Abstract
Background
Oxidative stress is an important factor in the pathomechanism of atherosclerosis. Advanced oxidation protein products (AOPPs) are considered markers of oxidative stress. Thickening of the carotid intima-media layers indicates subclinical atherosclerosis and can be detected by carotid ultrasound.
Objective
Our aim was to examine the association between carotid intima-media thickness (CIMT) and the level of AOPPs.
Methods
Carotid duplex scans and measurements of AOPPs were performed on 476 participants of a cardiovascular population study. The presence of conventional cardiovascular risk factors was investigated with a questionnaire, physical examination, and laboratory tests.
Results
There was a positive correlation between maximum CIMT and the level of AOPPs only in the male population (r = 0.219, p = 0.033). Multivariate analysis has revealed that the association between AOPPs and mean or maximum CIMT was independent of cardiovascular risk factors (OR = 1.458, p = 0.004, and OR = 2.038, p < 0.001).
Conclusions
Among males, the elevated level of AOPPs as a marker of oxidative stress may signal the existence of early atherosclerotic alterations.
Keywords: Carotid intima-media thickness, Advanced oxidation protein products, Oxidative stress
Background
Cardiovascular diseases (CVDs) are the main independent causes of morbidity and mortality worldwide, accounting for over 4 million deaths per year in the European Union [1]. In most cases, CVDs are due to atherosclerosis of the medium- and large-sized arteries [2]. Therefore, early detection of atherosclerosis in a subclinical stage has great importance in personalized risk assessment. The abnormal thickening of the carotid intima-media, which can be precisely measured by carotid ultrasonography, is a commonly accepted marker of subclinical atherosclerosis [3]. Thickening of the carotid intima-media layers is associated with total plaque burden according to histological studies [4]. Epidemiologic studies have shown a positive correlation between classical cardiovascular risk factors [e.g. hypertension [5], diabetes mellitus [6], and hypercholesterolemia [7]] and the abnormal changes of the carotid intima-media thickness (CIMT). A similar association exists between non-classical cardiovascular risk factors (e.g. elevated serum uric acid levels) and the abnormal CIMT [8]. Even the systematic use of CIMT measurement for risk assessment is no longer recommended in daily clinical routine by the current clinical guidelines [9] due to the technical difficulties, correctly performed carotid intima-media thickness measurement is also a known predictor of cardiovascular events and coronary heart disease (CHD) [10].
Atherosclerosis is considered a multifactorial chronic inflammatory disease, and its pathogenesis involves oxidative stress [11, 12]. In vivo, advanced oxidation protein products (AOPPs) are the end-products of a reaction between plasma albumin and chlorinated oxidants, such as hypochlorous acid, and formed through the myeloperoxidase [13]. Nonfunctional proteins contain di-tyrosine cross-links [14]. Once AOPPs are formed, they can lead to tissue damage as a result of an imbalance between the antioxidant and pro-oxidant levels and to the accumulation of reactive oxygen species (ROS), which are strong oxidizing agents.
Detection of AOPPs is usually a consequence of the aforementioned impaired balance of the redox homeostasis. As the measurement of ROS is difficult due to their diverse form and short half-life, AOPPs as biomarkers of oxidation-mediated protein damage can be used as reliable indicators reflecting oxidative stress status [15]. The association between AOPPs as oxidative stress markers and atherosclerosis has been already investigated, and it was shown that atherogenic risk is elevated in AOPPs-treated mice [16]. However, whether the association exists independently of conventional risk factors in an asymptomatic population is not known. Our aim was to examine oxidative stress status according to the level of AOPPs and its association with CIMT as a marker of subclinical atherosclerosis in a cross-sectional study.
Materials and methods
Participant selection
Budakalász Health Examination Survey, a cross-sectional voluntary cardiovascular screening program targeting the adult population (> 20 years, around 8000 inhabitants) of a Central-Hungarian town (Budakalász) was performed in 2011–2013 [17]. Medical history with special attention to CVD-related signs and symptoms, lifestyle, and family history were recorded by an experienced physician. Anthropometric parameters (height, weight) rounded to the nearest 0.1 cm and 0.1 kg were measured in the standing position while participants were wearing light indoor clothing without shoes.
Routine laboratory tests were performed in our Institution’s Central Laboratory with rigorous quality control. The concentration of lipid fractions was measured by using a colorimetric assay (Roche Diagnostics Ltd., Mannheim, Germany).
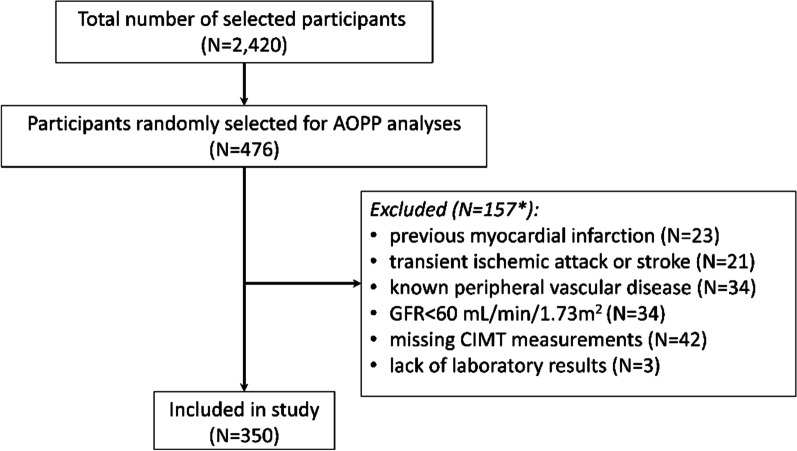
The participation rate in the Budakalász Health Examination Survey was around 30% (N = 2420) of the eligible total population. Measurement of AOPPs was performed in 476 participants selected randomly. Participants with the following cardiovascular history were excluded from further analysis: 23 participants (4.8%) with previous myocardial infarction, 21 participants (4.4%) with transient ischemic attack or stroke, 34 participants (7.1%) with known peripheral vascular disease, and 34 participants (7.1%) with glomerular filtration rate (GFR) < 60 mL/min/1.73 m2. Three participants (0.6%) due to the lack of laboratory results and 42 participants (8.7%) due to the missing CIMT measurements were also excluded (Fig. 1). As a participant could have more than one exclusion criterion, overall 350 participants were included in the study.
