Abstract
Background
Representative images of pathology in patients with skin of color are lacking in most medical education resources. This particularly affects training in dermatology, which relies heavily on the use of images to teach pattern recognition. The presentation of skin pathology can vary greatly among different skin tones, and this lack of representation of dark skin phototypes challenges providers' abilities to provide quality care to patients of color.
In Botswana and other countries in sub-Saharan Africa, this challenge is further compounded by limited resources and access to dermatologists. There is a need for improved and accessible educational resources to train medical students and local medical providers in basic skin lesion description and diagnosis.
Objectives
We examined whether online Perceptual and Adaptive Learning Modules (PALMs) composed of representative dark skin images could efficiently train University of Botswana medical students to more accurately describe and diagnose common skin conditions in their community.
Methods
Year 4 and 5 medical students voluntarily completed PALMs that teach skin morphology, configuration, and distribution terminology and diagnosis of the most common dermatologic conditions in their community. Pre-tests, post-tests and delayed-tests assessed knowledge acquisition and retention.
Results
PALMs training produced statistically significant (P≤0.0001) improvements in accuracy and fluency with large effect sizes (1.5–3.7) and good retention after a 12.5–21-week median delay. Limitations were a self-selected group of students, a single institution, slow internet connections, and high drop-out rates.
Conclusions
Overall, population-specific PALMs are a useful tool for efficient development of pattern recognition in skin disease description and diagnosis.
Keywords: Dermatology, HIV, Infectious disease, Acne, Dermatitis
Introduction
Medical education should reflect the diversity of society and disease presentation, yet a growing body of literature highlights the underrepresentation of patients of color in both textbooks and web-based resources.1–5 This disparity particularly affects training in dermatology, which relies heavily on the images within these resources to teach pattern recognition, a skill that is central to dermatology. Pattern recognition is the ability to properly categorize and interpret the various colors, morphologies, configurations and distributions of skin disease, allowing for more accurate diagnosis and management. Mastering pattern recognition typically requires seeing a large volume of relevant cases or examples.
Many of the key clinical features of skin disease are influenced by skin tone. Most notably, erythema in dark skin tones can be quite subtle or may appear more brown or purple. If not exposed to this presentation of erythema in training, inflammatory or infectious conditions may go unnoticed or misdiagnosed. As Nolen highlights with the example of erythema migrans, failure to recognize subtle erythema in patients with dark skin tones can result in delayed diagnosis.6 Such delays in care can have systemic consequences. Exposure to diverse skin types in training is needed in order to recognize skin pathology in all skin tones. Without it, providers may fail to provide equitable, timely and quality care.
Dermatology textbooks often lack the images across all skin tones, featuring mostly light skin images.2–4 A recent review of all images published in commonly used dermatology textbooks found that skin of color was depicted in only 22–32% of images.2 A more recent 2020 review of six commonly used dermatology textbooks found that dark skin images, defined more strictly as Fitzpatrick V-VI, represented only 10.3% of all images.3 In comparison, web-based resources offered greater representation, with VisualDx having the highest proportion of images (28.5%), likely in part due to the flexibility of online sources to add images and maintain large databases.3 This lack of representation in images affects dermatology education worldwide but may disproportionately affect medical providers serving communities where the majority of the population has deeply pigmented skin or learners without reliable access to online resources.
In addition to skin tone, skin disease can vary in prevalence and presentation depending on geography and population. The global burden of skin disease is substantial, ranking as the 4th leading cause of disability world wide.7 In many regions of sub-Saharan Africa, the HIV/AIDS epidemic further contributes to this burden and influences local patterns of skin disease.8 Published educational resources do not always reflect these population-specific patterns.4,5
In Botswana and other countries in sub-Saharan Africa, dermatologic care is strained, not only by the lack of representative educational resources, but also by limited access to trained dermatologists. With a high burden of skin disease and few available specialists, basic skills in dermatology assessment and terminology become particularly important for all medical providers.
As is true for many medical schools, dermatology curricular content at the University of Botswana Faculty of Medicine (UB FoM, admitting students since 2009) is somewhat limited. At the time of publication, it consisted of two dermatology lectures and two dermatology-focused clinical skills labs in the 1st year, two problem-based learning sessions during the 2nd year, and a 2-week clinical rotation during the 4th year. Because UB FoM lacks a dermatologist on faculty, education has been offered by various sources. Until 2016, rotating US dermatology residents and faculty under the Botswana-UPenn Partnership gave lectures and offered clinical supervision. Since 2016, a Ministry of Health-employed dermatologist has also participated in medical student education.
Outside of dermatology lectures and clinical exposure, UB medical students rely heavily on dermatology textbooks, but the lack of representative images makes it challenging for students to gain the necessary exposure to confidently recognize common skin findings in their patients. Clearly there is a need for educational resources that both effectively and reliably teach dermatologic descriptions and diagnoses and accurately reflect the patient population.
