This cohort study describes the death rates and drug types involved in fatal drug overdoses in the past 15 years among individuals experiencing homelessness in Boston, Massachusetts.
Key Points
Question
What are the temporal patterns in drug overdose mortality among people experiencing homelessness?
Findings
In this cohort study of 60 092 individuals experiencing homeless in Boston, Massachusetts, drug overdose accounted for 1 in 4 deaths. Mortality patterns over time showed a substantial increase in synthetic opioid overdose mortality and a predominance of opioid-involved polysubstance overdose deaths in recent years.
Meaning
The findings suggest that ongoing efforts to improve access to evidence-based opioid overdose prevention strategies and opioid use disorder treatment are needed for people experiencing homelessness.
Abstract
Importance
Despite high rates of drug overdose death among people experiencing homelessness, patterns in drug overdose mortality, including the types of drugs implicated in overdose deaths, remain understudied in this population.
Objective
To describe the patterns in drug overdose mortality among a large cohort of people experiencing homelessness in Boston vs the general adult population of Massachusetts and to evaluate the types of drugs implicated in overdose deaths over a continuous 16-year period of observation.
Design, Setting, and Participants
This cohort study analyzed adults aged 18 years or older who received care at Boston Health Care for the Homeless Program (BHCHP) between January 1, 2003, and December 31, 2017. Individuals were followed up from the date of their initial BHCHP encounter during the study period until the date of death or December 31, 2018. Data were analyzed from December 1, 2020, to June 6, 2021.
Main Outcomes and Measures
Drug overdose deaths and the types of drugs involved in each overdose death were ascertained by linking the BHCHP cohort to the Massachusetts Department of Public Health death records.
Results
In this cohort of 60 092 adults experiencing homelessness (mean [SD] age at entry, 40.4 [13.1] years; 38 084 men [63.4%]), 7130 individuals died by the end of the study period. A total of 1727 individuals (24.2%) died of a drug overdose. Of the drug overdose decedents, 456 were female (26.4%), 194 were Black (11.2%), 202 were Latinx (11.7%), and 1185 were White (68.6%) individuals, and the mean (SD) age at death was 43.7 (10.8) years. The age- and sex-standardized drug overdose mortality rate in the BHCHP cohort was 278.9 (95% CI, 266.1-292.3) deaths per 100 000 person-years, which was 12 times higher than the Massachusetts adult population. Opioids were involved in 91.0% of all drug overdose deaths. Between 2013 and 2018, the synthetic opioid mortality rate increased from 21.6 to 327.0 deaths per 100 000 person-years. Between 2004 and 2018, the opioid-only overdose mortality rate decreased from 117.2 to 102.4 deaths per 100 000 person-years, whereas the opioid-involved polysubstance mortality rate increased from 44.0 to 237.8 deaths per 100 000 person-years. Among opioid-involved polysubstance overdose deaths, cocaine-plus-opioid was the most common substance combination implicated throughout the study period, with Black individuals having the highest proportion of cocaine-plus-opioid involvement in death (0.72 vs 0.62 in Latinx and 0.53 in White individuals; P < .001).
Conclusions and Relevance
In this cohort study of people experiencing homelessness, drug overdose accounted for 1 in 4 deaths, with synthetic opioid and polysubstance involvement becoming predominant contributors to mortality in recent years. These findings emphasize the importance of increasing access to evidence-based opioid overdose prevention strategies and opioid use disorder treatment among people experiencing homelessness, while highlighting the need to address both intentional and unintentional polysubstance use in this population.
Introduction
Drug overdose mortality has increased substantially over the past 20 years in the United States.1 People experiencing homelessness have been disproportionately affected by this public health crisis, with drug overdose emerging as a leading cause of death at rates up to 30-fold higher than in the US general population.2,3,4 Despite these circumstances, temporal patterns in drug overdose mortality and the types of drugs implicated in overdose deaths remain understudied in this population.
In the US general population, drug overdose patterns have demonstrated substantial shifts in the types of drugs implicated in deaths over the past 2 decades. Prescription opioids were initially the predominant drugs involved in overdose-related deaths before a shift to heroin in 2010.5 However, between 2013 and 2019, overdose deaths involving synthetic opioids, such as illicitly manufactured fentanyl, increased by more than 11-fold.5 Polysubstance overdose mortality rates, particularly involving synthetic opioids combined with cocaine and psychostimulants, have also been increasing in recent years.5,6
Public health patterns in the general population are often magnified in people experiencing homelessness, most of whom have high levels of medical and psychosocial comorbidities and are overrepresented in Black and Latinx individuals.7 Understanding drug overdose patterns in this population over time is crucial to advancing health equity across racially, medically, and socioeconomically diverse communities and the health care systems that serve them. The primary objectives of this study were to (1) describe the patterns in drug overdose mortality among a large cohort of people experiencing homelessness in Boston compared with the general adult population of Massachusetts and (2) evaluate the types of drugs implicated in overdose deaths over a continuous 16-year period of observation. Because previous studies found that mortality patterns by race and ethnicity in the homeless community do not always reflect those seen in the larger population,3,8 we also examined drug overdose mortality patterns by race and ethnicity. We believe a comprehensive assessment of drug overdose mortality and the evolving types of drugs involved in overdose deaths will help to inform policy decisions and clinical practice for people experiencing homelessness.
