Abstract
Background
The world has been experiencing one of the most significant worldwide health pandemics in modern history. The result has been increased depression, anxiety, and loneliness in the general population. However, populations who demonstrated pre-pandemic emotional disturbance and social isolation, such as individuals with multiple sclerosis (MS), are likely uniquely vulnerable to such symptoms.
Objective
The purpose of the present investigation was to examine the emotional outcomes, including reports of loneliness, in individuals with MS during the COVID-19 pandemic. We additionally sought to examine how individuals’ experiences during the pandemic may contribute to a specific COVID-19-related depression or anxiety.
Methods
142 individuals with MS who previously participated in a national, online, survey-based study were asked to complete an online survey assessing their current level of depression, anxiety, loneliness, and perceived impact of the COVID-19 pandemic.
Results
Increases in the rates of depression and anxiety were noted, with approximately 54% and 33% reporting “new” depression or anxiety, respectively. Given this increase, we examined how individuals with “new” depression or anxiety differed from those without depression and anxiety and those with pre-pandemic depression and/or anxiety. Significant differences in person-specific factors (e.g., personality, self-efficacy) were noted between the groups. Increased loneliness was also found among both those with depression or anxiety regardless of whether “new” or pre-pandemic. Finally, all those depressed or anxious reported greater disruption and distress related to the COVID-19 pandemic with a trend for increased anxiety specifically related to the pandemic (e.g., fear or dying due to COVID-19) among those with new depression or anxiety when compared to those with existing depression or anxiety, suggesting an influence of the pandemic that is specific to reports of new depression or anxiety.
Conclusion
Findings suggest increased depression, anxiety, and loneliness among individuals with MS following the COVID-19 pandemic, with reports of “new” depression or anxiety, which appears to be related to the pandemic, specifically. Moreover, factors commonly associated with depression or anxiety in MS (e.g., personality, self-efficacy) were more common among those with existing depression or anxiety but not among those experiencing new depression or anxiety. These differences should be considered when attempting to ameliorate the impact of the COVID-19 among those experiencing emotional distress.
Keywords: COVID-19, Multiple sclerosis, Depression, Anxiety, Loneliness
1. Introduction
In March 2020, the United States entered one of the most significant worldwide health pandemics in modern history. The novelty of the virus, high rate of transmissibility, and, in some cases, lack of compliance with recommended safety precautions to aid in mitigating the pandemic renders an overarching sense of fear and despair for many. Moreover, the prescription of social distancing reduces social support and connectedness, which is well-known to have a protective and fostering effect on health and well-being (Cassel, 1976; Cobb, 1976).
Since the beginning of the COVID-19 pandemic, studies have shown increased mental health concerns (Peterson et al., 2021) and loneliness among those contending with the pandemic and societal restrictions. Social restriction to limit transmission have placed vulnerable populations, such as those with pre-existing conditions, at increased risk for in loneliness. In fact, among 315 individuals with chronic illnesses, these at-risk individuals reported significantly greater levels of loneliness only one month into social distancing, with rates of loneliness doubling during the pandemic (Elran-Barak and Mozeikov, 2020).
Mental health concerns and loneliness are common in persons with multiple sclerosis (MS), which may be exacerbated by such restrictions. The MS population experiences higher rates of depression and anxiety than the general population, thought to be in part due to brain pathology due to MS (e.g., lesion load) (Feinstein, 2004), as well as adjustment factors associated with living with a chronic illness (Arnett et al., 2008). With regard to the latter, adjustment to MS has been shown to be influenced by both psychological and social factors. Specifically, personality, self-efficacy, and locus of control (LOC) are all known predictors of depression, anxiety, and coping in MS (Tan-Kristanto and Kiropoulos, 2015; Strober, 2016) and perceived social support is a significant predictor of anxiety and depression in MS (Henry et al., 2019). In this context, individuals with MS may be more susceptible to increased depression and anxiety during this time, whether due to relapse of existing symptom patterns or lower threshold for mental health symptoms. Moreover, having an autoimmune disorder and for many, being on immunosuppressive or immunomodulatory therapies, theoretically poses a greater risk of COVID-19 infection (Bhise and Dhib-Jalbut, 2021; Zheng et al., 2020). A higher level of health-related anxiety and self-isolation among individuals with MS during this time, thus, seems appropriate. In fact, over half of individuals with MS self-isolate at a greater rate than imposed by their government (Seery et al., 2020). The potential resultant lack of social support or connectedness, a known predictor of depression, health, and reduced quality of life in MS, may thus worsen the situation. There is therefore a host of precipitating factors that can result in poor emotional functioning and increased loneliness among individuals with MS in this time of crisis.
The present investigation examined the emotional outcomes in individuals with MS, as well as reports of loneliness; we also sought to quantify the impact of COVID-19 among individuals with MS with regard to emotional distress, disruption in daily life, healthcare, and financial concerns, and COVID-19 related anxiety. We hypothesized increased rates of depression, anxiety, and loneliness. Moreover, given the impact of the pandemic, we examined how individuals’ concerns or disruption in life due to the pandemic may contribute to a possible new or COVID-19-related depression or anxiety.
2. Material and methods
2.1. Participants
This study utilized archival data collected during the course of two studies among individuals with clinically definite MS as baseline data for comparison to current emotional distress and impact of COVID-19. The prior studies, on employment and medication adherence, were national surveys conducted between 2013 and 2020. Participants were contacted via email with an opportunity to participate in an online survey study regarding the impact of the COVID-19 pandemic. A total of 142 individuals with MS agreed to participate in the current survey with data collected during the months of August and September (5,6 months from the initial restrictions being placed in the United States). The mean time elapsed between individuals’ previous assessment and assessment during the pandemic was 2.39 years (SD = 1.66; Range: 0–7 years) with the majority (86%) completing these studies within the past three years. The sample consisted of 23 males and 119 females ranging in age from 27 to 71 (M = 50.48, SD = 10.24).
2.2. Procedures
Participants completed an online survey assessing depression, anxiety, loneliness, and factors related to their employment and medication use in light of the COVID-19 pandemic. They also completed a general COVID-19 impact survey to document the financial, social, and emotional effects of the pandemic. Data previously collected included assessment of personality, self-efficacy, locus of control, depression, anxiety, and social support. These data were combined with the present data as factors related to adjustment and well-being during the crisis. All study procedures were approved by the Institutional Review Board of Kessler Foundation.
2.3. Measures
Previous assessment. The following measures were administered as part of the previous investigations.
Personality was assessed with the Ten Item Personality Inventory (TIPI) (Gosling et al., 2003) and includes subscales of Openness, Conscientiousness, Extraversion, Agreeableness, and Neuroticism. Individuals rate on a seven-point Likert scale the extent to which an attribute or behavioral tendency applies to them.
