Abstract
Parents of children with autism spectrum disorder (ASD) face challenges in accessing diagnostic and treatment services; these challenges vary by race, ethnicity, and culture. This systematic review examines parental perceptions of ASD within Latinx and Black American communities. Findings indicate that interconnections with family and religious groups promoted positive coping, and describe positive impacts of having a child with ASD. Relative to White families, community members reported reduced access to information and more inaccurate beliefs about ASD, higher levels of ASD-related stigma, and more negative experiences with healthcare providers; which serve to exacerbate healthcare disparities. Conclusions are limited by an underrepresentation of minority groups in research, and call for efforts to address the specific needs of racial and ethnic minorities.
Keywords: autism spectrum disorder, barriers to treatment, African American, Latino, healthcare disparities
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication, the presence of repetitive behaviors and interests, and atypical sensory processing. Although the disorder is equally prevalent across racial and ethnic groups (Christensen et al., 2018), research has repeatedly documented inequities in the diagnosis and treatment of non-White groups (Angell et al., 2018; Bishop-Fitzpatrick & Kind, 2017). Latinx and Black Americans are less likely than White children to have a documented diagnosis (Baio et al., 2018; Mandell et al., 2009); the diagnostic rates are even lower for Latinx children with two foreign-born parents (Schieve et al., 2012). They also receive these diagnoses later (Magaña et al., 2013; Mandell et al., 2002; Shattuck et al.,2011) and are less likely to be seen by specialists (Broder-Fingert et al., 2013) or to receive coordinated care and family-centered treatment (Jarquin et al.,2011; Magaña et al., 2012). Latinx children experience a delay between diagnosis and treatment (Magaña et al., 2013), and Black American children are more than twice as likely to be misdiagnosed (Mandell et al.,2007), when compared to White children. These disparities carry significant clinical consequences; parents of non-White children with ASD report reduced access to healthcare and less satisfaction with that healthcare (Liptak et al., 2008; Magaña et al., 2012).
Note that the more inclusive term “Latinx” is used rather than Latino/Latina. This review focuses on people from Spanish-speaking countries in Latin-America; it does not include Hispanics from other regions. “Black American” is used to denote the multi-ethnic nature of the Black community in the United States; for instance, African and Afro Caribbean immigrants are often included in the Black/African American group despite different cultural and ethnic backgrounds. As used here, the term does not include Black Latinxs.
Latinx and Black Americans are the largest non-White groups in the United States, accounting for approximately 30% of the U.S. population; according to projections from the Pew Research Center, by 2055, less than half of the U.S. population will consist of “non-Hispanic Whites” (“Modern Immigration Wave,” 2015). Although all families interpret children’s behaviors, strengths, and weaknesses in unique ways, their understanding of psychological concerns is strongly influenced by their cultural backgrounds (Bussing, Schoenberg, & Perwien, 1998; Lau, 2006; Yeh et al., 2004). For instance, non-White parents are less likely than White parents to endorse physical causes of developmental disorders (Yeh et al., 2004) or to use medical language in discussing their children’s difficulties (Bussing et al., 1998). Non-White parents of children with ASD endorse similar barriers to services as do White parents however, the extent of and reasons for these barriers differ. There is some overlap between Latinx and Black American caregivers’ perceptions of issues related to race and ethnicity, and their communities’ perceptions of ASD (Stahmer et al., 2019). Research also shows that socio-cultural factors influence how and when families seek diagnostic and intervention services (Dardennes et al., 2011; Hebert & Koulouglioti, 2010; Mandell & Novak, 2005; Singh & Bunyak, 2019). In a society that is rapidly diversifying, it is critical that we understand the specific socio-cultural and systemic factors that impact access to services for these communities.
Non-White individuals have been generally underrepresented in research on ASD (Hilton et al., 2010; Kalsner et al., 2018; West et al., 2016); inadequate reporting of race and ethnicity is also common. For example, non-White participants may be lumped together and described as “Other,” which, among other challenges, makes it impossible to meaningfully include them in meta-analyses (Pierce et al., 2014; Wolery & Garfinkle, 2002). This historical lack of research has limited our understanding of the specific, sociocultural needs and experiences of these communities; fortunately, the last few years have seen a surge in research. The current review provides an updated perspective, focusing on (a) parental and community perceptions of the causes and course of ASD; (b) experiences with stigma; (c) protective factors; and (d) religious, family, and gender values, as they relate to Latinx and Black Americans. We also review reports of experiences with healthcare professionals. Although health disparities reflect the impact of carrying any of a wide variety of marginalized identities (e.g., having a lower socioeconomic status, living in a rural area, or being non-White), the present work focuses specifically on those who identify as Latinx or Black American. In this article, we (a) present a systematic review of parental and community perceptions of ASD in Latinx and Black American communities; (b) discuss the clinical implications of these perceptions; and (c) provide recommendations to facilitate better research and clinical practice, and to increase equitable access to care.
Approach of the Current Review
The studies included in this review encompass a broad variety of factors that impact access to and quality of services. Against this background, we performed a systematic review following PRISMA guidelines; see Figure 1. The factors discussed in this review were chosen based on the following criteria: (a) they are important cultural values for the target populations, (b) they have been empirically linked to ASD-related healthcare disparities, and/or (c) they have potential to inform clinical practice. We performed a comprehensive review of the literature using PsychInfo, PubMed, EBSCO Dissertation Repository, and Google Scholar. Key search terms were: [ASD; autism; Asperger] and [Latin*; Hispanic; African American; African; Black], conjoined with: parental beliefs; perceptions; disparities; barriers; knowledge; faith; vaccines; coping; stress. Articles were included if they met the following criteria: (1) the sample included Latinx or African/Black American participants (or both); (2) the primary focus was on ASD; (3) the research addressed parental or community perceptions of ASD; (4) the research was conducted in the United States; and (5) the study discussed any of the following topics: (a) perceptions about the causes/course of ASD; (b) knowledge of ASD; (c) family stigma; (d) family stressors; or (e) the roles of religious, family, and gender values. The search was limited to articles between 2005 to 2019. After removing duplicates and screening titles and abstracts for eligibility, we were left with a total of 45 peer-reviewed articles and 5 dissertations, which were included in this review. Dissertations were included for the Black American group only due to limited research.
Figure 1. Scoping Review Procedure.
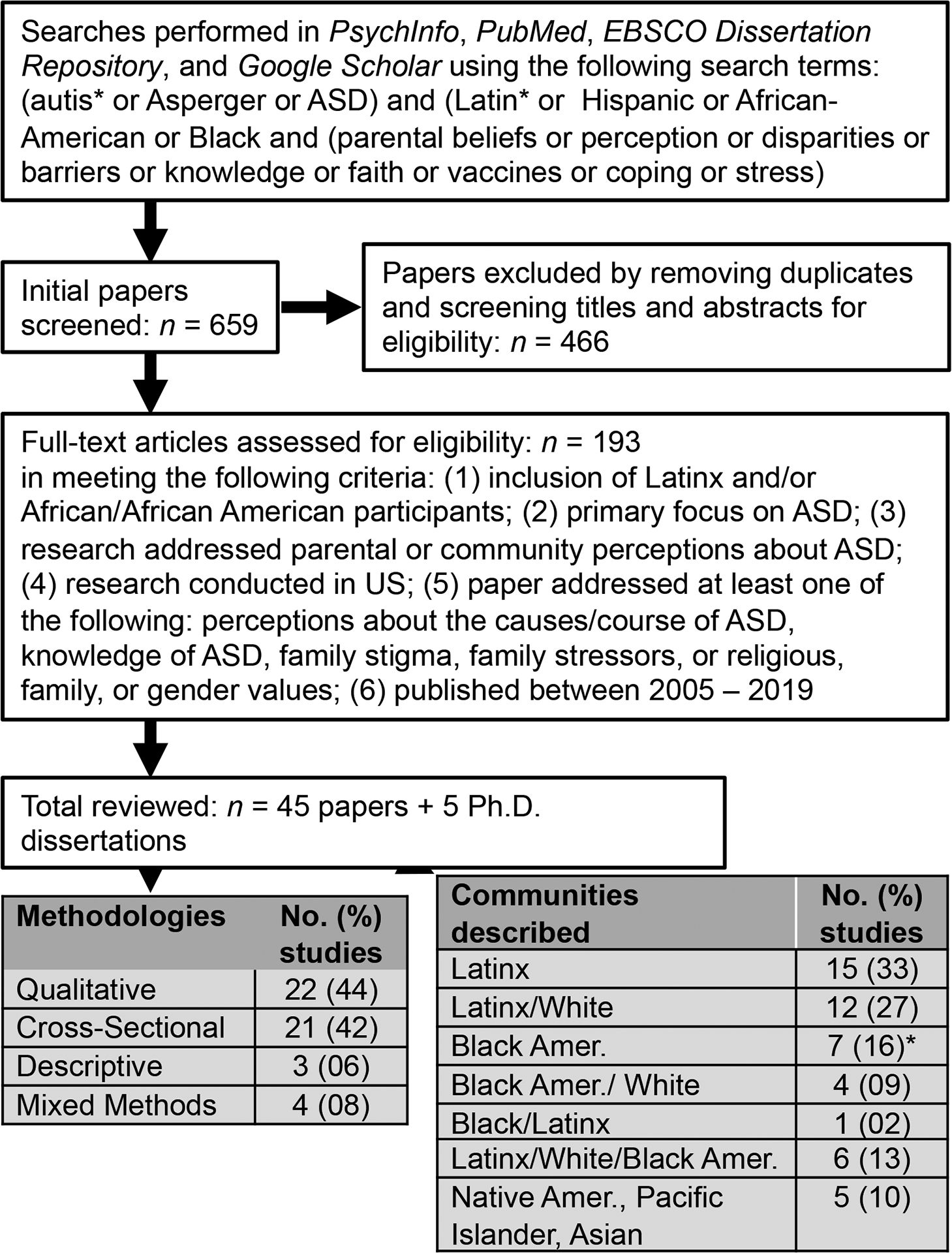
Note. *Excludes five unpublished dissertations described in this review.
The studies included in this review were assessed for quality using the Let Evidence Guide Every New Decision (LEGEND) system (Clark et al., 2009). After independently evaluating each study, the first two authors conferred and compared quality ratings (i.e., good, moderate, lesser). Interrater evaluation disagreements were discussed and resolved before finalizing quality ratings. Of the studies included, 48% achieved a good quality rating, 38% were deemed moderate, and 14% were considered of lesser quality; ratings were addressed in the discussion of findings that follow. Table 1 presents these quality ratings and describes the methodologies and study samples included in this review.
Table 1.
