Abstract
By adulthood, most males with FXS require support to navigate day-to-day settings. The present study cross-sectionally: (1) characterized the profile of daily living skills in males with FXS and (2) examined associated participant characteristics (i.e., FMRP expression, nonverbal cognition, language, ASD symptomatology, and anxiety symptomatology) using the Waisman-Activities of Daily Living questionnaire. Males with FXS (n = 57, ages 15 – 23 years) needed more help/support in the areas of domestic and community daily livings skills, than in the area of personal daily living skills. Significant associations were observed between reduced daily living skills and lower nonverbal cognition, receptive language, expressive language, and increased ASD symptomatology. Receptive language emerged as the strongest unique predictor of daily living skill performance.
Keywords: fragile X syndrome, daily living skills, language, autism spectrum disorder, FMRP
Introduction
Fragile X syndrome (FXS), the most common inherited cause of intellectual disability, is conservatively estimated to affect approximately 1 in 7000 males and 1 in 11,000 females (Hunter et al., 2014). FXS results from a mutation on the FMR1 gene of the X chromosome, in which a repetitive sequence of trinucleotides (CGG) is expanded beyond 200 repeats (the so-called “full mutation”). This repeat expansion subsequently causes either an absence of or a significant reduction in fragile X mental retardation protein (FMRP), a protein critical for experience-dependent neural development (Bassell & Warren, 2008). Importantly, because of the presence of a second unaffected X chromosome in females, which continues to produce FMRP, biological sex and FMRP expression are inherently confounded when exploring the FXS phenotype, with females being less severely affected on average than males (Hunter et al., 2014). Even in adulthood, most males with FXS require support to navigate day-to-day settings. In the present study, we characterize the profile of daily living skills in males with FXS, using the Waisman-Activities of Daily Living questionnaire, and examine associated participant characteristics including FMRP expression, nonverbal cognition, language, ASD symptomatology, and anxiety symptomatology.
For males with FXS, cognitive challenges are typically observed across multiple domains of function, including attention (Cornish, Cole, Longhi, Karmiloff-Smith, & Scerif, 2012), executive function (Hooper et al., 2008), memory (Ornstein et al., 2008), and language (Abbeduto, McDuffie, Thurman, & Kover, 2016). Moreover, the FXS phenotype in males is also characterized by the co-occurring presentation of several other behavioral characteristics that often persist into adulthood. In particular, anxiety (Cordeiro, Ballinger, Hagerman, & Hessl, 2011), hyperarousal (Klusek, Roberts, & Losh, 2015), hyperactivity (Grefer, Flory, Cornish, Hatton, & Roberts, 2016; Thurman, McDuffie, Hagerman, & Abbeduto, 2014), and autism spectrum disorder (Abbeduto, McDuffie, & Thurman, 2014; Klusek, Martin, & Losh, 2014a) are often observed in males with FXS. Although much is known about the FXS phenotype in males, there are relatively few studies focused specifically on the phenotypic presentation during adolescence and early adulthood, including the investigation of adaptive functioning. This period of development is a particularly important time to consider because it is not only associated with increased opportunities for growth, but also new challenges as youth shift into the phase of young adulthood (Blacher, 2001). Moreover, vocational and adaptive programs during this period often focus on goals supporting youth autonomy. Thus, studies focused on this developmental period may generate vital information that can in turn facilitate refining young adult transition and support programs designed to optimize the independence and quality of life of males with FXS.
Adaptive functioning is a broad term used to refer to the conceptual, social, and practical skills that people learn and use in their daily lives (American Association on Intellectual and Developmental Disabilities., 2021). Daily living skills represent a particular subset of adaptive functioning skills; specifically, the “practical” self-care skills that are learned and used across daily living settings, such as personal hygiene, meal preparation, and money/time management (Stabel et al., 2013). These skills are critical for living independently and obtaining employment; thus, underdevelopment of these skills limit an individual’s ability to function independently. Elucidating the nature of daily living skills of adolescents and young adults with FXS, and the factors supporting their development, will provide insights into interventions to enhance those skills and enhance family well-being (Järbrink, McCrone, Fombonne, Zandén, & Knapp, 2007). In addition, in the present study, we sought to characterize daily living skills and examine the participant characteristics that relate to daily living skills, and therefore may be predictive of independence, in males with FXS during late adolescence and early adulthood.
Daily Living Skills in FXS
By adulthood, most males with FXS demonstrate a limited capacity to function independently, and require support in order to navigate academic, employment, residential, and/or community settings (Bailey, Raspa, Holiday, Bishop, & Olmsted, 2009; Hartley et al., 2011). Data from a large-scale national caregiver-report study by Hartley et al. (2011) reported that males with FXS are described by caregivers as needing moderate or considerable assistance when navigating their everyday life, when considering the options of no assistance (4.87%), minimal amount of assistance (38.05%), or moderate or considerable amount of assistance (57.08%). That said, most males with FXS were still able to hold a part-time or full-time employment (79.56%), had at least 1 friend (80.99%), and participated in multiple (3+) leisure activities (86.73%). As part of the study, caregivers rated their adult children’s ability to perform 37 daily living skills, which were selected to be of interest by the study authors. Considering only those 20 skills that focused on personal daily living skills, such as eating, dressing, toileting, and bathing/personal hygiene, by the age of 20 years, most males (>85%) were reported to be able to eat, dress, bathe, and use the toilet either fairly well or very well. That said, fewer than 65% of males were able to eat at a normal pace, tie their shoes independently, wipe themselves independently, or brush their hair/teeth (Bailey et al., 2009). Hartley et al. (2011) found daily living skills (referred to by study authors as functional skills) to be the strongest predictor of overall independence, when also interpersonal skills and co-occurring mental health conditions (such as inattention, anxiety, and depression).
Limitations in daily living skills appear early in development for individuals with FXS, with delays apparent before the end of the first year of life (Caravella & Roberts, 2017). Moreover, not only are slower rates of development observed in individuals with FXS relative to their typically developing peers, but also considerable variability has been noted in the trajectories of skill acquisition (e.g., Caravella & Roberts, 2017; Hahn, Brady, Warren, & Fleming, 2015). However, few studies have considered daily living skills during adolescence and early adulthood. Because this developmental period marks a critical turning point for youth and families, investigations that elucidate the skills, experiences, and factors supporting development during this time may help clarify the needs of families and guide intervention.
Unfortunately, there are only limited data regarding the daily living skills of individuals with FXS during the important transition from adolescence into adulthood. Dykens and colleagues focused on participants ranging in age from 10 to 17 years and found that, when using the Vineland Adaptive Behavior Scale (VABS; Sparrow, Balla, & Cicchetti, 1984), age-equivalent (AE) scores for the Daily Living Skills domain were significantly higher than were AE scores in both the Communication and Socialization domains (Dykens, Hodapp, Ort, & Leckman, 1993). That said, it is important to recognize that the degree of delay can vary as a function of the types of daily living skills considered. For example, Fisch et al. (1999), when using the VABS, found that skills supporting functioning in the community were generally weaker than domestic skills or personal care skills for males with FXS between 4 and 14 years of age. In addition, considerable variability is often observed across participants (Dykens et al., 1996). Although these studies are important in documenting variability of delay across domains and individuals, the factors shaping skill acquisition in this age period are not clear. Moreover, whether the data from these studies, collected nearly 30 years ago, may generalize to today’s youth with FXS is unclear. Increasing our understanding of the daily living skills of youth with FXS during this developmental period is important in order to inform curriculum development in our educational and community programs and optimize the vocational rehabilitation services designed to support males with FXS in achieving independence.
Factors Relating to Daily Living Skills in FXS
Our understanding of the factors that contribute to the development of daily living skills in adolescents and young adults with FXS remains limited. Both the behavioral features associated with the FXS phenotype and its underlying neurobiology are likely to play a key role in that development.
FMRP expression.
In individuals with FXS, variability in FMRP expression is responsible, at least in part, for the phenotypic variation observed across individuals with FXS. However, findings on the relationship between FMRP and adaptive functioning skills in FXS has been inconsistent. For example, Cohen et al. (1996), used cross-sectional data from participants ranging from 1 to 19 years of age to compare phenotypic performance between full-mutation males and males who were mosaic, meaning their genotypes consisted of a combination of cells with the full mutation and cells that did not. In that study, Cohen et al. found that the correlation between chronological age and VABS Daily Living Skills AE scores was significantly stronger for the mosaic participants than it was for the full-mutation participants In contrast, a study by Glaser and colleagues (2003a), which included participants ranging in age from 6 to 17 years, failed to find an association between level of FMRP and VABS Daily Living Skills domain standard scores in a sample of males and females, when controlling for age, participant sex, and full scale IQ score. Importantly, instead of using mosaic status, Glasser and colleagues considered the percentage of lymphocytes expressing FMRP; this methodological difference may be a key contributor to the differences observed in study results. Moreover, other differences in the methodological approaches across these studies, including participant ages, specific covariates included in the analyses, and metrics used to assess adaptive functioning, may have also contributed to the differing findings observed across studies. In sum, more research is needed to clarify the extent to which FMRP level is related to the daily living skills of youth with FXS as they transition into adulthood.
Chronological Age.