Fig. 1.
Flow chart of participant selection. *A total of 31 participants fulfilled 2 or more exclusion criteria
Advanced oxidation protein products measurement
Blood samples were drawn in ethylenediaminetetraacetic acid (EDTA) treated tubes and then subjected to centrifugation. Plasma samples were stored at − 80 °C until the determination of AOPPs. Analysis of the unknown levels of AOPPs in the plasma samples was based on a spectrophotometric detection according to Witko-Sarsat et al. [18] and Taylor et al. [19]. The principle of the assay is a colorimetric reaction between plasma proteins and chlorinated oxidants (e.g. chloramine-T). All assays were carried out on triplicates. First, plasma samples were diluted 1:10 in phosphate-buffered saline (PBS), then 300 µL of the diluted plasma samples were added to each well of the microtiter plate (Sarstedt AG & Co. KG, Nümbrecht, Germany). For optimal accuracy, Chloramine-T hydrate (Sigma Ltd. St. Louis, MO, USA) standard solutions (300 µL; 0–100 µM) were also placed in the same plate and PBS served as a sample blank. Fifteen micro litter 1.16 M potassium iodide (KI; Sigma Ltd. St. Louis, MO, USA) was added to all wells, followed by incubation at room temperature for 2 min. After all, 30 µL glacial acetic acid (Sigma Ltd. St. Louis, MO, USA) was also added to all wells. Prior to reading the absorbance at 340 nm, plates were centrifuged at 5800 g for 5 min, and 230 µL precipitated-protein-free supernatant was transferred to a new 96-well microplate (Sarstedt AG & Co. KG, Nümbrecht, Germany). In all cases, the absorbance of the sample blank was subtracted from the sample wells before further analysis. The calculated chloramine-T equivalent concentrations of AOPPs were normalized to the total protein of each patient and expressed in µM/g protein.
Diagnostic criteria and clinical definitions
Medical history was regarded as positive for hypertension and hyperlipidemia if documented. The following cut-off points were used: > 140 mmHg systolic and/or > 90 mmHg diastolic for elevated blood pressure, and 5.2 mmol/L for total cholesterol, 3.4 mmol/L for low-density lipoprotein cholesterol (LDL-C), 1.7 mmol/L for triglyceride, and 1.1 mmol/L or below (females) and 0.9 mmol/L or below (males) for high-density lipoprotein cholesterol (HDL-C). Current and former regular smokers, who quit smoking at least one year before and smoke regularly at least for one year were both considered smokers. Body mass index (BMI) was calculated using the Quetelet's form.
Carotid intima-media thickness measurements
High-quality, B-mode longitudinal ultrasonography images (VIVID I, GE Healthcare, Wauwatosa, USA) of the common carotid artery (CCA) were acquired at end-diastole on both sides. Following the concepts of the 2012 Mannheim Consensus [20], a 10 mm length of a straight arterial segment without plaques was marked out on the far wall of the CCA at least 5 mm below the bifurcation for intima-media thickness measurement. All markings were performed by the same person. Then, a semiautomatic software (GE EchoPAC BT11, GE Healthcare, Wauwatosa, USA) calculated and recorded the maximum and mean values of CIMT. The maximum value was used for analysis, and the values of the left and right sides were averaged.
Statistical analysis
SPSS for Windows, version 25.0 (IBM, Armonk, NY, USA) was used for statistical analyses. A post hoc power analysis was conducted using an online calculator developed by MGH Biostatistics Center. The sample size of 350 was used for the statistical power analyses. The significance level used for this analysis was p < 0.05. The standard deviation of the dependent variable (maximal CIMT) was 0.16, the standard deviation of the independent variable (AOPP) was 0.08, the minimal detectable difference entered was 0.36. The post hoc analyses revealed that the probability is 91% that the study detects a relationship between the independent and the dependent variables. Distribution of AOPP in the population was tested by the Kolmogorov–Smirnov test and showed normal distribution (p = 0.065). Continuous variables were expressed as means with standard deviation (SD) or medians with interquartile ranges (IQRs) as appropriate, depending on the distribution of the values, whereas categorical variables were expressed as numbers (percentages). Comparisons of means, medians, and proportions were performed with Student’s t test, Mann–Whitney U-test, and Chi-square test, respectively. Spearman’s linear correlation was used to test the association between AOPPs and CIMT. Generalized linear model (GLZ) analysis was performed to screen the significant predictor risk factors adjusted for age, and gender. All analyses were two-tailed, and p < 0.05 was considered significant.
Results
Patient characteristics
Overall, 350 participants were included in the final analysis. The baseline clinical characteristics of the 350 participants are shown in Table 1.
