Abstract
Ethyl pyruvate (EP) has potent influence on redox processes, cellular metabolism, and inflammation. It has been intensively studied in numerous animal models of systemic and organ-specific disorders whose pathogenesis involves a strong immune component. Here, basic chemical and biological properties of EP are discussed, with an emphasis on its redox and metabolic activity. Further, its influence on myeloid and T cells is considered, as well as on intracellular signaling beyond its effect on immune cells. Also, the effects of EP on animal models of chronic inflammatory and autoimmune disorders are presented. Finally, a possibility to apply EP as a treatment for such diseases in humans is discussed. Scientific papers cited in this review were identified using the PubMed search engine that relies on the MEDLINE database. The reference list covers the most important findings in the field in the past twenty years.
Keywords: Ethyl pyruvate, Autoimmunity, Inflammation, Redox, Metabolism
Introduction
Pyruvate (CH3COCOO−), an anion of pyruvic acid, plays an essential role in intermediary cellular metabolism. After it was first determined that pyruvate had the ability to scavenge reactive oxygen species (ROS), studies showed that the utilization of exogenous pyruvate initiates antioxidative and anti-inflammatory effects, both in vitro and in vivo. Still, pyruvate spontaneously undergoes condensation and cyclization reactions in aqueous solutions, which could produce potentially toxic end products. To avoid that possibility, ethyl pyruvate (EP, CH3COCOOC2H5), a derivative of pyruvic acid, was tested as an alternative, and was found both stable and non-toxic in aqueous form [1, 2]. Furthermore, when applied in vivo in various disease models, EP is most commonly administered in Ringer’s solution, a Ca2+-containing balanced salt solution. In that setting, two molecules of EP associate with Ca2+ to form a chelate complex, which is highly stable [3]. Additionally, whereas pyruvate transport into the cell is dependent on monocarboxylate transporters, EP, being electrically neutral and more lipophilic than pyruvate, permeates biological membranes by diffusion to enter the cytoplasm or mitochondria [2, 4].
As it will be discussed throughout this review, EP has been shown to exert a number of beneficial effects in various in vitro/in vivo settings, including the modulation of the redox environment and prevention of ROS-mediated damage, promotion of cell metabolism and the ensuing energy production, and inhibition of inflammation by shaping immune cell signaling, activation and differentiation. All of these favorable effects of EP will be discussed in the context of its potential to treat autoimmune and chronic inflammatory diseases.
Ethyl pyruvate, a Jack of all trades
Redox mechanisms of EP
As ROS are inadvertently generated through multiple metabolic pathways in the mitochondria, eukaryotic cells synthesize a variety of endogenous antioxidants whose task is to provide protection from oxidative damage. If the delicate balance between oxidants and antioxidants becomes disrupted, which is the case during the pathogenesis of many chronic diseases, including autoimmune disorders, excessive ROS levels can modify the structure and function of lipids, proteins or DNA. These modifications can lead to aberrations in gene expression, energy metabolism, cell signaling and many other cellular functions, relevant for excessive immune cell activation and perpetuating inflammation [5, 6]. As ROS-mediated oxidation can directly cause lipid peroxidation, levels of lipid oxidation products are elevated under oxidative stress conditions [7].
Numerous animal studies have confirmed the notion that EP possesses ROS-scavenging abilities. The addition of EP to the Ringer's solution during resuscitation of rats from hemorrhagic shock decreased hepatic lipid peroxidation, to a level similar to that found in the sham control group [8]. Antioxidant potency of EP was also validated in studies on animal models of liver ischemia–reperfusion injury [9], off-pump coronary bypass [10], bacterial translocation after thermal injury [11] or cisplatin-induced nephrotoxicity [12]. In a rat model of extrahepatic cholestasis, treatment with EP decreased lipid peroxidation in the liver, while a trend of increased glutathione (GSH) was also detected [13]. GSH, by participating in many ROS- and reactive nitrogen species-detoxification reactions and thus preventing oxidative stress-induced cellular damage, serves as a “master antioxidant”. Importantly, diminished GSH has been observed in a number of inflammatory diseases [14]. Neuroprotective effects of EP that were demonstrated in an aluminum chloride-induced Alzheimer's disease model were partially a consequence of decreased lipid peroxidation and lower nitrite levels in the brain and increased levels of GSH, catalase, and superoxide dismutase [15]. Additionally, EP was able to inhibit glomerular NADPH oxidase activity and lower the resulting generation of ROS induced by diabetes in an animal model of diabetic nephropathy [16].
In vitro, EP protected human trabecular meshwork cells in culture from hydrogen peroxide-induced oxidative stress [17], and it also suppressed hydrogen peroxide-induced astrocyte cell death [18]. It is possible that these effects were at least partially mediated by EP’s direct scavenging of ROS, as it was found that EP could efficiently decompose hydrogen peroxide in the reaction mixture [19]. In the same study, EP showed a strong scavenging potential towards the superoxide anion radical (O2•−), possibly by acting as a reducing agent and donating a hydrogen atom to the superoxide anion.
EP was also able to stimulate the antioxidant systems in a number of different cell types. Astrocytes treated with EP exhibited higher activation of the nuclear factor E2-related factor 2 (Nrf2), a transcription factor that can translocate from the cytosol to the nucleus and bind to the antioxidant response element (ARE) positioned on the heme oxygenase 1 (HO-1) promoter. By increasing the synthesis of several antioxidant molecules downstream of Nrf2 (including HO-1 and GSH), EP ameliorated the oxidative damage of hydrogen peroxide [18]. In addition, EP attenuated both the oxidation of low-density lipoprotein (LDL) in vitro and the cytotoxic effects of highly oxidized LDL on a human vascular endothelial cell line [20].
On the other hand, while ameliorating lipopolysaccharide (LPS)-induced lipid peroxidation in a RAW 264.7 macrophage cell line, EP was also shown to decrease GSH cellular levels [21]. In this LPS-stimulated macrophage-like cell line, EP stimulated nuclear accumulation of Nrf2, ARE activity, and HO-1 expression, which was dependent on p38 mitogen-activated protein kinase (MAPK) phosphorylation. The depletion of intracellular GSH levels by EP presumably caused oxidative stress and changed the redox state of the cell, thus stimulating p38 MAPK and activating Nrf2 [22].
Similarly, dendritic cells (DC) differentiated in the presence of EP had increased Nrf2 activation and HO-1 expression compared to DC differentiated without EP. The effect was observed both in immature and in LPS-matured DC (our unpublished observations). Additionally, EP induced nuclear translocation of Nrf2 which bound to ARE on the HO-1 promoter and recruited p300, a transcriptional co-activator of both Nrf2 and p65, a subunit of NF-κB in a microglial cell line BV2. The resulting inhibition of the p65-p300 interaction prevented LPS-induced inducible nitric oxide (NO) synthase (iNOS) expression [23]. Likewise, EP suppressed NADPH oxidase, which generated ROS when activated by LPS in the same cell line. The EP-reduced ROS production resulted in JAK2 inactivation, which inhibited STAT1 and STAT3 phosphorylation and prevented their translocation into the nucleus, thus inhibiting the expression of iNOS and multiple pro-inflammatory cytokines [24]. These studies showcase the ability of EP to accomplish both antioxidative and anti-inflammatory effects through a shared mechanism of action.
Furthermore, as it will be reviewed in detail later, EP is possibly most known for being an inhibitor of HMGB1 expression/release. Theoretically, this effect might also be partially mediated by EP redox-modulating properties, as the oxidation state of HMGB1 dictates its (extra)cellular localization. Under mild oxidative stress, an intramolecular disulfide bond is formed in HMGB1 (Cys23-Cys45), which increases its nucleocytoplasmic translocation and extracellular secretion. Once outside the cell, HMGB1 can induce an immune response, and HMGB1 oxidation status can also determine its immune functions [25].
It is known that ROS, besides being potentially harmful, can also function as second messengers in receptor signaling, by regulating the activity of different transcriptional factors and signaling molecules [26]. Generally, inflammation and oxidative stress are considered closely linked and interdependent – while the inflammatory process can induce oxidative stress, the sequence of these events can also easily go in the opposite direction [27]. The forementioned studies which examined the antioxidative abilities of EP showed that, aside from being able to potentiate an endogenous antioxidant response and thus provide protection from ROS, its effects on the intracellular redox environment could modulate the inflammatory response as well. This overlap might be one of the reasons behind the efficacy with which EP has ameliorated the symptoms of disease in various animal models where damage has been inflicted by both a strong immune response and oxidative stress, which will also be the focus of the final section of this review.
Effect of EP on the cell metabolism
In the cytoplasm, pyruvate is generated as the end product of glycolysis, along with adenosine triphosphate (ATP), while the oxidized form of nicotinamide adenine dinucleotide (NAD+), a cofactor that functions as an electron carrier, becomes reduced (NADH). Pyruvate can then enter the mitochondria and be converted into acetyl-CoA to serve as a precursor for the tricarboxylic acid (TCA) cycle. Separately, pyruvate can be reduced to lactate in the cytoplasm, allowing the recycling of NADH back into NAD+, which is essential for glycolysis [28]. Once it crosses the plasma membrane, EP might provide exogenous pyruvate to further fuel cell metabolism. Additionally, EP might influence cellular energy production through its aforementioned activating effects on Nrf2, since Nrf2 is involved in regulating cell metabolism and can promote glycolysis, stimulate amino acid metabolism or regulate lipid metabolism, among other effects [29]. Because of this, numerous studies have looked into the possible effects of EP on cell metabolism.
