Abstract
Importance: Virtual reality in head-mounted displays (HMD-VR) may be a valuable tool in occupational therapy to address anxiety. Findings from the virtual reality exposure therapy (VRET) literature may facilitate translation of HMD-VR to occupational therapy psychosocial practice.
Objective: To explore how HMD-VR has been used to treat anxiety through VRET and could be translated to occupational therapy.
Data Sources: We searched seven electronic databases for articles published between 2000 and 2020: CINAHL, Cochrane Library, Embase, ERIC, Ovid MEDLINE, PsycINFO, and Web of Science. Search terms included HMD-VR constructs, products, and therapy concepts.
Study Selection and Data Collection: We used Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines to report studies implementing VRET to treat anxiety. At least two reviewers assessed each citation, and a third resolved disagreements. Articles were included if they were in English, reported experimental data, and used HMD-VR. Letters, commentaries, book chapters, technical descriptions, theoretical papers, conference proceedings (≤4 pages), and reviews were excluded.
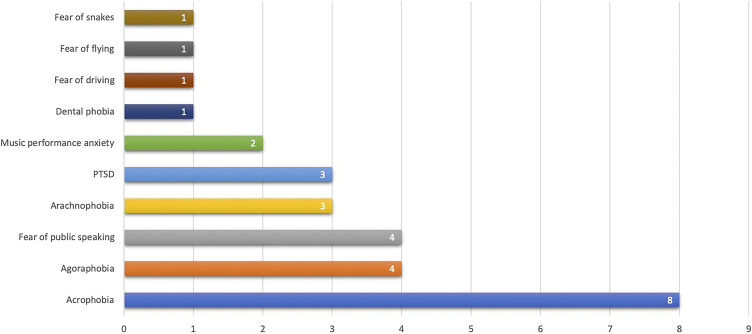
Findings: Twenty-eight studies used HMD-VR to treat posttraumatic stress disorder (n = 3), specific phobias (n = 19), and performance-based social anxiety (n = 6); protocols and levels of evidence varied (randomized controlled trials, n = 11; controlled trials without randomization, n = 6; case–control or cohort studies, n = 11). Qualitative examination indicates HMD-VR is an effective treatment tool.
Conclusions and Relevance: HMD-VR can be a valuable tool for occupational therapy to simulate environments where clients with anxiety disorders participate. Eliciting presence through multisensory features and body representation may enhance outcomes.
What This Article Adds: Drawing from the VRET literature, this scoping review suggests that HMD-VR can be used by occupational therapy practitioners to simulate ecologically valid environments, evaluate client responses to fearful stimuli, and remediate anxiety though immersion in virtual tasks when participation in natural contexts is unfeasible. Having ecologically valid environments is particularly important for people with anxiety disorders because they need support to cope when they encounter triggers in everyday life environments.
This scoping review suggests that HMD-VR can be used by occupational therapy practitioners to simulate ecologically valid environments, evaluate client responses to fearful stimuli, and remediate anxiety though immersion in virtual tasks when participation in natural contexts is unfeasible.
As many as one-third of adults experience an anxiety disorder in their lifetime that causes moderate to severe impairments (Bandelow & Michaelis, 2015). Occupational therapy is suited to address stress, trauma, and anxiety through remediation and compensation in areas of decreased functional performance, including supporting healthy routines, habits, and participation as well as addressing underlying triggers (American Occupational Therapy Association [AOTA], 2018, 2020). This course of action can involve guided exposure to anxiety-provoking thoughts or activities that challenge clients’ cognitive beliefs and dissociate the stimulus from the anxious response (AOTA, 2014; Phillips et al., 1997). Primary goals of occupational therapy treatment among people with anxiety disorders include reintegration into the community and participation in daily activities in naturalistic environments (Davis, 2011). Some mental health care settings are limited in their ability to guide therapeutic participation in the naturalistic environment because of time and safety precautions (Exley et al., 2011).
A convenient and affordable alternative for enhancing patient outcomes is exposing patients to realistic simulations of these environments through immersive virtual reality (VR), which provides “artificially generated sensory information in a form that people perceive as similar to real-world objects or events” (Wilson et al., 1997, p. 213). VR can be leveraged for creating ecologically valid environments and tasks regardless of the physical, temporal, and financial barriers of mental health care settings. Ecological validity is particularly important for treating anxiety because fears are triggered in daily life activities and environments. VR has been shown to be an effective and affordable way to treat anxiety disorders, including posttraumatic stress disorder (PTSD), phobias, and other specific anxieties that negatively affect participation. In addition, the need for remote and virtual therapy options to address mental illness is urgently growing, in part because of geographic, racial, ethnic, and insurance disparities that make it difficult to access high-quality care in person (Cook et al., 2013).
One approach that can be implemented in VR to treat anxiety is exposure therapy, which helps clients confront fear-inducing stimuli through guided exposures and is often paired with cognitive–behavioral therapy (CBT; American Psychological Association, Society of Clinical Psychology [APA-SCP], 2017). It is client-centered and facilitates habituation, extinction of associations with fearful stimuli, self-efficacy, emotional processing, and participation in life activities (APA-SCP, 2017). Exposure can take place in several forms: (1) in vivo exposure, in which clients face fear in real life; (2) imaginal exposure, in which clients vividly imagine the fear-evoking stimulus; and (3) interoceptive exposure, which replicates physiological signs of anxiety (APA-SCP, 2017).
This therapy also has several forms of pacing, including (1) graded exposure, in which treatment progresses through a client’s fear hierarchy; (2) flooding, which begins with the most fearful stimulus; and (3) systematic desensitization, which includes relaxation techniques (APA-SCP, 2017). VR exposure therapy (VRET) is a more convenient and cost-effective form of exposure therapy that uses well-crafted virtual environments (VEs) to elicit the sense of anxiety and presence that the client would experience during real exposures (Botella et al., 2017; Motraghi et al., 2014). Presence is the user’s subjective experience of being immersed in the VE. Presence contributes to the effectiveness of VR for behavior change (Slater & Sanchez-Vives, 2016) and is influenced by the sensory features of the VE, such as avatars (Malbos et al., 2013; Schäfer et al., 2015), type of display (cave automatic virtual environment [CAVE] vs. VR in head-mounted displays [HMD-VR]; Juan & Pérez, 2009; Krijn et al., 2004), and motion simulation (Mühlberger et al., 2005). VRET is typically used and studied in the context of psychotherapy; however, in this scoping review, we examine principles of VRET that can be used by occupational therapy practitioners in their holistic treatment of people with anxiety (Phillips et al., 1997).
Previous reviews analyzing the effectiveness of VRET for PTSD, phobias, and anxiety disorders included both immersive (HMD-VR) and nonimmersive VRET and found that VRET can be effective; however, clinical application is limited (Botella et al., 2017; Meyerbröker & Emmelkamp, 2010; Morina et al., 2015; Motraghi et al., 2014). Considering the potential application of HMD-VR to occupational therapy psychosocial practice for treating anxiety, the purpose of this scoping review is to (1) qualitatively examine recent literature from other disciplines using VRET in HMD-VR and (2) identify principles of this approach that can be translated to occupational therapy practice.
Method
Given the recent development of affordable HMD-VR and the limited number of randomized controlled trials (RCTs), a scoping methodology was used to explore exposure therapy with HMD-VR. Scoping reviews use analytic frameworks to identify relevant literature and gaps in the current evidence base. Scoping reviews do not assess or exclude studies on the basis of the quality of evidence and do not aggregate findings (Arksey & O’Malley, 2005). The overall objective of this scoping review is to identify implications for occupational therapy practice and discern gaps in the literature to guide future research. The following primary and secondary questions guided this scoping review: (1) How has HMD-VR been used for psychosocial rehabilitation in the treatment of anxiety-related disorders? (2) What principles of VRET in HMD-VR can be applied to occupational therapy practice?
In collaboration with a research librarian, we performed a comprehensive literature search of seven electronic databases: CINAHL, Cochrane Library, Embase, ERIC, PsycINFO, Ovid MEDLINE, and Web of Science. Search terms included HMD-VR constructs, products, and therapy concepts (Supplemental Table 1, available online with this article, contains a full list of search terms). The search included all publications since 2000. An initial search was conducted on July 25, 2018, and a supplemental search was completed on January 6, 2020, to capture recent literature in this rapidly evolving area of study. Results were uploaded to an EndNote Library with EndNote X8 (Clarivate Analytics, Philadelphia, PA), and duplicates were removed. All citations and abstracts were uploaded to Covidence (Melbourne, Victoria, Australia) for screening by at least two independent reviewers (Miranda R. Donnelly, Renee Reinberg, Kaori L. Ito, David Saldana, Meghan Neureither, Allie Schmiesing, Esther Jahng). Citations that passed the screening were included in a full-text eligibility review, which was conducted independently by at least two of the same reviewers. For both phases, a third reviewer (Sook-Lei Liew) resolved disagreements.