Online, image-based modules incorporating features that adapt to each learner’s performance may offer a superior resource for training pattern recognition compared to traditional lectures and textbooks alone. Recent advances in the learning sciences have shown that perceptual-learning approaches, when enhanced by adaptive-learning technologies, have the potential to improve rate of acquisition, levels of competence, and retention of pattern recognition in medical education.9–12 Through rapid, systematic exposure to a large number of relevant examples, image-based modules incorporating perceptual and adaptive learning strategies have been shown to efficiently and durably train medical students in the United States (US) to recognize basic histological patterns13 and tissue types14, describe skin lesions15, and interpret echocardiograms.16 More specifically, these Perceptual and Adaptive Learning Modules (PALMs) were previously provided to medical students at the University of California, Los Angeles to train skin lesion descriptive terminology. In this study, students had large and durable gains in their abilities to classify lesions according to morphology, configuration and distribution.15
As Burgin et al. call for in their action items for teaching diversity and achieving equity in dermatology education, “we must harness currently available resources to incorporate images for teaching that show the range of skin types and strive to create more resources.”5 To address inadequacies in training materials featuring skin of color and augment medical education in a resource-restricted setting, we adapted PALMs for UB medical students, incorporating de-identified images from patients seen in Botswana dermatology clinics and additional dark skin images donated from the Logical Images Inc. database. The same PALMs were re-designed with these representative dark skin images to teach morphology, configuration and distribution terminology. An additional PALM was designed for training discrimination among the 15 most common skin diagnoses observed in Botswana.
This study aims to evaluate the effectiveness of these novel, population-specific PALMs for training UB medical students to characterize and diagnose common skin conditions affecting their community. These modules are open-access and available at http://med.insightlt.com.
METHODS
PALM Development and Associated Assessments
PALM displays consist of a series of interactive learning trials. Each image appears along with four multiple-choice categories into which the image might be classified (Figure 1, Video 1).
Figure 1: Feedback examples for the morphology PALM.
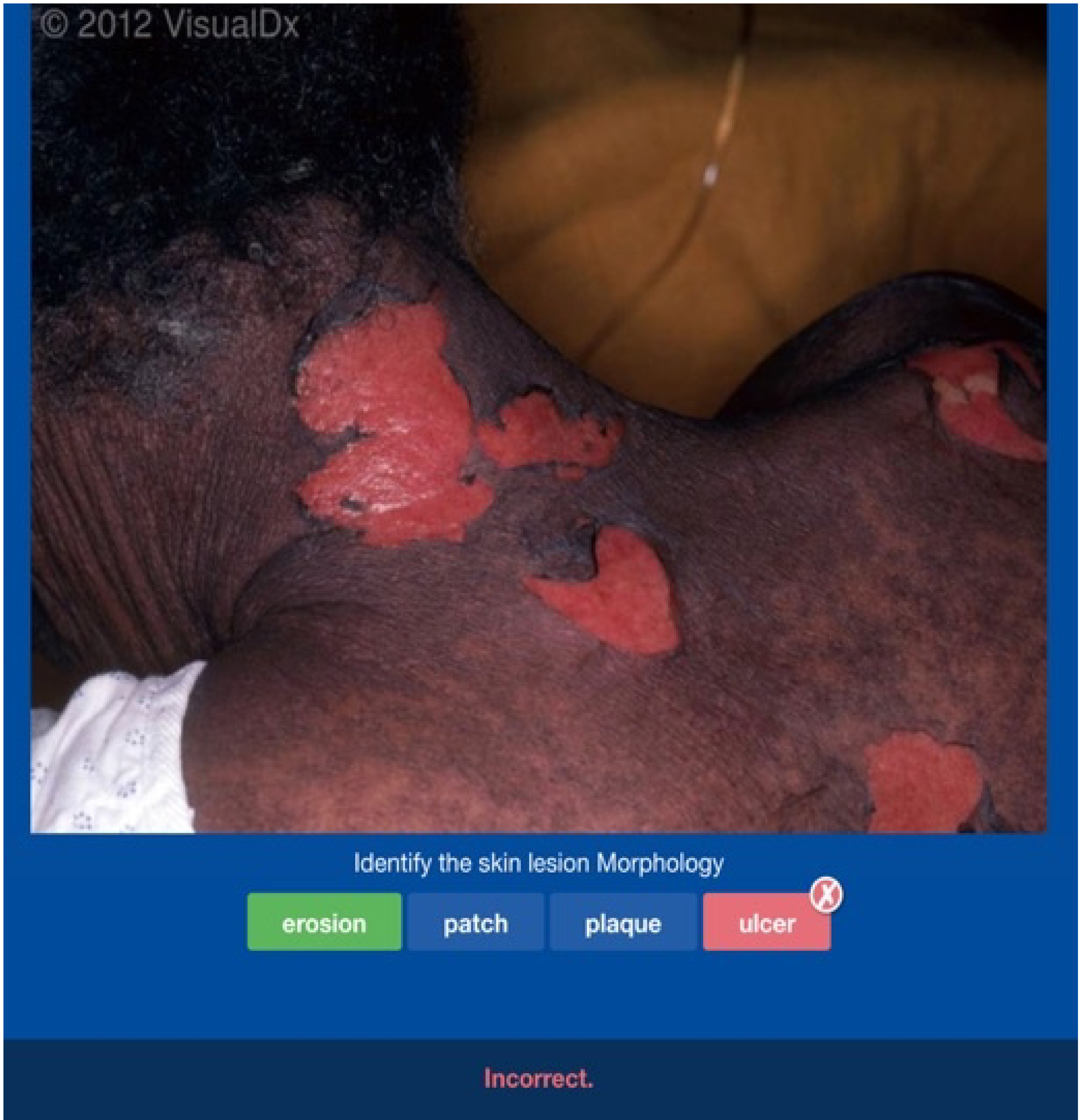
All PALMs use the same format. On each slide, the question consists of only the image and the four terms as answer choices. The learner selects a choice by clicking on the appropriate term below the image. Once selected, feedback is given when the correct answer highlights in green. Incorrect selections highlight red. Feedback on response time is given only for correct answers.