When the protective effects of EP and pyruvate were compared in a study performed on neonatal rat brain slices exposed to oxidative stress, the results showed that EP was more beneficial, and that it provided metabolic protection of ATP levels. It was also found that the application of 13C-labeled EP led to the production of the same TCA metabolites as when 13C-pyruvate was used, which indicated that the distinctive pharmacology of EP is at least partially based on its ability to enter the cells more rapidly [4]. This study demonstrated that EP can be used as a credible metabolic substrate. However, with a higher concentration of glucose in the substrate the brain slices were exposed to, EP contribution to energy metabolism was not overly significant, if not redundant [30]. Still, EP also prevented hydrogen peroxide-induced reduction of ATP and hexokinase (a glycolytic enzyme) activity in renal tubular endothelial cells [31]. Excessive ROS can impair mitochondria by inducing mutations in mitochondrial DNA or damaging the mitochondrial respiratory chain [32], which can lead to dysfunctional oxidative phosphorylation. Thus, it is quite possible that EP can help maintain cellular energy production by diminishing oxidative stress.
Treatment with EP prevented ATP depletion in the skeletal muscle in a mouse model of hind-limb ischemia–reperfusion injury [33]. Conversely, there were no significant changes in phosphoenergetics in the liver or hind limb in an ischemia–reperfusion model in pigs resuscitated with Ringer’s solution containing EP [34]. EP administration increased myocardial ATP levels in an off-pump coronary bypass model [10], and it also effectively modulated the energy metabolism in the liver of septic mice, reducing the sepsis-induced depletion of ATP, total adenylate, and energy charge levels (a parameter of cellular energy-rich phosphate binding) [35]. In a transient cerebral ischemia model, continuous perfusion with 13C-succinate helped show that the EP treatment enhanced the mitochondrial energy metabolism in the rat brain. EP raised the levels of several 13C-labeled TCA cycle intermediates, indicating their de novo synthesis, while raising endogenous TCA and purine metabolites levels [36], which showed that EP can potentiate energy production in vivo as well.
Since EP is known to possess a wide range of immunomodulatory abilities, studies were conducted to investigate the possible effects of EP on immune cell metabolism. While DC activated by LPS make a metabolic switch from oxidative phosphorylation to glycolysis, without proliferating [37], EP inhibited that switch in murine DC generated in culture and decreased mitochondrial respiration and subsequent ATP production, thus inhibiting their activation [38]. On the other hand, in vitro differentiated regulatory T cells (Treg) proliferated more when cultivated in the presence of EP, and were characterized by enhanced glycolysis (through hexokinase-1 upregulation) which resulted in stimulated ATP production [39]. T cell activation also requires a switch from oxidative phosphorylation to glycolysis, necessary to meet the metabolic demands of proliferation [40]. This suggests that EP might affect different signaling pathways depending on the type of immune cell and their proliferative capacity. That might be of importance for its possible therapeutic application, as immunometabolic reprogramming is crucial during the process of mounting an inflammatory response. As the pro- or anti-inflammatory capacity of different immune cells can be determined by their metabolic stage, pharmacological targeting of immunometabolic reprogramming could represent a way to tackle excessive inflammation [41].
EP makes the immune system walk the line
The influence of EP on signaling in immune cells
In addition to being a metabolic fuel for the cells, EP influences immune cells in ways largely unrelated to metabolism modulation. The effects of EP on immune cells are mostly anti-inflammatory and they are depicted by its impact on versatile intracellular molecular mechanisms and signaling pathways relevant for functional properties of various immune cells. In this review, the effects of EP on the immune system at the molecular and cellular level will be dissected.
Generally, it is thought that EP acts through the inhibition of the alarmin HMGB1 which acts as a damage-associated molecular pattern. As HMGB1 is primarily a nuclear protein, its presence in the intercellular environment is sensed by immune cells as a signal that cellular stress and damage are occurring. Indeed, HMGB1 released from the damaged cells binds to receptors present on immune cells, including the receptor for advanced glycation end products (RAGE), and Toll-like receptors (TLR) 2 and 4, thereby recruiting the immune system to initiate an inflammatory response to remove the damaged cells [42]. Although the inflammatory reaction is beneficial, it is well-known that in certain cases the inflammatory processes may become uncontrolled and lead to further tissue destruction, ultimately causing acute organ failure, as observed in acute respiratory distress syndrome or sepsis [43]. Furthermore, prolonged and uncontrolled inflammation is associated with the development of autoimmunity [44, 45]. It was found that EP inhibited HMGB1 translocation from the nucleus to the cytoplasm in RAW 264.7 macrophages and murine microglial cells in vitro [46, 47]. Also, EP inhibited nucleocytoplasmic translocation of HMGB1 in porcine circovirus type 2-infected swine macrophage cell lines, thus acting against viral replication in the cells [48]. In addition, EP blocked the release of HMGB1 from peritoneal murine macrophages primed with LPS and stimulated with ATP [49]. Suppression of HMGB1 release from the cells was associated with the inhibition of HMGB1 phosphorylation and acetylation in activated microglial cells and macrophages, respectively [50, 51]. The inhibition of HMGB1 acetylation in macrophages was a consequence of upregulation of SIRT1 signaling molecule which inhibited the phosphorylation of STAT1 [51]. The beneficial effects of EP in a model of central nervous system (CNS) autoimmunity were presumably associated with the inhibition of HMGB1 release, reflected by dominant cytoplasmic localization of HMGB1 in macrophages/microglia in the CNS [52]. Finally, EP was shown to be able to inhibit HMGB1 expression during CNS autoimmunity, in the macrophages/microglia in the CNS, as well as within mesenteric lymph nodes [52]. Thus, EP acts on HMGB1 at multiple levels and differently in diverse cells and milieus.
Another target of EP is one of the key inflammatory transcription factors—NF-κB. It was shown that EP inhibited the activation of NF-κB in astrocytes stimulated with IFN-γ and IL-17 [53]. EP also decreased NF-κB DNA-binding activity in LPS-stimulated macrophages through covalent binding to the p65 subunit at Cys(38) of NF-κB, without affecting the degradation of IκBα or IκBβ [54]. The net effect of NF-κB inhibition is probably the downregulation of related genes expression, such as TLR4 in macrophages [55].
MAPK also represent a target for EP action. It was documented that EP reduced the levels of phospho-p38 and phospho-ERK1/2 MAPK in the jejunum of S. typhimurium-infected mice, as well as in the myocardium of ischemia/reperfusion injured rat hearts [55, 56]. Also, EP inhibited ERK1/2 phosphorylation in LPS-stimulated murine DC, as well as p38 and ERK1/2 in human neutrophils and in a porcine enterocyte cell line IPEC-J2 [38, 57, 58]. Still, activation of p38 MAPK in RAW 264.7 macrophages by EP was observed in association with the upregulation of HO-1 [22], thus showing that the effect of EP on MAPK signaling does not always have to be negative.
Further, EP significantly reduced caspase 11 and gasdermin D action and thereby inhibited LPS-induced pyroptosis in macrophages [59]. In this way, EP limited the unwanted macrophage cell death during infection which promotes infection spreading. Finally, EP inhibited caspase 1-dependent NOD-like receptor 3 (NLRP3) inflammasome activation in murine and human macrophages [49]. It was shown that EP attenuated mitochondrial damage and consequently reduced the cytoplasmic level of mitochondrial DNA, which is a well-known activator of NLRP3 [49]. EP also inhibited the NLRP3 inflammasome in murine microglial cells primed with LPS and stimulated with nigericin in vitro [60]. Moreover, it inhibited the NLRP3 inflammasome in the hippocampus of mice affected by sepsis-associated encephalopathy (SAE) and in the myocardium of ischemia/reperfusion heart injury model in rats in vivo [56, 60].
The influence of EP on myeloid cells
Macrophage activation is severely impaired under the influence of EP in vitro and in vivo. Specifically, in vitro treatment with EP down-regulated pro-inflammatory IL-12, IL-6, and TNF production, iNOS expression and NO release, as well as ROS generation in LPS-stimulated murine macrophages [46, 53, 54]. Also, EP downregulated the expression of MHC class II and CD11b molecules in LPS-stimulated murine macrophages [53]. Further, EP treatment of S. typhimurium-infected macrophages decreased the levels of the Il-6, Il-1β and Tnf mRNA [55]. EP application reduced the number of activated macrophages/microglia (ED1+/Iba1+) in the CNS of rats with experimental autoimmune encephalomyelitis (EAE), an animal model of CNS autoimmunity [52]. However, EP did not affect the ratio between M1 pro-inflammatory and M2 anti-inflammatory macrophages during type 1 diabetes (T1D) in mice [61].
The effect of EP on DC is primarily tolerogenic. Application of EP in T1D in mice increased the number of CD11c+CD11b−CD103+ tolerogenic DC within the pancreatic tissue [61]. Direct evidence about EP ability to induce a tolerogenic phenotype in DC was obtained in our study performed on murine and human DC [62]. Bone marrow-derived cells obtained from mice and peripheral blood monocytes obtained from humans were differentiated into DC. The addition of EP to the cultures of monocytes during the process of differentiation to DC led to a marked decrease in expression of MHC class II molecules and co-stimulatory molecules CD86 and CD83 in DC exposed to maturation stimuli [62]. Thus, these cells had an inadequate capacity of antigen-presentation and T cell activation, which was also proven by the limited ability of EP-treated DC to stimulate an allogeneic T cell response. Importantly, the effect that EP exerted in human DC cultures was comparable to the well-known tolerogenic agent vitamin D3 [62]. It is also worth mentioning that EP was equally efficient in inducing tolerance in DC that were obtained from healthy individuals and in those from multiple sclerosis patients. Tolerogenic effects of EP on DC were also investigated in a study that was dedicated to the metabolic aspects of DC biology [38]. There, it was shown that EP promoted tolerogenic properties of DC by down-regulating the expression of maturation-related TLR7 and TLR9 through a decrease of glycolysis and mitochondrial respiration [38].
