Abstract
Background:
Periodontal disease also called gum disease is a serious gum infection that damages the soft tissue and, without treatment, can destroy the bone and result in different types of alveolar bone defects. That means that periodontal pockets are present and registered only in case of periodontal disease.
Objective:
The aim of this study is to observe the effect of 4MATRIX and PRF application in the treatment of infrabone defect over case report.
Material and Methods:
By using regenerative surgical periodontal therapy 4MATRIX bone substituent with 4MATRIX and PRF for elimination of deep pockets or periodontal disease was performed among patient at selected sites.
Case report:
The patient’s periodontal condition has followed 3, 6- and 9-month period. The patient’s oral health-related quality of life showed a marked improvement after periodontal surgery therapy.
Conclusion:
Additional application of PRF and 4MATRIX in conventional surgical treatment of infrabone defects showed decreased values of PPD and CAL registered in the segment treated after 9 months of treatment.
Keywords: Chronic periodontitis, periodontal regeneration, 4 MATRIX, PRF
1. BACKGROUND
Periodontal disease also called gum disease is a serious gum infection that damages the soft tissue and, without treatment, can destroy the bone and result in different types of alveolar bone defects. The Periodontal disease as a Pathology by which are sick a lot of peoples and especially adults is not new, and the evidence of alveolar bone loss affecting human remains dating from around 700,000 years ago in a lot of case reports (1). Basic pathognomonic signs of periodontal disease and the most important clinical sign of it is the presence of periodontal pockets. As pathology periodontal disease is present in the general population (2, 3).
A lot of different species of bacteria are present in the dental plaque, and they are capable of inducing an inflammatory response of the periodontal tissues (4). In the patients who are more sensitive and their general condition is down, this chronic inflammation will induce a breakdown of the periodontal ligament and the surrounding alveolar bone resulting in the formation of periodontal pockets around the roots thus causing periodontitis (5).
The first step of this treatment is to mechanically clean periodontal pockets from bacteria (debridement). When there are present the big and deep periodontal pockets and there is impossible to get access to the deepest portions of the pockets and properly clean them just mechanically and to reduce the depth of pockets, than can be indicated surgery as a way of treatment (6). We have found in the literature many preparations that are used as bone substitutes, but also as stimulators of osteoblasts to produce bone matrix (7-9).
One of the most important interventions recommended in this domain is guided tissue regeneration (GTR/GBR). To achieve more satisfactory effects in periodontal surgery, a variety of treatment procedures are applied involving the use of bone substitutes of different origins (auto transplants, allografts, and alloplastic materials) (10, 11).
2. OBJECTIVE
The aim of this study is to observe the effect of 4MATRIX and PRF application in the treatment of infrabone defect over case report.
3. CASE REPORT
1. Baseline examination
Forty one years old patient has visited the Clinical Dentistry University Center of Pristina with the complaint of gingival swelling, periodontitis, and depth pockets in upper jaw in region of right and left premolars region.
Symptoms registered at the first examination are: redness, swelling of the gingiva and mild luxation of the teeth as objective clinical signs. The patient was monitored every 3 months. in March, July and November. Occasional deteriorations and improvements in periodontal status have been reported in the patient follow-up period.
The following procedures are undertaken for therapeutic purposes: initial periodontal therapy, periodontal regenerative therapy, treatment for recovery of oral function and treatment for recovery of oral function (Table 1).
Table 1. Monitoring of the undertaken procedures during the first examination, after 3, 6 and 9 months.