Table 1.
Baseline clinical characteristics
| Characteristics | All participants | Female (N = 205) | Male (N = 145) | p value |
|---|---|---|---|---|
| Age (years), mean (SD) | 59.33 (10.31) | 60.86 (9.86) | 57.51 (10.85) | 0.016* |
| LDL-C (mmol/L), mean (SD) | 3.51 (0.99) | 3.47 (0.96) | 3.55 (1.05) | 0.57 |
| HDL-C (mmol/L), mean (SD) | 1.53 (0.48) | 1.65 (0.47) | 1.33 (0.39) | < 0.001* |
| Triglycerides (mmol/L), mean (SD) | 2.41 (1.41) | 2.28 (1.45) | 2.66 (1.58) | 0.064 |
| Cholesterol (mmol/L), mean (SD) | 5.81 (1.1) | 5.84 (1.05) | 5.75 (1.16) | 0.54 |
| HbA1c (%), mean (SD) | 5.76 (0.53) | 5.79 (0.49) | 5.72 (0.57) | 0.367 |
| BMI (kg/m2), mean (SD) | 28.78 (5.42) | 28.84 (6.03) | 28.54 (4.34) | 0.681 |
| Hypertension, N (%) | 122 (33.9) | 67 (50.8) | 55 (57.9) | 0.345 |
| DM, N (%) | 22 (6.3) | 10 (7.6) | 12 (12.6) | 0.265 |
| Smoking, N (%) | 21 (6) | 10 (7.6) | 11 (11.6) | 0.356 |
| Dyslipidemia, N (%) | 100 (28.5) | 62 (47) | 38 (40) | 0.343 |
| Creatinine (µmol/L), mean (SD) | 75.98 (18.33) | 75.43 (15.93) | 76.81 (18.87) | 0.555 |
| Serum uric acid (mg/dL), mean (SD) | 324.53 (77.69) | 303.89 (67.55) | 357.55 (82.69) | < 0.001* |
| Beta-blockers, N (%) | 52 (14.9) | 34 (25.8) | 18 (18.9) | 0.264 |
| ASA, N (%) | 23 (6.6) | 11 (8.3) | 12 (12.6) | 0.373 |
| ARB, N (%) | 35 (10) | 14 (10.6) | 21 (22.1) | 0.025* |
| ACEI, N (%) | 98 (28) | 59 (28.8) | 39 (36.9) | 0.719 |
| Diuretics#, N (%) | 15 (4.3) | 7 (5.3) | 8 (8.4) | 0.421 |
| Lipid-lowering medications#, N (%) | 46 (13.1) | 26 (19.7) | 20 (21.1) | 0.868 |
| Antidiabetics#, N (%) | 27 (7.7) | 17 (10.2) | 15 (13.6) | 0.434 |
| Normalized AOPPs (µM/g) mean (SD) | 0.36 (0.08) | 0.36 (0.07) | 0.38 (0.07) | 0.044* |
| Normalized AOPPs (µM/g) median (IQR) | 0.36 (0.12) | 0.35 (0.12) | 0.38 (0.12) | 0.33 |
| Maximal CIMT (mm), median (IQR) | 0.8 (0.22) | 0.8 (0.22) | 0.8 (0.24) | 0.839 |
| Maximal CIMT (mm), mean (SD) | 0.83 (0.168) | 0.83 (0.16) | 0.83 (0.17) | 0.857 |
| Mean CIMT (mm), mean (SD) | 0.68 (0.12) | 0.68 (0.12) | 0.68 (0.13) | 0.713 |
| Mean CIMT (mm), median (IQR) | 0.68 (0.15) | 0.68 (0.16) | 0.65 (01) | 0.616 |
| Carotid plaque, N (%) | 78 (22.3%) | 45 (22) | 33 (22.5) | 0.897 |
Mean ± SD or median (IQR) represented the continuous variables, and numbers (proportions) the categorical variables. Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; AOPP, advanced oxidation protein products; ARB, angiotensin receptor blockers; ASA, acetylsalicylic acid; BMI, body mass index; CIMT, carotid intima-media thickness; DM, diabetes mellitus; HbA1c, hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; IQR, interquartile range; LDL-C, low-density lipoprotein cholesterol; SD, standard deviation; #oral antidiabetics, *significant values
The mean age of the participants was 59.33–0.31 years. Fifty-seven point 5% were males, all patients belonged to the Caucasian race. The characteristics of female and male patients were compared (Table 1). We found, that there was no significant difference in terms of the general cardiovascular risk factors, except for HDL-C and serum uric acid. Males had lower HDL-C (1.65 vs. 1.33, p < 0.001) and higher serum uric acid levels (303.89 vs. 357.55, p < 0.001), although the females were significantly older than the males (60.86 vs. 57.51, p = 0.016). History of dyslipidemia and diabetes mellitus, as well as serum LDL-C, triglyceride, cholesterol levels did not significantly differ between the two groups. A list of chronic medications is also shown in Table 1. Of all patients studied, the three most common medications were angiotensin-converting enzyme inhibitor (ACEI) (28%), beta-blockers (14.9%) and lipid-lowering medications (13.1%). There was a significant difference found between the groups regarding the angiotensin receptor blockers (ARB) (10.6% vs. 22.1%, p = 0.025) therapy they were receiving.
The mean level of the normalized AOPPs was 0.36 µMg ± 0.07 in females, and it was significantly increased in male participants (0.38 µMg ± 0.07; p = 0.044). Further analysis showed that there was no statistically significant difference in the CIMT values between the two groups.