The influence of EP on T cells
An early report on the effect of EP on T cell biology came from a study on the influence of EP on thermal injury in rats. The injury impaired T cell capacity to proliferate, to utilize the nuclear factor of activated T cells (NFAT) signaling, and to express IL-2, while EP was shown to restore these T cell activities [63]. This effect of EP on T cells may be explained by its direct metabolic effect on T cells, as it could boost their metabolic needs [40]. The effect could also be indirect through its interference with HMGB1, as systemic HMGB1 levels were decreased in EP-treated rats. Indeed, HMGB1 was shown to potentiate Treg suppressive functions, and to limit proliferation and activity of conventional T cells [64]. Accordingly, in another study on the effects of EP on thermal injury, the suppressive activity of Treg, as well as their IL-10 production and CTLA-4 and FoxP3 expression were reduced under the influence of EP [65]. However, there are also reports that EP promotes the generation of Treg and inhibits pro-inflammatory CD4+ subsets. For instance, EP ameliorated T1D in mice while potentiating Treg [61]. Treg were more able to differentiate from naïve cells and had a higher proliferation rate in EP-treated mice in comparison to Treg from diabetic animals. Treg migration towards the pancreatic region also increased after EP administration along with their ability to specifically target Tbet+ Th1 cells. In addition, Treg from EP-treated mice exerted higher suppressive effects towards effector T cells, which was probably mediated through the enhanced CTLA-4 expression and IL-10 production. In vitro treatment of CD4+ T cells with EP suggested that this high suppressive ability might also be a consequence of increased expression of CTLA-4, GITR and PD-1 on Treg [61]. This effect of EP on Treg did not seem to have any relation to HMGB1 downregulation in Treg (our unpublished observations), but was rather a consequence of a stimulatory effect on glycolysis, i.e. EP probably provided sufficient amounts of energy for Treg proliferation and suppressive activity [39]. In vitro treatment with EP, when applied during the Treg differentiation process, increased the number of Treg, but also increased ROS production per cell [39]. This contradictory effect of EP might be actually explained by its transient ROS-scavenging activity followed by a relapse to the “normal” Treg state characterized by high ROS levels. In addition to these effects of EP both in vitro and during T1D pathogenesis, EP successfully stimulated Treg proliferation when given to healthy mice either intraperitoneally or orally [39].
In a colitis model in mice, treatment with EP downregulated the number of Th17 cells in the intestine, and it decreased both Th1 and Th17 numbers in the spleen and mesenteric lymph nodes [66]. Furthermore, its application in EAE ameliorated the disease and reduced IL-17 production in the cells infiltrating the CNS of the animals [53]. Moreover, IFN-γ and IL-17 release from human peripheral blood T cells challenged with purified protein derivative or tetanus toxoid, i.e. vaccine antigens, was inhibited by EP in vitro [53]. In accordance, in vitro application of EP inhibited the expression of RORγt and suppressed the differentiation of murine CD4+ T cells into Th17 cells [67].
It has to be noted that systemic application of EP did not result in a systemic effect on Th cells in animal models of T1D and rheumatoid arthritis (RA). Intraperitoneal EP administration did not affect the proportions of spleen Th1, Th2 or Th17 subsets in T1D mice [39], nor did it change Th1 and Th17 proportion in the spleen of mice with collagen-induced arthritis (CIA) [67].
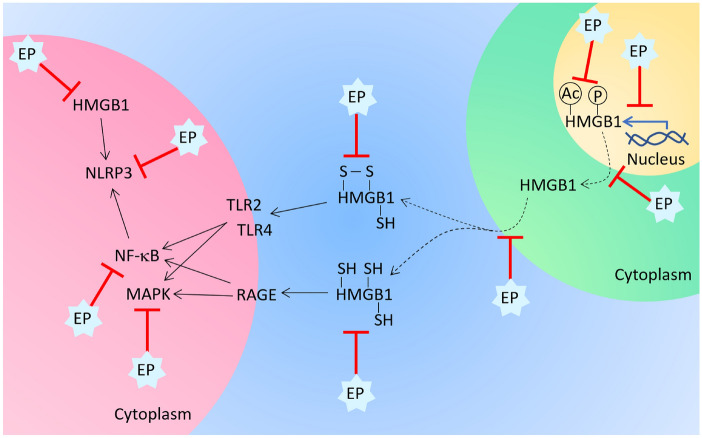
To summarize, EP has the ability to modulate multiple inflammatory signaling pathways in immune cells (Fig. 1). Its restrictive and modulatory effects on macrophages, DC and T cells are well documented and have profound importance for its beneficial influence observed in various models of autoimmune and chronic inflammatory disorders, as will be discussed in detail in the following sections.
Fig. 1.
Effects of EP on signaling in immune cells and on HMGB1. EP affects HMGB1 on multiple levels. It reduces HMGB1 mRNA expression, HMGB1 translocation from the nucleus into the cytoplasm, phosphorylation and acetylation of HMGB1, and its release from the cells. Also, EP influences the HMGB1 redox status, as it modulates the reduction of HMGB1 cysteines. Depending on the cysteine reduction state, HMGB1 acts through RAGE or TLR to stimulate NF-κB and MAPK signaling, and these signaling pathways can also be inhibited by EP. TLR engagement by HMGB1 leads to activation of NLRP3 inflammasome. NLRP3 is also activated by intracellular HMGB1. EP is able to inhibit both ways of NLRP3 activation
Chemical David for the autoimmune Goliath
EP in animal models
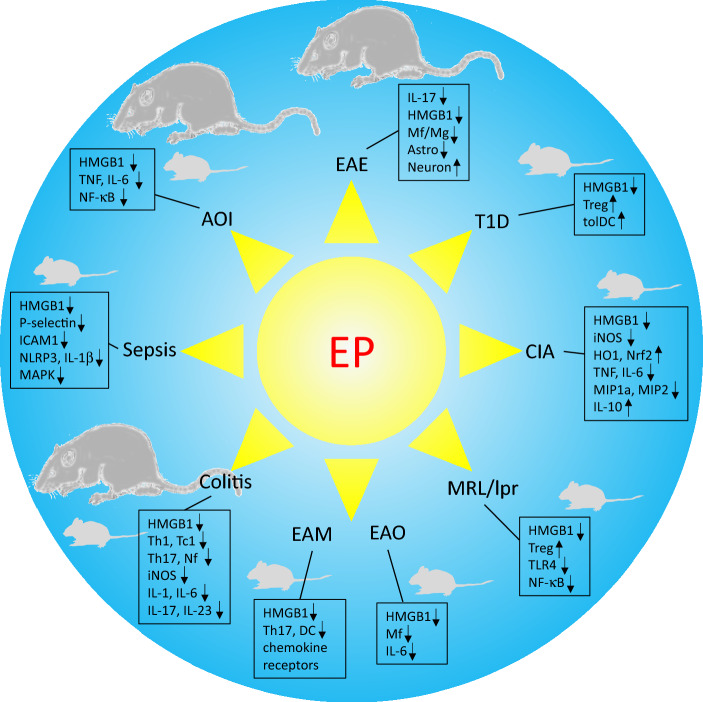
EP has been tested as a potential therapeutic in various animal models of autoimmune and inflammatory diseases. Some of the prominent examples of its efficacy in ameliorating such diseases are presented in the following text and in Fig. 2.
Fig. 2.
Effects of EP in animal models of autoimmunity and inflammation. Effects of EP on autoimmunity and inflammation have been explored in various animal models. For each of the models the main findings are listed. Rat and mouse symbols indicate whether data were obtained in rat or mouse animal models. AOI: acute organ injury, Astro: astrocyte, CIA: collagen-induced arthritis, EAE: experimental autoimmune encephalomyelitis, EAM: experimental autoimmune myocarditis, EAO: experimental autoimmune orchitis, Mf: macrophage, Mg: microglia, T1D: type 1 diabetes
EAE is a widely used animal model of multiple sclerosis, a chronic, inflammatory, and autoimmune disease of the CNS [68]. When our group applied EP in the effector phase of EAE in rats, EP significantly ameliorated the disease via downregulation of the Th1/Th17 axis [53]. In vivo effects of EP on EAE were accomplished through a reduction of infiltrates within the CNS and a lowered number of activated macrophages/microglia and proliferating astrocytes. Moreover, inhibition of HMGB1 production in activated macrophages/microglia within the CNS was also notable [52]. Anti-encephalitogenic effects of EP were mirrored in immunomodulatory effects in the gut-associated lymphoid tissue, as EP reduced both the number of activated CD4+ T cells and antigen-presenting cells and the expression of Th1/Th17-related molecules in mesenteric lymph nodes and Peyer’s patches [52]. The neuroprotective potential of EP was also investigated in cuprizone-induced demyelinating model of multiple sclerosis in mice [69]. There, treatment with EP led to the accumulation of astrocytes in the myelin sheath. In vivo and in vitro studies demonstrated that the accumulated astrocytes promoted the phagocytosis of myelin debris. Importantly, the EP treatment converted astrocytes into myelinating cells and therefore promoted remyelination [69]. In vitro results of the same group showed that EP improved microglia migration and augmented the phagocytosis of myelin debris by BV2 microglia and primary microglia. Notably, EP redirected microglia towards an M2 phenotype [70]. Accordingly, we showed that even extremely short exposure of microglial cells to EP (as short as 10 min) inhibited their inflammatory properties, such as production of IL-6, TNF and NO [71].
Our group also investigated EP in an animal model of T1D, an autoimmune disease that is characterized by the death of insulin-producing pancreatic β-cells [72], and consequent loss of blood sugar level regulation [73]. EP, applied prophylactically to mice treated with multiple low-doses of streptozotocin for T1D induction, reduced the disease development, as well as the number of islets with mononuclear infiltrates, while functional insulin-expressing β-cells were preserved in the treated animals [61]. Interestingly, HMGB1 expression in β-cells was successfully suppressed with EP treatment. However, the mechanism of EP protective action was largely attributed to the increased proportion of tolerogenic DC and Treg in the pancreatic infiltrates and surrounding lymph nodes and to the specific stimulation of Treg migration, proliferation and suppressive functions [61]. Diabetic nephropathy is one of T1D associated comorbidities, characterized by the oxidative stress-mediated accumulation of extracellular matrix proteins in the glomeruli and the renal interstitium which leads to kidney failure [16, 74]. Treatment with EP inhibited glomerular NADPH oxidase and therefore protected against kidney injury in an animal model of diabetic nephropathy. Also, the antioxidant effect of EP was shown beneficial in lessening the damage of renal structures in streptozotocin-induced diabetes in rats [74].
