Abstract
Background
The US rural disadvantage in life expectancy (LE) relative to urban areas has grown over time. We measured the contribution of cardiovascular disease (CVD), drug-overdose deaths (DODs) and other major causes of death to LE trends in rural and urban counties and the rural–urban LE gap.
Methods
Counterfactual life tables and cause-of-death decompositions were constructed using data on all US deaths in 1999–2019 (N = 51 998 560) from the Centers for Disease Control and Prevention.
Results
During 1999–2009, rural and urban counties experienced robust LE gains, but urban LE increased by 1.19 years more in women and 0.86 years more in men compared with rural LE. During 2010–2019, rural counties experienced absolute declines in LE (women −0.20, men −0.30 years), whereas urban counties experienced modest increases (women 0.55, men 0.29 years). Counterfactual analysis showed that slowed CVD-mortality declines, particularly in ages 65+ years, were the main reason why rural LE stopped increasing after 2010. However, slow progress in CVD-mortality influenced LE trends more in urban areas. If CVD-mortality had continued to decline at its pre-2010 pace, the rural–urban LE gap would have grown even more post 2010. DODs and other causes of death also contributed to the LE trends and differences in each period, but their impact in comparison to that of CVD was relatively small.
Conclusions
Rural disadvantage in LE continues to grow, but at a slower pace than pre 2010. This slowdown is more attributable to adverse trends in CVD and DOD mortality in urban areas than improvements in rural areas.
Keywords: Life expectancy, urbanicity, rural health, cardiovascular disease, demography
Key Messages.
The rural–urban life expectancy (LE) gap in the USA has grown over time, more so in the 1999–2009 period than in 2010–2019.
Stagnation in cardiovascular disease (CVD) mortality declines since 2010 contributed to a reversal in LE gains in rural areas, but stagnation was more dramatic in urban areas, slowing down the growth in the rural–urban LE gap.
Much of the effect of CVD-mortality stagnation on LE trends in both urban and rural areas is attributable to slowing mortality improvements among adults above the age of 65 years.
Multiple broad causes of death explain the growing rural–urban divide in LE, pointing to the need for wholistic health-promotion approaches.
Introduction
Geographic disparities in mortality and life expectancy (LE) in the USA have been widening since the at least the 1980s.1–5 The difference between rural and urban health is especially concerning, with 135 annual excess deaths per 100 000 persons in rural compared with urban areas in 2016.3 Since around 2010, LE in rural areas has declined, whereas it has remained relatively stagnant in non-rural areas.2,6 Understanding the forces behind recent trends in rural LE and the rural penalty in LE relative to urban areas is critical for reducing place-based health disparities .
Several conditions contribute to geographic mortality variation, including cardiovascular disease (CVD), the leading cause of death in the USA.7,8 The USA experienced decades of robust CVD-mortality declines thanks to the ‘CVD revolution’, which featured declines in cigarette smoking, improvements in hypertension control, increased use of statins and the advent of thrombolysis and stents.9,10 However, declines in CVD-mortality rates have stagnated since 2010, as have improvements in national LE.11 Rural areas have exhibited higher age-adjusted CVD-mortality rates than non-rural areas over the past two decades and across age, sex and race/ethnicity.12 Large, medium-sized and small metropolitan areas and rural areas have all experienced dramatic slows in the annual decline in CVD deaths since 2010.12
A recent study demonstrated that US LE at age 25 years would have been 1.14 years higher in 2017 if CVD-mortality had continued its pre-2010 rate of decline, representing a larger effect on LE trends than that of rising drug-overdose deaths (DODs).11 However, the effect of CVD stagnation on rural and urban LE trends and the rural–urban gap in LE have not been analysed. Given the dramatic increase in deaths from substance use and suicide in midlife,13,14 research on rural and urban disparities and on US LE trends have often focused on midlife mortality and non-CVD causes.8,15,16
Other causes of death beyond CVD-mortality also play important roles in explaining geographic variation in LE. Drug-related mortality, with its differential trends across regions,17 is a prime candidate. Among non-Hispanic White Americans, DODs reduced LE most in large metropolitan suburbs, followed by small/medium-sized metropolitan areas and then non-metropolitan areas.2 Other conditions relevant to rural–urban disparities include cancer and respiratory diseases related to smoking, as well as diabetes and liver disease related to diet and alcohol consumption, given that rural populations face barriers in adopting health behaviours for chronic disease prevention.18,19 Additionally, external causes of death such as unintended injuries may be important to the rural–urban LE gap, considering the increased burden of motor-vehicle crashes, increased alcohol consumption and lower access to rapid emergency treatment for trauma for rural populations.18