Methods
Participants and Setting
We created a retrospective cohort of adults (aged ≥18 years) who had 1 or more encounters at Boston Health Care for the Homeless Program (BHCHP) between January 1, 2003, and December 31, 2017. The Mass General Brigham Institutional Review Board approved this cohort study and waived the informed consent requirement because the study posed minimal risk to the individuals involved. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.9
Boston Health Care for the Homeless Program provides comprehensive health care services to more than 11 000 patients annually at more than 40 locations in the greater Boston, Massachusetts area.10 To enroll in care at BHCHP, individuals must be currently unhoused; however, some individuals may elect to continue receiving care at BHCHP after they have obtained housing. Internal BHCHP data suggest that approximately 16% to 20% of patients are housed during any given year, although many of these dwellings are in unstable settings that change over time. Thus, this study cohort included individuals who were living on the street, in shelters, or in unstable housing. Individuals were followed up from the date of their initial BHCHP encounter during the study period until the date of death or December 31, 2018.
Race and ethnicity data were obtained from BHCHP or CDC WONDER (Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research) records and were either self-identified or identified based on observation. The following race and ethnicity categories were analyzed: American Indian or Alaska Native, Asian or Pacific Islander, Black, Latinx, White, or other (including >1 race and unknown).
Vital Status
We identified deaths by cross-linking the BHCHP cohort to the Massachusetts Department of Public Health death records from January 1, 2003, to December 31, 2018, using Match*Pro, version 1.6.3 (IMS Inc). Match*Pro is a probabilistic record-linkage software program based on the Fellegi-Sunter method that computes linkage probability weights for possible record pairs.11 The linkage procedure used first and last name, date of birth, and Social Security number. Two of us (D.R.F. and K.A.D.) independently manually reviewed each possible record pair that achieved a probability score of 0.45 or higher. A pair was considered a true linkage if it matched on 1 or more of the following National Death Index criteria: (1) Social Security number; (2) first and last name, and month and year of birth (plus or minus 1 year); or (3) first and last name, and month and day of birth.12 The 2 investigators achieved high concordance and interrater reliability (κ > 0.99). A third investigator adjudicated the discrepancies found. To draw mortality comparisons with the adult population of Massachusetts, we obtained mortality data for the state from the CDC WONDER Underlying Cause of Death files for January 1, 2003, to December 31, 2018.1
Cause of Death
We used the ICD-10 (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision) codes for the underlying cause of death to define drug overdose deaths13 (eTable 1 in the Supplement). We used the multiple cause of death field ICD-10 T codes to identify the types of drugs involved in each drug overdose death14,15,16,17 (eTable 1 in the Supplement). A drug overdose death could involve more than 1 type of drug. T codes are based on toxicological specimens that were obtained during autopsy, from stand-alone postmortem testing, or from antemortem collection during a hospitalization.18 In this cohort, autopsy was performed in 1115 (64.6%) of the 1727 drug overdose decedents, with only 21 overdose decedents (1.2%) missing drug-specific information; these 21 individuals were excluded from drug-specific mortality analyses.
Statistical Analysis
We plotted age- and sex-standardized drug overdose mortality rates over time for the BHCHP cohort and the Massachusetts cohort. We applied indirect standardization, a procedure that calculates the expected mortality rate for an index population, using specific mortality rates stratified by the adjustment variables from a reference population. We used the aggregated Massachusetts adult population from January 1, 2004, to December 31, 2018, as the reference population to calculate age- and sex-standardized yearly mortality rates. We were unable to standardize annual rates by race and ethnicity because of the confidentiality constraints within CDC WONDER (data are suppressed for rows of <10 people). We excluded 2003 data from temporal pattern analyses because insufficient person-years of observation in the BHCHP cohort created highly uncertain mortality estimates for that particular year. However, 2003 data were included in all analyses that were aggregated across years. We presented mortality rates as the number of deaths per 100 000 person-years and fit 95% CIs using exact methods for standardized mortality ratios.
We examined temporal patterns in the drugs implicated in overdose deaths for the BHCHP cohort. Specifically, we evaluated crude drug overdose mortality rates over time by (1) major drug categories involved in death; (2) type of opioids involved in opioid overdose deaths; and (3) polysubstance vs single substance involvement in death, with a focus on deaths that involved opioids. We defined polysubstance-involved overdose mortality as deaths that implicated 2 or more categories of substances, including alcohol. Conversely, single substance–involved overdose mortality was defined as deaths that implicated only 1 drug category and not alcohol.
To assess the variations in drug overdose mortality patterns by race and ethnicity, we performed 3 additional analyses. First, we compared the race and ethnicity–stratified, age- and sex-standardized mortality rates between the BHCHP and Massachusetts cohorts using aggregated data for all study years. We calculated the standardized mortality rate ratios by dividing the standardized mortality rates in the BHCHP cohort by the standardized mortality rates in the Massachusetts cohort. Second, we plotted crude drug overdose mortality rates by race and ethnicity in the BHCHP cohort from 2004 through 2018. Third, we assessed opioid-involved polysubstance overdose mortality rates by race and ethnicity over the entire study period. We performed Fisher exact tests to evaluate the differences by race and ethnicity in the proportions of deaths in major polysubstance categories. A 2-sided P < .05 was considered to be statistically significant.
