Abstract
Background: Coronary artery disease is the most common cause of death worldwide as well as in Iran. The present study was designed to predict short and long-term survival rates after the first episode of myocardial infarction (MI).
Methods: The current research is a retrospective cohort study. The data were collected from the Myocardial Infarction Registry of Iran in a 12-month period leading to March 20, 2014. The variables analyzed included smoking status, past medical history of chronic heart disease, hypertension, diabetes, hyperlipidemia, signs and symptoms during an attack, post-MI complications during hospitalization, the occurrence of arrhythmias, the location of MI, and the place of residence. Survival rates and predictive factors were estimated by the Kaplan–Meier method, the log-rank test, and the Cox model.
Results: Totally, 21 181 patients with the first MI were studied. There were 15 328 men (72.4%), and the mean age of the study population was 62.10±13.42 years. During a 1-year period following MI, 2479 patients (11.7%) died. Overall, the survival rates at 28 days, 6 months, and 1 year were estimated to be 0.95 (95% CI: 0.95 to 0.96), 0.90 (95% CI: 0.90 to 0.91), and 0.88 (95% CI: 0.88 to 0.89). After the confounding factors were controlled, history of chronic heart disease (p<0.001), hypertension (p<0.001), and diabetes (p<0.001) had a significant relationship with an increased risk of death and history of hyperlipidemia (p<0.001) and inferior wall MI (p<0.001) had a significant relationship with a decreased risk of death.
Conclusion: The results of this study provide evidence for health policy-makers and physicians on the link between MI and its predictive factors.
Key Words: Cox Regression, Myocardial infarction, Survival rate, Hypertension
Introduction
Cardiovascular diseases (CVDs) constitute the most common cause of death in most countries of the world and Iran.1 In the past 2 decades, CVD-induced mortality has grown remarkably in low-middle income countries (over 3/4 of CVDs deaths), while it has declined in high-income nations.2 It has been predicted that by 2030, CVDs will remain the first cause of death worldwide, and almost 23.6 million people will have died from this illness.3 Despite advances in therapeutic approaches and a significant drop in the prevalence of coronary heart disease, the case fatality rate following the incidence of myocardial infarction (MI) in both sexes has remained high.4-6 According to the reports by the Iranian Ministry of Health, in 2013, 39% of the deaths were due to CVDs, and the mortality rate following MI was 85 per 100 000. CVDs are generally manifested by MI, and the World Health Organization (WHO) has suggested that in epidemiologic studies, the rate of MI be used as a proxy for CVDs.7 The type and location of MI are significant prognostic factors for predicting post-MI mortality.8
As the WHO MONICA project results suggest, MI attacks during the first 28 days are not considered separate; and if a person dies from one of these potential attacks in the first 28 days, his/her death should be considered due to the first attack.9
Repetition of cardiovascular accidents is common after the first occurrence in the first 6 months. Therefore, follow-ups for a longer period are necessary to show the impact of factors affecting survival.
Some studies have determined survival rates in Iranian provinces.10, 11 However, none of them has been population-based to consider the whole country using MI registry data. Accordingly, we designed this retrospective cohort study to predict short and long-term survival rates in patients with MI and its contributing factors in Iran based on the Iranian Myocardial Infarction Registry.
Methods
The current research is a retrospective cohort study, where the data were collected from 21 181 cases of MI recorded by the Iranian Myocardial Infarction Registry in a 12-month period leading to March 20, 2014.
The Iranian Myocardial Infarction Registry was established in 2009 by the Office of Cardiovascular Diseases of the Iranian Ministry of Health. The coverage of the registry was almost complete and applicable countrywide. The registry covers all hospitals (governmental, private, and military hospitals) equipped with a coronary care unit in all 31 Iranian provinces.
The variables analyzed were smoking status, past medical history of chronic heart disease/hypertension/ diabetes/hyperlipidemia, signs and symptoms during an attack, post-MI complications during hospitalization, the occurrence of arrhythmias, the location of MI, and the place of residence. The data regarding all these variables were collected during the hospitalization period.