Whereas numerous studies have identified the causes of death contributing to the rural–urban LE gap at various periods, there has been less focus on identifying the causes responsible for the growing gap, particularly in the post-2010 period when CVD-mortality changes have been flat. Recent exceptions include the studies by Monnat (2020) and Elo et al. (2019), both of which examined trends by causes. Both studies included only non-Hispanic Whites and the former was restricted to ages 25–64 years. This paper investigates the contribution of CVD and other major causes of death to trends in rural and urban LE and the rural–urban LE gap. In particular, this study aims to: (i) measure annual changes in rural and urban LE and the rural–urban LE gap before (1999–2009) and after (2010–2019) CVD-mortality stopped declining, which we refer to as the CVD-mortality stagnation; (ii) use counterfactual scenarios of continued CVD-mortality decline to quantify the role of CVD-mortality stagnation to post-2010 trends in rural and urban LE; and (iii) measure the relative contributions of CVD and 12 other major causes of death to the changing rural–urban LE gap in 1999–2009 and 2010–2019.
Methods
Data
Data on all US deaths from 1999–2019 (N = 51 998 560) came from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) detailed mortality files, which are publicly available at https://wonder.cdc.gov/.20 This period uses all years available in CDC WONDER. Rural–urban designations were based on the 2013 National Center for Health Statistics (NCHS) Urban-Rural Scheme, with large centre metro, large fringe metro, medium metro and small metro counties considered urban and micropolitan or noncore counties considered rural.21 Each death was categorized based on the county of the person’s legal residence. Where CDC WONDER populations were unavailable, population-count data came from Bridged-Race Population Estimates produced by the US Census Bureau and NCHS.22
CVD deaths were defined according to the International Classifications of Disease, 10th revision (ICD-10) 113 Cause List. This classification groups together ICD-10 codes I00–I78: diseases of heart (e.g. hypertensive heart disease, ischaemic heart diseases, heart failure), essential hypertension and hypertensive renal disease, cerebrovascular diseases, atherosclerosis and other diseases of the circulatory system. DODs included deaths from legal and illegal substances and intentional (e.g. suicides) and unintentional (e.g. accidents) drug-related causes (ICD-10: X40 to X44, X60 to X64, X85 and Y10 to Y14). We used conventional ICD-10 codes to classify other major death causes (Supplementary Table S1, available as Supplementary data at IJE online).
Statistical analysis
We used life tables to calculate LE at age 25 years (e25) by sex in rural and urban populations. We charted changes in e25 from 1999–2009 (pre-2010 period) and from 2010–2019 (post-2010 period), as well as changes in the rural–urban gap in e25. Then, we examined age-standardized trends in CVD-mortality (deaths per 100 000) from 1999 to 2019 by sex in rural and urban populations in 5-year age groups ranging from 25 to 85+ years old. Age-standardized results were based on standardizing to the US age distribution in 2009, the median year in this period.
Our main analysis comprised two components. First, we used counterfactual life tables under different mortality conditions to identify the role of post-2010 CVD-mortality stagnation in trends in rural and urban LE after 2010. We calculated hypothetical e25 in rural and urban populations under the counterfactual scenario that CVD-mortality rates in each sex and urbanicity group had continued to decline at their age-specific pre-2010 levels in 2010–2019. This counterfactual scenario is reasonable in an international context, as many high LE nations have experienced such continued declines in CVD in recent years.11 To explore the role of stagnation specifically at older ages, we calculated e25 under the counterfactual scenario that those aged ≥65 years continued CVD-mortality declines after 2010 whereas only those aged 25–64 years experienced CVD stagnation. To understand the contribution of CVD to the changing rural–urban LE gap relative to DODs, we calculated e25 in rural and urban populations under the counterfactual that DODs had remained at their 2010 level rather than quickly increasing.