Self-efficacy was measured by the General Self-Efficacy Scale (GSE), (Schwarzer and Jerusalem, 1995) a brief, 10-item measure assessing one's general sense of their ability to handle situations and challenges. Locus of Control was assessed by the International Personality Item Pool Locus of Control scale (IPIP-LOC) (Goldberg et al., 2006). The IPIP-LOC assesses the degree to which individuals perceive having an external versus internal locus of control.
Depression measures varied by study, with either the Chicago Multiscale Depression Inventory (CMDI) (Nyenhuis and Luchetta, 1998) or the Hospital Anxiety and Depression Scale (Zigmond and Snaith, 1983) being administered. Significant depression was operationally defined as a score of T-score of ≥ 65 on the CMDI mood subscale or a raw score ≥ 8 on the HADS depression subscale.
Anxiety was assessed by either the State Trait Anxiety Inventory (STAI) (Spielberger and Gorsuch, 1983) or the Hospital Anxiety and Depression Scale, depending on the study. Significant anxiety was operationally defined as a standard score ≥ 122 on the STAI or a raw score ≥ 8 on the HADS anxiety subscale.
COVID-19 assessment. The following measures were administered during the COVID-19 pandemic:
The COVID-19 Impact Survey, which was developed by Penedo et al. (2020) to assess the overall impact of the pandemic among individuals with cancer. It consists of ten subscales: anxiety, depression, distress, emotional distress, health care disruptions & concerns, disruptions in daily activities and social interactions, financial hardship, perceived benefits, functional social support, and perceived stress management. Ratings on the latter three subscales are reverse-scored so that higher scores on all subscales indicate greater levels of distress or disruption. For the purposes of the present investigation, the distress scale, the disruption composite (which consists of the healthcare disruptions & concerns, disruptions in daily activities and social interactions, and financial hardship subscales), and the anxiety scale were used. The anxiety scale pertains to COVID-19 or health-related anxiety and consists of items such as, “I worry about the possibility of dying from COVID-19″ and “I fear how the COVID-19 pandemic will impact my MS or treatment.”
The De Jong Loneliness Scale (De Jong-Gierveld and Kamphuls, 1985) assesses perceived loneliness with regard to feelings of emotional loneliness and social loneliness. Participants were to rate their feelings of loneliness during and before the COVID-19 pandemic (the latter retrospectively).
The Hospital Anxiety and Depression Scales were administered to assess anxiety and depression during and before the COVID-19 pandemic (the latter retrospectively).
2.4. Statistical analyses
All statistical analyses were conducted using SPSS version 26.0. Initial examination of the rates of depression and anxiety over three time points (previous assessment, immediately prior to COVID-19, and present during the pandemic) was conducted, including Chi-square analyses to determine if the presence of previous depression or anxiety was related to current emotional status. Demographic factors that differed between groups and that are frequently implicated in depression, anxiety, and loneliness were examined for potential use as model covariates. Given the possibility of an increase in rates due to a new-onset COVID-19-related depression or anxiety, group comparisons (Multivariate Analysis of Variance [MANOVAs]) were subsequently conducted between the three depression and anxiety groups (None, new, and existing) on person-specific factors, social support, perceived loneliness, and COVID-19 impact. Given the multiple comparisons, Bonferroni corrections were applied within each domain.
3. Results
A total of 142 individuals with MS completed the COVID-19 impact survey and had complete data from their previous assessment. Participants were primarily female (84%) and married (64%). The mean age was 50.48 (9.03) and mean disease duration was 15.81 (9.03). Finally, the sample was primarily Caucasian (85%) See Table 1 .
Table 1.
XXX.
| Mean (SD) or Frequency | Range | |
|---|---|---|
| Age | 50.48 (10.24) | 27–71 |
| Gender | 119 Female; 23 Male | |
| Ethnicity | 121C; 12AA; 5H; 1A; 1AI, 1O; 1 Undisclosed | |
| Marital Status | 91 M; 19S; 9CH; 17D; 1 W; 5 Undisclosed | |
| Disease Duration (Years) | 15.81 (9.03) | 2–45 |
Note. C = Caucasian; AA = African American; H = Hispanic; A = Asian; AI = American Indian; O = Other, More than one race; M = Married; S = Single; CH = Cohabitating; D = Divorced; W = Widowed.
Delineation of depression and anxiety groups. To quantify the relative incidence of depression and anxiety symptomatology that might be attributable to the pandemic, individuals were categorized into groups depending on their current and pre-COVID history of significant depression and anxiety as measured by self-report cutoffs. More specifically, three timepoints or assessments were utilized: (1) individuals’ previous assessment; (2) ratings immediately prior to pandemic (retrospective report); and (3) ratings during the pandemic (current report) (See Figs. 1 and 2 ).
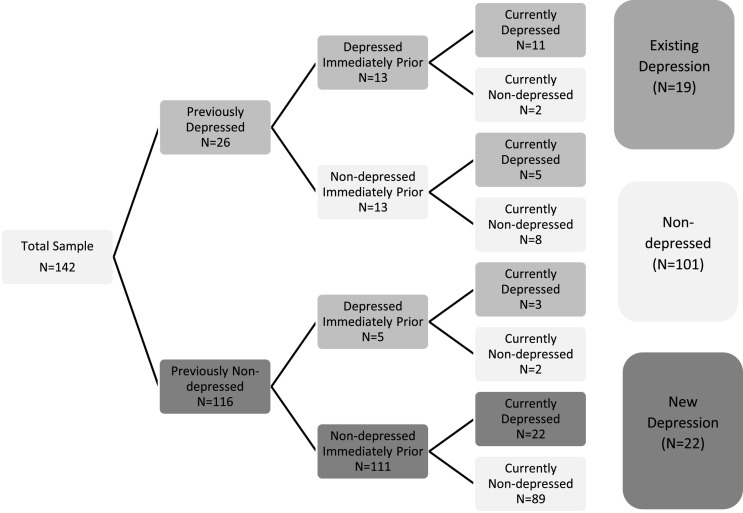
Fig. 1.
Flowchart depicting previous, prior, and current depression among the entire sample.
