Abstract
US state legislatures have proposed laws to prohibit abortion once the earliest embryonic electrical activity is detectable (fetal “heartbeat”). On average, this occurs roughly 6 wk after the last menstrual period. To be eligible for abortion, people must recognize pregnancy very early in gestation. The earliest symptom of pregnancy is a missed period, and irregular menstrual cycles—which occur frequently—can delay pregnancy detection past the point of fetal cardiac activity. In our analysis of 1.6 million prospectively recorded menstrual cycles, cycle irregularity was more common among young women, Hispanic women, and women with common health conditions, such as diabetes and polycystic ovary syndrome. These groups face physiological limitations in detecting pregnancy before fetal cardiac activity. Restriction of abortion this early in gestation differentially affects specific population subgroups, for reasons outside of individual control.
Keywords: abortion policy, pregnancy, menstruation
The Texas state legislature has prohibited abortion following fetal cardiac activity, and other state legislatures are debating similar laws. Electrical pulsing occurs as early as 23 d after fertilization (1) or, for people with 4-wk menstrual cycles, ∼6 wk after start of the previous menses. Socioeconomic barriers can limit the discovery of pregnancy this early (2). Equally important—but less often discussed—are limits imposed by menstrual variability.
The earliest symptom of pregnancy is typically a missed period—that is, the failure to menstruate around the expected date. (Over-the-counter pregnancy tests do not reach optimum sensitivity until after the expected menses.) Normal cycle length is often assumed to be 28 d, but there is substantial natural variation in menstrual cycle lengths (3–6). Environmental exposures, illness, and disease can add further irregularity (7).
The timing of ovulation and conception during the cycle also varies greatly, and people with irregular cycles can conceive as early as 12 d into their cycle (6). For these people, embryo development can easily reach fetal cardiac activity by the time of a missed menses. This creates a physiological obstacle to abortion eligibility. We describe how this disadvantage varies among people in the United States. We do not attempt to uncover biological mechanisms for cycle differences; instead we describe group differences in menses that could make abortion unequally accessible under abortion bans premised on fetal cardiac activity.
We use data from a commercial mobile-device app that allows people to record menstrual cycles. The distribution of reported cycle lengths in this app generally aligns with cycle length distributions reported in previous studies, including data from surveys as well as from similar apps (3, 4). In addition to menstrual data, users recorded characteristics such as race/ethnicity and medical diagnoses.
We use data on 1.6 million menstrual cycles reported by 267,209 US women between 2014 and 2016. We use the term “women” because >99% of users identified as women. Trans and gender-diverse people who menstruate are also affected by abortion legislation. We assessed group differences in women’s probability of cycle irregularity, adjusted for covariates and population poststratification weights to better reflect the US reproductive-age population (Materials and Methods).
Results
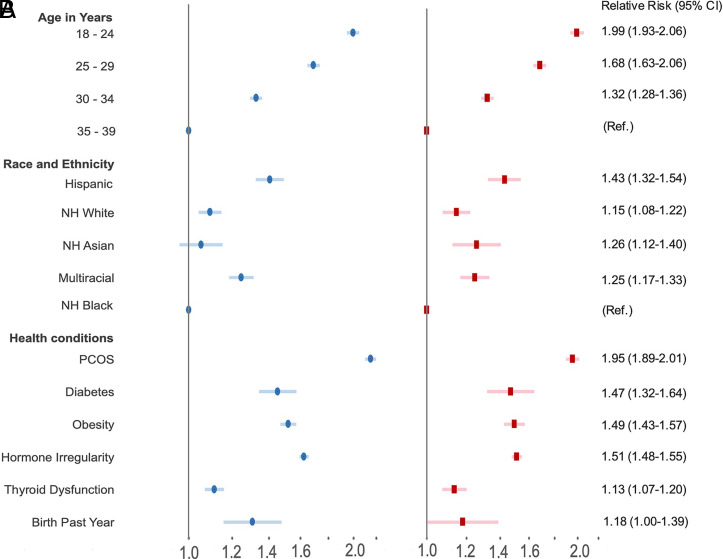
Twenty-two percent of women in the study experienced cycle irregularity, defined as women with consecutive cycles that differ by an average of 7+ d. Fig. 1 displays the relative risk of cycle irregularity, shown both with covariate adjustment and weighting (Fig. 1B, red) and without (Fig. 1A, blue). Relative risks are separately estimated by age, health conditions, and race/ethnicity. Reference categories are the group with lowest risk or, for health conditions, women without the condition.