Many studies have considered the influences of age on daily living scores in adolescence and early adulthood, with findings varying across studies. For example, Dykens and colleagues (1993) found that, when using the VABS (Sparrow et al., 1984) to follow up on participants ranging in age from 10 to 17 years of age two years later, Daily Living Skills AE scores decreased (i.e., a decrease from 7.17 years to 5.43 years). In a second cross-sectional study, Dykens et al. (1996) compared performance by males with FXS between 11 to 15 years to those between 16 to 20 years and found no evidence of improvement or decline with age. Dykens and colleagues posited that these data, taken together, suggest that that daily living skills reach peak performance between 10 and 15 years and plateau thereafter. It is important to note that there are inherent psychometric problems associated with age-equivalent scores that significantly limit their reliability and validity. More specifically, age-equivalent scores reflect the median raw score for a particular age within the norming sample and, therefore, are not on a ratio or interval scale of measurement. Thus, these types of scores are not recommended in analyses.
In contrast to the patterns reported by Dykens et al., Bailey et al. (2009) reported cross-sectional increases between an adolescent/early adult group (16 – 20 years) and an adult group (over 20 years) in terms of the proportion of males with FXS described as having “mastered” a number of daily living skills, selected to be of interest by the study authors, based on results from a national survey of parents. Similarly, Klaiman et al., using the VABS (Sparrow et al., 1984), reported Daily Living Skills standard scores to increase in males with FXS between 14 and 18 years of age (Klaiman et al., 2014) and Usher et al. (2020), using the Waisman-Activities of Daily Living (Maenner et al., 2013), also reported gains in daily living skills during early adulthood. Importantly, unlike age-equivalent scores, standard scores preserve the absolute difference between scores and describe the individual’s performance relative to chronological age expectations. If an individual is gaining skills at the average rate expected for his/her chronological age, the standard score will remain stable; if an individual is gaining skills at a rate faster than expected for his/her chronological age, standard scores will increase, as seen in Klaiman et al (2014). In sum, although the number of studies considering this developmental period is limited, there is some evidence that gains in daily living skills are observed during the adolescent and early adult years.
Cognitive abilities.
Another characteristic associated with the FXS phenotype is the co-occurring presence of cognitive impairments/delays. Virtually all males with FXS present with IQ scores below 85, but there remains a considerable range of cognitive affectedness (Hessl et al., 2009). Importantly, intelligence and adaptive functioning are clearly distinct constructs. Intelligence typically refers to an individual’s ability/capacity to “reason, plan, solve problems, think abstractly, comprehend complex ideas, learn quickly, and learn from experience” (Gottfredson, 1997, p. 13). In contrast, adaptive functioning typically refers to an individual’s ability to perform/use skills in their day to day lives, while managing societal expectations (Tassé, 2017). Nonetheless, the two constructs are intertwined, and measures of the two are often correlated.
Consequently, adaptive functioning is often assessed in relation to overall cognitive level of the individual. For example, Dykens et al. observed a significant correlation between overall mental age scores and daily living skills as measured by the VABS (Dykens et al., 1993). The authors posited that trajectories of daily living skills paralleled the trajectories observed in cognitive development. A similar association was observed by Bailey et al. (2009), in which a dichotomous variable representing cognitive functioning (poor/fair vs. good/very good) was significantly associated with daily living skills in participants ages 11 years or older, using a list of daily living skills selected by the study authors. Interestingly, in a study of individuals with FXS ranging in age from 6 to 17 years, overall IQ score was the only significant independent contributor to VABS daily living skills in males with FXS, in models including age, sex, and FMRP expression (Glaser et al., 2003). None of these studies, however, considered the differential effects of nonverbal and verbal ability.
There is considerable research showing that language skills are a key predictor of independence in adulthood in other disability groups, such as ASD (Billstedt, Carina Gillberg, & Gillberg, 2007; Eaves & Ho, 2008; Howlin, Goode, Hutton, & Rutter, 2004; Lord & Bailey, 2002). Surprisingly, there is only one study to date that has considered the direct relationship between language ability and daily living skills in FXS. When considering standard scores from the Vineland-II (Sparrow, Cicchetti, & Balla, 2012), Shaffer et al. (2020) found that no significant association between daily living skills and expressive syntax derived from a spoken language sample in males with FXS between the ages of 5 and 36 years of age. Due to the significant delays observed in males with FXS, which are known to increase with age, scores that provide a metric of absolute ability (such as a raw score or growth score) may be more likely to yield a positive association than standard scores, which reflect the individual’s standing relative to similarly aged individuals from the general population. Moreover, it is possible that other facets of language, such as receptive syntax, which is a relative weakness for individuals with FXS (Oakes, Kover, & Abbeduto, 2013), could show a relationship with daily living skills because learning such skills would seem to require understanding verbal instructions from other people. Thus, research considering the influences of nonverbal cognitive ability and language ability, including both expressive and receptive skills, on daily living skills in individuals with FXS is important and likely to improve our understanding of the factors influencing the development of daily living skills and supporting independence in this population.
Autism symptomatology.
Most males with FXS display behavioral features that are similar to those typically associated with the ASD phenotype, such as limited eye contact, restricted and repetitive behaviors (Abbeduto et al., 2014). Indeed, when using diagnostic instruments that have been designed to evaluate ASD in the general population (e.g., the Autism Diagnostic Observation Schedule, ADOS), it is estimated that 50–78% of males with FXS receive an ASD diagnosis (Abbeduto et al., 2014; Harris et al., 2008; Klusek, Martin, & Losh, 2014b). The presence and severity of ASD symptomatology in males with FXS has emerged as a potentially key factor for the development of adaptive functioning. For example, Hartley et al. (Hartley et al., 2011) found that parent report of the presence of ASD was significantly and negatively related to independence in adulthood for males with FXS 22 years of age and older. Similarly, Hustyi et al. (2015) found that higher levels of ASD severity, as measured by the Autism Diagnostic Observation Schedule (Lord et al., 2000), were associated with lower levels of independent living skills, using the Independent Living Scales (Loeb, 1996), in males and females with FXS ranging in age from 15 – 25 years, even after controlling for IQ. That said, findings reported by Smith and colleagues (2012) did not find the same pattern of results. More specifically, in a sample of males and females with FXS ages 12 years or older, a significant difference in overall adaptive functioning skills, as measured by the Revised Adaptive Daily Living Index (Seltzer & Krauss, 1989) was not found between individuals with FXS and individuals with FXS who had a comorbid ASD diagnosis. Differences across studies in the methods used to assess ASD symptomatology (i.e., categorial diagnosis vs. continuously distributed characteristics) may contribute to the differences in findings across studies (Abbeduto et al., 2014). More research is needed to clarify the extent to which ASD symptomatology contributes to daily living skills in males with FXS, particularly as they transition into adulthood and when controlling for other developmental characteristics known to be associated with ASD symptomology, such as language and nonverbal cognitive ability (Thurman, McDuffie, Kover, Hagerman, & Abbeduto, 2015).
Anxiety.
There is clear evidence that anxiety is a key feature of the FXS phenotype. Males with FXS have been reported to present with more severe anxiety symptoms, at least for certain domains of symptoms, when compared to individuals with other intellectual disability conditions (Cordeiro et al., 2011; Ezell et al., 2019; Kau, Reider, Payne, Meyer, & Freund, 2000; Thurman et al., 2014). Moreover, in males with FXS, social avoidance has been shown to be associated with increased anxiety symptoms (Thurman et al., 2014). The presence of increased anxiety can negatively impact daily functioning, by limiting one’s ability to learn from and interact with the environment (Angkustsiri et al., 2012). Indeed, significant associations have been found between overall anxiety and adaptive functioning in typically developing children and in 22.1.2 duplication syndrome, another neurodevelopmental disorder associated with increased anxiety. Despite the common occurrence of anxiety symptoms in FXS, and the potential overlap between ASD and anxiety symptomatology in youth with FXS (Hustyi et al., 2015; Roberts et al., 2018), no studies have considered the relationship between anxiety and daily living skills.
Present Study
Much remains to be understood about the profile and predictors of daily living skills in adolescents and adults with FXS. In this current cross-sectional study, we explored the daily living skills of 57 adolescent and young adult males with FXS between the ages of 15 and 23 years. The aims for the project were as follows:
To characterize the profile of daily living skills in males with FXS, focusing on the ability to perform types of skills independently. In addition, for exploratory analysis, we compared patterns of independence between the adolescent and adult participants enrolled in the project.
To examine the participant characteristics that may be predictive of independent performance of daily living skills. Specifically, the roles of FMRP, nonverbal cognition, language ability, ASD symptomatology, and anxiety symptomatology were considered.
Method
Participants
Participants for this project were drawn from a larger longitudinal study investigating language development in adolescent and young adult males with FXS or ASD. Several publications have focused on this dataset (e.g., Abbeduto et al., 2019; Matherly et al., 2017; Roberts et al., 2018), but none have focused on adaptive skills as an outcome. Participants with FXS were recruited nationally and were assessed at either the University of California Davis Health, MIND Institute or the University of South Carolina. The following inclusion criteria, based on parent report, were utilized in the larger study: (a) male ranging in age from 15 – 23 years, (b) native English speaker, (c) absence of physical or sensory impairment that would limit participation in the study, (d) speech is the primary means of communication, (e) regularly uses phrases of three-words or longer, and (g) resides with their biological mother at the time of their initial visit.
All the participants for whom Time 1 data were available on the Waisman Activities of Daily Living Scale were included in the present project. This criterion yielded a sample of 57 males with FXS, all of whom had a confirmed diagnosis of FMR1 full mutation (with or without mosaicism). Seven percent of participants in the present study identified as Hispanic/Latino. The racial composition of the sample was: 86% Caucasian, 7% African American, 3% American Indian or Alaskan Native, 2% Asian, 2% from two or more races. Participant characteristics are presented in Table 1.