These counterfactuals reveal the role of CVD-mortality stagnation and increases in DODs to LE trends in rural and urban areas but do not enumerate the causes of death contributing to the growing rural–urban LE gap. Therefore, we conducted a formal cause-specific decomposition of the change in the rural–urban LE gap in 1999–2009 and 2010–2019 using data from these tail years separately by sex. The decomposition included CVD, DOD, lung cancer, other cancers, respiratory diseases, diabetes, liver disease, kidney disease, infectious diseases, Alzheimer’s and dementias, suicide and other external causes (see Supplementary Table S1, available as Supplementary data at IJE online). Together, these causes account for nearly 90% of all US deaths, with a residual ‘other’ category for those remaining. We conducted the decomposition using an additive approach.23 As a sensitivity analysis, we re-estimated the decomposition using the contour method.24
Results
Trends in rural and urban LE
Table 1 shows rural and urban e25 and the rural–urban LE gap in 1999–2009 and 2010–2019. In the 1999–2009 period, LE increased in both urban counties (1.85 years for women and 2.20 years for men) and rural counties (0.66 years in women and 1.34 years in men). The increase in urban counties outpaced that of rural counties resulting in a growing rural–urban LE gap of 1.19 years in women (0.12 years per annum) and 0.86 years in men (0.09 years per annum). In 2010–2019, LE increases stalled in both rural and urban counties, but only in rural counties did LE decline (by −0.20 years in women and −0.30 years in men). After 2010, the rural–urban LE gap continued to grow, but at a more modest pace compared with the prior period, by 0.08 and 0.07 years per annum in women and men, respectively.
Table 1.
Rural and urban life expectancies (LEs) at age 25 years in years over time, by sex
| LE in 1999 | LE in 2009 | Change 1999–2009 | LE in 2010 | LE in 2019 | Change 2010–2019 | ||
|---|---|---|---|---|---|---|---|
| Women | Rural | 55.11 | 55.77 | 0.66 | 55.78 | 55.58 | −0.20 |
| Urban | 55.64 | 57.48 | 1.85 | 57.52 | 58.07 | 0.55 | |
| Rural–urban gap | 0.52 | 1.71 | 1.19 | 1.74 | 2.48 | 0.74 | |
| Men | Rural | 49.76 | 51.10 | 1.34 | 51.13 | 50.83 | −0.30 |
| Urban | 50.76 | 52.96 | 2.20 | 53.07 | 53.36 | 0.29 | |
| Rural–urban gap | 1.00 | 1.86 | 0.86 | 1.94 | 2.53 | 0.59 |
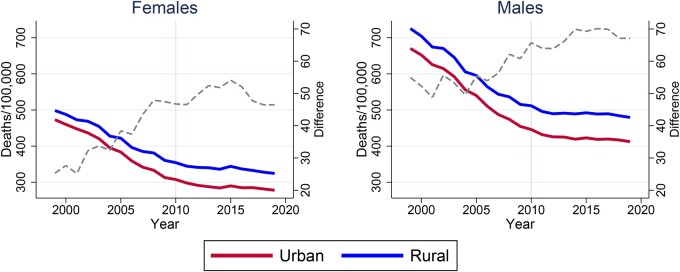
Trends in CVD-mortality
Rural counties exhibited higher age-standardized CVD-mortality from 1999 to 2019 and the rural disadvantage grew substantially over this 20-year period (Figure 1). In 1999, rural women experienced an age-standardized CVD death rate of 499 per 100 000 compared with 473 among urban females. By 2019, that absolute difference of 26 additional deaths per 100 000 had nearly doubled. The dashed line shows that most of the increase in the rural–urban absolute difference occurred before CVD-mortality declines stagnated in 2010. Pre 2010, the average annual change in age-standardized CVD deaths per 100 000 was −13.9 in rural women compared with −16.0 in urban women. Urban trends in CVD-mortality slowed more dramatically than rural trends after 2010, as both urban and rural women had an average annual change of −3.3 deaths per 100 000 during 2010–2019. Among men, average annual declines were −21.0 in rural men and −21.5 in urban men prior to 2010 and slowed to −3.7 and −3.8 in rural and urban men, respectively, after 2010.
