The success of multimodal chronic pain management is typically measured by changes in pain intensity, psychological distress, and disability (physical function and activity interference) [23,28,48,119]. Pain, distress, and disability are vitally important therapeutic targets. However, the social outcomes of pain - profoundly influencing both patients’ experience of chronic pain and quality of life [22,24,38,60] – are equally important from a clinical perspective, and may even be more important therapeutic targets from the patient and their families’ perspective. We argue for expanded measurement of the social consequences of pain in clinical research and practice, including satisfaction with social roles, perceived injustice, dyadic and family relationship functioning, social connectedness, and social support. More systematic and comprehensive measurement will allow us to evaluate the therapeutic impact of pain management on patients’ social outcomes, and the contribution of social outcomes to patients’ experience of pain, distress, and disability.
The social consequences of pain
The experience of chronic pain is associated with withdrawal from social activity [123], increased social isolation [126], feelings of loneliness [1,2,73], and the erosion of social identity [67]. These social consequences of pain can create feelings of guilt and worry which further heighten distress and impede pain self-care [134,135]. The “invisible” nature of chronic pain conditions (where pain persists after the visible healing of injury) can give rise to misunderstandings, mistrust, and workplace conflict, precipitate stigmatization, discrimination, and bullying [36,91,113,125], and exacerbate social and economic inequalities [3,20]. Pain can give rise to feelings of hostility [2], which may precipitate conflict between spouses [11,35,69,70,80] and dysfunction within families [46,95]. Having a primary caregiver with chronic pain is associated with poorer psychosocial functioning [132] and higher risk of acquiring chronic pain in children [50]. Taken together, it is clear that the consequences of chronic pain extend beyond distress and disability, and indeed beyond the individual, to affect the social lives of the person with pain and their family. These social experiences can, in turn, perpetuate and exacerbate pain, distress, and disability (Fig. 1).
Figure 1.
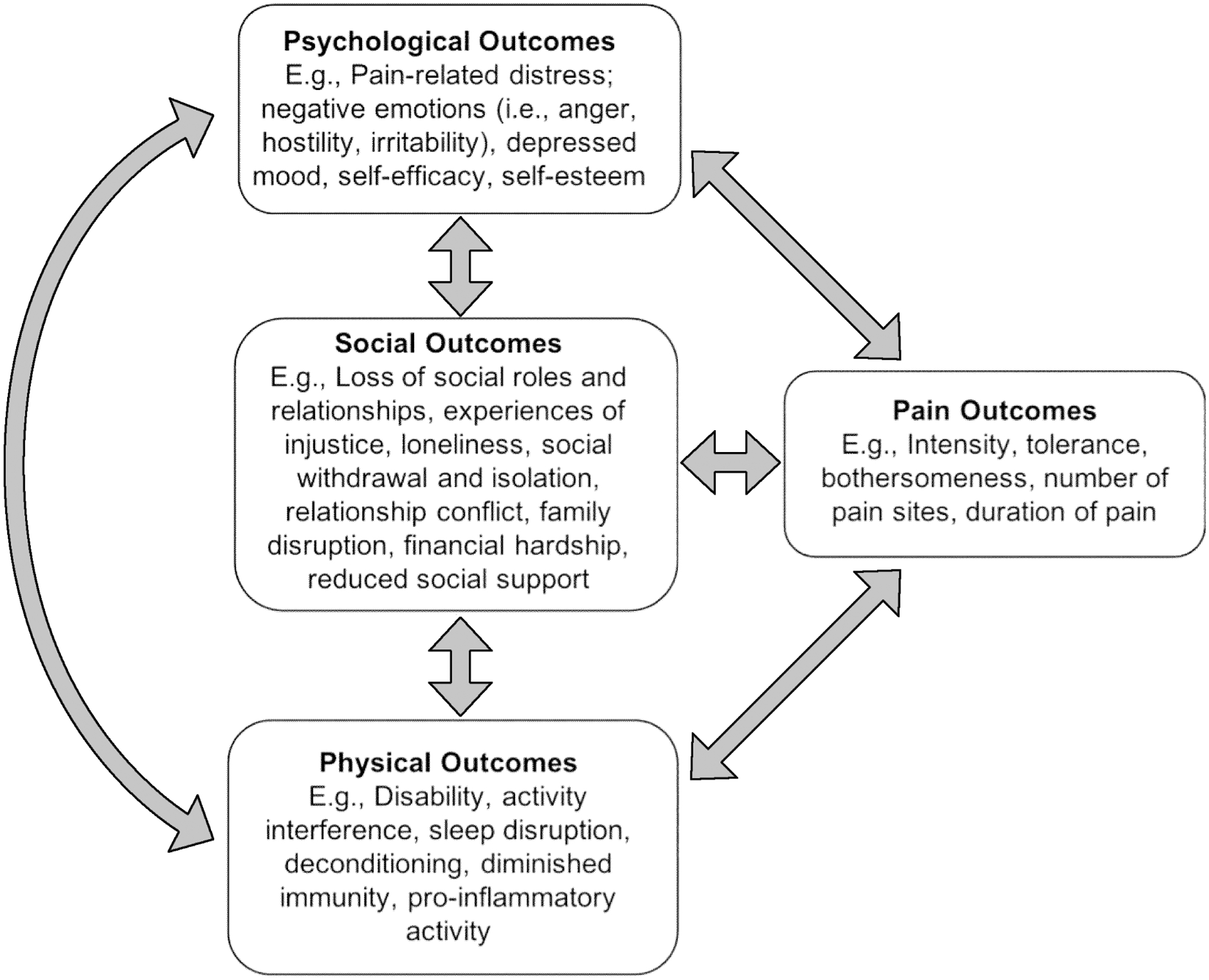
Relationship between psychological, social, and physical outcomes and pain.