The definition and diagnosis of patients with MI were based on the recommendations by the WHO, the International Classification of Diseases (ICD10), version 2016, codes from I21.0 to I21.9, and the past medical history of risk factors registered according to the reports of patients taking medications.
The ICD10 assigns a specific code to each location of acute MI: I21.0 to acute transmural MI of the anterior wall, I21.1 to acute transmural MI of the inferior wall, I21.2 to acute transmural MI of other sites, I21.3 to acute transmural MI of an unspecified site, I21.4 to acute subendocardial MI, and I21.9 to acute MI of an unspecified site.
Patients with no national codes or definite diagnoses by cardiologists were excluded from the study.
The follow-up of the patients commenced after hospitalization. Patients who died before hospital admission were not included in the study. The last point of follow-up was the time of death for all causes or administrative right censoring.
The survival or death status was obtained 3 years after hospitalization by the cross-match of the national codes of the patients in the Iranian Myocardial Infarction Registry and the National Organization for CIVIL Registration. If the patient’s national code was also registered in the National Organization for CIVIL Registration as a dead person, the date of death was extracted; otherwise, the patient was considered alive at the end of the follow-up.
The Ethics Committee of Shahid Beheshti University of Medical Sciences approved this study.
Survival rates were estimated by the Kaplan–Meier method, and P-values for the comparison of survival curves were determined by the log-rank test. Continuous variables were presented as the mean±the standard deviation (SD). Categorical variables were summarized as frequencies and percentages. For the comparison of the average age between the 2 sexes, the independent t-test was used. All the statistical tests were 2-tailed tests, and P-values<0.05 were considered significant.
Univariate and multivariate Cox models were used to investigate the relationship between the research variables and time to death. Variables with P-values≤0.20 and variables whose role was important from the point of view of confounding in the univariate analysis were entered into the multivariate analysis, and the adjusted hazard ratio (HR) for all the variables was calculated. For the fine adjustment of age as a major confounder, age was considered the origin of the risk time in the Cox analysis using Stata. The evaluation of the proportional hazard assumption was based on the Schoenfeld residuals. The analyses were performed using Stata software, version 14.
Results
Totally, 21 181 patients were studied with the first attack of MI in this survey. There were 15 328 men (72.4%) and 5853 women (27.6%). The mean age of the overall patient population was 62.10±13.42 years. The most frequent age group was that of 55–60 years. (14.3%), and most of the patients (46.4%) were uneducated. Before MI, 14 888 patients (70.3%) had some signs and symptoms such as dyspnea, sweating, vomiting/nausea, chest pain, left arm pain, and jaw pain, with the most common symptoms being left arm pain (46.6%), sweating (40.4%), and dyspnea (32%).
Hypertension, diabetes, and chronic heart disease were the most common risk factors among the patients. During the hospitalization, the most frequent complication was heart failure (7.9%), and the most prevalent type of arrhythmia was ventricular tachycardia (4.1%). The most common MI location was the transmural MI of the anterior wall (31.9%), followed by the transmural MI of the inferior wall (28.8%), subendocardial MI (14.9%), and the transmural MI of other sites (2.2%).
During a 1-year period following MI, 2479 patients (11.7%) died. Overall, survival rates at 28 days, 6 months, and 1 year were estimated to be 0.95 (95% CI: 0.95 to 0.96), 0.90 (95% CI: 0.90 to 0.91), and 0.88 (95% CI: 0.88 to 0.89).
Patients in the age group of 30–45 years had the highest short-term survival rate (28 d). In the lower age groups, because of the small number of patients, survival rates were not estimated. The highest long-term survival rate (1 y) was estimated in the age group of 35–45 years.
Patients with a past medical history of cigarette smoking had higher short and long-term survival rates than nonsmokers, and patients with a past medical history of chronic heart disease had lower short and long-term survival rates than those with no history of chronic heart disease.
