Abstract
Objective:
To describe characteristics of strangulation, and associated medical care, documentation, and injuries of women after non-fatal intimate partner strangulation (NF-IPS) who present for care to a community-based ED with an associated IPV advocacy program between 2008 and 2016.
Setting, Design, and Participants:
A retrospective review of 345 female ED patients’ medical records who sought care at a community hospital ED following a physical assault including strangulation by an intimate partner was conducted. Demographics, characteristics related to reported signs and symptoms, injuries, and subsequent imaging, diagnoses and discharge information were abstracted.
Results:
Commonly reported symptoms were neck pain (67.2%) and headache (45.8%), with fewer patients reporting more severe symptoms such as loss of consciousness (22.6%), dysphagia (25.0%), or dysphonia (26.7%). Rates of patients disclosing strangulation to the entire multidisciplinary team and dedicated neck imaging appeared to improve between 2008 and 2014. Among the 45 patients with noted head and neck findings, two patients were found to have an internal carotid artery dissection, two patients were found to have strokes, and one patient was found to have an intracranial hemorrhage.
Conclusions:
Survivors of NF-IPS may present to community-based hospitals, and existing imaging guidelines can support clinicians in identifying serious internal injury like carotid artery dissection and stroke. Further research is needed to better discern symptoms previously attributed to psychological trauma from post-strangulation brain injury. This study contributes to the growing literature on NF-IPS with data specific to community-based ED visits.
Keywords: strangulation, intimate partner violence, domestic violence, emergency department, diagnostic imaging, advocacy
Background
Non-fatal strangulation by a current or former intimate partner (NF-IPS) continues to gain recognition as a serious public health issue.1–3 Defined as pressure applied to a person’s neck that occludes blood vessels and/or the airway,4 strangulation is a pervasive mechanism of intimate partner violence (IPV). Although nearly 11 million U.S. women report experiencing NF-IPS in their lifetime,5 brain and head trauma research in this population still lags other primarily male groups like athletes and military personnel.6
Injury can result from direct neck trauma, neck hyper-extension or brain hypoxia/anoxia,7 in addition to inertial or traumatic assaults to the head during the altercation. Serious acute and long-term health risks for those surviving strangulation include cervical artery dissection, stroke, anoxic brain injury, and post-traumatic stress disorder.2,8 Assaults may occur in rapid succession before the brain has had time to heal and resulting central nervous symptoms may be attributed solely to psychological trauma.9 Multiple strangulations have been associated with increased reports of physical and psychological symptoms.10–11 Those surviving strangulation by a partner are at grave risk of future homicide.12–13
Health care clinicians face various challenges in recognizing and assessing NF-IPS, due in part to limited literature on characteristics of those presenting for care. Some survivors may be reluctant to disclose strangulation out of fear or shame; some may have difficulty remembering the event secondary to hypoxic insult or other brain injury, psychological trauma, or both; and external injuries may be difficult to visualize or absent. The limited existing literature leave a substantial gap regarding knowledge among community-based hospitals.1 Tools to support clinicians’ efforts are emerging, such as guidelines to identify and evaluate patients after strangulation.14–15 Interdisciplinary collaborations can also prove instrumental in advancing NF-IPS awareness and furthering use of these clinical tools. As practices begin to adopt these aids, it is important to share resultant data, strengthening the scientific knowledge base on post-strangulation care as well and informing future clinical guideline iterations. The purpose of this study is to describe characteristics of strangulation events, and associated medical care, documentation, and injuries of women after NF-IPS who present for care to a community-based ED with an associated IPV advocacy program between 2008 and 2016. We hypothesized that the quality initiatives implemented during this time period would improve the use of dedicated neck imaging and documentation of strangulation by the entire team.
Methods
Study Design, Setting, and Context
This study was conducted at a 250-bed community hospital near Baltimore, Maryland. Although the hospital does not provide trauma or obstetrics/newborn services, its busy ED serves 60,000 patients annually. As of 2004, nursing staff throughout the hospital screen patients for IPV and contact the in-house domestic violence program (“DOVE”) at any time for confirmed or possible cases. The hospital-employed advocates meet with the patient in-person to provide crisis counseling, risk assessment, safety planning, legal resource information, medical record documentation and photographing of injuries. Information that may impact medical care is shared with medical staff. DOVE follows up with patients post discharge, offering short-term emergency sheltering, advocacy, case management and counseling, court accompaniment, and referral to other local services including medical care.
Prior to 2008, advocates were often the first to become aware of strangulation, as they spent more time with the patient discussing details of their assault. Advocates realized there were times when other injuries caused more pain (e.g., facial fractures), and the patient frequently did not mention strangulation when briefly summarizing the assault. Advocates also noticed that physicians might briefly examine a patient’s neck and ask directed history questions but did not regularly order imaging to evaluate strangulation when it was disclosed. Patients sometimes contacted advocates days later complaining of headaches, problems swallowing or other symptoms, and were advised to return to the ED.
As DOVE’s awareness of strangulation’s lethality risk and medical implications increased, the program sought to improve response. DOVE received exempt status from the LifeBridge Health Institutional Review Board in 2008 as part of a quality improvement process and began tracking information on the presentation, assessment, and treatment of NF-IPS patients in this particular setting.