Social pains can affect treatment gains
Increasingly, researchers, clinicians, and public health organizations are recognizing the importance of relationship quality and social safety for health, wellbeing, and quality of life [8,51,76,110]. Strong supportive relationships are associated with greater adherence to treatment advice [25], hastened recovery from illness and injury [71,89], lower likelihood of developing chronic pain [103], lower stress [16], and higher subjective wellbeing [68]. By contrast, ‘social pains’ such as perceived social isolation, social exclusion, and feelings of loneliness are associated with reduced physical activity [45], disrupted sleep [9], increased pro-inflammatory activity [30], diminished immunity [26,96], and a range of chronic diseases including diabetes, cardiovascular disease, depression, and chronic pain [1,6,10]. Accordingly, for people living with chronic pain, social isolation and low perceived social support is associated with worsening pain, distress, and disability over time [18,33,44,59,63,70,75]. Cross-lagged longitudinal analyses reveal that patient-reported social isolation is associated with later pain interference, but not vice versa [59]. Hence, social impacts of pain management (e.g., restoration of social roles, relationships, and increased social integration) may be critical to the achievement and maintenance of therapeutic gains.
Social outcomes are patient-centred outcomes
Importantly, improved social relationships may be a primary goal of pain management for patients. In a survey of 800 patients with chronic pain, two-thirds rated social outcomes as “extremely important” [122]. Similarly, when asked what “recovery” meant to them, patients pointed to reduced pain and increased quality of life, including more satisfying relationships with others [52]. Consistent with these findings, a recent survey revealed that participation in social and family activities is among the most valued outcomes of chronic pain management [137]. These studies converge with research indicating that patient wellbeing and quality of life is not merely a matter of improved pain and physical functioning. Indeed, Sturgeon and colleagues [116] found that disruption to social relationships mediated the relationship between impaired physical functioning and emotional distress, indicating that satisfaction with social roles and relationships may be a more salient predictor of emotional wellbeing than physical functioning in patients with chronic pain.
Barriers to the measurement of social outcomes in pain management
The importance of social outcomes in the treatment of chronic pain is clear. It follows that social outcomes should be prioritised in the evaluation of pain management effectiveness. However, when the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) recommended core outcome measures for chronic pain clinical trials, interpersonal relationship functioning measures were not included among them [28]. Perhaps as a consequence, a recent systematic review [23] of 70 studies of multimodal pain therapy found that the most commonly reported outcomes were pain intensity, depressive symptoms, and physical functioning, with satisfaction with social roles and relationships reported in less than 10% of studies. Consistent with this, a 2020 survey of healthcare providers working in tertiary pain clinics found that social health outcomes were measured far less frequently than physical and mental health outcomes [137].
It is possible that the absence of social outcome measures in pain management research and practice reflects a lack of awareness of valid, reliable, and clinically relevant social outcome measures [137]. To assist clinicians and researchers in implementing social outcome measures we provide a selection of validated measures in Table 1. These measures can be accessed from the journals in which they are published, and map on to the social outcome domains that patients with chronic pain feel are most pertinent to their recovery: satisfaction with social roles and relationships, relationship functioning, family functioning, social connectedness, social support, perceived injustice, and self-care. As noted above, there is a bidirectional relationship between social experiences and pain, distress, and disability [19,73,86] (see also Figure 1). Hence, in a clinical context, what we have described here as social outcome measures may also be used to evaluate social contributors to pain and identify patients who might derive most benefit from interventions targeting social functioning (e.g., online peer-support groups [77]; relationship counselling [111]; family therapy [94]; communication skills training [74]).
Table 1.
Examples of clinically validated measures of social outcomes.
| Development Study | Instrument Name | Number of Items | Reliability | Chronic Illness Condition |
|---|---|---|---|---|
| Satisfaction with Social Roles and Relationships | ||||
| Hahn et al. [42]; Castel et al. [15] | PROMIS Satisfaction with Social Roles and Activities (v2.0) | 44 (CAT); 4, 6, 8 (Short Forms) | >.98 | Individuals with chronic heart failure, chronic obstructive pulmonary disease, chronic back pain, or depression [41]; individuals with chronic pain [116]; individuals undergoing outpatient rehabilitation [118] |
| Relationship Functioning | ||||
| Spanier [112]; Carey et al. [14] | Dyadic Adjustment Scale (DAS) | 32 | .70 – .95 | Individuals with chronic low back pain [130]; couples with chronic pain [84] |
| Busby et al. [7] | Dyadic Adjustment Scale - Revised (RDAS) | 14 | .90 | Individuals with chronic pain [17]; women with vestibulodynia [56] |
| Sabourin et al. [104] | Dyadic Adjustment Scale - Brief Version (DAS-4) | 4 | .84 | Couples with vulvodynia [101]; partners of men treated for prostate cancer [43] |
| Schwartz et al. [107] | Spouse Response Inventory (SRI) | 26 | .81 – .93 | Individuals with chronic pain [97] |
| Kerns et al. [62] | West-Haven Yale Multidimensional Pain Inventory (WHYMPI) – Part II | 14 | .74 – .84 | Individuals with chronic pain [13,34]; individuals with chronic fatigue syndrome [106]; individuals with coronary heart disease [54] |
| Locke and Wallace [72] | Locke-Wallace Marital Adjustment Test (MAT) | 15 | .90 | Individuals with chronic pain [13,34]; individuals with osteoarthritis [78,99]; couples seeking treatment for infertility [88] |
| Family Functioning | ||||
| Epstein et al. [32]; Miller et al. [83] | McMaster Family Assessment Device (FAD) | 60 | .66 – .76 | Children with chronic illness conditions [49]; children with pediatric sickle cell disease [85] |