Studies were included if they (1) used HMD-VR, (2) included a population with anxiety-based disorders, (3) administered the intervention in a practice area within the scope of occupational therapy, and (4) reported experimental data with human participants. We excluded letters, commentaries, textbook chapters, technical descriptions, dissertations, theses, theoretical papers, conference proceedings (≤4 pages), reviews, studies not reported in English, studies that used other virtual modalities (i.e., augmented reality, mixed reality, projection, computer screens), and studies for which the full text was not freely available.
We used a descriptive–analytical method to extract data, compare studies, and contextualize the presented outcomes (Arksey & O’Malley, 2005). In this scoping review, we analyzed the clinical population, the level of evidence, study sample characteristics, provider, HMD-VR technology and intervention, the frequency and duration of treatment (VR exposures and concurrent therapy), and total exposure time (total treatment time minus time spent on other therapeutic activities; Table A.1 in the appendix). In addition, we report specific sensory features of the VEs. We describe the level of evidence using Melnyk and Fineout-Overholt’s (2005) hierarchy, where Level 1 indicates the strongest evidence, including systematic reviews of RCTs and practice guidelines; Level 2 includes RCTs; Level 3 includes nonrandomized controlled trials; Level 4 includes case–control and cohort studies; Level 5 includes systematic reviews of descriptive and qualitative reports; Level 6 includes single descriptive or qualitative studies; and Level 7 includes expert opinions and reports. Evidence for Levels 1, 5, and 7 was excluded from this scoping review because studies with those levels of evidence do not report novel experimental data.
Results
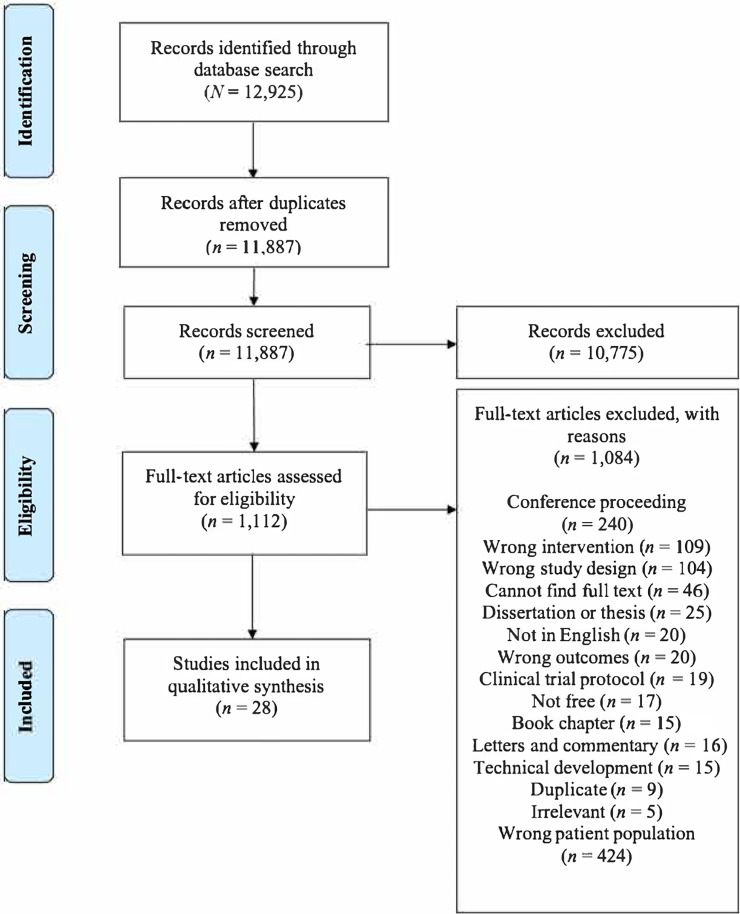
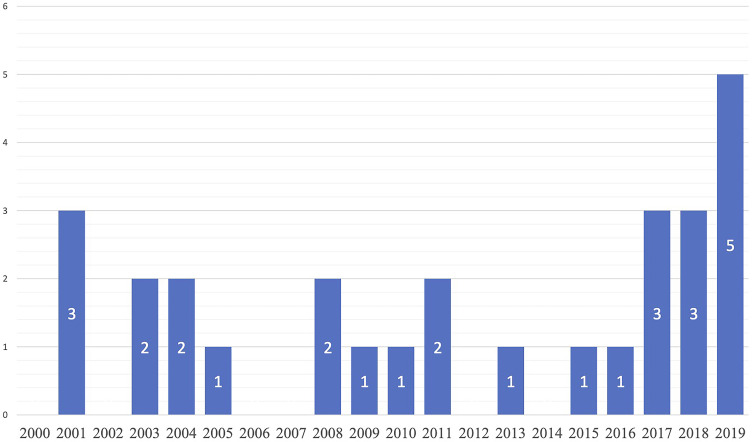
The initial search yielded 8,415 abstracts, and the supplemental search yielded 4,510 abstracts. After the removal of 1,038 duplicates, 11,887 underwent abstract screening, of which 10,775 did not meet the inclusion criteria. We completed full-text reviews of 1,112 articles, and 28 articles met the requirements for inclusion. Figure 1 shows the results of the search process with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines flow diagram (Moher et al., 2009). The results reveal an increase in articles applying HMD-VR to exposure therapy in recent years (Figure 2). The included articles were sorted by population through a post hoc manual analysis (Figure 3). In this scoping review, we describe HMD-VR for the treatment of PTSD (n = 3), specific phobias (n = 19), and performance-based social anxiety (n = 6).
Figure 1.
Flow diagram for inclusion and exclusion of peer-reviewed studies in the scoping review.
Note. Figure format from “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement,” by D. Moher, A. Liberati, J. Tetzlaff, and D. G. Altman; PRISMA Group, 2009, PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Figure 2.
No. of articles included in the scoping review by publication year.
Figure 3.
No. of articles included in the scoping review by population.
Note. PTSD = posttraumatic stress disorder.
Table A.1 shows the basis of analysis for each article. Eleven were RCTs (Level 2), 6 were controlled trials without randomization (Level 3), and 11 were case–control or cohort studies (Level 4). Sixteen articles did not report the therapy provider, and 1 study was fully self-guided. The remaining studies used psychologists (n = 5), music educators (n = 2), unspecified therapists (n = 3), and a dentist (n = 1). The most common HMD-VR used were the Oculus Rift (Oculus VR, Menlo Park, CA; n = 4), Samsung Gear VR system with smartphone (Samsung Electronics, Seoul, South Korea; n = 4), Virtual Research Systems V6 or V8 (Virtual Research Systems, Aptos, CA; n = 4), VFX-3D (Interactive Imaging Systems, Rochester, NY; n = 3), and a cardboard viewer with a smartphone (n = 2).
The total time spent in exposure varied widely among studies, from as short as 5 to 15 min (Bouchard et al., 2008; Donker et al., 2019; Gromer et al., 2019; Gujjar et al., 2019; Juan & Pérez, 2009; Pertaub et al., 2001; Schäfer et al., 2015) to as long as 8 to 12 hr (Cárdenas-López & Rosa-Gómez, 2011; Malbos et al., 2008; Walshe et al., 2003). Each study had different treatment schedules, total exposure time, and time in HMD-VR relative to time spent on other therapeutic activities. Because the reporting of timing was inconsistent, the estimations presented in Table A.1 are based on available information on the number of exposure sessions reported and time spent in each exposure. The VRET protocols varied across the studies, and we discuss differences in dosage, approach, and intervention for each study.
Posttraumatic Stress Disorder
Three studies used VRET paired with conventional therapy techniques to treat PTSD and found clinically significant improvements. One study implemented VRET with a victim of assault (Cárdenas-López & Rosa-Gómez, 2011), and 2 studies implemented VRET with combat veterans (McLay et al., 2011; Rothbaum et al., 2001). All 3 studies implemented repeated exposures over multiple weeks in a variety of VEs.
VRET was implemented with different exposure techniques across studies, although all three providers manipulated the environment in real time to maintain therapeutic levels of anxiety. Cárdenas-López and Rosa-Gómez (2011) used a graded approach through three virtual scenarios, progressing from standing in a dangerous area to being in a vehicle with a dangerous person. Similarly, an RCT by McLay et al. (2011) used graded exposure to progress through a custom hierarchy of veterans’ most salient traumatic memories. Rothbaum et al. (2001) used a variation of imaginal exposure to trigger salient traumatic memories while the psychologist manipulated the VE to match the veteran’s narration.