| December 2019 | March 2020 | July 2020 | November 2020 | |
|---|---|---|---|---|
| Intervention | ||||
| Initial periodontal therapy | ||||
| Plaque control | + | |||
| Quadrant Scaling and root planning | + | |||
| Oral hygiene instruction | + | |||
| Professional tooth cleaning | + | |||
| First Reevaluation | + | |||
| Plaque control | + | |||
| Oral hygiene instruction | + | |||
| Professional tooth cleaning | + | |||
| Surgical periodontal Therapy | + | |||
| Open flap debridement (#15,16) | + | |||
| Regenerative therapy with 4MATRIX ( #15,16) | + | |||
| Regenerative therapy with 4MATRIX+PRF membrane | + | |||
| Second Reevaluation | ||||
| Supportive periodontal Therapy | + | |||
| Oral hygiene instruction | + | |||
| Professional tooth cleaning | + | |||
| Third Reevaluation | ||||
| Supportive periodontal Therapy | + | |||
| Oral hygiene instruction | + | |||
| Professional tooth cleaning | + |
a) Initial periodontal therapy
After the first visit, we underwent initial therapy, which included: plaque control, Quadrant Scaling and root planning, Oral hygiene instruction and Professional tooth cleaning.
Initial periodontal therapy consisted mainly of tooth brushing instruction what is mean plaque home control by patient, quadrant scaling (# 13, 14, 15, 16). An initial examination revealed that around 45 % of sites had a probing depth (PD) of >4 mm and 30 % of bleeding on probing.
Radiographic examination revealed bone resorption and infrabony defects as far as the root apex in between 14 -15, 15-16, and 24-25, 25-26, vertical bone resorption in both sites and horizontal resorption in other regions in generally. Based on clinical examination and diagnosis of chronic periodontitis, the initial periodontal therapy was carried out following the periodontal surgery procedures and regenerative therapy.
2. Diagnosis
Table 2. Periodontal status at first examination, after 3, 6 and 9 months of treatment. Legend: PI - dental plaque deposits; GI- gingival inflammation; BOP - gingival bleeding; PPD - periodontal pocket CAL- clinical attachment loss.
| First examination | After 3 months | After 6 months | After 9 months | |||||
|---|---|---|---|---|---|---|---|---|
| Region | 14-15 | 15-16 | 14-15 | 15-16 | 14-15 | 15-16 | 14-15 | 15-16 |
| PI | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| GI | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| BOP | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| PPD | 4 | 4,5 | 4 | 4 | 4 | 4 | 3,5 | 4 |
| CAL | 4 | 4,5 | 4 | 4 | 4 | 4 | 3 | 3,5 |
| Region | 24-25 | 25-26 | 24-25 | 25-26 | 24-25 | 25-26 | 24-25 | 25-26 |
| PI | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| GI | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| BOP | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| PPD | 4 | 4 | 4 | 4 | 4 | 4 | 3,5 | 3,5 |
| CAL | 4 | 4,5 | 4 | 4 | 3,5 | 3,5 | 3 | 3 |
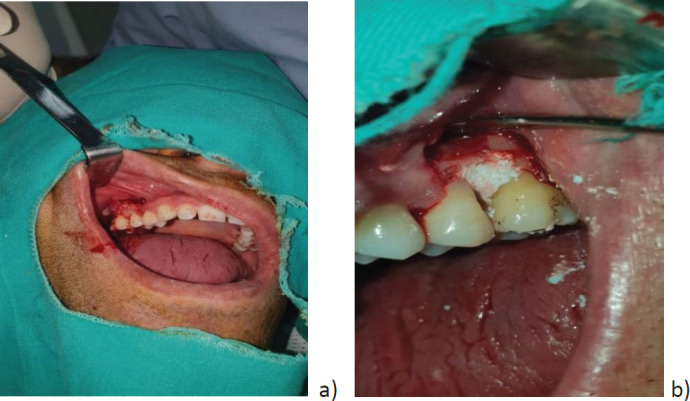
PD of> 4 mm during the first re-evaluation in addition to the conducted one plaque control, Quadrant Scaling and root planning, Oral hygiene instruction and Professional tooth cleaning. Oral hygiene instruction and Professional tooth cleaning, flap intervention was performed bilaterally in the upper jaw left and right (Figure 1). Bone substitute 4MATRIX is applied on the right, and 4MATRIX and PRF membrane are placed on the left of the intervened region (Figure 2).
Figure 1. Flap intervention: a) open flap in between 25,26; b) open flap in between 15,16.
