Abstract
Introduction
As a complication of anorexia or bulimia nervosa, gastrointestinal problems such as stomach dilatation and necrosis are extremely rare. Our purpose is this case to pay attention on anorexia and bulimia patients to envisage the occurrence of chronic digestive injuries by performing the accurate diagnosis and selective prompt treatment.
Case presentation
A 40-year old female patient admitted to the emergency department with complaints of digestive symptoms. In his history there was just anorexia nervosa. Computed tomography and X-rays showed major gastric distension reaching the pelvis and perforation of the fundus. The large curvature of the stomach and the necrotic part was removed surgically. But the patient died in the second day after admission in the hospital because he was affected by a septic shock as a complication of distribution the infection because the doctors didn't resect whole the stomach during the open surgery.
Discussion
We report a rare case that shows gastric dilatation and necrosis post-anorexia nervosa, which requires accurate X-ray and CT scan, but treatment depends on whether or not gastric necrosis is present and the size of the necrosis. According to what mentioned in the medical literature this is the second case that cause death of the patient after surgery for treatment the gastric dilatation as a complication of anorexia nervosa.
Conclusion
The thing that distinguishes this case is the large size of the extension of the stomach from the diaphragm to the pelvis and the perforation of the fundus with a diameter of 5 cm and the death of the patient after surgery, so we can add it in the medical literature to avoid the complications of these psychiatric diseases.
Keywords: Chronic gastric dilatation, Gastric perforation, Anorexia nervosa
Highlights
-
•
Gastric dilatation is a rare fatal complication of anorexia nervosa.
-
•
Gastric dilatation must be promptly diagnosed due to the potential fatality associated with this clinical situation.
-
•
Delay in starting treatment may jeopardise the survival of an emaciated patient.
-
•
Surgical intervention is required when conservative management fails or suspicion of necrosis or perforation is raised.
1. Introduction
Anorexia nervosa and bulimia nervosa are serious psychiatric illnesses related to disordered eating and distorted body images. Anorexia nervosa, is an eating disorder characterized by low weight, food restriction, body image disturbance, fear of gaining weight, and an overpowering desire to be thin, but regarding bulimia nervosa, it is an eating disorder characterized by binge eating followed by purging [1]. Low self-esteem, a sense of powerlessness, sadness, anxiety, and loneliness are all psychological variables that contribute to anorexia nervosa and norexics are perfectionists by nature, and most have obsessive-compulsive personality tendencies, which may make sticking to a restricted diet easier [2]. On the other hand, bulimia nervosa has many proposed causes, the most important of which are genetic and environmental factors. Anorexia nervosa, as well as the malnutrition that occurs from self-imposed starvation, can create problems in all of the body's major organ systems. Hypokalemia, or a drop in potassium levels in the blood, is a symptom of anorexia nervosa where potassium deficiency can lead to irregular heartbeats, constipation, weariness, muscular degeneration, and paralysis [3]. Symptoms of bulimia nervosa include chronic gastric reflux after eating, secondary to vomiting, dehydration, hypokalemia due to renal potassium loss in the presence of alkalosis and frequent vomiting [4], also hypoglycemia may occur after vomiting. These conditions are diagnosed based on the medical history, symptoms and family history, in addition to an examination of the mental state, with a focus on eating habits and meal frequency. In this paper we have a 40-year-old female patient with anorexia nervosa who suffers from chronic constipation and abdominal pain. When conducting radiological investigations, we discovered an enlargement in fundus of the stomach with a size of 50 cm with a hole in the bottom of the stomach with a size of 5 cm. Surgical intervention was made and the fundus was removed but after two days the patient died due to shock Sepsis as a result of not having a complete gastrostomy.
This case report has been reported in line with the SCARE criteria [5].
2. Case presentation
A 40-year-old woman presented to the emergency room at Ibn Al-Nafees Hospital, Damascus, Syria with a complaint of persistent abdominal pain, vomiting, chronic constipation, and a weight loss of 10 kg during the last 2 months. The patient has no fever or enlarged lymph nodes. Blood pressure at admission was 90/70 mm Hg and a pulse rate was 120/min. In her medical history she just had an anorexia nervosa and used to eat a jalapeno only (hot peppers) for 2 years and there was no history of surgery, medications, or allergies. In the family history the patient's mother was diagnosed with leukemia before 5 years ago and had died. Clinical examination of the head, neck, chest and extremities was normal and the neurological examination was normal. We did some serum testings, which total protein was: 2,8 g/dl, white blood count was: 11,200/ml, alpha-amylase was 425 units/L, serum calcium level was: 0,98 mg. pH level was: 7.54, partial pressure of carbon dioxide (pCO2): 35.5 40 mEq/L, and bicarbonate (HCO3): 30,4 40 mEq/L. Echocardiogram revealed inversion of the T wave on the electrodes IVF-II-III.IV omeprazole was administrated, a nasogastric tube were inserted and a drainage of a 3 L of undigested food and gastric normal secretions were obtained without improvement of the patient symptoms.
