Abstract
Introduction
Fibroadenomas are among the most common benign tumors in women. Juvenile giant fibroadenomas account for nearly 0.5% of all fibroadenomas. Due to its size, a giant juvenile fibroadenoma leaves a large defect or deformity after its resection. The optimal surgical management strategy for giant juvenile fibroadenomas remains unclear. Here, we report a case of successful breast reconstruction without residual deformity through gradual deflation of a saline-filled tissue expander after resection of a giant juvenile fibroadenoma.
Presentation of case
A 14-year-old girl with a growing tumor in her left breast presented to a private clinic. Given that the tumor was 8 cm in size, phyllodes could not be ruled out. Consequently, she was referred to our hospital for further examination and treatment. Core needle biopsy confirmed the tumor to be a fibroadenoma. We resected the tumor and inserted a tissue expander filled with 120 mL of saline, matching the area of the large defect caused by tumor resection. We removed approximately 25 mL of saline every 3 weeks to aid normal mammary tissue enlargement. After completely draining saline from the tissue expander and confirming an acceptable enlargement of the residual mammary gland, we performed an operation to remove the tissue expander. Follow-up revealed that the symmetry and contour of the breast were excellent after the second operation.
Conclusions
Our observations suggest that using a tissue expander to enlarge normal mammary tissue may help reconstruct large defects caused by excision of benign tumors.
Abbreviations: FA, Fibroadenoma; TE, Tissue expander
Keywords: Tissue expander, Giant juvenile fibroadenoma, Breast reconstruction
Highlights
-
•
Large breast benign tumor may cause breast deformity and breastfeeding dysfunction.
-
•
Re-construction can help mitigate the defect after removing a large breast tumor.
-
•
A saline-filled TE was inserted to dead space followed by gradual deflation.
-
•
After complete recovery of breast tissue, deflated TE was removed.
1. Introduction
Fibroadenomas (FAs) are among the most common benign tumors in women. They are caused by the proliferation of interstitial connective tissue components and epithelial components and are commonly observed in patients younger than 30 years of age. In individuals aged between 10 and 18 years, these tumors are called juvenile-type FAs [1]; juvenile FAs account for 0.5% of all FAs. An FA is categorized as a giant FA when it is larger than 5 cm, weighs more than 500 g, or occupies at least 80% of the breast; giant FAs account for 1%–8% of all adolescent FAs [2], [3]. Excision of an FA may cause a large mammary tissue deficit and lead to a breast deformity; thus, excision is a key issue associated with giant FAs. Despite the remarkable progress in this field, there are no specific guidelines for the optimal surgical management of benign tumors, including giant juvenile FAs. Breast reconstruction using a tissue expander (TE) and an implant is one way of managing excision-based defects. A TE is commonly used by gradually inflating it with sequential saline injections over a few months before the insertion of the implant. We present a case wherein we performed a successful breast reconstruction after resecting a giant juvenile FA; we inserted a saline-filled TE to cover the resulting defect and sequentially withdrew the saline as the normal mammary tissue grew. This case report was prepared in accordance with the SCARE guidelines [4].
2. Presentation of case
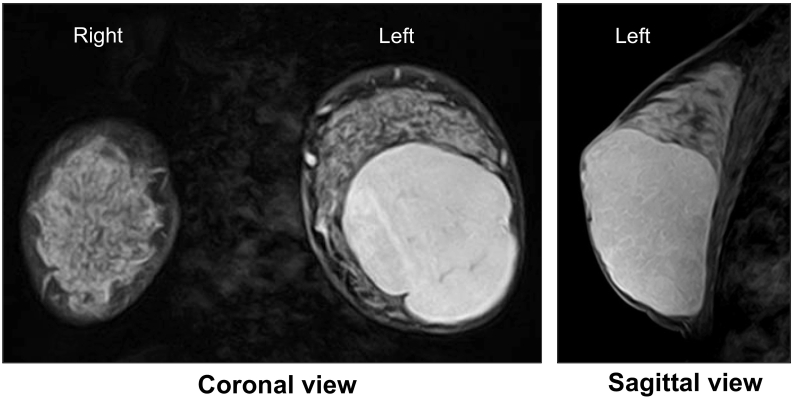
A 14-year-old girl presented to a private clinic with a 3-year history of a slowly growing mass in her left breast. Examinations revealed a tumor, 8 cm in diameter, in the lower two-thirds of the left breast. Although an FA was suspected, a phyllodes tumor could not be ruled out due to its large size. Thus, she was referred to our hospital for further treatment. On breast palpation, we found a large (10 × 7 cm), soft, and smooth mass with good mobility in the lower two-thirds of the left breast. There were no swollen axillary nodes. Mammography revealed a high-density 10-cm mass with a well-defined border in the lower two-thirds of the left breast. Ultrasound revealed a well-circumscribed 10-cm hypoechoic mass in the same region. Magnetic resonance imaging revealed a uniformly enhanced tumor occupying two-thirds of the left breast (Fig. 1). Core needle biopsy revealed a tissue composed of epithelial and stromal components with maintained biphasic epithelium. The MIB-1 was less than 1%, and an FA was confirmed.