RA is characterized by chronic inflammation of multiple joints, and consequent joint cartilage and bone destruction [75]. CIA is a widely used animal model of RA as it has many of the characteristics of the human autoimmune disease [76]. EP treatment of mice with CIA led to marked reduction of disease incidence and significantly reduced the hind paw swelling [77]. Furthermore, expression of chemokines, such as macrophage inflammatory protein 1a and 2 (MIP1a and MIP2), and neutrophil infiltration into inflamed joints were significantly reduced in the EP-treated mice. EP also decreased the plasma levels of pro-inflammatory cytokines while increasing the level of anti-inflammatory IL-10. Immunohistochemical analysis of the joints showed a significant reduction of iNOS staining in the treated animals. Furthermore, expression of antioxidant and cytoprotective HO-1 and Nrf2 was increased in the nuclei of the cells in the synovial space (such as fibroblasts) and chondrocytes in the joints of animals treated with EP [77]. In an additional study, the beneficial effect of EP in CIA was explained by a suppression of Th17 cells and inhibition of RORγt expression, as well as by a reduction of HMGB1 expression in the synovium [67].
Systemic lupus erythematosus (SLE) is a multi-systematic chronic autoimmune disorder that affects multiple organs [78]. To the best of our knowledge, only one paper has been published so far regarding the application of EP in an animal model of SLE [79]. The authors showed that treatment of MRL/lpr mice with EP successfully ameliorated the disease. Namely, the treatment improved the survival rate and alleviated the lupus nephritis by lowering the presence of HMGB1 in the serum of MRL/lpr mice. Accordingly, EP decreased the weight loss and the amount of proteins in the urine of the treated animals [79].
The effectiveness of EP was also investigated in experimental autoimmune orchitis (EAO), an animal model of chronic testicular inflammation that leads to infertility [80]. As an immune-privileged place, testes are protected from host immune responses [81], while a break of the immune privilege causes testis-specific autoimmunity [82]. By lowering the number of macrophages and reducing the levels of HMGB1 and IL-6 in the testis, EP treatment inhibited testicular inflammation and reduced EAO progression [83].
We have recently shown that EP is effective in experimental autoimmune myocarditis (EAM) [84]. EP alleviated heart inflammation, and CD11c+ antigen-presenting cells and Th17 cells were identified as the most prominent targets of EP activity in EAM. Moreover, HMGB1 expression and expression of various chemokine receptors were downregulated in the heart of EP-treated EAM mice [84].
EP was also investigated in the context of animal models of inflammatory bowel disease (IBD), a chronic inflammatory disorder of the intestine that leads to chronic intestinal damage due to the overproduction of ROS and inflammatory mediators [66, 85]. In a rat model of TNBS-induced colitis, treatment with EP suppressed the inflammatory mediators and significantly recovered the intestinal mucosa [86]. It was also shown that EP inhibited HMGB1 expression in both the serum and the colon and ameliorated the disease in a mouse model of IBD [46, 87]. Furthermore, the amelioration of colitis in mice was also related to EP-imposed reduction in Th1/Th17 activation [66].
Sepsis is a life-threatening state of acute inflammation caused by infection [88]. Numerous studies have shown that the beneficial effects of EP in animal models of sepsis were related to its HMGB1-inhibiting activity [22, 89, 90]. Further, EP efficiently reduced the inflammation in the mesenteric microcirculation via downregulation of P-selectin and intercellular adhesion molecule-1 (ICAM-1) in septic rats [91]. In a cecal ligation and puncture (CLP) model of sepsis, EP was shown to reduce the mortality of rats, and it also reduced mitochondrial swelling and dysfunction, as well as the mitochondrial expression of aquaporin-8, a water channel protein that significantly contributed to mitochondrial swelling [92]. Similar results were obtained in another study on a mouse CLP model, as EP efficiently ameliorated intestinal damage and increased the survival rate [35]. Furthermore, EP reduced the inflammatory response, oxidative damage, and metabolic acidosis in septic mice [35]. There are several other studies also showing remarkable effects of EP in animal models of sepsis [57, 59, 93].
EP was also shown to be effective in the treatment of various sepsis-associated diseases, such as intestinal damage or SAE. EP decreased the formation of neutrophil extracellular traps and alleviated sepsis-induced intestinal damage via inhibition of ROS-induced activation of MAPK ERK1/2 and p38 in a mouse sepsis model [57]. Activation of the inflammasome is a crucial step in the development of SAE [94–96]. After the administration of EP in a mouse model of SAE, NLRP3 inflammasome activation and IL-1β release from the microglia were significantly inhibited, while the cognitive decline was attenuated and neurogenesis was improved [60].
Additionally, EP was shown to ameliorate organ dysfunctions in various animal models [2, 97]. A number of acute organ injuries are related to the overexpression of HMGB1 [98]. For example, an exogenous HMGB1 injection caused liver damage in healthy mice [99]. It has been shown that HMGB1 contributes to renal ischemia–reperfusion injury [100], sepsis-induced kidney injury [101], severe acute pancreatitis-related kidney or lung injuries [102, 103], hemorrhagic shock-related acute lung injury [104], hypoxia-induced acute lung injury [105], and gut-mucosal injury [99]. Thus, the inhibitory effects of EP on HMGB1 can be beneficial in these conditions. Indeed, EP significantly alleviated pancreatic injury and necrosis by inhibiting inflammatory cell infiltration, expression of HMGB1 and pro-inflammatory cytokines (TNF, IL-6), and pancreatic NF-κB DNA binding [103, 106]. EP also ameliorated the hepatic inflammatory response and hepatic lipid peroxidation in experimental alcoholic liver injury [107], acute liver injury secondary to severe acute pancreatitis [108] and hepatic ischemia–reperfusion injury through its anti-inflammatory and anti-apoptotic mechanisms in mice [109]. Further, EP reduced the hyperoxia-induced acute lung injury [110].
The examples presented above clearly imply that EP is efficient in ameliorating immune-mediated disorders in experimental animals. It is therefore tempting to speculate that it would also be efficient as a therapeutic for human autoimmune and inflammatory disorders.
EP in clinical trials
Having in mind the efficacy of EP in animal models of various autoimmune and chronic inflammatory diseases, it is important to continue its translation into clinical trials. EP is widely used as a food additive and flavoring agent [111], and it is described as having a floral-fruity odor and a sweet and caramel-like taste [112]. So far, there has been only one clinical trial investigating EP, in which the safety and complication prevention in cardiac surgery patients on cardiopulmonary bypass were investigated (NCT00107666). It was a Phase II randomized, double-blind, placebo-controlled, parallel-group, multicenter clinical study. Patients undergoing cardiac surgery received 6 doses intravenously, one administrated before surgery and 5 more administrated every 6 h afterwards, with 102 participants included in the study. Analysis of Phase II data showed that there was no difference between the effectiveness of the placebo or EP in reducing the principal complications, such as death, mechanical ventilation, and/or acute renal failure any time after the first 48 h post-surgery [113]. As a consequence, the study was suspended. However, EP was proven to be safe in both healthy individuals and in patients that underwent cardiopulmonary bypass surgery in the same clinical trial [97].
There is one critical issue that has to be addressed when thinking about translating the application of EP from animal studies to clinical trials—the in vivo activation site of EP. When pyruvate interacts with hydrogen peroxide it forms an unstable intermediate 2-hydroperoxy-2-hydroxypropanoate, which then goes through rearrangement to produce acetate, carbon dioxide, and water. Its rearrangement is initiated by the release of carbon dioxide from the carboxyl group. In EP, the ester formation blocks the pyruvate carboxyl group, thus disabling the rearrangement to form the products listed above. Carboxylesterase is an enzyme that converts EP to pyruvate in vivo and it is uniformly present in mammalian cells. However, not all mammals have this enzyme in the blood plasma. Specifically, it is present in the blood plasma of rodents, but not humans [114, 115]. Therefore, when applied systemically in rodents, EP can be activated in the blood plasma to achieve sufficient extracellular concentration so that the derived pyruvate can reduce extracellular H2O2. However, in humans, EP can be activated only in the intracellular environment. The generated pyruvate will thus have little impact on hydrogen peroxide levels because pyruvate is rapidly metabolized. This can be one explanation for the discordance between the results obtained in animal and human studies [116]. Of course, not all of the beneficial effects of EP depend on its interaction with hydrogen peroxide, as explained in detail in the previous sections. Along this line, EP was shown effective in the treatment of hemorrhage in pigs, animals that, like humans, do not have carboxylesterase present in the blood plasma [117]. Namely, treatment with EP prevented inflammatory responses and organ damage by inhibiting TNF and HMGB1 serum levels, by reducing NF-κB activation in the spleen, and through restriction of cytokine production and myelopyroxidase activity in the terminal ileum [118]. EP was also efficient in the treatment of the swine model of cardiac arrest, and in a porcine model of resuscitated hyperdynamic endotoxemia [119, 120]. Furthermore, EP was not consistently efficient in horses, animals that, like rodents, have carboxylesterase present in the blood plasma [117]. While EP showed beneficial effects in a horse model of endotoxemia, it did not have a significant effect on postoperative variables in horses subjected to large colon volvulus surgery [121–123]. Thus, there is more to the effects of EP in vivo then its activation site. Its inefficiency in the cardiac surgery clinical trial should not prevent its clinical testing in autoimmune and chronic inflammatory disorders. Moreover, there is an option of an indirect utilization of EP in the treatment of such disorders, i.e. a tolerogenic cell-based therapy with immune cells conditioned with EP in vitro. Indeed, EP was shown to induce tolerogenic properties in human DC, including those obtained from multiple sclerosis patients [62]. Thus, further exploration of the application of EP-treated DC in the therapy of multiple sclerosis and other autoimmune diseases is warranted.