Important Events in the DOVE Program during the Study Timeline
Beginning in 2008, DOVE partnered with an ED nurse champion to improve knowledge of strangulation and IPV among the ED team. Training began in 2009, including DOVE program content in new employee orientation, annual hospital-wide unit meeting updates and outreach to fire, police, and emergency medical services regularly interfacing with ED staff. Training content focused on existing practice literature, patient presentation, signs and symptoms, potential serious medical outcomes, and radiological assessment. The multidisciplinary team also developed and implemented a strangulation assessment and management protocol for ED physicians/nurse practitioners/physician assistants (“prescribers”). The protocol included key factors for history-taking, physical examination and documentation, and involved more detailed guidelines for imaging, referral to otolaryngology, and hospital admission. Dedicated neck imaging was recommended for any patient reporting strangulation and any of the following symptoms: neck pain, loss of consciousness, dysphagia, dysphonia, or loss of bowel or bladder control. This organization-specific internal protocol, developed based on best available evidence and expert input, was updated to reflect national recommendations published in 2016.14 From 2013 to 2014, a part-time registered nurse (RN) was made available through grant funds to complete strangulation-related medical record reviews and provide near-real-time feedback to ED staff. While an RN remained on staff with the program after 2014, their responsibilities changed due to shifts in funding and practice priorities and less time was spent providing real-time feedback.
Study Participants
ED visit documentation was reviewed from 2008 to 2016 for all patients who disclosed NF-IPS to any of the following: DOVE advocate, ED prescriber, or ED RN. Patients were included if they were evaluated in the study site’s hospital ED, referred to DOVE for crisis intervention after a physical assault by an intimate partner, and documented by either an ED prescriber, ED RN, or DOVE advocate as having experienced strangulation as a part of the assault.
Data Collection
Information from patients’ medical records were reviewed, including progress notes by advocates, RNs, prescribers, and consultants, as well as diagnostic testing and imaging results. These were abstracted and compiled into a de-identified spreadsheet. A total of 31 variables to collect were determined a priori based on existing literature. These included patient and assailant demographics (e.g., race, gender), aspects of the strangulation assault (e.g., manual vs. ligature), signs and symptoms reported or noted during examination (e.g., dysphagia), injuries identified (e.g., hyoid fracture), medical decision-making (e.g., imaging tests), and patient disposition characteristics (e.g., admission status, final diagnosis). Any available photographs as part of the medical record were reviewed by two study team members during data abstraction for visible injuries. Specific medical follow-up information was not available in ED records and was not abstracted for this study.
Abstraction was completed by DOVE members with access to the medical and advocacy records as part of their routine job duties. Further coding for analysis was determined and applied by the study team during data review.
Analysis
Descriptive data analysis was performed using Microsoft Excel and SPSS Version 27.16 To examine longitudinal changes in strangulation identification and imaging evaluation, we used a Cochran-Armitage test of trends.17 Due both to a descriptive review of data and changes in implementation events as described above, we tested the trend from 2008 to 2014 and separately from 2014 to 2016. Two outcomes were examined over time, the proportion of patients whose strangulation was documented by the entire multidisciplinary team (i.e., advocate, RN, prescriber), and the proportion of patients who received dedicated neck imaging. This imaging is defined in the ED protocol as: computed tomography (CT) with intravenous (IV) contrast, CT angiogram (CTA) or carotid ultrasound. Although an acceptable neck imaging modality, magnetic resonance imaging [MRI] was not included in the protocol as it was not readily available in the study ED. As the primary aim of data collection and analyses were quality improvement, no a priori or post hoc power calculations were completed, and results must be interpreted within the appropriate limitations.18
Results
Patient, Strangulation Event, and Presentation for Care Characteristics
A total of 2,407 patients were referred to and evaluated by the DOVE program from 2008–2016. Patients were excluded from this analysis if there was no documentation of an acute physical assault (n=1,114) or strangulation (n=902). We excluded 46 additional individuals because they either reported assault perpetrated by someone other than an intimate partner (e.g., other family members, strangers) or were not evaluated in and referred from the ED. Due to their small proportion in the sample, we excluded six male patients.
A total of 345 women were included in this study. Patients’ racial and ethnic categories as documented in their medical records are shown in Table 1. These percentages are consistent with the racial and ethnic composition of all hospital referrals to this DOVE program and the surrounding ZIP Codes. The average patient age was 32 years (range: 15–77 years). Most patients reported strangulation occurred less than four days prior to their ED visit and the majority had police involvement (Table 1). Documentation reflected most assailants were male (97.4%) and the strangulation occurred in the setting of an active, cis-gender relationship. Of note, 30 patients were pregnant at the time of their ED visit (Table 1).