Fig. 1.
Coronal and sagittal views during magnetic resonance imaging reveal enhanced and well-circumscribed tumor occupying two-thirds of the left breast.
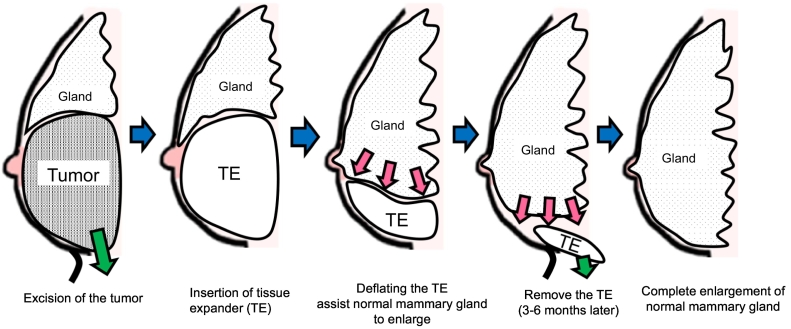
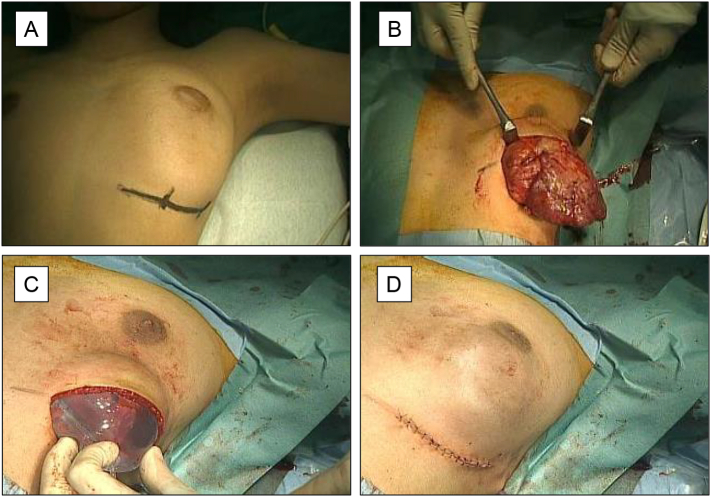
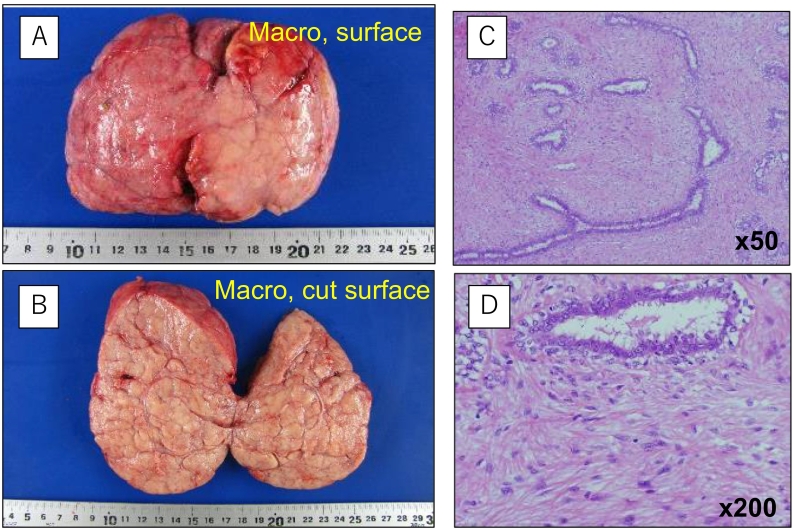
Because the excision of a giant tumor is known to leave behind a large defect [1], [5], we planned to minimize breast deformity by inserting a saline-filled TE (Fig. 2). Under general anesthesia, a 6-cm skin incision was made along the lower-left inframammary fold in the lower and outer regions of the breast (Fig. 3). After identifying the tumor capsule, we enucleated the mass along the capsule. After tumor excision, we inserted a TE (KOKEN R-1402) filled with 120 mL of saline into the space where the tumor was previously located. The operation time was 82 min, and the intraoperative blood loss was approximately 30 mL. The enucleated tumor was 13 × 9 × 4.5 cm in size, had a smooth surface, and weighed 267 g. It was macroscopically confirmed to be an FA. Histological examination of the tumor also confirmed an organoid type FA (Fig. 4).