Figure 1 illustrates survival rates according to different risk factors.
Figure 1.
The images illustrate comparisons of survival curves after myocardial infarction for patients with/without risk factors.
Concerning MI locations, patients with acute transmural MI of the anterior wall, the inferior wall, and other sites had the lowest survival rate, and those with acute transmural MI of the inferior wall had the highest survival rate. Table 1 presents descriptive information and survival rates by sex, risk factor, and MI location in the study patients.
Table 1.
Baseline characteristics and survival rates by sex, myocardial infarction location, and risk factors in patients hospitalized for myocardial infarction
| Frequency (%) | 28-Day Survival Rate (95% CI) |
6-Month Survival Rate (95% CI) |
1-Year Survival Rate (95% CI) |
Adjusted HR* (95% CI) |
P | |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 15328 (72.4%) | 0.96 (0.96-0.97) | 0.92 (0.91-0.93) | 0.90 (0.89-0.91) | Reference | |
| Female | 5853 (27.6%) | 0.93 (0.92-0.93) | 0.86 (0.85-0.87) | 0.83 (0.82-0.83) | 1.065 (0.99-1.14) | 0.082 |
| Past Medical History | ||||||
| Chronic heart disease (Yes) | 4447 (21.1%) | 0.93 (0.92-0.94) | 0.86 (0.85-0.87) | 0.83 (0.81-0.84) | 1.35 (1.26-1.45) | <0.001. |
| Hypertension (Yes) | 7656 (36.2%) | 0.94 (0.93-0.94) | 0.87 (0.86-0.88) | 0.84 (0.83-0.85) | 1.15 (1.08-1.23) | <0.001. |
| Diabetes (Yes) | 4820 (22.8%) | 0.94 (0.93-0.94) | 0.87 (0.86-0.88) | 0.84 (0.83-0.85) | 1.52 (1.41-1.64) | <0.001. |
| Hyperlipidemia (Yes) | 3818 (18.1%) | 0.95 (0.94-0.96) | 0.90 (0.88-0.91) | 0.88 (0.86-0.90) | 0.85 (0.78-0.93) | <0.001. |
| Cigarette smoking (Yes) | 6030 (28.5%) | 0.96 (0.96-0.97) | 0.93 (0.92-0.93) | 0.91 (0.90-0.92) | 0.93 (0.86-1.01) | 0.901 |
| Location of Myocardial Infarction | ||||||
| Acute subendocardial myocardial infarction |
3155 (14.9%) | 0.96 (0.95-0.96) | 0.90 (0.88-0.91) | 0.86 (0.85-0.87) | ||
| Acute transmural myocardial infarction of other sites |
477 (2.3%) | 0.96 (0.93-0.97) | 0.90 (0.86-0.92) | 0.89 (0.86-0.91) | 0.90 (0.72-1.14) | 0.391 |
| Acute transmural myocardial infarction of the inferior wall |
6094 (28.8%) | 0.96 (0.95-0.97) | 0.92 (0.91-0.93) | 0.91 (0.90-0.92) | 0.80 (0.73-0.89) | <0.001. |
| Acute transmural myocardial infarction of the anterior wall |
6737 (31.9%) | 0.95 (0.94-0.96) | 0.89 (0.88-0.90) | 0.87 (0.86-0.88) | 1.05 (0.95-1.14) | 0.333 |
| Acute transmural myocardial infarction of the anterior wall, the inferior wall, and other sites |
130 (0.6%) | 0.88 (0.81-0.92) | 0.77 (0.68-0.73) | 0.74 (0.66-0.81) | 1.38 (0.99-1.94) | 0.064 |
Every variable is adjusted for the contextual variables (viz, sex education, past medical history of chronic heart disease, hypertension/diabetes/hyperlipidemia, treatment with percutaneous coronary intervention/coronary artery bypass grafting surgery, and smoking), symptoms before myocardial infarction, arrhythmia, complications, medications received, and myocardial infarction location.