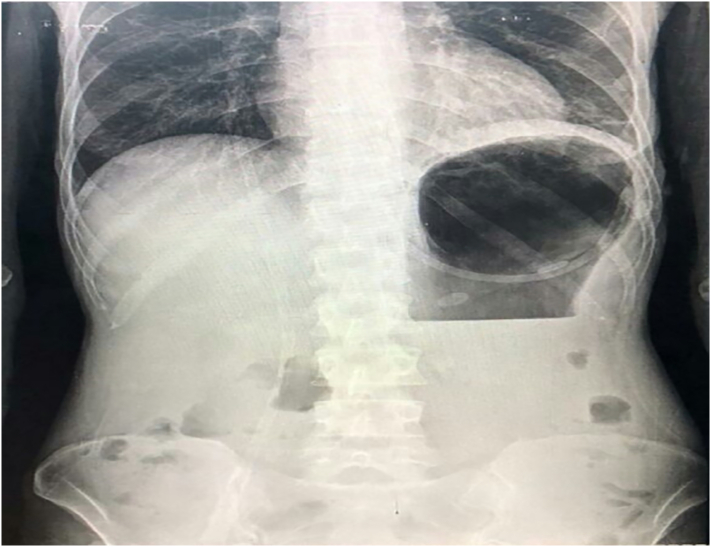
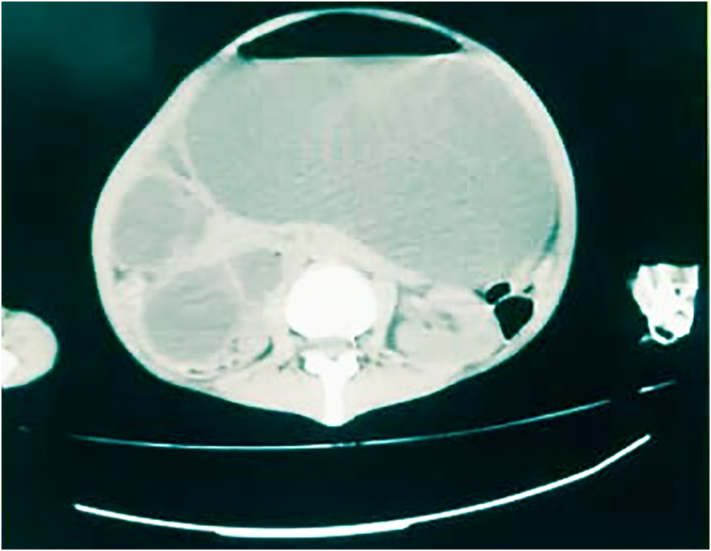
It was not possible to perform abdominal echo due to the enormous expansion of the stomach. The chest and abdomen X-rays revealed the extended fundus towards the base of the left lung and dilated stomach reaching the pelvis borders (Fig. 1). Computed tomography scan confirmed the presence of density at the expense of the left lung with the expansion of the stomach cavity (Fig. 2). An open surgery procedure was performed, performing general anesthesia using through a midline-incision above and below the navel towards reaching the abdominal cavity.
Fig. 1.
X-rays revealed the extended fundus and dilated stomach reaching the pelvis boarders.
Fig. 2.
Computed tomography confirmed the expansion of the stomach cavity.
A substantially enlarged stomach measuring 50 cm in length and a rupture measuring 5 cm in depth with necrotic features in the fundus were discovered during operation. Aside from the flow of acidic secretions and seeds that was accumulated in the stomach as a result of the patient's addiction to eating jalapeno. No volvulus or adhesions were seen. Seven liters of liquids and undigested food was removed from the peritoneal cavity and stomach. Normal pulsations were examined in the superior mesenteric artery. The large curvature of the stomach and the necrotic part was surgically removed by a fundectomy but we didn't resect whole of stomach due to the bad situation of the patient.
Even, the patient had a deteriorated postoperative status, became progressively hypotensive and developed renal failure. The platelet count dropped to 12,000/mm: and pro-thrombin and partial thromboplastic time was elevated to (15–5/12 and 45/36 respectively), also white blood count was: 20,000/ml.
Fibrin split products were absent. On the second hospital day the abdomen distended again and we confirmed the absence of bowel sounds. Re-exploration of the abdomen revealed infarction of the entire stomach and small intestine because we didn't resect all of stomach (gastrostomy).
Unlikely, the patient died a few hours later because he suffered from septic shock after distribution the infections postoperatively. The removed fundus of stomach specimen was massively gangrenous. Microscopically, trans mural ischemic necrosis was evident. The peritoneal cavity was soiled with gastric contents, including seeds of jalapeno. There was no occlusion of the coeliac, superior mesenteric or inferior mesenteric arteries.
The entire small intestine was dilated. The esophagus was unremarkable. Microscopically, fibroid necrosis of small mucosal and sub mucosal vessels of the small intestine were present, but fibrin thrombi characteristic of disseminated intravascular coagulation were conspicuously absent. Most of the findings in the parenchymal organs were those seen in severe shock which was focal infarction of the liver and spleen.