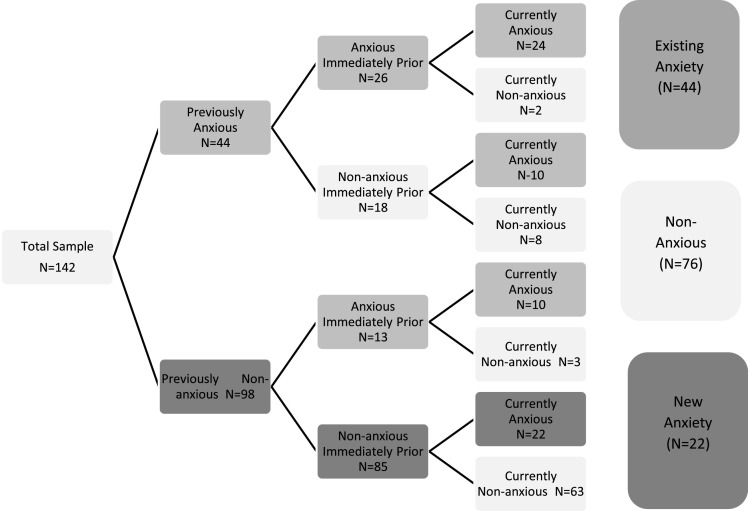
Fig. 2.
Flowchart depicting previous, prior, and current anxiety among the entire sample.
As can be seen in Figs. 1 and 2, the majority of the sample (101 [71%]) was not presently depressed and approximately half (76 [53%]) were not experiencing significant anxiety as measured by self-report cutoffs. Of those experiencing current depression, 22/41 (54%) were experiencing “new” depression (no prior depression but current depression) and 19/41 (46%) had existing depression (yes to both: past or prior depression and current significant depression). Of those currently experiencing anxiety, 22/66 (33%) were found to be experiencing “new” anxiety and 44/66 (67%) had existing anxiety that persisted during the pandemic. For the purposes of the present investigation, comparisons were made between these three groups of depression and anxiety – those with no current depression or anxiety; those with “new” depression or anxiety; and those with “existing” depression or anxiety.
3.1. Rates of clinically significant depression or anxiety pre-/post-pandemic
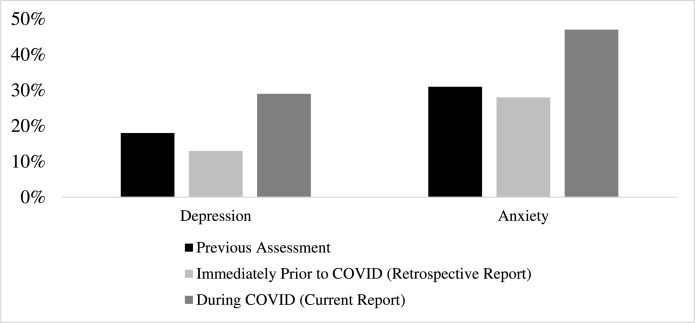
Results indicate increases in rates of depression and anxiety across three time points from pre-pandemic to mid-pandemic assessments. Specifically, rates of depression among this sample when assessed previously was 18% (26/142). Presently, 29% (41/142) endorsed significant levels of depression. This is in contrast to only 13% (18/142) retrospectively reporting significant depression immediately prior to the pandemic. Increases were also seen in rates of anxiety with 31% (44/142) at their previous assessment, 28% (39/142) immediately prior to pandemic, and 47% (66/142) presently (See Fig. 3 ).
Fig. 3.
Rates of depression at previous assessment, immediately prior to COVID-19 pandemic, and present.
Comparisons of the three groups on demographics revealed a significant group effect (p = .036) with individuals with “new” depression being significantly younger than those with existing depression (p = .035). Significant group effects were also found for anxiety (p = .047) with a trend suggesting that those with “new” anxiety were younger than those with no anxiety (p = .057). With regard to gender, there were no differences in gender distribution among the anxiety groups but there was a significantly greater proportion of men in the non-depressed group than the depressed groups (See Table 2 ).
Table 2.
Demographics of the three depression and anxiety groups.
| Non-depressed | New Depression | Existing Depression | ||
|---|---|---|---|---|
| Gender | 22 M/79F | 0 M/22F | 1 M/18F | Fisher's Exact, p = .009 |
| Age | 50.86 (1.00) | 45.86 (2.15) | 53.79 (2.31) | F(2139) = 3.41, p = .036 |
| Non-anxious | New Anxiety | Existing Anxiety | ||
| Gender | 12 M/64F | 6 M/16F | 5 M/39F | Fisher's Exact, p = .257 |
| Age | 52.29 (1.16) | 46.64 (2.15) | 49.27 (1.52) | F(2139) = 3.14, p = .047 |
Given these differences and potential confounding effects, correlational analyses with age and study outcome variables and group differences among gender were conducted. No significant associations or group differences were found.
3.2. Contribution of pre-pandemic depression and anxiety on post-pandemic depression and anxiety
To determine if current symptomatology during the pandemic is related to previous reports of depression and anxiety, Chi-square analyses were conducted. Of the 41 who reported current depression, 16 (39%) reported being depressed previously and 14 (34%) reported being depressed immediately prior to the pandemic. This is in comparison to 10% and 4%, respectively, of the 101 who were not presently experiencing depression (Χ2 = 16.54, p < 0.001 and Χ2 = 24.01, p < 0.001, respectively). Similar findings were found for anxiety with 34 of the 66 (52%) of those presently experiencing anxiety reporting anxiety historically or immediately prior to the pandemic. Among those not presently anxious, only 10 (13%) and 5 (7%) reported anxiety historically or immediately prior to the pandemic (Χ2 = 24.30, p < 0.001 and Χ2 = 35.80, p < 0.001, respectively) (See Table 3 ).
Table 3.
Proportion of presently depressed or anxious individuals with previous reports of depression or anxiety.
| Currently Depressed (N = 41) | Currently Not Depressed (N = 101) | |||
|---|---|---|---|---|
| No | Yes | No | Yes | |
| Previous report of depression | 25 (61%) | 16 (39%) | 91 (90%) | 10 (10%) |
| Depressed immediately prior to pandemic | 27 (66%) | 14 (34%) | 97 (96%) | 4 (4%) |
| Currently Anxious (N = 66) | Currently Not Anxious (N = 76) | |||
| No | Yes | No | Yes | |
| Previous report of anxiety | 32 (48%) | 34 (52%) | 66 (87%) | 10 (13%) |
| Anxious immediately prior to pandemic | 32 (48%) | 34 (52%) | 71 (93%) | 5 (7%) |
Based on these findings, we sought to determine if there were differences among those with “new” depression or anxiety versus those who reported not being presently depressed or anxious and those who reported being depressed or anxious during the pandemic, but who also had historical depression or anxiety (“existing” depression). Specifically, we examined the differences of person-specific factors (i.e., personality, self-efficacy, LOC), social support (previously assessed), perceived emotional and social loneliness immediately prior to and during the pandemic, and more importantly, the impact of the pandemic among these groups.
