Prevention of type 1 diabetes has been brought closer to reality through the ability to identify populations at increased risk and through therapies that can modify the disease course (1). Identification of those who are at risk is based on the detection of diabetes-related autoantibodies (Ab) that can be found many years before clinical diagnosis. Those identified as being at increased risk due to having a family member who lives with type 1 diabetes or who have an increased genetic risk based on high-risk HLA have been followed in a number of longitudinal cohort studies (2–8) The preclinical phase of type 1 diabetes is described as progression from genetic susceptibility and immune activation to the development of single and then multiple Ab, to early abnormalities of glucose tolerance, and finally to clinical diabetes (9). Those who are found to have multiple Ab almost inevitably progress to diabetes (10). However, the time from detection of multiple Ab to diagnosis varies widely. To move the goal of the prevention of type 1 diabetes from research to clinical reality, refinements of strategies to predict progression to diabetes are needed. Anand et al. (11) and Bonifacio et al. (12), in two articles in this issue of Diabetes Care, help to define characteristics of Ab development and diabetes progression in >24,000 children at risk.
The work by Anand et al. brings together data from five cohorts with a focus on the risk associated with the age at autoantibody (Ab) development, the number of Ab, and the HLA-DR-DQ genotype. The >16,000 children in these cohorts came from Germany, Sweden, Finland, Washington state, and Colorado and were tested for Ab before the age of 2.5 years and then followed at 3- to 36-month intervals, with >10 years of observation. Participants were from the general population, enrolled based on high-risk HLA haplotypes, or children of parents with diabetes. HLA genotyping was done differently in each of the studies and changed over time, so the authors developed a strategy to harmonize the HLA data into risk groups. For characterization of risk in a manner that could be translated to a screening program, risk was stratified by the number of Ab found at the time Ab were first detected rather than the number that appeared over time as has been done in previous analyses. HLA risk group was a significant factor, with 7% developing multiple Ab and 16% developing diabetes by age 15 years among the group at highest risk versus 1% and 2.5% among the group at lowest risk. The number of Ab found at the time that they were first detected was also significant with 45%, 85%, and 92% of those with one, two, and three Ab developing diabetes. In further analyses, cumulative incidence of diabetes in the group with a single Ab differed by Ab status 2 years after the Ab was first found, with 12% vs. 82% having diabetes in those who had zero and multiple Ab, respectively. Younger age at development of multiple Ab (<2 vs. > 7.4 years old) was associated with a 15 year cumulative diabetes risk varying from 95% to 54%.
This report provides more robust estimates of risk in children who develop Ab, highlighting the particularly high risk and rapid progression in those with multiple Ab at an early age. An additional major finding is the high degree of risk associated with a single Ab appearing at a young age. Previous publications have noted lower risk in those with a single Ab but included those who move from single to multiple Ab in the multiple Ab grouping. The findings further support the concept that high-risk HLA is a key factor in driving autoimmunity but is less important in progression from established autoimmunity (multiple Ab) to diabetes.
Bonifacio et al. (12) also address a question relevant to the translation of screening for diabetes Ab to future clinical use. Their work comes from The Environmental Determinants of Diabetes in the Young (TEDDY), a prospective cohort study of >8,500 children enrolled before the age of 4.5 months (13). These children were enrolled on the basis of high-risk HLA, coming from the general population and families with individuals with type 1 diabetes. At the time of analysis, they had been followed for 9–15 years. Previous publications from the TEDDY study and other birth cohorts with high-risk HLA have shown that the peak incidence of antibodies occurs in the first few years of life and then diminishes. The authors examined effects of genetics, demographics, and Ab patterns on the fall in rates of development of Ab and identified optimal ages for Ab screening. The risk of developing multiple Ab at 7.5 months was 4.3% but fell to 1.1% by age 6.25 years. HLA and other high-risk susceptibility genes affected the fall in 5-year risk in very young children, but risk converged by age 6 years. The fall in risk varied in those with multiple Ab by the pattern of Ab development, with the most rapid decay in those who developed insulin Ab first. The authors assessed sensitivity for developing diabetes by age 12 years and positive predictive value for 5-year risk of developing diabetes to identify optimal age for Ab screening. Peak sensitivity was at age 4 years, with one-third of cases identified by screening between ages 3 and 5 years. Highest positive predictive value was at age 1 year. Screening twice at age 2 and then at 5–6 or at age 3 and again at 6–7 years gave a sensitivity of 50%.
The article highlights that very young children with higher-risk HLA genetics develop early autoimmunity, with a diminishing risk in later childhood. In this population, antibody testing done between ages 3 and 5 years identified >33% of those who developed Ab. Screening twice increased the detection of Ab to 50%.