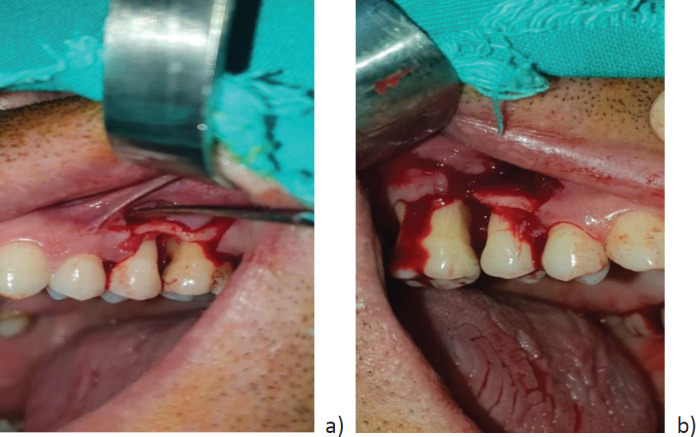
Figure 2. Flap intervention and artificial bone placed: a)14,15; b) 25-26;
3. Periodontal regenerative therapy
The first assessment of periodontal status was made by monitoring the dental plaque index (DP), gingival bleeding index (BOP), periodontal pocket depth (DP) and clinical attachment loss (CAL). In the right upper region 14-15 and 15-16 the bone substituent 4MATRIX was applied, and in the left upper quadrant (24-25, 25-26) the defect was filled with 4MATRIX and PRF membrane. Regenerative therapy with 4MATRIX bone substituent and PRF membrane by own blood of patient was then performed on tooth (24-25, 25-26).
4. Treatment for recovery of oral function
At 3 months after postoperatively there was no significant difference in bone formation in periodontal pockets where was performed 4MATRIX and PRF membrane. Six months later the finding was identical in the two treated regions of the upper jaw. After 9 months of the intervention, minimal but present bone gain is evident.
5. Supportive periodontal therapy
On re-monitoring, significantly reduced plaque accumulation, reduced gingival inflammation, but without correction of periodontal pocket depth and clinical attachment loss is evident. After 6 months the condition of the gingiva followed by gingival inflammation (GI) and gingival bleeding (BOP) was stable. After 9 months, a stable gingival periodontal finding was recorded. In this phase of re-evaluation, a PD finding was registered on the side treated with 4MATRIX and PRF membrane for CAL = 3 mm in the region 25-26 (Figure 3).
Figure 3. Periodontal pockets.
Following the findings obtained in the intervened regions with 4MATRIX bone substitute without PRF application (right) and left with 4MATRIX and PRF it is evident that during the control examinations after 3, 6 and 9 months PD, GI and BOP are unchanged. Certain changes are evident in different treated regions with 4MATRIX and 4MATRIX and PRF for DP and CAL values. The only improvement was observed in the values for DP and CAL after 9 months of the therapy in the region 14-15 (DP = 3.5, CAL = 3); 15-16 (DP = 4, CAL = 3, 5); where 4MATRIX bone substitute is applie. In the region 24-25 (DP = 3.5, CAL = 3.5); 25-26 (DP = 3, CAL = 3); where 4MATRIX is applied in combination with PRF. The results show modest clinically better therapeutic effects in the 4MATRIX and PRF-treated segment.
4. DISCUSSION
In the last twenty years, periodontal therapy has progressed significantly, from formerly used resective methods, to principles of preservation and regeneration of periodontal tissues which are used today Bembi et al., found no significant difference in the results of treatment with two materials, NovaBone Putty– CMF, and Frios Algipore, followed by clinical parameters of probe depth and clinical attachment level (12).
Therefore the results of the study of Gojkov-Vukelic et all. by using Maxresorb (Bottis dental) which is composed of 60% slowly resorbing hydroxyapatite (HA) and 40% fast resorbing beta-tricalcium phosphate (β-TCP) as regenerative grafts in periodontal pockets showed significant reduction in probing depth for both groups of patients (treated by open flap surgery and treated by open flap surgery in addition with Maxresorb), one and six months after the performed surgical therapy (13). Also the results of other papers which are talking about the other biomaterials as Bio Oss, .showed significant improvement for clinical parameters at sites treated with BioSS compared to control sites (14).