We developed four PALMs (Table 1). Three train students to apply 11–12 proper descriptive terms to examples of lesion morphology, configuration and anatomic distribution. A fourth teaches recognition of the 15 most common dermatology diagnoses in the region. These were determined based on review of clinical diagnoses recorded from three preceding years of the dermatology database at Princess Marina Hospital, the primary dermatology referral clinic in Botswana.
Table I:
Category discriminants trained in each dermatology PALM
| Morphology | Configuration | Distribution | Diagnosis |
|---|---|---|---|
| Bulla | Annular | Acral | Acne |
| Erosion | Arcuate | Dermatomal | Atopic dermatitis |
| Eschar | Follicular | Diaper area | Herpes simplex virus |
| Macule | Geometric | Extensor | Intertrigo |
| Nodule | Grouped | Flexural | Kaposi’s sarcoma |
| Papule | Linear | Intertriginous | Lichen planus |
| Patch | Oval | Lymphangitic | Lichen simplex chronicus |
| Plaque | Reticular | Photodistributed | Lupus |
| Pustule | Round | Scattered | Psoriasis |
| Ulcer | Serpiginous | Solitary | Seborrheic dermatitis |
| Vesicle | Targetoid | Symmetric extremities | Squamous cell carcinoma |
| Widespread | Tinea | ||
| Urticaria | |||
| Verruca | |||
| Vitiligo |
The modules are composed of de-identified clinical images of patients seen in Botswana clinics and skin of color images donated from the Logical Images Inc. database. Images were obtained by a medical student (CS), and accuracy of classification was subsequently validated by experienced dermatologists (CK and AYC).
By incorporating on average 33±2.9 unique exemplars of each category (see Table 1), the modules target pattern recognition rather than recall. As trainees classify each image, the underlying PALMs algorithm dynamically modifies the sequence and spacing for presenting a subsequent example from each category based on the individual’s accuracy and response time (RT), thereby adapting to each learner’s performance. Repetition of a category occurs soonest for incorrect answers, and the delay for repetition of correctly identified categories is shorter, the longer the RT for the answer.9–12 Prior to beginning the PALMs, users are instructed to select answers both accurately and expeditiously, with accuracy taking precedence over speed. The program provides immediate feedback and, if answered correctly, the RT (Figure 1). RT is calculated from the time the image completes downloading. A target RT was set to 6 seconds, based on dermatology PALMs studied previously.13,15
Two measures are recorded for each response, “accuracy” and “fluency” (accurate and within the target RT). Repetition of a given category requires a minimum of three intervening categories. Categories are retired as the learner achieves mastery, defined as fluent responses to three consecutive, spaced presentations of the category; however, exemplars from retired categories are used as “non-scored fillers” to maintain the spacing requirement towards the end of PALM completion, when four or fewer unretired categories remain.12 Retirement of all categories completes the PALM. [See Kellman and Krasne (2018) for additional details.]
Student performance on multiple-choice assessments taken immediately before (pre-test) and after (post-test) each PALM and at the end of the academic year (delayed test) assessed knowledge acquisition and retention. Each assessment consists of two previously unseen images per category, presented in the same question format as the modules but without feedback to the student or any adaptive features.
Study Design
Informed consent was obtained from all participants, and participation was voluntary. Every 2 weeks throughout the year, 2–3 fourth-year medical students (MS4, n=53) completed a dermatology rotation. Students were given protected time to (voluntarily) complete the dermatology PALMs and associated pre- and post-tests at the beginning of the rotation. Participants could perform each PALM separately and did not need to complete all four PALMs in one sitting. During the rotation, students could apply what they learned from the PALMs to patients in clinic. A delayed test was distributed to all MS4s at the end of the academic year.
The PALMs were also distributed to all 5th year medical students (MS5, n=37) at the beginning of the academic year (August). These students had completed the dermatology rotation as MS4s without exposure to PALMs. We excluded MS5s from this study who did not complete the PALMs and associated tests within the first month to avoid contamination on the pre-test from additional learning experiences associated with the MS5 curriculum since we noticed that clinical learning during that time enhanced their PALM performance.