Characteristics of Included Studies, Ordered by Method and Quality Rating
| Method | Populations | N (ordered by population) | Quality rating | Reference |
|---|---|---|---|---|
| Cross-sectional | Latinx | 67 | Good | Colbert et al., 2017 |
| Cross-sectional | Black Amer, Latinx, White | 682, 665, 3762 | Good | Magaña et al., 2012 |
| Cross-sectional | Latinx, White | 48, 56 | Good | Magaña et al., 2013 |
| Cross-sectional | Black Amer, Asian, Native Amer/Hawaiian, White | 2759 | Good | Neuhaus et al., 2018 |
| Cross-sectional | Latinx, White | 665, 3762 | Good | Parish et al., 2012 |
| Cross-sectional | Latinx, White | 160, 145 | Good | Reyes et al., 2018 |
| Cross-sectional | Black Amer, White | 51, 52 | Good | Williams et al., 2019 |
| Cross-sectional | Black Amer, White | 30, 80 | Moderate | Bishop et al., 2007 |
| Cross-sectional | Latinx, White | 73, 44 | Moderate | Ekas et al., 2016 |
| Cross-sectional | Black Amer, Latinx, Asian/Pacific Islander, Multiracial, White | 2, 10, 1, 4, 56 | Moderate | Ekas et al., 2019 |
| Cross-sectional | Black Amer | 34 | Moderate | Longtin et al., 2016 |
| Cross-sectional | Latinx, White | 46, 56 | Moderate | Lopez & Magaña, 2018 |
| Cross-sectional | Black Amer, Latinx, White, Other | 89, 118, 1056, 145 | Moderate | McLeod et al., 2019 |
| Cross-sectional | Black Amer, Latinx, White, Other | 89, 118, 1056, 145 | Moderate | Zuckerman et al., 2015 |
| Cross-sectional | Black Amer, Latinx, White | 26, 52, 91 | Lesser | Bazzano et al., 2012 |
| Cross-sectional | Black Amer, White | 17, 68 | Lesser | Carr et al., 2013 |
| Cross-sectional | Latinx, White | 28, 28 | Lesser | Ratto et al., 2016 |
| Cross-sectional | Latinx | 169 | Lesser | Voelkel et al., 2013 |
| Descriptive | Latinx | 267 | Good | Zuckerman et al., 2013 |
| Descriptive | Latinx | 96 | Moderate | Iland et al., 2012 |
| Descriptive | Latinx (1 White, 1 Asian) | 29 | Moderate | Williams et al., 2009 |
| Mixed Methods | Latinx | 25 | Good | Cohen et al., 2018 |
| Mixed Methods | Latinx, White | 28, 27 | Good | Dubay et al., 2018 |
| Mixed Methods | Black Amer | 17, 68 (Quantitative); 6 (Qualitative) | Moderate | Llorens, 2018 |
| Mixed Methods | Latinx, White | 15 | Moderate | Magaña & Smith, 2006 |
| Qualitative | Black Amer | Caregivers: 11; and 6 Cultural Brokers | Good | Brown, 2018 |
| Qualitative | Latinx | 24 | Good | Burke et al., 2019 |
| Qualitative | Black Amer | Caregivers: 24; and 28 Healthcare Providers | Good | Burkett et al., 2015 |
| Qualitative | Black Amer | 24 | Good | Burkett et al., 2017 |
| Qualitative | Black Amer | 22 | Good | Dababnah et al., 2018 |
| Qualitative | African immigrants | 29 | Good | Davies, 2019 |
| Qualitative | Black Amer, Latinx, Hawaiian/Pacific Islander, Multi, White | 4, 10, 1, 1, 5 (total n = 17) | Good | Iadarola et al., 2019 |
| Qualitative | Latinx | 0 | Good | Ijalba, 2016 |
| Qualitative | Latinx, White | 44, 52 | Good | Lopez et al., 2018 |
| Qualitative | Black Amer | 13 | Good | McCoy, 2018 |
| Qualitative | Black Amer, Latinx, Korean | Caregivers: 18, 26, 14; and 55 Healthcare Providers | Good | Stahmer et al., 2019 |
| Qualitative | Latinx | 30 | Good | Zuckerman, Sinche, Cobian, et al., 2014 |
| Qualitative | Black Amer | 14 | Moderate | Angell et al., 2014 |
| Qualitative | Latinx | 12 | Moderate | Angell et al., 2017 |
| Qualitative | Latinx | 15 | Moderate | Blanche et al., 2015 |
| Qualitative | Latinx | 14 | Moderate | Lobar, 2014 |
| Qualitative | Black Amer | Caregivers: 20; and 2 Healthcare Providers | Moderate | Parks, 2017 |
| Qualitative | Latinx | 34 | Moderate | Salkas et al., 2016 |
| Qualitative | Latinx | 33 | Moderate | Zuckerman, Sinche, Mejia, et al., 2014 |
| Qualitative | Latinx | 10 | Lesser | Estrada et al., 2014 |
| Qualitative | Black Amer | 3 | Lesser | Lovelace et al., 2018 |
| Qualitative | Black Amer | 16 | Lesser | Pearson et al., 2018 |
Overall, this review provides a specific, comprehensive overview of key factors that contribute to ASD-related health inequities in Latinx and Black American communities in the United States. We highlight communities and parent perceptions of the causes, course, and red flags of ASD; ASD-related feelings of stigma; family impact; protective factors (including religion, families, and gender roles); and patient-provider relationship quality as they relate to ASD diagnosis and treatment in these populations. The Discussion presents practical steps for reducing stigma and facilitating better access to healthcare services in members of Latinx and Black American communities.
Beliefs About the Etiology of ASD
Studies of Latinx community members’ beliefs about the etiology of ASD have yielded conflicting results. Voelkel and collaborators (2013) surveyed 168 Latinx community members and found that although most (70%) knew that vaccines do not cause ASD, many (46%) believed that emotional trauma played a significant role; most (64%) did not understand the role of genetics (Voelkel et al., 2013). Similarly, a qualitative interview study of 22 immigrant Latinx caregivers found that a majority (72%) attributed communication deficits in ASD to traumatic events, fears, or sadness during pregnancy (Ijalba, 2016).
Studies of Latinx parents receiving ASD services report some awareness of the genetic underpinnings of ASD, alongside misconceptions about etiology. In a qualitative interview study of 25 Latinx parents, most attributed their child’s ASD to genetics or a family history of disabilities (Cohen & Miguel, 2018); several also reported the (erroneous) belief that ASD “skips a generation.” Quantitative studies have found that Latinx parents are less likely to endorse genetic causes of ASD compared to White parents (McLeod & DiSabatino, 2019; Zuckerman et al., 2016). In a survey of 197 parents of children with ASD, 54% of Latinx parents endorsed the belief that vaccines cause autism, compared to 37% of White parents (Bazzano et al., 2012). Latinx parents are also likely to attribute symptoms to poor parenting or negative family relationships (DuBay et al., 2018; Salkas et al., 2016; Zuckerman, Sinche, Cobian, et al., 2014; Zuckerman, Sinche, Mejia, et al., 2014). These frequent misconceptions about the genetic underpinnings and other causes of ASD, expressed by families already enrolled in community clinics, suggest that parents are not receiving adequate information from treatment providers.
There is little research examining causal beliefs in Black American communities. Many Black American mothers attribute ASD to vaccinations, and they do so more often than White parents (58% vs. 37%, respectively) when controlling for socioeconomic status (SES; Bazzano et al., 2012). However, they are less likely to discontinue or change their child’s vaccination schedule after receiving an ASD diagnosis (Bazzano et al., 2012). Black American parents are also more likely to endorse beliefs about postnatal exposure causes of ASD (Zuckerman et al., 2016). An unpublished dissertation study on Black American parents’ perceptions of ASD (n = 45) found that most parents endorsed genetic causes (51%), vaccines (42%), and God’s will (42%) as primary causes of ASD. Only 29% of Black American parents ranked genetics as the most important aspect (Llorens, 2016).
Beliefs that ASD is a mystery (Zuckerman et al., 2015) or a result of traumatic experiences (Dardennes et al., 2011) are associated with reduced behavioral intervention; thus, better education may increase service utilization. Seeing ASD as a “mystery” can interact in unexpected ways with service use. A study of 305 mothers of children with ASD reported that those who described ASD as a “mystery” used more ASD intervention services, regardless of severity, race, ethnicity, or language (Reyes et al., 2018). Few studies have compared causal beliefs about ASD or how these beliefs impact service use across racial groups. Although every family is different, these results suggest that Latinx and Black American families’ misconceptions likely contribute to reduced service use.
Beliefs About the Course of ASD
Latinx families saw ASD as a temporary condition in several qualitative studies (Ijalba, 2016; Lobar., 2014; Voelkel et al. 2013; Zuckerman, Sinche, Cobian, et al., 2014). Larger quantitative studies reported mixed findings. Reyes and collaborators (2018) studied 305 mothers of children with ASD (English-proficient or limited-English-proficiency Latinx and White mothers). Parents across all groups saw ASD as a lifelong condition, with major consequences for their child, that could be influenced by intervention (Reyes et al., 2018). However, mothers with limited-English-proficiency were more likely to believe that ASD was a mystery, and mothers with less education (across groups) were more likely to believe that symptoms were unchangeable. Related research suggests that the belief that ASD is temporary is not related to levels of distress (McLeod & DiSabatino, 2019; Zuckerman et al., 2015). In one recent study, Black American parents reported beliefs that ASD is a chronic disorder and endorsed a moderately high degree of control over their child’s symptoms (Llorens, 2016). However, a survey of 1,420 families of children with special needs found that parents of Latinx and Black American children with ASD were more likely than White parents to see the condition as temporary, controlling for ASD severity. Across groups, lower SES was associated with the belief that ASD is a mystery, and lower education was associated with skepticism about the efficacy of treatment (McLeod & DiSabatino, 2019; Zuckerman et al., 2015). Altogether, these results suggest that race/ethnicity, SES, acculturation, and language proficiency each impact parental beliefs and the likelihood of seeking services.
Understanding Early Signs of ASD
Knowledge about ASD symptoms and child development influences the starting point of the diagnostic process (DuBay et al., 2018; Ijalba, 2016; Liptak et al., 2008; Longtin & Principne, 2016; Magaña et al., 2013; Ratto et al., 2016; Stahmer et al., 2019; Zuckerman, Sinche, Cobian, et al., 2014; Zuckerman, Sinche, Mejia, et al., 2014). In a questionnaire study, Latinx mothers of children with ASD (n = 28) had significantly less knowledge of ASD symptoms, developmental milestones, and adaptive skills, compared to White mothers (n = 28), controlling for maternal education (Ratto et al., 2016). This finding is echoed in multiple qualitative studies (DuBay et al., 2018; Ijalba, 2016; Lopez et al.,2018; Stahmer et al., 2019; Zuckerman, Sinche, Cobian, et al., 2014; Zuckerman, Sinche, Mejia, et al., 2014). For example, many Latinx mothers were unfamiliar with ASD prior to their child’s diagnosis (Ijalba, 2016; Lopez et al., 2018; Zuckerman, Sinche, Mejia, et al., 2014). Almost all Latinx mothers in another questionnaire study (n = 96) endorsed a need for more ASD information (Iland et al., 2012). Caregivers with limited-English-proficiency (n = 94) were more likely to endorse inadequate ASD knowledge as a barrier to services, and report fewer therapy hours and more unmet need, when compared to English-proficient Latinx (n = 95) or non-Latinx White (n = 163; Zuckerman et al., 2017) caregivers. Latinx parents are often presented with low-quality Spanish language resources (Blanche et al., 2015; Zuckerman, Sinche, Cobian, et al., 2014).
