Abstract
Background
Strategies to improve the community food environment have been recommended for addressing childhood obesity, but evidence substantiating their effectiveness is limited.
Objective
Our aim was to examine the impact of changes in availability of key features of the community food environment, such as supermarkets, small grocery stores, convenience stores, upgraded convenience stores, pharmacies, and limited service restaurants, on changes in children’s body mass index z scores (zBMIs).
Design
We conducted a longitudinal cohort study.
Participants/setting
Two cohorts of 3- to 15-year-old children living in 4 low-income New Jersey cities were followed during 2- to 5-year periods from 2009 through 2017. Data on weight status were collected at 2 time points (T1 and T2) from each cohort; data on food outlets in the 4 cities and within a 1-mile buffer around each city were collected multiple times between T1 and T2.
Main outcome measures
We measured change in children’s zBMIs between T1 and T2.
Statistical analysis
Changes in the food environment were conceptualized as exposure to changes in counts of food outlets across varying proximities (0.25 mile, 0.5 mile, and 1.0 mile) around a child’s home, over different lengths of time a child was exposed to these changes before T2 (12 months, 18 months, and 24 months). Multivariate models examined patterns in relationships between changes in zBMI and changes in the food environment.
Results
Increased zBMIs were observed in children with greater exposure to convenience stores over time, with a consistent pattern of significant associations across varying proximities and lengths of exposure. For example, exposure to an additional convenience store over 24 months within 1 mile of a child’s home resulted in 11.7% higher odds (P = 0.007) of a child being in a higher zBMI change category at T2. Lower zBMIs were observed in children with increased exposure to small grocery stores selling an array of healthy items, with exposure to an additional small grocery store within 1 mile over 24 months, resulting in 37.3% lower odds (P < 0.05) of being in a higher zBMI change category at T2. No consistent patterns were observed for changes in exposure to supermarkets, limited service restaurants, or pharmacies.
Conclusions
Increased availability of small grocery stores near children’s homes may improve children’s weight status, whereas increased availability of convenience stores is likely to be detrimental.
Keywords: Childhood obesity, Food environment, Change in BMI, Obesity, Children, Longitudinal study, Cohort study
The centers for disease control and prevention (CDC) and the Institute of Medicine have used the social ecological and systems framework to address the high prevalence and growing rates of childhood obesity.1–3 This approach has extended the focus from solely individual-level factors as determinants of obesity to also examining the role of policies and environments. In the past decade, organizations and communities have developed interventions that align with the social ecological framework to promote food-related policies and improve environments aiming to achieve population-level impacts on children’s weight outcomes.4,5 Such efforts have focused on expanding access to healthy food outlets, especially in areas considered food deserts,6 and on increasing availability of nutritious foods in retail and school venues.7 However, conclusive evidence of the impact of changes in specific aspects of the community food environment on weight outcomes is notably lacking.8,9 As a result, communities are left without a clear path for achieving intended health outcomes through interventions to improve their food environments.
Systematic reviews identified difficulties in specifying best practices, citing differing methodologies, as well as an absence of consensus among studies. Nonetheless, some consistent results have emerged. Cobb and colleagues8 reviewed 71 studies, 23 of which focused on effects among children. The vast majority of the studies included in the review reported null results, but half of the studies that focused on the relationship between convenience stores and weight outcomes found that children’s weight increased with greater convenience store exposure.8 Higher fast-food availability was associated with higher weight in children, but only in low-income populations.8 In their reviews, both Cobb and colleagues and Zhou and colleagues9 summarized the complex associations between supermarket availability and children’s weight status, finding no relationships in the majority of studies. Moreover, some studies reported negative associations (higher supermarket availability associated with lower weight), as well as positive associations (higher supermarket availability associated with higher weight).
Descriptive studies highlight disparities in healthy food access; specifically, lower-income communities, communities with higher percentages of racial or ethnic minorities, and communities with a higher burden of obesity10 tend to have both greater access to outlets that sell unhealthy food11 and lower access to those selling healthy food.12 Until recently, the bulk of the research examining the role of food environments and children’s weight outcomes has been cross-sectional in design.13,14 Although informative, these studies seldom control for potential confounding variables and do not allow for causal inferences.15,16 In addition, cross-sectional studies cannot account for ongoing changes in the environment, such as store openings and closings, or for the prospect that residents might choose to live in particular neighborhoods based on their preferences for particular food environments, and stores might locate in specific neighborhoods in response to anticipated demand among the resident population for their products.
In recent years, longitudinal studies have taken advantage of known, impending changes to community food environments, such as a planned opening of a new store.17,18 Although these pre–post studies can control for time-invariant confounders, they have been limited in their ability to account for contemporaneous changes occurring in the food environment,17 have typically assessed outcomes after only a relatively short period of exposure to changes,18,19 and have mostly focused on one specific environmental change, such as the opening of a new supermarket in a community,17,18 limiting the scope and generalizability of findings. Other recent efforts to establish a relationship between changes in the food environment and children’s weight status have relied on retrospective study designs.20–23 Although such studies have the benefit of longer follow-up periods, they typically rely on historical data on the food environment collected for nonresearch purposes. These commercial data are prone to biases and classification errors24; adequately addressing these inaccuracies requires that investigators reclassify stores using additional information collected in real time.25
The current study addressed many of these shortcomings by using a prospective cohort design with a high degree of control to examine the relationship between changes in availability of a comprehensive array of food environment features, such as supermarkets, small grocery stores, convenience stores, upgraded convenience stores, pharmacies, and limited service restaurants, and changes in children’s weight status, during a 2–5-year period.
METHODS
The New Jersey Child Heath Study, designed to answer the main research question addressed here, used the “natural experiment” framework that the National Institutes of Health identified as a key methodology for evaluating obesity prevention efforts in real-world settings.26 In this context, natural experiments examine variation in exposures resulting from planned or unplanned changes using design and analytical features that can support causal inference.27 During a 2- to 5-year period, the New Jersey Child Heath Study followed 2 cohorts of 3- to 15-year-old children living in low-income, high-minority cities, and captured detailed information on achievement of intended changes in the environment around children’s homes (eg, resulting from interventions implemented by community organizations as part of ongoing initiatives) and unintended changes (eg, naturally occurring or driven by market forces). Appropriate to application of the natural experiment framework, the 4 New Jersey cities—Camden, New Brunswick, Newark, and Trenton—were known to be initiating numerous policy and environmental changes aimed at childhood obesity prevention among school-aged children through a number of community-based initiatives undertaken independent of the investigators, including those supported by the Robert Wood Johnson Foundation, Campbell Soup Company, and CDC.28–30 The longitudinal design strengthened causal inferences that can be drawn from the data by following 2 cohorts of children over time, thereby controlling for unmeasured individual-level characteristics; assessing the relationship between changes in the community food environment and changes in weight status, thereby informing the causal direction of associations; and measuring each child’s exposure to changes in multiple features of the food environment, varying across the sample, allowing the analysis to control for key contemporaneous changes. Comprehensive data were collected at the individual, household, and community levels. The Rutgers and Arizona State University Institutional Review Boards approved the study protocol.
Household Survey
Between 2009 and 2017, survey data were collected in the 4 study cities at 2 time points (T1 and T2) from 2 cohorts of households, referred to as panel 1 (P1) and panel 2 (P2). P1, T1 interviews were conducted in 2009–2010. Households for this panel were selected using random-digit dialing of landline telephone numbers associated with the 4 cities. P1, T2 interviews were completed in 2014–2015. P2, T1 and P2, T2 interviews were conducted in 2014 and 2016–2017, respectively. P2 used a multiframe landline and cell phone sampling method within the geographical areas of the 4 cities to address the declining use of landline phones. Response rates for P1 T1 and P2 T1 surveys were 49% and 36%, respectively, which are similar to the response rates from the CDC New Jersey Behavioral Risk Factor Surveillance System31 for landline and cellphone samples. Details of the longitudinal sample are provided in Figure 1.
Figure 1.