Only outcomes for students completing all assessments were included in the study.
User Satisfaction
To assess user satisfaction, participants were asked to complete an anonymous survey (6 yes/no/unsure questions) following completion of the PALMs.
Analysis
Correct answers received 1 point for each accurate answer and 1 point for each fluent answer. Within-group comparisons between tests were assessed by paired, two-tailed t-tests. Independent two-tailed t-tests were used for between group analyses. Statistical significance was accepted for two-tailed p< 0.05. Effect size was calculated as Cohen’s d (the difference in means divided by the pooled standard deviation characterized by Cohen as small=0.2, medium=0.5, and large=0.8).17
This study was approved by IRBs of the University of Pennsylvania, the University of California Los Angeles, the University of Botswana, and the Botswana Ministry of Health and Wellness.
RESULTS
Depending on the particular PALM, 45–49 MS4s and 9–12 MS5s completed both the pre-tests and post-tests for response rates of 85–92% and 24–32%, respectively. However, data from only 6–8 MS5s—who completed the PALMs within the first month of the MS5 curriculum—were included. Completion times ranged from 16(±9) to 42(±22) minutes per PALM for MS4s and 13(±5) to 26(±10) minutes for MS5s with an average combined time spent on all PALMs being 1 hour 56 minutes for MS4s and 1 hour 17 minutes for MS5s. The average time for each test (pre, post- and delayed) was 5 to 6 minutes.
Data for both classes in Figure 2 shows that improvements from pre-test to post-test in both accuracy and fluency were large and statistically significant (data in figure 2 legend).
Figure 2: Pre-test and post-test performance for MS4 and MS5 students completing the dermatology PALMs.
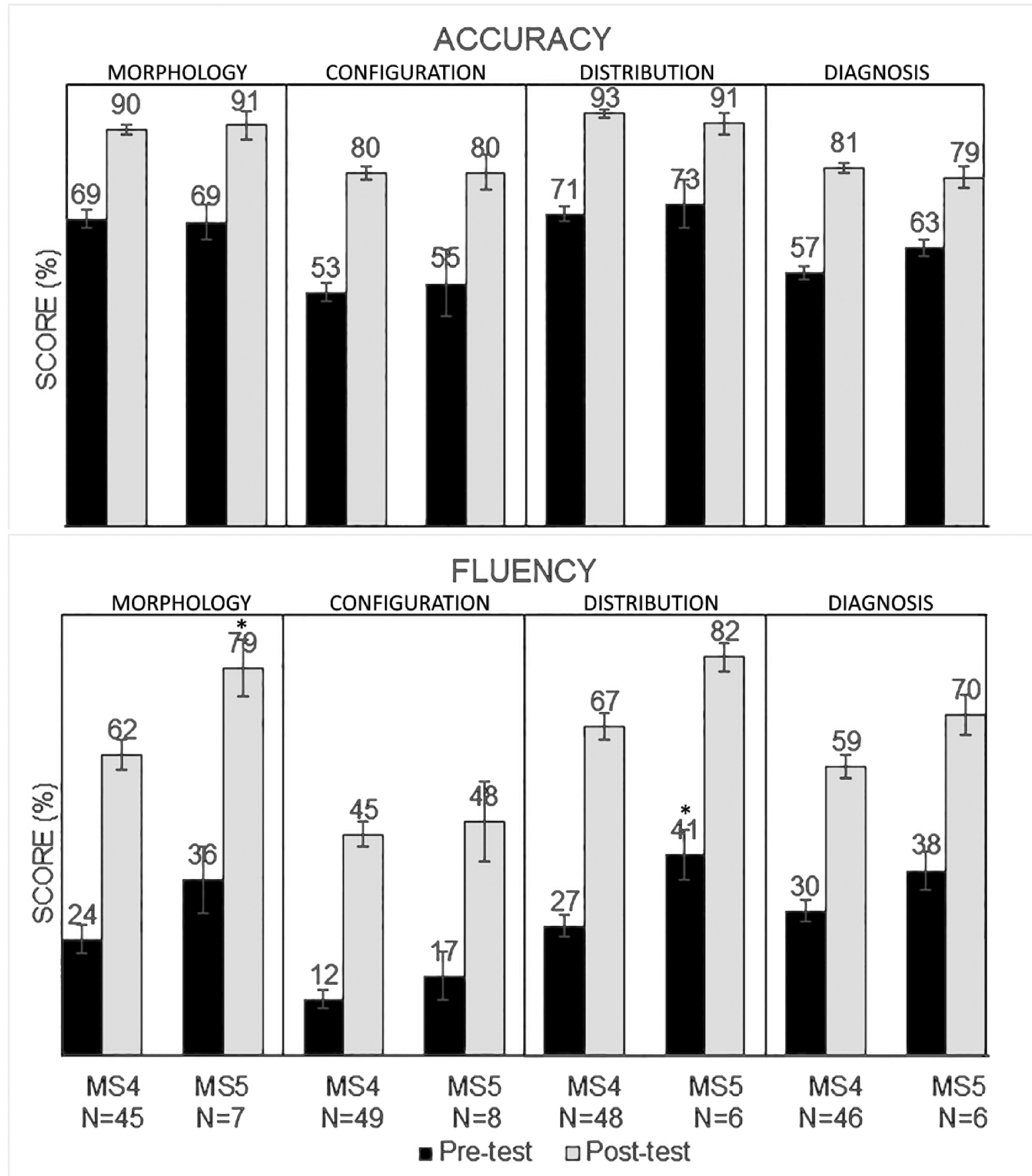
For all students, post-test performance (gray) for both accuracy (upper) and fluency (lower) were statistically higher than pre-test performance (black) and with large effect sizes. For MS4s, P<0.0001; d=1.8 to 2.5, and for MS5s, P<0.0001 to P=0.014; d=1.5 to 3.9. Fluency appears consistently higher for MS5s than MS4s but differences are only statistically significance for the distribution pre-test (p=0.03; d=1.1) and the morphology post-test (p=0.03; d=0.94); statistical significance for the distribution post-test fluency was borderline (p= 0.07; d=0.99).