In Black American communities, parents report reduced ASD awareness, and misinformation (Burkett et al., 2015; Iadarola et al., 2019; Stahmer et al., 2019), a finding echoed in several unpublished dissertations (Brown, 2018; Davies, 2018; McCoy, 2018). Parents also report that others in their communities might be reluctant to learn about ASD (Iadarola et al., 2019). A qualitative study of 24 Black American family members found that families were unaware of similar ASD prevalence across Black American and White communities, or of diagnostic delays and treatment differences between their communities (Burkett et al., 2015). A study of 34 urban Black American parents found that decreased knowledge of evidence-based interventions was associated with poverty (Longtin & Principe, 2016). Both Latinx and Black American caregivers express insufficient access to information about ASD resources and services, which results in delayed diagnosis and services (Stahmer et al., 2019).
ASD knowledge is critical for understanding early signs of ASD and accessing services. This knowledge is also influenced by factors interacting with race and ethnicity: acculturation (Colbert et al., 2017; Voelker et al., 2013), religiosity (Colbert et al., 2017), SES (Colbert et al., 2017; Longtin & Principe, 2016), social support (Colbert et al., 2017), and English language proficiency (Colbert et al., 2017; Reyes et al., 2018; Zuckerman, Sinche, Cobian, et al., 2014; Zuckerman et al., 2017). Lack of ASD knowledge is particularly salient within Latinx and Black American communities, even when parents are already in the healthcare system. It is associated with later age of first concern and age of diagnosis (Ratto et al., 2016); further, this presents a barrier to early identification and service use (Blanche et al., 2015; Burkett et al., 2015; McCoy, 2018; Zuckerman, Sinche, Mejia, et al., 2014; Zuckerman et al., 2017) and reduces parenting confidence (Lopez et al., 2018). Relevant to these findings, healthcare providers indicated that they perceive Latinx and Black American parents and caregivers as less knowledgeable about ASD than White parents (Zuckerman et al., 2013). Regardless of their accuracy, such perceptions could negatively impact the patient-provider relationship and treatment progress.
Stigma
Families of children with ASD experience significant stigma; that is, prejudicial attitudes, negative stereotypes, and acts of discrimination targeting a subgroup (Corrigan, 2004). This experience has negative effects on care-seeking behavior (Corrigan, 2004; Dos Reis, Barksdale, Sherman, Maloney & Charach, 2010; Gray 1993, 2002; Hatzenbuehler et al., 2013); it also exacerbates existing healthcare disparities for Black American and Latinx individuals, relative to White individuals (Conner et al., 2009; Das et al., 2006; Nadeem et al., 2007). Latinx and Black American parents of children with ASD are at a greater risk of experiencing stigma due to being a member of a marginalized group and having a child with ASD, a phenomenon known as double disadvantage (Dowd & Bengtson, 1978). ASD-related stigma may thus have a particularly strong influence on healthcare utilization for these populations (Hatzenbuehler et al., 2013).
Research with Latinx families indicates that stigma is a meaningful concern. Parents report that their communities often perceive disabilities as shameful and experience pressure to conceal their children’s atypical behaviors and diagnosis (Stahmer et al., 2019; Zuckerman, Sinche, Mejia, et al., 2014); family and community members may also question the credibility of the diagnosis (Iadarola et al., 2019; Stahmer et al., 2019). Parents report feeling discomfort in sharing concerns with healthcare providers and community members, fearing that their children will be judged or shunned and that their parenting skills will be questioned (Cohen et al., 2018; Dubay et al., 2018; Iadarola et al., 2019; Lobar, 2014; Stahmer et al., 2019; Zuckerman, Sinche, Mejia, et al., 2014). In an ethnographic study, 12 Latinx families reported that they were often deterred from advocating for services by fears of retaliation and judgement from professionals. Investigators also found that those who nonetheless advocated for services despite these fears were often questioned, underestimated, and ultimately denied access to services by school professionals (Angell & Solomon, 2017). Latinx parents report experiencing loneliness and limited support as a result (Stahmer et al., 2019). In a qualitative study with 44 Latinx and 52 White mothers, Latinx mothers reported feelings of guilt about their child’s ASD diagnosis, whereas White mothers reported relief, suggesting that stigmatizing messages might be internalized by Latinx parents (Lopez et al., 2018). Concerns about stigma can deter parents from accessing services and social support (Angell & Solomon, 2017; Idarola et al., 2019; Stahmer et al., 2019).
A quantitative study of stigma in Latinx families found that non-U.S.-born parents, and those with limited English-proficiency, experienced greater stigma than White parents (Zuckerman et al., 2018); stigma was also associated with poverty and greater symptom severity. Greater stigma was related to unmet treatment needs, controlling for the amount and type of treatment, suggesting that stigma has a significant impact on quality of care. Latinx families likely experience more stigma when providers are unprepared to interact with families of marginalized backgrounds, and when language barriers are present. Overall, ASD is highly stigmatized in Latinx communities, especially for lower-SES and limited-English-proficiency immigrants (Zuckerman et al., 2018. Taken together, these factors lead to social isolation, unmet treatment needs, and parental guilt (Blanche et al., 2015; Iadarola et al., 2019; Ijalba, 2016; Zuckerman et al., 2018).
Families of Black American children with ASD also experience significant ASD-related stigma. Parents express a lack of acceptance in their communities (Brown, 2018; Burkett et al., 2015; Lovelace et al., 2018; Parks, 2017; Stahmer et al., 2019) and report feeling guilty and blamed for their child’s ASD (Burkett et al., 2017; Lovelace et al., 2018; McCoy, 2018). Community members often attribute behavioral symptoms of ASD to a lack of discipline or poor parenting and question the ASD diagnosis; these experiences result in feelings of loneliness and isolation and a reluctance to share the diagnosis (Stahmer et al., 2019). Parents in an unpublished dissertation study reported that individuals with severe ASD are often feared (Brown, 2018). ASD-related stigma is also prevalent among African immigrants; an unpublished dissertation study reported that children could be abandoned or isolated and receive negative treatment and abuse from people in their communities (Davies, 2018). Denial, shame, and stigma delay treatment and decrease research participation (Dababnah et al., 2018; Davies, 2018; Stahmer et al., 2019). A recent qualitative cross-cultural study suggests that Latinx and Black American parents are more likely to have their parenting style questioned, compared to Korean parents (Stahmer et al., 2019). Overall, research suggests that Latinx and Black American parents experience significant stigma from their communities and the institutions designed to support families of children with ASD. These experiences of stigma contribute to service disparities.
Protective Factors
Some aspects of Latinx and Black American cultures serve to protect and buffer families from some of the stresses associated with parenting a child with ASD. Although caregivers of children with ASD generally report higher levels of parenting stress, this experience varies by culture. Both Latinx and Black American families describe the caregiver role as less burdensome than White American families (Connell & Gibson, 1997). For example, Latinx and Black American mothers reported greater positive contributions of their child’s ASD, which in turn related to lower levels of anxiety symptoms (Ekas et al., 2019). In a study of 88 White and 20 Latinx mothers of children with ASD, Latinx mothers reported less anger and fatigue, a greater sense of “mastery” of their own lives, and better psychological well-being, despite economic disadvantages (Magaña & Smith, 2006). They also reported greater satisfaction with their child, family cohesion, peace of mind, and personal growth. A study with 46 Latinx and 56 White mothers found fewer perceived family problems and less pessimism about the child’s future among Latinx participants (Lopez et al., 2018). Latinx mothers were more likely to report seeing a “silver lining” in adverse circumstances—a phenomenon known as benefit finding (Ekas et al., 2016). Notably, however, Latinx parents were more likely to report feeling “upset” about the ASD diagnosis, compared to parents of other races/ethnicities (McLeod & DeSabatino, 2019).
Studies with Black American families suggest more mixed results. A group of Black American mothers perceived the impact of their child’s ASD symptoms as less negative when compared to White mothers (Bishop et al., 2007); this finding remained 5 years later (Carr & Lord, 2013). Black American families reported more stress and reliance on a greater variety of coping strategies compared to White families, particularly when they were less acculturated toward the majority culture (Williams et al., 2019). Importantly, parents who perceived a more negative impact of the diagnosis had children who received more treatment hours (Carr & Lord, 2013), suggesting that positive perceptions may reduce motivation to access services. Family cohesiveness, interdependence and caregiving values may help parents find meaning in their responsibilities. Although this might reduce the impetus to seek services, a better understanding of these factors would facilitate a more informed approach to service delivery and enhance our understanding of how to better support Latinx and Black American families.
The Role of Religion
Religion plays an important role in family life (Caplan, 2019; Krok, 2018). On the negative side, religious beliefs are sometimes associated with passive and avoidant behavior (Strug et al., 2009); however, these beliefs can promote better planning, positive reframing, and active coping (Umezawa et al., 2012), and they can provide membership in communities. Religious beliefs influence how families cope with, understand, and manage challenges (Dyches et al., 2004). For instance, higher levels of spirituality are associated with mothers viewing their child with ASD as providing a positive contribution to the family (Ekas et al., 2019). In the case of ASD, Latinx caregivers are more likely to report that their child is a blessing, a test, or a message from God (Estrada & Deris, 2014; Lobar, 2014; Salkas et al., 2016). Latinx caregivers are also more likely to endorse the belief that a child can be cured through divine intervention (Ijalba, 2016). In a phenomenological study (relying primarily on interview and survey methods), most Latinx family members (7 out of 10) endorsed using “faith” as an at-home treatment (Estrada & Deris, 2014). Faith in God also helps Latinx parents advocate for services (Burke et al., 2019).
Religion also has a strong influence on beliefs, coping strategies, and treatment choices in the Black American and African immigrant communities. Black American parents report believing that ASD is God’s will or a blessing (Burkett et al., 2017; Llorens, 2016). Families in these communities tend to pray often and to report a belief that God will lead them (Estrada & Deris, 2014; Williams et al., 2019). Religious attributions and coping appear to be more frequent in individuals who endorse subscribing to Black American beliefs and traditions, compared to Black individuals who are more accultured towards mainstream U.S. culture (Williams et al., 2019). African immigrants are more likely to believe that ASD is caused by evil spirits or a curse. Engaging in spiritual interventions is also common, though most parents report that nonspiritual interventions are preferred (Davies, 2018). In sum, research indicates that both Latinx and Black families in the United States rely heavily on religion to cope with and understand their children’s disability.