The results of the Cox analysis showed that after the control of confounding factors, history of chronic heart disease (HR, 1.35; p<0.001), hypertension (HR, 1.15; p<0.001), and diabetes (HR, 1.52; p<0.001) had a significant relationship with an increased risk of death due to MI, and history of hyperlipidemia (HR, 0.85; p<0.001) and MI of the inferior wall (HR, 0.80; p<0.001) had a significant relationship with a decreased risk of death due to MI.
The HR of the different variables for death due to MI is shown in Table 1.
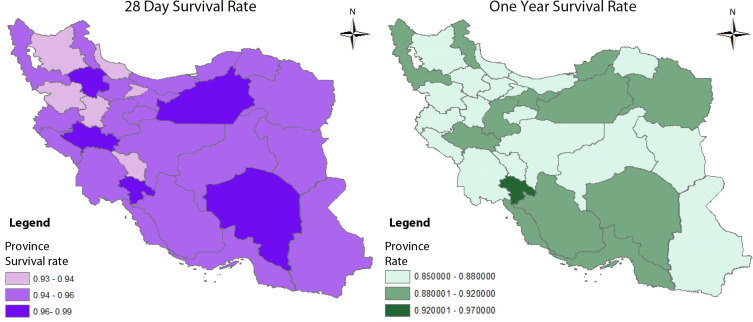
The lowest 28-day survival rates were observed in Hamadan, Chaharmahal-o-Bakhtiyari, Gilan, Alborz, East Azerbaijan, and Kurdistan provinces, whereas the highest 28-day survival rates were found in Kerman, Semnan, Kohgiloye-o-Boyer Ahmad, Zanjan, and Lorestan provinces.
The lowest 1-year survival rates were observed in Hamadan, Kurdistan, and South Khorasan provinces, while the highest 1-year survival rates were found in Kohgiloye-o-Boyer Ahmad, Semnan, and Kerman provinces.
Figure 2 illustrates the 28-day and 1-year survival rates in the provinces of Iran.
Figure 2.
The image depicts 28-day and 1-year survival rates in the provinces of Iran, 2013–2014.
Discussion
MI is one of the major causes of death in the world and Iran, hence the significance of the determination of its survival rate and associated factors in medical research. The present study has the largest population size of all similar studies and demonstrates post-MI short and long-term survival rates in Iran.
In this survey, the overall 28-day, 6-month, and 1-year survival rates after MI in 22 187 patients were 95%, 90%, and 88%, respectively.
Our results revealed a high incidence rate of MI in men. The high incidence of MI in men by comparison with women (72.4% vs 27.6%) and the high age of women at the time of MI compared with men (66.61±12.38 y vs 60.38±13.39 y) have also been shown in other studies.9, 12 These findings are consistent with those reported by previous studies in other countries.13-16 The 28-day, 6-month, and 1-year survival rates in women were lower than those in men (93%, 86%, and 83% vs 96%, 92, and 90%). These results are consistent with those found by Rosengren and other studies.6, 17 The higher age of women at the time of MI can be one of the reasons for this issue.