Table 1.
Descriptive statistics for participant characteristics.
| Mean | SD | Range | |
|---|---|---|---|
| Chronological Age (years) f | 18.23 | 2.26 | 15.03 – 22.92 |
| Nonverbal IQ Standard Scorea | 38.86 | 4.88 | 36 – 56d |
| Nonverbal IQ Growth Scorea, f | 462.13 | 12.67 | 420 – 490 |
| Receptive Language Standard Scoreb | 55.42 | 2.33 | 55 – 71d |
| Receptive Language Number of Blocks Passedb, f | 2.71 | 2.58 | 0–12 |
| Expressive Grammar – MLU-Mf | 3.88 | 1.96 | 1.00 – 9.85 |
| ASD Symptom Severityc, f | 5.79 | 2.25 | 1–10 |
|
| |||
| Anxiety Raw Scored, f | 5.89 | 3.26 | 0–14 |
|
| |||
| Daily Living Skills Raw Score f, g | 22.39 | 4.78 | 11–33 |
|
| |||
| FMRP Mosaic Status f | Full Mutation – Mosaic: 13 participants Full Mutation – Not Mosaic: 34 participants |
||
|
| |||
| Incomeh | Under 30,000: 8 participants 30,001 – 50,000: 5 participants 50,001 – 100,000: 18 participants 100,001 and above: 25 participants |
||
|
| |||
| Biological Mom Education: (% of sample) | High school graduate/GED: 8.8% (n = 5) Some college/technical college: 22.8% (n = 13) Associate’s or technical college degree: 14% (n = 8) Bachelor’s college degree: 22.8% (n = 13) Some graduate work: 10.5 % (n = 6) Graduate degree: 21.1% (n = 12) |
||
Leiter-R Brief NVIQ;
Test for Reception of Grammar-2;
Autism Diagnostic Observation Schedule-2
Anxiety, Depression, and Mood Scale;
Note: The lowest score possible is higher on the TROG-2 (55) than it is on the Leiter-R (36).
These measures are considered in study analyses.
Waisman-Activities of Daily Living Skills.
Missing data for 1 participant.
Procedures
Caregivers provide informed consent and youth provided assent. All procedures were approved by the Institutional Review Boards at both data collection sites. Written consent from the biological mothers of participants was acquired prior to the visit. All measures were collected over the course of a two-day visit completed on consecutive days.
Measures
Daily Living Skills.
The Waisman Activities of Daily Living Scale (W-ADL; Maenner et al., 2013), a 17-item informant questionnaire, was used to assess daily living skills. Biological mothers served as informants. The W-ADL was specifically designed to measure the daily living skills in adolescents and adults with developmental disabilities. Cronbach’s alpha for total scores (0.90 – 0.94) have been shown to indicate high internal consistency across multiple measurement occasions (Maenner et al., 2013; Smith, Greenberg, & Mailick, 2012). In addition, the total score has been shown to be strongly associated with Daily living scores on the Vineland (Maenner et al., 2013). In addition, the W-ADL has been used to assess daily living skills in other samples of participants with FXS (e.g., Maenner et al., 2013; Raspa et al., 2018; Usher et al., 2020). The W-ADL considers skills pertaining to caring for self/personal daily living skills (i.e., drink from a cup, eat from a plate, dress, toilet, wash/bathe, groom), caring for home/domestic daily living skills (i.e., prepare food, make bed, set/clear table, household task, wash dish, mix/cook food, laundry, home repairs, cook complete meal), and living in the community/community daily living skills (i.e., run errands, banking). Caregivers rate the individual’s level of independence for each skill as “independent”, “does with help”, or “does not do at all”. These descriptive ratings are assigned a score of 2, 1, and 0, respectively. This measure yields a single total raw score (maximum value 34), which was utilized in analyses.
FMRP Level.
To examine the contributions of variations in the genetic mutation causing FXS, blood samples were collected at the first annual visit at which the participant was able to tolerate the blood draw (Visit 1: 22 participants, Visit 2: 15 participants, Visit 3: 3 participants, and Visit 4: 3 participants). The presence of the FMRP was then quantified using an immunoassay based on a Luminex platform that detects FMRP in dried blood spots using the procedures described in LaFauci et al. (2013). In a study of 215 individuals with normal, premutation, and full-mutation FMR1 alleles, this assay demonstrated a sensitivity and specificity approaching 100% in identifying affected (full-mutation) males and differentiated mosaic from non-mosaic males (LaFauci et al., 2013). Further validation of this technique was established in a study of the variability of FMRP expression in 2,000 fresh newborn dried blood spots (Adayev et al., 2014). Samples were processed at the New York State Institute for Basic Research in Developmental Disabilities; the laboratory staff members who processed the blood were blind to the results of all behavioral testing. Classification according to mosaic status was utilized within analyses.
Nonverbal Cognition.
The Leiter International Performance Scale – Revised (Leiter-R; Roid & Miller, 1997) is a nonverbal cognitive battery administered using pantomime and nonverbal cues. In the present study, the four subscales that comprise the Brief IQ screener were administered: Figure Ground, Form Completion, Sequential Order, and Repeated Patterns. Chronbach’s alphas for these subscales have been shown to be 0.75, 0.88, 0.75, and 0.76, respectively. One participant had missing data on the Leiter-R due to examiner error. Because 62% of the sample earned an overall NVIQ standard score at floor (36), the Leiter-R growth score, which can be found in the norming tables, was used as the metric of nonverbal cognition in analyses. Growth scores provide an equal interval metric of absolute ability that take into account item difficulty, can be used to quantify small improvements/differences in the skills, and are less prone to floor effects than standard scores in populations with significant cognitive delays (Channell, Thurman, Kover, & Abbeduto, 2014). The test manual reports that the Leiter-R brief form correlates .85 with both the full version of the Leiter-R and the WISC-III. Internal consistency reliability is between .88 and .90 depending on age, and test-retest reliability is between .88–.96.
Receptive Syntax.
The Test for Reception of Grammar, Version 2 (TROG-2; Bishop, 2003) was used to assess receptive syntax skills. The TROG-2 assesses comprehension of syntactic constructions that are marked by inflection, function words, and word order in English. The TROG-2 consists of items organized into twenty blocks of four; each block assesses a single grammatical form. Internal consistency reliability is .88. Two participants had missing data due to administration error. Because 96.5% of the sample earned a standard score at floor, total number of blocks passed was utilized as the metric of receptive syntax in analyses.
Expressive Syntax.
Expressive syntax was assessed by computing the mean length of utterance in morphemes (MLU-M) during a conversation activity designed to elicit spontaneous speech using procedures developed by Abbeduto and colleagues (Abbeduto et al., 2020). During the conversation, each participant took part in an interview-style conversation with a single examiner with a target of 10 to 12 minutes of interaction. The activity was introduced by saying that the examiner and participant would sit and talk for about 10 minutes to get to know each other a little better. Reasonable standardization was ensured across examiners and participants using a script of topics and follow-up questions and prompts. The examiner attempted to use open-ended prompts (e.g., ‘Tell me everything you did in school yesterday’) and to limit her own speech, thereby eliciting as much talk from the participant as possible. Participant speech was transcribed, segmented into C-units (communication units), and analyzed using the computer algorithm for computing MLU in the software program Systematic Analysis of Language Transcripts (SALT; Miller & Iglesias, 2008). Details of the conversational scripts, examiner prompts, transcription, segmentation, and computation of MLU-M, as well as procedures for evaluating inter-transcriber agreement, can be found in Abbeduto et al. (2020). Moreover, this measure has been shown to have strong test-retest reliability and convergent validity in individuals with FXS (Abbeduto et al., 2020).
ASD Symptom Severity.
The Autism Diagnostic Observation Schedule, Second Edition (ADOS-2; Lord et al., 2012) is a semi-structured standardized assessment of ASD symptomatology. The ADOS-2 have been found to be a reliable and valid tool and is considered the gold-standard in the field for assessing ASD symptoms (Lord et al., 2012). In the current project, participants received modules 1 (n = 4), 2 (n = 28), or 3 (n = 24). Data were missing for one participant due to examiner error. The Calibrated Comparison Score was used to quantify the severity of overall ASD-related symptoms, derived from the ADOS-2. Because many participants were older than the norming sample of the ADOS-2, we used the upper age limit for each ADOS-2 module to compute the scores included in the present analyses. Project staff who administered the ADOS-2 were graduate-level professionals who had achieved research reliability. Cross-site reliability across all examiner at both data collection sites was assessed for 10% of the administrations, using videotape review. Mean percent agreement of each examiner relative to consensus scores (achieved through group discussion) was computed and averaged 80% for the ADOS-2.
Anxiety.
The Anxiety, Depression, and Mood Scale (ADAMS; Esbensen, Rojahn, Aman, & Ruedrich, 2003) is a behavior-based 28-item informant questionnaire designed to screen for anxiety, depression, and mood disorders specifically in individuals with intellectual disability. The ADAMS has been shown to be a psychometrically sound instrument for screening anxiety among individuals with intellectual disability, with high internal consistency and test-retest (Esbensen et al., 2003). In addition, subscales from this measure have been found to be correlated with DSM-IV diagnoses in FXS and distinguish individuals with FXS from those with nonsyndromic ASD (Cordeiro et al., 2011; Thurman et al., 2014). Biological mothers of participants were asked to rate the severity of behaviors on a 4-point Likert scale, ranging from 0 (not a problem) to 3 (severe problem). Raw scores from the three anxiety-related metrics generated from this measure (i.e., General Anxiety, Social Avoidance, and Compulsive Behavior) were utilized in analyses.