Fig. 2.
Scheme describing the surgical strategy of gradually deflating the tissue expander.
Fig. 3.
Surgical findings. An inframammary line incision (A) is made for tumor resection (B) and tissue expander insertion (C, D).
Fig. 4.
Gross (A, B) and pathological (C, D) tumor findings. Pathological findings demonstrate characteristics of a fibroadenoma, such as a glandular structure and a hypercellular fibromyxoid stroma.
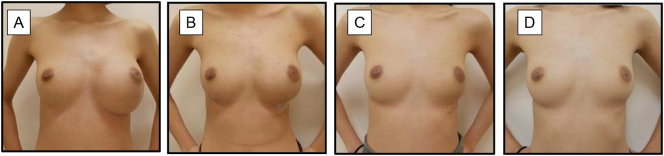
Approximately 25 mL of saline was withdrawn every 3 weeks to avoid sagging or wrinkling of the skin. When the saline inside the TE was completely removed, and the residual mammary gland was sufficiently enlarged, we performed surgery to remove the TE 4 months after the 1st surgery. Follow-up findings revealed that the symmetry and contour of the breast were excellent after the second operation (Fig. 5).
Fig. 5.
Clinical course of the appearance of the breast. A. Preoperative status. B. 5 weeks after fibroadenoma (FA) resection; no draining (residual 100/120 mL), C. 6 months after FA resection. D. 2 years after FA resection (1.5 years after the removal of the tissue expander).
3. Discussion
We have reported the successful surgical management of a giant FA and subsequent breast reconstruction with a TE in a 14-year-old girl. The differential diagnoses of FAs include benign proliferative lesions (such as lipomas), fibrocystic disease, and vaginal hypertrophy [6], [7]. Another important differential diagnosis is the phyllodes tumor, which exhibits more aggressive characteristics [6]. Due to its size, the excision of a juvenile giant FA may leave a large defect in the mammary tissue, resulting in potential breast deformities or breastfeeding disorders [1], [5]. To this end, immediate reconstruction is performed in most cases to preserve the breast symmetry [8]. The treatment of large FAs must allow a natural shrinkage of the stretched skin as well as natural recovery of the excluded mammary glands. However, primary closure sometimes results in a considerable deformity of the breast and an unnatural appearance of the skin. It is difficult to correct the breast deformity in a secondary procedure; therefore, our method is helpful to treat a giant tumor or if the skin has an unnatural appearance. Chang et al. stated three basic principles for symmetrical preservation of the breast: 1) preservation of the entire normal breast parenchyma, 2) addition of the skin envelope, and 3) positioning of the nipple symmetric to the other side of the breast [9]. Multiple methods of reconstruction have been reported previously. In a systemic review, Sosin et al. reported that prosthetic implants, local dermoglandular rearrangement, reduction mammaplasty techniques, and nipple grafting have been used for breast reconstruction and have frequently led to favorable outcomes [3]. However, currently, there is a lack of precise guidelines detailing the optimal surgical management strategies for juvenile giant FAs.
TEs and implants are widely used for breast reconstruction [10]. Conventionally, after the TE is placed in a submuscular pocket, it is filled with saline gradually over the next few months. In the current case, we placed a saline-filled TE inside the large defect left by tumor removal and depleted the saline over the next months to allow growth of the mammary tissue. A literature review revealed very few articles describing a procedure similar to ours; furthermore, only two cases (in addition to our case) were noted, which were reported by Kamei et al. One was of a 19-year-old woman who presented with an 11 × 10 × 5-cm giant FA of the left breast. The tumor was resected through an inframammary incision, and a 400-mL teardrop-shaped TE (filled with 180 mL of saline) was positioned in the cavity [5]. The other case was a 17-year-old girl who presented with a 10 × 9 × 8-cm giant FA of the left breast. The tumor was enucleated, and a 400-mL teardrop-shaped TE (filled with 170 mL of saline) was positioned in the cavity [5]. In both cases, the saline was gradually withdrawn from the TE over five months. Skin development over the expander was normal, and the final shape and volume of the breasts were excellent [5]. Kamei et al. achieved excellent outcomes in both cases using a method similar to ours; the reconstructed breast had a natural and symmetrical shape and size [5]. We thus believe that this technique can also be used to treat large defects in the mammary tissue caused by the excision of benign breast tumors. As a key advantage, this method helps preserve the normal mammary tissue by allowing its growth; hence, we believe it may be an acceptable option for recovery of compressed mammary tissue after giant cell tumor excision.