Experiences were also emphasized where PRF was used in periodontal regeneration BiOss, Emdogain (15-17). Though the PRF could be used as a safe and natural method for the correction of certain tissues, many researchers and clinicians in private practice tried to use PRF to regenerate the periodontal defects (18-20). Currently, many randomized clinical studies are available to compare the applied PRF (after an open curettage as a standard method or combined with other techniques) with other golden standards, such as EMD Matrix (21).
The goal of this treatment approach is healing by repair without formation of new periodontal attachment (22). The main parameters that we check after regenerative therapy are plaque index (PI), papillary bleeding index (PBI), and probing pocket depth (PPD). The ideal treatment would be to recover the periodontal tissues that have been lost (periodontal tissue regeneration). Several surgical techniques have been developed in the attempt to regenerate periodontal tissues including guided tissue regeneration (GTR), bone grafting (BG) and the use of the enamel matrix derivative (EMD). All these treatments have been shown to have the potential to regenerate at least some periodontal attachment in humans (23).
Periodontal regeneration mediated by EMD is based on a different concept. The enamel matrix is composed of a number of proteins, 90 % of which is amelogenin. One year after treatment, enamel matrix derivative (EMD) showed statistically significant improvements in probing attachment levels (PAL) (1,3mm) and probing pocket depths (PPD) reduction (1mm) in comparison with flap surgery. Henceforth, EMD seems simpler to use, may not need antibiotic coverage and does not need a second surgical intervention (if compared with non - resorptive barriers). In addition, no postoperative infections or adverse events were observed with EMD versus two cases of infection (not statistically significant) in the GTR group.
The findings from current case report presented identical results, by correction of periodontal pockets and clinical loss of attachment after 9 months of treatment with 4MATRIX substitute supplement PRF.
Platelet-rich-Plasma (PRP) is autologous plasma which has been enriched with platelets and leukocytes in addition to jellifying agents, growth factors, cytokines, bovine thrombin and anticoagulants. Comparing with PRF, PRP has some limitations because, the growth factors are released for a very short period of time, also the bovine clotting factors may react with human clotting factors to give rise to bleeding.
For complete regeneration, the distribution of growth factors in damaged areas of the destructed bone has great significance for the potential effects of bone transplants. PRF is considered to be the second generation of concentrated platelets, consisting of concentrated platelets that emit different growth factors, which are much more demanding for the bone grains, while useful in the healing process.
Roughly, during the process of healing natural wounds, blood plays an important role in accelerating tissue regeneration by providing various cells, growth factors, cytokines, and coagulation factors. Supraphysiologic doses of platelets (Platelet Plasma) have been developed to increase platelet counts at defect sites. However, additional use of substituent is necessary to stimulate and emphasize regenerative processes, although the assessment of treatment in this study is considered not optimal (24).
An alternative method for the production of a natural autologous PDGF was first introduced using PRP, an autologous growth factor of growth derived from typical platelets after centrifugation, which are mostly used for clinical and research purposes (25, 26).
PRP was first used by many doctors in the field of oral and maxillofacial surgery and has since been widely used in the regeneration of defects, mainly in combination with bone grafts (27).
4. CONCLUSION
Additional application of PRF and 4MATRIX in conventional surgical treatment of infrabone defects showed decreased values of PPD and CAL registered in the segment treated after 9 months of treatment.
Patient Consent Form:
The patient was informed orally on the aim of the study and the written informed consent was obtained.
Author's contribution:
All authors contributed correspondingly to this work and they approved the final proofreading.
Conflict of interest:
The authors declare no conflict of interest.
Financial support and sponsorship:
This research received no external funding.