Previous research has shown that a key way to manipulate users’ sense of presence in the VE is by adding sensory modalities (Slater & Sanchez-Vives, 2016). All 3 studies used auditory features, such as city or wartime sounds. Rothbaum et al. (2001) added haptic feedback, which includes any simulated touch provided by hardware (i.e., vibration, proprioceptive information), for the helicopter scenario to increase the realism of the experience.
All protocols included sessions of conventional therapy and education to supplement VRET. Specific interventions included development of fear hierarchies (Cárdenas-López & Rosa-Gómez, 2011), breathing relaxation (Rothbaum et al., 2001), and autonomic control training with biofeedback (McLay et al., 2011). McLay et al. (2011) compared the outcomes from VRET with those of a control group, which received standard psychotherapy treatment including a combination of exposure, cognitive therapy, medication, and other services as determined by their providers. Despite both groups receiving conventional therapy interventions, a higher percentage of veterans in the VRET group achieved a clinically significant improvement in fewer sessions (70.0% ; M = 12.3 sessions) than the treatment-as-usual group (12.5% ; M = 13.8).
These studies demonstrate that VRET can be effective for decreasing anxiety among people with PTSD; however, VRET may not be appropriate for every clinical case of PTSD. Although client-centered treatments appear to be effective, creating custom immersions for people with a wide range of trauma experiences may prove costly and unfeasible. For example, Rothbaum et al. (2001) excluded one-quarter (n = 3) of participants after beginning treatment because their trauma experiences were too dissimilar to the VEs available. Another challenge to translating HMD-VR from research to practice is the high rate of comorbid mental illnesses, including depression, substance use disorders, and other anxiety disorders (Brady et al., 2000). For example, McLay et al. (2011) excluded recruits with suicidality, homicidality, psychosis, and alcohol dependence, so it is unclear whether VRET is appropriate for people with these comorbid disorders. Conversely, Rothbaum et al. included participants with depression, past substance and alcohol abuse and dependence, and dysthymia. For occupational therapy practitioners treating PTSD (Edgelow et al., 2019), HMD-VR can be effective for treating people with comorbid disorders, but future research needs to determine clinical indicators of success.
Specific Phobias
Nineteen studies used VRET for people with specific phobias. To be classified as a phobia (vs. a fear), the fearful stimulus must consistently provoke anxiety disproportionate to the sociocultural context and the real danger it poses (American Psychiatric Association [APA], 2013). This scoping review includes studies of VRET for acrophobia (n = 8), agoraphobia (n = 4), arachnophobia (n = 3), fear of flying (n = 1), dental phobia (n = 1), fear of driving (n = 1), and fear of snakes (n = 1). Twelve of these studies reported that VRET is effective for decreasing anxiety. The 7 remaining studies evaluated the effect of features of the VE on presence and anxiety (Bouchard et al., 2008; Gromer et al., 2019).
Acrophobia
Eight studies reported on VRET as a treatment of acrophobia, which is a diagnosed fear of heights. Five of these studies evaluated the effectiveness of VRET and found that it reduced anxiety, and 3 studies examined anxiety and presence in the VE. Of the effectiveness studies, 1 study examined exposure in HMD-VR versus in real life (Abdullah & Shaikh, 2018). Participants were assigned to one of two groups and received either VR exposure to height scenarios (e.g., being on the top of a mountain and a city building) or real exposure to the same scenarios. Despite both groups having the same content, frequency, and duration of exposure, VRET with motion tracking was found to be more effective and feasible than real exposure for reducing anxiety.
Hong et al. (2017) also studied VRET with people with acrophobia, grouping them by low and high fear and exposing them to elevator taking, cliff driving, heli-skiing, and rooftop walking in a self-guided HMD-VR exposure. The virtual tasks elicited high levels of anxiety, and both groups demonstrated improved acrophobia symptoms after treatment, although the high-fear group had a greater reduction in anxiety than the low-fear group (Hong et al., 2017). Similarly, Choi et al. (2001) implemented self-guided exposures to a virtual open-sided elevator, progressing to the 25th floor over six sessions. In this case study, HMD-VR exposure to heights was effective for decreasing subjective distress with carryover of improved cognitive skills and acrophobic symptoms to an in vivo 60-floor elevator ride.
In an RCT, Donker et al. (2019) also implemented a self-guided treatment in which participants completed activities in a virtual theater, such as standing on balconies, ladders, and bridges, in conjunction with CBT modules. Compared with the control group, the acrophobia group had significantly reduced anxiety, and people who spent more time using the program experienced greater improvement, presence, and task mastery. Finally, Krijn et al. (2004) conducted an RCT comparing HMD-VR, CAVE, and no intervention, and they gradually exposed participants in the HMD-VR and CAVE groups to a four-floor shopping mall, a six-floor fire escape, a roof garden, and an eight-floor building site over three exposures. They found that CAVE exposure resulted in greater presence than HMD-VR exposure; however, HMD-VR and CAVE were equally effective for decreasing anxiety and avoidant behaviors for up to 6 mo afterward.
The 3 remaining studies analyzed anxiety and presence in acrophobic scenarios. One study questioned whether integrating the user’s own movements as an avatar in the VE increased subjective presence ratings. Previous literature has shown strong evidence that being present in a VE and feeling ownership of an avatar can trigger psychological, physiological, and behavioral changes (Slater & Sanchez-Vives, 2016). Schäfer et al. (2015) found a trend of greater presence among the motion tracking group but did not find differences in behavioral or physiological changes between groups. Gromer et al. (2019) conducted an RCT and exposed people with acrophobia to a fearful scenario and two control scenarios in HMD-VR. Participants were randomized to experience the VEs in either high or low realism, and researchers found that the high-realism group had higher presence and greater fear responses. Finally, Juan and Pérez (2009) conducted an RCT comparing levels of anxiety and presence in an acrophobic VE presented in CAVE or HMD-VR. Healthy participants were immersed in a terrorism scenario and instructed to find a suspicious package. While they searched the room, the researchers induced the sensation of falling through the floor. The exposure elicited anxiety and a sense of presence in both environments, but the CAVE group had higher presence.
Six of the 8 studies implemented graded exposure. Four studies were self-guided exposures in which participants paced their progression toward the most fearful stimuli. Three of these studies had a provider present for technological support and safety (Choi et al., 2001; Krijn et al., 2004; Schäfer et al., 2015), whereas Hong et al. (2017) had no provider present. In 2 studies, VRET was administered with conventional therapy. Choi et al. (2001) educated on relaxation techniques, including abdominal breathing and progressive muscle relaxation via a provider, whereas Donker et al. (2019) used self-guided 2D virtual CBT lessons.
Multisensory features of the VE were used to enhance immersion. In addition to audio instructions provided in some studies (Donker et al., 2019; Gromer et al., 2019; Hong et al., 2017; Juan & Pérez, 2009; Schäfer et al., 2015), Choi et al. (2001) used sounds of wind and a moving elevator in coordination with the visual display to elicit a sense of upward movement, noting high anxiety with exposure. Two studies used a Microsoft Kinect (Microsoft, Redmond, WA) to track user motion and update avatar movement accordingly (Abdullah & Shaikh, 2018; Schäfer et al., 2015). Movement tracking is used to increase realism, users’ sense of presence in the VE, and anxiety levels to optimize treatment benefits.
Finally, common comorbid conditions associated with acrophobia may influence the effectiveness of the treatments described here, including general anxiety and specific anxiety disorders (Kapfhammer et al., 2015), and each study had different inclusion or exclusion of comorbid conditions. Thus, although VRET appears to be effective for the treatment of acrophobia, more research is required to determine its effectiveness among people who have comorbid mental illness.
Agoraphobia
Four studies reported the use of VRET to treat people with agoraphobia, which is anxiety provoked by situations in which escape would be difficult or impossible, such as being in enclosed spaces or using public transportation; agoraphobia can be diagnosed with or without panic disorder (APA, 2013). Claustrophobia is a distinct condition but is included here because the exposures used were similar to agoraphobia.
All 4 studies exposed participants to several everyday life scenarios that evoked agoraphobic symptoms, such as taking public transportation, visiting a supermarket, and driving a car. Three studies evaluated the effectiveness of VRET, and 1 study evaluated the ability of VEs to elicit anxiety. The 3 effectiveness studies implemented exposures over multiple sessions, and all found decreased anxiety and symptoms of agoraphobia after treatment with HMD-VR (Malbos et al., 2008; Pérez-Ara et al., 2010; Rahani et al., 2018). An RCT found that improvements remained 3 mo after treatment (Pérez-Ara et al., 2010). The therapy protocols varied among these 3 studies: Malbos et al. (2008) and Rahani et al. (2018) used graded exposure, whereas Pérez-Ara et al. (2010) used interoceptive exposure. Conventional therapy and educational techniques were used concurrently with VRET and addressed anxiety, relaxation, and cognitive restructuring (Malbos et al., 2008; Pérez-Ara et al., 2010). The studies that paired VRET with other therapy yielded the most conclusive positive results.