Fig. 1.
Relative risk of cycle irregularity estimated from eight specifications of Eq. 1 separately testing differences by age, race/ethnicity, and six health conditions, (A) unweighted and unadjusted and (B) weighted and adjusted for app use frequency, contraceptive use, and pregnancy intentions. Race and health specifications: are also adjusted for age. The referent is the group with lowest risk (age: 35 y to 39 y; race/ethnicity: non-Hispanic Black persons); for health conditions: all without that condition. The 95% CIs are shown. Numeric relative risk values displayed in B are listed.
Women aged 18 y to 24 y are twice as likely to experience irregular cycles as women aged 35 y to 39 y (95% CI 1.9 to 2.1). There is also substantially greater risk of irregular cycles among women who report polycystic ovary syndrome (PCOS), type II diabetes, obesity, hormone irregularity, and thyroid dysfunction. Women with a birth in the past year have a statistically nonsignificant increased risk. Among race/ethnic groups, Hispanic women are 1.4 (1.3 to 1.5) times as likely to have irregular cycles as non-Hispanic Black women and 1.2 (1.2 to 1.3) times as likely to have irregular cycles as non-Hispanic White women.
Discussion
Menstrual irregularity—whether due to natural biological variability or illness—creates physiological barriers to abortion access under fetal cardiac activity bans. These barriers are higher for major portions of the US population: 16 million reproductive-age women are Hispanic, 5 million to 9 million have PCOS, and 30 million are obese (8, 9). This study did not include adolescents under age 18 y, among whom menstrual irregularity is especially common (10).
The mechanisms underlying group differences require further study. Categories of race/ethnicity are social and political constructs that encompass a constellation of cultural, behavioral, and environmental conditions. Specific exposures such as rotating shift work, pesticide exposure, racism, and stress can have biological effects on menstrual patterns (11, 12). Although there is little published information on ethnic variation in menstrual regularity, Hispanic women are more likely to have severe forms of PCOS, including higher rates of metabolic syndrome (11). The observed race and ethnic differences may contain artifacts of sample selectivity, although these patterns appear robust to poststratification weights (Fig. 1) and sensitivity analyses (13).
There has been widespread mischaracterization of early gestation abortion bans as “6-week” laws. Cardiac activity may be detectable 6 wk after an idealized 28-d menstrual period, but few women have regular 28-d cycles. Menstrual cycles are inherently variable, and this variability can be substantial. Even women who report being “regular” can have consecutive cycles that differ by several days. For the 22% of women in this study whose cycles unpredictably varied by 7 d or more, fetal cardiac activity can easily be detectable by the time women recognize a missed period, making abortion illegal under this legislation. These physiological limits may be compounded by mandatory waiting periods (currently in 26 US states) and transportation logistics (>20% of reproductive-age people live >40 miles from an abortion clinic) (14).
In short, legislation requiring detection of pregnancy before cardiac activity can differentially limit the availability of abortion for specific population subgroups, for physiological reasons outside of individual control.
Materials and Methods
We analyzed menstrual cycles between January 2014 and September 2016 among US residents aged 18 y to 39 y who use a commercial menstrual-tracking app. We define cycle length as the number of days from onset of one menses to the day before onset of the next. We follow previous studies (5) in minimizing reporting error by limiting the sample to cycles in which a user interacted with the app 5+ times in the month of menstruation and also in the month following. We trim the top 1% and bottom 1% of cycle lengths to further minimize reporting error; 267,209 women and 1,678,999 cycles were available for analysis, with a median of 9 cycles per woman (interquartile range 5 to 14).