3.3. Person-specific factors and perceived social support prior to pandemic related to clinically significant symptoms by group
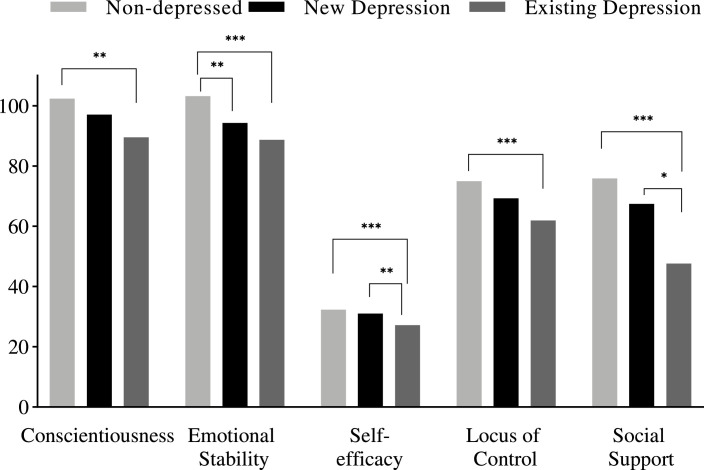
Significant group differences were found for person-specific factors and social support (F[16,264]= 3.25, p < .001; Wilk's Λ = 0.698, ηp 2= 0.17). Applying a Bonferroni correction (0.05/8 = 0.006), significant differences between the three depression groups were found on conscientiousness (F[2139]= 6.15, p = .003; ηp 2= 0.08), emotional stability (F[2139]= 12.72, p < .001; ηp 2= 0.16), self-efficacy (F[2139]= 12.04, p < .001; ηp 2= 0.15), LOC (F[2139]= 8.22, p < .001; ηp 2= 0.11), and social support (F[2139]= 10.91, p < .001; ηp 2= 0.14). Post-hoc analyses indicated that individuals with “existing” depression reported significantly lower levels of conscientiousness, emotional stability, self-efficacy, LOC, and perceived social support than non-depressed individuals (p's≤.001). Individuals with “new” depression reported significantly lower emotional stability compared to the non-depressed group (p = .004) and greater self-efficacy than those with “existing” depression (p = .004) (See Fig. 4 ).
Fig. 4.
Differences in person-specific factors and social support among the three depression groups.
Note. * = Sig. at 0.05; ** = Sig. at 0.01; *** = Sig. at 0.001.
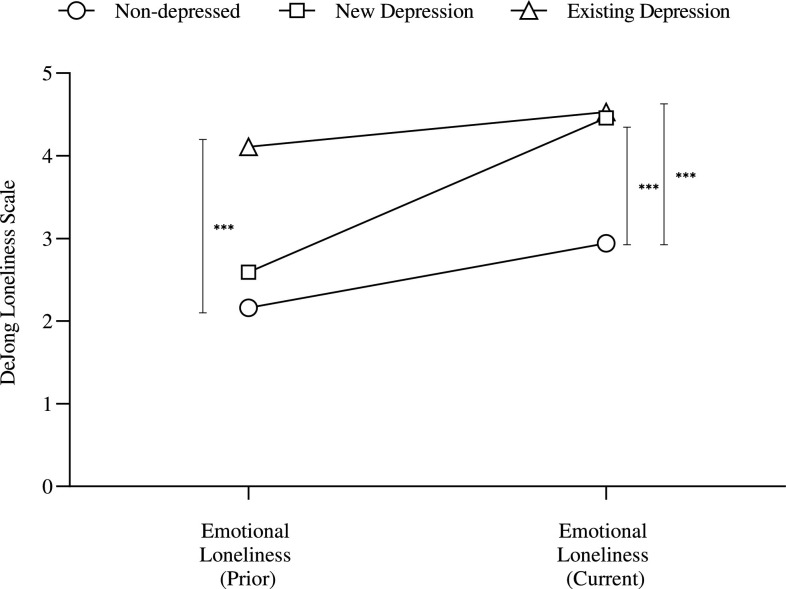
On a measure of perceived loneliness, significant group differences were also found for depression (F[8272]= 6.02, p < .001; Wilk's Λ = 0.722, ηp 2= 0.15). Applying a Bonferroni correction (0.05/4 = 0.013), the three groups differed on emotional loneliness (F[2139]= 7.00, p < .001; ηp 2= 0.09) and social loneliness (F[2139]= 9.75, p < .001; ηp 2= 0.12) prior to the pandemic. Similarly, they differed on emotional loneliness (F[2139]= 10.99, p < .001; ηp 2= 0.14) and social loneliness (F[2139]= 16.57, p < .001; ηp 2= 0.19) during the pandemic. More specifically, individuals with “existing” depression reported greater perceived emotional loneliness immediately prior to the pandemic when compared to non-depressed individuals (p < .001). However, reports during the pandemic, indicate that those with “new” depression report comparable levels of emotional loneliness as those with “existing” depression and both groups report significantly more emotional loneliness than those non-depressed (p's≤.001) (See Fig. 5 ).
Fig. 5.
Differences in perceived emotional loneliness immediately prior to and during the pandemic among the three depression groups.
Note. * = Sig. at 0.05; ** = Sig. at 0.01; *** = Sig. at 0.001.
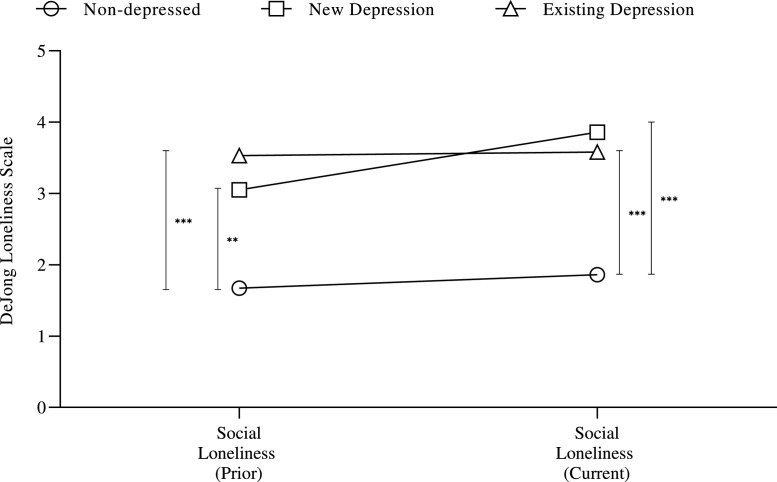
With regard to social loneliness, the two depression groups did not differ prior to or during the pandemic, but both reported significantly greater social loneliness than the non-depressed (p's<0.01) (See Fig. 6 ).
Fig. 6.
Differences in perceived social loneliness immediately prior to and during the pandemic among the three depression groups.
Note. * = Sig. at 0.05; ** = Sig. at 0.01; *** = Sig. at 0.001.