| Social Connectedness | ||||
| Van Orden et al. [124]; Freedenthal et al. [37] | Interpersonal Needs Questionnaire (INQ-12) | 12 | >.90 | Individuals with chronic pain [58,133] |
| Hahn et al. [42] | PROMIS Social Isolation | 14 (CAT); 4, 6, 8 (Short Forms) | >.98 | Individuals with chronic pain [59,115,136] |
| Russell [102]; Hays and DiMatteo [47] | UCLA Loneliness Scale (Version 3); ULS-8 | 20 | .89 – .94; .77 | Breast cancer survivors [55] |
| Gierveld and Tilburg [39] | De Jong Gierveld Loneliness Scale | 6 | .71 – .76 | Individuals with rheumatoid arthritis [127] |
| Social Support | ||||
| Broadhead et al. [4] | Duke-UNC Functional Social Support Questionnaire | 14 | .92 | Individuals with rheumatic disease [109]; individuals with chronic pain [75] |
| Sarason et al. [105] | Brief Social Support Questionnaire (SSQ6) | 6 | .90 – .93 | Individuals with spinal cord injury [114] |
| Zimet et al. [138]; [139] | Multidimensional Scale of Perceived Social Support (MSPSS) | 12 | .85 – .91 | Individuals with multiple sclerosis [93] |
| Ware Jr and Sherbourne [128]; McHorney et al. [81] | SF-36 Social Functioning Scale | 36 | .85 | Individuals with chronic pain [31] |
| Dowrick et al. [27]; Meltzer [82]; Dalgard [21] | Oslo Social Support Scale (OSSS-3) | 3 | .66 | Individuals with chronic pain [90] |
| Hahn et al. [42]; Castel et al. [15] | PROMIS Emotional Support | 16 (CAT); 4, 6, 8 (Short Forms) | >.98 | Individuals with upper extremity disability [92]; individuals with chronic pain [66] |
| Perceived Injustice | ||||
| Sullivan et al. [117] | Injustice Experiences Questionnaire (IEQ) | 12 | .92 | Individuals with chronic pain [115,117,136], individuals who have experienced traumatic injury [120] |
| Waugh et al. [129]; Ritsher et al. [100] | Internalized Stigma of Chronic Pain Scale | 28 | .90 | Individuals with chronic pain [129]; individuals living with HIV and chronic pain [40] |
| Molina et al. [87]; Rao et al. [98] | Stigma Scale for Chronic Illness (SSCI-8) | 8 | .89 | Individuals with chronic pain [108] |
| Williams et al. [131]; Kessler et al. [65] | Lifetime Perceived Discrimination Scale | 11 | .92 | Individuals with chronic pain [5] |
| Williams et al. [131]; Kessler et al. [65] | Daily Perceived Discrimination Scale | 9 | .70 – .93 | Individuals with chronic pain [5] |
| Factors Impacting Self-Care | ||||
| Ziadni et al. [135]; Ziadni et al. [134] | CARE Scale - 7 | 7 | .81 | Individuals with mixed etiology chronic pain [134,135] |
Note: These social outcome measures may also be used to assess social contributors to pain, distress, and disability.
An additional barrier to the implementation of social outcome measures may be clinicians’ tendency to take a unidimensional approach to pain management. In a survey of healthcare providers in tertiary, multidisciplinary pain clinics [137], 89% responded that patients’ social health was not relevant to their clinical practice or was outside their scope of practice. This highlights the importance of increasing healthcare education efforts to further develop trainee understanding of and competence in identifying and managing social aspects of pain. Indeed, healthcare providers’ lack of understanding and responsiveness to the social determinants and consequences of pain may be perpetuating unconscious bias and stigma, and contributing to patients feeling disconnected from healthcare providers.
A more troubling explanation for the absence of social outcome measures in pain management research and practice may be that clinician-researchers are reluctant to know what these measures reveal about our current pain treatments’ effectiveness. The effect sizes of multidisciplinary pain management programs on pain, distress, and disability are small to moderate [57], but their effectiveness for relieving social suffering is unknown. It may be that multidisciplinary pain management programs improve the quality of patients’ social relationships by improving mood and increasing participation in social activities. However, it is also possible that the damage inflicted on patients’ social functioning cannot be mended indirectly via interventions targeted at reducing pain, distress, and disability, but instead requires interventions directly targeting repairing social relationships and connections (e.g., spouse-assisted coping skills training, conflict negotiation [12,61,79]). Multidisciplinary approaches to pain management purport to be biopsychosocial [53], but it is possible that they are failing to adequately address the social aspects of pain in meaningful ways. Documenting unmet patient needs through greater measurement of social outcomes may enhance future advocacy efforts to include social-based treatment interventions.
Finally, the relative absence of social outcome measures in pain management research and practice may reflect a pervasive tendency for outcome measures to be clinician-centred rather than patient-centred. A fundamental principle of patient-centred care is that patients are engaged the development of treatment goals that are meaningful to them. Table 1 offers clinicians and researchers a number of options for measuring social outcomes across a variety of domains that have been demonstrated to contribute to the trajectory of chronic pain and patients’ day to day quality of life. Consistent with a co-production model of research and clinical care [29,64,121], we recommend that clinicians and researchers take a patient-centered approach to selecting social outcome measures, engaging with patients to determine which of these social outcome domains are most relevant for the individual or study cohort. Future studies should focus on the relative importance of each of the identified outcome domains from the patient’s perspective.
Conclusion
Although improved social outcomes are a critical goal of pain management for patients, the social outcomes of pain management are rarely evaluated. Failing to adequately address the social functioning of patients with chronic pain may hamper the longterm effectiveness of interventions, and may be a missed opportunity to mitigate the risk of intergenerational transmission of pain within families. With greater awareness of and access to validated social outcome measures, we hope to see greater scrutiny of the social outcomes of interventions for the management of chronic pain.
Acknowledgements
This study was supported by grants from the National Institute on Drug Abuse (T32DA035165 and K24DA029262). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest.
The authors have no conflicts of interest to disclose.