Relative risks in Fig. 1 are estimated with eight specifications of a generalized linear model with a binomial distribution, a log-link function, and iteratively reweighted least squares (Eq. 1) (15). Separate regressions test group differences in irregularity that are not overcontrolled; for example, we do not seek cycle differences by PCOS diagnosis net of diabetes diagnosis. A dichotomous indicator (ϕ, the mean difference in length of consecutive cycles of 7+ d) for individual i living in zipcode z is regressed on the demographic or health condition shown in Fig. 1 (Xiz). Control measures (Wiz) include trying to conceive, use of contraception (or contraception not reported), average frequency of app interaction (three-category variable), and, for specifications in which Xiz captures race or health, age coded in bins. The β’ and δ’ coefficient vectors are estimated. Controlling for app use frequency compares menstrual irregularity among users who interact similarly with the app. Sensitivity tests examined alternative indicators of irregularity: 1) ≥7 d between longest and shortest cycles, 2) ≥7 d total cycle length variance, and 3) ≥9 median days of difference in consecutive cycles (5). These produced similar results. Sensitivity tests adjusted for individual-level education and area-level poverty are similar. SEs are clustered at the zipcode level. Results are robust to multiple testing correction with Romano–Wolfe stepdown adjusted P values.
| [1] |
All users report age and efforts to conceive. Data on race/ethnicity, contraception, and diagnoses are less complete. Estimates are based on users with complete covariate data; sample sizes vary across estimates (Table 1). We use regression-specific poststratification weights constructed to make the analytic sample for each regression match the distribution of US reproductive-age women across zipcode-level socioeconomic status, race composition, and urbanicity. Zipcode is a well-established predictor of socioeconomic status and health. We use Census and American Community Survey data to classify zipcodes by poverty level (0 to 8%, 8 to 15%, 15 to 30%, and 30 to 100%), race/ethnic composition (majority non-Hispanic Black [>50%], majority Hispanic [>50%], majority non-Hispanic White [50 to 90%], predominantly non-Hispanic White [>90%], and all others), urban status (metropolitan, micropolitan, small town, rural), and missing Census criteria. We calculate the distribution of US reproductive-age women across this 81-cell space ([5 × 4 × 4] + 1), and the distribution of each analytic sample across this same space. The poststratification weight is the ratio of these distributions.
Table 1.
Analytic samples, unweighted
| Estimates | No. of people (%) | Percent irregular | Total no. of people | Total no. of cycles |
| Age, y | ||||
| 18 to 24 | 40,375 (15) | 31 | 267,209 | 1,678,999 |
| 25 to 29 | 80,441 (30) | 27 | ||
| 30 to 34 | 98,729 (37) | 21 | ||
| 35 to 39 | 47,664 (18) | 16 | ||
| Race | ||||
| NH Black | 6,683 (6) | 22 | 103,413 | 733,536 |
| Hispanic | 7,219 (7) | 30 | ||
| NH White | 69,530 (67) | 24 | ||
| NH Asian | 2,156 (2) | 23 | ||
| Multirace | 17,260 (17) | 27 | ||
| PCOS | 14,858 (11) | 43 | 129,754 | 888,663 |
| Type II diabetes | 1,059 (1) | 35 | 93,634 | 675,328 |
| Obesity | 11,256 (21) | 32 | 54,203 | 402,371 |
| Hormone irregularity | 32,345 (19) | 34 | 174,345 | 1,204,766 |
| Thyroid dysfunction | 6,341 (8) | 27 | 83,065 | 617,117 |
| Birth past year | 602 (1) | 28 | 41,164 | 283,686 |
NH, non-Hispanic.
The weights address sample selection on observed area-level dimensions. App users, however, may be nonrandom on unmeasured characteristics—for example, 5% of reproductive-age people do not own smartphones (16). Those with health conditions like PCOS may be more likely to use cycle-tracking apps, although the prevalence of users with PCOS in this sample (11%) is within the range estimated for reproductive-age women (6 to 12%) (9). To introduce bias, app users would have to differ from nonusers in the association between conditions like PCOS and irregularity. We have no reason to expect differences large enough to influence the findings; nonetheless, these findings should be replicated in studies with more complete ascertainment.
No nationally representative US study has prospectively tracked menstrual cycles. We are encouraged by the similarity of our cycle length distribution to published data not based on self-selection into app use. Although we control for contraception use, we had no data on specific methods that might affect cycle characteristics. We addressed this with a reanalysis of women not using contraception. Results were unchanged. Additional sensitivity tests were restricted to women trying to conceive for <6 mo at sign-up (i.e., not selected on difficulty conceiving), to women not trying to conceive, and with fixed effects for the number of cycles women contributed to the samples. Conclusions were the same. We also tested analyses using long cycles (mean 35+ d) as the outcome. Irregularity often accompanies long cycles, and results for long cycles are similar. This research was approved by the University of Wisconsin-Madison institutional review board. Sensitivity tests and additional sample description are on J.N.’s GitHub.