The most frequent age group was 55–60 years, and the 1-year fatality rate was the highest among the age group of 90 to 95 years old. According to the WHO, aging begins at 60. Our results showed high incidence and fatality rates for MI in the pre-elderly age group (55–60 y), which chimes in with the results of other studies.18, 20
Patients in the age group of 25–30 years had the highest short and long-term survival rates, and the results showed that the proportion of deaths from MI increased with age. This finding is consistent with that reported by Vaur.13
The mean age of patients with MI was 62.10±13.42 years, indicating that the mean age at the incidence of MI is higher in our study than in other studies done in Iran. The difference in the mean age across different studies could be attributed to different population age distributions, improved medical and health care, and improved treatment adherence by patients.11, 17
Hypertension, cigarette smoking, and diabetes were common among patients. In many other studies, diabetes and hypertension were the most common risk factors among patients.21, 22
A higher survival rate was observed in patients with a history of cigarette smoking than nonsmokers, and a low survival rate was seen in those with a past medical history of chronic heart disease by comparison with patients without such a history. The results found in the studies by Gerber, Barbash, and Gottlieb are consistent with our study.23-25 Some reasons have been propounded about the higher survival rate of smoking patients. In our study, the smoking status was determined at the hospitalization time; thus, we did not have any information about the smoking status of patients after discharge from the hospital. Usually patients with MI are strongly advised to quit smoking. Our finding may, therefore, point to the effect of smoking cessation among previous smokers in comparison with nonsmokers. Further, because of chronic hypoxia, which accompanies chronic smoking, the smoking population usually has more collateral vessels than the nonsmoking population. Additionally, because of the better effect of thrombolytic drugs on the collateral vessels of smokers, the survival rate of smoking patients can be higher than that of nonsmoking patients, although more complementary research should be done in this regard.23-25
Aging, diabetes, and hypertension are important risk factors for CVDs. In our study, past medical history of hypertension and diabetes, when adjusted for age, increased the risk of death following MI.
On the other hand, our results showed no difference apropos of short and long-term survival rates in patients with and without a past medical history of hyperlipidemia. Patients with a history of hyperlipidemia usually use drugs such as statins to control their hyperlipidemia, which might explain the similar survival rate of this group to normal patients. Tian et al26 showed that the use of statins reduced the risk of the incidence and recurrence of MI.
The most frequent MI location was acute transmural MI of the anterior wall. The location of MI is a predictive factor of death after MI, and acute MI of the anterior wall has a worse prognosis than infarction at other parts of the heart. This finding is in line with other studies.26, 27 One of the reasons is that in acute MI of the anterior wall, a large volume of myocardial tissue is damaged.
The 1-year survival rate in patients with anterior wall MI was lower than that in patients with inferior wall MI, which is congruent with the results reported by Haim et al.27 On the other hand, the survival rate in patients with acute transmural MI of the anterior wall, the inferior wall, and other sites simultaneously was lower than that of other locations of MI. Infarction in several areas of the heart indicates the spread of coronary artery disease, which reduces survival and decreases recovery after MI.
The present study did not include patients who died before hospital admission. Therefore, the 28-day survival rate is higher in our study than in other investigations that consider all cases, but it is the same as that reported by Tian et al.26
In this study, the lowest 28-day survival rates were observed in Hamadan, Chaharmahal-o-Bakhtiyari, Gilan, Alborz, East Azerbaijan, and Kurdistan provinces, whereas the highest 28-day survival rates were found in Kerman, Semnan, Kohkiloye-o-Boyer Ahmad, Zanjan, and Lorestan provinces. In provinces with the lowest 28-day survival rates, the prevalence of risk factors for CVDs was high compared with the country’s average and in provinces with the highest 28-day survival rates, the prevalence of risk factors for CVDs was low in comparison with the country’s average. Many studies have already reported the overall survival rates of 28-day and 1-year MI in some of the provinces of Iran. Overall, the survival rates at 28 days, 6 months, and 1 year were estimated to be 0.95, 0.90, and 0.88, respectively. Likewise, in a study by Arós et al,28 the 28-day survival rates were 87%, 88%, and 94% in 1995, 2000, and 2005, respectively, and 84%, 85%, and 91%, respectively, at 6 months. The survival rates at 28 days and 6 months in 2005 are similar to the findings of our study.
The current investigation has its strengths in that not only was it the first study on post-MI survival throughout Iran, but also it was hospital-based, encompassed all the provinces of Iran, and used definite diagnoses established by cardiologists and categorized by ICD-10, version 2016. We hope that our findings will pave the way for programs aimed at reducing disparities among the provinces and monitoring and managing MI at micro and macro levels in the Islamic Republic of Iran.