References
- [1].Allen SF, Gilbody S, Atkin K, van der Feltz-Cornelis C. The associations between loneliness, social exclusion and pain in the general population: AN= 502,528 cross-sectional UK Biobank study. Journal of psychiatric research 2020;130:68–74. [DOI] [PubMed] [Google Scholar]
- [2].Boggero IA, Sturgeon JA, Arewasikporn A, Castro SA, King CD, Segerstrom SC. Associations of pain intensity and frequency with loneliness, hostility, and social functioning: Cross-sectional, longitudinal, and within-person relationships. J Behav Med 2019;26(2):217–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Brekke M, Hjortdahl P, Kvien TK. Severity of musculoskeletal pain: relations to socioeconomic inequality. Social science & medicine 2002;54(2):221–228. [DOI] [PubMed] [Google Scholar]
- [4].Broadhead W, Gehlbach SH, De Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire: Measurement of social support in family medicine patients. Medical care 1988:709–723. [DOI] [PubMed] [Google Scholar]
- [5].Brown TT, Partanen J, Chuong L, Villaverde V, Griffin AC, Mendelson A. Discrimination hurts: the effect of discrimination on the development of chronic pain. Social Science & Medicine 2018;204:1–8. [DOI] [PubMed] [Google Scholar]
- [6].Brummett BH, Barefoot JC, Siegler IC, Clapp-Channing NE, Lytle BL, Bosworth HB, Williams RB Jr, Mark DB. Characteristics of socially isolated patients with coronary artery disease who are at elevated risk for mortality. Psychosomatic medicine 2001;63(2):267–272. [DOI] [PubMed] [Google Scholar]
- [7].Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: Construct hierarchy and multidimensional scales. Journal of Marital and family Therapy 1995;21(3):289–308. [Google Scholar]
- [8].Cacioppo JT, Cacioppo S. Social relationships and health: The toxic effects of perceived social isolation. Social and personality psychology compass 2014;8(2):58–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, Hobson JA. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science 2002;13(4):384–387. [DOI] [PubMed] [Google Scholar]
- [10].Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and aging 2010;25(2):453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cano A, Gillis M, Heinz W, Geisser M, Foran H. Marital functioning, chronic pain, and psychological distress. Pain 2004;107(1–2):99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Cano A, Tankha H. Spousal criticism and hostility in response to pain: what is the alternative? Pain 2018;159(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cano A, Weisberg JN, Gallagher RM. Marital satisfaction and pain severity mediate the association between negative spouse responses to pain and depressive symptoms in a chronic pain patient sample. Pain Med 2000;1(1):35–43. [DOI] [PubMed] [Google Scholar]
- [14].Carey MP, Spector IP, Lantinga LJ, Krauss DJ. Reliability of the dyadic adjustment scale. Psychol Assess 1993;5(2):238. [Google Scholar]
- [15].Castel LD, Williams KA, Bosworth HB, Eisen SV, Hahn EA, Irwin DE, Kelly MA, Morse J, Stover A, DeWalt DA. Content validity in the PROMIS social-health domain: a qualitative analysis of focus-group data. Quality of Life Research 2008;17(5):737–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological bulletin 1985;98(2):310. [PubMed] [Google Scholar]
- [17].Costa EC, Vale S, Sobral M, Graca Pereira M. Illness perceptions are the main predictors of depression and anxiety symptoms in patients with chronic pain. Psychology, health & medicine 2016;21(4):483–495. [DOI] [PubMed] [Google Scholar]
- [18].Coyne JC, DeLongis A. Going beyond social support: the role of social relationships in adaptation. Journal of consulting and clinical psychology 1986;54(4):454. [DOI] [PubMed] [Google Scholar]
- [19].Craig KD. The social communication model of pain. Canadian Psychology/Psychologie canadienne 2009;50(1):22. [Google Scholar]
- [20].Craig KD, Holmes C, Hudspith M, Moor G, Moosa-Mitha M, Varcoe C, Wallace B. Pain in persons who are marginalized by social conditions. Pain 2020;161(2):261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Dalgard O. Community health profile as tool for psychiatric prevention. Promotion of mental health 1996;5:681–695. [Google Scholar]
- [22].De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain 2016;157(8):1607–1610. [DOI] [PubMed] [Google Scholar]
- [23].Deckert S, Kaiser U, Kopkow C, Trautmann F, Sabatowski R, Schmitt J. A systematic review of the outcomes reported in multimodal pain therapy for chronic pain. Eur J Pain 2016;20(1):51–63. [DOI] [PubMed] [Google Scholar]
- [24].Dennis CH, Clohessy DS, Stone AL, Darnall BD, Wilson AC. Adverse childhood experiences in mothers with chronic pain and intergenerational impact on children. J Pain 2019;20(10):1209–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol 2004;23(2):207. [DOI] [PubMed] [Google Scholar]
- [26].Dixon D, Cruess S, Kilbourn K, Klimas N, Fletcher MA, Ironson G, Baum A, Schneiderman N, Antoni MH. Social support mediates loneliness and human herpesvirus type 6 (HHV‐6) antibody titers. Journal of applied social psychology 2001;31(6):1111–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Dowrick C, Casey P, Dalgard O, Hosman C, Lehtinen V, Vázquez-Barquero J-L, Wilkinson G. Outcomes of Depression International Network (ODIN): background, methods and field trials. The British Journal of Psychiatry 1998;172(4):359–363. [DOI] [PubMed] [Google Scholar]
- [28].Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113(1):9–19. [DOI] [PubMed] [Google Scholar]
- [29].editorial N The best research is produced when researchers and communities work together. Nature 2018;562(7). [DOI] [PubMed] [Google Scholar]
- [30].Eisenberger NI, Moieni M, Inagaki TK, Muscatell KA, Irwin MR. In sickness and in health: the co-regulation of inflammation and social behavior. Neuropsychopharmacology 2017;42(1):242–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Elliott TE, Renier CM, Palcher JA. Chronic pain, depression, and quality of life: correlations and predictive value of the SF-36. Pain Med 2003;4(4):331–339. [DOI] [PubMed] [Google Scholar]