REFERENCES
- 1.Dentino A, Lee S, Mailhot J, Hefti AF. Principles of periodontology. Periodontol 2000. 2013;61(1):16–53. doi: 10.1111/j.1600-0757.2011.00397.x. [DOI] [PubMed] [Google Scholar]
- 2.Greenstein G, Lamster I. Changing periodontal paradigms: therapeutic implications. Int J Periodontics Restorative Dent. 2000;20(4):336–357. [PubMed] [Google Scholar]
- 3.Glickman I, Smulow JB. Philadelphia: Saunders; 1974. Periodontal diseas: clinical, radiographic and histopathologic features. [Google Scholar]
- 4.Esposito M, Grusovin MG, Papanikolaou N, Coulthard P, Worthington HV. Enamel matrix derivative (Emdogain(R)) for periodontal tissue regeneration in intrabony defects. Cochrane Database Syst Rev. 2009;2009(4):CD003875. doi: 10.1002/14651858.CD003875.pub35. Published 2009 Oct 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366(9499):1809–1820. doi: 10.1016/S0140-6736(05)67728-8. [DOI] [PubMed] [Google Scholar]
- 6.Bowers GM, Chadroff B, Carnevale R, et al. Histologic evaluation of new attachment apparatus formation in humans. Part II. J Periodontol. 1989;60(12):675–682. doi: 10.1902/jop.1989.60.12.675. [DOI] [PubMed] [Google Scholar]
- 7.Aimetti M, Ferrarotti F, Mariani G, Fratini A, Giraudi M, Romano F. Enamel Matrix Derivative Proteins in Combination with a Flapless Approach for Periodontal Regeneration of Intrabony Defects: A 2-Year Prospective Case Series. Int J Periodontics Restorative Dent. 2016;36(6):797–805. doi: 10.11607/prd.2842. [DOI] [PubMed] [Google Scholar]
- 8.Staubli N, Schmidt JC, Buset SL, et al. Traditional or regenerative periodontal surgery?-a comparison of the publications between two periodontal journals over time. Clin Oral Investig. 2018;22(1):29–46. doi: 10.1007/s00784-017-2159-2. [DOI] [PubMed] [Google Scholar]
- 9.Del Corso M, Vervelle A, Simonpieri A, et al. Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 1: Periodontal and dentoalveolar surgery. Curr Pharm Biotechnol. 2012;13(7):1207–1230. doi: 10.2174/138920112800624391. [DOI] [PubMed] [Google Scholar]
- 10.Reynolds MA, Kao RT, Camargo PM, et al. Periodontal regeneration - intrabony defects: a consensus report from the AAP Regeneration Workshop. J Periodontol. 2015;86(2 Suppl):S105–S107. doi: 10.1902/jop.2015.140378. [DOI] [PubMed] [Google Scholar]
- 11.Needleman IG, Worthington HV, Giedrys-Leeper E, Tucker RJ. Guided tissue regeneration for periodontal infra-bony defects. Cochrane Database Syst Rev. 2006;(2):CD001724. doi: 10.1002/14651858.CD001724.pub2. Published 2006 Apr 19. [DOI] [PubMed] [Google Scholar]
- 12.Bembi NN, Bembi S, Mago J, Baweja GK, Baweja PS. Comparative Evaluation of Bioactive Synthetic NovaBone Putty and Calcified Algae-derived Porous Hydroxyapatite Bone Grafts for the Treatment of Intrabony Defects. Int J Clin Pediatr Dent. 2016;9(4):285–290. doi: 10.5005/jp-journals-10005-1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gojkov-Vukelic M, Hadzic S, Pasic E. Evaluation of Efficacy of Surgical Periodontal Therapy with the Use of Bone Graft in the Treatment of Periodontal Intrabony Defects. Med Arch. 2017;71(3):208–211. doi: 10.5455/medarh.2017.71.208-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gokhale ST, Dwarakanath CD. The use of a natural osteoconductive porous bone mineral (Bio-Oss™) in infrabony periodontal defects. J Indian Soc Periodontol. 2012;16(2):247–252. doi: 10.4103/0972-124X.99270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lei L, Yu Y, Ke T, Sun W, Chen L. The Application of Three-Dimensional Printing Model and Platelet-Rich Fibrin Technology in Guided Tissue Regeneration Surgery for Severe Bone Defects. J Oral Implantol. 2019;45(1):35–43. doi: 10.1563/aaid-joi-D-17-00231. [DOI] [PubMed] [Google Scholar]