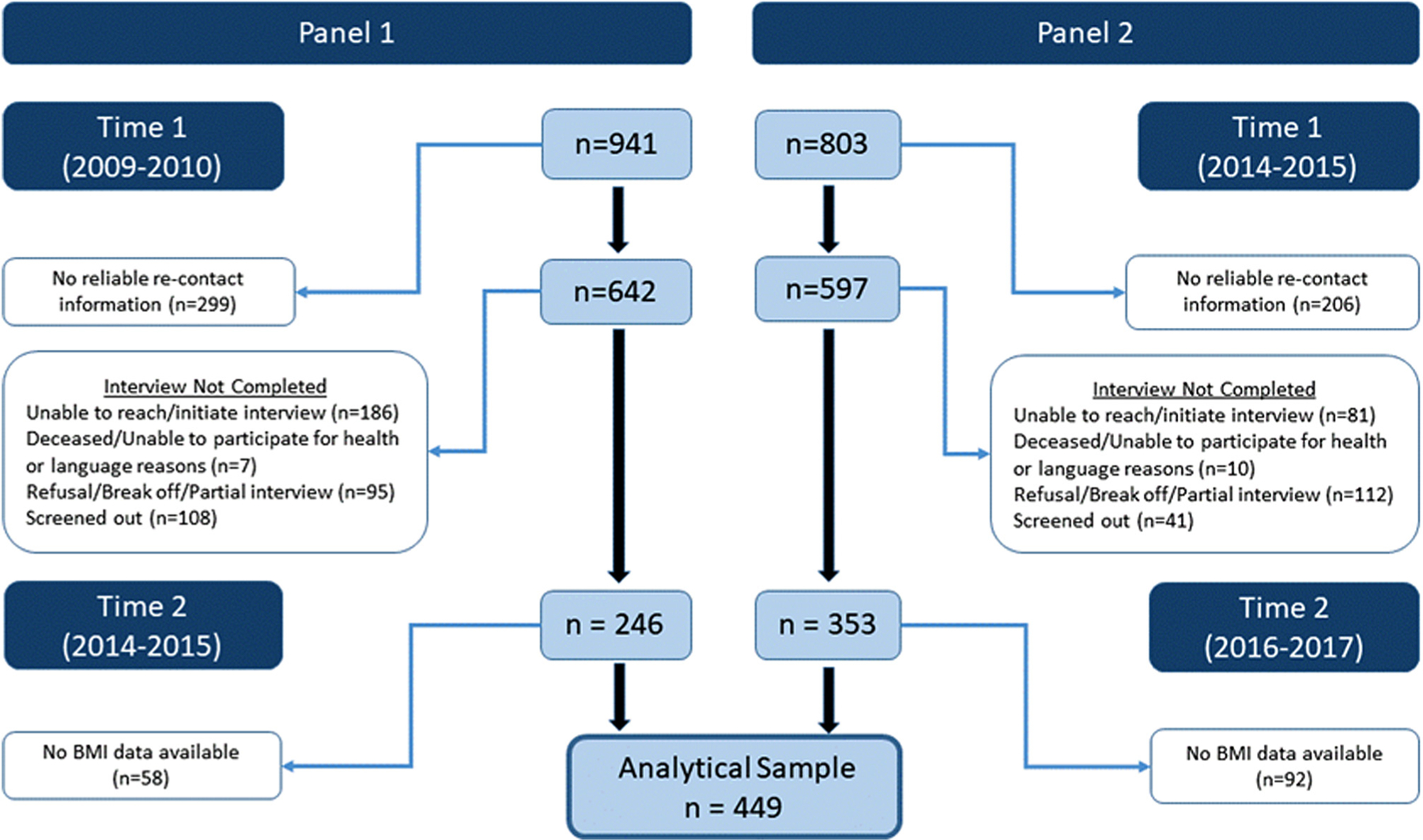
Description of the study timeline and the longitudinal analytic sample: New Jersey Child Health Study (2009–2017). BMI = body mass index.
For both panels, the respondent reporting on each child was an adult at least 18 years old, who was primarily responsible for food-purchasing decisions for the family; in more than 94% of the cases this was a parent or a grandparent and is referred to as “parent” hereafter. In both panels, a household was eligible for inclusion in the study if the household was located within the study city and had at least 1 child in the study age group (3 to 15 years old). Computer-aided telephone interviews32 were conducted in English or Spanish by trained interviewers. Respondents provided oral consent before the survey was administered. After obtaining information on all household members on their age, sex, and relationship to the respondent, data were collected on the respondent and on 1 child (referred to as the index child). In households with multiple age-eligible children, the index child was selected randomly using a computer program. On average, interviews took 30 to 36 minutes to complete; respondents were asked about relevant demographic characteristics at T1, and at both time points were asked about their and the index child’s height and weight, health status, food and physical activity behaviors, as well as household socioeconomic status and perceptions about their community environment. From the 2 panels combined, completed interviews at 2 time points were available for 599 households; height and weight data of the index child were available at both time points in 449 cases (Figure 1). Children lost to follow-up from T1 to T2 did not differ from the rest of the sample on any demographic characteristics.
A longitudinal home address database was created to track the different locations where each child lived during the study period. Participating households provided current home addresses (or nearest cross streets) during the T1 and T2 interviews. At T2, respondents were also asked whether the child had lived at any other address, along with duration of residence, in the years between T1 and T2. All addresses were geocoded. Based on survey dates and respondents’ reported duration of residency at a given address, the longitudinal address database assigned each household a location for every month elapsed between T1 and T2. More than 97% of the households had complete address information and 77% (n = 461) had the same address at baseline and follow-up. Exposure to aspects of the food environment around a child’s home were calculated for each month between T1 and T2 using this longitudinal home address database and the community food environment data described below.
Community Food Environment
Changes in the food environments around children’s homes included changes in the presence of various outlets resulting from opening and closing of stores, changes resulting from the household moving to a new location, and upgrades to existing food stores, fostered by initiatives implemented by community organizations in all 4 cities to improve offerings in convenience stores.33
Food Outlets.
To assess availability of different types of outlets around a child’s home, data on characteristics and addresses of food outlets were obtained in 2009, 2012, 2013, 2014, 2015, and 2017 from 2 commercial data companies, InfoUSA34 and Trade Dimensions/Nielsen,35 for each of the 4 cities, as well as a 1-mile radial buffer around the city boundaries. For each year, using an established protocol25 based on previous literature,36,37 stores were categorized as supermarkets, small grocery stores, convenience stores, pharmacies, full service restaurants, or limited service restaurants; information for making the classifications included North American Industry Classification System38 codes, sales volume, name recognition, as well as availability and quantity of specific foods stocked by the store. Stores with sales of more than $2 million and 4 or more checkouts were classified as supermarkets; superstores that did not require a membership fee were included in this category. Stores with less than $1 million in annual sales and those from larger chains, such as Wawa and 7-Eleven, were classified as corner or convenience stores (corner store and convenience store are used interchangeably in this article). Stores with sales volumes between $1 million and $2 million were called and asked whether they sold a specified selection of healthy items. Building on previous literature,39,40 stores with inventory meeting 3 of the following 4 criteria were classified as small grocery stores: 5 different types of fruits, 5 different types of vegetables, lower-fat milk, and fresh or frozen meat. Those not meeting the criteria were classified as convenience stores. Fruit and vegetable markets were also classified as small grocery stores. All study cities had ongoing initiatives to upgrade convenience stores to increase their offerings of healthy items; a list of stores participating in these efforts was provided to the study team. Each convenience store participating in such an initiative was audited using a validated observational checklist41 to assess the availability of healthy offerings. Upgraded stores were then removed from the convenience store list and classified into a separate category for upgraded convenience stores. Local and national pharmacy chains and stores identifying as pharmacies were categorized as such. Restaurants were classified as full or limited service based on name recognition, key words in the restaurant name, and whether patrons paid before (limited service) or after (full service) eating. All store locations were geocoded and, as a final step, data from multiple sources were deduplicated and checked for misclassifications. The location of each store at the time of data acquisition was assigned to all months of that calendar year.
Demographic and Contextual Factors
Children’s age, sex, race or ethnicity, and household income were collected from parents in the household survey. Based on race or ethnicity, children were classified as non-Hispanic White, non-Hispanic Black, Hispanic, and other. Household poverty level was calculated as the ratio of the household income to the federal poverty level for the year in which the survey was conducted. Total population and median household income for the census block in which each respondent lived was collected from the American Community Survey 5-year data files42 corresponding with the years of household surveys.
Variable Construction
Key Predictors: Change in Exposure to Food Outlets.
Using geocoded addresses of all respondent residences and annual lists of confirmed store locations, the road network distance from the respondent’s home to all food outlets within the city and the 1-mile buffer around the city was estimated using the OD (origin-destination) Cost Matrix analysis tool in the Network Analysis extension of the Geographical Information System ArcGIS, versions 10.1 to 10.6.43 As a base, the analyses used NJ Road Network data from the New Jersey Department of Transportation and New Jersey Office of GIS.44 Interstate highways and toll roads, where walking is strictly prohibited, were removed from the data set. For purposes of the analyses, the shortest walking path was calculated between each origin (child’s home) and destination (outlet), resulting in a comprehensive origin-destination matrix for each city for each year.
