ABSTRACT
Endoscopic sphincterotomy (ES) is commonly performed during endoscopic retrograde cholangiopancreatography, and bleeding is a severe adverse event. PuraStat is a peptide developed as a hemostatic agent for endoscopy. We report its use as a hemostatic strategy in post-ES bleeding refractory to combined hemostasis. A patient with choledocholithiasis underwent endoscopic retrograde cholangiopancreatography for stone removal. After the ES, severe bleeding refractory to the injection of diluted epinephrine around the bleeding source and metal stent placement occurred. Hemostasis was achieved with the application of the hemostatic gel. We reported the use of novel self-assembling hemostatic gel as an effective therapeutic tool for post-ES refractory bleeding.
INTRODUCTION
Endoscopic sphincterotomy (ES) is frequently performed during endoscopic retrograde cholangiopancreatography (ERCP), and post-ES bleeding is a severe adverse event occurring in 0.3%–2%.1 The injection of dilute epinephrine into and around the sphincterotomy site, alone or in combination with thermal and/or mechanical hemostasis, is commonly used in intraprocedural bleeding, and it is effective in most cases.2 Although it is possible to try different endoscopic treatment modalities to stop the bleeding, almost 20% of the patients experienced rebleeding after initial successful endoscopic hemostasis.3 Recent studies reported an effective use of fully covered self-expandable metallic stents (FC-SEMSs) placement in patients with post-ES refractory bleeding.1,4 PuraStat (3D-Matrix Europe SAS, France) is a novel self-assembled, clear, fully synthetic hydrogel peptide, developed as a hemostatic agent for endoscopic and surgical procedures; for this, in recent years, there has been an increasing use for the prevention and treatment of bleeding after endoscopic resections and for refractory gastrointestinal bleeding.5 In this case, we report an effective use of novel self-assembling peptide hemostatic gel in refractory post-ES bleeding.
CASE REPORT
A 52-year-old man with a 2-month intermittent history of biliary colic and a recent appearance of jaundice and pruritus was referred to our center for a clinical evaluation.
The blood test showed high values of alkaline phosphatase (348 U/L) and gamma glutamyltransferase (189 U/L), with normal values of hemoglobin (14.1 g/dL), bilirubin 4.3 mg/dL, and liver enzymes. An abdominal ultrasound revealed mild dilation of the common bile duct (11 mm) with a distal portion that could not be assessed because of air artifact. Owing to the clinical suspicion of choledocholithiasis, an ultrasound was performed confirming the diagnosis of common bile duct stone.
After obtaining informed consent for the procedure and appropriate sedation, ERCP was performed. The ampulla appeared enlarged and very prominent. The cholangiography showed a mildly dilated common bile duct with a single fluoroscopic image showing lithiasis of approximately 6 mm in the juxtapapillary site. Sphincterotomy was performed, resulting in spontaneous stone extraction. However, the procedure was complicated by immediate bleeding. Injection of 5 mL of diluted epinephrine was performed into and around the sphincterotomy site without success. Owing to severe bleeding, the physicians decided to place a FC-SEMS. Despite SEMS, continuous superficial bleeding from the oral side of the ES cutting site was appreciated (Figure 1). It was decided to apply 3 mL of hemostatic gel on the bleeding source using an endoscopic catheter, achieving hemostasis (Figure 2). The hemostasis persisted during a 5-minute observation time, so the procedure was concluded (Figure 3). After the procedure, the patient's clinical and biochemical condition improved, with no evidence of hemoglobin drop or post-ERCP pancreatitis. He was discharged after 4 days with plans to remove SEMS in 6 months.
Figure 1.