To present a comprehensive analysis of drug overdose mortality patterns among people experiencing homelessness, we performed these same 3 analyses by sex as well. We used RStudio, version 1.2.5033 (RStudio) and Microsoft Excel (Microsoft Corp) for all analyses, which were conducted from December 1, 2020, to June 6, 2021.
Results
Cohort Characteristics
A total of 60 092 adults experiencing homelessness who were enrolled to receive care at BHCHP were followed up for a median duration of 8.7 years, yielding 520 429.6 person-years of observation. This BHCHP cohort had a mean (SD) age at entry of 40.4 (13.1) years and was composed of 38 084 men (63.4%) and 22 008 women (36.6%). Of these patients, 15 928 were of Black (26.5%), 10 773 of Latinx (17.9%), and 26 364 of White (43.9%) race and ethnicity (Table).
Table. Characteristics of Adults Enrolled in the Boston Health Care for the Homeless Program (BHCHP) Cohort From 2003 to 2017.
| Characteristic | No. (%) | ||
|---|---|---|---|
| BHCHP cohort | Decedents (n = 7130) | ||
| Drug overdose | Other causes of death | ||
| No. of enrolled adults | 60 092 | 1727 | 5403 |
| Age at enrollment, mean (SD), y | 40.4 (13.1) | 38.5 (10.3) | 50.9 (11.6) |
| Sex | |||
| Male | 38 084 (63.4) | 1271 (73.6) | 4258 (78.8) |
| Female | 22 008 (36.6) | 456 (26.4) | 1145 (21.2) |
| Race and ethnicitya | |||
| American Indian or Alaska Native | 316 (0.5) | 6 (0.3) | 27 (0.5) |
| Asian or Pacific Islander | 749 (1.2) | 6 (0.3) | 35 (0.6) |
| Black | 15 928 (26.5) | 194 (11.2) | 1306 (24.2) |
| Latinx | 10 773 (17.9) | 202 (11.7) | 508 (9.4) |
| White | 26 364 (43.9) | 1185 (68.6) | 3201 (59.2) |
| Otherb | 5962 (9.9) | 134 (7.8) | 326 (6.0) |
| Age at death, mean (SD), y | NA | 43.7 (10.8) | 56.9 (12.2) |
| Autopsy performed | NA | 1115 (64.6) | 1301 (24.1) |
| Place of death | |||
| Hospital | NA | 448 (25.9) | 2568 (47.5) |
| Dead on arrival to hospital | NA | 231 (13.4) | 126 (2.3) |
| Residence | NA | 376 (21.8) | 532 (9.8) |
| Nursing home or assisted living | NA | 433 (25.1) | 1464 (27.1) |
| Hospice | NA | 3 (0.2) | 544 (10.1) |
| Other or unknown | NA | 236 (13.7) | 169 (3.1) |
Abbreviation: NA, not applicable.
Race and ethnicity data were obtained from BHCHP records and were either self-identified or identified based on observation.
Other race and ethnicity included more than 1 race and unknown.
A total of 7130 patients died by the end of the study period. Drug overdose accounted for 1727 deaths (24.2%). Among those who died from a drug overdose, 1271 (73.6%) were male, 456 were female (26.4%), 194 were Black (11.2%), 202 were Latinx (11.7%), and 1185 were White (68.6%) individuals. The mean (SD) age at death was 43.7 (10.8) years among those who died of drug overdose compared with 56.9 (12.2) years among those who died of other causes.
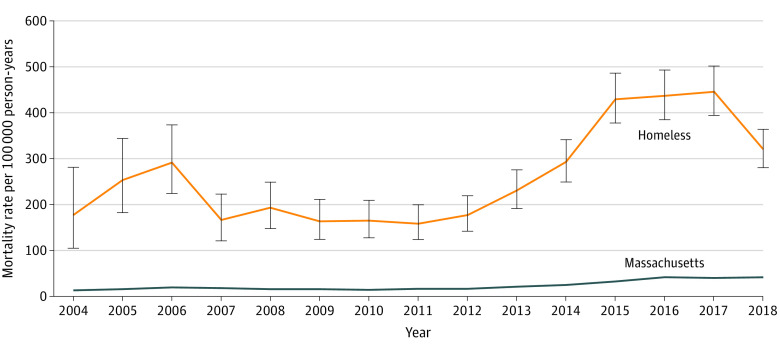
Drug Overdose Mortality in BHCHP vs Massachusetts Cohort
The age- and sex-standardized drug overdose mortality rate in the BHCHP cohort was 12 times higher than in the Massachusetts general population (278.9 [95% CI, 266.1-292.3] vs 23.2 [95% CI, 22.8-23.5] deaths per 100 000 person-years). Between 2004 and 2018, the drug overdose mortality rate increased from 177.6 to 321.1 deaths per 100 000 person-years in the BHCHP cohort (Figure 1).
Figure 1. Drug Overdose Mortality in the Boston Health Care for the Homeless Program (BHCHP) Cohort vs the Massachusetts Adult Population From 2004 to 2018.