Comparing MS4 and MS5 performance, both classes obtained similar accuracy scores on all pre-tests and post-tests. Fluency scores, however, were higher for MS5s compared to the MS4s on all pre-tests and post-tests but only statistically significant for the distribution pre-test and the morphology post-test, with significance for the distribution post-test fluency being borderline (see figure 2 legend).
Figure 3 compares MS4 delayed-test scores, obtained at the end of the academic year, with their pre-test scores at the beginning of their dermatology clinic rotations. Because dermatology clinic rotations were staggered, the median length of time between completion of a PALM and its associated delayed test varied, ranging from 10.5 to 21 weeks. Only 14–19 MS4s completed a given delayed tests, perhaps because MS4 students were no longer in their dermatology rotations. Compared to their pre-test scores, students performed better on all delayed tests except for morphology fluency; the improved accuracy performances were large and statistically significant except for distribution module (data in figure 3 legend).
Figure 3: MS4 delayed test performance to assess knowledge retention.
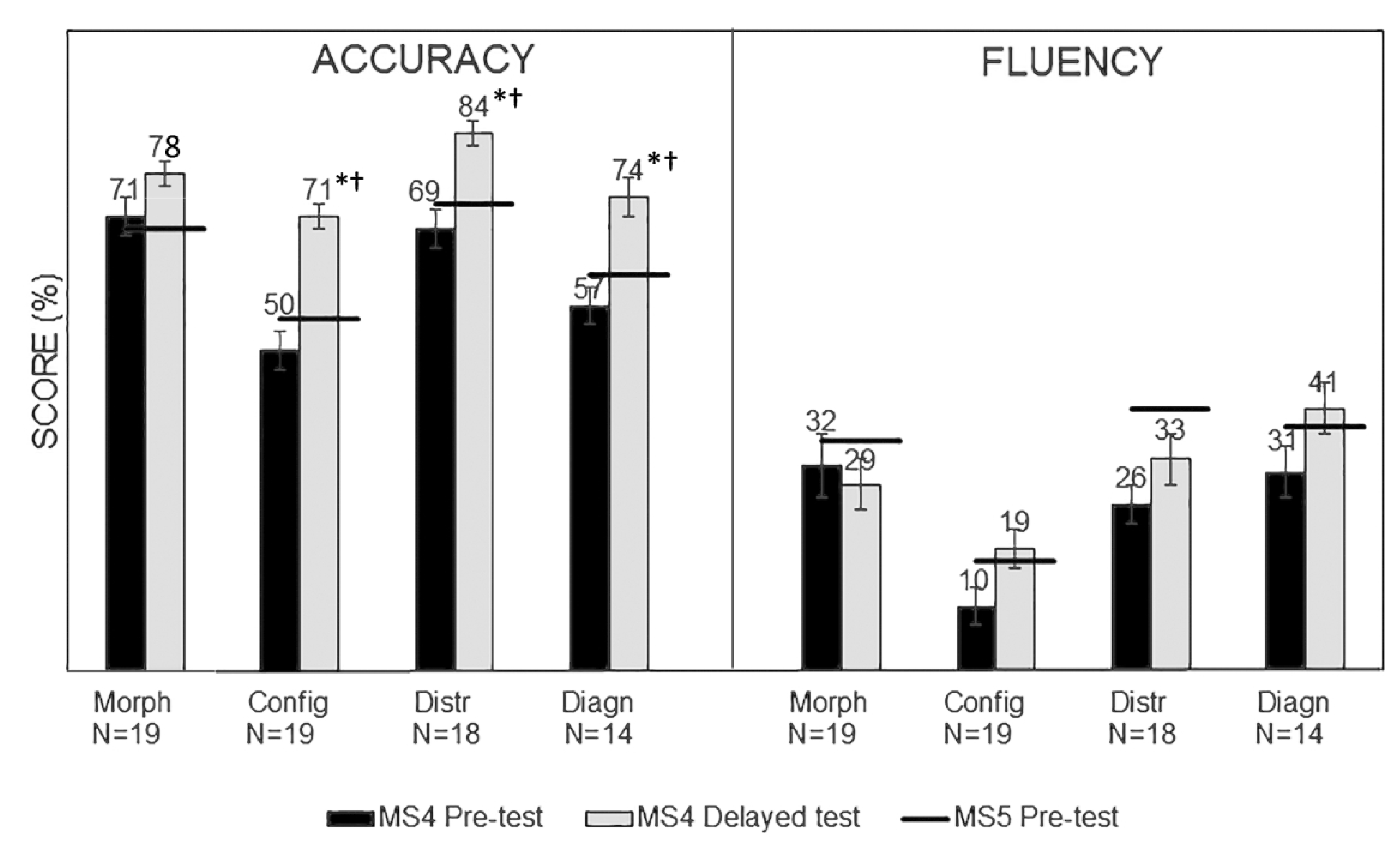
MS4 pre-tests (black) are compared to MS4 delayed tests (gray) to assess overall knowledge retention over a median period of 10.5–21 weeks, depending on the specific PALM. Statistically significant differences between MS4 pre-test and delayed test performance, indicated by "*", ranged from P=<0.0001 to 0.0003 and d=1.23 to 1.65. MS5 pre-test scores, indicated by the horizontal black bars, can also be compared to the MS4 delayed tests. Statistically significant differences between the MS4 delayed test and MS5 pre-test performance are indicated by "†" with values ranging from P=0.006 to 0.04 and d=0.95–1.3.
Figure 3 also displays average pre-test performances on each module for the included MS5 students (black bars). These students had all completed the dermatology clinical rotation during the previous year and were completing these pre-tests about 4 months later than the time the MS4s were completing the delayed tests, during which they had some additional clinical experiences. For all but the morphology PALM, MS4 delayed-test accuracies were statistically significantly higher than the corresponding MS5 pre-test accuracies with large effect sizes (data in figure legend); no significant differences existed between the corresponding MS4 and MS5 fluencies however.