In the current literature, access to different types of food outlets has been characterized using various measures of proximity, including distance to nearest, presence of specific outlet types, and counts within a certain distance from the residence, with no consensus on a conceptually or empirically optimal measure.45,46 For the present analysis, the change in exposure to a specific type of outlet was measured as change in counts for that outlet type in various roadway network buffers (a network of connected roads within specified distances) around a child’s home. The counts of stores better captured variability in the exposure and provided a more comprehensive picture of the changes taking place over time than the other options.
Using the origin-destination matrix, the numbers (ie, counts) of each type of outlet within a 0.25−, 0.5−, and 1-mile buffer around a child’s home at T1 and T2, and for each month in between were calculated. Next, for each distance around a child’s home, the difference between the average of monthly counts during a period preceding the T2 interview (12 months, 18 months, and 24 months) and the count value at the time of the T1 interview was calculated. Using a monthly average of the period (12, 18, or 24 months) preceding T2 allowed for accounting for not only the changes that occurred between T1 and T2 in the exposure measure, but also the timing and duration of these changes. Additional details, including a graphical illustration of the method for computing exposure to changes in counts during different periods of time, is provided in Figure 2.
In the absence of an evidence-based criterion for an appropriate length of exposure or distance, and similar to other studies examining exposure over time,47 a number of distance and length of exposure combinations were examined, with the aim of identifying patterns of association over time. For each outlet type, change in food environment was calculated for 9 distance/length-of-exposure combinations (T2l – T1)d, where l refers to the length of time for which the exposure was averaged before T2 (12 months, 18 months, and 24 months) and d refers to the road network buffer distance around the child’s home (0.25 mile, 0.5 mile, and 1 mile).
Outcome Variable: Change in Body Mass Index z-Scores
The outcome variable was calculated as the change in children’s body mass index z scores (zBMI) between T1 and T2. Age- and sex-specific zBMI were calculated following the standard CDC methodology.48 A continuous variable, zBMI represents the child’s BMI transformed into a scale expressing the number of standard deviation units it is from the mean of the reference population of the same age and sex. Although BMI percentile–based weight status categories are the most common measures used for screening and surveillance purposes, use of zBMI has been considered more appropriate to evaluate changes in child weight status over time.49–51
Valid height and weight data at both time points were available for 449 children. Table 1 provides details on sources of height and weight data used in these analyses. In the majority of cases (n = 390 [86.9%]), parent estimates of children’s heights and weights were used to calculate age- and sex-specific zBMI, as these measurements were available for both T1 and T2. When parent-estimated values were missing, parent-measured or professionally measured values, obtained for a validation study on a subsample of children from the current study, were used. This decision was based on the results of the validation study showing that, compared with professional measurements, parent-estimated and parent-measured methods each yielded accurate estimates of children’s weight status.52 The outcome variable change in zBMI is the difference between zBMI at T2 and T1. Physiologically meaningful changes in zBMI were identified, acknowledging that a decrease of approximately 0.5 or 0.6 units in zBMI is considered an indication of reduction in adiposity51—the ultimate goal of obesity prevention efforts. Accordingly, a 3-level ordered categorical variable was created as follows: 1) negative change indicates children’s zBMI decreased more than 0.50 (zBMI change < −0.50); 2) no change indicates children’s zBMI did not change more than 0.50 in absolute value (−0.50 ≤ zBMI change ≤ +0.50); and 3) positive change indicates children’s zBMI increased more than 0.50 (zBMI change > +0.50).
Table 1.
Sources of weight and height measurements for children in the longitudinal analytical sample from the New Jersey Child Health Study (2009–2017)a
| Source of weight and height data | Parent-estimated (time 2) | Parent-measured (time 2) | Professionally measured (time 2) | Total (time 2) |
|---|---|---|---|---|
|
|
||||
| Parent-estimated (time 1) | 390 (86.9) | 8 (1.8) | 5 (1.1) | 403 (89.8) |
| Parent-measured (time 1) | 39 (8.7) | 2 (0.4) | 4 (0.9) | 45 (10.0) |
| Professionally measured (time 1) | 1 (0.2) | 0 (0.0) | 0 (0.0) | 1 (0.2) |
| Total (time 1) | 430 (95.8) | 10 (2.2) | 9 (2.0) | 449 (100.0) |
Parent-estimated values were obtained from parents during the household phone survey. Parent-measured and professionally measured values were obtained for a validation study on a subsample of children from the current study.52
Statistical Analysis
Because the study outcome is an ordered 3-category variable, a series of proportional-odds cumulative logit (ordinal logit)53 regression models were estimated separately for each of the distance/length-of-exposure variables described. In the ordered logit specification, the estimation returns a single set of coefficients that apply to each combination of contiguous outcome categories. An estimated coefficient indicates the effect that a 1-unit increase in a predictor is expected to have on the outcome, specifically on the log-odds of being below vs above any level of the categorical outcome, holding all of the other predictors constant. For ease of interpretation, the estimated coefficients are transformed into odds ratios (ORs). For example, an OR > 1 indicates that for every unit increase in exposure, the child had greater odds of being in the no change or positive change category compared with negative change category. Similarly, the same estimated OR > 1 would indicate that the child had greater odds of being in the positive change category compared with the no change or negative change category. A more formal description of ordinal logit regression models can be found elsewhere.54
Changes in counts for all food outlet types examined (key exposure variables) were entered into the models simultaneously. All models adjusted for child age at T1 (categorized as 3 to 11 years old and 12 to 15 years old to differentiate between young children and adolescents), sex, and race; whether the child was classified as obese at T1; change in household income level between T1 and T2; changes in total population and median income at the census block group level between T1 and T2; number of months between T1 and T2; and food environment (counts of different outlet types) at T1. All models included longitudinal survey weights to account for sample attrition and adjusted for the nested structure of the data at the city level using the svy command in Stata software, version 15.55 All statistical comparisons were considered significant at P < 0.05.
Sensitivity Analyses
To assess the robustness of our findings and test whether the results were consistent across several alternative analytic designs, a series of sensitivity analyses were conducted. Briefly, these analyses included models with different specifications of the outcome variable measuring the change in zBMI (in a continuous form, and using CDC’s modified zBMI that addresses concerns about compression of z scores at extreme values of BMI),56,57 as well as models with additional adjustments, including a measure of children’s physical activity and an indicator of height and weight data source (parent-reported vs measured). In addition, to determine whether the association between key exposures and weight outcomes differed by demographic characteristics, models with interaction terms between exposure to outlet and child and household level demographics were examined. Finally, all analyses were replicated using multiple imputation58 for missing predictor variables.
RESULTS
Descriptive Results
Descriptive statistics of the sample are presented in Table 2. At T1, the mean zBMI was 0.7 and one-fourth (25.2%) of the children were classified as obese. The mean change in zBMI between T1 and T2 was −0.2, with 41.2% of children experiencing no change (between −0.5 and +0.5), 33.6% experiencing a negative change (< −0.5), and 25.2% experiencing a positive change (> +0.5). The mean age at T1 was 10.2 years; male children comprised 53.2% of the sample. Almost half (48.3%) of the children were non-Hispanic Black, 34.3% were Hispanic, and the remaining 17.4% were non-Hispanic White or other. The mean income was 2.6 times the federal poverty level, and the mean interval between T1 and T2 interviews was 40.6 months (approximately 3 years and 3 months). Characteristics of the sample of children with height and weight data at both time points (n = 449) were generally similar to those of the overall longitudinal sample (n = 599). However, children with complete height and weight data at T1 and T2 were slightly older (mean age 10.2 vs 7.9 years), less likely to be non-Hispanic Black (48.3% vs 57.8%) and Hispanic (34.4% vs 39.5%), and more likely to be from less poor families (mean income 2.6 times the federal poverty level vs 1.5 times the federal poverty level) (Table 3; available at www.jandonline.org).
Table 2.
Descriptive characteristics for children in the longitudinal analytical sample. New Jersey Child Health Study (2009–2017)
| Variable | Data |
|---|---|
| Characteristics at time 1 | |
| Age, n (%) | |
| 3–11 y | 276 (61.5) |
| 12–15 y | 173 (38.5) |
| Sex, n (%) | |
| Male | 239 (53.2) |
| Female | 210 (46.7) |
| Race and ethnicity, n (%) | |
| Non-Hispanic Black | 217 (48.3) |
| Hispanic | 154 (34.3) |
| Non-Hispanic White/other | 78 (17.4) |
| Obesea n (%) | |
| No | 334 (74.4) |
| Yes | 115 (25.6) |
| zBMIb score, mean (SDc) | 0.7 (1.4) |
| Household poverty level,d mean (SD) | 2.6 (3.9) |
| Census block group population,e mean (SD) | 1,424 (635) |
| Census block group annual household income, $,e mean (SD) | 35,899 (19,782) |
| Months between time 1 and time 2, mean (SD) | 40.6 (18.1) |
| zBMI change (time 2 – time 1), mean (SD) | −0.2 (1.5) |
| zBMI change category, n (%) | |
| Negative change (< −10.5) | 151 (33.6) |
| No change ( ≥0.5 and ≤ +0.5) | 185 (41.2) |
| Positive change (> +0.5) | 113 (25.2) |
| N | 449 |
Obesity is defined using the Center for Disease Control and Prevention’s definition1 as a BMI ≥ 95th percentile for children of the same age and sex.
zBMI = body mass index z score.