Age and sex indirect standardization was applied each year to both the BHCHP cohort (orange line) and the Massachusetts population (blue line) using the aggregated 2004 to 2018 Massachusetts adult population as the reference population. Error bars represent 95% CIs.
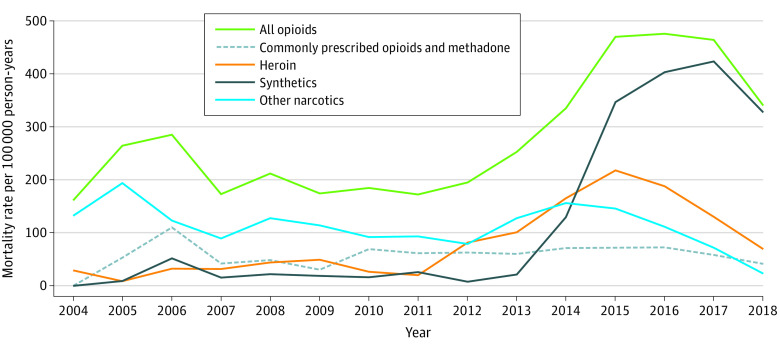
Drugs Implicated in Overdose Deaths
Opioids were the leading drug category involved in overdose deaths (1571 of 1727 [91.0%]), followed by cocaine (632 [36.6%]) and benzodiazepines (279 [16.2%]). Between 2004 and 2018, the opioid-involved overdose mortality rate increased from 161.2 to 340.2 deaths per 100 000 person-years (Figure 2). The composition of opioid-involved deaths changed over time. Between 2013 and 2018, the synthetic opioid mortality rate increased from 21.6 to 327.0 deaths per 100 000 person-years (Figure 3). In 2018, synthetic opioids were involved in 96.1% of all opioid-involved deaths (199 of 207) compared with 0% (0 of 11) in 2004.
Figure 2. Drug Overdose Mortality in the Boston Health Care for the Homeless Program Cohort by Type of Drug Involved From 2004 to 2018.
aOther includes antidepressants, antipsychotics, barbiturates, and other neuroleptics and sedatives. Drug categories are not mutually exclusive.
Figure 3. Opioid-Involved Mortality in the Boston Health Care for the Homeless Program Cohort by Type of Opioid Involved From 2004 to 2018.
Opioid categories are not mutually exclusive.
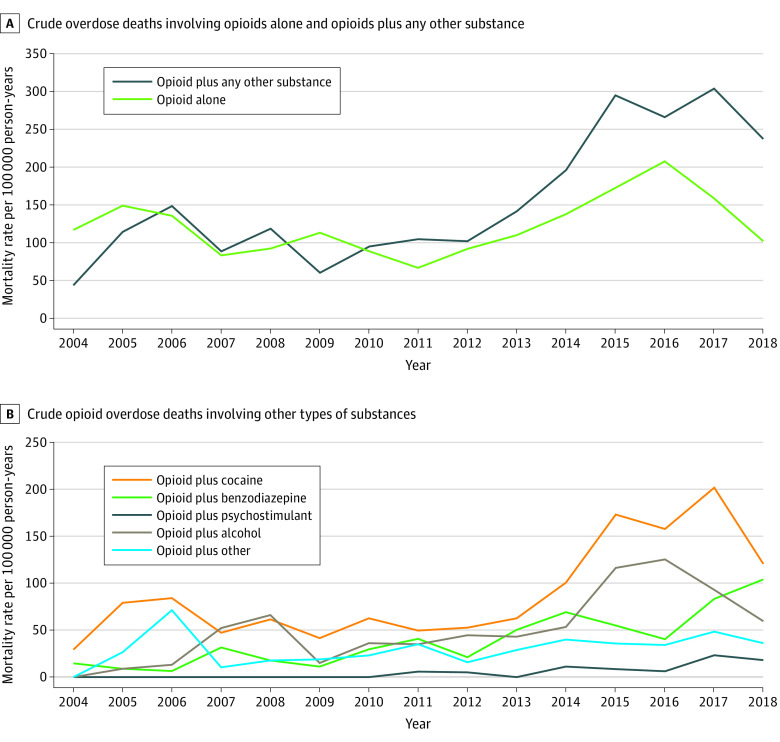
Opioids were involved in 93.6% of all polysubstance-involved deaths (923 of 986) (eTable 2 in the Supplement). Between 2004 and 2018, the opioid-only mortality rate decreased from 117.2 to 102.4 deaths per 100 000 person-years, whereas the opioid-involved polysubstance mortality rate increased from 44.0 to 237.8 deaths per 100 000 person-years (Figure 4). In 2018, opioid-involved polysubstance deaths accounted for 64.6% of all drug overdose deaths (144 of 223). Cocaine-plus-opioid was the most common substance combination implicated in opioid-involved polysubstance deaths across the study period (Figure 4).
Figure 4. Opioid-Involved Polysubstance Overdose Mortality in the Boston Health Care for the Homeless Program Cohort From 2004 to 2018.
Categories of substance combination involvement are not mutually exclusive.