Lastly, Figure 4 shows MS4 survey questions and responses. Clearly students thought the PALMs were useful, increased their confidence in both lesion description and diagnosis, and helped them to learn more effectively during their clinical rotation. Although a majority thought the PALMs took too long to complete, they overwhelmingly wanted similar modules designed for other curriculum subjects. Regarding their sense that the PALMs took too long, on average, students estimated that they spent 3 hours and 12 minutes on the four PALMs and assessments, whereas the actual data for average time spent was under 2 hours. They attributed long times to poor internet connectivity that slowed image loading.
Figure 4: MS4 Survey Responses.
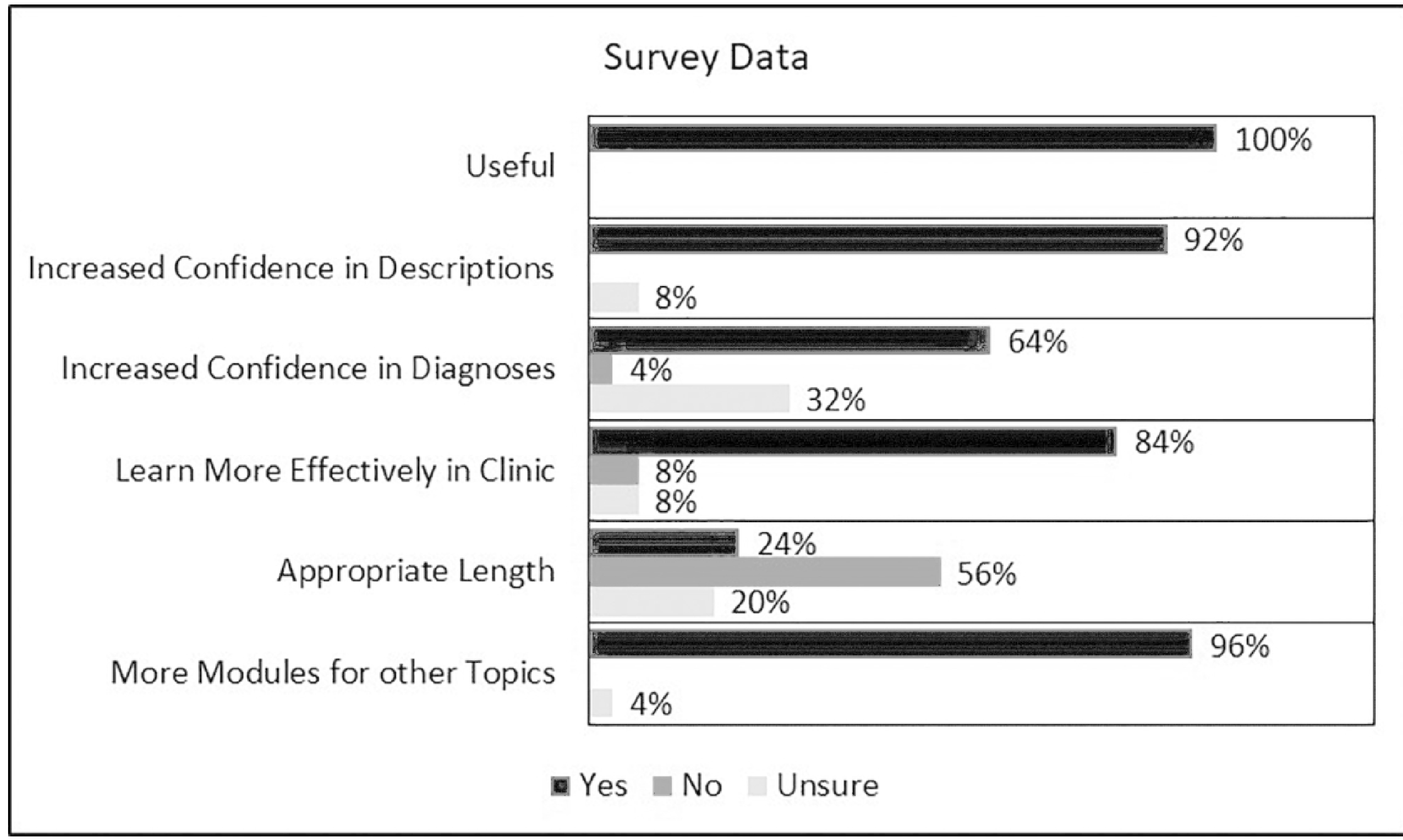
To assess user satisfaction, participants were asked to complete an anonymous survey consisting of 6 yes/no/unsure questions following completion of the PALMs: Overall, did you find the dermatology modules to be useful? Did the dermatology modules make you feel more confident with describing skin lesions? Did the dermatology modules make you feel more confident with recognizing common diagnoses? Did completing the modules on the first day of your dermatology rotation help you to learn more effectively in clinic? Were the modules an appropriate length? Would it be helpful to have modules like this designed for other subjects in the curriculum? Students thought the PALMs were useful, that they increased their confidence in both lesion description and diagnosis, and helped them to learn more effectively during their clinical rotation. Although a majority thought the PALMs took too long to complete, they overwhelmingly wanted similar modules designed for other subjects in the curriculum.
DISCUSSION
We have successfully designed population-specific, skin of color dermatology PALMs and demonstrated their effectiveness in improving medical student application of basic descriptive terminology and recognition of diagnoses. Students markedly improved their accuracy in describing and diagnosing skin lesions and made these discriminations more quickly, suggesting development of pattern recognition. In addition, all four PALMs took students a combined total of under 2 hours to complete (an average of 16–42 minutes per PALM); therefore, this training approach was both effective and efficient. Our observations mirror those reported previously for PALM-based training in a variety of clinical contexts.13,15,16 These PALMs are open-access and available at http://med.insightlt.com.