SD = standard deviation.
Poverty level was calculated as the ratio of annual household income and federal poverty level for the year in which the survey was conducted.
Census Block Group data were obtained from the American Community Survey 5-year data files,42 corresponding with the years of the survey.
As expected, the number of food outlets around each child’s home increased when larger network buffers were considered (Table 4; available at www.jandonline.org). For example, at T1, within a road network buffer of 0.25 mile around a child’s residence, there were on average 0.1 supermarkets, 0.2 small healthy outlets, 0.5 pharmacies, 1.7 convenience stores, and 1.8 limited service restaurants; the mean count of each type of outlet was higher when the applied network buffer was 0.5 or 1 mile. The key predictor variables captured the changes in the count (T2l – T1)d of specific food outlets within different road network distance buffers around a child’s home (d = 0.25; 0.5; or 1 mile) over varying lengths of exposure before T2 (l = 12; 18; or 24 months) (Figure 2; available at www.jandonline.org). Similar to the counts at baseline, there was variation in distribution of change in counts depending on the size of the road network buffer around the child’s home. As illustrated in Figure 3A through 3F, for most types of food outlets, when considering (T2l = 18 – T1)d = 0.25 (18-month length of exposure before T2 at the 0.25 mile buffer), there was very limited change, except for convenience stores and limited service restaurants, which were the most prevalent types of outlets. A larger change in the count of outlets was observed, along with greater variability, for larger (0.5-mile and 1-mile) network buffers around the child’s home. However, notable differences exist across outlet types. Specifically, the more prevalent the outlets, the more variable their distribution of change. A complete descriptive comparison of patterns of change in counts across all geographies and all lengths of exposures examined is presented in Figure 5A–5E (available at www.jandonline.org).
Figure 3.
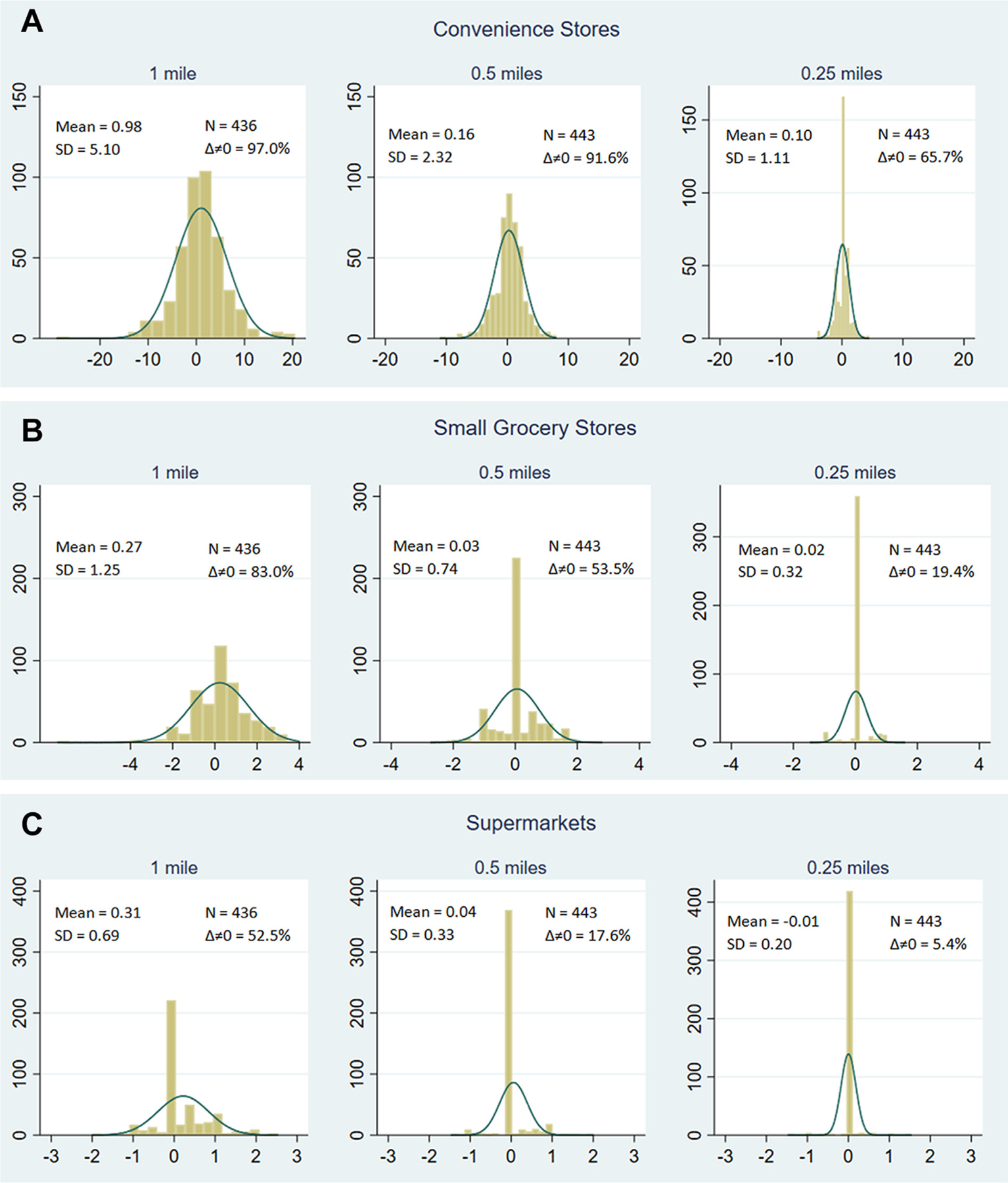

Distribution of change in number of counts for specific outlets for (T2l = 18 – T1)d = 0.25; 0.5; 1a in the longitudinal sample of children in the New Jersey Child Health Study (2009–2017). Summary statistics include mean, standard deviation (SD), sample size (N), and proportion of sample with non-zero change in count values between T1 and and T2l = 18 (∆ ≠ 0). T1 = time 1 survey; T2 = time 2 survey. a Change in exposures over time was calculated using the difference between the average of counts during an 18-month period preceding the T2 interview and the count value at the time of the T1 interview for 3 roadway network buffers (0.25 miles, 0.5 miles, 1 mile) around a child’s home.
Multivariable Model Results
To present the patterns of associations between changes in food environment and zBMI change categories, the results are shown by outlet type in Figures 4A through 4F. Across most models, exposure to increases in convenience stores over time increased the odds of being in a higher zBMI change category, meaning that children were more likely to have experienced an increase in zBMI over time (Figure 4A). For instance, for distance/length of exposure represented by (T2l = 24 – T1)d = 1.0, a 1-unit increase in the exposure variable (change in convenience store counts), resulted in 11.7% higher odds of a child being in a higher zBMI change category (P =0.007). This relationship was statistically significant (P < 0.05) at the 1-mile radius (where CIs are smaller due to a higher prevalence of change) for all lengths of exposure, and the pattern was consistent across models representing other distance/length of exposure combinations. The opposite pattern was observed for small grocery stores. For example, for (T2l = 18 – T1)d = 1.0, a 1-unit increase in the exposure variable (change in small grocery store counts) resulted in 37.3% lower odds of being in a higher zBMI change category (P < 0.05). This relationship was consistent across all models, but estimates based on smaller buffers had larger CIs (Figure 4B). The results for supermarkets did not show a consistent pattern (Figure 4C). However, caution is warranted in interpreting these results because for most children there were no changes in the number of supermarkets around their home over time, especially within a 0.25-mile radius (Figure 5C; available at www.jandonline.org). Upgraded convenience stores and pharmacies (Figure 4D and 4E) did not show a clear pattern, with estimates having large CIs resulting from a smaller number of changes observed for these features of the food environment. Changes in exposure to limited service restaurants (Figure 4F) were also not associated with zBMI change categories.
Figure 4.