Table 1:
Patient and Strangulation Characteristics
| n | % | |
|---|---|---|
| Age Range | ||
| Under 18 | 6 | 1.7 |
| 18–24 | 91 | 26.4 |
| 25–39 | 168 | 48.7 |
| 40–59 | 75 | 21.7 |
| 60+ | 5 | 1.4 |
| Race/Ethnicity | ||
| African American | 265 | 76.8 |
| Caucasian | 62 | 18.0 |
| Hispanic | 13 | 3.8 |
| Other | 5 | 1.4 |
| Days Between Strangulation and ED Visit | ||
| Less than 4 days | 313 | 90.7 |
| Between 5 and 7 days | 11 | 3.2 |
| Between 8 and 14 days | 10 | 2.9 |
| More than 14 days | 11 | 3.2 |
| Method of Strangulation | ||
| Manual | 338 | 98.0 |
| Ligature | 4 | 1.2 |
| Both manual and ligature | 2 | 0.6 |
| Unsure | 1 | 0.3 |
| Police Involvement | ||
| Police involved | 288 | 83.5 |
| Police not involved | 57 | 16.5 |
| Gender of Assailant | ||
| Male | 336 | 97.4 |
| Female | 9 | 2.6 |
Patients subsequently referred to DOVE for some form of violence did not always report strangulation to the ED clinicians. At the onset of data collection in 2008, 53% of patient records had documented strangulation disclosure to all three disciplines (DOVE, RN, prescriber), with approximately one in four patients (23.1%) disclosing strangulation to the DOVE advocate only. Following education and initiation of the practices described above, the percent of patients with documented strangulation disclosure by all three disciplines involved in their care increased, reaching 91.9% in 2016 (Figure 1). This increase in documented reporting was statistically significant during the initial implementation period with no significant change from 2014 to 2016 (2008–2014 Cochran-Armitage [CA]: 38.1, p<0.001; 2014–2016 CA: 0.18, p=0.67). This important first step in appropriate assessment and treatment of strangulation sequelae by the ED team demonstrates clinically significant progress towards identifying patients who have been strangled.
Figure 1:
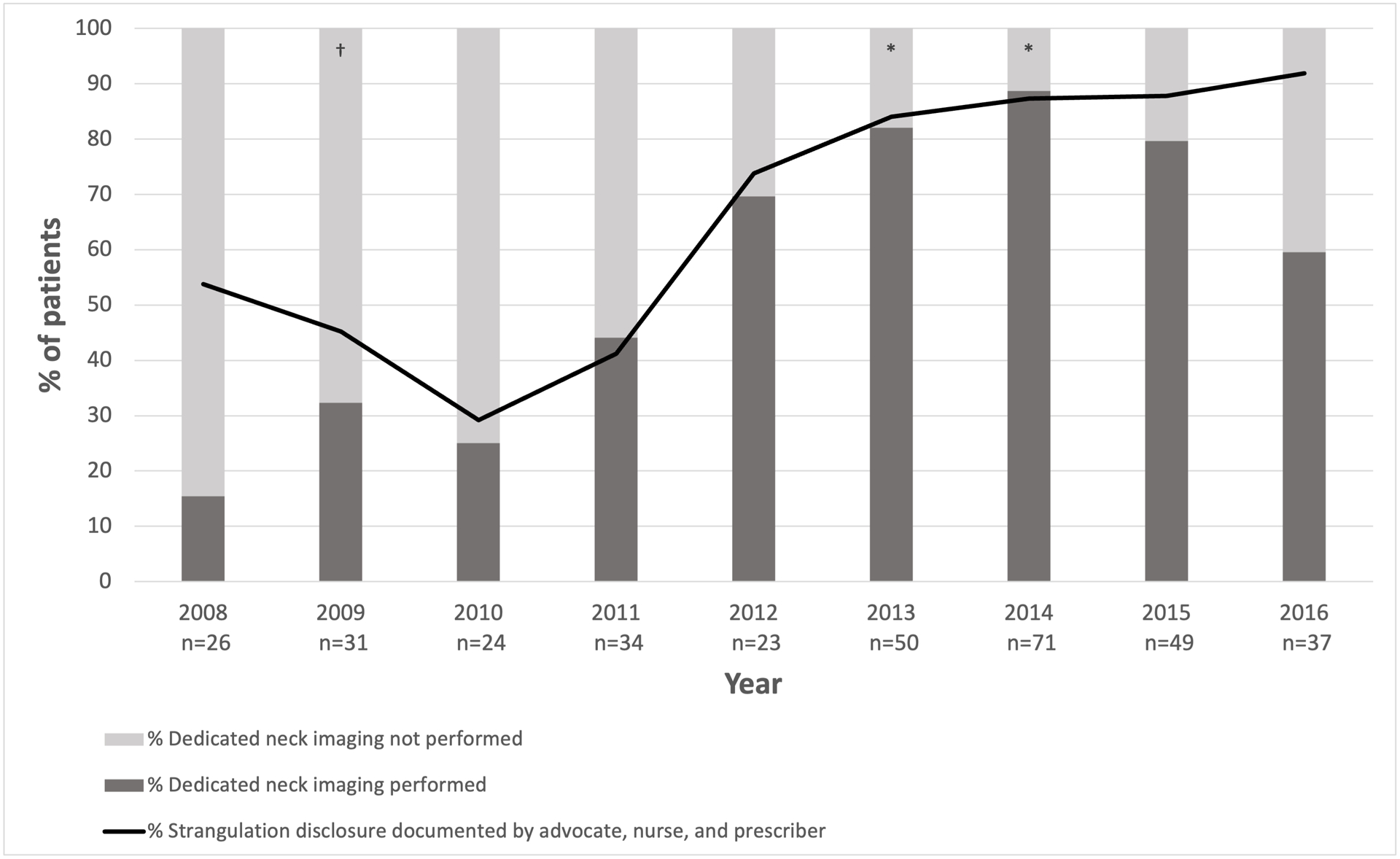
Neck Imaging and Strangulation Documentation by Multidisciplinary Team Over Time. (N=345)
†In 2009 the ED protocol for strangulation was initiated. This protocol included guidance for prescribers on pertinent questions to ask during a history, key areas of a physical examination to focus on, and documentation of findings. It also included criteria for imaging, otolaryngology consultation, and hospital admission.