Correlation of AOPP with risk factors
In the whole population, we observed a significant negative correlation between the value of the normalized mean AOPP with HDL-C (r = − 0.232, p < 0.001) (Table 2) and positive correlation between normalized mean AOPP and LDL-C (r = 0.162, p < 0.016). While this trend existed in females (HDL-C: r = − 0.235, p = 0.007; LDL-C (r = 0.162, p = 0.038), in males only correlation of HDL-C and mean AOPP was noticed (HDL-C: r = − 0.202, p = 0.049). Moreover, BMI correlated positively with normalized mean AOPP (r = − 0.209, p = 0.042) only in males. Maximum CIMT and mean plasma level of AOPPs showed a significant positive correlation (r = 0.184, p = 0.006) in the total study population (Table 2). This tendency could also be recognized in males (r = 0.219, p = 0.033), but not in females. In contrast, there was no significant correlation between AOPP and mean CIMT in the univariate analysis.
Table 2.
Correlation of normalized mean AOPP level with risk factors
| Parameter | All participants | Female | Male | |||
|---|---|---|---|---|---|---|
| Correlation coefficient (r) | p value | Correlation coefficient (r) | p value | Correlation coefficient (r) | p value | |
| Age | 0.025 | 0.705 | 0.081 | 0.354 | − 0.003 | 0.974 |
| BMI | − 0.105 | 0.114 | − 0.043 | 0.628 | − 0.209 | 0.042* |
| HDL-C | − 0.232 | < 0.001* | − 0.235 | 0.007* | − 0.202 | 0.049* |
| LDL-C | 0.162 | 0.016* | 0.183 | 0.038* | 0.107 | 0.313 |
| HbA1c | − 0.083 | 0.217 | − 0.069 | 0.438 | − 0.057 | 0.587 |
| Serum creatinine | 0.035 | 0.596 | 0.012 | 0.890 | 0.067 | 0.587 |
| Serum uric acid | 0.078 | 0.242 | 0.104 | 0.237 | − 0.05 | 0.623 |
| Maximum CIMT | 0.184 | 0.006* | 0.166 | 0.058 | 0.219 | 0.033* |
| Mean CIMT | 0.086 | 0.195 | 0.084 | 0.340 | 0.101 | 0.328 |
AOPPs, Advanced oxidation protein products; BMI, body mass index; CIMT carotid intima-media thickness; HbA1c, hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; p and r values are for Spearman’s correlation; *significant values
Multivariate analysis
Generalized linear model analysis of mean and maximum CIMT was performed with adjustment for age and AOPPs. In this model AOPPs were significantly associated with both mean and maximal CIMT in males (OR = 1.92, p = 0.02 and OR = 1.68, p = 0.001; respectively) but not in females.
Further adjustments have been performed for known cardiovascular risk factors such as smoking status, hypertension, dyslipidemia, diabetes mellitus, HDL-C level, LDL-C level, HbA1c level and for ARB therapy (Tables 3 and 4). Multivariate analysis revealed that age was significantly associated with mean and maximum CIMT in the total study population, regardless the gender. The level of AOPP was significantly associated with mean and maximum CIMT in males (OR = 1.458, p = 0.004; OR = 2.038, p < 0.001, respectively) only. (Tables 3 and 4).
Table 3.
Multivariate analysis of risk factors related to mean CIMT
| Mean CIMT | Females | Males | ||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | OR | p value | 95% CI | OR | p value | 95% CI | ||
| Lower | Upper | Lower | Upper | |||||
| Age | 1.006 | < 0.001* | 1.182 | 2.144 | 1.008 | < 0.001* | 1.006 | 1.011 |
| AOPPs | 0.980 | 0.879 | 0.753 | 1.274 | 1.458 | 0.004* | 1.125 | 1.889 |
| Smoker | 1.041 | 0.136 | 0.987 | 1.098 | 1.036 | 0.191 | 0.982 | 1.093 |
| Hypertension | 1.029 | 0.168 | 0.988 | 1.071 | 0.976 | 0.370 | 0.925 | 1.03 |
| Dyslipidemia | 0.998 | 0.907 | 0.960 | 1.036 | 0.936 | 0.001* | 0.901 | 0.972 |
| Diabetes | 1.014 | 0.656 | 0.952 | 1.081 | 1.035 | 0.293 | 0.971 | 1.104 |
| BMI | 0.999 | 0.371 | 0.996 | 1.002 | 1.005 | 0.079 | 0.999 | 1.01 |
| HDL-C | 0.973 | 0.183 | 0.934 | 1.013 | 1.007 | 0.752 | 0.964 | 1.052 |
| LDL-C | 0.944 | 0.492 | 0.975 | 1.012 | 1.018 | 0.049* | 1.001 | 1.035 |
| HbA1c | 0.944 | 0.257 | 0.953 | 1.036 | 1.032 | 0.079 | 0.996 | 1.069 |
| ARB therapy | 0.956 | 0.257 | 0.885 | 1.033 | 0.967 | 0.164 | 0.922 | 1.015 |
AOPPs, Advanced oxidation protein products; ARB, angiotensin receptor blockers; BMI, body mass index; HbA1c, hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; *significant values
Table 4.