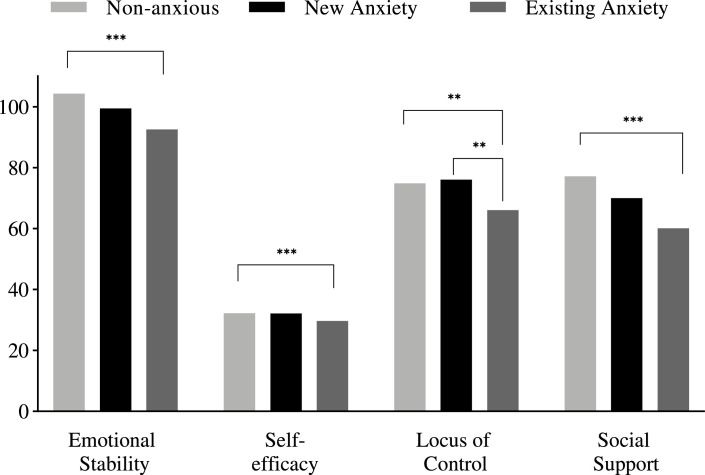
When examining differences among the three anxiety groups, similar, significant group differences were noted (F[16,264]= 2.55, p = .001; Wilk's Λ = 0.750, ηp 2= 0.13). Applying a Bonferroni correction (0.05/8 = 0.006), the groups differed on emotional stability (F[2139]= 11.62, p < .001; ηp 2= 0.14), LOC (F[2139]= 6.93, p = .001; ηp 2= 0.09), and social support (F[2139]= 6.39, p = .002; ηp 2= 0.08). Post-hoc analyses revealed that individuals with “existing” anxiety reported significantly lower levels of emotional stability, LOC, social support (p's≤.001) and self-efficacy (p = .002) compared to non-anxious individuals There were no differences between individuals with “new” anxiety and non-anxious individuals. Finally, individuals with “new” anxiety reported significantly greater LOC than those with “existing” anxiety (p = .005) (See Fig. 7 ).
Fig. 7.
Differences in person-specific factors and social support among the three anxiety groups.
Note. * = Sig. at 0.05; ** = Sig. at 0.01; *** = Sig. at 0.001.
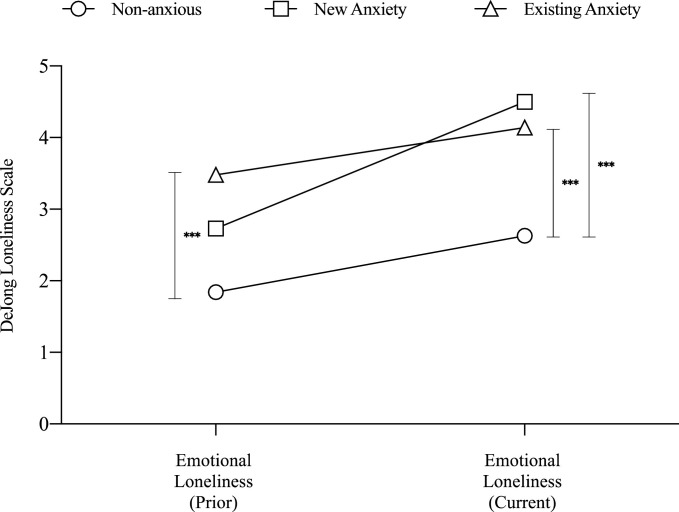
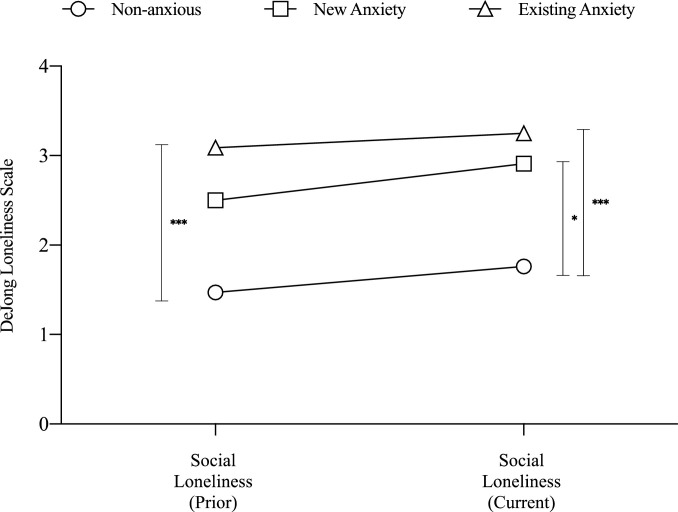
Significant group differences were also noted on perceived loneliness (F[8272] = 5.32, p < .001; Wilk's Λ = 0.748, ηp 2= 0.14). Applying a Bonferroni correction (0.05/4 = 0.013), the three groups differed on emotional loneliness (F[2139]= 8.96, p < .001; ηp 2= 0.11) and social loneliness (F[2139]= 9.72, p < .001; ηp 2= 0.12) prior to the pandemic. Similarly, significant group effects exist for emotional loneliness (F[2139]= 15.91, p < .001; ηp 2= 0.19) and social loneliness (F[2139]= 10.19, p < .001; ηp 2= 0.13) during the pandemic. Individuals with “existing” anxiety reported greater levels of emotional and social loneliness immediately prior to the pandemic than non-anxious individuals (p's<0.001). Individuals with “new” anxiety did not differ from either of the two groups prior to the pandemic. However, during the pandemic, individuals with “new” anxiety reported comparable levels of emotional and social loneliness as those with “existing” anxiety. Both those with existing anxiety and new anxiety reported significantly greater emotional loneliness (p's<0.001) and social loneliness (p < .001 and 0.011, respectively) than those non-anxious (See Figs. 8 and 9 ).
Fig. 8.
Differences in perceived emotional loneliness immediately prior to and during the pandemic among the three depression groups.
Note. * = Sig. at 0.05; ** = Sig. at 0.01; *** = Sig. at 0.001.
Fig. 9.
Differences in perceived social loneliness immediately prior to and during the pandemic among the three depression groups.
Note. * = Sig. at 0.05; ** = Sig. at 0.01; *** = Sig. at 0.001.