Figure 1.
Age-standardized US cardiovascular disease (CVD) mortality by sex and rural–urban distinction, showing rural–urban absolute difference in deaths per 100 000. Based on 5-year age groups, aged 25–85+ years. Standard population is the age distribution of the US population in 2009. Data (1999-2019) from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research. Rural–urban designation based on the 2013 National Center for Health Statistics’ Urban-Rural Scheme, with urban areas encompassing large centre metro, large fringe metro, medium metro and small metro, whereas rural areas were micropolitan or noncore.
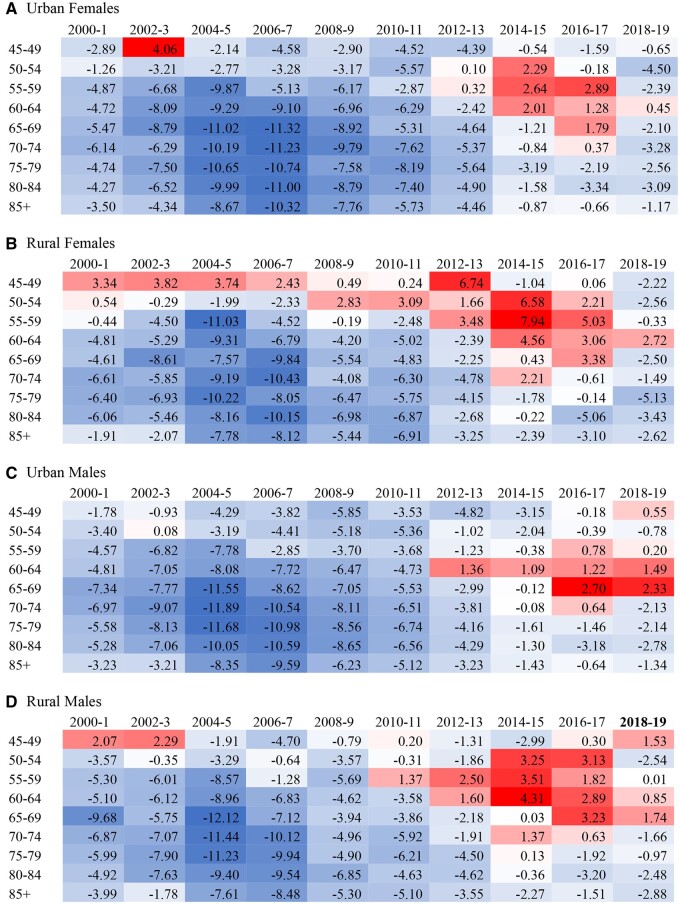
Figure 2 depicts the percentage change over 2-year periods in CVD-mortality by 5-year age groups in rural and urban men and women. Moving across time in each row shows CVD stagnation, as declines slowed and sometimes reversed. In urban men and women, dark blue cells show strong declines in CVD pre 2010, especially in those aged 65+ years. These age groups fade to a neutral white as declines slow in more recent years. Red cells show small increases in CVD-mortality after 2014 in midlife (ages 50–69 years). In rural areas, the pattern is similar, but recent increases in midlife CVD-mortality are larger and appear to begin earlier.
Figure 2.
Percent change in cardiovascular disease (CVD) mortality over time by 5-year age groups, stratified by sex and rural–urban distinction. (A) Urban females; (B) rural females; (C) urban males; (D) rural males. Years 2000–2001 compared with 1999 death rates. Data from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research. Rural–urban designation based on the 2013 National Center for Health Statistics’ Urban-Rural Scheme, with urban areas encompassing large centre metro, large fringe metro, medium metro and small metro, whereas rural areas were micropolitan or noncore .