The Role of Families
Latinx and Black American families report that family members play a central role in their experiences of raising a child with a developmental disability. Family-centered values in Latinx communities are linked to better quality of life among mothers of children with intellectual disability (Cohen et al., 2014), and are correlated with more supportive co-parenting behaviors (Lindsey, 2018). Extended family members of children with ASD may be the first to raise concerns about a child’s development; Latinx respondents in a qualitative study believed that the family was uniquely able to understand the child (Lobar, 2014). Latinx parents report relying on other family members for childcare, transportation, and financial support; co-housing is common (Estrada & Deris, 2014; Stahmer et al., 2019). In one qualitative study, Latinx mothers reported receiving less help from their families relative to White mothers (Lopez & Magaña, 2018); in contrast, in a quantitative study, Latinx and White mothers reported similar levels of emotional bonding within the family and perceptions of family support (Ekas et al., 2016). In Black American communities, family members provide critical emotional, economic, and logistical support (Burkett et al., 2017; Stahmer et al., 2019). Latinx and Black American parents express the importance of involving family in the diagnostic process, as they are often the ones recognizing first signs and recommending evaluation (Stahmer et al., 2019). Clearly, extended family members are a vital source of support for both Black American and Latinx caregivers. At the same time, close-knit family relationships can be problematic. Latinx values of familismo, or the central importance of family (Davila et al., 2011), may lead families to first seek advice and guidance within the family (Edgerton & Karno, 1971), potentially delaying the diagnostic process. Family members may provide counterproductive advice by advocating firm discipline or a “wait and see” approach (Blanche et al., 2015; Dubay et al., 2018; Ijalba, 2016; Lopez et al., 2018; Stahmer et al., 2019).
A similar pattern is described in Black American families. When families of children with disabilities seek guidance from family, friends, and church members, they receive social support (Burkett et al., 2015; Rogers-Dulan & Blacher, 1995; Stahmer et al., 2019), but this process can delay diagnosis. Black American parents report that family members often deny the existence of the disability, blame them for their child’s symptoms, believe children will grow out of it, or suggest that parents turn to faith (Brown, 2018; Llorens et al., 2016; Lovelace et al., 2018; Pearson & Meadan, 2018; Stahmer et al., 2019). Some parents also report feeling abandoned by their extended family members and perceiving a lack of familial support (Brown, 2018; McCoy, 2018). Though family support alone does not account for racial and ethnic disparities in service utilization, understanding these values is central to assessing coping and to developing culturally sensitive interventions.
Gender Roles
Research assessing how gender roles impact health care utilization is limited. Latinx cultures are broadly characterized by strong gender roles, in which mothers are most responsible for caregiving and describe motherhood as their primary role (Estrada & Deris, 2014; Magaña & Smith, 2006). Such gender roles may contribute to diagnostic delays, if mothers must negotiate the logistics of clinical care alone. In a quantitative study of 33 Latinx families, machismo, or adherence to traditional gender roles, was described by mothers as exacerbating stigma, with fathers believing that their child with ASD reflected negatively on them (Zuckerman, Sinche, Mejia, et al., 2014). Fathers with more machismo were more likely to dismiss their partner’s concerns, to be uncooperative with the diagnostic process, and to participate less in childcare. Machismo has been linked to less supportive coparenting behaviors in Latinx communities (Lindsey, 2014). A study of 15 Latinx families reported that fathers were generally less involved and understood less about their child’s symptoms (Blanche et al., 2015). A majority (72%) of Latinx mothers in a questionnaire study endorsed needing support to help their spouses accept their child’s condition (Iland et al., 2012). Another study of 46 Latinx caregivers found that female participants reported advocating more assertively on behalf of their child, compared to their more passive husbands (Burke et al., 2019). A study comparing coping styles between Latinx fathers (n = 43) and mothers (n= 46) found that mothers reported greater depressive symptoms and greater use of positive and support coping than fathers; however, both mothers and fathers reported similar levels of optimism and similar reliance upon avoidant coping (Willis et al., 2016)
Studies of Black American families also indicate gender differences in rearing responsibilities. Families report concerns about self-sufficiency (Burkett et al., 2017), with mothers more focused on independence in activities of daily living (e.g., dressing, making lunch), and fathers more focused on preventing harm from others and guarding against racism. Parents report sharing the responsibilities of child rearing (Burkett et al., 2017). On the other hand, an unpublished dissertation study suggests that pressure to conform to the expectation that Black women should be strong, independent, and able to manage difficulties alone can lead to delays in seeking help (Parks, 2017).
Patient-Provider Relationship
Latinx and Black American communities value open and frequent communication, and close personal relationships with their healthcare providers (HCP) that are grounded in respect, trust, and flexibility. Latinx parents often prefer to include extended family members in their child’s therapies, and express greater interest in group interventions with other parents (DuBay et al., 2018). Black American parents express a desire for providers to show respect for their values, beliefs, and parenting abilities, and want providers to integrate the family’s child-rearing practices into treatment plans and to adapt therapies for home use (Burkett et al., 2015).
Although ASD healthcare disparities among Latinx and Black Americans may reflect the impact of factors like stigma and a lack of ASD knowledge on service utilization, consistent differences in the quality of the patient-provider relationship, and in access to high-quality, culturally competent services relative to White families may also play a key role (Magaña et al., 2012; Parish et al., 2012). The quality of the relationship with HCPs impacts a family’s engagement in treatment and the time of diagnosis (Parish et al., 2012). Unfortunately, members of Latinx and Black American communities report more unsatisfying and difficult experiences with their HCPs, in part because HCPs frequently underestimate non-White parents’ education and knowledge (Angell & Solomon, 2017; Gourdine et al., 2011; Stahmer et al., 2019; Zuckerman, Sinche, Mejia, et al., 2014). Latinx and Black American parents are often met with providers who suggest a “wait and see” approach and normalize their behavioral concerns; Spanish-speaking and Black American caregivers often understand this to be a reaction to their race or culture and feel invalidated (Stahmer et al., 2019). Families who describe their HCP as “dismissive” are more likely to have delays in diagnosis (Stahmer et al., 2019; Zuckerman, Sinche, Mejia, et al., 2014). Parents receive confusing and conflicting recommendations, and many also experience unprofessional HCP behavior (DuBay et al., 2018). Parents with limited-English-proficiency are more likely to endorse distrust in the HCP as a barrier to service use (Zuckerman et al., 2017); to report receiving conflicting information that is not explained clearly (Stahmer et al., 2019); and to describe feeling discriminated against by professionals for not speaking English (Burke et al., 2019). They also grapple with limited Spanish-language information and services (Blanche et al., 2015; DuBay et al., 2018; Iadarola, 2019; Stahmer et al., 2019; Zuckerman Sinche, Mejia, et al., 2014). Even when materials are available in Spanish, the information quality is often poor, inaccurately translated, or filled with medical jargon (Zuckerman Sinche, Cobian, et al., 2014).
Furthermore, many parents are advised by HCPs to speak only English with their children (Ijalba, 2016); this advice is misguided, given strong evidence that bilingual children with ASD fare as well as monolingual children and may benefit from broader inclusion of family members in caregiving (Dai et al., 2018; Hambly & Fombonne, 2012; Ohashi et al., 2012; Petersen et al., 2012). Parents also describe provider confusion around what language their child should speak (Stahmer et al., 2019). Latinx parents report that they receive less information about ASD, compared to White parents (Iadarola, 2019). Black American parents report similarly difficult experiences with HCPs who ignore or disregard family members and their concerns (Burkett et al., 2015; Dababnah et al., 2018; Llorens, 2016; Lovelace et al., 2018; Stahmer et al., 2019). They report that HCPs lack cultural knowledge and implicitly criticize or question child-rearing practices and competence (Burkett et al., 2015). Parents describe receiving fewer services and services of lesser quality, and also having to advocate for services that are routinely offered to others (Brown, 2018). Of 22 Black American mothers, nearly all (n = 20) reported that their HCP ignored their initial concerns and did not provide referrals for ASD screening services (Dababnah et al., 2018). Incidents of racism and microaggressions by providers are often described (Dababnah et al., 2018; Gourdine et al., 2011; Lovelace et al., 2018). Black children’s health records are often not written in a family-centered manner, which causes parents to feel judged and misrepresented (Angell & Salomon, 2014). For example, a report might describe a mother as “unemployed” or, in a more family-centered fashion, as a “full-time homemaker;” the latter might more effectively portray family members as they see themselves. Distrust of medical professionals impacts how Black American parents seek services (McCoy et al., 2018).
In general, parents of Latinx and Black American children with ASD receive lower-quality healthcare (Magaña et al., 2012; Parish et al., 2012). Clinicians are less likely to recognize the signs and symptoms of ASD in Latinx children (Zuckerman et al., 2013), tend to underestimate the impact of the language of assessment on outcomes (Williams et al., 2009), show bias when evaluating vignettes of culturally diverse children with ASD (Begeer et al., 2009), and are less concordant with parent reports of symptoms in younger Black American children (Neuhaus et al., 2018). The most widely used ASD assessment tools are normed on predominantly White samples, and administration guidelines have little guidance regarding cultural considerations (Harris et al., 2014). Racial and ethnic disparities are exacerbated by a lack of culturally competent healthcare. To date, the healthcare system has failed to accommodate the needs of a rapidly growing, racially and ethnically diverse population.
Discussion
Research on ASD in Latinx and Black American communities documents disparities in diagnosis, quality of care, and service utilization. The two largest non-White groups in the United States have long been invisible in ASD literature. Though the literature is growing, we still have much to learn. This review described (a) parental and community perceptions about the causes and course of ASD; (b) ASD knowledge; (c) the experience of stigma; (d) protective factors; and (e) the role of religious, family, and gender values in Latinx and Black American communities. We also reviewed community-level factors that influence experiences with healthcare professionals. Understanding these factors will allow providers to better respond to the needs of their patients.
Our review yields several tentative findings. First, these populations struggle with relatively limited knowledge about ASD. They are less likely to be familiar with the “red flags” of ASD, and more likely to believe that ASD is caused by emotional trauma, ineffective parenting practices, or vaccines. They are also more likely to believe that ASD is a temporary condition. Such beliefs can lead to delays in diagnosis and intervention and increased stigma. More high-quality qualitative research is needed to substantiate these findings, as well as quantitative research that captures the magnitude of the impact of these factors on service use. However, the current findings indicate that more targeted education efforts might lead to meaningful changes in time of diagnosis and ultimately engender improved long-term outcomes.