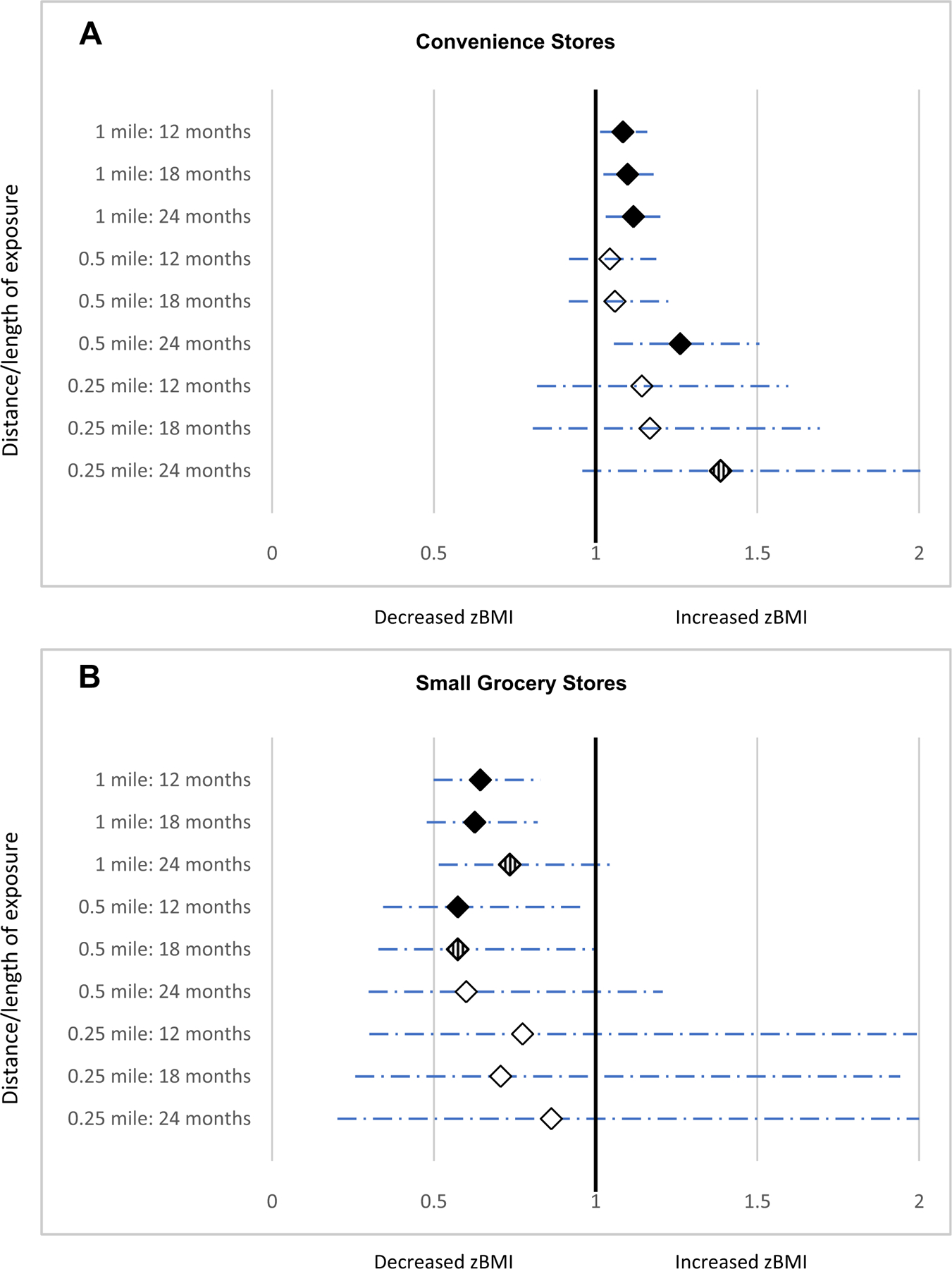

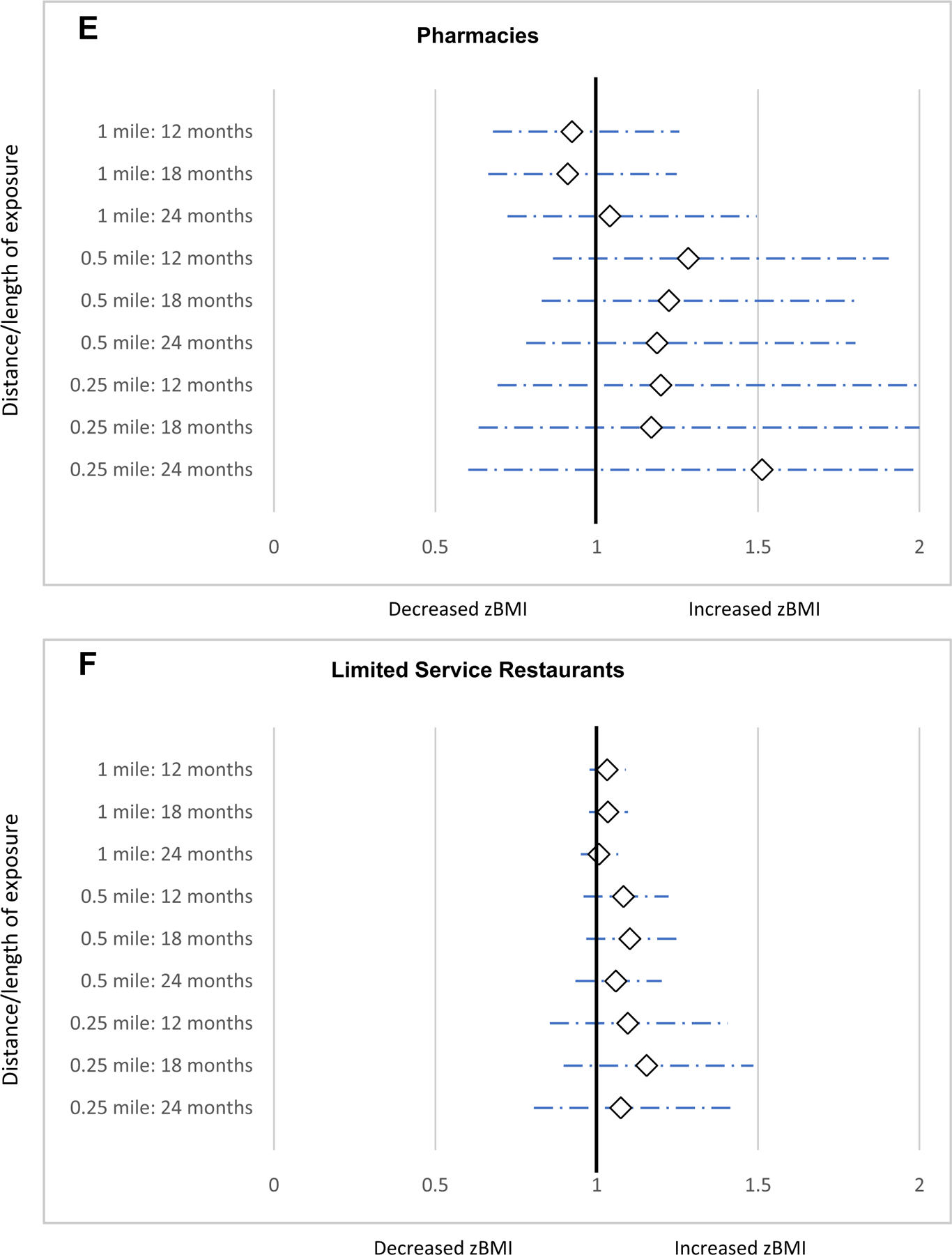
Odds ratios (ORs) and 95% CIs from ordinal logit regression models examining the impact of change in count of specific outlets in 9 distancea/length of exposureb combinations on body mass index z score (zBMI) change.c T1 = time 1 survey; T2 = time 2 survey.
 P < 0.05 for OR different from 1.
P < 0.05 for OR different from 1.  P < 0.10 for odds ratio different from 1.
P < 0.10 for odds ratio different from 1.  P > 0.10 for odds ratio different from 1. aChange in counts of outlets within 3 different roadway network distances: 0.25 mile, 0.5 mile, and 1 mile.bChange in counts over varying lengths of exposure was calculated as the difference between the average of monthly counts during a period preceding the T2 interview (12 months, 18 months, and 24 months) and the count value at the time of the T1 interview. cSeparate models were run for each proximity/length of time combination. All models adjusted for child age, sex, and race; whether the child was classified as obese at T1; number of months between T1 and T2; as well as for food environment (counts of different outlet types) at T1; and difference between T2 – T1 for the following variables: household income level as ratio of federal poverty level, total population and median income at the census block group level. Sample size for models: 1 mile, 12 months: n = 424; 1 mile, 18 months: n = 427; 1 mile, 24 months: n = 329; 0.5 miles, 12 months: n = 431; 0.5 miles, 18 months: n = 434; 0.5 miles, 24 months: n = 335; 0.25 miles, 12 months: n = 431; 0.25 miles, 18 months: n = 434; 0.25 miles, 24 months: n = 335.