Multivariate analysis of risk factors related to maximum CIMT
| Maximum CIMT | Females | Males | ||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | OR | p value | 95% CI | OR | p value | 95% CI | ||
| Lower | Upper | Lower | Upper | |||||
| Age | 1.008 | < 0.001* | 1.32 | 2.68 | 1.009 | < 0.001* | 1.006 | 1.013 |
| AOPPs | 1.184 | 0.347 | 0.833 | 1.683 | 2.038 | < 0.001* | 1.441 | 2.883 |
| Smoker | 1.034 | 0.3 | 0.97 | 1.102 | 1.013 | 0.714 | 0.944 | 1.088 |
| Hypertension | 1.019 | 0.505 | 0.964 | 1.078 | 0.988 | 0.759 | 0.918 | 1.088 |
| Dyslipidemia | 0.972 | 0.288 | 0.921 | 1.025 | 0.927 | 0.004* | 0.88 | 0.976 |
| Diabetes | 1.043 | 0.307 | 0.962 | 1.13 | 1.081 | 0.036* | 1.005 | 1.162 |
| BMI | 1 | 0.935 | 0.995 | 1.004 | 1.008 | 0.021* | 1.001 | 1.015 |
| HDL-C | 0.957 | 0.124 | 0.906 | 1.012 | 1.002 | 0.413 | 0.970 | 1.078 |
| LDL-C | 0.987 | 0.268 | 0.963 | 1.011 | 1.034 | 0.003* | 1.011 | 1.057 |
| HbA1c | 0.958 | 0.089 | 0.911 | 1.007 | 1.038 | 0.134 | 0.989 | 1.089 |
| ARB therapy | 0.949 | 0.322 | 0.855 | 1.053 | 0.953 | 0.166 | 0.890 | 1.02 |
We have performed a multivariate analysis with carotid plaque as a dependent variable adjusted for age and AOPPs for both genders. In these models, AOPPs were not significantly associated with carotid atherosclerosis
Discussion
In this study, we presented an independent association of AOPPs with mean or maximum CIMT in males in an asymptomatic Caucasian population. In logistic regression analyses, AOPPs were independent predictors and showed significantly increased odds (OR = 1.458 and OR = 2.038) for the presence of higher mean and maximal CIMT values in males but not in females.
Ultrasound measurement of carotid intima-media thickness is a valuable tool to assess the vascular status, as the abnormal CIMT value is a known biomarker of subclinical atherosclerosis. Although in the literature there is no general definition of abnormal CIMT, it has been indicated that mean CIMT above 0.9 mm correlates with atherosclerosis [21], traditional cardiovascular risk factors [22–24] as well as increased prevalence and incidence of CVD [22]. The analysis of mean and maximum CIMT in our study did not confirm any significant gender differences in carotid intima-media thickness between females and males.
The level of AOPPs measured in our study population was similar to the results of other population-based studies, including clinically healthy participants [25]. We found that there was a significantly higher level of normalized AOPPs in male participants compared to females (0.38 vs. 0.36, p = 0.044) this result is in line with other studies [26]. The level of AOPP significantly correlated with maximum CIMT (r = 0.184, p = 0.006) in the whole population. Analyzing this correlation by gender revealed that AOPP and maximal CIMT correlated in the male population (r = 0.219 p = 0.033), but this could not be observed in females. In contrast, no significant correlation was detected related to mean CIMT in the univariate analysis.
The association between CIMT and other markers of oxidative stress was investigated in various studies. Ashfaq et al. revealed that glutathione redox state, an in vivo measure of intracellular oxidative stress, correlated with mean CIMT in a healthy population [27]. Yagi et al. found that biological antioxidant potential negatively correlated with CIMT, which suggests a positive association of oxidative stress with CIMT [28]. In a pilot study, Seyedsadjadi et al. showed that a comprehensive redox balance lifestyle score was significantly associated with the risk for increased CIMT [29].
After multivariate adjustment for cardiovascular risk factors, age was a weak, but independent predictor for both mean and maximum CIMT in females and males. In the male population, both mean and maximum CIMT correlated with AOPPs (OR = 1.458, p = 0.004 and OR = 2.038, p < 0.001, respectively) as further variables, such as LDL-C level and dyslipidemia but not in females.
It is generally accepted that there are gender differences in cardiovascular diseases. Female gender is associated with lower prevalence of CVD [30] and cardiovascular diseases tend to develop later in women than in men [31] and this is known to be associated with the protective antioxidant effects of female hormones [32]. AOPP levels seem to be associated with gender according to our and other’s results [26].
The level of AOPPs reflects the oxidative stress state in the extracellular space. Oxidative stress may lead to atherosclerosis through several mechanisms. Reactive oxygen species overproduction can cause impaired nitric oxide synthesis, and the function is associated with endothelial dysfunction that is an important factor in the development of atherosclerosis [33]. Also, AOPPs are transported to the subendothelial space where they enhance oxidative stress and inflammation, thus triggering plaque formation [34]. Surprisingly, in our study no correlation was found between AOPP and carotid plaque formation. An increase in the level of AOPPs has already been reported in several diseases such as uremia [35], diabetes mellitus [36], rheumatoid arthritis [37], and coronary artery disease [38]. In a study by Piwowar et al., the level of AOPPs was elevated in diabetic patients and associated with macroangiopathy in this patient group [39]. Liu et al. reported a causal relationship between chronic accumulation of AOPPs and atherosclerosis in an animal model [40].