Analysis Plan
Maternal ratings from the W-ADL were first used to characterize the profile of daily living skills for the adolescent and young adult males within our sample. Exploratory analyses were also conducted to characterize the profile of daily living skills separately for adolescents (CA less than 18 years) versus adults (18 years old and above). Analyses were then conducted to explore the hypothesized influence of concurrent participant characteristics (e.g., FMRP, chronological age, nonverbal cognition, receptive and expressive syntax, severity of ASD symptomatology, and anxiety) on daily living skill performance. Due to non-normal distributions, nonparametric bivariate correlations were conducted using Spearman’s rho. Follow-up descriptive analyses were also conducted to facilitate interpretation of results. Finally, a regression analysis was conducted to identify unique predictors of daily living skills along with follow-up analyses to facilitate interpretation of results.
Results
Profile of independence in daily living skills
The first aim of the project was to characterize the profile of daily living skills in males with FXS between 15 and 23 years of age. Overall, as seen in Figure 1, caregivers reported that the majority of participants were able to independently perform all items on the W-ADL pertaining to personal daily living skills. Across all the W-ADL items assessing personal daily living skills, the percent of participants reported to be able to independently perform each skill (i.e., obtained a score of 2 on each item) ranged from 59.6% - 100%. In addition, across items assessing personal daily living skills, the percent of participants requiring help (i.e., obtained a score of 1 on each item) when performing skills ranged from 10.3% for the dressing and undressing to 41.4% for grooming, brushing teeth, and combing/brushing hair. Finally, apart from grooming, there were no participants whose caregiver reported the status of the skill as “does not do at all (i.e., obtained a score of 0 on each item)”.
Figure 1.
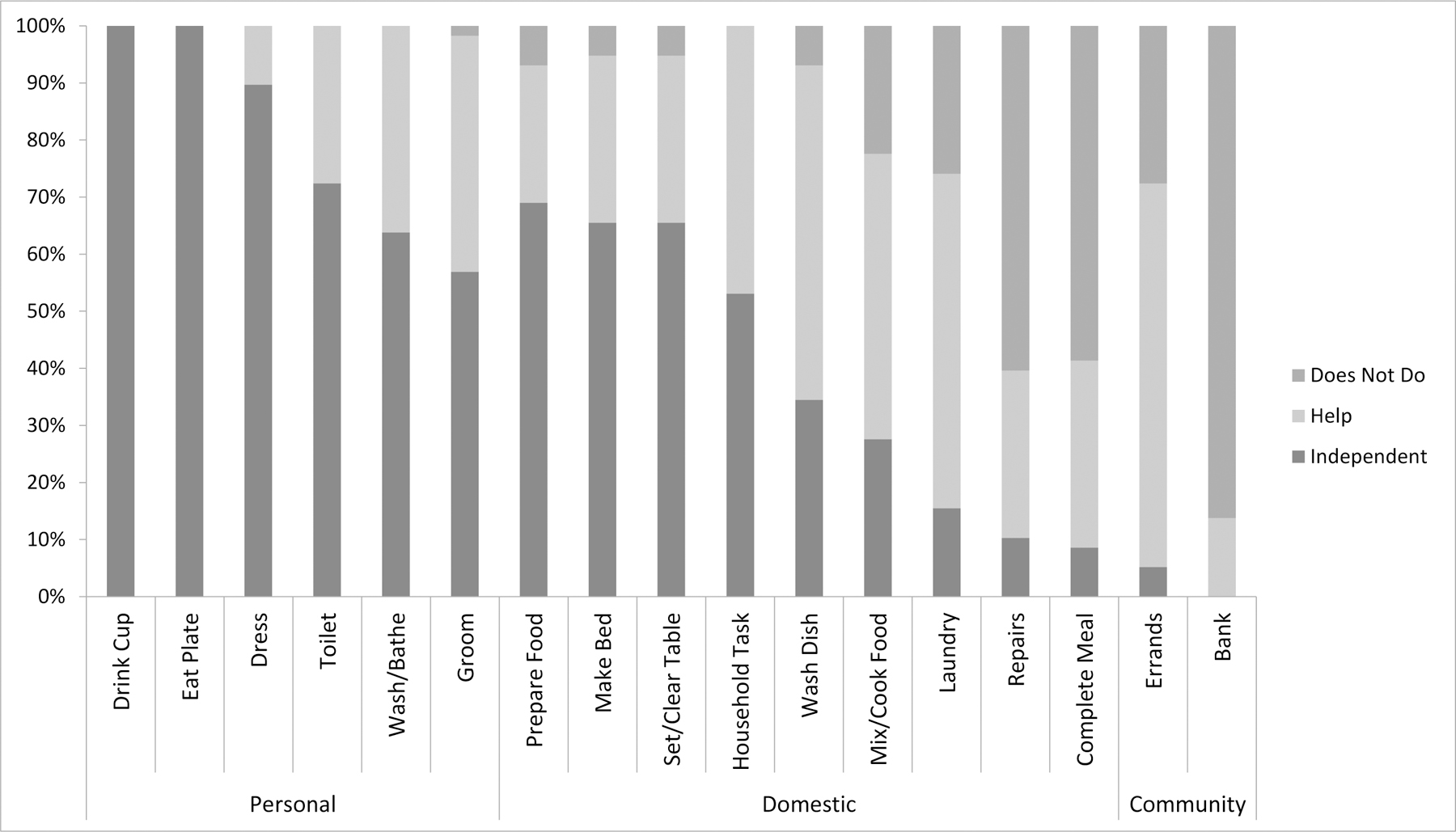
Percentage of adolescent and adult participants reported by caregivers as independently able, able with help, and not able to complete W-ADL items without assistance
With regard to items assessing domestic daily living skills, the majority of participants (>50%) were able to independently prepare simple foods (e.g., sandwiches, cold cereal), make a bed, set/clear a table, and perform simple household tasks (e.g., put things away, light housecleaning). In contrast to personal daily living skills, there were a number of items assessing domestic daily living skills for which the majority of participants were reported to need help in order to complete the task, such as washing dishes (58.6%), doing laundry (58.6%), mixing/cooking simple foods (e.g., fry eggs, heat food in microwave; 50%), and completing simple household tasks (48.8%). Finally, a majority of caregivers (>50%) reported that home repairs (e.g., changing light bulbs) and preparation of complete meals were skills the participants did not do at all.
The two items on the W-ADL that assess community daily living skills appeared to be particularly difficult for participants. Only one participant was reported as independently able to run errands; 67.2% of participants were reported to be able to run errands with help. Banking/managing daily finances (e.g., keeping track of cash, checking account, paying bills) emerged as the skill that the largest percentage of caregivers reported the adolescent or young adults with FXS as not being able to do at all; only 13.8% of participants were reported to be able bank/manage daily finances with help.
Follow up descriptive analyses focused on considering the data separately for the adolescent (n = 29, M(age) = 16.35, SD = 0.83; range = 15.03 – 17.75 years) and adult participants (n = 28, M(age) = 20.28; SD = 1.48; range = 18.05 – 22.92 years) with FXS in the sample. As seen in Figure 2, there was preliminary evidence to suggest that more adults than adolescents are able to mix/cook simple foods, do their laundry, prepare complete meals, and complete tasks for banking/management of daily finances, at least with help. For these items, the percent of participants who were described as not performing a skill at all was lower by 15% or more between the adolescents and the adults, ranging from a 15.5% decrease for preparing a complete meal to a 30.4% decrease for doing laundry. Indeed, chi-square analyses indicated significant differences between the adolescent and adult participants when considering the ability to do laundry (ᵪ2(2, 57) = 7.14, p = .03) and in the ability to complete tasks related to banking/management of daily finances (ᵪ2(1, 57) = 5.48, p = .02). These data suggest the potential for continued development of at least some daily living skills as males with FXS enter adulthood.
Figure 2.