- [32].Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. Journal of marital and family therapy 1983;9(2):171–180. [Google Scholar]
- [33].Evers AW, Kraaimaat FW, Geenen R, Jacobs JW, Bijlsma JW. Pain coping and social support as predictors of long-term functional disability and pain in early rheumatoid arthritis. Behaviour research and therapy 2003;41(11):1295–1310. [DOI] [PubMed] [Google Scholar]
- [34].Flor H, Turk DC, Rudy TE. Relationship of pain impact and significant other reinforcement of pain behaviors: The mediating role of gender, marital status and marital satisfaction. Pain 1989;38(1):45–50. [DOI] [PubMed] [Google Scholar]
- [35].Flor H, Turk DC, Scholz OB. Impact of chronic pain on the spouse: Marital, emotional and physical consequences. Journal of psychosomatic research 1987;31(1):63–71. [DOI] [PubMed] [Google Scholar]
- [36].Forgeron PA, King S, Stinson JN, McGrath PJ, MacDonald AJ, Chambers CT. Social functioning and peer relationships in children and adolescents with chronic pain: A systematic review. Pain Research and Management 2010;15(1):27–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Freedenthal S, Lamis DA, Osman A, Kahlo D, Gutierrez PM. Evaluation of the psychometric properties of the Interpersonal Needs Questionnaire‐12 in samples of men and women. Journal of Clinical Psychology 2011;67(6):609–623. [DOI] [PubMed] [Google Scholar]
- [38].Froud R, Patterson S, Eldridge S, Seale C, Pincus T, Rajendran D, Fossum C, Underwood M. A systematic review and meta-synthesis of the impact of low back pain on people’s lives. BMC musculoskeletal disorders 2014;15(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Gierveld JDJ, Tilburg TV. A 6-item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Research on aging 2006;28(5):582–598. [Google Scholar]
- [40].Goodin BR, Owens MA, White DM, Strath LJ, Gonzalez C, Rainey RL, Okunbor JI, Heath SL, Turan JM, Merlin JS. Intersectional health-related stigma in persons living with HIV and chronic pain: implications for depressive symptoms. AIDS care 2018;30(sup2):66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Hahn EA, Beaumont JL, Pilkonis PA, Garcia SF, Magasi S, DeWalt DA, Cella D. The PROMIS satisfaction with social participation measures demonstrated responsiveness in diverse clinical populations. J Clin Epidemiol 2016;73:135–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hahn EA, DeVellis RF, Bode RK, Garcia SF, Castel LD, Eisen SV, Bosworth HB, Heinemann AW, Rothrock N, Cella D. Measuring social health in the patient-reported outcomes measurement information system (PROMIS): item bank development and testing. Quality of Life Research 2010;19(7):1035–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Harden JK, Sanda MG, Wei JT, Yarandi H, Hembroff L, Hardy J, Northouse LL, Group PCS. Partners’ long-term appraisal of their caregiving experience, marital satisfaction, sexual satisfaction, and quality of life 2 years after prostate cancer treatment. Cancer nursing 2013;36(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Hawe P, Shiell A. Social capital and health promotion: a review. Social science & medicine 2000;51(6):871–885. [DOI] [PubMed] [Google Scholar]
- [45].Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: cross-sectional & longitudinal analyses. Health Psychol 2009;28(3):354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Hayaki C, Anno K, Shibata M, Iwaki R, Kawata H, Sudo N, Hosoi M. Family dysfunction: A comparison of chronic widespread pain and chronic localized pain. Medicine 2016;95(49). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Hays RD, DiMatteo MR. A short-form measure of loneliness. Journal of personality assessment 1987;51(1):69–81. [DOI] [PubMed] [Google Scholar]
- [48].Heiskanen T, Roine RP, Kalso E. Multidisciplinary pain treatment–Which patients do benefit? Scandinavian journal of pain 2012;3(4):201–207. [DOI] [PubMed] [Google Scholar]
- [49].Herzer M, Godiwala N, Hommel KA, Driscoll K, Mitchell M, Crosby LE, Piazza-Waggoner C, Zeller MH, Modi AC. Family functioning in the context of pediatric chronic conditions. Journal of developmental and behavioral pediatrics: JDBP 2010;31(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Hoftun GB, Romundstad PR, Rygg M. Association of parental chronic pain with chronic pain in the adolescent and young adult: family linkage data from the HUNT Study. JAMA pediatrics 2013;167(1):61–69. [DOI] [PubMed] [Google Scholar]
- [51].Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS medicine 2010;7(7):e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Hush JM, Refshauge K, Sullivan G, De Souza L, Maher CG, McAuley JH. Recovery: what does this mean to patients with low back pain? Arthritis Care & Research 2009;61(1):124–131. [DOI] [PubMed] [Google Scholar]
- [53].IASP. Multidisciplinary Pain Center Development Manual: IASP Multidisciplinary Pain Center Toolkit Advisory Group, 2021. [Google Scholar]
- [54].Itkowitz NI, Kerns RD, Otis JD. Support and coronary heart disease: the importance of significant other responses. Journal of behavioral medicine 2003;26(1):19–30. [DOI] [PubMed] [Google Scholar]
- [55].Jaremka LM, Fagundes CP, Glaser R, Bennett JM, Malarkey WB, Kiecolt-Glaser JK. Loneliness predicts pain, depression, and fatigue: understanding the role of immune dysregulation. Psychoneuroendocrinology 2013;38(8):1310–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Jodoin M, Bergeron S, Khalifé S, Dupuis M-J, Desrochers G, Leclerc B. Attributions about pain as predictors of psychological symptomatology, sexual function, and dyadic adjustment in women with vestibulodynia. Archives of Sexual Behavior 2011;40(1):87–97. [DOI] [PubMed] [Google Scholar]