Conclusions
This review clearly presents potent immunomodulatory properties of EP, a Jack of all trades, a molecule able to modulate redox processes, metabolism and immune reactivity in living organisms. Immunomodulatory activity of EP is based both on its redox-related and -unrelated effects on the cells of the immune system. Notably, many of the observed effects are mediated through the influence of EP on HMGB1, which seems to be the crucial target of EP during the immune response. Importantly, EP has been shown able to act on each of the steps in HMGB1 biology, including its transcription, translocation from the nucleus into the cytoplasm, export from the cells, extracellular redox modifications, signaling downstream of its membrane receptors, and its direct intracellular interactions with other biomolecules. HMGB1 is one of the main inflammatory mediators and its regulation is the key for restraining over-reactivity of the immune system. Thus, through its actions upon HMGB1, but also upon many other relevant biomolecules, EP makes the immune system walk the line. Accordingly, EP has been shown effective in amelioration of inflammatory disorders. Studies cited in this review clearly show that EP is effective in various autoimmune diseases, sepsis, and inflammatory bowel disease. Thus, we can say that EP is a chemical David for the autoimmune Goliath. Moreover, EP could be considered as the molecule of choice for the therapy of other disorders with profound inflammatory nature, such as atopy and asthma, or acute respiratory distress syndrome (ARDS). While the influence of EP on the former two has already been investigated [124, 125], its effects on the latter are still unknown. Our ongoing research on a murine model of ARDS is giving promising results which indicate that EP could be a useful therapeutic in ARDS. This has a special significance, having in mind the current reality of SARS-Cov2 pandemic, and ARDS as one of the life-threatening consequences of the infection [126]. Thus, intensifying this specific line of investigation, as well as widening the focus of EP research over the spectra of inflammation-related diseases are viable research options. As a final point, translation of EP into clinical trials of autoimmune and chronic inflammatory diseases should be the ultimate goal of future studies.
Acknowledgements
This work was supported by Ministry of Education, Science and Technological Development of Republic of Serbia #451-03-9/2021-14/200007.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Das UN. Is pyruvate an endogenous anti-inflammatory molecule? Nutrition. 2006;22(9):965–972. doi: 10.1016/j.nut.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Kao KK, Fink MP. The biochemical basis for the anti-inflammatory and cytoprotective actions of ethyl pyruvate and related compounds. Biochem Pharmacol. 2010;80(2):151–159. doi: 10.1016/j.bcp.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Shin JH, Kim ID, Kim SW, Lee HK, Jin Y, Park JH, et al. Ethyl pyruvate inhibits HMGB1 phosphorylation and release by chelating calcium. Mol Med. 2015;20(1):649–657. doi: 10.2119/molmed.2014.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeng J, Liu J, Yang GY, Kelly MJ, James TL, Litt L. Exogenous ethyl pyruvate versus pyruvate during metabolic recovery after oxidative stress in neonatal rat cerebrocortical slices. Anesthesiology. 2007;107(4):630–640. doi: 10.1097/01.anes.0000281898.01966.1e. [DOI] [PubMed] [Google Scholar]
- 5.Newsholme P, Cruzat VF, Keane KN, Carlessi R, de Bittencourt Jr PI. Molecular mechanisms of ROS production and oxidative stress in diabetes. Biochem J. 2016;473(24):4527–4550. doi: 10.1042/BCJ20160503C. [DOI] [PubMed] [Google Scholar]
- 6.Sharifi-Rad M, Anil Kumar NV, Zucca P, Varoni EM, Dini L, Panzarini E, et al. Lifestyle, oxidative stress, and antioxidants: back and forth in the pathophysiology of chronic diseases. Front Physiol. 2020;11:694. doi: 10.3389/fphys.2020.00694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoshida Y, Umeno A, Shichiri M. Lipid peroxidation biomarkers for evaluating oxidative stress and assessing antioxidant capacity in vivo. J Clin Biochem Nutr. 2013;52(1):9–16. doi: 10.3164/jcbn.12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tawadrous ZS, Delude RL, Fink MP. Resuscitation from hemorrhagic shock with Ringer's ethyl pyruvate solution improves survival and ameliorates intestinal mucosal hyperpermeability in rats. Shock. 2002;17(6):473–477. doi: 10.1097/00024382-200206000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Tsung A, Kaizu T, Nakao A, Shao L, Bucher B, Fink MP, Murase N, Geller DA. Ethyl pyruvate ameliorates liver ischemia-reperfusion injury by decreasing hepatic necrosis and apoptosis. Transplantation. 2005;79(2):196–204. doi: 10.1097/01.tp.0000151681.07474.2e. [DOI] [PubMed] [Google Scholar]
- 10.Taylor MD, Grand TJ, Cohen JE, Hsu V, Liao GP, Zentko S, et al. Ethyl pyruvate enhances ATP levels, reduces oxidative stress and preserves cardiac function in a rat model of off-pump coronary bypass. Heart Lung Circ. 2005;14(1):25–31. doi: 10.1016/j.hlc.2004.12.021. [DOI] [PubMed] [Google Scholar]
- 11.Karabeyoğlu M, Unal B, Bozkurt B, Dolapçi I, Bilgihan A, Karabeyoğlu I, Cengiz O. The effect of ethyl pyruvate on oxidative stress in intestine and bacterial translocation after thermal injury. J Surg Res. 2008;144(1):59–63. doi: 10.1016/j.jss.2007.02.050. [DOI] [PubMed] [Google Scholar]
- 12.Kelle I, Akkoc H, Tunik S, Nergiz Y, Erdinc M, Erdinc L. Protective effects of ethyl pyruvate in cisplatin-induced nephrotoxicity. Biotechnol Biotechnol Equip. 2014;28(4):674–680. doi: 10.1080/13102818.2014.942489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang P, Gong G, Wei Z, Li Y. Ethyl pyruvate prevents intestinal inflammatory response and oxidative stress in a rat model of extrahepatic cholestasis. J Surg Res. 2010;160(2):228–235. doi: 10.1016/j.jss.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 14.Teskey G, Abrahem R, Cao R, Gyurjian K, Islamoglu H, Lucero M, et al. Glutathione as a marker for human disease. Adv Clin Chem. 2018;87:141–159. doi: 10.1016/bs.acc.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Chavali VD, Agarwal M, Vyas VK, Saxena B. Neuroprotective effects of ethyl pyruvate against aluminum chloride-induced alzheimer's disease in rats via inhibiting toll-like receptor 4. J Mol Neurosci. 2020;70(6):836–850. doi: 10.1007/s12031-020-01489-9. [DOI] [PubMed] [Google Scholar]
- 16.Ju KD, Shin EK, Cho EJ, Yoon HB, Kim HS, Kim H, et al. Ethyl pyruvate ameliorates albuminuria and glomerular injury in the animal model of diabetic nephropathy. Am J Physiol Renal Physiol. 2012;302(5):F606–F613. doi: 10.1152/ajprenal.00415.2011. [DOI] [PubMed] [Google Scholar]
- 17.Famili A, Ammar DA, Kahook MY. Ethyl pyruvate treatment mitigates oxidative stress damage in cultured trabecular meshwork cells. Mol Vis. 2013;19:1304–1309. [PMC free article] [PubMed] [Google Scholar]
- 18.Shin JH, Kim SW, Jin Y, Kim ID, Lee JK. Ethyl pyruvate-mediated Nrf2 activation and hemeoxygenase 1 induction in astrocytes confer protective effects via autocrine and paracrine mechanisms. Neurochem Int. 2012;61(1):89–99. doi: 10.1016/j.neuint.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 19.Kładna A, Marchlewicz M, Piechowska T, Kruk I, Aboul-Enein HY. Reactivity of pyruvic acid and its derivatives towards reactive oxygen species. Luminescence. 2015;30(7):1153–1158. doi: 10.1002/bio.2879. [DOI] [PubMed] [Google Scholar]
- 20.Rossmann C, Nusshold C, Paar M, Ledinski G, Tafeit E, Koestenberger M, et al. Ethyl pyruvate inhibits oxidation of LDL in vitro and attenuates oxLDL toxicity in EAhy926 cells. PLoS ONE. 2018;13(1):191477. doi: 10.1371/journal.pone.0191477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song M, Kellum JA, Kaldas H, Fink MP. Evidence that glutathione depletion is a mechanism responsible for the anti-inflammatory effects of ethyl pyruvate in cultured lipopolysaccharide-stimulated RAW 264.7 cells. J Pharmacol Exp Ther. 2004;308(1):307–316. doi: 10.1124/jpet.103.056622. [DOI] [PubMed] [Google Scholar]
- 22.Jang HJ, Kim YM, Tsoyi K, Park EJ, Lee YS, Kim HJ, et al. Ethyl pyruvate induces heme oxygenase-1 through p38 mitogen-activated protein kinase activation by depletion of glutathione in RAW 264.7 cells and improves survival in septic animals. Antioxid Redox Signal. 2012;17(6):878–889. doi: 10.1089/ars.2011.3994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim SW, Lee HK, Shin JH, Lee JK. Up-down regulation of HO-1 and iNOS gene expressions by ethyl pyruvate via recruiting p300 to Nrf2 and depriving It from p65. Free Radic Biol Med. 2013;65:468–476. doi: 10.1016/j.freeradbiomed.2013.07.028. [DOI] [PubMed] [Google Scholar]