*In 2013 and 2014 a part time registered nurse was grant funded to partner with the DOVE program to complete regular chart reviews and provide ongoing education to staff regarding strangulation.
Notes: 2008 to 2014 Cochran-Armitage test p<0.05 for both outcomes, 2014 to 2016 Cochran-Armitage test p>0.05 for strangulation disclosed to advocate, nurse and provider, p<0.05 for dedicated neck imaging.
Signs, Symptoms, and Injuries Documented
Among all patients, the most reported signs and symptoms related to strangulation were neck pain (67.2%), headache (45.8%), dysphonia (26.7%), breathing changes (26.4%) and difficulty swallowing (24.9%). Symptom patterns among all patients, patients who reported loss of consciousness, patients with positive head/neck findings on imaging, and pregnant patients are presented in Table 3. Patients with visible injuries to the neck (n=216, 62.6%) and those photographed using a commercially-available digital camera (n=105, 30.4% of all patients or 48.6% of patients with documented visible injury) are noted in Table 2.
Table 3:
Strangulation Signs and Symptoms Documented in Medical Records
| All patients (N=345) |
Patients with LOC (n=78) |
Patients who were pregnant (n=30) |
Patients with positive head and/or neck findings on imaging (n=45) |
|||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Neck pain | 232 | 67.2 | 58 | 74.4 | 20 | 66.7 | 34 | 75.6 |
| Headache | 158 | 45.8 | 40 | 51.3 | 9 | 30.0 | 24 | 53.3 |
| Dysphonia | 92 | 26.7 | 28 | 37.2 | 7 | 23.3 | 14 | 31.1 |
| Breathing changes | 91 | 26.4 | 29 | 35.9 | 13 | 43.3 | 13 | 28.9 |
| Dysphagia | 86 | 25.0 | 28 | 25 | 6 | 20.0 | 13 | 28.9 |
| Loss of consciousness | 78 | 22.6 | - | - | 4 | 13.3 | 11 | 24.4 |
| Dizziness | 47 | 13.6 | 17 | 21.8 | 4 | 13.3 | 9 | 20.0 |
| Vision changes | 41 | 11.9 | 13 | 16.7 | 4 | 13.3 | 5 | 11.1 |
| Numbness/weakness | 19 | 5.5 | 5 | 6.4 | 2 | 6.7 | 0 | 0 |
| Incontinent of urine or stool | 16 | 4.6 | 16 | 20.5 | 0 | 0 | 1 | 2.2 |
| Altered mental state | 14 | 4.1 | 6 | 7.7 | 2 | 6.7 | 2 | 4.4 |
| Tinnitus | 4 | 1.2 | 2 | 2.6 | 0 | 0 | 2 | 4.4 |
| Speech difficulty | 2 | 0.6 | 0 | 0 | 2 | 6.7 | 1 | 2.2 |
| Seizure | 1 | 0.3 | 1 | 1.3 | 0 | 0 | 0 | 0 |
Table 2:
Injuries and Imaging Documented
| n | % | |
|---|---|---|
| Patients (N=345) with documentation of: | ||
| Any visible injury to the neck | 216 | 62.6 |
| Neck injuries photographed (of n=216 with visible injuries) | 105 | 48.6 |
| Any imaging* | 315 | 91.3 |
| Dedicated neck vasculature imaging** | 216 | 62.6 |
| Offered and declined dedicated neck imaging | 12 | 3.5 |
| Among patients with any imaging (n=315): | ||
| Types of head imaging | ||
| CT head without contrast | 95 | 30.2 |
| CT head with contrast | 2 | 0.6 |
| CT facial bones without contrast | 5 | 1.6 |
| CT head and facial bones without contrast | 46 | 14.6 |
| Types of neck imaging | ||
| CT with IV contrast | 200 | 63.5 |
| CT angiogram | 6 | 1.9 |
| Carotid ultrasound | 10 | 3.2 |
| Among patients with any imaging (n=315): | ||
| Documented imaging findings to non-head/neck areas (n=10 patients *** ): | ||
| Finger fracture | 3 | 1.0 |
| Rib fracture | 2 | 0.6 |
| Pleural effusion | 1 | 0.3 |
| Ligament tear | 1 | 0.3 |
| Intrathoracic hemorrhage | 1 | 0.3 |
| Shoulder dislocation | 1 | 0.3 |
| Finger edema | 1 | 0.3 |
| Finger laceration | 1 | 0.3 |
| Documented imaging findings to the head or neck (n=45 patients *** ): | ||
| Facial edema | 11 | 3.5 |
| Neck muscle spasm | 8 | 2.5 |
| Facial fracture | 7 | 2.2 |
| Neck edema | 3 | 1.0 |
| Neck contusion | 3 | 1.0 |
| Facial contusion | 2 | 0.6 |
| Epiglottal swelling | 2 | 0.6 |
| Enlarged lymph nodes | 2 | 0.6 |
| Carotid artery dissection | 2 | 0.6 |
| Hyoid fracture | 2 | 0.6 |
| Herniated disk | 2 | 0.6 |
| Stroke | 2 | 0.6 |
| Scalp hematoma | 1 | 0.3 |
| Intracranial hemorrhage | 1 | 0.3 |
| Cervical spondylosis | 1 | 0.3 |
| Cervical fracture | 1 | 0.3 |
Includes: Any imaging test to any area of the patient, not specific to head or neck.
Includes: CTA, CT with IV contrast, or ultrasound specific to neck
Findings are not mutually exclusive (e.g., one person can have multiple reported types of imaging with this category or imaging findings).