3. Discussion
Anorexia nervosa, which is described as a lack of appetite and/or reduced food consumption, is a well-known geriatric condition [6]. The effects of anorexia on the elderly are expected to worsen. The serious complications of anorexia nervosa are incredibly varied, ranging from minor biological and physical damage to extremely serious and life-threatening conditions; the mortality rate of young subjects with Just an is 4–11%, with a risk of death about 12 times higher than those of subjects of the same age in the general public [7]. In the medical literature there are few cases that reported death after anorexia or bulimia due to gastric dilatation. According to Seung-Mok Youm et al. [8], a 21-year-old girl with a history of bulimia nervosa complained of nausea and retching. The patient's legs changed colour due to abdominal distension. The results of a computed tomography scan revealed significant stomach dilation. In the operating room, they conducted an exploratory laparotomy, but the patient died due to metabolic acidosis and pulmonary alkalosis. A 22-year-old woman with treated anorexia nervosa complained of stomach discomfort and constipation, according to S H Saul et al. [9] Gastric dilatation to the pelvis was verified by abdominal X-rays. The esophagus was closed after the total gastrostomy. The patient died as a result of infarction and perforation caused by acute stomach dilatation, as well as severe and permanent shock. A 19-year-old lady was discovered dead kneeling by the water-closet, according to I. Sinicina et al. [10].
The abdomen was noticeably bloated. A solitary 15-centimeter puncture of the gastric body's front wall was identified. In comparison to previously described cases, our patient differs in a number of ways.
First and mainly, this looks to be the second death in a patient with anorexia nervosa and severe stomach dilation. Second, earlier examples described acute stomach dilatation with moderately perforation.
There was a gastric dilatation of 50 cm in diameter (the expansion of the stomach from the bottom of the diaphragm to the pelvis) and a 5 cm perforation at the level of the fundus in this case.
4. Conclusion
Anorexia nervosa-related gastric perforation is an uncommon and life-threatening complication. As a result, a precise diagnosis must be established as quickly as appropriate, followed by suitable therapy. This should raise clinicians' awareness about the importance of following up on patients with anorexia and bulimia nervosa to investigate the occurrence of digestive disorders. In addition the importance of the prompt surgical treatment or laparotomy of these cases especially resecting all necrotic parts.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Consent
Written informed consent was obtained from the patient's family for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
N/A.
Funding
There are no sources of funding.
Guarantor
Weaam Ezzdean.
Research registration number
Not applicable.
CRediT authorship contribution statement
Sarya Swed: contributed in study concept and design, data collection, and writing the paper.
Weaam Ezzdean: contributed in writing the paper and collecting the data.
Bisher Sawaf: contributed in reviewing the paper.
Declaration of competing interest
All authors declare no conflict of interest.
Acknowledgments
Acknowledgement
We are grateful to Dr. Hidar Alibrahim for aid in data collecting and reviewing the manuscript.
References
- 1.Bardone-Cone A.M., Wonderlich S.A., Frost R.O., Bulik C.M., Mitchell J.E., Uppala S., Simonich H. Perfectionism and eating disorders: current status and future directions. Clin. Psychol. Rev. 2007;27(3):384–405. doi: 10.1016/j.cpr.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Anderluh M.B., Tchanturia K., Rabe-Hesketh S., Treasure J. Childhood obsessive-compulsive personality traits in adult women with eating disorders: defining a broader eating disorder phenotype. Am. J. Psychiatry. 2003;160(2):242–247. doi: 10.1176/appi.ajp.160.2.242. [DOI] [PubMed] [Google Scholar]
- 3.Miller K.K. Endocrine effects of anorexia nervosa. Endocrinol. Metab. Clin. N. Am. 2013;42(3):515–528. doi: 10.1016/j.ecl.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehler P.S., Crews C., Weiner K. Bulimia: medical complications. J. Women's Health (Larchmt) 2004;13(6):668–675. doi: 10.1089/jwh.2004.13.668. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Landi F., Calvani R., Tosato M., Martone A.M., Ortolani E., Savera G., Sisto A., Marzetti E. Anorexia of aging: risk factors, consequences, and potential treatments. Nutrients. 2016;8(2):69. doi: 10.3390/nu8020069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gravina G., Milano W., Nebbiai G., Piccione C., Capasso A. Medical complications in anorexia and bulimia nervosa. Endocr Metab Immune Disord Drug Targets. 2018;18(5):477–488. doi: 10.2174/1871530318666180531094508. [DOI] [PubMed] [Google Scholar]
- 8.Youm S.M., Kim J.Y., Lee J.R. Acute gastric dilatation causing fatal outcome in a young female with eating disorder: a case report. Korean J. Anesthesiol. 2015;68(2):188–192. doi: 10.4097/kjae.2015.68.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saul S.H., Dekker A., Watson C.G. Acute gastric dilatation with infarction and perforation. Report of fatal outcome in patient with anorexia nervosa. Gut. 1981;22(11):978–983. doi: 10.1136/gut.22.11.978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sinicina I., Pankratz H., Büttner A., Mall G. Death due to neurogenic shock following gastric rupture in an anorexia nervosa patient. Forensic Sci. Int. 2005;155(1):7–12. doi: 10.1016/j.forsciint.2004.10.021. [DOI] [PubMed] [Google Scholar]