However, this method has the following limitations. First, it may not be suitable for the elderly, given that compared to younger patients, the recovery of normal breast tissues in elderly patients might not be satisfactory [5]. Second, there are no clear guidelines for patient selection. Although our case obtained a favorable expected result, we might have to replace the TE with the breast implant if the residual breast did not recover properly. Third, the use of TE was covered by Japanese health insurance in this case; insertion of TE was approved by insurance in 2018 even for the reconstruction of the deficit due to the excision of a benign breast tumor. This is a rare case, and we must confirm whether the same decision will be favorable in the future.
4. Conclusions
Here, we present a case of a giant juvenile FA successfully treated by assisting the growth of normal mammary tissue using TE. We believe that this method could be an option for patients, especially young patients, who wish to utilize their tissues for reconstruction.
Funding
None.
Guarantor
M.F. (Manabu Futamura).
Research registration number
Not applicable.
Ethics approval
Not applicable.
Consent for publication
Written consent was obtained from the patient for the publication of this case report and any accompanying images. The consent form will be provided to the editors of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
M.K. and M.F. conceived and designed the study. M.K. prepared the original draft of the manuscript. M.F. and Y.T. reviewed and edited the manuscript. M.F., M.K., K.K. and A.N. contributed to data collection. K.Y. supervised the case report and obtained the pathological pictures. All authors have read and approved the final manuscript for submission.
Declaration of competing interest
All authors have no competing interests to declare.
Contributor Information
Manabu Futamura, Email: mfutamur@gifu-u.ac.jp.
Kazuhiro Yoshida, Email: kyoshida@gifu-u.ac.jp.
References
- 1.Islam S., Saroop S., Bheem V., Naraynsingh V. Largest giant juvenile fibroadenoma of the breast. BMJ Case Rep. 2019;12 doi: 10.1136/bcr-2018-227277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jayasinghe Y., Simmons P.S. Fibroadenomas in adolescence. Curr. Opin. Obstet. Gynecol. 2009;21:402–406. doi: 10.1097/GCO.0b013e32832fa06b. [DOI] [PubMed] [Google Scholar]
- 3.Sosin M., Pulcrano M., Feldman E.D., Patel K.M., Nahabedian M.Y., Weissler J.M., Rodriguez E.D. Giant juvenile fibroadenoma: a systematic review with diagnostic and treatment recommendations. Gland. Surg. 2015;4:312–321. doi: 10.3978/j.issn.2227-684X.2015.06.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline updating consensus Surgical CAse REport (SCARE) guidelines. Int. J Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Kamei Y., Torii S. Natural skin reduction and breast recovery using a tissue expander after enucleation of a giant breast tumour. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2000;34:383–385. doi: 10.1080/028443100750059183. [DOI] [PubMed] [Google Scholar]
- 6.Gobbi D., Dall’Igna P., Alaggio R., Nitti D., Cecchetto G. Giant fibroadenoma of the breast in adolescents: report of 2 cases. J. Pediatr. Surg. 2009;44:e39–e41. doi: 10.1016/j.jpedsurg.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 7.Hiller A., Lee T.J., Henderson J., Ajkay N., Wilhelmi B.J. Oncoplastic reduction pattern technique following removal of giant fibroadenoma. Eplasty. 2018;18 [PMC free article] [PubMed] [Google Scholar]
- 8.Du F., Dong R., Zeng A., Liu Z., Yu N., Wang X., Zhu L. Surgical management of giant juvenile fibroadenoma with skin reducing tumor resection and immediate breast reconstruction: a single-center experience. J. Surg. Oncol. 2020;121:441–446. doi: 10.1002/jso.25828. [DOI] [PubMed] [Google Scholar]
- 9.Chang D.S., McGrath M.H. Management of benign tumors of the adolescent breast. Plast. Reconstr. Surg. 2007;120:13e–19e. doi: 10.1097/01.prs.0000264396.03452.62. [DOI] [PubMed] [Google Scholar]
- 10.Bellini E., Pesce M., Santi P., Raposio E. Two-stage tissue-expander breast reconstruction: a focus on the surgical technique. Biomed. Res. Int. 2017;2017:1791546. doi: 10.1155/2017/1791546. [DOI] [PMC free article] [PubMed] [Google Scholar]