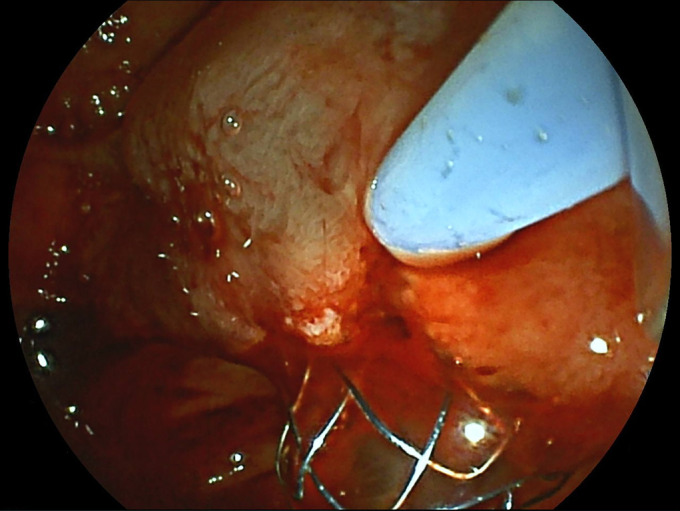
Bleeding originating from the oral side of the endoscopic sphincterotomy cutting site despite self-expandable metallic stent placement.
Figure 2.
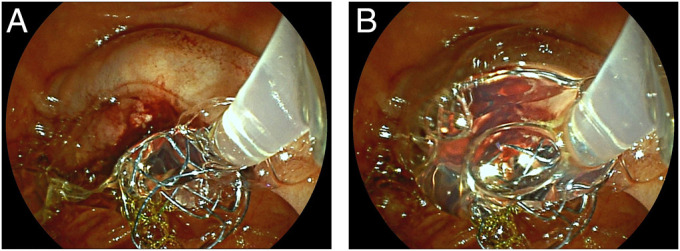
(A and B) Endoscopic application of hemostatic gel on bleeding source.
Figure 3.
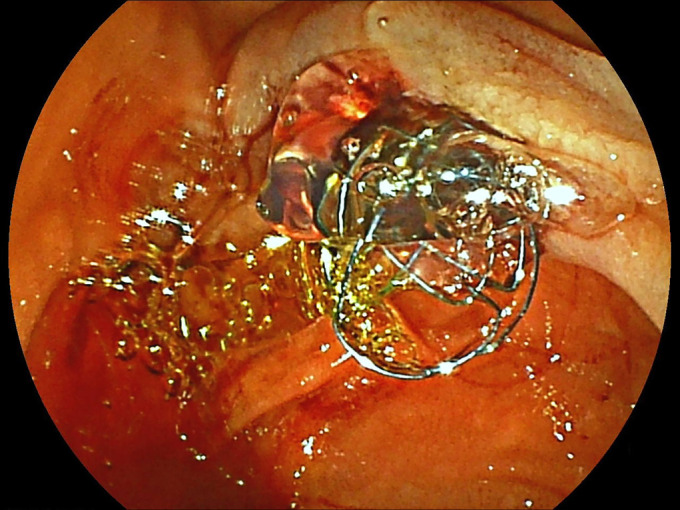
Persistent hemostasis with hemostatic gel.
DISCUSSION
We discuss the endoscopic application of novel self-assembling peptide hemostatic gel as a third-line hemostatic strategy for post-ES bleeding. Intraprocedural bleeding is a common complication of ES.1,6,8 The American Society for Gastrointestinal Endoscopy guidelines suggest some strategies to minimize post-ES bleeding, especially in patients with >1 risk factor for bleeding. The treatments of post-ES bleeding are medical management and endoscopic injection of diluted epinephrine (1:10,000) around the bleeding site that is effective in most cases.9 In the case of failed hemostasis with epinephrine injection, the next step in the therapeutic algorithm is the use of thermal (multipolar electrocautery and argon plasma coagulation) and mechanical (balloon tamponade of the ES site or the use of through-the-scope clips) hemostasis or the combination of these. However, the application of through-the-scope clips using a duodenoscope could be extremely challenging in some cases, with the need to place them using a forward-viewing endoscope.