The 4th study evaluated nine graded VEs to determine whether they could evoke sufficient stress responses among people with agoraphobia (Malbos et al., 2013). To enhance realism, each VE featured a first-person perspective of a virtual body, realistic images, advanced artificial intelligence of other virtual characters, and dynamic shadows. In addition, the user could interact with the VE to effect change and navigate a car using a steering wheel with vibration feedback. All nine VEs were perceived as fearful and anxiety eliciting, which is key to the effectiveness of HMD-VR as a treatment tool.
Three of the 4 agoraphobia studies in this scoping review included people with comorbid phobias and panic disorder and reported positive outcomes (Malbos et al., 2008, 2013; Pérez-Ara et al., 2010). In addition, 2 studies demonstrated carryover of skills after VRET treatment (Malbos et al., 2008; Pérez-Ara et al., 2010).
Arachnophobia
Three studies used VRET to treat arachnophobia, an extreme anxious response to spiders that impairs social and occupational functioning (APA, 2013). Minns et al. (2018) conducted an RCT and found that watching 3D graded exposure footage of a spider in HMD-VR with concurrent psychoeducation about spiders and anxiety was more effective for reducing anxiety than education alone. In addition, the HMD-VR group showed higher levels of immersion than the group that watched a control video about music in 2D; however, it is unclear whether it was the spider-related content or the HMD-VR (or both) that affected immersion.
Miloff et al. (2019) also conducted an RCT and found that a graded puzzle game in HMD-VR was less effective than standard in vivo exposure therapy, suggesting that this VRET game was not effective for treating arachnophobia. It is interesting to note that despite using realistic footage, Miloff et al. found that the puzzle game elicited far less anxiety than real exposure and that the participants were disappointed by the treatment.
The 3rd study explored how fear triggers interact with body representations in HMD-VR to determine whether the presence of a virtual hand facilitates higher levels of therapeutic anxiety (Peperkorn et al., 2016). They were able to elicit high levels of anxiety in the arachnophobia group compared with the healthy group and found that the presence of a virtual hand near a virtual spider significantly increased anxiety. This finding suggests that a first-person body representation may facilitate higher levels of immersion, presence, and anxiety when a fearful stimulus is present. Overall, these studies suggest that body representation in VR and realistic footage may be important features when designing VEs for the treatment of arachnophobia; however, more research is needed to understand how exposure frequency and duration optimize patient outcomes.
Other Specific Phobias
Four studies reported the use of VRET for other specific phobias that negatively affect participation in daily occupations, including fear of flying, dental phobia, fear of driving, and fear of snakes. In an RCT of people with a fear of flying, Mühlberger et al. (2005) studied the effect of haptic motion simulation during HMD-VR exposure on fear reactions. All participants received education about fear of flying, coping methods, cognitive therapy, and four virtual flight simulations. Half the participants also received motion simulation during their HMD-VR exposure, whereas the other half did not. Although both groups showed similar anxiety during the flight simulations and outcomes, only the motion group showed increased heart rate, skin conductance responses, and slower habituation.
Gujjar et al. (2019) compared the effectiveness of VRET versus an informational pamphlet among people with dental phobia in an RCT. After 10 min of exposure to dental scenarios from the first-person perspective, the mean anxiety scores decreased significantly, whereas the pamphlet evoked no change.
Walshe et al. (2003) implemented VRET with people who had a fear of driving and found notable reductions in travel distress, avoidance, and maladaptive driving strategies posttreatment when combined with breathing education and cognitive reappraisal. Despite positive results for participants who completed the study, Walshe et al. excluded half (n = 7) of participants because they could not become immersed in the VE, even with the combination of visual, auditory, and haptic features.
Finally, Bouchard et al. (2008) questioned whether anxiety directly affected presence. In this RCT, people with snake phobia experienced three VEs: a control, a desert they were told had no snakes, and a desert they were told did have snakes. Despite never actually seeing a virtual snake, the knowledge that snakes were present elicited high levels of anxiety and subjective presence compared with the other VEs.
Performance-Based Social Anxiety
Six studies examined the use of VRET for performance-based social anxiety, including the fear of public speaking (n = 4) and music performance (n = 2). Pertaub et al. (2001) implemented VRET for public speaking anxiety with confident and phobic participants. Participants in both groups gave speeches in HMD-VR to either an empty room or an audience of avatars. The phobia group had the highest anxiety in the audience condition, but they experienced higher anxiety in both conditions compared with the confident group, who remained stable.
In another study, clinical psychologists used one session of VRET with adolescents who had a fear of public speaking (Kahlon et al., 2019). Participants were exposed to an audience of avatars and prompted to complete seven speech activities in addition to CBT education. Public speaking anxiety considerably improved, with stability at 1- and 3-mo follow-ups.
In a 3rd study, Kim et al. (2017) evaluated a self-guided VRET training program for social anxiety, in which participants completed graded public speaking tasks in a virtual school, a business environment, and other everyday life scenarios. Both the healthy and anxious groups showed decreased anxiety, with larger decreases in anxiety for the anxious group.
Another self-guided VRET by Stupar-Rutenfrans et al. (2017) showed that students with moderate to high public speaking anxiety were able to lower their anxiety through three sessions of practice speeches in graded VEs. Similar to the previous studies, this therapy was the most effective for those with high levels of anxiety.
The 2 studies conducted by Orman (2003, 2004) applied VRET with saxophone students to decrease performance anxiety. Orman (2003) exposed students to music performance venues, including a practice room, a student audience, a faculty audience, and a room with the band director. Qualitative investigation revealed that students had higher heart rate, a sign of anxiety, in the practice room but had higher subjective discomfort in the audience scenarios. Gaze observation showed that participants avoided looking at the faculty and director avatars. Orman (2004) found that VRET with the aforementioned VEs was feasible and effective in eliciting performance anxiety in musicians.
Discussion
The purpose of this scoping review was to qualitatively examine literature that applies HMD-VR to anxiety disorder treatment and to identify principles of VRET that are applicable to occupational therapy psychosocial practice. After a rigorous search process, we identified 28 studies that met the inclusion criteria, and we grouped results by clinical population. All articles in this review used HMD-VR to provide exposure therapy to people with anxiety, which affects participation in daily occupations and environments.
The qualitative results of this scoping review indicate that HMD-VR can be a useful therapeutic tool for decreasing symptoms among people with anxiety disorders, including PTSD, specific phobias, and performance-based anxiety. Of the 28 studies included, 17 found that VR exposures yielded positive patient outcomes. One study found no notable difference between standard care and VR-based treatment (Pérez-Ara et al., 2010). Another study found that standard care was significantly more effective than VR exposures (Miloff et al., 2019), which may be explained by the lack of realism of the stimuli (i.e., cartoon spiders) in the VE rather than the effectiveness of VRET as a therapy. The remaining 9 studies did not examine the efficacy of VRET but instead analyzed whether the VEs could elicit therapeutic levels of anxiety. They all found HMD-VR was a feasible method for inducing anxiety, but 1 study found that CAVE VR could induce even greater anxiety (Juan & Pérez, 2009).
Virtual Reality in Head-Mounted Displays in Occupational Therapy Psychosocial Rehabilitation
Given the findings that realistic VEs presented in HMD-VR can induce anxiety comparable with the anxiety experienced in naturalistic environments, HMD-VR may be a useful tool in occupational therapy psychosocial rehabilitation. Immersive VR can be used by occupational therapy practitioners to simulate complex, naturalistic environments for discharge planning and task practice when participation in clients’ natural environments is unfeasible. For example, inpatient psychosocial care focuses on stabilization and discharge planning; however, it is often unfeasible to observe clients participate in their home and community environments before discharge because of temporal, safety, regulatory, and financial barriers. HMD-VR is a safe, affordable, and time-effective tool for exposing clients to simulated, ecologically valid home and community environments and for evaluating readiness for discharge.