- 16.Proksch S, Bittermann G, Vach K, Nitschke R, Tomakidi P, Hellwig E. hMSC-Derived VEGF Release Triggers the Chemoattraction of Alveolar Osteoblasts. Stem Cells. 2015;33(10):3114–3124. doi: 10.1002/stem.2119. [DOI] [PubMed] [Google Scholar]
- 17.Zhang YF. Bioinductive biomaterials for periodontal regeneration. Zhonghua Kou Qiang Yi Xue Za Zhi. 2017;52(10):615–619. doi: 10.3760/cma.j.issn.1002-0098.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Guo T, Nie R, Xin X, et al. Tissue preservation through socket-shield technique and platelet-rich fibrin in immediate implant placement: A case report. Medicine (Baltimore) 2018;97(50):e13175. doi: 10.1097/MD.0000000000013175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou J, Li X, Sun X, et al. Bone regeneration around immediate placed implant of molar teeth with autologous platelet-rich fibrin: Two case reports. Medicine (Baltimore) 2018;97(44):e13058. doi: 10.1097/MD.0000000000013058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joshi AA, Padhye AM, Gupta HS. Platelet derived growth factor-BB levels in gingival crevicular fluid of localized intrabony defect sites treated with platelet rich fibrin membrane or collagen membrane containing recombinant human platelet derived growth factor-BB: A randomized clinical and biochemical study. J Periodontol. 2019;90(7):701–708. doi: 10.1002/JPER.18-0496. [DOI] [PubMed] [Google Scholar]
- 21.Shirakata Y, Miron RJ, Shinohara Y, et al. Healing of two-wall intra-bony defects treated with a novel EMD-liquid-A pre-clinical study in monkeys. J Clin Periodontol. 2017;44(12):1264–1273. doi: 10.1111/jcpe.12825. [DOI] [PubMed] [Google Scholar]
- 22.Bowers GM, ChadroffB , Carnevale R, Mellonig J, Corio R, Emerson J, et al. Histologic evaluation of new attachment apparatus formation in humans. Part 1. J of Periodontol. 1989;60(12):664–674. doi: 10.1902/jop.1989.60.12.664. [DOI] [PubMed] [Google Scholar]
- 23.Bowers GM, Chadroff B, Carnevale R, Mellonig J, Corio R, Emerson J, Stevens M, Romberg E. Histologic evaluation of new attachment apparatus formation in humans. Part II. J Periodontol. 1989;60(12):675–682. doi: 10.1902/jop.1989.60.12.675. [DOI] [PubMed] [Google Scholar]
- 24.Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89(3):219–229. doi: 10.1177/0022034509359125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mazzucco L, Borzini P, Gope R. Platelet-derived factors involved in tissue repair-from signal to function. Transfus Med Rev. 2010;24(3):218–234. doi: 10.1016/j.tmrv.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 26.Harnack L, Boedeker RH, Kurtulus I, Boehm S, Gonzales J, Meyle J. Use of platelet-rich plasma in periodontal surgery - a prospective randomised double blind clinical trial. Clin Oral Investig. 2009;13(2):179–187. doi: 10.1007/s00784-008-0223-7. [DOI] [PubMed] [Google Scholar]
- 27.Yassibag-Berkman Z, Tuncer O, Subasioglu T, Kantarci A. Combined use of platelet-rich plasma and bone grafting with or without guided tissue regeneration in the treatment of anterior interproximal defects. J Periodontol. 2007;78(5):801–809. doi: 10.1902/jop.2007.060318. [DOI] [PubMed] [Google Scholar]