Imaging
A CT with IV contrast, CTA or carotid ultrasound was documented n 216 records, with a demonstrable change in dedicated neck imaging from 15.4% in 2008 to 89% in 2014. This percentage then decreased to 59% by 2016 (Figure 1). These trends were significant at both time points examined (2008–2014 CA: 78.6, p<0.001; 2014–2016 CA: 12.0, p=0.001).
An internal injury to the head/neck was noted on imaging for 45 patients (e.g., facial bone fracture, edema – Table 3). In ten of the 315 patients who received imaging, there was an injury to another area of the body noted on imaging likely related to the same assault but unrelated to the strangulation. Only one patient had both neck/head and body injuries noted on imaging.
Two patients were diagnosed with carotid artery dissection, both exhibited few overall symptoms. The two symptoms that both patients endorsed were neck pain and headache, consistent with the two most exhibited symptoms by all patients in our sample. One patient also reported breathing changes, while the other experienced an altered mental state and dysphonia. It was only this latter patient that had visible injuries to her neck. Both patients were diagnosed after vascular imaging was performed. Three additional patients, with few neurologic symptoms noted in the medical record (e.g., headache; headache and neck pain; headache, neck pain, and dysphonia), were found to have strokes (n=2) and an intracranial hemorrhage (n=1) on head imaging. Patients with hyoid bone fractures (n=2) and epiglottal edema (n=2) reported more symptoms than those identified with vascular findings. All four of these patients reported breathing changes, three reported neck pain, two had visible external neck injuries, two had dysphonia, one reported difficulty swallowing, and one noted headache and loss of consciousness.
Examining the subset of 30 pregnant women who presented for care, 60.0% (n=20) had dedicated vascular imaging (8 with ultrasound, 12 with CTA or CT with IV contrast). None of the ultrasound studies reflected clinically significant findings. One CT demonstrated a carotid artery dissection requiring transfer to another health care center for management. One pregnant patient presented after NF-IPS to the ED with stroke-like symptoms (e.g., speech changes, facial droop, difficulty swallowing), and was transferred for high-risk obstetric and specialty neurology services without further imaging evaluation.
Final Diagnoses and Discharge Status
Most patients were discharged from the ED (n=322, 93.3%). Admissions for observation or inpatient care occurred for 17 (4.9%) patients, and 6 patients (1.7%) were transferred to other hospitals for specialty care or escalated to another facility providing a higher level of care. Example indications for these admissions and transfers are listed in Table 4. Despite all patients in the sample being referred to DOVE for an acute assault, only half (n=183, 53.0%) received a final diagnosis explicitly stating a physical or sexual assault, with even fewer (19.1%) including one suggestive of IPV (e.g., “domestic abuse”). “Strangulation” was noted in the final diagnoses of one in four patient charts (27.8%), “choking” in 2.6%, and the qualifiers “attempted,” “alleged,” or “accidental” in nearly 5% of final diagnoses. In total, 17.4% of cases included no diagnosis specifically related to the assault, strangulation, or IPV (e.g., vasovagal syncope) and, while 23.2% described injuries related to the assault (e.g., threatened abortion, facial injury), many did not specify assault or IPV as the causative mechanism.
Table 4:
Examples of Admission or Transfers among Patients Following Strangulation
| Reasons for Admission or Transfer Among Strangulation Patients |
|---|
|
Suicidal ideation (SI) was noted in 22 medical records (6.4%): with 18 of those 22 (81.8%) noted at the time of their initial ED visit. Four patients without documented SI at their initial visit later revisited the ED and reported SI: two within two weeks (9.1%) and two within two months (9.1%). Standard procedure for care of patients reporting suicidality in the ED included further assessment and care planning by a prescriber or psychiatric nurse. Suicidality (either attempt or ideation) was documented as the reason for admission or transfer for three patients (0.9%).
Discussion
Multidisciplinary Approach
Our descriptive data demonstrate how strangulation identification and evaluation can improve over time using a multidisciplinary team process, education, and policies. Vigilance and persistence are needed for sustainable improvements. While education and implementation of a strangulation protocol appear to have increased identification of NF-IPS and evaluation with neck imaging over time, dedicated regular follow-up with a grant-funded RN position during 2013 and 2014 may have made an even greater impact, as demonstrated by the increased numbers of NF-IPS patients identified and imaged during these years and a decrease following the discontinuation of these activities.
Multiple factors likely influenced full team documentation of strangulation cases. The advocacy team who, in 2009, initially received the highest disclosure rates maintained a consistent manager throughout the implementation period and were responsible for coordination of strangulation policy and education efforts. As a result, disclosures to the advocacy team were likely reported to medical and nursing team members in an effort to ensure appropriate multidisciplinary care. Quality review for protocol compliance was limited to the dedicated RN’s medical record audits and subsequent feedback to the treatment team. Consistent with challenges cited in existing literature,19 when near real time quality efforts were ceased, practice changes such as prescriber ordering of dedicated neck imaging were not sustained.
While this work was completed in a community-based ED setting, the findings have appreciable relevance to other settings that care for patients after traumatic violence. Not all patients readily disclosed or were evaluated for strangulation prior to initiation of the protocol. Thus, individuals working with patients in acute care and rehabilitation settings may also benefit from multidisciplinary team practices to identify patients at risk for having experienced strangulation and ensure comprehensive assessment.