Another application of HMD-VR within occupational therapy psychosocial rehabilitation across the continuum of care is the use of realistic VEs for practicing skills in novel environments. For example, occupational therapy practitioners help clients learn coping strategies to manage symptoms of illness, establish healthy habits and routines, and make decisions that support their wellness (AOTA, 2016). For clients whose anxieties and phobias make it difficult for them to practice the skills they learn through occupational therapy in the real environment, ecologically valid VEs displaying supermarkets, parks, malls, streets, or homes, among others, can serve as proxy environments. Because VRET is affordable and portable, occupational therapy practitioners can take VRET to community mental health consumers’ homes, homeless shelters, places of employment, and other contexts or provide therapy remotely when access to mental health providers is limited (Cook et al., 2013). Occupational therapy practitioners can observe consumers’ triggers during daily activity in real environments, then manipulate the VE to provide controlled task practice that may not be feasible in reality but will promote the transfer of skills to other natural contexts. Task performance and skill practice in HMD-VR support the treatment plan and complement other occupational therapy approaches.
Principles of Virtual Reality in Head-Mounted Displays for Occupational Therapy Practice
This scoping review demonstrates that HMD-VR is a useful and evidence-based tool for treating anxiety through virtual exposures to anxiety-provoking environments. We also identify ways that occupational therapy practitioners can use HMD-VR as a tool for treating anxiety within a treatment plan. As the results suggest, not all virtual exposures are effective, but features of VEs can be optimized to improve the success of treatment. Having a sense of presence in HMD-VR is important for eliciting anxiety for effective exposures, although no specific threshold of presence was identified and presence is not the only indicator that a VE will yield therapeutic outcomes. Features of VRET that were reported to enhance patient outcomes include sensory features, body representation, time, concurrent treatments, and client factors. Occupational therapy practitioners can translate these findings from VRET to occupational therapy–specific applications of HMD-VR for treating anxiety.
Sensory Features
The use of sensory features in VEs, including visual and auditory stimulation, haptic feedback, and motion tracking, may influence presence and anxiety when they create a realistic environment (Gromer et al., 2019). When taken together, the results about sensory features of VR from this scoping review suggest that (1) visual and auditory stimulation are fairly standard and appear to give rise to a sense of presence, and (2) haptic feedback and motion tracking can increase realism of the VE but may not be necessary.
In this scoping review, 19 studies used auditory input, including voiceover guidance, ambient sounds, or feedback, and it was found to be beneficial. Only Orman (2003) found that audio detracted from the realism of the virtual experience because of low-fidelity sounds. Audio that aligns with the task and environment should be used when applying HMD-VR clinically to increase realism and evoke a sense of presence.
Four studies in this scoping review found that haptic feedback was successful at improving the realism of the VEs, including simulated vibrations of aircraft (Mühlberger et al., 2005; Rothbaum et al., 2001) and vibration-feedback steering wheels (Malbos et al., 2013; Walshe et al., 2003). Despite the benefit of improved realism, haptic feedback did not always increase users’ sense of presence (Walshe et al., 2003). Even when haptic feedback did evoke a greater sense of presence, this result did not improve patient outcomes significantly (Mühlberger et al., 2005). Motion tracking was implemented in 2 studies but was not credited with significantly improving patient outcomes (Abdullah & Shaikh, 2018; Schäfer et al., 2015). In terms of clinical feasibility, this scoping review does not provide strong evidence for investing in haptic features or motion tracking for applying HMD-VR with people who have anxiety disorders.
Embodiment
Two studies showed that body representation increased the realism of the VE and elicited a greater sense of presence and fear at subjective and behavioral levels (Peperkorn et al., 2016; Schäfer et al., 2015). This finding may be explained by previous literature showing that when users see a first-person representation of themselves in the VE (an avatar) and experience visuomotor synchrony with it, the illusion of body ownership arises. This illusion allows users to feel a sense of embodiment in the avatar and interact with the VE more naturally (Slater & Sanchez-Vives, 2016). This scoping review supports previous literature reporting that the use of avatars can be helpful for clinical applications in HMD-VR.
Dosage
A third consideration for applying HMD-VR to occupational therapy practice is dosage. Anecdotally, the schedule and total exposure time for PTSD treatment were longer than for other clinical groups. For some clinical groups, such as people with acrophobia, the longer protocols yielded more conclusive and positive patient outcomes. However, in other clinical groups, such as people with arachnophobia, time did not seem to be associated with outcomes. These observations indicate that the amount of time clients are exposed to anxiety-provoking stimuli may affect the effectiveness of HMD-VR–based anxiety treatment. However, there appears to be variability based on the type of anxiety or phobia and client experiences of presence (Gromer et al., 2019). Taken with previous findings, we speculate that time interacts with sense of presence, body representation, and comorbidities to influence outcomes. More research is needed to determine dosage for HMD-VR for treating people with anxiety and the interactions between time and other features of HMD-VR.
Concurrent Treatment
Finally, more than half of the studies (n = 15) used conventional therapy techniques in addition to HMD-VR. Across these studies, fear hierarchies, education about anxiety, relaxation training, and CBT-based cognitive restructuring were among the most common interventions, which are also methods that can be used in psychosocial occupational therapy practice. Additional interventions included providing participants with written information about fearful stimuli, particularly in the case of specific phobias, and preparatory activities for carryover to exposures in daily life. Results suggest that HMD-VR should be used as a modality within the context of a broader treatment plan.
Future Directions for Occupational Therapy Research
Evidence supports HMD-VR as a feasible and effective tool for reducing anxiety through controlled, therapeutic exposures; however, gaps in the literature should be addressed when translating findings to occupational therapy practice. First, to advance the science of HMD-VR as a tool for psychosocial occupational therapy, consistent reporting guidelines should be established. This scoping review revealed gaps in which features of the VE and therapy protocol are reported, which makes it challenging for clinicians to make evidence-based decisions about duration, sensory features, and client indicators of success. Increasing transparency of methods will improve reproducibility and translation to the clinical space.
Second, occupational therapy theory describes interactions between the person and the environment, and this perspective should be represented in future studies using HMD-VR to enhance psychosocial rehabilitation. Anxiety disorders are complex conditions that arise from multiple sources and are interwoven into daily life. Occupational therapy practitioners address the complex and naturalistic sources of anxiety, but this role is not reflected in the literature applying HMD-VR in populations with anxiety. The current gaps in understanding the features of the VE and client characteristics that lead to optimized outcomes are complementary to occupational therapy’s insights about environmental influences of participation, patterns of behavior, physiological measures of wellness, and emotional regulation. In addition, future research should evaluate the use of HMD-VR with other occupational therapy treatment approaches. Occupational therapy is well positioned to engage in the ongoing development of complex interventions that use HMD-VR for anxiety.
Implications for Occupational Therapy Practice
The evidence presented in this scoping review indicates that HMD-VR is a valuable tool for occupational therapy psychosocial rehabilitation to simulate environments and activities that clients can take part in as they progress toward anxiety-free participation in meaningful activity. In addition to finding that HMD-VR treatment can be effective for reducing anxiety, we also parsed out some of the key features of VRET for translation to occupational therapy clinical practice:
HMD-VR is a safe, affordable, and effective tool that can allow occupational therapy practitioners to simulate natural contexts in the clinic for activities of daily living, instrumental activities of daily living, and coping skills practice.
HMD-VR interventions should include visual and auditory features to evoke a sense of presence, and other sensory features may not be necessary.
VEs can be easily manipulated to optimize the congruence between the person and environment.
Conclusion
The findings of this scoping review support the use of HMD-VR as a tool to treat people with anxiety in psychosocial occupational therapy practice. VEs presented in HMD-VR can serve as proxies for clients’ naturalistic environments in cases in which exposure to real anxiety-inducing stimuli is not feasible. Inducing anxiety in HMD-VR can facilitate the therapeutic process by giving clients safe environments in which to apply the skills they have developed in therapy and providing therapists the opportunity to observe clients’ engagement in nonclinical environments. Further occupational therapy research is needed to identify best practices for implementing HMD-VR with clients who experience disruptions to their participation in occupations as a result of anxiety.
Supplementary Material
Acknowledgments
This research was funded by American Heart Association Grant 16IRG26960017, U.S. Army Research Office Grant W911NNF-14-D-0005, and National Institutes of Health Grant K01HD091283. We thank Jennifer Dinalo for guidance and facilitation through this process.
Appendix. Evidence Tables for the Scoping Review of Virtual Reality for the Treatment of Anxiety Disorders
Table A.1.
