clinical samples. The Lancet Infectioius Diseases, 20(4), 411–412. https://doi.org/10.1016/S1473-3099(20)30113-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, Y. , Choe, Y. , Park, O. , Park, S. , Kim, Y. , & Kim, J. (2020). Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emergergency Infectious Disease, 26(10), 2465–2468. https://doi.org/10.3201/eid2610.201315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel, R. , Awan, S. , Barkmeier-Kraemer, J. , Courey, M. , Deliyski, D. , Eadie, T. , Paul, D. , Svec, J. G. , & Hillman, R. (2018). Recommended protocols for instrumental assessment of voice: American Speech-Language-Hearing Association expert panel to develop a protocol for instrumental assessment of vocal function. American Journal of Speech-Language Pathology, 27(3), 887–910. https://doi.org/10.1044/2018_AJSLP-17-0009 [DOI] [PubMed] [Google Scholar]
- Rameau, A. , Young, V. , Amin, M. , & Sulica, L. (2020). Flexible laryngoscopy and COVID-19. Otolaryngology—Head & Neck Surgery, 162(6), 813–815. https://doi.org/10.1177/0194599820921395 [DOI] [PubMed] [Google Scholar]
- Rangarathnam, B. , Gilroy, H. , & Mccullough, G. (2016). Do patients treated for voice therapy with telepractice show similar changes in voice outcome measures as patients treated face-to-face. Evidence-Based Practice Briefs, 11(5), 1–6. [Google Scholar]
- Rangarathnam, B. , McCullough, G. H. , Pickett, H. , Zraick, R. I. , Tulunay-Ugur, O. , & McCulloughber-Flusberg, K. (2015). Telepractice versus in-person delivery of voice therapy for primary muscle tension dysphonia. American Journal of Speech-Language Pathology, 24(3), 386–399. https://doi.org/10.1044/2015_AJSLP-14-0017 [DOI] [PubMed] [Google Scholar]
- Reddy, P. , Nguyen, S. , & Deschler, D. (2020). Bronchoscopy, laryngoscopy, and esophagoscopy during the COVID-19 pandemic. Head & Neck, 42(7), 1634–1637. https://doi.org/10.1002/hed.26221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riollano-Cruz, M. , Akkoyun, E. , Briceno-Brito, E. , Kowalsky, S. , Posada, R. , Sordillo, E. M. , Tosi, M. , Trachtman, R. , & Paniz-Mondolfi, A. (2020). Multisystem inflammatory syndrome in children (MIS-C) related to COVID-19: A New York City experience. Journal of Medical Virology, 1–10. https://doi.org/10.1002/jmv.26224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royal College of Speech and Language Therapists. (2020). RCSLT guidance on personal protective equipment (PPE) and COVID-19. https://www.rcslt.org/-/media/docs/Covid/RCSLT-PPE-guidance-3-April-2020_FINAL.PDF?la=en&hash=BD9532BE5695A2BBF36CC549912BF73BC8C69395
- Santarpia, J. L. , Rivera, D. N. R. , Herrara, V. , Morwitzer, M. J. , Creager, H. , Santarpia, G. , Crown, K. K. , Brett-Major, D. , Schnaubelt, E. , Broadhurst, M. J. , Lawler, J. V. , Reid, P. , & Lowe, J. J. (2020). Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska Medical Center. MedRxiv. https://doi.org/10.1101/2020.03.23.20039446 [Google Scholar]
- Somsen, G. A. , van Rijn, C. , Kooij, S. , Bem, R. A. , & Bonn, D. (2020). Small droplet aerosols in poorly ventilated spaces and SARS-CoV-2 transmission. Lancet Respiratory Medicine, 8(7), 658–659. https://doi.org/10.1016/S2213-2600(20)30245-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speech-Language & Audiology Canada. (2020). Update on aerosol-generating medical procedures. https://www.sac-oac.ca/news-events/news/update-aerosol-generating-medical-procedures
- Speech Pathology Australia. (2020). COVID-19 News and Information. https://www.speechpathologyaustralia.org.au/SPAweb/About_us/COVID-19_News_and_Information/SPAweb/About_Us/News/COVID-19.aspx?hkey=0bee894c-a70a-4608-8217-a5df8161063f
- Tan, V. , Zhang, E. , Daniel, D. , Sadovoy, A. , Teo, N. , Kiong, K. , & Yuen, H. W. (2020). Respiratory droplet generation and dispersal during nasoendoscopy and upper respiratory swab testing. Head & Neck, 42(10), 2779–2781. https://doi.org/10.1002/hed.26347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Irish Association of Speech & Language Therapists. (2020). IASLT position statement regarding the use of personal protective equipment (PPE). https://www.iaslt.ie/news.php?newsitem=1593617931&display=access