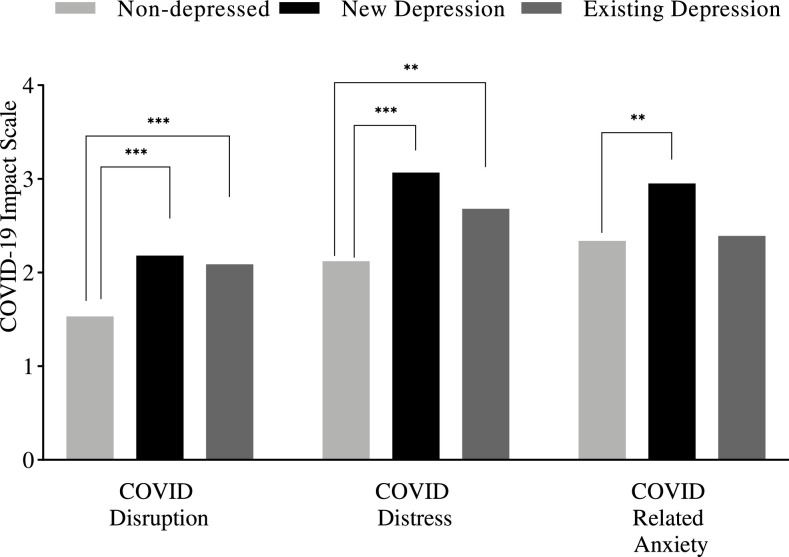
3.4. Impact of COVID-19
Finally, we compared the three depression and three anxiety groups on a measure assessing the impact of the COVID-19 pandemic on individuals’ perceived distress and disruptions in healthcare, daily activities and social interactions, and financial hardship. There was a significant difference for the depression groups (F[6274]= 9.51, p < .001; Wilk's Λ = 0.685, ηp 2= 0.17). Applying a Bonferroni correction (p = .05/3 = 0.017), large effects were found for disruption (F[2139]= 16.45, p < .001; ηp 2= 0.19) and distress (F[2139]= 18.29, p < .001; ηp 2= 0.20). Small effects were seen for COVID-related anxiety, albeit statistically significant (F[2139]= 3.87, p = 0.023; ηp 2= 0.05). As can be seen in Fig. 10 , individuals with “new” or “existing” depression reported significantly greater disruption (p's < 0.001) and emotional distress due to COVID-19 than those non-depressed (p < .001 and p = .002, respectively). There were no differences between “existing” and “new” depression. With regard to COVID-related anxiety, individuals with “new” depression expressed greater COVID-related anxiety than those non-depressed (p = .006). There was no difference between those with “new” or “existing” depression. However, while not significantly different, individuals with “new” depression reported greater levels of distress (p = .090) and COVID-related anxiety (p = .058) associated with COVID-19 than those with “existing” depression.
Fig. 10.
Differences in perceived impact of COVID-19 among the three depression groups.
Note. * = Sig. at 0.05; ** = Sig. at 0.01; *** = Sig. at 0.001.
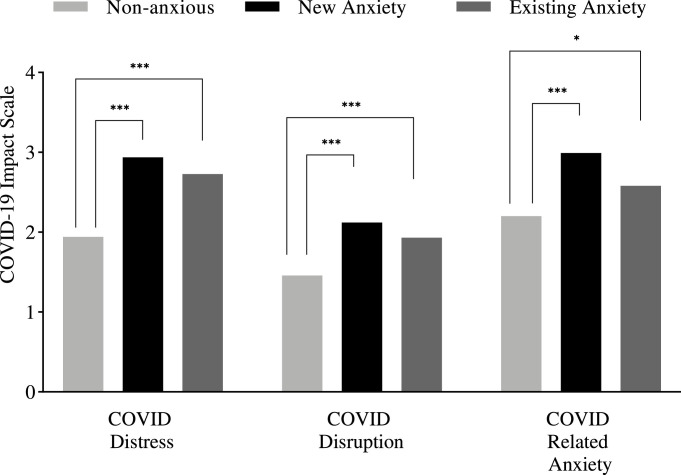
Similar findings were found for anxiety (F[6274]= 11.80, p < .001; Wilk's Λ = 0.631, ηp 2= 0.21) with, again, fairly large effects for both disruption (F[2139]= 16.05, p < .001; ηp 2= 0.19) and distress (F[2139]= 28.48, p < .001; ηp 2= 0.29) and medium effects for COVID-related anxiety (F[2139]= 6.96, p = .001; ηp 2= 0.09). Specifically, individuals with “new” or “existing” anxiety reported significantly greater disruption and distress than those non-anxious (p's < 0.001). There were no differences between “existing” and “new” anxiety with regard to the disruption and distress associated with COVID-19. Again, individuals with “new” anxiety expressed greater COVID-related anxiety than those non-anxious (p = .001). There was no difference between those with “new” or “existing” anxiety. Similarly, while not significantly different, individuals with “new” anxiety reported greater levels of COVID-related anxiety (p = .093) than those with “existing” anxiety (See Fig. 11 ).
Fig. 11.
Differences in perceived impact of COVID-19 among the three anxiety groups.
Note. * = Sig. at 0.05; ** = Sig. at 0.01; *** = Sig. at 0.001.
4. Discussion
The purpose of the present investigation was to examine the effects of the COVID-19 pandemic on mental health among individuals with MS. This study provides a unique contribution to the growing literature on the effects of COVID-19 on the MS population due to its utilization of pre-pandemic data for the study sample. In other words, this longitudinal study design allows us to determine whether a specific cohort of individuals experienced an increase in mental health symptoms, and to examine pre-existing characteristics that may have made them more or less resilient. Given the vulnerability to depression and anxiety in this population and the effects of social isolation or loneliness, it was anticipated that we would observe relative increases in depression and anxiety during this time, consistent with other cross-sectional studies that have been published recently (Morris-Bankole and Ho, 2021; Motolese et al., 2020; Donisi et al., 2021; Costabile et al., 2021; Uhr et al., 2021; Alirezaei et al., 2021). When examining the overall rates of depression and anxiety prior to and during the pandemic, we indeed found an increase in the rate of depression from 13% to 29% and an increase in the rate of anxiety from 28% to 47%. Closer examination of the trajectories of depression and anxiety over time, as seen in Table 2, suggests a combination of both consistency and novelty in mental health symptoms from pre-pandemic status. In other words, many of our participants remained stable, such that a prior history of depression or anxiety tended to beget current depression or anxiety, and that most individuals with no history of depression or anxiety did not report current depression or anxiety during the pandemic. However, as also shown in Figs. 1 and 2, more than half of the 41 individuals (54%) who reported current significant depression did not previously report any depression and 33% of the 66 individuals who reported currently experiencing anxiety did not report anxiety previously, suggesting a presence of depression and anxiety that is specific to the COVID-19 pandemic. Efforts to understand and ameliorate this situational depression and anxiety are warranted.