- 24.Kim HS, Cho IH, Kim JE, Shin YJ, Jeon JH, Kim Y, et al. Ethyl pyruvate has an anti-inflammatory effect by inhibiting ROS-dependent STAT signaling in activated microglia. Free Radic Biol Med. 2008;45(7):950–963. doi: 10.1016/j.freeradbiomed.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 25.Kwak MS, Kim HS, Lee B, Kim YH, Son M, Shin JS. Immunological significance of HMGB1 post-translational modification and redox biology. Front Immunol. 2020;11:1189. doi: 10.3389/fimmu.2020.01189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsubata T. Involvement of reactive oxygen species (ROS) in BCR signaling as a second messenger. Adv Exp Med Biol. 2020;1254:37–46. doi: 10.1007/978-981-15-3532-1_3. [DOI] [PubMed] [Google Scholar]
- 27.Biswas SK. Does the interdependence between oxidative stress and inflammation explain the antioxidant paradox? Oxid Med Cell Longev. 2016;2016:5698931. doi: 10.1155/2016/5698931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zangari J, Petrelli F, Maillot B, Martinou JC. The multifaceted pyruvate metabolism: role of the mitochondrial pyruvate carrier. Biomolecules. 2020;10(7):1068. doi: 10.3390/biom10071068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.He F, Ru X, Wen T. NRF2, a transcription factor for stress response and beyond. Int J Mol Sci. 2020;21(13):4777. doi: 10.3390/ijms21134777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu J, Segal M, Yoo S, Yang GY, Kelly M, James TL, Litt L. Antioxidant effect of ethyl pyruvate in respiring neonatal cerebrocortical slices after H(2)O(2) stress. Neurochem Int. 2009;54(2):106–110. doi: 10.1016/j.neuint.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 31.Bloom J, Patel N, Wagmaister J, Choudhury M, Eshghi M, Konno S. Prophylactic effect of ethyl pyruvate on renal ischemia/reperfusion injury mediated through oxidative stress. Int Urol Nephrol. 2019;51(1):85–92. doi: 10.1007/s11255-018-2020-9. [DOI] [PubMed] [Google Scholar]
- 32.Guo C, Sun L, Chen X, Zhang D. Oxidative stress, mitochondrial damage and neurodegenerative diseases. Neural Regen Res. 2013;8(21):2003–2014. doi: 10.3969/j.issn.1673-5374.2013.21.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crawford RS, Albadawi H, Atkins MD, Jones JJ, Conrad MF, Austen WG, Jr, et al. Postischemic treatment with ethyl pyruvate prevents adenosine triphosphate depletion, ameliorates inflammation, and decreases thrombosis in a murine model of hind-limb ischemia and reperfusion. J Trauma. 2011;70(1):103–110. doi: 10.1097/TA.0b013e3182031ccb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mulier KE, Beilman GJ, Conroy MJ, Taylor JH, Skarda DE, Hammer BE. Ringer's ethyl pyruvate in hemorrhagic shock and resuscitation does not improve early hemodynamics or tissue energetics. Shock. 2005;23(3):248–252. doi: 10.1097/01.shk.0000153553.58341.ff. [DOI] [PubMed] [Google Scholar]
- 35.Kang H, Mao Z, Zhao Y, Yin T, Song Q, Pan L, et al. Ethyl pyruvate protects against sepsis by regulating energy metabolism. Ther Clin Risk Manag. 2016;12:287–294. doi: 10.2147/TCRM.S97989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nygaard KH, Havelund JF, Nielsen TH, Nordström CH, Færgeman NJ, Poulsen FR, et al. Ethyl pyruvate increases post-ischemic levels of mitochondrial energy metabolites: a 13C-labeled cerebral microdialysis study. Metabolites. 2020;10(7):287. doi: 10.3390/metabo10070287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krawczyk CM, Holowka T, Sun J, Blagih J, Amiel E, DeBerardinis RJ, et al. Toll-like receptor-induced changes in glycolytic metabolism regulate dendritic cell activation. Blood. 2010;115(23):4742–4749. doi: 10.1182/blood-2009-10-249540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chakhtoura M, Chain RW, Sato PY, Qiu CC, Lee MH, Meissler JJ, et al. Ethyl pyruvate modulates murine dendritic cell activation and survival through their immunometabolism. Front Immunol. 2019;10:30. doi: 10.3389/fimmu.2019.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koprivica I, Gajić D, Pejnović N, Paunović V, Saksida T, Stojanović I. Ethyl pyruvate promotes proliferation of regulatory t cells by increasing glycolysis. Molecules. 2020;25(18):4112. doi: 10.3390/molecules25184112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chang CH, Curtis JD, Maggi LB, Jr, Faubert B, Villarino AV, O'Sullivan D, et al. Posttranscriptional control of T cell effector function by aerobic glycolysis. Cell. 2013;153(6):1239–1251. doi: 10.1016/j.cell.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kumar V. Inflammation research sails through the sea of immunology to reach immunometabolism. Int Immunopharmacol. 2019;73:128–145. doi: 10.1016/j.intimp.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 42.Paudel YN, Angelopoulou E, Piperi C, Balasubramaniam VRMT, Othman I, Shaikh MF. Enlightening the role of high mobility group box 1 (HMGB1) in inflammation: updates on receptor signalling. Eur J Pharmacol. 2019;858:172487. doi: 10.1016/j.ejphar.2019.172487. [DOI] [PubMed] [Google Scholar]
- 43.Semeraro N, Ammollo CT, Semeraro F, Colucci M. Sepsis, thrombosis and organ dysfunction. Thromb Res. 2012;129(3):290–295. doi: 10.1016/j.thromres.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 44.Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019;25(12):1822–1832. doi: 10.1038/s41591-019-0675-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Magna M, Pisetsky DS. The role of HMGB1 in the pathogenesis of inflammatory and autoimmune diseases. Mol Med. 2014;20(1):138–146. doi: 10.2119/molmed.2013.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davé SH, Tilstra JS, Matsuoka K, Li F, DeMarco RA, Beer-Stolz D, et al. Ethyl pyruvate decreases HMGB1 release and ameliorates murine colitis. J Leukoc Biol. 2009;86(3):633–643. doi: 10.1189/jlb.1008662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Massey N, Puttachary S, Bhat SM, Kanthasamy AG, Charavaryamath C. HMGB1-RAGE signaling plays a role in organic dust-induced microglial activation and neuroinflammation. Toxicol Sci. 2019;169(2):579–592. doi: 10.1093/toxsci/kfz071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sun R, Sun S, Zhang Y, Zhou Y, Shan Y, Li X, Fang W. PCV2 induces reactive oxygen species to promote nucleocytoplasmic translocation of the viral DNA binding protein HMGB1 to enhance its replication. J Virol. 2020;94(13):e00238–e320. doi: 10.1128/JVI.00238-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li S, Liang F, Kwan K, Tang Y, Wang X, Tang Y, et al. Identification of ethyl pyruvate as a NLRP3 inflammasome inhibitor that preserves mitochondrial integrity. Mol Med. 2018;24(1):8. doi: 10.1186/s10020-018-0006-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shin JH, Lee HK, Lee HB, Jin Y, Lee JK. Ethyl pyruvate inhibits HMGB1 phosphorylation and secretion in activated microglia and in the postischemic brain. Neurosci Lett. 2014;558:159–163. doi: 10.1016/j.neulet.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 51.Kim YM, Park EJ, Kim JH, Park SW, Kim HJ, Chang KC. Ethyl pyruvate inhibits the acetylation and release of HMGB1 via effects on SIRT1/STAT signaling in LPS-activated RAW264.7 cells and peritoneal macrophages. Int Immunopharmacol. 2016;41:98–105. doi: 10.1016/j.intimp.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 52.Djedović N, Stanisavljevic S, Jevtić B, Momčilović M, Lavrnja I, Miljković D. Anti-encephalitogenic effects of ethyl pyruvate are reflected in the central nervous system and the gut. Biomed Pharmacother. 2017;96:78–85. doi: 10.1016/j.biopha.2017.09.110. [DOI] [PubMed] [Google Scholar]
- 53.Miljković D, Blaževski J, Petković F, Djedović N, Momčilović M, Stanisavljević S, et al. A comparative analysis of multiple sclerosis-relevant anti-inflammatory properties of ethyl pyruvate and dimethyl fumarate. J Immunol. 2015;194(6):2493–2503. doi: 10.4049/jimmunol.1402302. [DOI] [PubMed] [Google Scholar]
- 54.Han Y, Englert JA, Yang R, Delude RL, Fink MP. Ethyl pyruvate inhibits nuclear factor-kappaB-dependent signaling by directly targeting p65. J Pharmacol Exp Ther. 2005;312(3):1097–1105. doi: 10.1124/jpet.104.079707. [DOI] [PubMed] [Google Scholar]
- 55.Dong N, Xu X, Xue C, Wang C, Li X, Shan A, et al. Ethyl pyruvate protects against Salmonella intestinal infection in mice through down-regulation of pro-inflammatory factors and inhibition of TLR4/MAPK pathway. Int Immunopharmacol. 2019;71:155–163. doi: 10.1016/j.intimp.2019.03.019. [DOI] [PubMed] [Google Scholar]