Summary of Evidence Regarding VRET for Treating Anxiety, by Population, Included in the Scoping Review
| Author/Year | Level of Evidence | Sample and Population | Provider | HMD-VR Technology | HMD-VR Intervention | Frequency/Duration | Estimated Exposure Time |
|---|---|---|---|---|---|---|---|
| Posttraumatic Stress Disorder | |||||||
| Cárdenas-López & Rosa-Gómez (2011) | Level 4 | N = 1 veteran with PTSD | Therapist (unspecified) | Vuzix iWear® VR920 (Vuzix, Rochester, NY) | Repetitions of the traumatic memory on the streets of Mexico City, on a pedestrian bridge, and in a vehicle | 10 weekly, 90-min sessions | Up to 9 hr |
| McLay et al. (2011) | Level 2 |
N = 20 veterans with PTSD n = 10 control participants n = 10 participants receiving VRET |
Licensed psychologist | Unspecified VR goggles with built-in headphones used with joystick controller | Simulation of Iraq or Afghanistan approximating most salient traumatic experiences | 1–2 sessions/wk, up to 10 wk, 50 min each | Between 160 and 320 min |
| Rothbaum et al. (2001) | Level 4 | N = 10 veterans with PTSD | Clinical psychologist | Virtual Research V6 (Virtual Research Systems, Aptos, CA) used with electro magnetic tracking (Polhemus, Colchester, VT) | 2 VEs: virtual jungle clearing and virtual helicopter Imaginal exposure with therapist controlling VE to mirror patient’s description |
8–16 biweekly, 90-min sessions | Approximately 6 hr |
| Specific Phobias: Acrophobia | |||||||
| Abdullah & Shaikh (2018) | Level 3 |
N = 20 participants with acrophobia n = 10 participants receiving in vivo exposure n = 10 participants receiving VRET |
Unspecified | Gear VR with Samsung Galaxy S7 Edge (Samsung Electronics, Seoul, South Korea) used with Microsoft Kinect (Microsoft, Redmond, WA) | 2 height exposure scenarios: atop a mountain and a city building | 8 weekly, 25-min sessions | Approximately 200 min |
| Choi et al. (2001) | Level 4 | N = 1 participant with acrophobia | Unspecified | ProView™ XL50 (Kaiser Electro-Optics, Ann Arbor, MI) used with motion tracking (Polhemus, Colchester, VT) and Nascar Force Pro™ driving simulator (Thrustmaster, Carentoir, France) | Riding a 4-sided open elevator starting from the 1st floor through the 25th floor while looking down | 6 sessions, 30 min each | Between 80 and 100 min |
| Donker et al. (2019) | Level 2 |
N = 193 participants with acrophobia n = 96 participants receiving VRET n = 97 wait‒list control participants |
Self-guided | Google Cardboard (Google, Mountain View, CA) used with unspecified smartphone | Completing tasks in a 3D theater environment: standing on a tall ladder, standing on balconies, walking on a high bridge, and bungee jumping | 6 modules (5–40 min each) over 3 wk; only 1 module completed in HMD-VR |
Between 5 and 40 min |
| Gromer et al. (2019) | Level 2 | N = 49 participants who were fearful of heights | Unspecified | HTC Vive (HTC, New Taipei City, Taiwan) | Height scenario (edge of a deep canyon) and a control forest scenario | 1 session, 3 exposures | Approximately 3 min |
| Hong et al. (2017) | Level 3 |
N = 48 participants with acrophobia n = 24 participants with low fear n = 24 participants with high fear |
Unspecified | Gear VR with Galaxy S6 (Samsung Electronics, Seoul, South Korea) | 4 missions: elevator taking, cliff driving, heli-skiing, and rooftop walking | 4 sessions over 2 wk (20 min each) | Approximately 40 min |
| Juan & Pérez (2009) | Level 2 | N = 25 healthy participants | Unspecified | 5DT (Virtual Realities, League City, TX) used with WingMan Cordless Rumblepad (Logitech, Lausanne, Switzerland) | Acrophobia scene: floor falling away | 1 immersion lasting 7 min | 7 min |
| Krijn et al. (2004) | Level 2 |
N = 30 participants with acrophobia n = 10 participants receiving HMD VRET n = 14 participants receiving CAVE VRET n = 11 wait‒list control participants (some progressed to the experimental group) |
Unspecified | Visette Pro (Cybermind, Leicestershire, United Kingdom) | 4-floor shopping mall, a 6-floor fire escape, a roof garden on a building, and an 8-floor virtual building site | 3 sessions (1.5 hr each; 1 hr of exposure) | 3 hr |
| Schäfer et al. (2015) | Level 3 |
N = 42 healthy participants with acrophobia tendencies n = 21 participants with body tracking n = 21 participants without body tracking |
Therapist (unspecified) | Oculus Rift DK1 (Oculus VR, Menlo Park, CA) used with Microsoft Kinect (Microsoft, Redmond, WA) and SixAxis Controller (Sony Corporation, Tokyo, Japan) | Acclimatization at street level, balcony with railings, and protrusion without railings | 1 session | Average = 295 s |
| Specific Phobias: Agoraphobia | |||||||
| Malbos et al. (2008) | Level 4 | N = 6 participants with claustrophobia | Unspecified | Glasstron LDI-100B (Sony Corporation, Tokyo, Japan) used with a head tracker (Intersense Intertrax, Bedford, MA) | 9 VEs containing a combination of 7 elements: houses, corridors, hallways, caverns, concrete channels, underground access, and elevators | 50–55 min per VE over 8 sessions (5 sessions in HMD-VR) | Between 7.50 and 8.25 hr |
| Malbos et al. (2013) | Level 4 | N = 18 participants with panic disorder and agoraphobia | Unspecified | 42 Pro HMD (Virtual Realities, League City, TX) used with a wireless controller and Logitech Momo steering wheel with vibration and force feedback (Logitech, Lausanne, Switzerland) | 9 VEs: a valley, the outback, lifts, supermarket, subway stations, car parks, a cinema, flying on an airplane, and driving on a highway | 30- to 35-min sessions, unspecified number of sessions | Between 180 and 225 min |
| Pérez-Ara et al. (2010) | Level 2 |
N = 29 participants with agoraphobia, with and without panic disorder n = 14 participants receiving VRET n = 15 participants receiving traditional therapy |
Psychologist | V6 HMD (Virtual Research Systems, Aptos, CA) | Agoraphobic scenarios and audio and visual effects of rapid heartbeat, panting, blurred vision, double vision, and tunnel vision | 8 sessions with up to 6 exposures for the VRET group (50 min each) and 6 exposures for the traditional group (25 min each) | Between 5.0 and 5.5 hr |
| Rahani et al. (2018) | Level 3 |
N = 33 participants n = 14 participants with agoraphobia n = 19 healthy participants |
Therapist (unspecified) | Oculus Rift (Oculus VR, Menlo Park, CA) | A video about fear of closed environments, an elevator in a 10-story building, and a building with an MRI room | Unspecified | Unspecified |
| Specific Phobias: Arachnophobia | |||||||
| Miloff et al. (2019) | Level 2 |
N = 100 participants with arachnophobia n = 50 participants receiving standard treatment n = 50 participants receiving VRET |
Licensed psychologist and psychotherapist | Gear VR (Samsung Electronics, Seoul, South Korea) with smartphone | A serious game with 8 levels of increasingly realistic spider images in puzzles and activities | 3-hr exposures (M = 142.82 min, SD = 21.85) | Approximately 3 hr |
| Minns et al. (2018) | Level 2 |
N = 77 participants with arachnophobia n = 38 participants receiving VRET n = 39 wait‒list participants |
Unspecified | Oculus Rift DK1 (Oculus VR, Menlo Park, CA) | Video footage: spider being held by a model, spider positioned closer to the camera, and spider positioned even closer and moving toward camera | 6 videos (5 min each) | 30 min |
| Peperkorn et al. (2016) | Level 3 |
N = 64 participants n = 32 participants with arachnophobia n = 32 healthy participants |
Unspecified | Z800 3DVisor (eMagin, Hopewell Junction, NY) | Viewing a snake or spider under a glass container in VR while reaching toward the alternate stimulus in the real world | 1 session with 2 blocks (21 min each) | 42 min |
| Specific Phobias: Other | |||||||
| Bouchard et al. (2008) | Level 2 | N = 31 participants with snake phobia | Unspecified | I-Glass (I-O Display Systems, Sacramento, CA) used with Microsoft joystick (Microsoft, Redmond, WA) | Desert with induced anxiety, desert without induced anxiety, and control environment | 3 immersions lasting 5 min | 15 min |
| Gujjar et al. (2019) | Level 2 |
N = 30 participants with dental phobia n = 15 participants receiving VRET n = 15 control participants |