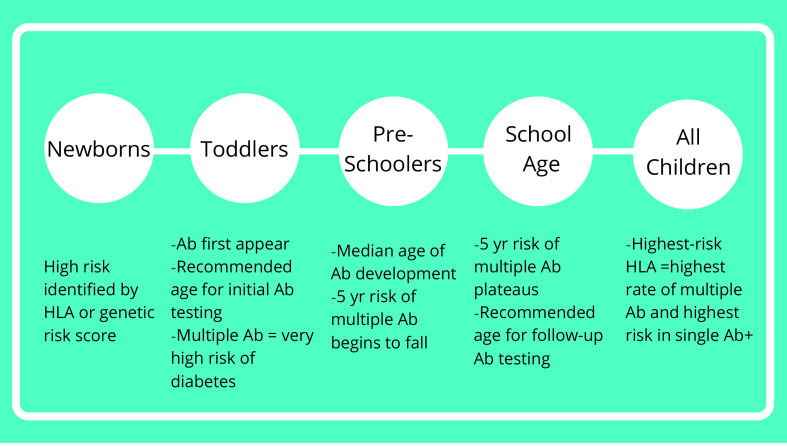
Both articles have significant strengths with large numbers of study participants and rigorously conducted long-term follow-up. They provide additional detail about factors known to contribute to autoimmunity and diabetes in those with high genetic risk (Figure 1). Both provide valuable insights into planning parameters for potential screening programs and clinical trials for children at high genetic risk. As the authors point out, all of these studies largely include Caucasian children at high genetic risk coming from a limited number of regions in the U.S., Finland, Germany, and Sweden, so there are limitations to the generalizability of the results. The translation of these results to the general population will require study of more ethnically diverse populations from a broader range of countries. If a general population screening program targeted older children rather than newborns, the risk estimates may be different. The findings focus on development of diabetes over a maximum of 15 years from multiple Ab development, with fewer participants who developed Ab at a later age, as median age of Ab development was 3–4 years, limiting the translation to older teens and adults who may have later-onset autoimmunity.
Figure 1.
Key features of type 1 diabetes development by age in children at high risk. Toddlers, age 1–2 years; preschoolers, age 3–4 years; school age, age 6–7 years. Single Ab+, those positive for a single Ab; yr, year.
The findings of both groups of authors refine our understanding of the course of the presymptomatic phase of type 1 diabetes in children, highlighting factors associated with rapid progression and supporting the very high risk associated with multiple Ab at younger ages. This will aid in planning of clinical trials by virtue of providing more exact estimates of risk and rate of diabetes development based on characteristics of trial participants. It also suggests that in public health interventions and clinical trials involving screening for Ab and follow-up for development of additional Ab, stratification of timing of testing could be done based on age, HLA, and/or genetic risk score to optimize detection of Ab before diabetes develops to reduce costs. Future work should define additional predictors of time to progression to diabetes to provide a more precise estimate of the timing of development of diabetes. Creation of an individualized risk calculator for those with multiple Ab providing estimates of future risk over defined time intervals could be envisioned to assist families in understanding of risk.
Article Information
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Footnotes
References
- 1. Herold KC, Bundy BN, Krischer JP; Type 1 Diabetes TrialNet Study Group . Teplizumab in relatives at risk for type 1 diabetes. Reply. N Engl J Med 2019;381:1880–1881 [DOI] [PubMed] [Google Scholar]
- 2. Krischer JP, Liu X, Vehik K, et al.; TEDDY Study Group . Predicting islet cell autoimmunity and type 1 diabetes: an 8-year TEDDY study progress report. Diabetes Care 2019;42:1051–1060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lundgren M, Lynch K, Larsson C; Diabetes Prediction in Skåne study group . Cord blood insulinoma-associated protein 2 autoantibodies are associated with increased risk of type 1 diabetes in the population-based Diabetes Prediction in Skåne study. Diabetologia 2015;58:75–78 [DOI] [PubMed] [Google Scholar]
- 4. Pöllänen PM, Ryhänen SJ, Toppari J, et al. Dynamics of islet autoantibodies during prospective follow-up from birth to age 15 years. J Clin Endocrinol Metab 2020;105:e4638–e4651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Steck AK, Johnson K, Barriga KJ, et al. Age of islet autoantibody appearance and mean levels of insulin, but not GAD or IA-2 autoantibodies, predict age of diagnosis of type 1 diabetes: diabetes autoimmunity study in the young. Diabetes Care 2011;34:1397–1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vehik K, Beam CA, Mahon JL, et al.; TrialNet Natural History Study Group . Development of autoantibodies in the TrialNet Natural History Study. Diabetes Care 2011;34:1897–1901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wion E, Brantley M, Stevens J, et al. Population-wide infant screening for HLA-based type 1 diabetes risk via dried blood spots from the public health infrastructure. Ann N Y Acad Sci 2003;1005:400–403 [DOI] [PubMed] [Google Scholar]
- 8. Ziegler AG; BABYDIAB-BABYDIET Study Group . Age-related islet autoantibody incidence in offspring of patients with type 1 diabetes. Diabetologia 2012;55:1937–1943 [DOI] [PubMed] [Google Scholar]
- 9. Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care 2015;38:1964–1974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ziegler AG, Rewers M, Simell O, et al. Seroconversion to multiple islet autoantibodies and risk of progression to diabetes in children. JAMA 2013;309:2473–2479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Anand V, Li Y, Liu B, et al.; T1DI Study Group . Islet autoimmunity and HLA markers of presymptomatic and clinical type 1 diabetes: joint analyses of prospective cohort studies in Finland, Germany, Sweden, and the U.S. Diabetes Care 2021:44:2269–2276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bonifacio E, Weiß A, Winkler C, et al.; TEDDY Study Group . An age-related exponential decline in the risk of multiple islet autoantibody seroconversion during childhood. Diabetes Care 2021;44:2260–2268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Krischer JP, Lynch KF, Schatz DA, et al.; TEDDY Study Group . The 6 year incidence of diabetes-associated autoantibodies in genetically at-risk children: the TEDDY study. Diabetologia 2015;58:980–987 [DOI] [PMC free article] [PubMed] [Google Scholar]