- 56.Jun JH, Shim JK, Oh JE, Shin EJ, Shin E, Kwak YL. Protective effect of ethyl pyruvate against myocardial ischemia reperfusion injury through regulations of ROS-related nlrp3 inflammasome activation. Oxid Med Cell Longev. 2019;2019:4264580. doi: 10.1155/2019/4264580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang X, Sun S, Duan Z, Yang C, Chu C, Wang K, et al. Protective effect of ethyl pyruvate on gut barrier function through regulations of ROS-related NETs formation during sepsis. Mol Immunol. 2021;132:108–116. doi: 10.1016/j.molimm.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 58.Dong N, Xu X, Xue C, Wang C, Li X, Bi C, Shan A. Ethyl pyruvate inhibits LPS induced IPEC-J2 inflammation and apoptosis through p38 and ERK1/2 pathways. Cell Cycle. 2019;18(20):2614–2628. doi: 10.1080/15384101.2019.1653106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Qiu X, Cheng X, Zhang J, Yuan C, Zhao M, Yang X. Ethyl pyruvate confers protection against endotoxemia and sepsis by inhibiting caspase-11-dependent cell pyroptosis. Int Immunopharmacol. 2020;78:106016. doi: 10.1016/j.intimp.2019.106016. [DOI] [PubMed] [Google Scholar]
- 60.Zhong X, Xie L, Yang X, Liang F, Yang Y, Tong J, et al. Ethyl pyruvate protects against sepsis-associated encephalopathy through inhibiting the NLRP3 inflammasome. Mol Med. 2020;26(1):55. doi: 10.1186/s10020-020-00181-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Koprivica I, Vujičić M, Gajić D, Saksida T, Stojanović I. Ethyl pyruvate stimulates regulatory T cells and ameliorates type 1 diabetes development in mice. Front Immunol. 2019;9:3130. doi: 10.3389/fimmu.2018.03130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Djedovic N, Mansilla MJ, Jevtić B, Navarro-Barriuso J, Saksida T, Martínez-Cáceres EM, Miljković Ð. Ethyl pyruvate induces tolerogenic dendritic cells. Front Immunol. 2019;10:157. doi: 10.3389/fimmu.2019.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang LT, Yao YM, Dong YQ, Dong N, Yu Y, Sheng ZY. Relationship between high-mobility group box 1 protein release and T-cell suppression in rats after thermal injury. Shock. 2008;30(4):449–455. doi: 10.1097/SHK.0b013e3181672495. [DOI] [PubMed] [Google Scholar]
- 64.Wild CA, Bergmann C, Fritz G, Schuler P, Hoffmann TK, Lotfi R, et al. HMGB1 conveys immunosuppressive characteristics on regulatory and conventional T cells. Int Immunol. 2012;24(8):485–494. doi: 10.1093/intimm/dxs051. [DOI] [PubMed] [Google Scholar]
- 65.Huang LF, Yao YM, Zhang LT, Dong N, Yu Y, Sheng ZY. The effect of high-mobility group box 1 protein on activity of regulatory T cells after thermal injury in rats. Shock. 2009;31(3):322–329. doi: 10.1097/SHK.0b013e3181834070. [DOI] [PubMed] [Google Scholar]
- 66.Guo X, Guo R, Luo X, Zhou L. Ethyl pyruvate ameliorates experimental colitis in mice by inhibiting the HMGB1-Th17 and Th1/Tc1 responses. Int Immunopharmacol. 2015;29(2):454–461. doi: 10.1016/j.intimp.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 67.Jung SM, Lee J, Baek SY, Lee J, Jang SG, Hong SM, et al. Ethyl pyruvate ameliorates inflammatory arthritis in mice. Int Immunopharmacol. 2017;52:333–341. doi: 10.1016/j.intimp.2017.09.027. [DOI] [PubMed] [Google Scholar]
- 68.Constantinescu CS, Farooqi N, O'Brien K, Gran B. Experimental autoimmune encephalomyelitis (EAE) as a model for multiple sclerosis (MS) Br J Pharmacol. 2011;164(4):1079–1106. doi: 10.1111/j.1476-5381.2011.01302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.He Y, An J, Yin JJ, Miao Q, Sui RX, Han QX, et al. Ethyl Pyruvate-derived transdifferentiation of astrocytes to oligodendrogenesis in cuprizone-induced demyelinating model. Neurotherapeutics. 2021;18(1):488–502. doi: 10.1007/s13311-020-00947-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.He Y, An J, Yin JJ, Sui RX, Miao Q, Ding ZB, et al. Ethyl pyruvate enhances spontaneous remyelination by targeting microglia phagocytosis. Int Immunopharmacol. 2019;77:105929. doi: 10.1016/j.intimp.2019.105929. [DOI] [PubMed] [Google Scholar]
- 71.Stanisavljević S, Jevtić B, Djedović N, Miljković D. Short term exposure to ethyl pyruvate has long term anti-inflammatory effects on microglial cells. Biomed Pharmacother. 2015;72:11–16. doi: 10.1016/j.biopha.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 72.DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;391(10138):2449–2462. doi: 10.1016/S0140-6736(18)31320-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Meetoo D, McGovern P, Safadi R. An epidemiological overview of diabetes across the world. Br J Nurs. 2007;16(16):1002–1007. doi: 10.12968/bjon.2007.16.16.27079. [DOI] [PubMed] [Google Scholar]
- 74.Bahadir MV, Yildirim Y, Baran OP, Polat S, Akkoc H, Tunik S. The potential beneficial effects of ethyl pyruvate on diabetic nephropathy: an experimental and ultrastructural study. Pol J Pathol. 2016;67(3):250–257. doi: 10.5114/pjp.2016.63777. [DOI] [PubMed] [Google Scholar]
- 75.McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365(23):2205–2219. doi: 10.1056/NEJMra1004965. [DOI] [PubMed] [Google Scholar]
- 76.Brand DD, Latham KA, Rosloniec EF. Collagen-induced arthritis. Nat Protoc. 2007;2(5):1269–1275. doi: 10.1038/nprot.2007.173. [DOI] [PubMed] [Google Scholar]
- 77.Di Paola R, Mazzon E, Galuppo M, Esposito E, Bramanti P, Fink MP, Cuzzocrea S. Ethyl pyruvate therapy attenuates experimental severe arthritis caused by type II collagen (CII) in the mouse (CIA) Int J Immunopathol Pharmacol. 2010;23(4):1087–1098. doi: 10.1177/039463201002300413. [DOI] [PubMed] [Google Scholar]
- 78.Shen B, Feng G, Tang W, Huang X, Yan H, He Y, et al. The quality of life in Chinese patients with systemic lupus erythematosus is associated with disease activity and psychiatric disorders: a path analysis. Clin Exp Rheumatol. 2014;32(1):101–107. [PubMed] [Google Scholar]
- 79.Ji J, Fu T, Dong C, Zhu W, Yang J, Kong X, et al. Targeting HMGB1 by ethyl pyruvate ameliorates systemic lupus erythematosus and reverses the senescent phenotype of bone marrow-mesenchymal stem cells. Aging (Albany) 2019;11(13):4338–4353. doi: 10.18632/aging.102052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Naito M, Terayama H, Hirai S, Qu N, Lustig L, Itoh M. Experimental autoimmune orchitis as a model of immunological male infertility. Med Mol Morphol. 2012;45(4):185–189. doi: 10.1007/s00795-012-0587-2. [DOI] [PubMed] [Google Scholar]
- 81.Meinhardt A, Hedger MP. Immunological, paracrine and endocrine aspects of testicular immune privilege. Mol Cell Endocrinol. 2011;335(1):60–68. doi: 10.1016/j.mce.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 82.Fijak M, Iosub R, Schneider E, Linder M, Respondek K, Klug J, Meinhardt A. Identification of immunodominant autoantigens in rat autoimmune orchitis. J Pathol. 2005;207(2):127–138. doi: 10.1002/path.1828. [DOI] [PubMed] [Google Scholar]
- 83.Aslani F, Schuppe HC, Guazzone VA, Bhushan S, Wahle E, Lochnit G, et al. Targeting high mobility group box protein 1 ameliorates testicular inflammation in experimental autoimmune orchitis. Hum Reprod. 2015;30(2):417–431. doi: 10.1093/humrep/deu320. [DOI] [PubMed] [Google Scholar]
- 84.Gajić D, Despotović S, Koprivica I, Miljković Đ, Saksida T. Ethyl pyruvate ameliorates experimental autoimmune myocarditis. Biomol. 2021;11:1768. doi: 10.3390/biom11121768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448(7152):427–434. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 86.Algieri F, Rodriguez-Nogales A, Garrido-Mesa J, Camuesco D, Vezza T, Garrido-Mesa N, et al. Intestinal anti-inflammatory activity of calcium pyruvate in the TNBS model of rat colitis: comparison with ethyl pyruvate. Biochem Pharmacol. 2016;103:53–63. doi: 10.1016/j.bcp.2015.12.022. [DOI] [PubMed] [Google Scholar]
- 87.Maeda S, Hikiba Y, Shibata W, Ohmae T, Yanai A, Ogura K, et al. Essential roles of high-mobility group box 1 in the development of murine colitis and colitis-associated cancer. Biochem Biophys Res Commun. 2007;360(2):394–400. doi: 10.1016/j.bbrc.2007.06.065. [DOI] [PubMed] [Google Scholar]
- 88.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ulloa L, Ochani M, Yang H, Tanovic M, Halperin D, Yang R, et al. Ethyl pyruvate prevents lethality in mice with established lethal sepsis and systemic inflammation. Proc Natl Acad Sci USA. 2002;99(19):12351–12356. doi: 10.1073/pnas.192222999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fink MP. Ethyl pyruvate: a novel treatment for sepsis. Curr Drug Targets. 2007;8(4):515–518. doi: 10.2174/138945007780362791. [DOI] [PubMed] [Google Scholar]
- 91.Guarda IF, Correia CJ, Breithaupt-Faloppa AC, Ferreira SG, Moreno AC, Martinez MB, et al. Effects of ethyl pyruvate on leukocyte-endothelial interactions in the mesenteric microcirculation during early sepsis treatment. Clinics (Sao Paulo) 2015;70(7):508–514. doi: 10.6061/clinics/2015(07)08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jiang Z, Li X, Lin Z, Chen J, Guan X, Chen M. Ethyl pyruvate reduces hepatic mitochondrial swelling and dysfunction in a rat model of sepsis. Int J Clin Exp Pathol. 2015;8(7):7774–7785. [PMC free article] [PubMed] [Google Scholar]