Potentially more difficult to remediate are the findings that Latinx and Black American families struggle with high levels of ASD-related stigma in their communities. Communities tend to perceive disabilities as shameful; parents experience pressure to hide children who are atypical, and fear judgement of their parenting. Again, stigma contributes to delays in diagnosis and accessing services, is associated with unmet treatment needs, exacerbates social isolation and self-blame among parents, and decreases research participation. Although Latinx and Black American communities likely struggle with higher levels of ASD-related stigma relative to White families, only one study to date has directly compared stigma levels between Latinx and White families (Zuckerman et al., 2018), and there is no research comparing Black American and White families. Additional comparative studies are needed.
Although reduced knowledge and ASD-related stigma exacerbate healthcare disparities, there are important community-specific protective factors. Latinx and Black American families may rely on family members and religious beliefs more than their White peers. Relatedly, parents in these communities tend to report fewer negative impacts of having a child with ASD. Family and religiosity are vital sources of support. Understanding these cultural values is important to promote effective coping strategies. Increasing access to useful information within these communities can help counterbalance diagnostic delays related to waiting for family input.
Culturally-specific gender roles can either support mothers in the caregiving process or increase their burden. Latinx mothers worry that their male partners feel shame about their child’s ASD, dismiss their concerns, struggle to accept the diagnosis, and are less involved in caretaking, all of which increase maternal burden. In Black American families, mothers and fathers appear to prioritize distinct goals related to their respective gender norms (i.e., promoting independence versus preventing harm), and couples may share caregiving tasks equitably. Interpretations of these findings should be made with caution; the body of research directly assessing the impact of gender roles on caregiving among Latinx and Black American parents of children with ASD is limited by its small size and reliance upon maternal perspectives. More studies—particularly those including perspectives of fathers and other male caregivers—are needed to draw more definite conclusions.
In their relationships with HCPs, Latinx and Black American families desire close and trusting relationships, direct communication, and having their values respected. Unfortunately, these expectations often go unmet, and Latinx and Black Americans experience lower healthcare quality (Magaña et al., 2012; Parish et al., 2012). All too often, HCPs dismiss parents’ concerns, underestimate their knowledge, engage in racial and ethnic microaggressions, and fail to understand and respect cultural values and rearing practices. They also struggle to recognize signs of ASD in non-White children, and account for bilingual or nonfluent language status during assessments. Families report inadequate access to Spanish-language information and Spanish-speaking providers. There are few culturally-appropriate assessments. These factors all increase healthcare disparities, but could be addressed, at least in part, by education that targets healthcare providers.
There is little research examining how ASD-related stigma, knowledge, and patient-provider relationships contribute to racial and ethnic healthcare disparities. Existing quantitative research is limited by small sample sizes and an undercharacterization of study samples in terms of race, ethnicity, and other sociodemographic and cultural characteristics; this limitation is particularly salient because, as reviewed here, immigration status, acculturation, language, SES, and religious beliefs interact with race and ethnicity. Existing qualitative research utilizes well-characterized samples, but often lacks in-depth exploration of how race, ethnicity, and other sociodemographic correlates of ASD disparities—namely SES and parent education level—interact to uniquely impact ASD disparities within Latinx and Black American communities. The specificity of sample characteristics required for strong qualitative research, although informative about similar groups, also limits the extent to which results can be generalized to the general population. As a whole, the available literature—including the research reviewed here—often misses important sociocultural nuances within broader categories of race and ethnicity, such as within-group differences among Blacks (e.g., Black Americans, Jamaican Americans, and Nigerian Americans) and Latinx (e.g., Mexicans, Cubans, and Puerto Ricans) communities. Furthermore, many studies treat Latinx and Black populations as mutually exclusive, without capturing those individuals who share both identities. This obscures the unique impact that race and ethnicity have on Black and Latinx individuals and their access to ASD services. The best practice for future research is to describe the detailed and complex racial, ethnic, and sociocultural backgrounds of Latinx and Black participants. Doing so will increase our understanding of and ability to address how these nuances impact access to ASD services.
One of the biggest limitations of this research is that Black American communities are underrepresented; only 40% of the published studies in this review include Black Americans, and the results of these studies are not widely generalizable. We cannot hope for better outcomes without a more comprehensive understanding of the current limitations faced by Black American families in need of ASD treatment services. Furthermore, the research does not include families who are not receiving services; obviously, these families are the most difficult to recruit and engage in research, but only by understanding their concerns and needs can we hope to increase their engagement. Creative approaches are needed to reach these families at home and in their communities.
Next Steps
This review of the existing literature, along with our own clinical experiences, suggests several practical strategies that could reduce current inequities. First and foremost, researchers and clinicians alike must acknowledge and remain mindful of the profound role that racial and ethnic biases play in both ASD research and clinical practice. It is vital to recognize the nuanced nature of race, ethnicity, and culture when interpreting the results of research and making treatment recommendations. A failure to do so could lead to the infliction of unintended harm on already vulnerable populations. Second, we must reduce language barriers. Latinx patients will be better served if intervention services recruit Spanish-speaking individuals with the relevant cultural background to deliver interventions (Magaña et al., 2017). Interpreters should be fluent in the client’s language and familiar with their specific culture because language use (e.g., terminology, pragmatics, meaning) varies across Latinx cultures; see Hadziabdic & Hielm (2013) for practical guidance on the use of interpreters in healthcare settings. Written materials such as pamphlets, questionnaires, and so forth, should be reviewed by a community member to ensure that the language is clear and appropriate (Lajonchere et al., 2016). HCPs should consider identifying or forming Spanish-speaking support groups to serve Latinx families (Dubay et al., 2018). Recruiting more Spanish-speaking individuals to medical school and other healthcare professions will surely also help to address this challenge.
We can also work to reduce some of the structural barriers that often limit Latinx’s and Black Americans’ access to ASD diagnostic and treatment services. For example, providers can offer extended hours for caregivers who cannot afford to take a day off from work for an appointment; help them arrange transportation or childcare; or provide web- or community-based services (i.e., telehealth and mobile screenings; Nowell et al., 2015); one outcome of the 2020 COVID-19 pandemic has been increased availability of telehealth services. Furthermore, community-based clinics could partner with local sponsors and public health organizations to offer families access to assessment, consultations, and service recommendations. The Rhode Island Consortium for Autism Research and Treatment (RI-CART) is a working model, bringing together families and people with ASD, researchers, clinicians, educators, and local agencies, with a mission of (a) providing education, (b) improving access to intervention and support services, and (c) promoting research (Gerber et al., 2014). Home-based intervention or parent-training might be especially appropriate for this population (Dubay et al., 2018).
Because family ties are critical in both Latinx and Black American communities, including extended family members in treatment can increase intervention efficacy (Buzhardt et al., 2016; Magaña et al., 2015). This approach will also reduce stigma by increasing awareness and knowledge of the disorder in all family members. For example, providers could encourage parents to bring influential extended family members to appointments. Doing so could enhance family-provider relationships and allow for more comprehensive clinical observation. HCPs should explicitly ask about parenting values and incorporate these values into treatment planning (Zayas & Solari, 1994). These values may be at odds with evidence-based intervention approaches; clinicians must engage in shared decision making and partnership with families to determine appropriate treatment options. Stiggelbout and collaborators (2012) present some useful strategies on how to engage families in such partnerships.
Providers should also aim to understand their clients’ cultural backgrounds, identities, and belief systems. Explicitly asking about these attributes, for example by using the semistructured Cultural Formulation Interview (Lewis-Fernández et al., 2016), can aid this process. Being respectful and aware of religious beliefs (Johnson & Van Hecke, 2015) and cultural sayings (Magaña et al., 2017) can increase the connection between HCPs and their patients. Although not all families are devout, HCPs should be open to explicit conversations about spiritual beliefs (Salkas et al., 2016). With regards to gender roles, HCPs should probe how each family negotiates caretaking responsibilities, helping families to build on each parent’s strengths. One of the simplest and most important strategies HCPs can use is to invest time in fostering a trusting relationship with parents. This is especially important when working with Latinx and Black American families because of historical mistrust between these populations and the medical community.
The scientific and clinical communities should collaborate to reduce the knowledge gap in Latinx and Black American families by (a) helping parents understand the symptoms and causes of ASD; (b) informing them about services; (c) minimizing the stigma of ASD; and (d) clarifying common misconceptions like the belief that vaccines, bad parenting, or trauma cause ASD. Educational material should be free of jargon and include photos of people from non-White groups (Lajonchere et al., 2016). Providing video recordings of materials will make them more accessible to individuals with lower literacy (Durkin et al., 2010; Zuckerman, Sinche, Cobian, et al., 2014). Latinx community members have also suggested targeted radio and TV campaigns that provide concrete and straightforward information (Zuckerman, Sinche, Mejia, et al., 2014). Literature can be distributed by community organizations and announcements regarding services can be broadcast in community spaces. Given the link between low SES and ASD knowledge, information would be particularly impactful when provided by organizations that serve low-SES families.
Researchers and HCPs should also consider partnerships between existing clinics and community gatekeepers (e.g., elders, pastors, deacons, etc.) or organizations; this will help expand their own cultural knowledge, gain trust within the communities they serve, and promote ASD awareness (Johnson & Van Hecke, 2015; Moody et al., 2019). For example, one pilot study successfully trained religious leaders to use culturally appropriate materials (e.g., videos of Black American children with ASD symptoms, integrating religious scriptures into the materials) to recognize early signs of ASD and to talk to families about services (Johnson & Van Hecke, 2015). Programs such as the Appreciative Inquiry/Bootcamp Translation program utilize a community-based participatory research framework (Israel et al., 2008) to engage community members and develop practical actions to reduce ASD disparities (Moody et al., 2019); this approach is promising though clearly more research is needed. Stronger relationships with cultural leaders will contribute to greater understanding of the community’s cultural context (Moodley & Sutherland, 2010).
One final strategy for reducing health-care disparities is for clinicians to utilize validated autism screeners, such as the M-CHAT-R and the RITA-T, which have demonstrable diagnostic efficacy across racial and ethnic backgrounds (Choueiri & Wagner, 2015; Herlihy et al., 2014). Because non-White and lower SES families receive evaluations less frequently, screeners should be administered at opportune moments rather than at specific milestones or ages (Adamson et al., 2003). Culturally appropriate assessment norms and cultural considerations should be used when available; efforts to improve these cultural components are urgently needed. This approach will minimize bias in assessment.
Reducing ASD healthcare disparities requires a multifaceted response from both HCPs and the scientific community. Providers should take a more holistic and culturally sensitive approach to care and ensure that they develop trusting relationships with families. Universal screening is also needed. Researchers must include more non-White participants in their studies and actively study how socio-demographic factors like race and ethnicity influence service use and outcomes. It is essential that professionals in the field recognize and consider the systemic and socio-cultural barriers that decrease Latinx and Black American access to ASD services. This awareness will help clinicians and scientists take deliberate action to reduce barriers and improve the quality of healthcare for the largest proportion of families affected by ASD.