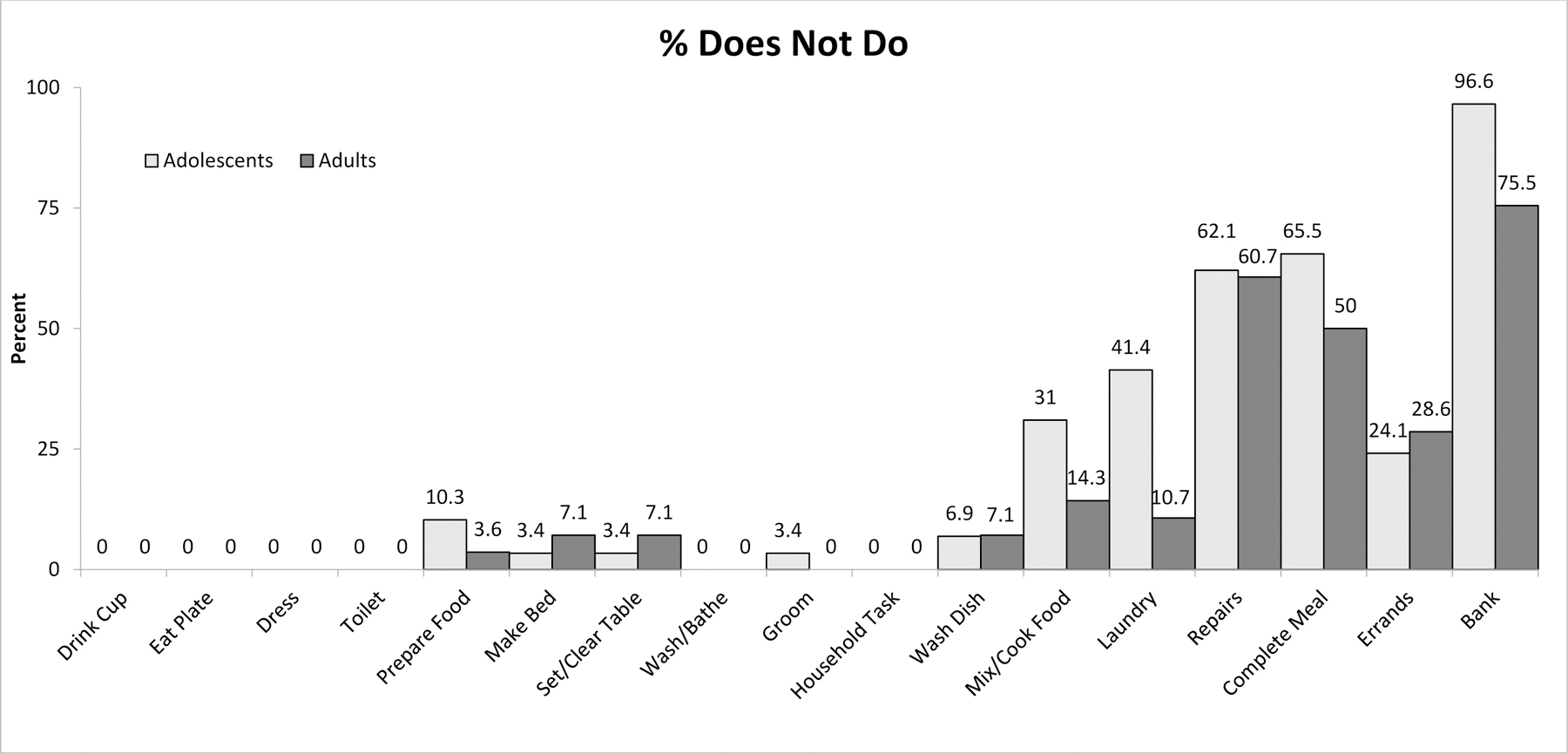
Percentage of adolescent versus adult participants reported by caregivers as not being able to complete W-ADL items without assistance.
Predictors associated with daily living skill performance
The second aim of the project was to examine individual characteristics of participants that may be predictive of independence in daily living skills. Bivariate associations between the putative predictor variables and W-ADL scores were considered first (see Table 2). Results indicated that W-ADL total scores used to measure independence in daily living skills were significantly associated with nonverbal cognition (p < .001), receptive syntax (p < .001), expressive syntax (p < .001), and ASD symptom severity (p = .003). With regard to anxiety, results indicated that none of the anxiety metrics considered (General Anxiety: p =.97; Social Avoidance: r = −.16, p =.24; Compulsive Behavior: r = −.10, p =.48) were significantly associated with W-ADL scores. Finally, the correlation between W-ADL scores and age (r = .23, p = .08) or FMRP (r = .27, p = .07) did not reach criterion for a significant association.
Table 2.
Descriptive statistics for participant characteristics.
| FMRP-Mosaic Status | CA | Nonverbal Cognition | Receptive Grammar | Expressive Grammar | ASD Severity | Anxiety | |
|---|---|---|---|---|---|---|---|
| Daily Living Skills | .27 | .23 | .64*** | .67*** | .58*** | −.39** | .005 |
| FMRP-Mosaic Status | −.02 | .19 | .27 | .31* | −.20 | .10 | |
| CA | .17 | .24 | .29* | −.05 | .19 | ||
| Nonverbal Cognition | .68*** | .65*** | −.36** | −.05 | |||
| Receptive Grammar | .77*** | −.24 | .09 | ||||
| Expressive Grammar | −.34* | .19 | |||||
| ASD Severity | .10 |
p < .05,
p < .01,
p < .001
All significant putative predictors were then entered into a regression analysis. Because of multicollinearity concerns, the receptive syntax and expressive syntax measures were not included in the same model (r = .76); instead, two separate regression models, one with receptive syntax and one with expressive syntax, were conducted. Results of the first regression model, which included nonverbal cognition, receptive syntax, and ASD symptom severity resulted in a significant model, F(3, 49) = 21.98, p < .001, with an R2adjusted value of .55. Nonverbal cognition and receptive syntax significantly contributed to this prediction; ASD symptom severity was not a significant unique contributor to this prediction (see Table 3). The second regression model, which included expressive syntax performance instead of receptive syntax performance, also resulted in a significant model, F(3, 51) = 18.89, p < .001, with an R2adjusted value of .50. Nonverbal cognition significantly contributed to this prediction and the contribution of expressive grammar and ASD symptom severity was not significant (see Table 3).
Table 3.
Linear regression analyses evaluating predictors of daily living skills.
| B (unstandardized) | SEB | β | p value | Semi-partial correlation | |
|---|---|---|---|---|---|
| Model 1 | |||||
| Nonverbal Cognitiona | .129 | .046 | .344 | .007 | .371 |
| Receptive Languageb | .730 | .227 | .393 | .002 | .418 |
| ASD Symptom Severityc | −.429 | .220 | −.203 | .057 | −.268 |
| Model 2 | |||||
| Nonverbal Cognitiona | .172 | .045 | .459 | <.001 | .470 |
| Expressive Languagee | .568 | .295 | .234 | .06 | .26 |
| ASD Symptom Severityc | −.422 | .224 | −.198 | .07 | −.254 |
Leiter-R,
TROG,
ADOS-2,
To assess the impact of the correlation between nonverbal cognition and both receptive and expressive syntax (r = .64 and r = .53, respectively), follow-up analyses were computed to fit models in which nonverbal cognition, receptive syntax, and expressive syntax were considered in separate regressions. All three variables were significantly associated with the W-ADL performance when considered individually. When examining the coefficients of the variables from these models, the coefficient for nonverbal cognition was relatively consistent across models (0.21 when alone, 0.13 when receptive syntax was included, and 0.17 when expressive syntax was included). In comparison, the coefficients for receptive syntax (1.07 when alone) and expressive syntax (1.07 when alone) were attenuated with the inclusion of nonverbal cognition (receptive syntax: 0.76 and expressive syntax 0.44).
Discussion
Daily living skills represent the “practical” self-care skills an individual learns and uses across settings (Stabel et al., 2013). Most males with FXS require support in adulthood in order to navigate academic, employment, residential, and community settings (Bailey et al., 2009). Thus, research elucidating the nature of daily living skills in adolescents and young adult males with FXS has the potential to provide insight into the ways in which the acquisition of daily living skills can be supported in this population. The present study was designed to begin to address this need by examining the profile of daily living skills in males with FXS. In addition, we considered the potential influences of nonverbal cognition, syntax skills, and ASD and anxiety symptomatology on the daily living skills of adolescent and young adult males with FXS.
Profile of independence in daily living skills
Based on caregiver-report, most of the males within our sample (CA range: 15 – 23 years) were able to independently perform all of the personal daily living skills considered, although there was variability observed across items. Moreover, it is important to recognize the basic nature of the skills in this domain assessed relative to normative expectations for typically developing adolescents and young adults. Nonetheless, sizeable proportions of our participants still needed at least some help with basic skills, such as dressing/undressing, using the toilet, washing/bathing, and grooming. Although there were differences in the measures used to assess personal daily living skills, our results appear reasonably consistent with the data presented by Bailey et al. (2009). These findings suggest a need for further research designed to enhance the impact of interventions supporting development of these basic personal skills to increase independence.
In the domain of domestic daily living skills, we observed considerable variability across skills. Specifically, there were some tasks that the majority of participants were able to do independently, including preparing simple food that does not require cooking (69%), making a bed (65.5%), setting/clearing a table (65.5%), and performing simple household tasks (55.2%). There were also a number of tasks, however, that the majority of participants were only able to do with help, such as washing dishes, mixing and cooking simple foods, and doing laundry. Home repairs and preparing a complete meal, however, were unlikely to be performed, even with help. Further research designed to better understand variability across these domestic skills can be used as guide development of young adult transition program and life skills curricula, providing specific targets for intervention to support a greater degree of independence in adulthood.
Finally, in terms of community daily living skills, our measure assessed only the ability to run errands and manage banking and finances. The majority of our participants were able to run errands with help. In contrast, few were reported to be able to manage banking/daily finances, although exploratory analyses indicated significant improvements in the ability to complete tasks relating to banking/management of finances from adolescence into adulthood. Nonetheless, the importance of being able to handle one’s financial resources to achieve optimal autonomy when living in the community indicates a need for future research designed to better understand why some young adult males with FXS develop this skill whereas others do not. Data are also needed on the nature, accessibility, and efficacy of current high school and young adult transition programs, which play a key role in helping young adult males with FXS reach their full potential for independence.