The quality of the hospital registry of MI data in the Islamic Republic of Iran has been reported to be acceptable; nonetheless, failure to register MI patients who die outside the hospital and/or at home was one of the limitations of the present study. Other notable limitations were the lack of access to the specific cause of the death of patients and any probable risk factors or prescribed drugs after discharge from the hospital.
Conclusion
Reports of the survival rates of MI in developing countries, particularly by province or state, are rare. We report for the first time the MI survival rates of hospitalized patients at the provincial level in the Islamic Republic of Iran.
MI is the principal cause of death in the community. The estimates of MI survival rates by province are valuable in health policy-making and resource allocation vis-à-vis CVDs and their prioritization, prevention, and control.
MI patients who died at home or outside the hospital were not included in our estimates of MI survival rates. We recommend that the Iranian Myocardial Infarction Registry officials devise a system for registering outside-hospital deaths and cause-specific mortality in order to derive the actual MI survival rate in our country.
We also suggest that more studies be undertaken on the cause of higher survival rates among smokers and also the reasons behind discrepancies in survival rates in different provinces of Iran.
Acknowledgments
Part of this manuscript was reported in the 19th International Congress on Cardiovascular Updates and Euro-Asian Pharmacoepidemiology Congress 2018 (EAPEC 2018).
We gratefully thank Dr Saeed Ranjbar, PhD, FESC, the Department of Cardiothoracic Surgery, Maastricht University Medical Center, Maastricht, the Netherlands, and the personnel of the Cardiology Office and Information technology (IT) of the Ministry of Health and Medical Education of the Islamic Republic of Iran. Many thanks are also due to Shahid Beheshti University of Medical Sciences for its support of this thesis.
Notes:
This paper should be cited as: Mozaffarian S, Etemad K, Aghaali M, Khodakarim S, Sotoodeh Ghorbani S, Hashemi Nazari SS. Short and Long-Term Survival Rates Following Myocardial Infarction and Its Predictive Factors: A Study Using National Registry Data. J Teh Univ Heart Ctr 2021;16(2):68-74.
References
- 1.Sarraf-Zadegan N, Boshtam M, Malekafzali H, Bashardoost N, Sayed-Tabatabaei FA, Rafiei M, Khalili A, Mostafavi S, Khami M, Hassanvand R. Secular trends in cardiovascular mortality in Iran, with special reference to Isfahan. Acta Cardiol. 1999 Dec;54(6):327–33. PMID: 10672288. [PubMed] [Google Scholar]
- 2.Kim AS, Johnston SC. Global variation in the relative burden of stroke and ischemic heart disease. Circulation. 2011;124:314–323. doi: 10.1161/CIRCULATIONAHA.111.018820. [DOI] [PubMed] [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abildstrom SZ, Rasmussen S, Rosén M, Madsen M. Trends in incidence and case fatality rates of acute myocardial infarction in Denmark and Sweden. Heart. 2003;89:507–511. doi: 10.1136/heart.89.5.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, Davis K, Killip T, Passamani E, Norris R, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994;344:563–570. doi: 10.1016/s0140-6736(94)91963-1. [DOI] [PubMed] [Google Scholar]
- 6.Maynard C, Every NR, Martin JS, Kudenchuk PJ, Weaver WD. Association of gender and survival in patients with acute myocardial infarction. Arch Intern Med. 1997;157:1379–1384. [PubMed] [Google Scholar]