Drug Overdose Mortality Patterns by Race and Ethnicity
When comparing the aggregated drug overdose mortality rate in the BHCHP cohort vs the Massachusetts cohort, the standardized mortality rate ratio was the lowest in Black individuals (5.5; 95% CI, 4.8-6.3) and the highest in Asian or Pacific Islander individuals (44.3; 95% CI, 18.0-92.2) (eFigure 1 in the Supplement). Between 2004 and 2018, the drug overdose mortality rate increased from 128.4 to 148.0 deaths per 100 000 person-years among Black individuals, from 77.2 to 245.6 deaths per 100 000 person-years among Latinx individuals, and from 367.9 to 557.1 deaths per 100 000 person-years among White individuals (eFigure 2 in the Supplement).
Substance combinations in opioid-involved polysubstance mortality differed by race and ethnicity. Black individuals had the highest proportion of cocaine-plus-opioid (0.72 vs 0.62 in Latinx and 0.53 in White individuals; P < .001) and alcohol-plus-opioid (0.44 vs 0.41 in Latinx and 0.33 in White individuals; P = .009) involvement in overdose death, whereas White individuals had the highest proportion of benzodiazepine-plus-opioid involvement (0.32 vs 0.07 in Black and 0.20 in Latinx individuals; P < .001) (eTable 3 in the Supplement).
Drug Overdose Mortality Patterns by Sex
When comparing the aggregated drug overdose mortality rate in the BHCHP cohort vs the Massachusetts cohort, the standardized mortality rate ratio among men was 11.3 (95% CI, 10.7-11.9) and 16.2 (95% CI, 14.8-17.8) among women (eFigure 3 in the Supplement). Across the study period, drug overdose mortality rates were higher among men (eFigure 4 in the Supplement). Drug combinations in opioid-involved polysubstance mortality differed by sex. Men had a higher proportion of alcohol-plus-opioid involvement in overdose death compared with women (0.37 vs 0.25; P = .002), whereas women had a higher proportion of benzodiazepine-plus-opioid involvement compared with men (0.34 vs 0.25; P = .009) (eTable 4 in the Supplement).
Discussion
This comprehensive, large-scale cohort study of drug overdose mortality patterns among adults experiencing homelessness presents 4 major findings. First, drug overdose mortality increased 81% between 2004 and 2018, with a standardized mortality rate that was 12 times higher than in the Massachusetts cohort when aggregated across all years. Second, synthetic opioid–involved mortality increased sharply during the study period, with synthetic opioids almost universally present in opioid-involved overdose deaths by 2018. Third, polysubstance opioid overdose deaths have surpassed opioid–only overdose deaths. Fourth, drug overdose mortality patterns varied by race and ethnicity.
As has been reported in previous studies that evaluated patterns in drug overdose mortality among people experiencing homelessness,19,20 drug overdose was the leading cause of death in this population, with drug overdoses accounting for 1 in every 4 deaths. In contrast to these previous studies, which consisted of cohorts in California and had a predominance of psychostimulant-involved deaths, the present study found that opioids were involved in 91.0% of all overdose deaths. Although the overdose mortality rate in the BHCHP cohort declined in 2018 (the last year for which mortality data were available at the time of the analysis), data from the US general population suggested that this decrease could be short lived. In 2018, the US experienced a reduction in drug overdose mortality for the first time in more than 3 decades21; however, these rates started to increase again in 201922 and accelerated throughout 2020 during the COVID-19 pandemic.23
In the BHCHP cohort, synthetic opioid mortality surged by more than 1400% between 2013 and 2018. Opioid overdose mortality became nearly synonymous with synthetic opioid overdose mortality in this population. Synthetic opioids, such as illegally manufactured fentanyl, were involved in 96.1% of opioid-related deaths in 2018. Because opioids were implicated in nearly all drug overdose deaths, synthetic opioids became predominant in drug overdose mortality in the BHCHP cohort.
Polysubstance overdose deaths involving opioids increased in prevalence during the study period, accounting for 2 of every 3 drug overdose deaths (64.6%) in 2018. This pattern has been reported in the US general population, although with mortality rates that were substantially lower than those in the BHCHP cohort.5,16,22 As previously found in the Massachusetts population, most opioid-involved polysubstance deaths in the BHCHP cohort included cocaine.24
Drug overdose mortality was higher among all racial and ethnic groups in the BHCHP cohort than in the Massachusetts cohort. However, the relative difference in mortality was substantially larger among White individuals than that observed among Black and Latinx individuals. Similar findings have been observed in previous mortality studies of people experiencing homelessness3,8 and may reflect the underlying mechanisms of structural racism. The path toward homelessness often differs according to a person’s race and ethnicity, with factors such as discriminatory housing policies, unequal economic opportunities, and disproportionate involvement in the criminal-legal system playing an outsized role for Black and Latinx individuals.25 Conversely, mental illness and substance use disorders are more prevalent factors associated with homelessness among White individuals,26 potentially contributing to more adverse substance use disorder–related outcomes. In addition, limited access to opioid overdose prevention programs and lack of long-term retention in addiction treatment among housed Black and Latinx individuals27,28,29,30,31,32,33,34 may further contribute to the reduced disparity between these individuals and their unhoused counterparts as compared with housed and unhoused White individuals. Between 2010 and 2017, the mortality patterns by race and ethnicity in the BHCHP cohort reflected those observed in the US general population,35 with Black and Latinx individuals experiencing faster relative increases in drug overdose mortality compared with White persons.