Given this new incidence of emotional symptomatology, we sought to first determine if there were differences in the role of person-specific factors among those with existing depression and anxiety and those with “new” depression and anxiety. Specifically, it was hypothesized that person-specific factors such as personality and self-efficacy, which are known predictors of depression and anxiety in MS (Amtmann et al., 2012; Garfield and Lincoln, 2012), would continue to reign as significant predictors of those with existing depression or anxiety, in the context of myriad additional stressors present during the COVID pandemic. In contrast, these factors may not play as significant of a role among those whose depression or anxiety seemed more related to the pandemic, or situational and external factors. Present findings confirmed this latter hypothesis. Specifically, while those with existing depression reported lower levels of conscientiousness, emotional stability, self-efficacy, and locus of control than non-depressed individuals, individuals with “new” depression did not significantly differ on the majority of these factors from those non-depressed. Additionally, those with “new” depression reported significantly higher levels of self-efficacy than those with existing depression, akin to those non-depressed. Similar findings were noted with anxiety, with individuals with existing anxiety reporting significantly lower levels of emotional stability, self-efficacy, and locus of control compared to non-anxious individuals and no differences being found between those with “new” anxiety and non-anxious individuals. And again, those with “new” anxiety reported greater locus of control than those with existing anxiety. Together, these findings confirm the hypothesis that role of person-specific factors are greater among those with existing depression and anxiety and less on current, “new” experiences of depression and anxiety during the pandemic.
These findings have significant implications for proper mental health diagnosis and treatment as we attempt to address the increased mental health concerns associated with the COVID-19 pandemic. For instance, improving self-efficacy is a common target for reducing depression and loneliness in MS. However, in this situation, individuals with “new” depression actually did not differ from the non-depressed and had greater self-efficacy than those with existing depression. This may suggest that for those with “new” depression, cognitive behavioral interventions might focus more on education regarding situational depression and efforts to increase coping, resilience, social network, and engagement in positive mental health habits (e.g., sleep hygiene, exercise, diet, relaxation) as individuals adjust to the pandemic and related stressors, as opposed to say challenging negative, automatic thoughts. The latter may be more relevant to those with existing depression, particularly those whose depression or anxiety has worsened with the pandemic.
The role of social support on depression and anxiety is also well appreciated in MS and is a significant determinant, in general times. When examining its role with regard to present depression and anxiety during the COVID pandemic, it was found that, comparable to person-specific factors, social support was a greater predictor for those with existing depression and anxiety and not for those with “new” depression or anxiety. On the other hand, reports of emotional loneliness prior to and during the pandemic, suggests an increase for those with “new” depression and anxiety but consistently high reports among those with existing depression. Such findings suggest that while emotional loneliness may be a consequence or antecedent of longstanding depression and anxiety, it is also an artifact of the pandemic among those with “new’ depression or anxiety. Indeed, this is consistent with recent cross-sectional investigations linking high rates of depression in persons with MS to decreased perception of social support in the context of the pandemic (Bonavita et al., 2021). Reports of emotional or social loneliness did not seem to increase among those non-depressed or non-anxious.
Finally, to further determine the direct impact of COVID-19 and its association with mental health, we compared the three depression and three anxiety groups on the COVID impact scale. Regardless of experiencing “new” or existing depression or anxiety, all individuals with current depression or anxiety reported greater disruption and distress related to the pandemic than those non-depressed. Of note, individuals with “new’ depression or anxiety also expressed greater COVID-related anxiety than those non-depressed or non-anxious and a trend when compared to those with existing depression or anxiety. This finding is illuminating and consistent with the idea that individuals with “new” depression or anxiety may be experiencing greater depression or anxiety as it relates specifically to the pandemic and associated fears or anxieties. Items pertaining to COVID-related anxiety included feeling anxious about getting COVID, fear of infecting others, fear of having a close friend or family member die from COVID, fear of dying from COVID, and fear of how COVID will affect their MS. Given this, efforts to mitigate individuals’ fears and anxiety regarding COVID-19 may also be indicated for those with “new” depression or anxiety. This may include education regarding COVID-19 and MS, assurance that they are maintaining their MS treatment safely and engaging in positive health-related behaviors, assistance in reducing their exposure, encouragement of speaking to a counselor during this time, identification of the things that are within one's control and those that are not, and identification of strategies to create a “new normal” with regard to social interaction, activities within the home, etc., as they contend with the pandemic and its uncertainty.
The present study is not without limitations. First, data collection during the COVID pandemic occurred between late August and October 2020, which is approximately 4–6 months removed from the pandemic's first major effects in the United States. The impact of the pandemic varied in effect and scope since the official lockdown in March 2020. By the time we reached out to participants to initiate data collection, the infection rate had slowed significantly since the first wave in the spring and early summer, and the initial crunch of socioeconomic consequences had subsided as virtual solutions (e.g., remote work, e-commerce, telehealth appointments) became more mainstream. As such, our results may represent a more optimistic picture of mental health in the MS population than what was experienced in early 2020 or during the subsequent waves in late 2020 and early 2021. Future research should seek to capture data from these periods of higher pandemic effects to gain a clearer view of total mental health impact. Similarly, follow-up assessments on cohorts such as these are warranted to examine the long-term impact of the COVID pandemic on mental health symptoms. Second, our dataset is comprised of individuals with MS who have participated in previous survey-based research over the span of seven years, from which we drew information about previous mental health symptoms. In other words, categorization of participants based on previous symptoms is based strictly on endorsement of clinically significant depression or anxiety at these prior visits, rather than a comprehensive lifetime history of mental health symptoms. This means that we may have misclassified a portion of individuals has having “new” symptoms, when in fact, their history of symptoms occurred outside of their previous assessment epochs. Additionally, our population was largely comprised of individuals with relapsing-remitting MS, who may experience relatively lower levels of disability and could have therefore been less impacted by the pandemic. Future work should examine disease specific factors that could modify these results, including MS diagnosis, level of disability, and time since diagnosis. Lastly, these findings may not be unique to MS, and might be worth exploring in comparable neurological conditions with heightened mental health risk.
Overall, this study suggests that depression and anxiety in individuals with MS following the COVID-19 is not homogeneous, and that COVID-related stress plays a significant role in a subset of individuals. MS clinicians should take care to understand the nature of their patient's mood and anxiety symptoms, particularly if new onset post-pandemic, to ensure appropriate treatment targets.
CRediT authorship contribution statement
L. Strober: Conceptualization, Methodology, Formal analysis, Data curation, Writing – original draft, Visualization. E. Weber: Conceptualization, Methodology, Writing – review & editing. A. Lequerica: Conceptualization, Methodology, Writing – review & editing. N. Chiaravalloti: Writing – review & editing.
Declaration of Competing Interest
The author(s) declare that there is no conflict of interest.
Acknowledgments
This work was supported, in part, by the National Institutes of Health, Robert E. Leet & Clara Guthrie Patterson Trust, and Sanofi Genzyme.