- 7.Ahmadi A, Soori H, Mehrabi Y, Etemad K, Samavat T, Khaledifar A. Incidence of acute myocardial infarction in Islamic Republic of Iran: a study using national registry data in 2012. East Mediterr Health J. 2015;21:5–12. doi: 10.26719/2015.21.1.5. [DOI] [PubMed] [Google Scholar]
- 8.Gomez JF, Zareba W, Moss AJ, McNitt S, Hall WJ. Prognostic value of location and type of myocardial infarction in the setting of advanced left ventricular dysfunction. Am J Cardiol. 2007;99:642–646. doi: 10.1016/j.amjcard.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 9.Mohammadian M, Hosseini S, Salehiniya H, Sadeghi M, Sarrafzadegan N, Roohafza HR, Khazaei S, Soltani S, Sarrafkia A, Golshahi J, Mohammadian-Hafshejani A. Prognostic factors of 28 days survival rate in patients with a first acute myocardial infarction based on gender in Isfahan, Iran (2000-2009) ARYA Atheroscler. 2015;11:332–3340. [PMC free article] [PubMed] [Google Scholar]
- 10.Toluey M, Ghaffari S, Tajlil A, Nasiri B, Rostami A. The impact of cigarette smoking on infarct location and in-hospital outcome following acute ST-elevation myocardial infarction. J Cardiovasc Thorac Res. 2019;11:209–215. doi: 10.15171/jcvtr.2019.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abdolazimi M, Khosravi A, Sadeghi M, Mohammadian-Hafshejani A, Sarrafzadegan N, Salehiniya H, Golshahi J. Predictive factors of short-term survival from acute myocardial infarction in early and late patients in Isfahan and Najafabad, Iran. ARYA Atheroscler. 2016;12:59–67. [PMC free article] [PubMed] [Google Scholar]
- 12.Abduelkarem AR, El-Shareif HJ, Sharif SI. Evaluation of risk factors in acute myocardial infarction patients admitted to the coronary care unit, Tripoli Medical Centre, Libya. East Mediterr Health J. 2012;18:332–336. doi: 10.26719/2012.18.4.332. [DOI] [PubMed] [Google Scholar]
- 13.Vaur L, Danchin N, Genès N, Dubroca I, Etienne S, Ferrières J, Cambou JP. Epidemiology of myocardial infarction in France: therapeutic and prognostic implications of heart failure during the acute phase. Am Heart J. 1999;137:49–58. doi: 10.1016/s0002-8703(99)70459-x. [DOI] [PubMed] [Google Scholar]
- 14.Kubota I, Ito H, Yokoyama K, Yasumura S, Tomoike H. Early mortality after acute myocardial infarction: observational study in Yamagata, 1993-1995. Jpn Circ J. 1998;62:414–418. doi: 10.1253/jcj.62.414. [DOI] [PubMed] [Google Scholar]
- 15.You J, Condon JR, Zhao Y, Guthridge S. Incidence and survival after acute myocardial infarction in Indigenous and non-Indigenous people in the Northern Territory, 1992-2004. Med J Aust. 2009;190:298–302. doi: 10.5694/j.1326-5377.2009.tb02416.x. [DOI] [PubMed] [Google Scholar]
- 16.Martin CA, Thompson PL, Armstrong BK, Hobbs MS, de Klerk N. Long-term prognosis after recovery from myocardial infarction: a nine year follow-up of the Perth Coronary Register. Circulation. 1983;68:961–969. doi: 10.1161/01.cir.68.5.961. [DOI] [PubMed] [Google Scholar]
- 17.Rosengren A, Spetz CL, Köster M, Hammar N, Alfredsson L, Rosén M. Sex differences in survival after myocardial infarction in Sweden; data from the Swedish National Acute Myocardial Infarction Register. Eur Heart J. 2001;22:314–322. doi: 10.1053/euhj.2000.2368. [DOI] [PubMed] [Google Scholar]
- 18.Gottlieb S, Moss AJ, McDermott M, Eberly S. Comparison of posthospital survival after acute myocardial infarction in women and men. Am J Cardiol. 1994;74:727–730. doi: 10.1016/0002-9149(94)90319-0. [DOI] [PubMed] [Google Scholar]