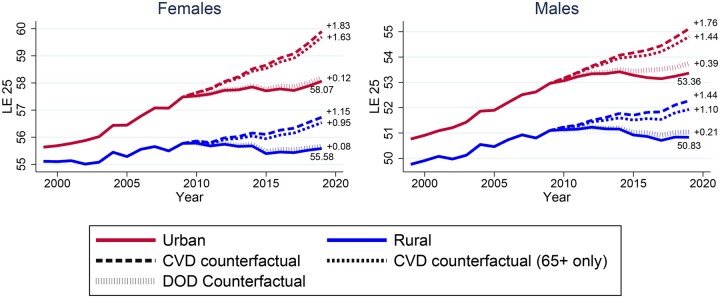
Effect of CVD stagnation on rural and urban LE
Figure 3 shows actual (solid lines) and counterfactual (dashed lines) rural and urban e25 from 1999 to 2019 by sex. Rural and urban LEs diverged as early as 2000, when CVD-mortality rates were still declining quickly. The CVD counterfactual line shows that, if rural and urban men and women had experienced CVD-mortality declines at their age-specific 1999–2009 pace in 2010 and afterwards, they would have all experienced large improvements in LE (up to 1.83 additional years). However, this CVD counterfactual results in larger rural–urban LE differences in 2019 than actual disparities (3.2 vs 2.5 years in women and 2.9 vs 2.5 years in men). In other words, allowing CVD-mortality to continue its pre-2010 declines would have improved LE more in urban areas (1.83 years gained for women and 1.76 years for men) than in rural areas (1.15 years gained for women and 1.44 years for men). Supplementary Figure S1 (available as Supplementary data at IJE online) shows that applying a shared rural–urban rate of decline post 2010 still results in a larger rural–urban LE gap than the actual gap.
Figure 3.
Rural and urban life expectancies (LE) at age 25 years by sex under observed and counterfactual conditions. CVD, cardiovascular disease; DOD, drug-overdose death. Annotations show actual LE age 25 years and differences between actual and counterfactual values. CVD counterfactual estimates of LE if the 1999–2009 CVD-mortality rates in rural and urban areas had continued through 2010–2019. The CVD counterfactual (65+ years only) applies 1999–2009 rates of decline only to the age groups of ≥65 years, whereas ages 25–64 years have actual mortality rates. The DOD counterfactual estimates LE if drug-overdose deaths remained at their 2010 level through 2019. Data from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research. Rural–urban designation based on the 2013 National Center for Health Statistics’ Urban-Rural Scheme, with urban areas encompassing large centre metro, large fringe metro, medium metro and small metro, whereas rural areas were micropolitan or noncore.
Much of the effect of CVD-mortality stagnation on LE is attributable to adults above the age of 65 years. If the 1999–2009 rates of CVD decline had continued for older adults only, rural and urban counties could have achieved almost the same LE as when halting CVD stagnation at all ages (0.95 and 1.63 additional years in rural and urban women, and 1.10 and 1.44 additional years in rural and urban men, respectively). The largest difference between the two counterfactuals in 2019 e25 was 0.34 years in rural men. This counterfactual shows the outsized impact of CVD-mortality in old age, especially among women. Examining the counterfactual of no rise in DOD deaths after 2010 revealed much smaller increases in LE compared with the CVD counterfactuals, with the largest improvement being 0.39 years among urban men. Like the CVD counterfactual, eliminating DOD increases the LE gap by improving LE more in urban compared with rural areas.