Clinical Implications
The two identified cases of carotid artery dissection in our sample presented primarily with neck pain and headache, underscoring the importance of imaging to detect this potentially devastating injury. In our sample, it is likely that they received this imaging due to the presence of the ED protocol which recommended vascular imaging on all patients presenting with strangulation, regardless of the presence of neurological signs or symptoms.20–21 In 2008, prior to the protocol initiation only four of 26 patients seen for NF-IPS (15.4%) received dedicated neck imaging. By 2014, 63 of 71 patients (88.7%) received imaging – and between during this time period two strokes, an intracranial hemorrhage, and two carotid artery dissections were identified. Carotid artery dissection is a leading cause of stroke for patients under the age of 45.22 The most common known cause of carotid dissection is trauma. Case studies have demonstrated stroke occurring hours to months after neck trauma, including strangulation.23–26 Without timely recognition and appropriate clinical management, cervical vessel dissection can potentially result in thrombus formation and subsequent ischemic stroke, with subsequent disabilities or death.
This study highlights that strangulation survivors can and do seek care in community-based EDs. Current research suggests only a small percentage of NF-IPS survivors seek medical attention or are recognized and documented as having experienced strangulation.27 When survivors of IPV are identified, it is important to gain an understanding of the assault and ensure thorough examination is conducted. Similar challenges to identification and evaluation also exist in other care environments: strangulation survivors may minimize, be unaware of risks, experience cognitive and/or memory deficits from resulting brain injury, feel embarrassed or ashamed and, thus, not report, underreport, or downplay the assault.2,28 This, coupled with minimal visible injuries and few symptoms, may contribute to under-detection.
Additionally, a gap exists in both clinical guidelines and research regarding routine brain injury screening in patients surviving strangulation.29 To our knowledge, no national recommendations exist for standardized screening, assessments or referrals to experts such as neurology, occupational therapy, or head trauma rehabilitation teams. Future work is imperative and can begin by engaging these experts along with the existing body of work in other brain injury sub-populations like those sustaining motor vehicle crashes, contact sports or military trauma.
Our sample also included a small group of patients who were pregnant at the time they were strangled (n=30). Among these patients, the proportion who did not receive any dedicated neck imaging was high (33%, n=10) and the proportion who received carotid ultrasound was similarly high (26.6%, n=8). As one of the 12 pregnant patients who did receive a CT was diagnosed with a carotid dissection, the importance of complete and accurate imaging of neck vasculature among pregnant patients should not be overlooked. While not available during the study period, imaging recommendations for adult, pregnant post-strangulation patients have since been introduced (2018).15 These recommendations support updated practices based on available evidence of safe and appropriate imaging use in pregnancy. Carotid ultrasound is not advised as a first line imaging study, given its inability to fully evaluate the internal carotid and vertebral arteries.15
Anecdotally, it was observed by DOVE advocates that patients who experienced NF-IPS with other painful injuries (e.g., facial fractures) focused on those injuries and did not inform ED staff about the strangulation, disclosing only after specific inquiry. It is easy for first responders, survivors, and health care personnel alike to become distracted by obvious injury and overlook strangulation, which appeared to cause minimal symptoms or visible injuries. The lack of specific symptoms, injuries, or other distinguishing criteria among patients identified to have potentially devastating vascular injury supports current guidelines encouraging liberal use of dedicated neck imaging for patients following strangulation.14–15
Future Directions
An unexpected finding in these data was that 6.4% of NF-IPS patients presented with suicide attempts or ideation. While the specific relationship is not clear, prior research demonstrates increased death by suicide, suicidal ideation, and suicide attempts in individuals with recent and previous traumatic brain injury.30 Strangulation can decrease oxygenated blood flow to the brain or cause build up and rupture of blood vessels, resulting in a range of brain damage. When an IPV survivor exhibits suicidal behavior, there is often an assumption of psychological trauma or underlying mental health disorder causing the behavior, when there could be contributing physical trauma from strangulation impacting brain functioning. Implications for screening and universal education regarding IPV for patients with suicide ideation and screening NF-IPS patients for suicidality are important future considerations.
Identifying NF-IPS survivors for future research is complicated by medical coding. Prior work calls attention to challenges associated with coding such as lack of alignment with reimbursement priorities, unfamiliarity with IPV-specific codes, and medical record privacy concerns.27 This same study highlights IPV coding was uncommon in a nationally representative ED dataset, with co-occurring strangulation and IPV medical codes present in only 1.2% of visits.27 While our sample saw a higher rate of having IPV and strangulation in the final diagnosis (with 5.5% noting both), 100% of our study patients’ charts could have included both diagnoses. Final diagnoses often included only the resulting injury, less often noting it in conjunction with an assault or, more specifically, related to IPV. This further raises questions about the accuracy when using billing and coding data to obtain representative information regarding NF-IPS.
Limitations
Our sample of NF-IPS patients includes women who sought medical care at one community hospital. As prior research has demonstrated many women do not seek care following NF-IPS, our results may not be applicable to all individuals who experience strangulation. The injury patterns noted may not be consistent with those who do not seek care – as those who do are typically facing multiple injuries, multiple strangulations, or both.10,11 It is also possible the team may not have recognized all NF-IPS patients, precluding those missed from analysis.