Dentist | Oculus DK2 (Oculus VR, Menlo Park, CA) | Dental operatory for 2 min each for 5 scenarios while sitting in a real dental chair: dental instruments and virtual dentist; virtual dentist moves toward patient with mirror; virtual dentist holds a syringe and moves toward patient; virtual dentist carries a drill without sound, then with sound, toward the patient | 1 session, lasting at least 10 min | Unspecified; each scenario repeated until low anxiety reached |
| Mühlberger et al. (2005) | Level 2 |
N = 25 participants with fear of flying n = 12 participants who underwent motion simulation n = 13 participants who did not undergo motion simulation |
Unspecified | V6 HMD (Virtual Research Systems, Aptos, CA) used with electromagnetic tracking (Polhemus, Colchester, VT) | 4 flight simulations | 1 session of 4 flights (18 min each) | Approximately 80 min |
| Walshe et al. (2003) | Level 4 | N = 14 participants with situational phobia of driving, with or without PTSD | Unspecified | VFX-3D HMD (Interactive Imaging Systems, Rochester, NY) used with WingMan Formula Force GP Wheel and Pedals (Logitech, Lausanne, Switzerland) | Driving in rural and city environments | 12 weekly, 1-hr sessions | Up to 12 hr |
| Performance-Based Social Anxiety | |||||||
| Kahlon et al. (2019) | Level 4 | N = 27 adolescents with fear of public speaking | Clinical psychologist | Unspecified cardboard headset with iPhone 7 (Apple, Cupertino, CA) | 7 speech-related tasks (1–2 min each) in a classroom with 10 adolescent avatars sitting at desks with gaze toward user; empty classroom; lobby | 1 session lasting 90 min (60 min in exposure) | Approximately 1 hr |
| Kim et al. (2017) | Level 4 |
N = 52 participants n = 22 participants with social anxiety disorder n = 30 healthy participants |
Unspecified | Gear VR with Galaxy S6 (Samsung Electronics, Seoul, South Korea) | Public speaking in 3 social situations (school, business, everyday life), each with 4 levels of increasing difficulty and 3 speech topics | 8 self-training sessions over 2 wk | Unspecified |
| Orman (2003) | Level 4 | N = 8 saxophone students | Music instructor | VFX-3D HMD (Forte Technologies, Rochester, NY) | Music performance venues: practice room, classroom with a student audience, room with music faculty members, and room with the director of bands | 12 weekly, 15- to 20-min sessions | Between 3 and 4 hr |
| Orman (2004) | Level 4 | N = 3 saxophone students | Music instructor | VFX-3D HMD (Forte Technologies, Rochester, NY) | Music performance venues: practice room, classroom with a student audience, room with music faculty members, and room with the director of bands; nature setting | 2 sessions, unspecified duration | Unspecified |
| Pertaub et al. (2001) | Level 3 |
N = 16 participants n = 8 participants with public speaking phobia n = 8 confident public speakers |
Unspecified | VR8 HMD (Virtual Research Systems, Aptos, CA) used with electromagnetic tracking (Polhemus, Colchester, VT) | Public speaking to either an empty room or to animated avatars displaying neutral behaviors | 1 immersion lasting 5 min | 5 min |
| Stupar-Rutenfrans et al. (2017) | Level 4 | N = 35 students with moderate to high anxiety of public speaking | Self-guided | Unspecified HMD | Empty hall, small audience, large audience | 3 sessions with 5-min videos (repeated 3–4 times each) | Approximately 1 hr |
Note. CAVE = cave automatic virtual environment; HMD = head-mounted display; HMD-VR = virtual reality in head-mounted displays; PTSD = posttraumatic stress disorder; VE = virtual environment; VR = virtual reality; VRET = virtual reality exposure therapy.
Footnotes
Indicates studies included in the scoping review.
References
- *Abdullah, M., & Shaikh, Z. A. (2018). An effective virtual reality based remedy for acrophobia. International Journal of Advanced Computer Science and Applications , 9, 162–167. 10.14569/IJACSA.2018.090623 [DOI] [Google Scholar]
- American Occupational Therapy Association. (2016). Occupational therapy’s role in mental health recovery. https://www.aota.org/About-Occupational-Therapy/Professionals/MH/mental-health-recovery.aspx
- American Occupational Therapy Association. (2018). AOTA’s societal statement on stress, trauma, and posttraumatic stress disorder. American Journal of Occupational Therapy , 72(Suppl. 2), 7212410080. 10.5014/ajot.2018.72S208 [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association. (2020). Occupational therapy practice framework: Domain and process (4th ed.). American Journal of Occupational Therapy , 74(Suppl. 2), 7412410010. 10.5014/ajot.2020.74S2001 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. 10.1176/appi.books.9780890425596.dsm05 [DOI] [Google Scholar]
- American Psychological Association, Society of Clinical Psychology. (2017). What is exposure therapy? [Clinical practice guideline]. https://apa.org/ptsd-guideline/patients-and-families/exposure-therapy.pdf
- Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology , 8, 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Bandelow, B., & Michaelis, S. (2015). Epidemiology of anxiety disorders in the 21st century. Dialogues in Clinical Neuroscience , 17, 327–335. 10.31887/DCNS.2015.17.3/bbandelow [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botella, C., Fernández-Álvarez, J., Guillén, V., García-Palacios, A., & Baños, R. (2017). Recent progress in virtual reality exposure therapy for phobias: A systematic review. Current Psychiatry Reports , 19, 42. 10.1007/s11920-017-0788-4 [DOI] [PubMed] [Google Scholar]
- *Bouchard, S., St-Jacques, J., Robillard, G., & Renaud, P. (2008). Anxiety increases the feeling of presence in virtual reality. Presence , 17, 376–391. 10.1162/pres.17.4.376 [DOI] [Google Scholar]
- Brady, K. T., Killeen, T. K., Brewerton, T., & Lucerini, S. (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. Journal of Clinical Psychiatry , 61(Suppl. 7), 22–32. [PubMed] [Google Scholar]
- *Cárdenas-López, G., & Rosa-Gómez, A. (2011). Post-traumatic stress disorder treatment with virtual reality exposure for criminal violence: A case study in assault with violence. International Journal on Disability and Human Development , 10, 379–383. 10.1515/IJDHD.2011.061 [DOI] [Google Scholar]
- *Choi, Y. H., Jang, D. P., Ku, J. H., Shin, M. B., & Kim, S. I. (2001). Short-term treatment of acrophobia with virtual reality therapy (VRT): A case report. CyberPsychology and Behavior , 4, 349–354. 10.1089/109493101300210240 [DOI] [PubMed] [Google Scholar]
- Cook, B. L., Doksum, T., Chen, C. N., Carle, A., & Alegría, M. (2013). The role of provider supply and organization in reducing racial/ethnic disparities in mental health care in the U.S. Social Science and Medicine , 84, 102–109. 10.1016/j.socscimed.2013.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, J. (2011). Anxiety disorders. In Brown C. & Stoffel V. C. (Eds.), Occupational therapy in mental health: A vision for participation (pp. 167–178). F. A. Davis. [Google Scholar]
- *Donker, T., Cornelisz, I., van Klaveren, C., van Straten, A., Carlbring, P., Cuijpers, P., & van Gelder, J. L. (2019). Effectiveness of self-guided app-based virtual reality cognitive behavior therapy for acrophobia: A randomized clinical trial. JAMA Psychiatry , 76, 682–690. 10.1001/jamapsychiatry.2019.0219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgelow, M. M., MacPherson, M. M., Arnaly, F., Tam-Seto, L., & Cramm, H. A. (2019). Occupational therapy and posttraumatic stress disorder: A scoping review. Canadian Journal of Occupational Therapy , 86, 148–157. 10.1177/0008417419831438 [DOI] [PubMed] [Google Scholar]
- Exley, S. M., Thompson, C. A., & Hays, C. A. (2011). State hospitals. In Brown C. & Stoffel V. C. (Eds.), Occupational therapy in mental health: A vision for participation (pp. 546–558). F. A. Davis. [Google Scholar]
- *Gromer, D., Reinke, M., Christner, I., & Pauli, P. (2019). Causal interactive links between presence and fear in virtual reality height exposure. Frontiers in Psychology , 10, 141. 10.3389/fpsyg.2019.00141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Gujjar, K. R., van Wijk, A., Kumar, R., & de Jongh, A. (2019). Efficacy of virtual reality exposure therapy for the treatment of dental phobia in adults: A randomized controlled trial. Journal of Anxiety Disorders , 62, 100–108. 10.1016/j.janxdis.2018.12.001 [DOI] [PubMed] [Google Scholar]