According to the results of Sanchez et al., the level of AOPPs is associated with cardiovascular risk factors such as BMI and lipid profiles in apparently healthy young adults [41]. Previous studies of patients with renal disease demonstrated that AOPPs were reliable markers of the oxidant-mediated protein damage in hypertriglyceridemia, CHD, and atherosclerosis. Kocak et al. investigated the association between CIMT and AOPPs in peritoneal dialyzed (PD) patients and found that the level of AOPPs was higher in PD patients when compared to controls [42]. Also, AOPPs level correlated with CIMT in the PD group. In contrast to our results, they found no association of AOPP and CIMT in non-dialyzed controls. Of note, the population they analyzed was approximately 20 years younger on average than ours and none of the patients were hypertensive, hyperlipidemic or active smokers unlike in our general study population without clinical signs of atherosclerosis but with the presence of risk factors. Despite all this, we have not found other studies that investigated AOPPs in an asymptomatic population of such a sample size as ours.
To the best of our knowledge, this is the first study demonstrating an independent positive association between the plasma level of AOPPs and the value of CIMT in an asymptomatic population and its’s gender difference.
Our study has some limitations. As the participation in the study was on a voluntary basis, there is the possibility that subjects with known hypertension or other factors associated with subclinical atherosclerosis and elevated CIMT had a greater propensity to participate. Secondly, due to the cross-sectional study type, a cause-and-effect relationship cannot be identified. Therefore, we cannot conclude that CIMT increased because of oxidative stress, the namely elevated level of AOPPs.
In conclusion, in a male population without previous cardiovascular events, mean and maximum CIMT were associated with the elevated level of AOPPs.
Conclusion
In this study, we found that the elevated level of AOPPs in the male population may be used as an early marker of atherosclerotic alterations.
Acknowledgements
The authors express their gratitude to Ms Nóra Fekete, Ms Zsófia Szász and Mr Márton Kalabay for their contribution to the success of the work.
Abbreviations
- AOPP
Advanced oxidation protein products
- ARB
Angiotensin receptor blocker
- ASA
Acetylsalicylic acid
- BMI
Body mass index
- CCA
Common carotid artery
- CHD
Coronary heart disease
- CIMT
Carotid intima-media thickness
- CVD
Cardiovascular diseases
- DM
Diabetes mellitus
- EDTA
Ethylenediaminetetraacetic acid
- HbA1c
Hemoglobin A1c
- HDL-C
High-density lipoprotein cholesterol
- GLZ
Generalized linear model
- GFR
Glomerular filtration rate
- LDL-C
Low-density lipoprotein cholesterol
- PD
Peritoneal dialyzed
- ROS
Reactive oxygen species
Authors' contributions
ZsB, AT, LoK, EdD and LaK drafted the manuscript. ZsB and ElD. carried out statistical analysis. ZsB, AT, LaK, OL, EP and BM participated in the design of the study. ZsB, LoK, PS, ZsSz performed the data collection from the patients. AT, EP, OL and LaK performed biochemical measurements. RV and TDN performed the carotid intima-media measurement. All authors read and approved the final manuscript.
Funding
Open Access funding provided by Semmelweis University. This work was supported by the National Research, Development and Innovation Office of Hungary [NVKP-16-1-2016-0017] and by the Development of scientific workshops of medical-, health- and pharmaceutical sciences educations [EFOP-3.6.3-VEKOP-16-2017-00009]. The research was financed by the Higher Education Institutional Excellence Program of the Ministry of Human Capacities in Hungary, within the framework of the Therapeutic Development thematic program of Semmelweis University. The funder had no role in the design of this study; in the collection, analysis, and interpretation of data; or in writing the manuscript.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Hungarian Scientific and Research Ethics Committee of the Medical Research Council (Approval No: 8224-0/2011/EKU [265/PI/11]). All procedures were done following the ethical standards of the responsible committee on human experimentation (institutional and national) and the Helsinki Declaration of 1975, as revised in 2000 [5]. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest regarding the publication of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zsolt Bagyura, Angéla Takács, László Kőhidai and Béla Merkely contributed equally to this work
Contributor Information
Zsolt Bagyura, Email: bagyura@gmail.com.
Angéla Takács, Email: takacs.angela@med.semmelweis-univ.hu, Email: angela.takacs1@gmail.com.
Loretta Kiss, Email: kisslotti@gmail.com.
Edit Dósa, Email: dosa.edit@med.semmelweis-univ.hu.
Réka Vadas, Email: vadasreka@gmail.com.
Tin Dat Nguyen, Email: nguyentindatdat@gmail.com.
Elek Dinya, Email: dinya.elek@public.semmelweis-univ.hu.
Pál Soós, Email: soospal@gmail.com.
Zsolt Szelid, Email: szelid.zsolt@kardio.sote.hu.
Orsolya Láng, Email: langorsi@gmail.com.
Éva Pállinger, Email: eva.pallinger@gmail.com.
László Kőhidai, Email: kohlasz2@gmail.com.
Béla Merkely, Email: merkely.bela@gmail.com.