- [57].Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, Van Tulder M. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. Bmj 2015;350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Kanzler KE, Bryan CJ, McGeary DD, Morrow CE. Suicidal ideation and perceived burdensomeness in patients with chronic pain. Pain Practice 2012;12(8):602–609. [DOI] [PubMed] [Google Scholar]
- [59].Karayannis NV, Baumann I, Sturgeon JA, Melloh M, Mackey SC. The impact of social isolation on pain interference: a longitudinal study. Annals of Behavioral Medicine 2019;53(1):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Karos K, Williams ACdC, Meulders A, Vlaeyen JW. Pain as a threat to the social self: a motivational account. Pain 2018;159(9):1690–1695. [DOI] [PubMed] [Google Scholar]
- [61].Keefe FJ, Caldwell DS, Baucom D, Salley A, Robinson E, Timmons K, Beaupre P, Weisberg J, Helms M. Spouse‐assisted coping skills training in the management of osteoarthritic knee pain. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology 1996;9(4):279–291. [DOI] [PubMed] [Google Scholar]
- [62].Kerns RD, Turk DC, Rudy TE. The west haven-yale multidimensional pain inventory (WHYMPI). Pain 1985;23(4):345–356. [DOI] [PubMed] [Google Scholar]
- [63].Kerns RD, Weiss LH. Family influences on the course of chronic illness: A cognitive-behavioral transactional model. Annals of Behavioral Medicine 1994;16(2):116–121. [Google Scholar]
- [64].Kertesz SG, McCullough MB, Darnall BD, Varley AL. Promoting Patient-Centeredness in Opioid Deprescribing: a Blueprint for De-implementation Science. Journal of General Internal Medicine 2020;35(3):972–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of health and social behavior 1999:208–230. [PubMed] [Google Scholar]
- [66].Khan JS, Hah JM, Mackey SC. Effects of smoking on patients with chronic pain: a propensity-weighted analysis on the Collaborative Health Outcomes Information Registry. Pain 2019;160(10):2374–2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Kowal J, Wilson KG, McWilliams LA, Péloquin K, Duong D. Self-perceived burden in chronic pain: relevance, prevalence, and predictors. PAIN® 2012;153(8):1735–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Lamu AN, Olsen JA. The relative importance of health, income and social relations for subjective well-being: An integrative analysis. Social Science & Medicine 2016;152:176–185. [DOI] [PubMed] [Google Scholar]
- [69].Leonard MT, Cano A. Pain affects spouses too: Personal experience with pain and catastrophizing as correlates of spouse distress. Pain 2006;126(1–3):139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Leonard MT, Cano A, Johansen AB. Chronic pain in a couples context: a review and integration of theoretical models and empirical evidence. J Pain 2006;7(6):377–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Lett HS, Blumenthal JA, Babyak MA, Catellier DJ, Carney RM, Berkman LF, Burg MM, Mitchell P, Jaffe AS, Schneiderman N. Social support and prognosis in patients at increased psychosocial risk recovering from myocardial infarction. Health Psychol 2007;26(4):418. [DOI] [PubMed] [Google Scholar]
- [72].Locke HJ, Wallace KM. Short marital-adjustment and prediction tests: Their reliability and validity. Marriage and family living 1959;21(3):251–255. [Google Scholar]
- [73].Loeffler A, Steptoe A. Bidirectional longitudinal associations between loneliness and pain, and the role of inflammation. Pain 2021;162(3):930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Lonsdale C, Hall AM, Murray A, Williams GC, McDonough SM, Ntoumanis N, Owen K, Schwarzer R, Parker P, Kolt GS. Communication skills training for practitioners to increase patient adherence to home-based rehabilitation for chronic low back pain: results of a cluster randomized controlled trial. Archives of physical medicine and rehabilitation 2017;98(9):1732–1743. e1737. [DOI] [PubMed] [Google Scholar]
- [75].López-Martínez AE, Esteve-Zarazaga R, Ramírez-Maestre C. Perceived social support and coping responses are independent variables explaining pain adjustment among chronic pain patients. J Pain 2008;9(4):373–379. [DOI] [PubMed] [Google Scholar]
- [76].Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: A national longitudinal study. Social science & medicine 2012;74(6):907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Mariano TY, Wan L, Edwards RR, Jamison RN. Online teletherapy for chronic pain: a systematic review. Journal of telemedicine and telecare 2021;27(4):195–208. [DOI] [PubMed] [Google Scholar]
- [78].Martire LM, Keefe FJ, Schulz R, Ready R, Beach SR, Rudy TE, Starz TW. Older spouses’ perceptions of partners’ chronic arthritis pain: Implications for spousal responses, support provision, and caregiving experiences. Psychology and aging 2006;21(2):222. [DOI] [PubMed] [Google Scholar]
- [79].Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of behavioral medicine 2010;40(3):325–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Martire LM, Zhaoyang R, Marini CM, Nah S, Darnall BD. Daily and bidirectional linkages between pain catastrophizing and spouse responses. Pain 2019;160(12):2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].McHorney CA, Ware JE Jr, Lu JR, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical care 1994:40–66. [DOI] [PubMed] [Google Scholar]
- [82].Meltzer H Development of a common instrument for mental health, Novisky i and Gudex(eds.) EUROHIS: Developing Common Instruments for Health Surveys: IOS Press, 2003. [Google Scholar]
- [83].Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster family assessment device: reliability and validity. Journal of Marital and Family Therapy 1985;11(4):345–356. [Google Scholar]
- [84].Miller LR, Cano A, Wurm LH. A motivational therapeutic assessment improves pain, mood, and relationship satisfaction in couples with chronic pain. J Pain 2013;14(5):525–537. [DOI] [PubMed] [Google Scholar]
- [85].Mitchell MJ, Lemanek K, Palermo TM, Crosby LE, Nichols A, Powers SW. Parent perspectives on pain management, coping, and family functioning in pediatric sickle cell disease. Clinical Pediatrics 2007;46(4):311–319. [DOI] [PubMed] [Google Scholar]