Our sample was primarily African American patients, which may impact broader generalizability. Of note, in our data not reported, race was not found to be significantly associated with the presence of visible neck injuries. While internal injuries, assessment and treatment should not be impacted by race, structural racism and unconscious biases do exist within the medical and criminal justice systems. Racism may be more likely to negatively impact help-seeking from law enforcement and health care. In our sample, the willingness to seek help may suggest escalating violence in the relationship, increasing physical and psychosocial risks, and perceived lack of other available options.31
Similarly, the DOVE program relies on medical staff identifying IPV patients, either through screening or self-disclosure. Patients declining to disclose abuse may not prompt a response from a DOVE advocate and would not be included in our dataset. Retrospective chart review limits analysis as only data documented in the records were included. The multitude of staff involved in both medical treatment and advocacy over the years lends itself to variations in documentation. Retrospective data necessarily limits conclusions regarding causality. Furthermore, while we have data from patients who presented over an eight year period, each individual patients’ data were cross-sectional in nature and thus longitudinal follow-up was not included. Follow-up data is of utmost importance to understanding the long-term outcomes of strangulation.
This study was conducted in a community hospital without obstetrics, neonatology, or trauma services. Cases requiring these specialties are taken directly or transferred to another hospital with those services. However, our data demonstrate that even in this setting, 8.7% of NF-IPS patients were pregnant, 14.3% had head/neck injuries on imaging, and 6.6% required admission or transfer for additional care, reinforcing that all settings need to be prepared for strangulation identification, assessment, and management.
While our data were important to implementing new clinical policies and demonstrate a potential increase in post-strangulation identification and imaging evaluation over time, the use of retrospective records data must not be used as irrefutable evidence. Prospective, multisite data collection with direct patient follow up is needed to determine optimal options for NF-IPS management.
Conclusions
Implementation of a multidisciplinary team approach to identifying and assessing patients who have experienced NF-IPS in a community-based hospital setting demonstrated the ability to improve identification, documentation, imaging, and treatment of these patients. These data add to the growing literature regarding clinical samples of patients seeking care after NF-IPS. Importantly, we identified that the DOVE-ED partnership enabled sharing of strangulation disclosures more readily and longitudinally increased dedicated neck imaging. As patients may not be aware of strangulation risks, it is imperative for teams to continue patient identification efforts and provide timely evaluation and care.
Acknowledgements:
The authors wish to thank Rosalyn Berkowitz, RN, BSN, FNE-A/P, Kristen Kalinowski, MS, BSN, RN, Ann M. Myers, RN and Northwest Hospital for their generous support of the DOVE Program; Kelley Jones, PhD, MPH, for advisement on statistical analysis; and Jill Messing, PhD, MSW for helpful comments on earlier drafts of this manuscript.
Conflicts of Interest and Source of Funding:
All authors declare no conflicts of interest.
The authors gratefully acknowledge the following funding sources:
National Institutes of Alcohol Abuse and Alcoholism (K23AA027288, PI: Anderson)
The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding associations.
References
- 1.Monahan K, Bannon SM, Dams-O’Connor K. Nonfatal strangulation (NFS) and intimate partner violence: a brief overview. J Fam Viol. 2020. October; 10.1007/s10896-020-00208-7. [DOI] [Google Scholar]
- 2.Patch M, Anderson JC, Campbell JC. Injuries of women surviving intimate partner strangulation and subsequent emergency health care seeking: an integrative evidence review. J Emerg Nurs. 2018. July; 44(4): 384–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valera EM, Campbell J, Gill J, Iverson KM. Correlates of brain injuries in women subjected to intimate partner violence: identifying the dangers and raising awareness. J Aggress Maltreat Trauma. March 2019:1–19. doi: 10.1080/10926771.2019.1581864 [DOI] [Google Scholar]
- 4.Sauvageau A, Boghossian E. Classification of asphyxia: the need for standardization. J Forensic Sci. 2010; 55(5): 1259–1267. [DOI] [PubMed] [Google Scholar]
- 5.Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow M, Chen J. The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 data brief – updated release. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. 2018. [Google Scholar]
- 6.Iverson KM, Dardis CM, Grillo AR, Galovski TE, Pogoda TK. Associations between traumatic brain injury from intimate partner violence and future psychosocial health risks in women. Compr Psychiatry. 2019;92:13–21. doi: 10.1016/j.comppsych.2019.05.001 [DOI] [PubMed] [Google Scholar]
- 7.Vilke GM, Chan TC. Evaluation and management for carotid dissection in patients presenting after choking or strangulation. J Emerg Med. 2011; 40(3): 355–358. [DOI] [PubMed] [Google Scholar]
- 8.Bichard H, Byrne C, Saville CWN, Coetzer R. The neuropsychological outcomes of non-fatal strangulation in domestic and sexual violence: A systematic review. Neuropsychol Rehabil. January 2021:1–29. doi: 10.1080/09602011.2020.1868537 [DOI] [PubMed] [Google Scholar]
- 9.Campbell JC, Anderson JC, McFadgion A, Gill J, Zink E, Patch M, Callwood G, Campbell D. The effects of intimate partner violence and probable traumatic brain injury on central nervous system symptoms. J Womens Health. 2018; 27(6): 761–767. doi: 10.1089/jwh.2016.6311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith DJ Jr, Mills T, Taliaferro EH. Frequency and relationship of reported symptomology in victims of intimate partner violence: the effect of multiple strangulation attacks. J Emerg Med. 2001. October; 21(3): 323–329. [DOI] [PubMed] [Google Scholar]
- 11.Messing JT, Patch M, Wilson JS, Kelen GD, Campbell J. Differentiating among attempted, completed, and multiple nonfatal strangulation in women experiencing intimate partner violence. Womens Health Issues. 2018; 28(1): 104–111. [DOI] [PubMed] [Google Scholar]
- 12.Glass N, Laughon K, Campbell J, Blcok CR, Hanson G, Phyllis PW, Taliaferro E. Non-fatal strangulation is an important risk factor for homicide of women. J Emerg Med. 2008. October; 35(3): 329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spencer CM, Stith SM. Risk factors for male perpetration and female victimization of intimate partner homicide: a meta-analysis. Trauma Violence Abuse. 2020;21(3):527–540. doi: 10.1177/1524838018781101 [DOI] [PubMed] [Google Scholar]
- 14.Smock B, Sturgeon S. Recommendations for the medical/radiographic evaluation of acute adult, non-fatal strangulation. https://www.strangulationtraininginstitute.com/resources/library/medical-radiographic-imaging-recommendations/. Published April 8, 2019. Accessed 6/28/21
- 15.Weaver M, Bachmeier B. Recommendations for the medical/radiographic evaluation of the pregnant adult patient with non-fatal strangulation. https://www.familyjusticecenter.org/resources/recommendations-for-pregnant-victim/. Published May 2018. Accessed June 30, 2021.