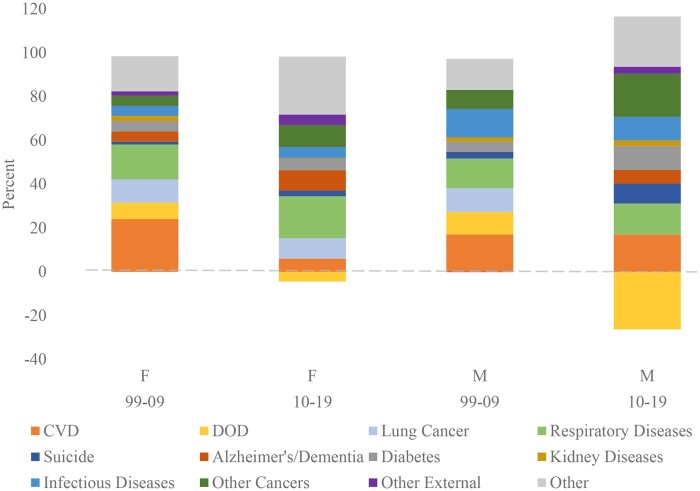
Cause-of-death decomposition
In 1999–2009, when the gap between rural and urban LE grew by 1.19 years among women and 0.86 years among men, CVD accounted for 24% and 17% of that change for women and men, respectively (Figure 4). In the 2010–2019 period, the LE gap grew by 0.74 years in women and 0.59 years in men, with CVD accounting for 6% and 17%, respectively. Therefore, for women, CVD was a larger contributor to lagging rural LE pre 2010, when CVD-mortality was robustly declining. For men, CVD contributed more in years to the changing gap pre 2010, but the growth in the gap was much smaller in the post-2010 period, resulting in the same percentage explained by CVD.
Figure 4.
Decomposition of change in rural–urban life-expectancy gap over 1999–2009 and 2010–2019 by sex. CVD, cardiovascular disease; DOD, drug-overdose death. Showing the percentage of the change in the rural–urban life-expectancy gap in the pre- and post-2010 periods that can be attributed to each cause of death based on an additive decomposition. ICD-10 codes used for cause-of-death classifications can be found in Supplementary Table S1, available as Supplementary data at IJE online. Data from each tail year (1999, 2009, 2010 and 2019 ) separately by sex came from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research. Rural–urban designation based on the 2013 National Center for Health Statistics’ Urban-Rural Scheme, with urban areas encompassing large centre metro, large fringe metro, medium metro and small metro, whereas rural areas were micropolitan or noncore .
DODs were a small contribution to the rural–urban LE gap in the pre-2010 period and had negative contributions in the post-2010 period (−4% for women and −26% for men). Therefore, increases in DODs after 2010 reduced LE more in urban areas than in rural areas. Among other causes of death, there was no one factor that dominantly explained change in the rural–urban LE gap. Large contributors pre 2010 included respiratory diseases, lung cancer, infectious diseases and other causes. Post 2010, cancers besides lung cancer, respiratory diseases, diabetes and infectious disease were large contributors among men, with respiratory disease and other causes largest among women.
Our sensitivity analysis using the contour-decomposition method resulted in similar conclusions to the additive decomposition in our main analysis (see Supplementary Figure S2, available as Supplementary data at IJE online). Trends in the rural-minus-urban difference in mortality are plotted in Supplementary Figure S3 (available as Supplementary data at IJE online). The rural–urban gap increased over time for most causes, with the notable exceptions of a plateauing gap for CVD in the most recent years (with declines after 2015) and a recent declining gap for DODs.
Discussion
Without stagnation in CVD-mortality declines, LE in rural counties would have increased rather than decreased post 2010. Even so, the rural–urban LE gap would have been even larger in 2019 without stagnation than with actual trends. The contribution of CVD to preventing LE improvements occurred mostly at older ages, despite recent attention on mortality in midlife. Therefore, promoting the continued decline of CVD-mortality across the USA and especially in older adults and in urban areas will be essential to improving US LE, even though it may not narrow rural–urban LE differences. DODs were more detrimental to urban than rural LE trends in males in recent years. Overall, there is not one clear cause of death to target to help rural LE reach urban levels, and wholistic approaches that reduce deaths from CVD, cancer, respiratory diseases and diabetes are warranted.
Examining CVD-mortality trends by urbanicity can provide insights into the mechanisms behind stalls in CVD declines and LE improvements, given the geographic variation in socio-economic status, racial/ethnic diversity, behavioural risk factors and healthcare factors.2,25,26 Our analysis revealed a widening rural–urban disparity in CVD-mortality over time, especially pre 2010 when CVD was quickly declining. These findings are consistent with recent work highlighting higher CVD-mortality rates in rural compared with more urban areas and showing slowing declines (and some subgroup increases) in age-adjusted mortality rates after 2010.12 Our findings reveal the overall LE implications of these trends, placing them in the context of other major causes of death. Given the large contribution of CVD to trends in rural and urban LE, our analysis indicates that reducing CVD-mortality would have a larger impact on LE than reducing death rates from other causes including DODs.