P > 0.10 for odds ratio different from 1. aChange in counts of outlets within 3 different roadway network distances: 0.25 mile, 0.5 mile, and 1 mile.bChange in counts over varying lengths of exposure was calculated as the difference between the average of monthly counts during a period preceding the T2 interview (12 months, 18 months, and 24 months) and the count value at the time of the T1 interview. cSeparate models were run for each proximity/length of time combination. All models adjusted for child age, sex, and race; whether the child was classified as obese at T1; number of months between T1 and T2; as well as for food environment (counts of different outlet types) at T1; and difference between T2 – T1 for the following variables: household income level as ratio of federal poverty level, total population and median income at the census block group level. Sample size for models: 1 mile, 12 months: n = 424; 1 mile, 18 months: n = 427; 1 mile, 24 months: n = 329; 0.5 miles, 12 months: n = 431; 0.5 miles, 18 months: n = 434; 0.5 miles, 24 months: n = 335; 0.25 miles, 12 months: n = 431; 0.25 miles, 18 months: n = 434; 0.25 miles, 24 months: n = 335.
Sensitivity analyses using linear models with continuous dependent variables (change in zBMI) are reported in Figures 6A through 6E (available at www.jandonline.org), showing generally consistent findings. Additional sensitivity analysis using modified zBMI and imputed values for missing predictor variables produced similar findings. Likewise, models including interaction terms for main exposure variables and child characteristics (ie, age, sex, race, and baseline obesity status) or baseline number of stores did not indicate that patterns of associations between exposures and outcomes differed across subgroups. Lastly, models controlling for the source of data for children’s height and weight (parent-reported vs measured), models including the change in physical activity behaviors, and models based on multiple imputations also produced results similar to main analysis. Results from sensitivity analyses that are not included in Figure 6 (available at www.jandonline.org) are available from authors on request.
DISCUSSION
Using a longitudinal cohort study design, within the National Institutes of Health natural experiment framework,26 relationships between changes in exposure to key features of the food environment, including supermarkets, small grocery stores, convenience stores, pharmacies, and limited service restaurants, and changes in children’s zBMI over time were examined. To enhance the robustness of findings, drawing on the comprehensive nature of the data collected for the study and acknowledging the lack of consensus in the field, patterns of associations across a meaningful range of proximities and lengths of exposure were examined, rather than reporting selected, isolated statistically significant findings.
Less-healthy changes in weight outcomes were observed among children (ie, they were more likely to be in a higher zBMI change category) when their exposure to convenience stores increased over time. This pattern was consistent across all distances and exposures examined, although not all results were statistically significant. These findings are consistent with previous cross-sectional research showing that children living in close proximity to convenience stores have higher odds of being classified as overweight or obese.14,59 Similarly, Leung and colleagues40 found that higher exposure to convenience stores within a 0.25-mile network buffer of girls’ homes was associated with a higher zBMI 3 years later. Although most households do the bulk of their shopping at supermarkets,60 smaller stores, such as convenience stores, which sell mostly highly processed, energy-dense foods,59 are often frequented for snack items and beverages. Confirming the linkage between unhealthy outcomes and proximity to convenience stores, the present study adds substantially to the literature by incorporating an unprecedented degree of control; the same children were followed over time, eliminating potential confounding effects of child-level characteristics, and the methodology measured and accounted for the influence of numerous simultaneous changes at the individual, family, and environment levels in statistical models.
Another notable feature of the current study is that food store data from commercial sources were reclassified using an established protocol in real time during the study period, with information obtained by calling and visiting stores. These steps allowed identification of small grocery stores that often sell a variety of healthy items but are not large enough to be classified as supermarkets. Children exposed to additional small grocery stores near their homes over time were less likely to experience an increase in zBMI. This finding was consistent across all distances and lengths of exposures examined. Chen and Wang,21 using Early Childhood Longitudinal Study-Kindergarten data, similarly found that a newly opened small grocery store was associated with lower BMI in 5th grade girls 3 years after the outlet opened. As with convenience stores, the occurrence of any change in exposure to small grocery stores was less common when examining smaller network distances (ie, 0.25 mile) around children’s homes, resulting in larger CIs and nonsignificant findings.
Over time, small but statistically significant improvement in weight status among children with greater exposure to small grocery stores was observed. These findings have important implications for future initiatives that aim to improve the community food environment. This is especially important given the null findings in these analyses in regard to the relationship between exposure to upgraded convenience stores and weight outcomes. Upgraded convenience stores (those participating in healthy food initiatives), compared with non-upgraded convenience stores, stock greater quantities of healthy items61; however, the level of improvement might not be sufficiently high to bring about a change in weight outcomes. To date, studies have not examined the relationship between specific levels of upgrades and meaningful changes in weight status. Findings from this study suggest that upgraded corner stores might need to carry a healthier inventory at levels similar to that of the small grocery stores observed in this study to have a beneficial impact on children’s weight status. Additional interventions and evaluations of healthy upgrade initiatives should build on the current findings, focusing on the level of change in inventory promoted and achieved.
No consistent pattern in the impact of changes in availability of supermarkets near children’s homes was observed. The vast majority of the sample in these densely populated cities had access to supermarkets. Supermarkets offer a wide variety of healthy and unhealthy options at competitive prices62 and most people, irrespective of proximity, do most of their shopping at these stores60; consequently, it follows that changes in proximity to supermarkets over time might not impact children’s weight status.
No statistically significant relationships were observed between changes in children’s weight status and changes in access to limited service restaurants or pharmacies. Infrequent changes in counts of pharmacies preclude making meaningful conclusions. Other studies have found significant associations between proximity to limited service restaurants and weight outcomes, but most have been cross-sectional in design.63 Such studies have found that, compared with children who do not eat at fast-food restaurants, children who do consume more calories and fewer nutrient-dense foods64,65 and have worse weight outcomes.66 The lack of significant associations here suggests that families patronizing limited service restaurants might not be influenced by their proximity and that other interventions might be needed to reduce consumption of energy-dense foods at these locations.
The granular data in this study captured exposure to different types of stores using multiple metrics—physical proximity, length of exposure, and in-store availability of healthy items— and allowed for an examination of patterns in relationships between changes in the food environment and changes in children’s weight status across a range of exposure levels rather than adopting a fixed measure of proximity or length of exposure. The current status of knowledge in the field does not justify testing whether or not a particular distance/duration combination is more predictive of BMI changes. Consequently, patterns of associations across several meaningful distances and lengths of exposure were examined in these analyses. Existing research often takes advantage of specific known changes in an identified neighborhood having particular demographic and geographic characteristics; this approach limits generalizability of findings and does not account for several other factors that are likely to affect outcomes. In contrast, the present research design allowed for consideration of a child’s experience growing up in a community where the food environment is dynamic and multiple changes occur simultaneously. In addition, a number of sensitivity analyses were conducted incorporating alternative specifications of the outcome variable, additional controls, and imputation of missing data. Across all model specifications, the patterns of association were consistent, increasing confidence in the robustness of the study findings. Subgroup analyses by age, sex, and race of the child, and household-level socioeconomic factors also revealed consistent findings.
The study is subject to some limitations. Although a wide-ranging set of food outlet types was examined, other outlet types, such as dollar stores, farmers’ markets, and mobile markets, were not captured in the data. Similarly, other factors affecting food choices, including availability of culturally appropriate foods, price, individual preferences, and school food environment, are important to the overall health and well being of children, but were beyond the scope of the current study. Although these analyses were confined to examining the community food environment within a mile of a child’s home, evidence from national studies suggests that shoppers travel longer distances (up to 3.8 miles) to their preferred store.60 Low-income shoppers in particular have been found to shop outside their neighborhoods to access discount and chain supermarkets.67,68 However, more than 60% of families in this study did most of their food shopping in their neighborhood, defined as a 20-minute walk, 5-minute drive, or 1 mile in any direction from home; 80% lived within 1 mile of a supermarket, more than 90% lived within 1 mile of a small grocery store, and almost all had a convenience store and fast-food restaurant within 1 mile of their home.14 Consistent with prior research,69 a 1-mile radius around a participant’s home was considered an appropriate upper limit for examination. Finally, our study is based on a broad conception of a natural experiment26 rather than a stricter econometric definition, which refers to a quasirandom activity that is clearly not generated in relation to the outcome of interest. It is possible that the observed estimated effects could have been confounded by unmeasured factors relating to decisions made by businesses to locate outlets in particular communities.