Recently, the use of FC-SEMSs has been recognized as a safe and effective hemostatic approach in post-ES refractory bleeding, at the expense of high cost and an additional procedure to remove the stent.4 Recently, Orlandini et al7 showed the effectiveness of injection of fibrin glue for post-ES refractory bleeding. The novel hemostatic gel is a clear, self-assembling hydrogel peptide composed by repeating amino acid sequences of arginine (R), alanine (A), aspartic acid (D), and alanine (A), resulting in 4 repeating amino acid sequence RADARADARADARADA (RADA16). At neutral pH, it appears as a viscous and transparent hydrogel; when it comes into contact with body fluids, it can self-assemble into fibers forming an extracellular matrix that acts as a mechanical barrier on the bleeding source providing a hemostatic effect.5 It is available in a single-use sterile prefilled syringe (1, 3, and 5 mL) to be stored in a refrigerator (from 2 to 8°C). It is applied using an endoscopic catheter inserted in the operative channel of the duodenoscope (Figure 4).
Figure 4.
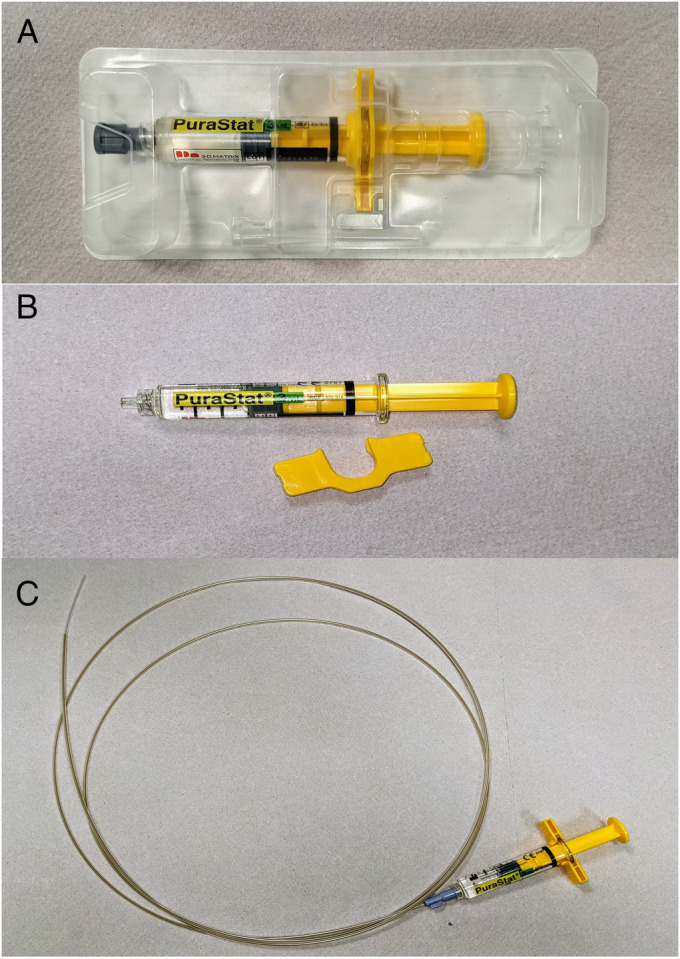
Preparation of PuraStatstep by step. (A) PuraStat is supplied in a prefilled syringe, (B) after removing the safety device, and (C) Purastat is applied using an endoscopic catheter suitable for a 2.8-mm working channel.
The tip of the catheter should be positioned close to the lesion, and the gel should be applied, taking into account the effect of gravity on the distribution of the gel. After the application, the endoscopist should avoid the aspiration or the injection of water until effective hemostasis has been reached. In recent years, there has been an increased use of this agent for the prevention and treatment of bleeding after endoscopic resections and refractory gastrointestinal bleeding.10 Theoretical risks of using the hemostatic gel are thromboembolic complications after migration of the gel into the blood vessels or biliopancreatic obstruction because of the peptide network; although these complications are virtually possible, the authors consider them highly unlikely, consistent with the high safety profile in the current literature.