- Tian, W. N. , Huang, Y. H. , & Dai, C. (2020). The effect of the COVID-19 pandemic on the medical mode of patients with inflammatory bowel disease in China. Inflammatory Bowel Diseases, 26(10), e116–e117. https://doi.org/10.1093/ibd/izaa197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tikka, T. , Kavanagh, K. , Lowit, A. , Jiafeng, P. , Burns, H. , Nixon, I. , Paleri, V. , & MacKenzie, K. (2020). Head and neck cancer risk calculator (HaNC-RC)—V.2. Adjustments and addition of symptoms and social history factors. Clinical Otolaryngology, 45(3), 380–388. https://doi.org/10.1111/coa.13511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towery, M. (2012). Speech therapy telepractice for vocal cord dysfunction (VCD): MaineCare (Medicaid) cost savings. International Journal of Telerehabilitation, 13, 4(1), 33–36. https://doi.org/10.5195/ijt.2012.6095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen, N. , Bushmaker, T. , Morris, D. H. , Holbrook, M. G. , Gamble, A. , Williamson, B. , Tamin, A. , Harcourt, J. , Thornburg, N. , Gerber, S. , Lloyd-Smith, J. , Wit, E. , & Munster, V. (2020). Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. MedRxiv. https://doi.org/10.1101/2020.03.09.20033217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Z. , Zhou, Q. , Wang, C. , Shi, Q. , Lu, S. , Ma, Y. , Luo, X. , Xun, Y. , Li, W. , Baskota, M. , Yang, Y. , Zhai, H. , Fukuoka, T. , Ahn, H. S. , Lee, M. S. , & Chen, Y. (2020). Clinical characteristics of children with COVID-19: A rapid review and meta-analysis. Annals of Translational Medicine, 8(10), 620. https://doi.org/10.21037/atm-20-3302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson, E. , Walker, A. , Bhaskaran, K. , Bacon, S. , Bates, C. , Morton, C. , … Goldacre, B. (2020). OpenSAFELY: Factors associated with COVID-19 death in 17 million patients. Nature, 584(7821), 430–436. https://doi.org/10.1038/s41586-020-2521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wölfel, R. , Corman, V. M. , Guggemos, W. , Seilmaier, M. , Zange, S. , Müller, M. A. , Niemeyer, D. , Jones, T. C. , Vollmar, P. , Rothe, C. , Hoelscher, M. , Bleicker, T. , Brunink, S. , Schneider, J. , Ehmnann, R. , Zwirglmaier, K. , Drosten, C. , & Wendtner, C. (2020). Virological assessment of hospitalized patients with COVID-2019. Nature, 581(7809), 465–469. https://doi.org/10.1038/s41586-020-2196-x [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2014). Infection prevention and control of epidemic and pandemic prone acute respiratory infections in health care. https://apps.who.int/iris/bitstream/handle/10665/112656/9789241507134_eng.pdf;jsessionid=136B6345F707421ACD161A0973B28E3E?sequence=1 [PubMed]
- World Health Organization. (2020). Transmission of SARS-CoV-2: Implications for infection prevention precautions. https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions
- Xu, K. , Chen, Y. , Yuan, J. , Yi, P. , Ding, C. , Wu, W. , Li, Y. , Ni, Q. , Zou, R. , Li, X. , Zhang, Y. , Zhao, H. , Zhang, X. , Yu, L. , Su, J. , Lang, Q. , Liu, J. , Wu, X. , Guo, Y. , … Li, L. (2020). Factors associated with prolonged viral RNA shedding in patients with coronavirus disease 2019 (COVID-19). Clinical Infectious Diseases, 71(15), 799–806. https://doi.org/10.1093/cid/iaa351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaga, C. J. , Pandian, V. , Brodsky, M. B. , Wallace, S. , Cameron, T. S. , Chao, C. , Orloff, L. A. , Atkins, N. E. , McGrath, B. A. , Lazarus, C. L. , Vogel, A. P. , & Brenner, M. J. (2020). Speech-language pathology guidance for tracheostomy during the COVID-19 pandemic: An international multidisciplinary perspective. American Journal of Speech-Language Pathology, 29(3), 1320–1334. https://doi.org/10.1044/2020_AJSLP-20-00089 [DOI] [PubMed] [Google Scholar]
- Zughni, L. A. , Gillespie, A. I. , Hatcher, J. L. , Rubin, A. D. , & Giliberto, J. P. (2020). Telemedicine and the interdiscplinary clinic model: During the COVID-19 pandemic and beyond. Otolaryngology—Head & Neck Surgery, 163(4), 673–675. https://doi.org/10.1177/0194599820932167 [DOI] [PubMed] [Google Scholar]