- 93.Chen W, Lian J, Ye JJ, Mo QF, Qin J, Hong GL, et al. Ethyl pyruvate reverses development of Pseudomonas aeruginosa pneumonia during sepsis-induced immunosuppression. Int Immunopharmacol. 2017;52:61–69. doi: 10.1016/j.intimp.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 94.Yende S, D'Angelo G, Kellum JA, Weissfeld L, Fine J, Welch RD, et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177(11):1242–1247. doi: 10.1164/rccm.200712-1777OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Erickson MA, Banks WA. Cytokine and chemokine responses in serum and brain after single and repeated injections of lipopolysaccharide: multiplex quantification with path analysis. Brain Behav Immun. 2011;25(8):1637–1648. doi: 10.1016/j.bbi.2011.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Annane D, Sharshar T. Cognitive decline after sepsis. Lancet Respir Med. 2015;3(1):61–69. doi: 10.1016/S2213-2600(14)70246-2. [DOI] [PubMed] [Google Scholar]
- 97.Fink MP. Ethyl pyruvate. Curr Opin Anaesthesiol. 2008;21(2):160–167. doi: 10.1097/ACO.0b013e3282f63c2e. [DOI] [PubMed] [Google Scholar]
- 98.Yang R, Zhu S, Tonnessen TI. Ethyl pyruvate is a novel anti-inflammatory agent to treat multiple inflammatory organ injuries. J Inflamm (Lond) 2016;13:37. doi: 10.1186/s12950-016-0144-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sappington PL, Yang R, Yang H, Tracey KJ, Delude RL, Fink MP. HMGB1 B box increases the permeability of Caco-2 enterocytic monolayers and impairs intestinal barrier function in mice. Gastroenterology. 2002;123(3):790–802. doi: 10.1053/gast.2002.35391. [DOI] [PubMed] [Google Scholar]
- 100.Lau A, Wang S, Liu W, Haig A, Zhang ZX, Jevnikar AM. Glycyrrhizic acid ameliorates HMGB1-mediated cell death and inflammation after renal ischemia reperfusion injury. Am J Nephrol. 2014;40(1):84–95. doi: 10.1159/000364908. [DOI] [PubMed] [Google Scholar]
- 101.Hu YM, Pai MH, Yeh CL, Hou YC, Yeh SL. Glutamine administration ameliorates sepsis-induced kidney injury by downregulating the high-mobility group box protein-1-mediated pathway in mice. Am J Physiol Renal Physiol. 2012;302(1):F150–F158. doi: 10.1152/ajprenal.00246.2011. [DOI] [PubMed] [Google Scholar]
- 102.Sawa H, Ueda T, Takeyama Y, Yasuda T, Shinzeki M, Nakajima T, Kuroda Y. Blockade of high mobility group box-1 protein attenuates experimental severe acute pancreatitis. World J Gastroenterol. 2006;12(47):7666–7670. doi: 10.3748/wjg.v12.i47.7666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Luan ZG, Ma XC, Zhang H, Zhang C, Guo RX. Protective effect of ethyl pyruvate on pancreas injury in rats with severe acute pancreatitis. J Surg Res. 2013;181(1):76–84. doi: 10.1016/j.jss.2012.05.066. [DOI] [PubMed] [Google Scholar]
- 104.Kao RL, Xu X, Xenocostas A, Parry N, Mele T, Martin CM, Rui T. Induction of acute lung inflammation in mice with hemorrhagic shock and resuscitation: role of HMGB1. J Inflamm (Lond) 2014;11(1):30. doi: 10.1186/s12950-014-0030-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tsai BM, Lahm T, Morrell ED, Crisostomo PR, Poynter J, Wang M, Meldrum DR. Ethyl pyruvate inhibits hypoxic pulmonary vasoconstriction and attenuates pulmonary artery cytokine expression. J Surg Res. 2008;145(1):130–134. doi: 10.1016/j.jss.2007.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yang R, Uchiyama T, Alber SM, Han X, Watkins SK, Delude RL, Fink MP. Ethyl pyruvate ameliorates distant organ injury in a murine model of acute necrotizing pancreatitis. Crit Care Med. 2004;32(7):1453–1459. doi: 10.1097/01.ccm.0000130835.65462.06. [DOI] [PubMed] [Google Scholar]
- 107.Yang R, Han X, Delude RL, Fink MP. Ethyl pyruvate ameliorates acute alcohol-induced liver injury and inflammation in mice. J Lab Clin Med. 2003;142(5):322–331. doi: 10.1016/S0022-2143(03)00138-0. [DOI] [PubMed] [Google Scholar]
- 108.Yang R, Shaufl AL, Killeen ME, Fink MP. Ethyl pyruvate ameliorates liver injury secondary to severe acute pancreatitis. J Surg Res. 2009;153(2):302–309. doi: 10.1016/j.jss.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 109.Shen M, Lu J, Dai W, Wang F, Xu L, Chen K, et al. Ethyl pyruvate ameliorates hepatic ischemia-reperfusion injury by inhibiting intrinsic pathway of apoptosis and autophagy. Mediators Inflamm. 2013;2013:461536. doi: 10.1155/2013/461536.Erratum.In:MediatorsInflamm.2016;2016:5434275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Entezari M, Javdan M, Antoine DJ, Morrow DM, Sitapara RA, Patel V, et al. Inhibition of extracellular HMGB1 attenuates hyperoxia-induced inflammatory acute lung injury. Redox Biol. 2014;2:314–322. doi: 10.1016/j.redox.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Durak MZ, Churey JJ, Gates M, Sacks GL, Worobo RW. Decontamination of green onions and baby spinach by vaporized ethyl pyruvate. J Food Prot. 2012;75(6):1012–1022. doi: 10.4315/0362-028X.JFP-12-008. [DOI] [PubMed] [Google Scholar]
- 112.Api AM, Belmonte F, Belsito D, Biserta S, Botelho D, Bruze M, et al. RIFM fragrance ingredient safety assessment, ethyl pyruvate, CAS Registry Number 617–35-6. Food Chem Toxicol. 2019;134(Suppl 2):111008. doi: 10.1016/j.fct.2019.111008. [DOI] [PubMed] [Google Scholar]
- 113.Bennett-Guerrero E, Swaminathan M, Grigore AM, Roach GW, Aberle LG, Johnston JM, Fink MP. A phase II multicenter double-blind placebo-controlled study of ethyl pyruvate in high-risk patients undergoing cardiac surgery with cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2009;23(3):324–329. doi: 10.1053/j.jvca.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 114.Berry LM, Wollenberg L, Zhao Z. Esterase activities in the blood, liver and intestine of several preclinical species and humans. Drug Metab Lett. 2009;3(2):70–77. doi: 10.2174/187231209788654081. [DOI] [PubMed] [Google Scholar]
- 115.Bahar FG, Ohura K, Ogihara T, Imai T. Species difference of esterase expression and hydrolase activity in plasma. J Pharm Sci. 2012;101(10):3979–3988. doi: 10.1002/jps.23258. [DOI] [PubMed] [Google Scholar]
- 116.Guarino VA, Oldham WM, Loscalzo J, Zhang YY. Reaction rate of pyruvate and hydrogen peroxide: assessing antioxidant capacity of pyruvate under biological conditions. Sci Rep. 2019;9(1):19568. doi: 10.1038/s41598-019-55951-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lockridge O, Quinn DM. Esterases comprehensive toxicology (2nd edn). In: McQueen CA, editor. 2010;4, p. 243–73. 10.1016/B978-0-08-046884-6.00414-0.
- 118.Dong W, Cai B, Peña G, Pisarenko V, Vida G, Doucet D, et al. Ethyl pyruvate prevents inflammatory responses and organ damage during resuscitation in porcine hemorrhage. Shock. 2010;34(2):205–213. doi: 10.1097/SHK.0b013e3181cc0c63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Suffoletto BP, Salcido DD, Logue ES, Caprio TW, Menegazzi JJ. Ethyl pyruvate enhances intra-resuscitation hemodynamics in prolonged ventricular fibrillation arrest. Resuscitation. 2009;80(12):1411–1416. doi: 10.1016/j.resuscitation.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 120.Hauser B, Kick J, Asfar P, Ehrmann U, Albicini M, Vogt J, et al. Ethyl pyruvate improves systemic and hepatosplanchnic hemodynamics and prevents lipid peroxidation in a porcine model of resuscitated hyperdynamic endotoxemia. Crit Care Med. 2005;33(9):2034–2042. doi: 10.1097/01.ccm.0000178177.03979.ce. [DOI] [PubMed] [Google Scholar]
- 121.Jacobs CC, Holcombe SJ, Cook VL, Gandy JC, Hauptman JG, Sordillo LM. Ethyl pyruvate diminishes the inflammatory response to lipopolysaccharide infusion in horses. Equine Vet J. 2013;45(3):333–339. doi: 10.1111/j.2042-3306.2012.00634.x. [DOI] [PubMed] [Google Scholar]
- 122.Schroeder EL, Holcombe SJ, Cook VL, James MD, Gandy JC, Hauptman JG, Sordillo LM. Preliminary safety and biological efficacy studies of ethyl pyruvate in normal mature horses. Equine Vet J. 2011;43(3):341–347. doi: 10.1111/j.2042-3306.2010.00214.x. [DOI] [PubMed] [Google Scholar]
- 123.Johnson LM, Holcombe SJ, Shearer TR, Watson V, Gandy J, Southwood LL, et al. Multicenter placebo-controlled randomized study of ethyl pyruvate in horses following surgical treatment for ≥ 360° large colon volvulus. Front Vet Sci. 2020;7:204. doi: 10.3389/fvets.2020.00204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tang H, Zhao H, Song J, Dong H, Yao L, Liang Z, Lihong Y, Zou F, Cai S. Ethyl pyruvate decreases airway neutrophil infiltration partly through a high mobility group box 1-dependent mechanism in a chemical-induced murine asthma model. Int Immunopharmacol. 2014;21(1):163–170. doi: 10.1016/j.intimp.2014.04.024. [DOI] [PubMed] [Google Scholar]
- 125.Chen S, Wang Y, Gong G, Chen J, Niu Y, Kong W. Ethyl pyruvate attenuates murine allergic rhinitis partly by decreasing high mobility group box 1 release. Exp Biol Med (Maywood) 2015;240(11):1490–1499. doi: 10.1177/1535370214566563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Shah MD, Sumeh AS, Sheraz M, Kavitha MS, Venmathi Maran BA, Rodrigues KF. A mini-review on the impact of COVID 19 on vital organs. Biomed Pharmacother. 2021;143:112158. doi: 10.1016/j.biopha.2021.112158. [DOI] [PMC free article] [PubMed] [Google Scholar]