References
- 1.Townsend N, Nichols M, Scarborough P, Rayner M. Cardiovascular disease in Europe–epidemiological update 2015. Eur Heart J. 2015;36(40):2696–2705. doi: 10.1093/eurheartj/ehv428. [DOI] [PubMed] [Google Scholar]
- 2.Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ Res. 2016;118(4):535–546. doi: 10.1161/CIRCRESAHA.115.307611. [DOI] [PubMed] [Google Scholar]
- 3.Salonen JT, Salonen R. Ultrasound B-mode imaging in observational studies of atherosclerotic progression. Circulation. 1993;87(3):56–65. [PubMed] [Google Scholar]
- 4.Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74(6):1399–1406. doi: 10.1161/01.cir.74.6.1399. [DOI] [PubMed] [Google Scholar]
- 5.Takase H, Sugiura T, Murai S, Yamashita S, Ohte N, Dohi Y. Carotid intima-media thickness is a novel predictor of new onset of hypertension in normotensive subjects. Medicine. 2017;96(31):e7710–1. doi: 10.1097/MD.0000000000007710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang M, Sui J, Wang S, Wang X. Correlations of carotid intima-media thickness with endothelial function and atherosclerosis degree in patients with type 2 diabetes mellitus. Clin Hemorheol Microcirc. 2019;72(4):431–439. doi: 10.3233/CH-180486. [DOI] [PubMed] [Google Scholar]
- 7.Nakagomi A, Shibui T, Kohashi K, Kosugi M, Kusama Y, Atarashi H, et al. Differential effects of atorvastatin and pitavastatin on inflammation, insulin resistance, and the carotid intima-media thickness in patients with dyslipidemia. J Atheroscler Thromb. 2015;22(11):1158–1171. doi: 10.5551/jat.29520. [DOI] [PubMed] [Google Scholar]
- 8.Kiss LZ, Bagyura Z, Csobay-Novak C, Lux A, Polgar L, Jermendy A, et al. Serum uric acid is independently associated with coronary calcification in an asymptomatic population. J Cardiovasc Transl Res. 2019;12(3):204–210. doi: 10.1007/s12265-018-9843-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the european society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European association for cardiovascular prevention and rehabilitation (EACPR) Eur Heart J. 2016;37(29):2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular health study collaborative research group. N Engl J Med. 1999;340(1):14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 11.Schaftenaar F, Frodermann V, Kuiper J, Lutgens E. Atherosclerosis: the interplay between lipids and immune cells. Curr Opin Lipidol. 2016;27(3):209–215. doi: 10.1097/MOL.0000000000000302. [DOI] [PubMed] [Google Scholar]
- 12.Pignatelli P, Menichelli D, Pastori D, Violi F. Oxidative stress and cardiovascular disease: new insights. Kardiol Pol. 2018;76(4):713–722. doi: 10.5603/KP.a2018.0071. [DOI] [PubMed] [Google Scholar]
- 13.Ou H, Huang Z, Mo Z, Xiao J. The characteristics and roles of advanced oxidation protein products in atherosclerosis. Cardiovasc Toxicol. 2017;17(1):1–12. doi: 10.1007/s12012-016-9377-8. [DOI] [PubMed] [Google Scholar]
- 14.Melough MM, Sun X, Chun OK. The role of AOPP in age-related bone loss and the potential benefits of berry anthocyanins. Nutrients. 2017;9(7):789. doi: 10.3390/nu9070789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gryszczynska B, Formanowicz D, Budzyn M, Wanic-Kossowska M, Pawliczak E, Formanowicz P, et al. Advanced oxidation protein products and carbonylated proteins as biomarkers of oxidative stress in selected atherosclerosis-mediated diseases. Biomed Res Int. 2017;2017:4975264. doi: 10.1155/2017/4975264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mo ZC, Xiao J, Tang SL, Ouyang XP, He PP, Lv YC, et al. Advanced oxidation protein products exacerbates lipid accumulation and atherosclerosis through downregulation of ATP-binding cassette transporter A1 and G1 expression in apolipoprotein E knockout mice. Circ J. 2014;78(11):2760–2770. doi: 10.1253/circj.cj-14-0193. [DOI] [PubMed] [Google Scholar]
- 17.Bagyura Z, Kiss L, Edes E, Lux A, Polgar L, Soos P, et al. Cardiovascular screening programme in the central hungarian region the budakalasz study. Orvosi Hetilap. 2014;155(34):1344–52. doi: 10.1556/OH.2014.29969. [DOI] [PubMed] [Google Scholar]
- 18.Witko-Sarsat V, Friedlander M, Capeillere-Blandin C, Nguyen-Khoa T, Nguyen AT, Zingraff J, et al. Advanced oxidation protein products as a novel marker of oxidative stress in uremia. Kidney Int. 1996;49(5):1304–1313. doi: 10.1038/ki.1996.186. [DOI] [PubMed] [Google Scholar]
- 19.Taylor EL, Armstrong KR, Perrett D, Hattersley AT, Winyard PG. Optimisation of an Advanced Oxidation Protein Products Assay: Its Application to Studies of Oxidative Stress in Diabetes Mellitus. Oxidative Med Cell Longev. 2015;2015:496271. doi: 10.1155/2015/496271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012;34(4):290–6. doi: 10.1159/000343145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paul J, Shaw K, Dasgupta S, Ghosh MK. Measurement of intima media thickness of carotid artery by B-mode ultrasound in healthy people of India and Bangladesh, and relation of age and sex with carotid artery intima media thickness: an observational study. J Cardiovasc Dis Res. 2012;3(2):128–131. doi: 10.4103/0975-3583.95367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115(4):459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 23.Yang C, Sun Z, Li Y, Ai J, Sun Q, Tian Y. The correlation between serum lipid profile with carotid intima-media thickness and plaque. BMC Cardiovasc Disord. 2014;14(1):181. doi: 10.1186/1471-2261-14-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ciccone MM, Bilianou E, Balbarini A, Gesualdo M, Ghiadoni L, Metra M, et al. Task force on: 'Early markers of atherosclerosis: influence of age and sex'. J Cardiovasc Med (Hagerstown) 2013;14(10):757–766. doi: 10.2459/JCM.0b013e328362078d. [DOI] [PubMed] [Google Scholar]