Daily living skills are often described as an area of relative strength in males with FXS. For example, when considering the different domains of adaptive functioning skills in teenage youth with FXS, multiple studies have found daily living skills scores to be higher than adaptive functioning scores in the communication domain (Dykens et al., 1993; Klaiman et al., 2014). In contrast, results from the present study suggest a more nuanced view of daily living skills. Indeed, we found specific areas of substantial weakness in daily living skills in many males with FXS, especially those more akin to the skills expected of typically developing adolescents and adults, and thus, the need to develop more effective interventions in transition programs for those areas. In particular, there is considerable variability in terms of independent performance in the areas of domestic and community daily living skills, with lower overall levels of performance relative to personal daily living skills. Therefore, programs with a greater emphasis on domestic and community daily living skills in addition to personal daily living skills may be particularly helpful in supporting enhanced long-term outcomes in this population
Predictors associated with daily living skill performance
There are a number of behavioral features associated with the FXS phenotype that are likely to play key roles in the development of daily livings skills. Thus, the second aim of the present project focused on identifying the youth characteristics predictive of daily living skills. Results from the present study supported prior research finding a positive association between nonverbal cognition and daily living skills and a negative association between ASD symptom severity and daily living skills (Bailey et al., 2009; Dykens et al., 1993; Glaser et al., 2003; Hartley et al., 2011; Hustyi et al., 2015).
We also built on previous findings by considering, for the first time, the influences of syntax skills on daily living skill performance. Significant positive associations were observed between daily living skills and both receptive and expressive syntax performance. Although the present study is the first to consider the potential relationship between syntax skills and daily living skills in FXS, the importance of language skills in adult outcomes has been demonstrated in other clinical populations. For example, language skills, particularly “meaningful” speech acquired before the age of 5 years, is considered to be the most consistent predictor of independence in adulthood for adults with ASD (Billstedt et al., 2007; Eaves & Ho, 2008; Howlin et al., 2004). Moreover, individuals with stronger language skills are able to participate more fully in both learning and social activities (Kasari & Smith, 2013; Liptak, Kennedy, & Dosa, 2011). Thus, syntax skills are an important intervention target to consider when the goal is supporting increased independence in the adult years. It is important to point out that, not only do dimensions of language continue to grow into adulthood for typically developing individuals (Bowles, Grimm, & Mcardle, 2005; Channell, Loveall, Conners, Harvey, & Abbeduto, 2018; Nippold, Ward-Lonergan, & Fanning, 2005; Williams, 2019), but also McDuffie and colleagues have shown that interventions can lead to improved language skills in youth with FXS even during the adolescent years (McDuffie et al., 2018, 2016; McDuffie, Thurman, Channell, & Abbeduto, 2017; Thurman et al., 2020). Thus, language targets, particularly syntax, may provide a useful pathway for improving daily living skills.
We considered, for the first time, the influences of anxiety on daily living skill performance in individuals with FXS. In the present study, no significant associations were observed between daily living skill performance and the anxiety metrics considered in the present study. Although this is the first study to consider the relation between anxiety symptomatology and daily living skills in FXS, research considering the relations between these domains in 22q11.22 duplication syndrome, another neurodevelopmental disorder associated with increased rates of anxiety, noted variability in the types of anxiety symptomatology relating to daily living skills. Angkustsiri et al. (2012) did not observe an association between adaptive functioning and either generalized anxiety or social phobia in their participants with 22q.11.23 duplication syndrome; although different assessment tools were used, these findings appear similar to our findings in FXS. That said, although Angkustsiri et al. (2012) observed an association between adaptive functioning and compulsive disorder for participants with 22q.11.23 duplication syndrome, in FXS we did not observe a similar association. In principle, it does seem plausible that the presence of increased anxiety can negatively impact daily functioning, by limiting one’s ability to learn from and interact with the environment. Thus, more research is needed to understand the extent to which findings from the present study translates to other metrics/types of anxiety symptomatology, developmental periods, and aspects of daily living skills.
Our data indicate that increased ASD symptom severity is associated with reduced daily living skill performance. This is consistent with the growing body of literature suggesting that ASD symptomatology in males with FXS may be a key factor in the development of adaptive functioning skills (Hartley et al., 2011; Hustyi et al., 2015). To date, however, it remains unclear what aspect(s) of ASD symptomatology may be driving this effect. For example, it is possible that the social affective difficulties associated with the ASD phenotype may pose a barrier to learning and/or following models of these skills. A deeper, more nuanced examination of individual ASD symptoms or symptom clusters is likely needed to fully understand this relationship and develop interventions to support acquisition of daily living skills (Abbeduto et al., 2014).
In our analyses, the association between age and overall level of daily living skill performance was small and did reach criterion for statistical significance. That said, it is still likely that adolescents and adults will continue to gain skills as they age, as long as opportunities for growth continue to be provided. Indeed, there were some items in the present study for which improvements were observed. For example, caregivers reported increased independence for the adults relative to adolescents in the areas of doing laundry (ᵪ2(2, 57) = 7.14, p = .03) and in the ability to manage tasks relating to managing finances/banking (ᵪ2(1, 57) = 5.48, p = .02). In addition, the association between FMRP and daily living skill performance was small and did not reach criterion for a statistical significance. The findings of previous studies on the relationship between FMRP and adaptive functioning skills in FXS has been inconsistent. One explanation for these inconsistencies is likely the samples sizes and participants represented. Indeed, because FMRP is significantly reduced in full mutation males with FXS, the amount of variability represented in a study sample is likely a key contributor to study findings. In addition, it is possible that although there is some contribution from FMRP to youth skills, the influence of this factor is indirect, operating through possibly other developmental mechanisms, such as cognitive ability. Consequently, whether an effect of FMRP is observed is likely to depend on the participants included in the study sample as well as the other domains of cognitive and behavioral functioning assessed.
Finally, when considering the influences of all significant putative predictors together, we were able to predict approximately half the variance observed in the daily living skills in the participant sample. Moreover, receptive syntax and ASD symptom severity emerged as the strongest individual predictors of daily living skill performance. Prior research has demonstrated significant positive interactions between ASD symptom severity and both nonverbal cognition and syntax performance. Importantly, by including these different factors in the same model we are able to demonstrate ASD symptomatology also independently contributes to daily living skill performance, replicating prior reports (Hustyi et al., 2015). It is also notable that, when nonverbal cognition and expressive syntax were entered into the same model, nonverbal cognition emerged as a significant unique predictor of daily living skill performance, but expressive syntax did not. Nonverbal cognition, receptive syntax, and expressive syntax are often highly correlated in individuals with neurodevelopmental disorders, making it difficult to disentangle the unique contributions of each of these constructs. Within the present study, the effect of receptive syntax on daily living skills was not as attenuated by the inclusion of nonverbal cognition as was the effect of expressive syntax. Nonetheless, during this developmental period, programs that simultaneously target cognition and syntactic language (in either the receptive or expressive modality), as well as specific daily living skills, are needed to enhance independence and improve quality of life for individuals with FXS.
Limitations
There are limitations associated with the present study. First, although the sample size is consistent with and adds to the findings of most other studies within in the literature focused on FXS, the sample size is relatively small. Moreover, recruitment was limited to only those males who have some phrase speech and the ability to travel to the testing sites, which limits the generalizability of the findings. Second, we have included only males in the present study, due to the increased prevalence of FXS in males and the fact that FXS is an X-linked disorder, affecting girls differently than boys. It is vital that these research questions be investigated in females with FXS. Third, the present study utilized a cross-sectional approach to examine age differences in daily living skills. Longitudinal examinations of the factors influencing daily living skills in males with FXS as they transition into adulthood are needed. Fourth, the factors considered in the present study accounted for approximately half of the variance in daily living skills. More research is needed to identify additional factors that influence the daily living skill development of youth with FXS. Fifth, in the present study, we did not collect data regarding the extent to which caregivers provide youth with FXS opportunities to learn the daily living skills assessed in the present study. In addition, we do not have specific information regarding the educational/vocational or social opportunities of these participants. The collection of this information in future studies would be a contribution to the field. Finally, although caregiver-report measures, like those used in the present study, are commonly used in studies of males with FXS even into adulthood due to the level of cognitive impairment associated with FXS, self-report or objective measures would be helpful for a fuller understanding these skills in individuals with FXS.
Conclusion
Data from the present study suggest that although male youth with FXS between 15 and 23 years of age are able to perform a number of daily living skills independently, there are indeed skill for which further research is needed to better inform intervention and long-term outcomes. In particular, males with FXS appear to need more support to complete domestic and community daily living skills during this developmental period. Thus, supporting further development and accessibility of programs targeting domestic and community daily living skills are likely to help support long-term outcomes in this population. In addition, by considering the influences of nonverbal cognition, syntax, anxiety (which was posited to instead be an effect of constructs closer to self-determination/mastery), and ASD symptom severity, we were able to account for approximately half of the variance in daily living skills. These data suggest that there are multiple determinants of, and thus multiple pathways for intervening with, daily living skills in youth with FXS.
Acknowledgements:
This research was supported by grants R01HD024356 and U54 HD079125 from the National Institute of Child Health and Human Development, and UL1TR000002 from the National Center for Advancing Translational Sciences. The authors thank the participants and their families for their participation in this study. The authors also thank the many research staff involved in the project, but especially the project coordinators, testers, and transcribers involved in the project. Preliminary data from this project was presented at the National Fragile X Foundation International Fragile X Conference in 2016.