- [86].Mogil JS. Social modulation of and by pain in humans and rodents. Pain 2015;156:S35–S41. [DOI] [PubMed] [Google Scholar]
- [87].Molina Y, Choi SW, Cella D, Rao D. The stigma scale for chronic illnesses 8-item version (SSCI-8): development, validation and use across neurological conditions. J Behav Med 2013;20(3):450–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology 2004;63(1):126–130. [DOI] [PubMed] [Google Scholar]
- [89].Murphy BM, Elliott PC, Le Grande MR, Higgins RO, Ernest CS, Goble AJ, Tatoulis J, Worcester MU. Living alone predicts 30-day hospital readmission after coronary artery bypass graft surgery. European Journal of Preventive Cardiology 2008;15(2):210–215. [DOI] [PubMed] [Google Scholar]
- [90].Newton-John TR, Mason C, Hunter M. The role of resilience in adjustment and coping with chronic pain. Rehabil Psychol 2014;59(3):360. [DOI] [PubMed] [Google Scholar]
- [91].Noll RB, Reiter-Purtill J, Vannatta K, Gerhardt CA, Short A. Peer relationships and emotional well-being of children with sickle cell disease: A controlled replication. Child Neuropsychology 2007;13(2):173–187. [DOI] [PubMed] [Google Scholar]
- [92].Nota SP, Spit SA, Oosterhoff TC, Hageman MG, Ring DC, Vranceanu A-M. Is social support associated with upper extremity disability? Clinical Orthopaedics and Related Research® 2016;474(8):1830–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Osborne TL, Jensen MP, Ehde DM, Hanley MA, Kraft G. Psychosocial factors associated with pain intensity, pain-related interference, and psychological functioning in persons with multiple sclerosis and pain. Pain 2007;127(1–2):52–62. [DOI] [PubMed] [Google Scholar]
- [94].Palermo TM, Wilson AC, Peters M, Lewandowski A, Somhegyi H. Randomized controlled trial of an Internet-delivered family cognitive–behavioral therapy intervention for children and adolescents with chronic pain. Pain 2009;146(1–2):205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Payne B, Norfleet MA. Chronic pain and the family: a review. Pain 1986;26(1):1–22. [DOI] [PubMed] [Google Scholar]
- [96].Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychol 2005;24(3):297. [DOI] [PubMed] [Google Scholar]
- [97].Raichle KA, Romano JM, Jensen MP. Partner responses to patient pain and well behaviors and their relationship to patient pain behavior, functioning, and depression. PAIN® 2011;152(1):82–88. [DOI] [PubMed] [Google Scholar]
- [98].Rao D, Choi SW, Victorson D, Bode R, Peterman A, Heinemann A, Cella D. Measuring stigma across neurological conditions: the development of the stigma scale for chronic illness (SSCI). Quality of life research 2009;18(5):585–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Reese JB, Somers TJ, Keefe FJ, Mosley-Williams A, Lumley MA. Pain and functioning of rheumatoid arthritis patients based on marital status: is a distressed marriage preferable to no marriage? J Pain 2010;11(10):958–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry research 2003;121(1):31–49. [DOI] [PubMed] [Google Scholar]
- [101].Rosen NO, Bois K, Mayrand M-H, Vannier S, Bergeron S. Observed and perceived disclosure and empathy are associated with better relationship adjustment and quality of life in couples coping with vulvodynia. Archives of Sexual Behavior 2016;45(8):1945–1956. [DOI] [PubMed] [Google Scholar]
- [102].Russell DW. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of personality assessment 1996;66(1):20–40. [DOI] [PubMed] [Google Scholar]
- [103].Sabbioni ME, Eugster S. Interactions of a history of migration with the course of pain disorder. Journal of psychosomatic research 2001;50(5):267–269. [DOI] [PubMed] [Google Scholar]
- [104].Sabourin S, Valois P, Lussier Y. Development and validation of a brief version of the dyadic adjustment scale with a nonparametric item analysis model. Psychol Assess 2005;17(1):15. [DOI] [PubMed] [Google Scholar]
- [105].Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: Practical and theoretical implications. Journal of social and personal relationships 1987;4(4):497–510. [Google Scholar]
- [106].Schmaling KB, Smith WR, Buchwald DS. Significant other responses are associated with fatigue and functional status among patients with chronic fatigue syndrome. Psychosomatic Medicine 2000;62(3):444–450. [DOI] [PubMed] [Google Scholar]
- [107].Schwartz L, Jensen MP, Romano JM. The development and psychometric evaluation of an instrument to assess spouse responses to pain and well behavior in patients with chronic pain: The Spouse Response Inventory. J Pain 2005;6(4):243–252. [DOI] [PubMed] [Google Scholar]
- [108].Scott W, Yu L, Patel S, McCracken LM. Measuring stigma in chronic pain: Preliminary investigation of instrument psychometrics, correlates, and magnitude of change in a prospective cohort attending interdisciplinary treatment. J Pain 2019;20(10):1164–1175. [DOI] [PubMed] [Google Scholar]
- [109].Shim E-J, Song YW, Park S-H, Lee K-M, Go DJ, Hahm B-J. Examining the relationship between pain catastrophizing and suicide risk in patients with rheumatic disease: the mediating role of depression, perceived social support, and perceived burdensomeness. J Behav Med 2017;24(4):501–512. [DOI] [PubMed] [Google Scholar]
- [110].Slavich GM. Social safety theory: a biologically based evolutionary perspective on life stress, health, and behavior. Annual review of clinical psychology 2020;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Smith SM, Li R, Wolfe H, Swanger-Gagne MS, Bonham AD, Kreher DA, Poleshuck EL. Couple Interventions for Chronic Pain. Clin J Pain 2019;35(11):916–922. [DOI] [PubMed] [Google Scholar]
- [112].Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family 1976:15–28. [Google Scholar]
- [113].Strine TW, Okoro CA, McGuire LC, Balluz LS. The associations among childhood headaches, emotional and behavioral difficulties, and health care use. Pediatrics 2006;117(5):1728–1735. [DOI] [PubMed] [Google Scholar]