- 25.Wybranowski T, Ziomkowska B, Cyrankiewicz M, Kruszewski S. The impact of oxidative stress on binding of drugs with plasma proteins studied by fluorescence anisotropy methods. Gen Physiol Biophys. 2018;37(6):647–655. doi: 10.4149/gpb_2018017. [DOI] [PubMed] [Google Scholar]
- 26.Raberin A, Connes P, Barthélémy JC, Robert P, Celle S, Hupin D, et al. Role of gender and physical activity level on cardiovascular risk factors and biomarkers of oxidative stress in the elderly. Oxid Med Cell Longev. 2020;2020:1315471. doi: 10.1155/2020/1315471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ashfaq S, Abramson JL, Jones DP, Rhodes SD, Weintraub WS, Hooper WC, et al. The relationship between plasma levels of oxidized and reduced thiols and early atherosclerosis in healthy adults. J Am Coll Cardiol. 2006;47(5):1005–1011. doi: 10.1016/j.jacc.2005.09.063. [DOI] [PubMed] [Google Scholar]
- 28.Yagi H, Sumino H, Yoshida K, Aoki T, Tsunekawa K, Araki O, et al. Biological antioxidant potential negatively correlates with carotid artery intima-media thickness. Int Heart J. 2016;57(2):220–225. doi: 10.1536/ihj.15-389. [DOI] [PubMed] [Google Scholar]
- 29.Seyedsadjadi N, Berg J, Bilgin AA, Grant R. A pilot study providing evidence for a relationship between a composite lifestyle score and risk of higher carotid intima-media thickness: is there a link to oxidative stress? Oxid Med Cell Longev. 2018;2018:4504079. doi: 10.1155/2018/4504079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mosca L, Barrett-Connor E, Wenger NK. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation. 2011;124(19):2145–2154. doi: 10.1161/CIRCULATIONAHA.110.968792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010;18(12):598–602. doi: 10.1007/s12471-010-0841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ganatra DA, Johar KS, Parmar TJ, Patel AR, Rajkumar S, Arora AI, et al. Estrogen mediated protection of cytoskeleton against oxidative stress. Indian J Med Res. 2013;137(1):117–124. [PMC free article] [PubMed] [Google Scholar]
- 33.Meza CA, La Favor JD, Kim D-H, Hickner RC. Endothelial dysfunction: is there a hyperglycemia-induced imbalance of NOX and NOS? Int J Mol Sci. 2019;20(15):3775. doi: 10.3390/ijms20153775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo ZJ, Niu HX, Hou FF, Zhang L, Fu N, Nagai R, et al. Advanced oxidation protein products activate vascular endothelial cells via a RAGE-mediated signaling pathway. Antioxid Redox Signal. 2008;10(10):1699–1712. doi: 10.1089/ars.2007.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Witko-Sarsat V, Friedlander M, Nguyen Khoa T, Capeillere-Blandin C, Nguyen AT, Canteloup S, et al. Advanced oxidation protein products as novel mediators of inflammation and monocyte activation in chronic renal failure. J Immunol. 1998;161(5):2524–32. [PubMed] [Google Scholar]
- 36.Kalousova M, Skrha J, Zima T. Advanced glycation end-products and advanced oxidation protein products in patients with diabetes mellitus. Physiol Res. 2002;51(6):597–604. [PubMed] [Google Scholar]
- 37.Baskol G, Demir H, Baskol M, Kilic E, Ates F, Karakukcu C, et al. Investigation of protein oxidation and lipid peroxidation in patients with rheumatoid arthritis. Cell Biochem Funct. 2006;24(4):307–311. doi: 10.1002/cbf.1257. [DOI] [PubMed] [Google Scholar]
- 38.Danzig V, Mikova B, Kuchynka P, Benakova H, Zima T, Kittnar O, et al. Levels of circulating biomarkers at rest and after exercise in coronary artery disease patients. Physiol Res. 2010;59(3):385–392. doi: 10.33549/physiolres.931764. [DOI] [PubMed] [Google Scholar]
- 39.Piwowar A, Knapik-Kordecka M, Warwas M. AOPP and its relations with selected markers of oxidative/antioxidative system in type 2 diabetes mellitus. Diabetes Res Clin Pract. 2007;77(2):188–192. doi: 10.1016/j.diabres.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 40.Liu SX, Hou FF, Guo ZJ, Nagai R, Zhang WR, Liu ZQ, et al. Advanced oxidation protein products accelerate atherosclerosis through promoting oxidative stress and inflammation. Arterioscler Thromb Vasc Biol. 2006;26(5):1156–1162. doi: 10.1161/01.ATV.0000214960.85469.68. [DOI] [PubMed] [Google Scholar]
- 41.Villalpando Sánchez DC, Alvarez Aguilar C, Gómez GA. Advanced oxidation protein products and their relationship with cardiovascular risk factors in young apparently healthy people. Clin Investig Arterioscler. 2017;29(5):209–215. doi: 10.1016/j.arteri.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 42.Kocak H, Gumuslu S, Sahin E, Ceken K, Gocmen YA, Yakupoglu G, et al. Advanced oxidative protein products are independently associated with endothelial function in peritoneal dialysis patients. Nephrology (Carlton) 2009;14(3):273–280. doi: 10.1111/j.1440-1797.2008.01062.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.