Our counterfactuals suggest that, in addition to continued attention on promoting rural health, efforts should be directed towards improving cardiovascular health in urban areas. According to an analysis of data from the Behavioral Risk Factor Surveillance System, adults in rural areas are more likely to be smokers, less likely to maintain normal body weight and less likely to meet physical-activity recommendations compared with adults in urban areas.19 Future research is needed to investigate factors that contribute to the disproportionate slowing of CVD-mortality in urban compared with rural areas. One potential explanation is the role of airborne particulate matter, which is associated with myocardial infarction, stroke, heart failure, arrhythmias and venous thromboembolism.27
When looking at trends over time in 5-year age groups, our study showed that much of the CVD-mortality stagnation is occurring in those over the age of 65 years and that reversing stagnation in this age group alone would have almost as large an impact on LE as reversing the trend at all ages. Therefore, concerns about increased mortality in midlife should not overshadow the effect of reduced progress in late-life mortality.
Our decomposition analysis pointed to causes besides CVD that had contributed to the rural–urban LE gap. Consistent with findings from Elo et al. (2019), causes of death linked to smoking (namely lung cancer and respiratory diseases) were substantial contributors, especially among women.2 Whereas Elo and colleagues focused only on non-Hispanic White Americans, our results reveal that this finding holds when including other racial and ethnic groups. Our findings also indicate that cancers besides lung cancer are important to the rural–urban LE gap among men post 2010. DODs served as a countervailing force to the growing rural–urban gap, reducing urban LE more than rural LE among men in recent years, likely due to the influx of fentanyl in urban areas.8 Once again, this finding highlights the need for research and interventions in urban areas. Finding that nearly all causes of death contribute to the growing rural–urban LE gap points to the importance of examining upstream factors, such as educational attainment, poverty and work, that may be afflicting rural areas.8
In conclusion, CVD stagnation has occurred ubiquitously across rural and urban counties in the USA, preventing LE improvements in both groups, but especially in urban men and women. Future research should investigate the contributions of metabolic disorders, smoking and access to healthcare to stagnation in CVD-mortality declines to return robust CVD declines to rural and urban populations. These efforts will be essential to improving long-run LE trends in the USA.
Supplementary data
Supplementary data are available at IJE online.
Ethics approval
This research uses de-identified publicly available data and, as such, is considered not regulated by the Institutional Review Board.
Funding
This research is funded by grants from the US National Institute on Aging [R03AG060404, P30 AG059301] and from the Alfred P. Sloan Foundation .
Data availability
The data used in this analysis, detailed mortality files and bridged-race populations are publicly available through the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) at https://wonder.cdc.gov/.
Supplementary Material
Acknowledgements
We thank Peng Li for technical assistance.
Conflict of interest
None declared.
References
- 1. Fenelon A. Geographic divergence in mortality in the United States. Popul Dev Rev 2013;39:611–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Elo IT, Hendi AS, Ho JY, Vierboom YC, Preston SH.. Trends in non-Hispanic White mortality in the United States by metropolitan-nonmetropolitan status and region, 1990–2016. Popul Dev Rev 2019;45:549–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cosby AG, Maya McDoom-Echebiri M, James W, Khandekar H, Brown W, Hanna HL.. Growth and persistence of place-based mortality in the United States: the rural mortality penalty. Am J Public Health 2019;109:155–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. James W, Cossman J, Wolf JK.. Persistence of death in the United States: the remarkably different mortality patterns between America’s Heartland and Dixieland. Demogr Res 2018;39:897–910. [Google Scholar]
- 5. Singh GK, Siahpush M.. Widening rural-urban disparities in life expectancy, U.S., 1969-2009. Am J Prev Med 2014;46:e19–29. [DOI] [PubMed] [Google Scholar]
- 6.National Advisory Committee on Rural Health and Human Services. Mortality and Life Expectancy in Rural America: Connecting the Health and Human Service Safety Nets to Improve Health Outcomes over the Life Course. 2015.