This study also demonstrated the durability of PALM-based learning, at least when accompanied by opportunities to apply the learned information clinically during dermatology rotations. Since fluency deteriorated more quickly than accuracy, PALM refreshers may be desirable to reinforce pattern recognition, especially when opportunities to apply the learned information are not regularly encountered in clinical practice.
MS4 and MS5 classes achieved similar accuracy on pre-tests and post-tests, suggesting that both groups began with similar funds of knowledge prior to PALM training and achieved the same level of knowledge afterwards, despite MS5s having previously rotated through the dermatology clinic and having additional general clinical experience. Thus, additional knowledge gained from the dermatology rotation alone appeared not to be retained with the current clinical curriculum. The greater fluency of MS5s on the pre- and post-tests, albeit not statistically significant, may suggest greater mastery and more automatic recognition than for MS4s. Thus, while the two groups attained similar levels of competence, as revealed by their accuracy scores, the differences are consistent with more highly developed pattern recognition for certain patterns of descriptors and/or diagnoses in MS5s, for which the MS4s still required more effortful, analytical processing. Added clinical exposure of the MS5s during the 4 intervening months between MS4 delayed and MS5 pre-tests may have led to increased confidence in those descriptions and diagnoses that they interpreted accurately.
On the delayed tests, the MS4s had higher accuracy compared to MS5 pre-test accuracy suggesting durable learning gains resulted from PALM incorporation into the curriculum.
In addition to effectively teaching skin lesion descriptions and diagnosis, PALMs received highly favorable student feedback. UB students had previously reported difficulty accessing helpful dermatology educational resources, noting that many of their textbooks contained too few images of each disease and that images most often featured subjects with lighter skin phototypes. Students appreciated access to PALMs as an online, tailored resource that emphasizes the skin phototypes and prevalent cutaneous diseases representative of their community. The positive feedback from students suggests that these PALMs might be a welcome addition to medical curricula.