Acknowledgments
We acknowledge funding support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (Grants R01HD102207), a private family foundation through the UW Collaborative for Reproductive Equity, and the NICHD-supported Center for Demography and Ecology (Grants P2CHD047873 and T32HD007014). We thank Donna Baird, Russell Dimond, Eric Grodsky, Amar Hamoudi, Quaker Harmon, Jenny Higgins, Anne Marie Jukic, Katrina Kimport, Sheila Miller, Miriam Seifter, and Amy Williamson.
Footnotes
The authors declare no competing interest.
Data Availability
Sensitivity tests and additional sample descriptions have been deposited in GitHub (https://github.com/jen-nej/cycles) (13). Data are available from the commercial developers of the menstrual tracking application. To protect user privacy and confidentiality restrictions apply to the availability of the data, and so they are not publicly released. Data are available upon reasonable request and with necessary data protections, reviews, and agreements.
References
- 1.Wisser J., Dirschedl P., Embryonic heart rate in dated human embryos. Early Hum. Dev. 37, 107–115 (1994). [DOI] [PubMed] [Google Scholar]
- 2.Kost K., Lindberg L., Pregnancy intentions, maternal behaviors, and infant health: Investigating relationships with new measures and propensity score analysis. Demography 52, 83–111 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Treloar A. E., Boynton R. E., Behn B. G., Brown B. W., Variation of the human menstrual cycle through reproductive life. Int. J. Fertil. 12, 77–126 (1967). [PubMed] [Google Scholar]
- 4.Bull J. R., et al. , Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. npj Dig. Med. 2, 83 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li K., et al. , Characterizing physiological and symptomatic variation in menstrual cycles using self-tracked mobile-health data. npj Dig. Med. 3, 79 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilcox A. J., Dunson D., Baird D. D., The timing of the “fertile window” in the menstrual cycle: day specific estimates from a prospective study. BMJ 321, 1259–1262 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowland A. S., et al. , Influence of medical conditions and lifestyle factors on the menstrual cycle. Epidemiology 13, 668–674 (2002). [DOI] [PubMed] [Google Scholar]
- 8.US Census Bureau, 2019 Population estimates by age, sex, race and hispanic origin. https://www.census.gov/newsroom/press-kits/2020/population-estimates-detailed.html. Accessed 20 July 2021.
- 9.Centers for Disease Control and Prevention, PCOS (polycystic ovary syndrome) and diabetes. https://www.cdc.gov/diabetes/basics/pcos.html. Accessed 20 July 2021.
- 10.Gunn H. M., Tsai M. C., McRae A., Steinbeck K. S., Menstrual patterns in the first gynecological year: A systematic review. J. Pediatr. Adolesc. Gynecol. 31, 557–565.e6 (2018). [DOI] [PubMed] [Google Scholar]
- 11.Engmann L., et al. , Reproductive Medicine Network, Racial and ethnic differences in the polycystic ovary syndrome metabolic phenotype. Am. J. Obstet. Gynecol. 216, 493.e1 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawson C. C., et al. , Rotating shift work and menstrual cycle characteristics. Epidemiology 22, 305–312 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.J. Nobles, L. Cannon, A. J. Wilcox, Cycles. GitHub. https://github.com/jen-nej/cycles. Deposited 22 November 2021. [Google Scholar]
- 14.Bearak J. M., Burke K. L., Jones R. K., Disparities and change over time in distance women would need to travel to have an abortion in the USA: A spatial analysis. Lancet Public Health 2, e493–e500 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardin J. W., Hilbe J. M., Generalized Linear Models and Extensions (Stata, College Station, TX, ed. 4, 2018). [Google Scholar]
- 16.Pew Research Center, Demographics of mobile device ownership and adoption in the United States. https://www.pewresearch.org/internet/fact-sheet/mobile/. Accessed 20 July 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Sensitivity tests and additional sample descriptions have been deposited in GitHub (https://github.com/jen-nej/cycles) (13). Data are available from the commercial developers of the menstrual tracking application. To protect user privacy and confidentiality restrictions apply to the availability of the data, and so they are not publicly released. Data are available upon reasonable request and with necessary data protections, reviews, and agreements.