- *Hong, Y. J., Kim, H. E., Jung, Y. H., Kyeong, S., & Kim, J. J. (2017). Usefulness of the mobile virtual reality self-training for overcoming a fear of heights. Cyberpsychology, Behavior, and Social Networking , 20, 753–761. 10.1089/cyber.2017.0085 [DOI] [PubMed] [Google Scholar]
- *Juan, M. C., & Pérez, D. (2009). Comparison of the levels of presence and anxiety in an acrophobic environment viewed via HMD or CAVE. Presence , 18, 232–248. 10.1162/pres.18.3.232 [DOI] [Google Scholar]
- *Kahlon, S., Lindner, P., & Nordgreen, T. (2019). Virtual reality exposure therapy for adolescents with fear of public speaking: A non-randomized feasibility and pilot study. Child and Adolescent Psychiatry and Mental Health , 13, 47. 10.1186/s13034-019-0307-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapfhammer, H. P., Huppert, D., Grill, E., Fitz, W., & Brandt, T. (2015). Visual height intolerance and acrophobia: Clinical characteristics and comorbidity patterns. European Archives of Psychiatry and Clinical Neuroscience , 265, 375–385. 10.1007/s00406-014-0548-y [DOI] [PubMed] [Google Scholar]
- *Kim, H., Hong, Y., Kim, M., Jung, Y., Kyeong, S., & Kim, J. (2017). Effectiveness of self-training using the mobile-based virtual reality program in patients with social anxiety disorder. Computers in Human Behavior , 73, 614–619. 10.1016/j.chb.2017.04.017 [DOI] [Google Scholar]
- *Krijn, M., Emmelkamp, P. M., Biemond, R., de Wilde de Ligny, C., Schuemie, M. J., & van der Mast, C. A. (2004). Treatment of acrophobia in virtual reality: The role of immersion and presence. Behaviour Research and Therapy , 42, 229–239. 10.1016/S0005-7967(03)00139-6 [DOI] [PubMed] [Google Scholar]
- *Malbos, E., Mestre, D. R., Note, I. D., & Gellato, C. (2008). Virtual reality and claustrophobia: Multiple components therapy involving game editor virtual environments exposure. CyberPsychology and Behavior , 11, 695–697. 10.1089/cpb.2007.0246 [DOI] [PubMed] [Google Scholar]
- *Malbos, E., Rapee, R. M., & Kavakli, M. (2013). Creation of interactive virtual environments for exposure therapy through game-level editors: Comparison and tests on presence and anxiety. International Journal of Human–Computer Interaction , 29, 827–837. 10.1080/10447318.2013.796438 [DOI] [Google Scholar]
- *McLay, R. N., Wood, D. P., Webb-Murphy, J. A., Spira, J. L., Wiederhold, M. D., Pyne, J. M., & Wiederhold, B. K. (2011). A randomized, controlled trial of virtual reality–graded exposure therapy for post-traumatic stress disorder in active duty service members with combat-related post-traumatic stress disorder. Cyberpsychology, Behavior, and Social Networking , 14, 223–229. 10.1089/cyber.2011.0003 [DOI] [PubMed] [Google Scholar]
- Melnyk, B. M., & Fineout-Overholt, E. (2005). Evidence-based practice in nursing and healthcare: A guide to best practice. Lippincott Williams & Wilkins. [Google Scholar]
- Meyerbröker, K., & Emmelkamp, P. M. G. (2010). Virtual reality exposure therapy in anxiety disorders: A systematic review of process-and-outcome studies. Depression and Anxiety , 27, 933–944. 10.1002/da.20734 [DOI] [PubMed] [Google Scholar]
- *Miloff, A., Lindner, P., Dafgård, P., Deak, S., Garke, M., Hamilton, W., & Carlbring, P. (2019). Automated virtual reality exposure therapy for spider phobia vs. in-vivo one-session treatment: A randomized non-inferiority trial. Behaviour Research and Therapy , 118, 130–140. 10.1016/j.brat.2019.04.004 [DOI] [PubMed] [Google Scholar]
- *Minns, S., Levihn-Coon, A., Carl, E., Smits, J. A. J., Miller, W., Howard, D., & Powers, M. B. (2018). Immersive 3D exposure-based treatment for spider fear: A randomized controlled trial. Journal of Anxiety Disorders , 58, 1–7. 10.1016/j.janxdis.2018.05.006 [DOI] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G.; PRISMA Group. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Medicine , 6(7), e1000097. 10.1371/journal.pmed1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morina, N., Ijntema, H., Meyerbröker, K., & Emmelkamp, P. M. G. (2015). Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behaviour Research and Therapy , 74, 18–24. 10.1016/j.brat.2015.08.010 [DOI] [PubMed] [Google Scholar]
- Motraghi, T. E., Seim, R. W., Meyer, E. C., & Morissette, S. B. (2014). Virtual reality exposure therapy for the treatment of posttraumatic stress disorder: A methodological review using CONSORT guidelines. Journal of Clinical Psychology , 70, 197–208. 10.1002/jclp.22051 [DOI] [PubMed] [Google Scholar]
- *Mühlberger, A., Wiedemann, G., & Pauli, P. (2005). Subjective and physiologic reactions of flight phobics during VR exposure and treatment outcome: What adds motion simulation? Annual Review of Cybertherapy and Telemedicine , 3, 185–192. [Google Scholar]
- *Orman, E. K. (2003). Effect of virtual reality graded exposure on heart rate and self-reported anxiety levels of performing saxophonists. Journal of Research in Music Education , 51, 302–315. 10.2307/3345657 [DOI] [Google Scholar]
- *Orman, E. K. (2004). Effect of virtual reality graded exposure on anxiety levels of performing musicians: A case study. Journal of Music Therapy , 41, 70–78. 10.1093/jmt/41.1.70 [DOI] [PubMed] [Google Scholar]
- *Peperkorn, H. M., Diemer, J. E., Alpers, G. W., & Mühlberger, A. (2016). Representation of patients’ hand modulates fear reactions of patients with spider phobia in virtual reality. Frontiers in Psychology , 7, 268. 10.3389/fpsyg.2016.00268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pérez-Ara, M. A., Quero, S., Botella, C., Baños, R., Andreu-Mateu, S., García-Palacios, A., & Bretón-López, J. (2010). Virtual reality interoceptive exposure for the treatment of panic disorder and agoraphobia. Studies in Health Technology and Informatics , 154, 77–81. [PubMed] [Google Scholar]
- *Pertaub, D. P., Slater, M., & Barker, C. (2001). An experiment on fear of public speaking in virtual reality. Studies in Health Technology and Informatics , 81, 372–378. [PubMed] [Google Scholar]
- Phillips, M. E., Bruehl, S., & Harden, R. N. (1997). Work-related post-traumatic stress disorder: Use of exposure therapy in work-simulation activities. American Journal of Occupational Therapy , 51, 696–700. 10.5014/ajot.51.8.696 [DOI] [PubMed] [Google Scholar]
- *Rahani, V. K., Vard, A., & Najafi, M. (2018). Claustrophobia game: Design and development of a new virtual reality game for treatment of claustrophobia. Journal of Medical Signals and Sensors , 8, 231–237. 10.4103/jmss.JMSS_27_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rothbaum, B. O., Hodges, L. F., Ready, D., Graap, K., & Alarcon, R. D. (2001). Virtual reality exposure therapy for Vietnam veterans with posttraumatic stress disorder. Journal of Clinical Psychiatry , 62, 617–622. 10.4088/JCP.v62n0808 [DOI] [PubMed] [Google Scholar]
- *Schäfer, P., Koller, M., Diemer, J., & Meixner, G. (2015). Development and evaluation of a virtual reality-system with integrated tracking of extremities under the aspect of acrophobia. In Proceedings of the 2015 SAI Intelligent Systems Conference (pp. 408–417). IEEE. 10.1109/IntelliSys.2015.7361173 [DOI] [Google Scholar]
- Slater, M., & Sanchez-Vives, M. (2016). Enhancing our lives with immersive virtual reality. Frontiers in Robotics and AI , 3, 74. 10.3389/frobt.2016.00074 [DOI] [Google Scholar]
- *Stupar-Rutenfrans, S., Ketelaars, L. E. H., & van Gisbergen, M. S. (2017). Beat the fear of public speaking: Mobile 360° video virtual reality exposure training in home environment reduces public speaking anxiety. Cyberpsychology, Behavior, and Social Networking , 20, 624–633. 10.1089/cyber.2017.0174 [DOI] [PubMed] [Google Scholar]
- *Walshe, D. G., Lewis, E. J., Kim, S. I., O’Sullivan, K., & Wiederhold, B. K. (2003). Exploring the use of computer games and virtual reality in exposure therapy for fear of driving following a motor vehicle accident. CyberPsychology and Behavior , 6, 329–334. 10.1089/109493103322011641 [DOI] [PubMed] [Google Scholar]
- Wilson, P. N., Foreman, N., & Stanton, D. (1997). Virtual reality, disability and rehabilitation. Disability and Rehabilitation , 19, 213–220. 10.3109/09638289709166530 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.