CONCLUSIONS
The primary focus of this study was to assess how changes in the food environment in close proximity to children’s homes affect changes in children’s BMI. Children with increased exposure to convenience stores were more likely to experience an increase in zBMI. In contrast, those with greater exposure to small grocery stores selling a selection of healthy items were less likely to experience an increase in zBMI. No consistent patterns were observed for other types of outlets. Importantly, convenience store upgrades were not associated with any changes in child weight status. This suggests that elevating the healthfulness of food offered at upgraded stores to levels similar to those of small grocery stores has the potential to improve children’s weight status.
Supplementary Material
RESEARCH SNAPSHOT.
Research Question:
What is the impact of change in availability of key features of the community food environment on changes in children’s (3 to 15 years old) body mass index z scores?
Key Findings:
In this longitudinal cohort study, changes in key aspects of the community food environment, specifically availability of small stores in the neighborhood surrounding children’s homes, had a significant impact on changes in children’s weight; body mass index z score increases were observed over time when children had greater exposure to convenience stores and body mass index z score decreases were observed with higher exposure to small grocery stores.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Michelle Kennedy, MPH for leading and managing data collection teams at Rutgers University and Sarah Martinelli, MS, RDN, Cori Lorts, PhD, RDN, and Jessie Gruner, PhD, RDN for managing data collection as part of the Arizona State University team. We are grateful to our undergraduate and graduate students at Rutgers University and Arizona State University for helping us throughout the research process. We have received permission from everyone named in the Acknowledgements section.
FUNDING/SUPPORT
This research was supported by grants from the Robert Wood Johnson Foundation, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (1R01HD071583-01A1), and the National Heart, Lung, and Blood Institute, National Institutes of Health (1R01HL137814-01).
Footnotes
STATEMENT OF POTENTIAL CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
Supplementary materials:
Tables 3 and 4 and Figures 2, 5, and 6 are available at www.jandonline.org
Contributor Information
Punam Ohri-Vachaspati, College of Health Solutions, Arizona State University, Phoenix..
Francesco Acciai, College of Health Solutions, Arizona State University, Phoenix..
Kristen Lloyd, Center for State Health Policy, Institute for Health, Health Care Policy and Aging Research, Rutgers University, New Brunswick, NJ..
David Tulloch, Department of Landscape Architecture, Rutgers University, New Brunswick, NJ..
Robin S. DeWeese, College of Health Solutions, Arizona State University, Phoenix..
Derek DeLia, MedStar Health Research Institute, Hyattsville, MD, and a professor, Department of Plastic and Reconstructive Surgery, Georgetown University School of Medicine, Washington, DC..
Michael Todd, Edson College of Nursing and Health Innovation, Arizona State University, Phoenix..
Michael J. Yedidia, Center for State Health Policy, Institute for Health, Health Care Policy and Aging Research, Rutgers University, New Brunswick, NJ..
References
- 1.Defining childhood obesity. Overweight & obesity Centers for Disease Control and Prevention. Published July 3, 2018. Accessed September 18, 2020, www.cdc.gov/obesity/childhood/defining.html. [Google Scholar]
- 2.Koplan JP, Liverman CT, Kraak VI. Preventing Childhood Obesity: Health in the Balance 1st ed. Washington, DC: The National Academies Press; 2005. [PubMed] [Google Scholar]
- 3.The Social-Ecological Model: A framework for prevention. Violence Prevention. Centers for Disease Control and Prevention. Published January 28, 2020. Accessed July 21, 2020, www.cdc.gov/violenceprevention/publichealthissue/social-ecologicalmodel.html. [Google Scholar]
- 4.Ohri-Vachaspati P, Leviton L, Bors P, Brennal L, Brownson RC, Strunk S. Strategies proposed by Healthy Kids, Healthy Communities partnerships to prevent childhood obesity. Prev Chronic Dis 2012;9:E11. [PMC free article] [PubMed] [Google Scholar]
- 5.Keener D, Goodman K, Lowry A, Zaro S, Kettel Khan L. Recommended community strategies and measurements to prevent obesity in the United States: Implementation and measurement guide US Department of Health and Human Services, Centers for Disease Control and Prevention. Published 2009. Accessed February 10, 2020, www.cdc.gov/obesity/downloads/community_strategies_guide.pdf. [Google Scholar]
- 6.Dubowitz T, Orleans T, Nelson C, May LW, Sloan JC, Chandra A. Creating healthier, more equitable communities by improving governance and policy. Health Aff (Millwood) 2016;35(11):1970–1975. [DOI] [PubMed] [Google Scholar]
- 7.Block JP, Subramanian SV. Moving beyond “food deserts”: Reorienting United States policies to reduce disparities in diet quality. PLoS Med 2015;12(12). 2015;e1001914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson CAM. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results: The Local Food Environment and Obesity. Obesity 2015;23(7):1331–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou Q, Zhao L, Zhang L, et al. Neighborhood supermarket access and childhood obesity: A systematic review. Obes Rev Published online September 3, 2019. 10.1111/obr.12937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ogden CL, Carroll MD, Fakhouri TH, et al. Prevalence of obesity among youths by household income and education level of head of household—United States 2011e2014. MMWR Morb Mortal Wkly Rep 2018;67(6):186–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanchez-Vaznaugh EV, Weverka A, Matsuzaki M, Sánchez BN. Changes in fast food outlet availability near schools: Unequal patterns by income, race/ethnicity, and urbanicity. Am J Prev Med 2019;57(3):338–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kolak M, Bradley M, Block DR, et al. Urban foodscape trends: Disparities in healthy food access in Chicago, 2007e2014. Health Place 2018;52:231–239. [DOI] [PubMed] [Google Scholar]
- 13.Larsen K, Cook B, Stone MR, Faulkner GEJ. Food access and children’s BMI in Toronto, Ontario: Assessing how the food environment relates to overweight and obesity. Int J Public Health 2015;60(1):69–77. [DOI] [PubMed] [Google Scholar]
- 14.Ohri-Vachaspati P, Lloyd K, DeLia D, Tulloch D, Yedidia MJ. A closer examination of the relationship between children’s weight status and the food and physical activity environment. Prev Med 2013;57(3):162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev 2007;29(1):129–143. [DOI] [PubMed] [Google Scholar]
- 16.Sallis JF, Glanz K. Physical activity and food environments: Solutions to the obesity epidemic. Milbank Q 2009;87(1):123–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dubowitz T, Ghosh-Dastidar M, Cohen D, et al. A New Supermarket in a Food Desert: Is Better Health in Store? Santa Monica, CA: RAND Corporation; 2015. [Google Scholar]
- 18.Elbel B, Moran A, Dixon LB, et al. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children’s dietary intakes. Public Health Nutr 2015;18(15):2881–2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff (Millwood) 2014;33(2):283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaparro MP, Whaley SE, Crespi CM, et al. Influences of the neighbourhood food environment on adiposity of low-income preschool-aged children in Los Angeles County: A longitudinal study. J Epidemiol Community Health 2014;68(11):1027–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen H-J, Wang Y. Changes in the neighborhood food store environment and children’s body mass index at peripuberty in the United States. J Adolesc Health 2016;58(1):111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang Y, Jia P, Cheng X, Xue H. Improvement in food environments may help prevent childhood obesity: Evidence from a 9-year cohort study. Pediatr Obes 2019;14(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zeng D, Thomsen MR, Nayga RM, Bennett JL. Supermarket access and childhood bodyweight: Evidence from store openings and closings. Econ Hum Biol 2019;33:78–88. [DOI] [PubMed] [Google Scholar]
- 24.Han E, Powell LM, Zenk SN, Rimkus L, Ohri-Vachaspati P, Chaloupka F. Classification bias in commercial business lists for retail food stores in the US. Int J Behav Nutr Phys Act 2012;9(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ohri-Vachaspati P, Martinez D, Yedidia MJ, Petlick N. Improving data accuracy of commercial food outlet databases. Am J Health Promot 2011;26(2):116–122. [DOI] [PubMed] [Google Scholar]
- 26.Emmons K, Doubeni C, Fernandez M, Miglioretti D, Samet J. National Institutes of Health (NIH) pathways to prevention workshop: Methods for evaluating natural experiments in obesity Published December 5, 2017. Accessed August 10, 2020, prevention.nih.gov/sites/default/files/2018-06/P2P_Obesity_Panel_Report_Final.pdf. [DOI] [PubMed]
- 27.Craig P, Cooper C, Gunnell D, et al. Using natural experiments to evaluate population health interventions: Guidance for producers and users of evidence Medical Research Council. Published 2010. Accessed September 18, 2020, mrc.ukri.org/documents/pdf/natural-experiments-guidance/%20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nutrition and fitness. NJ Health State of New Jersey Department of Health. Published November 29, 2017. Accessed August 10, 2020, nj.gov/health/nutrition/. [Google Scholar]
- 29.Shaping NJ. New Jersey State Obesity Prevention Plan. The Office of Nutrition and Fitness Published 2013. Accessed August 10, 2020, www.state.nj.us/health/nutrition/documents/obesity_prevention_plan.pdf.