We believe the findings of this study have important policy and clinical implications. The substantial increase in opioid overdose deaths, particularly synthetic opioid–involved deaths, highlights the need to improve access to evidence-based opioid use disorder treatment and overdose prevention strategies, such as supervised injection facilities,36 fentanyl testing strips,37 and naloxone distribution,38 among people experiencing homelessness. During the years under study, BHCHP provided substance use disorder treatment primarily in office-based settings.39 To better reach this population, addiction and harm-reduction services may need to be provided in nontraditional settings, such as mobile addiction vans, shelters, supportive housing, and other places where homeless-experienced individuals with substance use disorders congregate.39,40 Furthermore, given the high burden of comorbid mental health disease in this population,41 expanding access to behavioral health services may improve outcomes.
The predominance of opioid-involved polysubstance overdose deaths reflects a nationwide shift in drug overdose patterns.5,16,22 Clinicians who serve people experiencing homelessness should take a broad approach to assessing for all types of drug use to appropriately tailor treatment. Although evidence-based treatment options for other drug use disorders are somewhat limited, contingency management has been found to be an effective treatment strategy for both opioid use disorder and stimulant use disorder.42,43 Polysubstance use can be intentional, but individuals who use drugs are sometimes inadvertently or unknowingly exposed to other drugs, particularly synthetic opioids. The same harm-reduction strategies mentioned earlier, in addition to a low-barrier, safer drug supply44 and educational efforts that address unintentional opioid exposure, need to be accessible to all homeless-experienced individuals who use drugs.
Limitations
This study has several limitations. The findings may not be generalizable to people experiencing homelessness in Boston who sought care outside of BHCHP or who do not engage with the health care system at all. Although it is difficult to accurately characterize the general homeless population, limited demographic data from the City of Boston’s annual homeless census suggest that the BHCHP cohort’s racial and ethnic breakdown is similar to that of Boston’s general homeless population.45 In addition, drug overdose patterns differ by geographic region; thus, the findings of this study may not be generalizable to nonurban or non–East Coast settings.
Death categorization in death certificates can lack sensitivity and specificity. In the US general population, only 8% of deceased individuals undergo an autopsy,46 with up to 25% of all drug overdose deaths missing drug-specific information in the multiple cause of death fields.47 In the BHCHP cohort, however, the autopsy rate among drug overdose decedents was 64.6%, with only 1.2% missing drug-specific information, thereby providing some reassurance that the cause of death information was more complete than the information available for the US general population. In addition, it is likely that the drugs involved in overdose deaths were sometimes coded into the broadest category available, limiting the accuracy of drug-specific estimates. Furthermore, the lack of specific drug codes for fentanyl and methamphetamine made it difficult to accurately quantify these drug-specific mortality rates. Many of these limitations are inherent in any study of drug overdose mortality and are not unique to the BHCHP cohort.
Conclusions
In this large, Boston-based cohort of people experiencing homelessness, drug overdose mortality was 12 times higher than in the general Massachusetts population and accounted for approximately 1 in every 4 deaths. Opioids were implicated in most drug overdose deaths, with synthetic opioids and polysubstance involvement becoming predominant in recent years. These findings highlight the need to improve access to evidence-based opioid overdose prevention strategies and opioid use disorder treatment and to address both intentional and unintentional polysubstance use in this population. Variations in overdose patterns by race and ethnicity emphasize the need to remove structural barriers to addiction care.
eTable 1. ICD-10 Codes Defining Drug Overdose and the Types of Drugs Implicated in Deaths
eTable 2. Polysubstance Drug Overdose Mortality by Drug Categories Involved in Death in the Boston Health Care for the Homeless Cohort From 2004 to 2018
eFigure 1. Drug Overdose Mortality in the Boston Health Care for the Homeless Cohort, Stratified by Race and Ethnicity
eFigure 2. Crude Drug Overdose Mortality in the Boston Health Care for the Homeless Cohort From 2004 to 2018, Stratified by Race and Ethnicity
eTable 3. Opioid-Involved Overdose Mortality by Race and Ethnicity in the Boston Health Care for the Homeless Cohort
eFigure 3. Drug Overdose Mortality in a Cohort of Homeless-Experienced Adults, Stratified by Sex
eFigure 4. Crude Drug Overdose Mortality in the Boston Health Care for the Homeless Cohort From 2004 to 2018, Stratified by Sex
eTable 4. Opioid-Involved Overdose Mortality by Sex in the Boston Health Care for the Homeless Cohort
References
- 1.CDC WONDER . About underlying cause of death, 1999-2019. Accessed April 24, 2021. https://wonder.cdc.gov/ucd-icd10.html