Acknowledgments
Portions of this work were supported by NIMH R01MH112687–01A1 (I.M. Eigsti, PI), by NSF 1144399 (J.S. Magnuson, PI), and by a UConn Provost’s Research Award (I.M. Eigsti, PI).
References
- Adamson J, Ben-Shlomo Y, Chaturvedi N, & Donovan J (2003). Ethnicity, socio-economic position and gender—Do they affect reported health-care seeking behaviour? Social Science & Medicine, 57(5), 895–904. [DOI] [PubMed] [Google Scholar]
- Angell AM, Empey A, & Zuckerman KE (2018). A review of diagnosis and service disparities among children with autism from racial and ethnic minority groups in the United States. In Hodapp RM & Fidler DJ (Eds.), International review of research in developmental disabilities (Vol. 55, pp. 145–180). Academic Press. 10.1016/bs.irrdd.2018.08.003 [DOI] [Google Scholar]
- Angell AM, & Solomon O (2014). The social life of health records: Understanding families’ experiences of autism. Social Science & Medicine, 117, 50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angell AM, & Solomon O (2017). “If I was a different ethnicity, would she treat me the same?”: Latino parents’ experiences obtaining autism services. Disability & Society, 32(8), 1142–1164. 10.1080/09687599.2017.1339589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, Kurzius-Spencer M, Zahorodny W, Robinson Rosenberg C, White T, Durkin MS, Imm P, Nikolaou L, Yeargin-Allsopp M, Lee LC, Harrington R, Lopez M, Fitzgerald RT, Hewitt A, Pettygrove S, Constantino JN, Vehorn A, Shenouda J, Hall-Lande J, Van Naarden Bround K, & Dowling NF (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2014. Morbidity and Mortality Weekly Report Surveillance Summaries, 67(6), 1–23. 10.15585/mmwr.ss6706a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzano A, Zeldin A, Schuster E, Barrett C, & Lehrer D (2012). Vaccine-related beliefs and practices of parents of children with autism spectrum disorders. American Journal on Intellectual and Developmental Disabilities, 117(3), 233–242. [DOI] [PubMed] [Google Scholar]
- Begeer S, El Bouk S, Boussaid W, Terwogt MM, & Koot HM (2009). Underdiagnosis and referral bias of autism in ethnic minorities. Journal of Autism and Developmental Disorders, 39(1), 142–148. 10.1007/s10803-008-0611-5 [DOI] [PubMed] [Google Scholar]
- Bishop SL, Richler J, Cain AC, & Lord C (2007). Predictors of perceived negative impact in mothers of children with autism spectrum disorder. American Journal on Mental Retardation, 112(6), 450–461. 10.1352/0895-8017(2007)112[450:POPNII]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, & Kind AJH (2017). A scoping review of health disparities in autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(11), 3380–3391. 10.1007/s10803-017-3251-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanche EI, Diaz J, Barretto T, & Cermak SA (2015). Caregiving experiences of Latino families with children with autism spectrum disorder. American Journal of Occupational Therapy, 69(5), 1–11. 10.5014/ajot.2015.017848 [DOI] [PubMed] [Google Scholar]
- Broder-Fingert S, Shui A, Pulcini CD, Kurowski D, & Perrin JM (2013). Racial and ethnic differences in subspecialty service use by children with autism. Pediatrics, 132(1), 94–100. 10.1542/peds.2012-3886 [DOI] [PubMed] [Google Scholar]
- Brown IC (2018). Experiences of African American parents of students with autism and school partnerships [Unpublished doctoral dissertation]. San Francisco State University. [Google Scholar]
- Burke MM, Rios K, Garcia M, Sandman L, Lopez B, & Magaña S (2019). Examining the perspectives of Latino families of children with autism spectrum disorder towards advocacy. Exceptionality, 27(3), 201–214. [Google Scholar]
- Burkett K, Morris E, Anthony J, Shambley-Ebron D, & Manning-Courtney P (2017). Parenting African American children with autism: The influence of respect and faith in mother, father, single-, and two-parent care. Journal of Transcultural Nursing, 28(5), 496–504. 10.1177/1043659616662316 [DOI] [PubMed] [Google Scholar]
- Burkett K, Morris E, Manning-Courtney P, Anthony J, & Shambley-Ebron D (2015). African American families on autism diagnosis and treatment: The influence of culture. Journal of Autism and Developmental Disorders, 45(10), 3244–3254. 10.1007/s10803-015-2482-x [DOI] [PubMed] [Google Scholar]
- Bussing R, Schoenberg NE, & Perwien AR (1998). Knowledge and information about ADHD: evidence of cultural differences among African-American and white parents. Social science & medicine, 46(7), 919–928. 10.1016/S0277-9536(97)00219-0 [DOI] [PubMed] [Google Scholar]
- Buzhardt J, Rusinko L, Heitzman‐Powell L, Trevino‐Maack S, & McGrath A (2016). Exploratory evaluation and initial adaptation of a parent training program for Hispanic families of children with autism. Family Process, 55(1), 107–122. 10.1111/famp.12146 [DOI] [PubMed] [Google Scholar]
- Caplan S (2019). Intersection of cultural and religious beliefs about mental health: Latinos in the faith-based setting. Hispanic Health Care International, 17(1), 4–10. [DOI] [PubMed] [Google Scholar]
- Carr T, & Lord C (2013). Longitudinal study of perceived negative impact in African American and Caucasian mothers of children with autism spectrum disorder. Autism, 17(4), 405–417. 10.1177/1362361311435155 [DOI] [PubMed] [Google Scholar]
- Choueiri R, & Wagner S (2015). A new interactive screening test for autism spectrum disorders in toddlers. The Journal of Pediatrics, 167(2), 460–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen DL, Braun KVN, Baio J, Bilder D, Charles J, Constantino JN, Daniels J, Durkin MS, Fitzgerald RT, Kurzius-Spencer M, Lee LC, Pettygrove S, Robinson C, Schulz E, Wells C, Wingate MS, Zahorodny W, & Yeargin-Allsopp M (2018). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2012. Morbidity and Mortality Weekly Report Surveillance Summaries, 65(13), 1–23. 10.15585/mmwr.ss6513a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark E, Burkett K, & Stanko-Lopp D (2009). Let evidence guide every new decision (LEGEND): An evidence evaluation system for point-of-care clinicians and guideline development teams. Journal of Evaluation in Clinical Practice, 15(6), 1054–1060. 10.1111/j.1365-2753.2009.01314.x [DOI] [PubMed] [Google Scholar]
- Cohen S, Holloway S, Domínguez‐Pareto I, & Kuppermann M (2014). Receiving or believing in family support? Contributors to the life quality of Latino and non‐Latino families of children with intellectual disability. Journal of Intellectual Disability Research, 58(4), 333–345. [DOI] [PubMed] [Google Scholar]
- Cohen SR, & Miguel J (2018). Amor and social stigma: ASD beliefs among immigrant Mexican parents. Journal of Autism and Developmental Disorders, 48(6), 1995–2009. [DOI] [PubMed] [Google Scholar]
- Colbert AM, Webber J, & Graham R (2017). Factors that influence autism knowledge in Hispanic cultures: A pilot study. Journal of Racial and Ethnic Health Disparities, 4(2), 156–164. [DOI] [PubMed] [Google Scholar]
- Connell CM, & Gibson GD (1997). Racial, ethnic, and cultural differences in dementia caregiving: Review and analysis 1. The Gerontologist, 37(3), 355–364. 10.1093/geront/37.3.355 [DOI] [PubMed] [Google Scholar]
- Conner KO, Koeske G, & Brown C (2009). Racial differences in attitudes toward professional mental health treatment: The mediating effect of stigma. Journal of Gerontological Social Work, 52(7), 695–712. 10.1080/01634370902914372 [DOI] [PubMed] [Google Scholar]
- Corrigan P (2004). How stigma interferes with mental health care. American Psychologist, 59(7), 614–625. 10.1037/0003-066X.59.7.614 [DOI] [PubMed] [Google Scholar]
- Dababnah S, Shaia WE, Campion K, & Nichols HM (2018). “We had to keep pushing”: Caregivers’ perspectives on autism screening and referral practices of Black children in primary care. Intellectual and Developmental Disabilities, 56(5), 321–336. [DOI] [PubMed] [Google Scholar]
- Dai YG, Burke JD, Naigles L, Eigsti IM, & Fein DA (2018). Language abilities in monolingual- and bilingual-exposed children with autism or other developmental disorders. Research in Autism Spectrum Disorders, 55, 38–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dardennes RM, Al Anbar NN, Prado-Netto A, Kaye K, Contejean Y, & Al Anbar NN (2011). Treating the cause of illness rather than the symptoms: Parental causal beliefs and treatment choices in autism spectrum disorder. Research in Developmental Disabilities, 32(3), 1137–1146. [DOI] [PubMed] [Google Scholar]
- Das AK, Olfson M, Mccurtis HL, & Weissman MM (2006). Depression in African Americans: Breaking barriers to detection and treatment. The Journal of Family Practice, 55(1), 30–40. [PubMed] [Google Scholar]
- Davies L (2018). Understanding use of care for African immigrants with autistic children [Unpublished doctoral dissertation]. Walden University. [Google Scholar]
- Davila YR, Reifsnider E, & Pecina I (2011). Familismo: Influence on Hispanic health behaviors. Applied Nursing Research, 24(4), e72. [DOI] [PubMed] [Google Scholar]
- DosReis S, Barksdale CL, Sherman A, Maloney K, & Charach A (2010). Stigmatizing experiences of parents of children with a new diagnosis of ADHD. Psychiatric Services, 61(8), 811–816. 10.1176/ps.2010.61.8.811 [DOI] [PubMed] [Google Scholar]
- DuBay M, Watson LR, & Zhang W (2018). In search of culturally appropriate autism interventions: Perspectives of Latino caregivers. Journal of Autism and Developmental Disorders, 48(5), 1623–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin MS, Maenner MJ, Meaney FJ, Levy SE, DiGuiseppi C, Nicholas JS, Kirby RS, Pinto-Martin JA, & Schieve LA (2010). Socioeconomic inequality in the prevalence of autism spectrum disorder: Evidence from a U.S. cross-sectional study. PLoS ONE, 5(7), e11551. 10.1371/journal.pone.0011551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyches TT, Wilder LK, Sudweeks RR, Obiakor FE, & Algozzine B (2004). Multicultural issues in autism. Journal of Autism and Developmental Disorders, 34(2), 211–222. https://doi.org/JADD.0000022611.80478.73 [DOI] [PubMed] [Google Scholar]
- Edgerton RB, & Karno M (1971). Mexican-American bilingualism and the perception of mental illness. Archives of General Psychiatry, 24(3), 286–290. [DOI] [PubMed] [Google Scholar]
- Ekas NV, Ghilain C, Pruitt M, Celimli S, Gutierrez A, & Alessandri M (2016). The role of family cohesion in the psychological adjustment of non-Hispanic white and Hispanic mothers of children with autism spectrum disorder. Research in Autism Spectrum Disorders, 21, 10–24. 10.1016/j.rasd.2015.09.002 [DOI] [Google Scholar]
- Ekas NV, Tidman L, & Timmons L (2019). Religiosity/spirituality and mental health outcomes in mothers of children with autism spectrum disorder: The mediating role of positive thinking. Journal of Autism and Developmental Disorders, 49(11), 4547–4558. [DOI] [PubMed] [Google Scholar]