- 30.Our Partners. NJ Partnership for Healthy Kids Robert Wood Johnson Foundation. Accessed August 10, 2020, www.njhealthykids.org/about-us/our-partners/. [Google Scholar]
- 31.Qayad MG, Pierannunzi C, Chowdhury PP, Hu S, Town GM, Balluz LS. Landline and cell phone response measures in Behavioral Risk Factor Surveillance System. Surv Pract 2013;6(3):1–11. [Google Scholar]
- 32.Lavraka P Computer-assisted telephone interviewing (CATI). Sage Research Methods Published 2008. Accessed August 10, 2020, methods.sagepub.com/reference/encyclopedia-of-survey-research-methods/n83.xml.
- 33.Ramos A, Weiss S, Manon M, Harries C. Supporting Healthy Corner Store Development in New Jersey Philadelphia, PA: The Food Trust. Published 2015. Accessed November 20, 2019. thefoodtrust.org/uploads/media_items/supporting-healthy-corner-store-development-in-new-jersey-1.original.pdf%20 [Google Scholar]
- 34.InfoUSA. Business lists Published 2020. Accessed July 21, 2020, www.infousa.com/business-lists/.
- 35.Consumer & business data. Claritas Published 2020. Accessed July 21, 2020, www.claritas.com/data.html.
- 36.Designed for disease: The link between local food environments and obesity and diabetes California Center for Public Health Advocacy, PolicyLink, and the UCLA Center for Health Policy Research. Published 2008. Accessed June 25, 2019, escholarship.org/uc/item/9zc7p54b%20. [Google Scholar]
- 37.Supermarket facts Food Marketing Institute. Published 2019. Accessed August 10, 2020, www.fmi.org/research-resources/supermarket-facts. [Google Scholar]
- 38.Introduction to NAICS. North American Industry Classification System US Census Bureau. Published February 26, 2020. Accessed July 21, 2020, www.census.gov/eos/www/naics/. [Google Scholar]
- 39.Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med 2002;22(1):23–29. [DOI] [PubMed] [Google Scholar]
- 40.Leung CW, Laraia BA, Kelly M, et al. The influence of neighborhood food stores on change in young girls’ body mass index. Am J Prev Med 2011;41(1):43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.DeWeese RS, Todd M, Karpyn A, et al. Short-form audit instrument for assessing corner store healthfulness. Am J Health Promot 2018;32(1):224–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Summary file data American Community Survey (ACS). US Census Bureau. Published 2018. Accessed July 21, 2020, www.census.gov/programs-surveys/acs/data/summary-file.2013.html. [Google Scholar]
- 43.OD cost matrix analysis ArcMap. Published 2019. Accessed November 22, 2019, desktop.arcgis.com/en/arcmap/latest/extensions/network-analyst/od-cost-matrix.htm%20.
- 44.GIS data Department of Transportation, State of New Jersey. Accessed August 10, 2020, www.state.nj.us/transportation/refdata/gis/data.shtm. [Google Scholar]
- 45.Mavoa S, Bagheri N, Koohsari MJ, et al. How do neighbourhood definitions influence the associations between built environment and physical activity? Int J Environ Res Public Health 2019;16(9):1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wilkins E, Morris M, Radley D, Griffiths C. Methods of measuring associations between the retail food environment and weight status: Importance of classifications and metrics. SSM Popul Health 2019;8: 100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frongillo EA, Fawcett SB, Ritchie LD, et al. Community policies and programs to prevent obesity and child adiposity. Am J Prev Med 2017;53(5):576–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.A SAS program for the 2000 CDC growth charts (ages 0 to <20 years) Growth Chart Training. Centers for Disease Control, Division of Nutrition, Physical Activity, and Obesity. Published February 26, 2019. Accessed March 30, 2019, www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. [Google Scholar]
- 49.Bell LM, Byrne S, Thompson A, et al. Increasing body mass index z-score is continuously associated with complications of overweight in children, even in the healthy weight range. J Clin Endocrinol Metab 2007;92(2):517–522. [DOI] [PubMed] [Google Scholar]
- 50.Himes JH. Challenges of accurately measuring and using BMI and other indicators of obesity in children. Pediatrics 2009;124(suppl 1): S3–S22. [DOI] [PubMed] [Google Scholar]
- 51.Hunt LP, Ford A, Sabin MA, Crowne EC, Shield JPH. Clinical measures of adiposity and percentage fat loss: Which measure most accurately reflects fat loss and what should we aim for? Arch Dis Child 2007;92(5):399–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ohri-Vachaspati P, Acciai F, DeLia D, Lloyd K, Yedidia MJ. Accuracy of parent-measured and parent-estimated heights and weights in determining child weight status. JAMA Pediatr 2019;173(8):793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Agresti A Analysis of Ordinal Categorical Data 2nd ed. Hoboken, NJ: John Wiley & Sons; 2010. [Google Scholar]
- 54.Agresti A An Introduction to Categorical Data Analysis 3rd ed. Hoboken, NJ: John Wiley & Sons; 2019. [Google Scholar]
- 55.Stata Statistical Software [computer program]. Release 15 College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 56.Freedman DS, Butte NF, Taveras EM, et al. BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999–2000 to 2013–2014. Obesity 2017;25(4):739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Freedman DS, Berenson GS. Tracking of BMI z scores for severe obesity. Pediatrics 2017;140(3). 2017;e20171072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.von Hippel PT. 4. Regression with missing Ys: An Improved strategy for analyzing multiply imputed data. Sociol Methodol 2007;37(1):83–117. [Google Scholar]
- 59.Laska MN, Hearst MO, Forsyth A, Pasch KE, Lytle L. Neighbourhood food environments: Are they associated with adolescent dietary intake, food purchases and weight status? Public Health Nutr 2010;13(11):1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ver Ploeg M, Mancino L, Todd JE, Clay DM, Scharadin B. Where do Americans usually shop for food and how do they travel to get there? Initial findings from the National Household Food Acquisition and Purchase Survey US Department of Agriculture, Economic Research Service. Published 2015. Accessed January 4, 2019, www.ers.usda.gov/publications/eib-economic-information-bulletin/eib138. [Google Scholar]
- 61.DeWeese RS, Todd M, Karpyn A, et al. Healthy store programs and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), but not the Supplemental Nutrition Assistance Program (SNAP), are associated with corner store healthfulness. Prev Med Rep 2016;4:256–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Krukowski RA, West DS, Harvey-Berino J, Elaine Prewitt T. Neighborhood impact on healthy food availability and pricing in food stores. J Community Health 2010;35(3):315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: The role of built, socioeconomic, and social environments. Soc Sci Med 2013;95:106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Powell LM, Nguyen BT. Fast-food and full-service restaurant consumption among children and adolescents: Effect on energy, beverage, and nutrient intake. JAMA Pediatr 2013;167(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sebastian RS, Wilkinson Enns C, Goldman JD. US adolescents and MyPyramid: Associations between fast-food consumption and lower likelihood of meeting recommendations. J Am Diet Assoc 2009;109(2):226–235. [DOI] [PubMed] [Google Scholar]
- 66.Braithwaite I, Stewart AW, Hancox RJ, et al. Fast-food consumption and body mass index in children and adolescents: An international cross-sectional study. BMJ Open 2014;4(12). 2014;e005813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.LeDoux TF, Vojnovic I. Going outside the neighborhood: The shopping patterns and adaptations of disadvantaged consumers living in the lower eastside neighborhoods of Detroit, Michigan. Health Place 2013;19:1–14. [DOI] [PubMed] [Google Scholar]
- 68.Aggarwal A, Cook AJ, Jiao J, et al. Access to supermarkets and fruit and vegetable consumption. Am J Public Health 2014;104(5):917–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dutko P, Ver Ploeg M, Farrigan T. Characteristics and influential Factors of Food Deserts, ERR 140 US Department of Agriculture, Economic Research Service; August 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