- 2.Jasuja GK, Bettano A, Smelson D, et al. Homelessness and veteran status in relation to nonfatal and fatal opioid overdose in Massachusetts. Med Care. 2021;59(suppl 2):S165-S169. doi: 10.1097/MLR.0000000000001437 [DOI] [PubMed] [Google Scholar]
- 3.Baggett TP, Hwang SW, O’Connell JJ, et al. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med. 2013;173(3):189-195. doi: 10.1001/jamainternmed.2013.1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massachusetts Department of Public Health . Data brief: an assessment of opioid-related overdoses in Massachusetts 2011-2015. Accessed May 13, 2021. https://www.mass.gov/doc/chapter-55-data-brief-2017/download
- 5.Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths - United States, 2013-2019. MMWR Morb Mortal Wkly Rep. 2021;70(6):202-207. doi: 10.15585/mmwr.mm7006a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones CM, Underwood N, Compton WM. Increases in methamphetamine use among heroin treatment admissions in the United States, 2008-17. Addiction. 2020;115(2):347-353. doi: 10.1111/add.14812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henry M, de Sousa T, Roddey C, Gayen S, Bednar TJ. The 2020. Annual Homeless Assessment Report (AHAR) to Congress: Part 1: Part-in-Time Estimates of Homelessness. US Department of Housing and Urban Development, Office of Community Planning and Development; 2021. Accessed November 30, 2021. https://www.huduser.gov/portal/sites/default/files/pdf/2020-AHAR-Part-1.pdf
- 8.Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331(5):304-309. doi: 10.1056/NEJM199408043310506 [DOI] [PubMed] [Google Scholar]
- 9.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-577. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 10.Boston Health Care for the Homeless Program . Accessed April 21, 2021. https://www.bhchp.org/
- 11.Surveillance, Epidemiology, and End Results Program . Match*Pro status update. Accessed April 21, 2021. https://seer.cancer.gov/seerdms/portal/face-to-face-meetings/2018-face-to-face-meeting/matchproseermtg.pdf
- 12.National Center for Health Statistics . National Death Index user’s guide. Accessed January 13, 2021. https://www.cdc.gov/nchs/data/ndi/ndi_users_guide.pdf
- 13.Substance Abuse and Mental Health Services Administration . Using International Classification of Diseases (ICD) codes to assess opioid-related overdose deaths. Accessed January 20, 2021. https://mnprc.org/wp-content/uploads/2019/01/using-icd-10-codes-to-assess-opioid-related-overdose-deaths.pdf
- 14.Wilson N, Kariisa M, Seth P, Smith H IV, Davis NL. Drug and opioid-involved overdose deaths - United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290-297. doi: 10.15585/mmwr.mm6911a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010-2016. JAMA. 2018;319(17):1819-1821. doi: 10.1001/jama.2018.2844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lim JK, Earlywine JJ, Bagley SM, Marshall BDL, Hadland SE. Polysubstance involvement in opioid overdose deaths in adolescents and young adults, 1999-2018. JAMA Pediatr. 2021;175(2):194-196. doi: 10.1001/jamapediatrics.2020.5035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential - United States, 2003-2017. MMWR Morb Mortal Wkly Rep. 2019;68(17):388-395. doi: 10.15585/mmwr.mm6817a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prahlow JA, Brooks EG, Jones P Jr. Drug overdose deaths and toxicology tests: let’s talk. CAP Today. Accessed October 25, 2021. https://www.captodayonline.com/drug-overdose-deaths-and-toxicology-tests-lets-talk/2/?print=pdf
- 19.Los Angeles County Department of Public Health, Center for Health Impact Evaluation . Recent trends in mortality rates and causes of death among people experiencing homelessness in Los Angeles County. January 2021. Accessed October 25, 2021. http://www.publichealth.lacounty.gov/chie/reports/HomelessMortality2020_CHIEBrief_Final.pdf
- 20.Cawley CL, Kanzaria HK, Kushel M, Raven MC, Zevin B. Mortality among people experiencing homelessness in San Francisco 2016-2018. J Gen Intern Med. Published online April 9, 2021. doi: 10.1007/s11606-021-06769-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999-2018. NCHS Data Brief, no 356. January 2020. Accessed May 3, 2021. https://www.cdc.gov/nchs/data/databriefs/db356-h.pdf [PubMed]
- 22.National Institute on Drug Abuse . Overdose death rates. Accessed May 3, 2021. https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates
- 23.Centers for Disease Control and Prevention . Overdose deaths accelerating during COVID-19. Accessed May 3, 2021. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
- 24.Barocas JA, Wang J, Marshall BDL, et al. Sociodemographic factors and social determinants associated with toxicology confirmed polysubstance opioid-related deaths. Drug Alcohol Depend. 2019;200:59-63. doi: 10.1016/j.drugalcdep.2019.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olivet J, Wilkey C, Richard M, et al .. Racial inequity and homelessness: findings from the SPARC Study. Ann Am Acad Pol Soc Sci. 2021;693(1):82-100. doi: 10.1177/0002716221991040 [DOI] [Google Scholar]
- 26.North CS, Smith EM. Comparison of White and nonWhite homeless men and women. Soc Work. 1994;39(6):639-647. [PubMed] [Google Scholar]