One area of concern, that the time needed to complete the PALMs was too long, was most likely a reaction to slow downloading of images when bandwidth was limited. Developing technology, such as “apps” with an offline mode, in which the images reside on a user’s computer or tablet may improve access for regions with poor or intermittent internet connectivity. Another limitation was the high drop-out rate of MS4s in completing the delayed test. Whereas MS4s had time set aside during their dermatology rotations to complete the pre-tests, PALMs and post-tests, they had to find their own time for the delayed tests, perhaps accounting in part for the high dropout rate for these tests. Also, participation at the end of the MS4 year, when the students were no longer in a dermatology clinic rotation, may have reduced student motivation. The MS5s did not have protected time to complete the PALMs, nor were these associated with their curriculum at the beginning of the year. Thus, there was little incentive for their participation, which occurred over several months. Further studies are needed to evaluate retention and the ideal spacing of refresher training.
Expanding on prior studies of PALMs in US medical education, our study supports PALM training with context-relevant images to improve UB medical students’ knowledge acquisition and retention of terminology for morphology, configuration, and distribution, as well as common skin diagnoses. These basic skills in skin disease assessment may allow for improvements in dermatologic care in resource-limited settings through improved and more reliable utilization of clinical decision support tools and more effective triaging of referrals to available dermatologists.
Across studies, PALMs received consistently favorable reviews by medical trainees.13,15,16 To improve the diversity of teaching in dermatology, we should consider the use of technologies like PALMs to provide systematic and personalized training with relevant, tailorable content. Resources like PALMs offer valuable tools with the potential to improve trainee exposure to variations of disease manifestation in differing skin types, a necessary step towards mitigating health disparities in dermatology.
Supplementary Material
ACKNOWLEDGEMENTS:
We are indebted to Tim Burke and Zhen Gu for expert programming support, and we acknowledge generous support from Logical Images, Inc. (http://www.visualdx.com) and Insight Learning Technologies Inc. (http://med.insightlt.com)
FUNDING:
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
DECLARATION OF CONFLICT OF INTERESTS: The Authors declare that there is no conflict of interest
REFERENCES
- 1.Louie P, Wilkes R. Representations of race and skin tone in medical textbook imagery. Soc Sci Med 2018; 202:38–42. [DOI] [PubMed] [Google Scholar]
- 2.Lester JC, Taylor SC, Chren MM. Under-representation of skin of colour in dermatology images: not just an educational issue. Br J Dermatol 2019; 180: 1521–1522. [DOI] [PubMed] [Google Scholar]
- 3.Alvarado SM, Feng H. Representation of dark skin images of common dermatologic condition in educational resources: a cross-sectional analysis. J Am Acad Dermatol 2020; doi: 10.1016/j.jaad.2020.06.041 [DOI] [PubMed] [Google Scholar]
- 4.Ebede T, Papier A. Disparities in dermatology educational resources. J Am Acad Deramtol 2006; 55:687–90. [DOI] [PubMed] [Google Scholar]
- 5.Burgin S, Dlova NC, Goldsmith LA. Dermatological education for the 21st century: prioritizing diversity. Br J Dermatol 2020; doi: 10.1111/bjd.19663. [DOI] [PubMed] [Google Scholar]
- 6.Nolen L. How medical education is missing the bull’s-eye. N Engl J Med 2020;382:2489–91. [DOI] [PubMed] [Google Scholar]
- 7.Karimkhani C, Dellavalle RP, Coffeng LE et al. Global skin disease morbidity and mortality: An update from the global burden of disease study 2013. JAMA Dermatol 2017; 153:406–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Altman K, Vanness E, Westergaard RP. Cutaneous manifestations of human immunodeficiency virus: a clinical update. Current infectious disease reports 2015; 17:464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kellman PJ, Massey CM, Son JY. Perceptual learning modules in mathematics: enhancing students' pattern recognition, structure extraction, and fluency. Top Cogn Sci 2010; 2:285–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kellman PJ, Garrigan P. Perceptual learning and human expertise. Phys Life Rev 2009; 6:53–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mettler E, Kellman PJ. Adaptive response-time-based category sequencing in perceptual learning. Vision Res 2014; 99:111–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kellman PJ, Krasne S. Accelerating expertise: Perceptual and adaptive learning technology in medical training. Med Teach 2018;40:797–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krasne S, Hillman JD, Kellman PJ, Drake TA. Applying perceptual and adaptive learning techniques for teaching introductory histopathology. J Pathol Inform 2013; 4:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parker EU, Reder NP, Glasser D et al. NDER: A Novel web application for teaching histology to medical students. Acad Pathol 2017; doi: 10.1177/2374289517691061. [DOI] [PMC free article] [PubMed]
- 15.Rimoin L, Altieri L, Craft N, et al. Training pattern recognition of skin lesion morphology, configuration, and distribution. J Am Acad Dermatol 2015;72:489–95. [DOI] [PubMed] [Google Scholar]
- 16.Romito BT, Krasne S, Kellman PJ, Dhillon A. The impact of a perceptual and adaptive learning module on transoesophageal echocardiography interpretation by anaesthesiology residents. Br J Anaesth 2016; 117:477–81. [DOI] [PubMed] [Google Scholar]
- 17.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd Edition. Routledge, New York: 1988. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