References
- Abbeduto L, Berry-Kravis EM, Sterling AM, Sherman S, Edgin JO, McDuffie AS, … Thurman AJ (2020). Expressive language sampling as a source of outcome measures for treatment studies in fragile X syndrome: Feasibility, practice effects, test-retest reliability, and construct validity. Journal of Neurodevelopmental Disorders, 12(1), 10. 10.1186/s11689-020-09313-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbeduto L, McDuffie AS, & Thurman AJ (2014). The fragile X syndrome-autism comorbidity: what do we really know? Frontiers in Genetics, 5. 10.3389/fgene.2014.00355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbeduto L, McDuffie AS, Thurman AJ, & Kover ST (2016). Language development in individuals With intellectual and developmental disabilities: From phenotypes to treatments. In International Review of Research in Developmental Disabilities (Vol. 50). 10.1016/bs.irrdd.2016.05.006 [DOI] [Google Scholar]
- Abbeduto L, Thurman AJ, McDuffie A, Klusek J, Feigles RJ Brown WT, Harvey DJ, Adayev T, LaFauci G, Dobkins C, & Roberts J. (2019). ASD Comorbidity in fragile X syndrome: Symptom profile and predictors of symptom severity in adolescent and young adult males. Journal of Autism and Developmental Disorders, 49, 960–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Association on Intellectual and Developmental Disabilities. (2021). Intellectual disability: definition, classification, and systems of supports, 12th Edition. American Association on Intellectual and Developmental Disabilities. [DOI] [PubMed] [Google Scholar]
- Angkustsiri K, Leckliter I, Tartaglia N, Beaton EA, Enriquez J, & Simon TJ (2012). An examination of the relationship of anxiety and intelligence to adaptive functioning in children with chromosome 22q11.2 deletion syndrome. Journal of Developmental and Behavioral Pediatricsehavioral Pediatrics, 33(9), 713–720. 10.1097/DBP.0b013e318272dd24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey DB, Raspa M, Holiday D, Bishop E, & Olmsted M. (2009). Functional skills of individuals with fragile X syndrome: A lifespan cross-sectional analysis. American Journal on Intellectual and Developmental Disabilities, 114(4), 289–303. 10.1352/1944-7558-114.4.289-303 [DOI] [PubMed] [Google Scholar]
- Bassell GJ, & Warren ST (2008). Fragile X Syndrome: Loss of Local mRNA Regulation Alters Synaptic Development and Function. Neuron, 60(2), 201–214. 10.1016/j.neuron.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billstedt E, Carina Gillberg I, & Gillberg C. (2007). Autism in adults: symptom patterns and early childhood predictors. Use of the DISCO in a community sample followed from childhood. Journal of Child Psychology and Psychiatry, 48(11), 1102–1110. 10.1111/j.1469-7610.2007.01774.x [DOI] [PubMed] [Google Scholar]
- Bishop DVM (2003). Test for Reception of Grammar: TROG-2 Version 2. London: Psychological Corporation. [Google Scholar]
- Blacher J. (2001). Transition to Adulthood: Mental Retardation, Families, and Culture. American Journal on Mental Retardation, 106(2), 173–188. [DOI] [PubMed] [Google Scholar]
- Bowles RP, Grimm KJ, & Mcardle JJ (2005). A structural factor analysis of vocabulary knowledge and relations to age. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60(5), 234–241. Retrieved from 10.1093/geronb/60.5.P234 [DOI] [PubMed] [Google Scholar]
- Caravella KE, & Roberts JE (2017). Adaptive skill trajectories in infants with fragile X syndrome contrasted to typical controls and infants at high risk for autism. Research in Autism Spectrum Disorders, 40, 1–12. 10.1016/j.rasd.2017.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Channell MM, Loveall SJ, Conners FA, Harvey DJ, & Abbeduto L. (2018). Narrative language sampling in typical development: Implications for clinical trials. American Journal of Speech-Language Pathology, 27(1), 123–135. 10.1044/2017_AJSLP-17-0046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Channell MM, Thurman AJ, Kover ST, & Abbeduto L. (2014). Patterns of change in nonverbal cognition in adolescents with Down syndrome. Research in Developmental Disabilities, 35(11). 10.1016/j.ridd.2014.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen IL, Nolin SL, Sudhalter V, Ding XH, Dobkin CS, & Brown WT (1996). Mosaicism for the FMR1 gene influences adaptive skills development in fragile X-affected males. American Journal of Medical Genetics, 64(2), 365–369. [DOI] [PubMed] [Google Scholar]
- Cordeiro L, Ballinger E, Hagerman R, & Hessl D. (2011). Clinical assessment of DSM-IV anxiety disorders in fragile X syndrome: prevalence and characterization. Journal of Neurodevelopmental Disorders, 3(1), 57–67. 10.1007/s11689-010-9067-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornish KM, Cole V, Longhi E, Karmiloff-Smith A, & Scerif G. (2012). Does attention constrain developmental trajectories in fragile X syndrome? A 3-year prospective longitudinal study. American Journal on Intellectual and Developmental Disabilities, 117(2), 103–120. 10.1352/1944-7558-117.2.103 [DOI] [PubMed] [Google Scholar]
- Dykens EM, Hodapp RM, Ort SI, & Leckman JF (1993). Trajectory of adaptive behavior in males with fragile X syndrome. Journal of Autism and Developmental Disorders, 23(1), 135–145. 10.1007/BF01066423 [DOI] [PubMed] [Google Scholar]
- Dykens EM, Ort SI, Cohen I, Finucane B, Spiridigliozzi GA, Lachiewicz A, … O’Connor R. (1996). Trajectories and profiles of adaptive behavior in males with fragile X syndrome: Multicenter studies. Journal of Autism and Developmental Disorders, 26(3), 287–301. 10.1007/BF02172475 [DOI] [PubMed] [Google Scholar]
- Eaves LC, & Ho HH (2008). Young adult outcome of autism spectrum disorders. Journal of Autism and Developmental Disorders, 38(4), 739–747. 10.1007/s10803-007-0441-x [DOI] [PubMed] [Google Scholar]
- Esbensen AJ, Rojahn J, Aman MG, & Ruedrich S. (2003, December). Reliability and validity of an assessment instrument for Anxiety, Depression, and Mood among individuals with mental retardation. Journal of Autism and Developmental Disorders, Vol. 33, pp. 617–629. 10.1023/B:JADD.0000005999.27178.55 [DOI] [PubMed] [Google Scholar]
- Ezell J, Hogan A, Fairchild A, Hills K, Klusek J, Abbeduto L, & Roberts J. (2019). Prevalence and Predictors of Anxiety Disorders in Adolescent and Adult Males with Autism Spectrum Disorder and Fragile X Syndrome. Journal of Autism and Developmental Disorders, 49(3), 1131–1141. 10.1007/s10803-018-3804-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisch GS, Carpenter NJ, Holden JJA, Simensen R, Howard-Peebles PN, Maddalena A, … Nance W. (1999). Longitudinal assessment of adaptive and maladaptive behaviors in fragile X males: Growth, development, and profiles. American Journal of Medical Genetics, 83(4), 257–263. [DOI] [PubMed] [Google Scholar]
- Glaser B, Hessl D, Dyer-Friedman J, Johnston C, Wisbeck J, Taylor A, & Reiss A. (2003). Biological and environmental contributions to adaptive behavior in fragile X syndrome. American Journal of Medical Genetics, 117A(1), 21–29. 10.1002/ajmg.a.10549 [DOI] [PubMed] [Google Scholar]
- Gottfredson LS (1997). Mainstream science on intelligence: An editorial with 52 signatories, history, 27 and bibliography. Intelligence, 24(1), 13–23. 10.1016/s0160-2896(97)90011-8 [DOI] [Google Scholar]
- Grefer M, Flory K, Cornish KM, Hatton DD, & Roberts J. (2016). The emergence and stability of attention deficit hyperactivity disorder in boys with fragile X syndrome. Journal of Intellectual Disability Research, 60(2), 167–178. 10.1111/jir.12226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn LJ, Brady NC, Warren SF, & Fleming KK (2015). Do children with fragile X syndrome show declines or plateaus in adaptive behavior? American Journal on Intellectual and Developmental Disabilities, 120(5), 412–432. 10.1352/1944-7558-120.5.412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris SW, Hessl D, Goodlin-Jones B, Ferranti J, Bacalman S, Barbato I, … Hagerman RJ (2008). Autism profiles of males with fragile X syndrome. American Journal on Mental Retardation, 113(6), 427–438. 10.1352/2008.113:427-438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley SL, Seltzer MM, Raspa M, Olmstead M, Bishop E, & Bailey DB (2011). Exploring the adult life of men and women with fragile X syndrome: Results from a national survey. American Journal on Intellectual and Developmental Disabilities, Vol. 116, pp. 16–35. 10.1352/1944-7558-116.1.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hessl D, Nguyen DV, Green C, Chavez A, Tassone F, Hagerman RJ, … Hall S. (2009). A solution to limitations of cognitive testing in children with intellectual disabilities: The case of fragile X syndrome. Journal of Neurodevelopmental Disorders, 1(1), 33–45. 10.1007/s11689-008-9001-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper SR, Hatton DD, Sideris J, Sullivan KM, Hammer J, Schaaf J, … Bailey DB (2008). Executive functions in young males with fragile X syndrome in comparison to mental age-matched controls: Baseline findings from a longitudinal study. Neuropsychology, 22(1), 36–47. 10.1037/0894-4105.22.1.36 [DOI] [PubMed] [Google Scholar]
- Howlin P, Goode S, Hutton J, & Rutter M. (2004). Adult outcome for children with autism. Journal of Child Psychology and Psychiatry, 45(2), 212–229. 10.1111/j.1469-7610.2004.00215.x [DOI] [PubMed] [Google Scholar]