- Estrada L, & Deris AR (2014). A phenomenological examination of the influence of culture on treating and caring for Hispanic children with autism. International Journal of Special Education, 28(3), 4–15. [Google Scholar]
- Gerber A, Morrow E, Sheinkopf SJ, & Anders T (2014). The Rhode Island consortium for autism research and treatment (RI-CART): A new statewide autism collaborative. Rhode Island Medical Journal (2013), 97(5), 31–34. [PMC free article] [PubMed] [Google Scholar]
- Gourdine RM, Baffour TD, & Teasley M (2011). Autism and the African American community. Social Work in Public Health, 26(4), 454–470. [DOI] [PubMed] [Google Scholar]
- Gray DE (1993). Perceptions of stigma: The parents of autistic children. Sociology of Health & Illness, 15(1), 102–120. [Google Scholar]
- Gray DE (2002). “Everybody just freezes. Everybody is just embarrassed”: Felt and enacted stigma among parents of children with high functioning autism. Sociology of Health & Illness, 24(6), 734–749. [Google Scholar]
- Hadziabdic E, & Hjelm K (2013). Working with interpreters: Practical advice for use of an interpreter in healthcare. International Journal of Evidence-Based Healthcare, 11(1), 69–76 [DOI] [PubMed] [Google Scholar]
- Hambly C, & Fombonne E (2012). The impact of bilingual environments on language development in children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(7), 1342–1352. [DOI] [PubMed] [Google Scholar]
- Harris B, Barton EE, & Albert C (2014). Evaluating autism diagnostic and screening tools for cultural and linguistic responsiveness. Journal of Autism and Developmental Disorders, 44(6), 1275–1287. 10.1007/s10803-013-1991-8 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, & Link BG (2013). Stigma as a fundamental cause of population health inequalities. American Journal of Public Health, 103(5), 813–821. 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert EB, & Koulouglioti C (2010). Parental beliefs about cause and course of their child’s autism and outcomes of their beliefs: A review of the literature. Issues in Comprehensive Pediatric Nursing, 33(3), 149–163. 10.3109/01460862.2010.498331 [DOI] [PubMed] [Google Scholar]
- Herlihy LE, Brooks B, Dumont-Mathieu T, Barton ML, Fein D, Chen CM, & Robins DL (2014). Standardized screening facilitates timely diagnosis of autism spectrum disorders in a diverse sample of low-risk toddlers. Journal of Developmental and Behavioral Pediatrics, 35(2), 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilton CL, Fitzgerald RT, Jackson KM, Maxim RA, Bosworth CC, Shattuck PT, Geschwind DH, & Constantino JN (2010). Brief report: Under-representation of African Americans in autism genetic research: A rationale for inclusion of subjects representing diverse family structures. Journal of Autism and Developmental Disorders, 40(5), 633–639. 10.1007/s10803-009-0905-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iadarola S, Pérez-Ramos J, Smith T, & Dozier A (2019). Understanding stress in parents of children with autism spectrum disorder: A focus on under-represented families. International Journal of Developmental Disabilities, 65(1), 20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ijalba E (2016). Hispanic immigrant mothers of young children with autism spectrum disorders: How do they understand and cope with autism? American Journal of Speech-Language Pathology, 25(2), 200–213. 10.1044/2015_AJSLP-13-0017 [DOI] [PubMed] [Google Scholar]
- Iland ED, Weiner I, & Murawski WW (2012). Obstacles faced by Latina mothers of children with autism. Californian Journal of Health Promotion, 10(SI-Latino), 25–36. [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ III, & Guzman R (2008). Critical issues in devleoping and following CBPR prinicples. In Minkler M & Wallerstein N (Eds.), Community-based participatory research for health: From process to outcomes (pp. 47–66). Jossey-Bass. [Google Scholar]
- Jarquin VG, Wiggins LD, Schieve LA, & Van Naarden-Braun K (2011). Racial disparities in community identification of autism spectrum disorders over time; Metropolitan Atlanta, Georgia, 2000–2006. Journal of Developmental and Behavioral Pediatrics, 32(3), 179–187. 10.1097/DBP.0b013e31820b4260 [DOI] [PubMed] [Google Scholar]
- Johnson N, & Van Hecke A (2015). Increasing autism awareness in inner-city churches: A brief report. Journal of Pediatric Nursing, 30(6), e69. 10.1016/j.pedn.2015.04.008 [DOI] [PubMed] [Google Scholar]
- Kalsner L, Twachtman‐Bassett J, Tokarski K, Stanley C, Dumont‐Mathieu T, Cotney J, & Chamberlain S (2018). Genetic testing including targeted gene panel in a diverse clinical population of children with autism spectrum disorder: Findings and implications. Molecular Genetics & Genomic Medicine, 6(2), 171–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krok D (2018). Examining the role of religion in a family setting: Religious attitudes and quality of life among parents and their adolescent children. Journal of Family Studies, 24(3), 203–218. [Google Scholar]
- Lajonchere CM, Wheeler BY, Valente TW, Kreutzer C, Munson A, Narayanan S, Kazemzadeh A, Cruz R, Martinez I, Schrager SM, Schweitzer L, Chklovski T & Hwang D (2016). Strategies for disseminating information on biomedical research on autism to Hispanic parents. Journal of Autism and Developmental Disorders, 46(3), 1038–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau AS (2006). Making the case for selective and directed cultural adaptations of evidence‐based treatments: Examples from parent training. Clinical Psychology: Science and Practice, 13(4), 295–310. [Google Scholar]
- Lewis-Fernández R, Aggarwal NK, Hinton L, Hinton DE, & Kirmayer LJ (Eds.). (2016). DSM-5 handbook on the cultural formulation interview. American Psychiatric Publishing. [Google Scholar]
- Lindsey EW (2018). Cultural values and coparenting quality in families of Mexican origin. Journal of Cross-Cultural Psychology, 49(10), 1523–1538. [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, Nolan KW, Thingvoll MA, Wade CM, & Fryer GE (2008). Disparities in diagnosis and access to health services for children with autism: Data from the national survey of children’s health. Journal of Developmental and Behavioral Pediatrics, 29(3), 152–160. 10.1097/DBP.0b013e318165c7a0 [DOI] [PubMed] [Google Scholar]
- Llorens A (2016). African American parents’ beliefs about autism spectrum disorders [Unpublished dissertation]. University of Houston. [Google Scholar]
- Lobar SL (2014). Family adjustment across cultural groups in autistic spectrum disorders. Advances in Nursing Science, 37(2), 174–186. 10.1097/ANS.0000000000000026 [DOI] [PubMed] [Google Scholar]
- Longtin SE, & Principe G (2016). The relationship between poverty level and urban African American parents’ awareness of evidence-based interventions for children with autism spectrum disorders: Preliminary data. Focus on Autism and Other Developmental Disabilities, 31(2), 83–91. 10.1177/1088357614522293 [DOI] [Google Scholar]
- Lopez K, & Magaña S (2018). Perceptions of family problems and pessimism among Latina and non-Latina White mothers raising children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 50, 2360–2374. [DOI] [PubMed] [Google Scholar]
- Lopez K, Magaña S, Xu Y, & Guzman J (2018). Mother’s reaction to autism diagnosis: A qualitative analysis comparing Latino and White parents. Journal of Rehabilitation, 84(1), 41–50. [Google Scholar]
- Lovelace TS, Tamayo S, & Robertson RE (2018). Experiences of African American mothers of sons with autism spectrum disorder: Lessons for improving service delivery. Education and Training in Autism and Developmental Disabilities, 53(1), 3–16. [Google Scholar]
- Magaña S, Li H, Miranda E, & Paradiso de Sayu R (2015). Improving health behaviours of Latina mothers of youths and adults with intellectual and developmental disabilities. Journal of Intellectual Disability Research, 59(5), 397–410. [DOI] [PubMed] [Google Scholar]
- Magaña S, Lopez K, Aguinaga A, & Morton H (2013). Access to diagnosis and treatment services among Latino children with autism spectrum disorders. Intellectual and Developmental Disabilities, 51(3), 141–153. 10.1352/1934-9556-51.3.141 [DOI] [PubMed] [Google Scholar]
- Magaña S, Lopez K, & Machalicek W (2017). Parents taking action: A psycho‐educational intervention for Latino parents of children with autism spectrum disorder. Family Process, 56(1), 59–74. 10.1111/famp.12169 [DOI] [PubMed] [Google Scholar]
- Magaña S, Parish SL, Rose RA, Timberlake M, & Swaine JG (2012). Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Intellectual and Developmental Disabilities, 50(4), 287–299. 10.1352/1934-9556-50.4.287 [DOI] [PubMed] [Google Scholar]
- Magaña S, Parish SL, & Son E (2015). Have racial and ethnic disparities in the quality of health care relationships changed for children with developmental disabilities and ASD? American Journal on Intellectual and Developmental Disabilities, 120(6), 504–513. 10.1352/1944-7558-120.6.504 [DOI] [PubMed] [Google Scholar]
- Magaña S, & Smith MJ (2006). Psychological distress and well-being of Latina and non-Latina White mothers of youth and adults with an autism spectrum disorder: Cultural attitudes towards coresidence status. American Journal of Orthopsychiatry, 76(3), 346–357. 10.1037/0002-9432.76.3.346 [DOI] [PubMed] [Google Scholar]
- Mandell DS, Ittenbach RF, Levy SE, & Pinto-Martin J (2007). Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. Journal of Autism and Developmental Disorders, 37(9), 1795–1802. 10.1007/s10803-006-0314-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell DS, Listerud J, Levy SE, & Pinto-Martin J (2002). Race differences in the age at diagnosis among Medicaid-eligible children with autism. Journal of the American Academy of Child & Adolescent Psychiatry, 41(12), 1447–1453. 10.1097/00004583-200212000-00016 [DOI] [PubMed] [Google Scholar]
- Mandell DS, & Novak M (2005). The role of culture in families’ treatment decisions for children with autism spectrum disorders. Mental Retardation & Developmental Disabilities Research Reviews, 11(2), 110–115. 10.1002/mrdd.20061 [DOI] [PubMed] [Google Scholar]
- Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, Durkin MS, Giarelli E, Morrier MJ, Nicholas JS, Pinto-Martin JA, Shattuck PT, Thomas KC, Yeargin-Allsopp M, & Kirby RS (2009). Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health, 99(3), 493–498. 10.2105/AJPH.2007.131243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy AD (2018). Autism spectrum disorder diagnosis from the African American parents’ perspective [Unpublished doctoral dissertation]. The University of Texas at Austin. [Google Scholar]