- 19.van Oeffelen AA, Agyemang C, Bots ML, Stronks K, Koopman C, van Rossem L, Vaartjes I. The relation between socioeconomic status and short-term mortality after acute myocardial infarction persists in the elderly: results from a nationwide study. Eur J Epidemiol. 2012;27:605–613. doi: 10.1007/s10654-012-9700-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stevenson R, Ranjadayalan K, Wilkinson P, Roberts R, Timmis AD. Short and long term prognosis of acute myocardial infarction since introduction of thrombolysis. BMJ. 1993;307:349–353. doi: 10.1136/bmj.307.6900.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord. 2017;17:53. doi: 10.1186/s12872-017-0482-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lisowska A, Makarewicz-Wujec M, Filipiak KJ. Risk factors, prognosis, and secondary prevention of myocardial infarction in young adults in Poland. Kardiol Pol. 2016;74:1148–1153. doi: 10.5603/KP.a2016.0098. [DOI] [PubMed] [Google Scholar]
- 23.Gerber Y, Rosen LJ, Goldbourt U, Benyamini Y, Drory Y Israel Study Group on First Acute Myocardial Infarction. Smoking status and long-term survival after first acute myocardial infarction a population-based cohort study. J Am Coll Cardiol. 2009;54:2382–7238. doi: 10.1016/j.jacc.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 24.Barbash GI, Reiner J, White HD, Wilcox RG, Armstrong PW, Sadowski Z, Morris D, Aylward P, Woodlief LH, Topol EJ. Evaluation of paradoxic beneficial effects of smoking in patients receiving thrombolytic therapy for acute myocardial infarction: mechanism of the "smoker's paradox" from the GUSTO-I trial, with angiographic insights. Global Utilization of Streptokinase and Tissue-Plasminogen Activator for Occluded Coronary Arteries. J Am Coll Cardiol. 1995;26:1222–1229. doi: 10.1016/0735-1097(95)00299-5. [DOI] [PubMed] [Google Scholar]
- 25.Gottlieb S, Boyko V, Zahger D, Balkin J, Hod H, Pelled B, Stern S, Behar S. Smoking and prognosis after acute myocardial infarction in the thrombolytic era (Israeli Thrombolytic National Survey) J Am Coll Cardiol. 1996;28:1506–1513. doi: 10.1016/s0735-1097(96)00334-8. [DOI] [PubMed] [Google Scholar]
- 26.Tian L, Yang Y, Zhu J, Liu L, Liang Y, Li J, Yu B. Impact of Previous Stroke on Short-Term Myocardial Reinfarction in Patients With Acute ST Segment Elevation Myocardial Infarction: An Observational Multicenter Study. Medicine (Baltimore) 2016;95:e2742. doi: 10.1097/MD.0000000000002742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haim M, Hod H, Reisin L, Kornowski R, Reicher-Reiss H, Goldbourt U, Boyko V, Behar S. Comparison of short- and long-term prognosis in patients with anterior wall versus inferior or lateral wall non-Q-wave acute myocardial infarction. Secondary Prevention Reinfarction Israeli Nifedipine Trial (SPRINT) Study Group. Am J Cardiol. 1997;79:717–721. doi: 10.1016/s0002-9149(96)00856-9. [DOI] [PubMed] [Google Scholar]
- 28.Arós F, Heras M, Vila J, Sanz H, Ferreira-González I, Permanyer-Miralda G, Cuñat J, López-Bescós L, Cabadés A, Loma-Osorio A, Marrugat J en representación de los investigadores de los registros PRIAMHO I, II y MASCARA. Reducción de la mortalidad precoz y a 6 meses en pacientes con IAM en el periodo 1995-2005. Datos de los registros PRIAMHO I, II y MASCARA [Reduction in 28 days and 6 months of acute myocardial infarction mortality from 1995 to 2005. Data from PRIAMHO I, II and MASCARA registries] Rev Esp Cardiol. 2011;64:972–980. doi: 10.1016/j.recesp.2011.05.011. [DOI] [PubMed] [Google Scholar]