- Hunter J, Rivero-Arias O, Angelov A, Kim E, Fotheringham I, & Leal J. (2014). Epidemiology of fragile X syndrome: A systematic review and meta-analysis. American Journal of Medical Genetics, Part A, 164(7), 1648–1658. 10.1002/ajmg.a.36511 [DOI] [PubMed] [Google Scholar]
- Hustyi KM, Hall SS, Quintin EM, Chromik LC, Lightbody AA, & Reiss AL (2015). The Relationship Between Autistic Symptomatology and Independent Living Skills in Adolescents and Young Adults with Fragile X Syndrome. Journal of Autism and Developmental Disorders, 45(6), 1836–1844. 10.1007/s10803-014-2342-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Järbrink K, McCrone P, Fombonne E, Zandén H, & Knapp M. (2007). Cost-impact of young adults with high-functioning autistic spectrum disorder. Research in Developmental Disabilities, 28(1), 94–104. 10.1016/j.ridd.2005.11.002 [DOI] [PubMed] [Google Scholar]
- Kasari C, & Smith T. (2013). Interventions in schools for children with autism spectrum disorder: methods and recommendations. Autism: The International Journal of Research and Practice, 17(3), 254–267. 10.1177/1362361312470496 [DOI] [PubMed] [Google Scholar]
- Kau ASM, Reider EE, Payne L, Meyer WA, & Freund L. (2000). Early behavior signs of psychiatric phenotypes in fragile X syndrome. American Journal on Mental Retardation, 105(4), 286–299. [DOI] [PubMed] [Google Scholar]
- Klaiman C, Quintin EM, Jo B, Lightbody AA, Hazlett HC, Piven J, … Reiss AL (2014). Longitudinal profiles of adaptive behavior in fragile X syndrome. Pediatrics, 134(2), 315–324. 10.1542/peds.2013-3990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Martin GE, & Losh M. (2014a). Consistency between research and clinical diagnoses of autism among boys and girls with fragile X syndrome. Journal of Intellectual Disability Research, 58(10), 940–952. 10.1111/jir.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Martin GE, & Losh M. (2014b). Consistency between research and clinical diagnoses of autism among boys and girls with fragile X syndrome. Journal of Intellectual Disability Research, 58(10), 940–952. 10.1111/jir.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Roberts JE, & Losh M. (2015). Cardiac autonomic regulation in autism and fragile X syndrome: A review NIH Public Access. Psychol Bull, 141(1), 141–175. 10.1037/a0038237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaFauci G, Adayev T, Kascsak R, Kascsak R, Nolin S, Mehta P, … Dobkin C. (2013). Fragile X screening by quantification of FMRP in dried blood spots by a luminex immunoassay. Journal of Molecular Diagnostics, 15(4), 508–517. 10.1016/j.jmoldx.2013.02.006 [DOI] [PubMed] [Google Scholar]
- Liptak GS, Kennedy JA, & Dosa NP (2011). Social participation in a nationally representative sample of older youth and young adults with autism. Journal of Developmental & Behavioral Pediatrics, 32(4), 277–283. 10.1097/DBP.0b013e31820b49fc [DOI] [PubMed] [Google Scholar]
- Loeb PA (1996). Independent living scales manual. San Antonio, TX. [Google Scholar]
- Lord C, & Bailey A. (2002). Autism spectrum disorders. In Child and Adolescent Psychiatry (pp. 664–681). Oxford: Blackwell Scientific. [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, Dilavore PC, … Rutter M. (2000). The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. 10.1023/A:1005592401947 [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S, Gotham K, & Bishop SL (2012). Autism Diagnostic Observation Schedule-Second edition (ADOS-2). [Google Scholar]
- Maenner MJ, Smith LE, Hong J, Makuch R, Greenberg JS, & Mailick MR (2013). Evaluation of an activities of daily living scale for adolescents and adults with developmental disabilities. Disability and Health Journal, 6(1), 8–17. 10.1016/j.dhjo.2012.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matherly SM, Klusek J, Thurman AJ, McDuffie A, Abbeduto L, & Roberts JE (2018). Cortisol profiles differentiated in young adult males with fragile X syndrome versus autism spectrum disorder. Developmental Psychobiology, 60, 78–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDuffie AS, Banasik A, Bullard L, Nelson S, Feigles RT, Hagerman R, & Abbeduto L. (2018). Distance delivery of a spoken language intervention for school-aged and adolescent boys with fragile X syndrome. Developmental Neurorehabilitation, 21(1), 48–63. 10.1080/17518423.2017.1369189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDuffie AS, Machalicek W, Bullard L, Nelson S, Mello M, Tempero-Feigles R, … Abbeduto L. (2016). A spoken-language intervention for school-aged boys with fragile X syndrome. American Journal on Intellectual and Developmental Disabilities, 121(3), 236–265. 10.1352/1944-7558-121.3.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDuffie AS, Thurman AJ, Channell MM, & Abbeduto L. (2017). Language disorders in children with intellectual disability of genetic origin. In Handbook of Child Language Disorders: 2nd Edition. 10.4324/9781315283531 [DOI] [Google Scholar]
- Miller J, & Iglesias A. (2008). Systematic Analysis of Language Transcripts (SALT), 2012 [Computer Software]. Middleton, WI: SALT Software, LLC. [Google Scholar]
- Nippold MA, Ward-Lonergan JM, & Fanning JL (2005). Persuasive writing in children, adolescents, and adults. Language, Speech, and Hearing Services in Schools. 10.1044/0161-1461(2005/012) [DOI] [PubMed]
- Ornstein PA, Schaaf JM, Hooper SR, Hatton DD, Mirrett P, & Bailey DB (2008). Memory skills of boys with fragile X syndrome. American Journal on Mental Retardation, 113(6), 453–465. 10.1352/2008.113:453-465 [DOI] [PubMed] [Google Scholar]
- Raspa M, Franco V, Bishop E, Wheeler AC, Wylie A, & Bailey DB (2018). A comparison of functional academic and daily living skills in males with fragile X syndrome with and without autism. Research in Developmental Disabilities, 78, 1–14. 10.1016/J.RIDD.2018.04.024 [DOI] [PubMed] [Google Scholar]
- Roberts JE, Ezell JE, Fairchild AJ, Klusek J, Thurman AJ, McDuffie AS, & Abbeduto L. (2018). Biobehavioral composite of social aspects of anxiety in young adults with fragile X syndrome contrasted to autism spectrum disorder. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 177(7), 665–675. 10.1002/ajmg.b.32674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roid G, & Miller L. (1997). Leiter International Performance Scale—Revised. Wood Dale: Stoelting. [Google Scholar]
- Seltzer MM, & Krauss MW (1989). Aging parents with adult mentally retarded children: family risk factors and sources of support. American Journal of Mental Retardation, 94(3), 303–312. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2803748 [PubMed] [Google Scholar]
- Shaffer RC, Schmitt L, John Thurman A, Abbeduto L, Hong M, Pedapati E, … Erickson CA (2020). The relationship between Expressive Language Sampling and clinical measures in fragile X syndrome and typical development. Brain Sciences, 10(2), 66. 10.3390/brainsci10020066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Barker ET, Seltzer MM, Abbeduto L, & Greenberg JS (2012). Behavioral phenotype of fragile X syndrome in adolescence and adulthood. American Journal on Intellectual and Developmental Disabilities, 117(1), 1–17. 10.1352/1944-7558-117.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Greenberg JS, & Mailick MR (2012). Adults with Autism: Outcomes, Family Effects, and the Multi-Family Group Psychoeducation Model. Current Psychiatry Reports2, 14, 732–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow SS, Balla DA, & Cicchetti D. (1984). Vineland Adaptive Behavior Scales. Circle Pines, MN: American Guidance Service. [Google Scholar]
- Sparrow SS, Cicchetti D, & Balla DA (2012). Vineland Adaptive Behavior Scales, Second Edition. American Psychological Association. [Google Scholar]
- Stabel A, Kroeger-Geoppinger K, McCullagh J, Weiss D, McCullagh J, Schneider N, … Califano C. (2013). Daily Living Skills. In Encyclopedia of Autism Spectrum Disorders (pp. 839–840). 10.1007/978-1-4419-1698-3_1417 [DOI] [Google Scholar]
- Tassé MJ (2017). Adaptive Behavior. In Handbook of Positive Psychology in Intellectual and Developmental Disabilities (pp. 201–215). 10.1007/978-3-319-59066-0_14 [DOI] [Google Scholar]
- Thurman AJ, McDuffie AS, Hagerman R, & Abbeduto L. (2014). Psychiatric symptoms in boys with fragile X syndrome: A comparison with nonsyndromic autism spectrum disorder. Research in Developmental Disabilities, 35(5). 10.1016/j.ridd.2014.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurman AJ, McDuffie AS, Kover ST, Hagerman RJ, & Abbeduto L. (2015). Autism symptomatology in noys with fragile X syndrome: A cross-sectional developmental trajectories comparison with nonsyndromic autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(9). 10.1007/s10803-015-2443-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurman AJ, Potter LA, Kim K, Tassone F, Banasik A, Potter SN, … Abbeduto L. (2020). Controlled trial of lovastatin combined with an open-label treatment of a parent-implemented language intervention in youth with fragile X syndrome. Journal of Neurodevelopmental Disorders, 12(1), 12. 10.1186/s11689-020-09315-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher LV, DaWalt LS, Hong J, Greenberg JS, & Mailick MR (2020). Trajectories of Change in the Behavioral and Health Phenotype of Adolescents and Adults with Fragile X Syndrome and Intellectual Disability: Longitudinal Trends Over a Decade. Journal of Autism and Developmental Disorders, 1–14. 10.1007/s10803-020-04367-w [DOI] [PMC free article] [PubMed]
- Williams KT (2019). Expressive Vocabulary Test- Third Addition. Minneapolis, MN: NCS Pearson. [Google Scholar]