Advantages of the endoscopic application of hemostatic gel for the treatment of post-ES are linked to the intrinsic feasibility and efficacy of the product (ie, easy preparation before use, easy application, and low learning curve for the physicians). To the best of our knowledge, there is a single observational, open-label, consecutive case series study reporting the efficacy of novel self-assembling peptide hemostatic gel as rescue therapy for refractory acute gastrointestinal bleeding, including 5 cases of ERCP bleeding.5 Although its intrinsic limitation, this case report could be evaluated as further proof of the effectiveness and feasibility of novel self-assembling peptide hemostatic gel as therapy for intraprocedural ERCP bleeding.
DISCLOSURES
Author contributions: M. Gagliardi and G. Oliviero, M. Napoli, M. Fusco, and A. Sica revised the article. A. Maurano and C. Zulli analyzed data. M. Gagliardi and M. Sica wrote the article. M. Gagliardi is guarantor of this article.
Acknowledgments: We thank all the hospital staff who helped us to perform the procedure and develop the case report, including nurses and auxiliary staff.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Contributor Information
Giovanni Oliviero, Email: giovanni.olivierounina2@gmail.com.
Michele Fusco, Email: fusco.michele90@gmail.com.
Marco Napoli, Email: marco.napoli.md@gmail.com.
Andrea Sica, Email: sica.andrea@gmail.com.
Attilio Maurano, Email: amauran@tin.it.
Mariano Sica, Email: sica.mariano@gmail.com.
Claudio Zulli, Email: zulli.claudio@gmail.com.
REFERENCES
- 1.Chandrasekhara V, Khashab MA, Muthusamy VR, et al. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85:32–47. [DOI] [PubMed] [Google Scholar]
- 2.Wilcox CM, Canakis J, Mönkemüller KE, Bondora AW, Geels W. Patterns of bleeding after endoscopic sphincterotomy, the subsequent risk of bleeding, and the role of epinephrine injection. Am J Gastroenterol. 2004;99:244–8. [DOI] [PubMed] [Google Scholar]
- 3.Lee MH, Tsou YK, Lin CH, et al. Predictors of re-bleeding after endoscopic hemostasis for delayed post-endoscopic sphincterotomy bleeding. World J Gastroenterol. 2016;22:3196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Itoi T, Yasuda I, Doi S, Mukai T, Kurihara T, Sofuni A. Endoscopic hemostasis using covered metallic stent placement for uncontrolled post-endoscopic sphincterotomy bleeding. Endoscopy. 2011;43:369–72. [DOI] [PubMed] [Google Scholar]
- 5.de Nucci G, Reati R, Arena I, et al. Efficacy of a novel self-assembling peptide hemostatic gel as rescue therapy for refractory acute gastrointestinal bleeding. Endoscopy. 2020;52:773–9. [DOI] [PubMed] [Google Scholar]
- 6.Bae SS, Lee DW. Risk factor of bleeding after endoscopic sphincterotomy in average risk patients. Surg Endosc. 2019;33:3334–40. [DOI] [PubMed] [Google Scholar]
- 7.Orlandini B, Schepis T, Tringali A. Fibrin glue injection: A rescue treatment for refractory post-sphincterotomy and post-papillectomy bleedings. Dig Endosc. 2020;33:815–21. [DOI] [PubMed] [Google Scholar]
- 8.Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastrointest Endosc. 1991;37:383–93. [DOI] [PubMed] [Google Scholar]
- 9.Matsushita M, Takakuwa H, Shimeno N, Uchida K, Nishio A, Okazaki K. Prophylactic injection of hypertonic saline-epinephrine oral to the papilla for prevention of postsphincterotomy bleeding. J Clin Gastroenterol. 2010;44:e167–70. [DOI] [PubMed] [Google Scholar]
- 10.Oumrani S, Barret M, Bordaçahar B, et al. Application of a self-assembling peptide matrix prevents esophageal stricture after circumferential endoscopic submucosal dissection in a pig model. PLoS One. 2019;14:e0212362. [DOI] [PMC free article] [PubMed] [Google Scholar]