- McLeod JD, & DiSabatino L (2019). Structured variation in parental beliefs about autism. Journal of Health and Social Behavior, 60(1), 36–54. 10.1177/0022146518820581. [DOI] [PubMed] [Google Scholar]
- Moodley R, & Sutherland P (2010). Psychic retreats in other places: Clients who seek healing with traditional healers and psychotherapists. Counselling Psychology Quarterly, 23(3), 267–282. [Google Scholar]
- Moody EJ, Harris B, Zittleman L, Nease D, & Westfall JM (2019). It’s time for a change!: The Appreciative Inquiry/Bootcamp Translation to address disparities in the Latino community with autism spectrum disorders. Cultural Diversity & Ethnic Minority Psychology, 25(1), 113–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, & Miranda J (2007). Does stigma keep poor young immigrant and U.S.-born African and Latina women from seeking mental health care? Psychiatric Services, 58(12), 1547–54 10.1176/ps.2007.58.12.1547 [DOI] [PubMed] [Google Scholar]
- Neuhaus E, Beauchaine TP, Bernier RA, & Webb SJ (2018). Child and family characteristics moderate agreement between caregiver and clinician report of autism symptoms. Autism Research, 11(3), 476–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowell KP, Brewton CM, Allain E, & Mire SS (2015). The influence of demographic factors on the identification of autism spectrum disorder: A review and call for research. Review Journal of Autism and Developmental Disorders, 2, 300–309. [Google Scholar]
- Ohashi JK, Mirenda P, Marinova-Todd S, Hambly C, Fombonne E, Szatmari P, Bryson S, Roberts W, Smith I, Vaillancourt T, Volden J, Waddell C, Zwaigenbaum L, Georgiades S, Duku E, & Thompson A (2012). Comparing early language development in monolingual- and bilingual-exposed young children with autism spectrum disorders. Research in Autism Spectrum Disorders, 6(2), 890–897. [Google Scholar]
- Parish S, Magaña S, Rose R, Timberlake M, & Swaine JG (2012). Health care of Latino children with autism and other developmental disabilities: Quality of provider interaction mediates utilization. American Journal on Intellectual and Developmental Disabilities, 117(4), 304–315. 10.1352/1944-7558-117.4.304 [DOI] [PubMed] [Google Scholar]
- Parks SK (2017). Parenting autism: An exploratory study of the culture and experience of African-American parents of children diagnosed with autism [Unpublished doctoral dissertation]. Creighton University. [Google Scholar]
- Pearson JN, & Meadan H (2018). African American parents’ perceptions of diagnosis and services for children with autism. Education and Training in Autism and Developmental Disabilities, 53(1), 17–32. [Google Scholar]
- Petersen JM, Marinova-Todd SH, & Mirenda P (2012). Brief report: An exploratory study of lexical skills in bilingual children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 42(7), 1499–1503. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2015, September 28). Modern immigration wave brings 59 million to U.S., driving population growth and change through 2065: Views of immigration’s impact on U.S. society mixed [Report]. https://www.pewresearch.org/hispanic/2015/09/28/modern-immigration-wave-brings-59-million-to-u-s-driving-population-growth-and-change-through-2065/
- Pierce NP, O’Reilly MF, Sorrells AM, Fragale CL, White PJ, Aguilar JM, & Cole HA (2014). Ethnicity reporting practices for empirical research in three autism-related journals. Journal of Autism and Developmental Disorders, 44(7), 1507–1519. 10.1007/s10803-014-2041-x [DOI] [PubMed] [Google Scholar]
- Ratto AB, Reznick JS, & Turner-Brown L (2016). Cultural effects on the diagnosis of autism spectrum disorder among Latinos. Focus on Autism and Other Developmental Disabilities, 31(4), 275–283. 10.1177/1088357615587501 [DOI] [Google Scholar]
- Reyes NM, Lindly OJ, Chavez AE, Folan A, Macias K, Smith KA, Reynolds A, & Zuckerman K (2018). Maternal beliefs about autism: A link between intervention services and autism severity in white and latino mothers. Research in Autism Spectrum Disorders, 51, 38–48. 10.1016/j.rasd.2018.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers-Dulan J, & Blacher J (1995). African American families, religion, and disability: A conceptual framework. Mental Retardation, 33(4), 226–238. [PubMed] [Google Scholar]
- Salkas K, Magaña S, Marques I, & Mirza M (2016). Spirituality in Latino families of children with autism spectrum disorder. Journal of Family Social Work, 19(1), 1–18. 10.1080/10522158.2015.1114060 [DOI] [Google Scholar]
- Schieve LA, Boulet SL, Blumberg SJ, Kogan MD, Yeargin-Allsopp M, Boyle CA, Visser SN, & Rice C (2012). Association between parental nativity and autism spectrum disorder among US-born non-Hispanic White and Hispanic children, 2007 national survey of children’s health. Disability and Health Journal, 5(1), 18–25. 10.1016/j.dhjo.2011.09.001 [DOI] [PubMed] [Google Scholar]
- Shattuck PT, Wagner M, Narendorf S, Sterzing P, & Hensley M (2011). Post-high school service use among young adults with an autism spectrum disorder. Archives of Pediatrics & Adolescent Medicine, 165(2), 141–146. 10.1001/archpediatrics.2010.279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh JS, & Bunyak G (2019). Autism disparities: A systematic review and meta-ethnography of qualitative research. Qualitative Health Research, 29(6), 796–808. [DOI] [PubMed] [Google Scholar]
- Stahmer AC, Vejnoska S, Iadarola S, Straiton D, Segovia FR, Luelmo P, Morgan EH, Lee HS, Javed A, Bronstein B, Hochheimer S, Cho EM, Aranbarri A, Mandell D, Hassrick E, Smith T, & Kasari C (2019). Caregiver voices: Cross-cultural input on improving access to autism services. Journal of Racial and Ethnic Health Disparities, 6(4), 752–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiggelbout AM, Van der Weijden T, De Wit MP, Frosch D, Légaré F, Montori VM, Trevena L, & Elwyn G (2012). Shared decision making: Really putting patients at the centre of healthcare. The BMJ, 344, e256. [DOI] [PubMed] [Google Scholar]
- Strug DL, Mason SE, & Auerbach C (2009). How older Hispanic immigrants in New York City cope with current traumatic stressors: Practice implications. Journal of Gerontological Social Work, 52(5), 503–516. [DOI] [PubMed] [Google Scholar]
- Umezawa Y, Lu Q, You J, Kagawa-Singer M, Leake B, & Maly R (2012). Belief in divine control, coping, and race/ethnicity among older women with breast cancer. Annals of Behavioral Medicine, 44(1), 21–32. 10.1007/s12160-012-9358-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voelkel H, LeCroy CW, Williams LR, & Holschuh J (2013). The full spectrum: Hispanic understanding of autism. Best Practices in Mental Health: An International Journal, 9(1), 31–46. [Google Scholar]
- West EA, Travers JC, Kemper TD, Liberty LM, Cote DL, McCollow MM, & Stansberry Brusnahan LL (2016). Racial and ethnic diversity of participants in research supporting evidence-based practices for learners with autism spectrum disorder. Journal of Special Education, 50(3), 151–163. 10.1177/0022466916632495 [DOI] [Google Scholar]
- Williams ME, Atkins M, & Soles T (2009). Assessment of autism in community settings: Discrepancies in classification. Journal of Autism and Developmental Disorders, 39(4), 660–669. 10.1007/s10803-008-0668-1 [DOI] [PubMed] [Google Scholar]
- Williams TV, Hartmann K, Paulson JF, Raffaele CT, & Urbano MR (2019). Life after an autism spectrum disorder diagnosis: A comparison of stress and coping profiles of African American and Euro-American caregivers. Journal of Autism and Developmental Disorders, 49(3), 1024–1034. [DOI] [PubMed] [Google Scholar]
- Willis K, Timmons L, Pruitt M, Schneider HL, Alessandri M, & Ekas NV (2016). The relationship between optimism, coping, and depressive symptoms in Hispanic mothers and fathers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(7), 2427–2440. [DOI] [PubMed] [Google Scholar]
- Wolery M, & Garfinkle A (2002). Measures in intervention research with young children who have autism. Journal of Autism and Developmental Disorders, 32(5), 463–478. https://doi.org/1020598023809 [DOI] [PubMed] [Google Scholar]
- Yeh M, Hough RL, McCabe K, Lau A, & Garland A (2004). Parental beliefs about the causes of child problems: Exploring racial/ethnic patterns. Journal of the American Academy of Child and Adolescent Psychiatry, 43(5), 605–612. 10.1097/00004583-200405000-00014 [DOI] [PubMed] [Google Scholar]
- Zayas LH, & Solari F (1994). Early childhood socialization in Hispanic families: Context, culture, and practice implications. Professional Psychology: Research and Practice, 25(3), 200–206. [Google Scholar]
- Zuckerman KE, Lindly OJ, Reyes NM, Chavez AE, Cobian M, Macias K, Reynolds AM, & Smith KA (2018). Parent perceptions of community autism spectrum disorder stigma: Measure validation and associations in a multi-site sample. Journal of Autism and Developmental Disorders, 48, 3199–3209. 10.1007/s10803-018-3586-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Lindly OJ, Reyes NM, Chavez AE, Macias K, Smith KN, & Reynolds A (2017). Disparities in diagnosis and treatment of autism in Latino and non-Latino White families. Pediatrics, 139(5), e20163010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Lindly OJ, & Sinche B (2016). Parent beliefs about the causes of learning and developmental problems among children with autism spectrum disorder: Results from a national survey. American Journal on Intellectual and Developmental Disabilities, 121(5), 432–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Lindly OJ, Sinche BK, & Nicolaidis C (2015). Parent health beliefs, social determinants of health, and child health services utilization among US school-age children with autism. Journal of Developmental and Behavioral Pediatrics, 36(3), 146–157. 10.1097/DBP.0000000000000136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Mattox K, Donelan K, Batbayar O, Baghaee A, & Bethell C (2013). Pediatrician identification of Latino children at risk for autism spectrum disorder. Pediatrics, 132(3), 445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Sinche B, Cobian M, Cervantes M, Mejia A, Becker T, & Nicolaidis C (2014). Conceptualization of autism in the Latino community and its relationship with early diagnosis. Journal of Developmental and Behavioral Pediatrics, 35(8), 522–532. 10.1097/DBP.0000000000000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Sinche B, Mejia A, Cobian M, Becker T, & Nicolaidis C (2014). Latino parents’ perspectives on barriers to autism diagnosis. Academic Pediatrics, 14(3), 301–308. 10.1016/j.acap.2013.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]