References
- Alirezaei M., Eskandarieh S., Sahraian M.A., Moghadasi A.N. Depression, anxiety, and fear of COVID-19 in patients with multiple sclerosis in pandemic era: a cross-sectional study. Neurol. Sci. 2021:1–8. doi: 10.1007/s10072-021-05612-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amtmann D., Bamer A.M., Cook K.F., Askew R.L., Noonan V.K., Brockway J.A. University of Washington self-efficacy scale: a new self-efficacy scale for people with disabilities. Arch. Phys. Med. Rehabil. 2012;93(10):1757–1765. doi: 10.1016/j.apmr.2012.05.001. [DOI] [PubMed] [Google Scholar]
- Arnett P.A., Barwick F.H., Beeney J.E. Depression in multiple sclerosis: review and theoretical proposal. J. Int. Neuropsychol. Soc. 2008;14(5):691–724. doi: 10.1017/S1355617708081174. [DOI] [PubMed] [Google Scholar]
- Bhise V., Dhib-Jalbut S. Potential risks and benefits of multiple sclerosis immune therapies in the COVID-19 era: clinical and immunological perspectives. Neurotherapeutics. 2021;18(1):244–251. doi: 10.1007/s13311-021-01008-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonavita S., Sparaco M., Russo A., Borriello G., Lavorgna L. Perceived stress and social support in a large population of people with multiple sclerosis recruited online through the COVID-19 pandemic. Eur. J. Neurol. 2021;28(10):3396–3402. doi: 10.1111/ene.14697. [DOI] [PubMed] [Google Scholar]
- Cassel J. The contribution of the social environment to host resistance: the fourth wade hampton frost lecture. Am. J. Epidemiol. 1976;104(2):107–123. doi: 10.1093/oxfordjournals.aje.a112281. [DOI] [PubMed] [Google Scholar]
- Cobb S. Social support as a moderator of life stress. Psychosom. Med. 1976;38(5):300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- Costabile T., Carotenuto A., Lavorgna L., et al. COVID-19 pandemic and mental distress in multiple sclerosis: implications for clinical management. Eur. J. Neurol. 2021;28(10):3375–3383. doi: 10.1111/ene.14580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jong-Gierveld J., Kamphuls F. The development of a rasch-type loneliness scale. Appl. Psychol. Meas. 1985;9(3):289–299. [Google Scholar]
- Donisi V., Gajofatto A., Mazzi M.A., et al. Insights for fostering resilience in young adults with multiple sclerosis in the aftermath of the COVID-19 emergency: an Italian survey. Front. Psychiatry. 2021;11:1660. doi: 10.3389/fpsyt.2020.588275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elran-Barak R., Mozeikov M. One month into the reinforcement of social distancing due to the COVID-19 outbreak: subjective health, health behaviors, and loneliness among people with chronic medical conditions. Int. J. Environ. Res. Public Health. 2020;17(15):5403. doi: 10.3390/ijerph17155403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein A. The neuropsychiatry of multiple sclerosis. Can. J. Psychiatry. 2004;49(3):157–163. doi: 10.1177/070674370404900302. [DOI] [PubMed] [Google Scholar]
- Garfield A., Lincoln N. Factors affecting anxiety in multiple sclerosis. Disabil. Rehabil. 2012;34(24):2047–2052. doi: 10.3109/09638288.2012.667503. [DOI] [PubMed] [Google Scholar]
- Goldberg L.R., Johnson J.A., Eber H.W., et al. The international personality item pool and the future of public-domain personality measures. J. Res. Personal. 2006;40(1):84–96. [Google Scholar]
- Gosling S.D., Rentfrow P.J., Swann W.B. A very brief measure of the big-five personality domains. J. Res. Personal. 2003;37(6):504–528. [Google Scholar]
- Henry A., Tourbah A., Camus G., et al. Anxiety and depression in patients with multiple sclerosis: the mediating effects of perceived social support. Mult. Scler. Relat. Disord. 2019;27:46–51. doi: 10.1016/j.msard.2018.09.039. [DOI] [PubMed] [Google Scholar]
- Morris-Bankole H., Ho A.K. The COVID-19 pandemic experience in multiple sclerosis: the good, the bad and the neutral. Neurol. Ther. 2021;10(1):279–291. doi: 10.1007/s40120-021-00241-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motolese F., Rossi M., Albergo G., et al. The psychological impact of COVID-19 pandemic on people with multiple sclerosis. Front. Neurol. 2020;11:1255. doi: 10.3389/fneur.2020.580507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyenhuis D.L., Luchetta T. The development, standardization, and initial validation of the Chicago multiscale depression inventory. J. Personal. Assess. 1998;70(2):386–401. doi: 10.1207/s15327752jpa7002_14. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Cohen L, Bower J, Antoni MH. Impact of the COVID-19 pandemic in Cancer survivors. Unpublished questionnaire. 2020 [Google Scholar]
- Peterson J.A., Chesbro G., Larson R., Larson D., Black C.D. Short-term analysis (8 weeks) of social distancing and isolation on mental health and physical activity behavior during COVID-19. Front. Psychol. 2021;12:738. doi: 10.3389/fpsyg.2021.652086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer R., Jerusalem M. Generalized self-efficacy scale. Measures in health psychology: A user's portfolio Causal and control beliefs. 1995;1:35–37.
- Seery N., Li V., Nguyen A.L., et al. Evaluating the perspective of patients with MS and related conditions on their DMT in relation to the COVID-19 pandemic in one MS centre in Australia. Mult. Scler. Relat. Disord. 2020;46 doi: 10.1016/j.msard.2020.102516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C.D., Gorsuch R.L. Mind Garden, Incorporated; 1983. State-Trait Anxiety Inventory for Adults: Manual, Instrument, and Scoring Guide. [Google Scholar]
- Strober L. Personality in multiple sclerosis (MS): impact on health, psychological well-being, coping, and overall quality of life. Psychol. Health Med. 2016;22(2):152–161. doi: 10.1080/13548506.2016.1164321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan-Kristanto S., Kiropoulos L.A. Resilience, self-efficacy, coping styles and depressive and anxiety symptoms in those newly diagnosed with multiple sclerosis. Psychol. Health Med. 2015;20(6):635–645. doi: 10.1080/13548506.2014.999810. [DOI] [PubMed] [Google Scholar]
- Uhr L., Rice D.R., Mateen F.J. Sociodemographic and clinical factors associated with depression, anxiety, and general mental health in people with multiple sclerosis during the COVID-19 pandemic. Mult. Scler. Relat. Disord. 2021;56 doi: 10.1016/j.msard.2021.103327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng C., Kar I., Chen C.K., et al. Multiple sclerosis disease-modifying therapy and the COVID-19 pandemic: implications on the risk of infection and future vaccination. CNS Drugs. 2020;34(9):879–896. doi: 10.1007/s40263-020-00756-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]