- 7. Heron M. National Vital Statistics Reports Volume 68, Number 6, June 24, 2019, Deaths: Leading Causes for 2017. 2019. https://www.cdc.gov/nchs/products/index.htm (29 July 2020, date last accessed). [PubMed]
- 8. Monnat SM. Trends in U.S. Working-age non-Hispanic White mortality: rural–urban and within-rural differences. Popul Res Policy Rev 2020;39:805–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mensah GA, Wei GS, Sorlie PD. et al. Decline in cardiovascular mortality: possible causes and implications. Circ Res 2017;120:366–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vallin J, Meslé F.. Convergences and divergences in mortality: a new approach of health transition. Demogr Res 2004;S2:11–44. [Google Scholar]
- 11. Mehta NK, Abrams LR, Myrskylä M.. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proc Natl Acad Sci U S A 2020;117:6998–7000. 10.1073/pnas.1920391117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cross SH, Mehra MR, Bhatt DL. et al. Rural-urban differences in cardiovascular mortality in the US, 1999-2017. JAMA 2020;323:1852–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Case A, Deaton A.. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci USA 2015;112:15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Case A, Deaton A.. Mortality and morbidity in the 21st century. Brookings Pap Econ Act 2017;2017:397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Woolf SH, Schoomaker H.. Life expectancy and mortality rates in the United States, 1959-2017. JAMA 2019;322:1996–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Woolf SH, Chapman DA, Buchanich JM, Bobby KJ, Zimmerman EB, Blackburn SM.. Changes in midlife death rates across racial and ethnic groups in the United States: systematic analysis of vital statistics. BMJ 2018;362: 1–16. 10.1136/bmj.k3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hedegaard H, Spencer MR.. Urban–Rural Differences in Drug Overdose Death Rates, 1999–2019. 2021. https://www.cdc.gov/nchs/products/index.htm (3 May 2021, date last accessed). [PubMed]
- 18. Garcia MC, Faul M, Massetti G. et al. Reducing potentially excess deaths from the five leading causes of death in the rural United States. MMWR Surveill Summ 2017;66:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Matthews KA, Croft JB, Liu Y. et al. Health-related behaviors by urban-rural county classification-United States, 2013. MMWR Surveill Summ 2017;66:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United States Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999-2018 on CDC WONDER Online Database, released in 2020. Data are from the Multiple Cause of Death Files, 1999-2018. 2020. http://wonder.cdc.gov/ucd-icd10.html (28 April 2021, date last accessed).
- 21. Ingram DD, Franco SJ.. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2 2014;166:1–73. [PubMed] [Google Scholar]
- 22.United States Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Bridged-Race Population Estimates, United States July 1st resident population by state, county, age, sex, bridged-race, and Hispanic origin. Compiled from 1990-1999 Bridged-Race Intercensal Population Estimates. 2020. http://wonder.cdc.gov/bridged-race-v2019.html (28 April 2021, date last accessed).
- 23. Andreev EM, Shkolnikov VM.. An Excel spreadsheet for the decomposition of a difference between two values of an aggregate demographic measure by stepwise replacement running from young to old ages. MPIDR Tech Rep 2012;49:6. [Google Scholar]
- 24. Jdanov DA, Shkolnikov VM, Raalte AA, van Andreev EM.. Decomposing current mortality differences into initial differences and differences in trends: the Contour Decomposition Method. Demography 2017;54:1579–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW. et al. Inequalities in life expectancy among US Counties, 1980 to 2014. JAMA Intern Med 2017;177:1003–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gurka MJ, Filipp SL, DeBoer MD.. Geographical variation in the prevalence of obesity, metabolic syndrome, and diabetes among US adults. Nutr Diabetes 2018;8:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Martinelli N, Olivieri O, Girelli D.. Air particulate matter and cardiovascular disease: a narrative review. Eur J Intern Med 2013;24:295–302. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this analysis, detailed mortality files and bridged-race populations are publicly available through the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) at https://wonder.cdc.gov/.