- [114].Stroud MW, Turner JA, Jensen MP, Cardenas DD. Partner responses to pain behaviors are associated with depression and activity interference among persons with chronic pain and spinal cord injury. J Pain 2006;7(2):91–99. [DOI] [PubMed] [Google Scholar]
- [115].Sturgeon JA, Carriere JS, Kao M-CJ, Rico T, Darnall BD, Mackey SC. Social disruption mediates the relationship between perceived injustice and anger in chronic pain: a collaborative health outcomes information registry study. Annals of Behavioral Medicine 2016;50(6):802–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Sturgeon JA, Dixon EA, Darnall BD, Mackey SC. Contributions of physical function and satisfaction with social roles to emotional distress in chronic pain: a Collaborative Health Outcomes Information Registry (CHOIR) study. Pain 2015;156(12):2627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [117].Sullivan MJ, Adams H, Horan S, Maher D, Boland D, Gross R. The role of perceived injustice in the experience of chronic pain and disability: scale development and validation. Journal of occupational rehabilitation 2008;18(3):249–261. [DOI] [PubMed] [Google Scholar]
- [118].Tamminga SJ, van Vree FM, Volker G, Roorda LD, Terwee CB, Goossens PH, Vlieland TPV. Changes in the ability to participate in and satisfaction with social roles and activities in patients in outpatient rehabilitation. Journal of Patient-Reported Outcomes 2020;4(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Tardif H, Arnold C, Hayes C, Eagar K. Establishment of the Australasian electronic persistent pain outcomes collaboration. Pain Med 2017;18(6):1007–1018. [DOI] [PubMed] [Google Scholar]
- [120].Trost Z, Agtarap S, Scott W, Driver S, Guck A, Roden-Foreman K, Reynolds M, Foreman ML, Warren AM. Perceived injustice after traumatic injury: Associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabil Psychol 2015;60(3):213. [DOI] [PubMed] [Google Scholar]
- [121].Turakhia P, Combs B. Using principles of co-production to improve patient care and enhance value. AMA journal of ethics 2017;19(11):1125–1131. [DOI] [PubMed] [Google Scholar]
- [122].Turk DC, Dworkin RH, Revicki D, Harding G, Burke LB, Cella D, Cleeland CS, Cowan P, Farrar JT, Hertz S. Identifying important outcome domains for chronic pain clinical trials: an IMMPACT survey of people with pain. PAIN® 2008;137(2):276–285. [DOI] [PubMed] [Google Scholar]
- [123].Van Damme S, Crombez G, Eccleston C. Coping with pain: a motivational perspective. Pain 2008;139(1):1–4. [DOI] [PubMed] [Google Scholar]
- [124].Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE Jr. Suicidal desire and the capability for suicide: Tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of consulting and clinical psychology 2008;76(1):72. [DOI] [PubMed] [Google Scholar]
- [125].Vannatta K, Getzoff EA, Powers SW, Noll RB, Gerhardt CA, Hershey AD. Multiple perspectives on the psychological functioning of children with and without migraine. Headache: The Journal of Head and Face Pain 2008;48(7):994–1004. [DOI] [PubMed] [Google Scholar]
- [126].Wallace LS, Wexler RK, McDougle L, Miser WF, Haddox JD. Voices that may not otherwise be heard: a qualitative exploration into the perspectives of primary care patients living with chronic pain. J Pain Res 2014;7:291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Waltz M, Kriegel W, Bosch PVTP. The social environment and health in rheumatoid arthritis: marital quality predicts individual variability in pain severity. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology 1998;11(5):356–374. [DOI] [PubMed] [Google Scholar]
- [128].Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical care 1992:473–483. [PubMed] [Google Scholar]
- [129].Waugh OC, Byrne DG, Nicholas MK. Internalized stigma in people living with chronic pain. J Pain 2014;15(5):550. e551,–550. e510. [DOI] [PubMed] [Google Scholar]
- [130].Waxman SE, Tripp DA, Flamenbaum R. The mediating role of depression and negative partner responses in chronic low back pain and relationship satisfaction. J Pain 2008;9(5):434–442. [DOI] [PubMed] [Google Scholar]
- [131].Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of health psychology 1997;2(3):335–351. [DOI] [PubMed] [Google Scholar]
- [132].Wilson AC, Stone AL, Poppert Cordts KM, Holley AL, Mackey S, Darnall BD, Palermo TM. Baseline Characteristics of a Dyadic Cohort of Mothers With Chronic Pain and Their Children. Clin J Pain 2020;36(10):782–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [133].Wilson KG, Heenan A, Kowal J, Henderson PR, McWilliams LA, Castillo D. Testing the interpersonal theory of suicide in chronic pain. Clin J Pain 2017;33(8):699–706. [DOI] [PubMed] [Google Scholar]
- [134].Ziadni M, You DS, Chen A, Wilson AC, Darnall BD. Validation of CARE Scale-7 in treatment-seeking patients with chronic pain: measurement of sex invariance. Pain reports 2020;5(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Ziadni M, You DS, Wilson AC, Darnall BD. CARE Scale-7: Development and preliminary validation of a measure to assess factors impacting self-care in chronic pain. Clin J Pain 2018;34(9):818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Ziadni MS, You DS, Sturgeon JA, Mackey SC, Darnall BD. Perceived Injustice Mediates the Relationship Between Perceived Childhood Neglect and Current Function in Patients with Chronic Pain: A Preliminary Pilot Study. Journal of clinical psychology in medical settings 2020:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Zidarov D, Zidarova-Carrié A, Visca R, Miller JM, Brecht K, Viens N, Ahmed S. Core patient-reported outcome domains for routine clinical care in chronic pain management: patients’ and healthcare professionals’ perspective. Quality of Life Research 2020;29(7):2007–2020. [DOI] [PubMed] [Google Scholar]
- [138].Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. Journal of personality assessment 1988;52(1):30–41. [DOI] [PubMed] [Google Scholar]
- [139].Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. Journal of personality assessment 1990;55(3–4):610–617. [DOI] [PubMed] [Google Scholar]