- 16.IBM SPSS Statistics for Windows [computer Program]. Version 23.0. Armonk, NY: IBM Corporation. 2020. [Google Scholar]
- 17.Agresti A Categorical Data Analysis (2nd Ed.). New York: Wiley. 2002. [Google Scholar]
- 18.Hoenig JM, Heisey DM. The abuse of power. Am Stat. 2001;55(1):19–24. doi: 10.1198/000313001300339897 [DOI] [Google Scholar]
- 19.Rapport F, Clay-Williams R, Churruca K, Shih P, Hogden A, Braithwaite J. The struggle of translating science into action: foundational concepts of implementation science. J Eval Clin Pract. 2018;24(1):117–126. doi: 10.1111/jep.12741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McKee GB, Gill-Hopple K, Oesterle DW, Daigle LE, Gilmore AK. New perspectives on risk factors for non-fatal strangulation and post-assault imaging [published online ahead of print, 2020 Oct 13]. J Interpers Violence. 2020;886260520966673. doi: 10.1177/0886260520966673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matusz EC, Schaffer JT, Bachmeier BA, et al. Evaluation of nonfatal strangulation in alert adults. Ann Emerg Med. 2020;75(3):329–338. doi: 10.1016/j.annemergmed.2019.07.018 [DOI] [PubMed] [Google Scholar]
- 22.Patel R, Adam R, Maldjian C, et al. Cervical Carotid Artery Dissection. Cardiology in Review. 2012; 20 (3):145–152. doi: 10.1097/CRD.0b013e318247cd15. [DOI] [PubMed] [Google Scholar]
- 23.Clarot F, Vaz E, Papin F, Proust B. Fatal and non-fatal bilateral delayed carotid artery dissection after manual strangulation. Forensic Sci Int. 2005. May 10; 149(203): 143–150. [DOI] [PubMed] [Google Scholar]
- 24.Le Blanc-Louvry I, Papin F, Vaz E, Proust B. Cervical arterial injury after strangulation--different types of arterial lesions. J Forensic Sci. 2013. November; 58(6): 1640–1643. [DOI] [PubMed] [Google Scholar]
- 25.Malek AM, Higashida RT, Halbach VV, Dowd CF, Phatouros CC, Lempert TE, Meyers PM, Smith WS, Stoney R. Patient presentation, angiographic features, and treatment of strangulation-induced bilateral dissection of the cervical internal carotid artery. Report of three cases. J Neurosurg. 2000. March; 92(3): 481–487. [DOI] [PubMed] [Google Scholar]
- 26.Wu XM, Zhang XD, Yun LB, Liu M, Yi XF. Sudden death from ruptured intracranial vascular malformations during mechanical asphyxia: a domestic violence case report. Am J Forensic Med Pathol. 2017. March; 38(1): 35–38. [DOI] [PubMed] [Google Scholar]
- 27.Patch M, Farag YMK, Anderson JC, Perrin N, Kelen G, Campbell JC. United States ED visits by adult women for nonfatal intimate partner strangulation, 2006 to 2014: prevalence and associated characteristics. J Emerg Nurs. 2021;47(3):437–448. doi: 10.1016/j.jen.2021.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strack GB, McClane GE, Hawley D. A review of 300 attempted strangulation cases. Part I: criminal legal issues. J Emerg Med. 2001. October; 21(3): 303–309. [DOI] [PubMed] [Google Scholar]
- 29.St Ivany A, Schminkey D. Intimate partner violence and traumatic brain injury: state of the science and next steps. Fam Community Health. 2016;39(2):129–137. doi: 10.1097/FCH.0000000000000094 [DOI] [PubMed] [Google Scholar]
- 30.Harrison-Felix CL, Whiteneck GG, Jha A, et al. : Mortality over four decades after traumatic brain injury rehabilitation: a retrospective cohort study. Arch Phys Med Rehabil. 2009; 90:1506–1513. [DOI] [PubMed] [Google Scholar]
- 31.Harper SB. “I’m just like, you know what, it’s now or never”: exploring how women of color experiencing severe abuse and homicide risk journey toward formal help-seeking. J Interpers Violence. April 2021:8862605211005150. [DOI] [PubMed] [Google Scholar]