- 27.Goedel WC, Shapiro A, Cerdá M, Tsai JW, Hadland SE, Marshall BDL. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3(4):e203711. doi: 10.1001/jamanetworkopen.2020.3711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Netherland J, Hansen H. White opioids: pharmaceutical race and the war on drugs that wasn’t. Biosocieties. 2017;12(2):217-238. doi: 10.1057/biosoc.2015.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. 2019;76(9):979-981. doi: 10.1001/jamapsychiatry.2019.0876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hansen H, Netherland J. Is the prescription opioid epidemic a White problem? Am J Public Health. 2016;106(12):2127-2129. doi: 10.2105/AJPH.2016.303483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kilaru AS, Xiong A, Lowenstein M, et al. Incidence of treatment for opioid use disorder following nonfatal overdose in commercially insured patients. JAMA Netw Open. 2020;3(5):e205852. doi: 10.1001/jamanetworkopen.2020.5852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weinstein ZM, Kim HW, Cheng DM, et al. Long-term retention in office based opioid treatment with buprenorphine. J Subst Abuse Treat. 2017;74:65-70. doi: 10.1016/j.jsat.2016.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kinnard EN, Bluthenthal RN, Kral AH, Wenger LD, Lambdin BH. The naloxone delivery cascade: identifying disparities in access to naloxone among people who inject drugs in Los Angeles and San Francisco, CA. Drug Alcohol Depend. 2021;225:108759. doi: 10.1016/j.drugalcdep.2021.108759 [DOI] [PubMed] [Google Scholar]
- 34.Madden EF, Qeadan F. Racial inequities in U.S. naloxone prescriptions. Subst Abus. 2020;41(2):232-244. doi: 10.1080/08897077.2019.1686721 [DOI] [PubMed] [Google Scholar]
- 35.Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. JAMA. 2019;322(20):1996-2016. doi: 10.1001/jama.2019.16932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kennedy MC, Hayashi K, Milloy MJ, Wood E, Kerr T. Supervised injection facility use and all-cause mortality among people who inject drugs in Vancouver, Canada: a cohort study. PLoS Med. 2019;16(11):e1002964. doi: 10.1371/journal.pmed.1002964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krieger MS, Goedel WC, Buxton JA, et al. Use of rapid fentanyl test strips among young adults who use drugs. Int J Drug Policy. 2018;61:52-58. doi: 10.1016/j.drugpo.2018.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. doi: 10.1136/bmj.f174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fine DR, Lewis E, Weinstock K, Wright J, Gaeta JM, Baggett TP. Office-based addiction treatment retention and mortality among people experiencing homelessness. JAMA Netw Open. 2021;4(3):e210477. doi: 10.1001/jamanetworkopen.2021.0477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meges D, Zevin B, Cookson E, et al, eds. Adapting Your Practice: Recommendations for the Care of Homeless Patients With Opioid Use Disorders. Health Care for the Homeless Clinicians’ Network, National Health Care for the Homeless Council, Inc; 2014. Accessed May 4, 2021. https://opioidresponsenetwork.org/ResourceMaterials/hch-opioid-use-disorders_adapting-your-practice-final-to-post.pdf
- 41.Bauer LK, Brody JK, León C, Baggett TP. Characteristics of homeless adults who died of drug overdose: a retrospective record review. J Health Care Poor Underserved. 2016;27(2):846-859. doi: 10.1353/hpu.2016.0075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ronsley C, Nolan S, Knight R, et al. Treatment of stimulant use disorder: a systematic review of reviews. PLoS One. 2020;15(6):e0234809. doi: 10.1371/journal.pone.0234809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bolívar HA, Klemperer EM, Coleman SRM, DeSarno M, Skelly JM, Higgins ST. Contingency management for patients receiving medication for opioid use disorder: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(10):1092-1102. doi: 10.1001/jamapsychiatry.2021.1969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ivsins A, Boyd J, Beletsky L, McNeil R. Tackling the overdose crisis: the role of safe supply. Int J Drug Policy. 2020;80:102769. doi: 10.1016/j.drugpo.2020.102769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.City of Boston. Annual homeless census. Accessed October 25, 2021. https://www.boston.gov/sites/default/files/file/2021/04/2021%20Census%20Memo.pdf
- 46.Goldman L. Autopsy 2018: still necessary, even if occasionally not sufficient. Circulation. 2018;137(25):2686-2688. doi: 10.1161/CIRCULATIONAHA.118.033236 [DOI] [PubMed] [Google Scholar]
- 47.Warner M, Paulozzi LJ, Nolte KB, Davis GG, Nelson LS. State variation in certifying manner of death and drugs involved in drug-intoxication deaths. Acad Forensic Pathol. 2013;3(2):231-237. doi: 10.23907/2013.029 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. ICD-10 Codes Defining Drug Overdose and the Types of Drugs Implicated in Deaths
eTable 2. Polysubstance Drug Overdose Mortality by Drug Categories Involved in Death in the Boston Health Care for the Homeless Cohort From 2004 to 2018
eFigure 1. Drug Overdose Mortality in the Boston Health Care for the Homeless Cohort, Stratified by Race and Ethnicity
eFigure 2. Crude Drug Overdose Mortality in the Boston Health Care for the Homeless Cohort From 2004 to 2018, Stratified by Race and Ethnicity
eTable 3. Opioid-Involved Overdose Mortality by Race and Ethnicity in the Boston Health Care for the Homeless Cohort
eFigure 3. Drug Overdose Mortality in a Cohort of Homeless-Experienced Adults, Stratified by Sex
eFigure 4. Crude Drug Overdose Mortality in the Boston Health Care for the Homeless Cohort From 2004 to 2018, Stratified by Sex
eTable 4. Opioid-Involved Overdose Mortality by Sex in the Boston Health Care for the Homeless Cohort