Abstract
Technological interventions in the healthcare sector, namely, telemedicine services, have helped the government and people in these extraordinarily challenging times of ongoing COVID-19 pandemic. We identify and group key success factors relevant to telemedicine services under 7 contextual criteria. Furthermore, we explore the causal relations among them using the decision-making trial and evaluation laboratory (DEMATEL) method. Then, by applying the Bayesian best-worst method (BWM), we compute the relative importance of these criteria. Thereafter, we rank six hospitals that have provided telemedicine services through a comparative evaluation using the VIsekriterijumsko KOmpromisno Rangiranjie (VIKOR) method. The threefold findings of our study reveal that (i) the technological criteria provide the highest causal impact, while the environmental criteria provide the least causal impact. (ii) The hierarchical model of criteria, achieved through the Bayesian BWM score, shows that the criteria weights for both technological and organizational criteria are maximum (0.205) and minimum (0.087), respectively. (iii) The evaluation of six hospitals with VIKOR based on seven criteria ranks the Himalayan hospital as first, showing that it is best in providing telemedicine services to patients. Public health policymakers could use the results of our study to devise an effective plan for patient care in crisis, like COVID-19.
Keywords: Healthcare technology, Telemedicine services, COVID-19 pandemic, Multicriteria decision-making, Patient care, Policymaking
1. Introduction
The ongoing COVID-19 pandemic has thoroughly tested even the world's best healthcare services while significantly disrupting the normal course of patient care. At the height of this pandemic, several countries encouraged both their private and public healthcare players to adopt the telemedicine services model for patient care to minimize foot traffic in hospitals and to contain the rampant spread of the virus (Hollander and Carr, 2020; Kalenzi, 2020; Siwicki, 2020; Wang et al., 2020).
E-health services use electronic tools coupled with information and communication technology (ICT) platforms to deliver the required healthcare support and services (Armfield et al., 2015; Lolich et al., 2019; Portnoy et al., 2020). In the process, it reduces nonessential visits of patients to hospitals and thereby significantly minimizes the physical interaction between a patient, doctor, and other healthcare staff (Hollander and Carr, 2020; Portnoy et al., 2020). e-health services include mobile health, medical knowledge management, and telemedicine services (Adenuga et al., 2017).
Before the COVID-19 pandemic, telemedicine services received limited attention, especially in developing nations. Therefore, infrastructural, technological, and the psychological preparedness of both patients and medical staff has been limited in adopting the services at a larger scale (Siwicki, 2020). However, its effectiveness and prospective impact in dealing with COVID-19 have changed people's mindsets globally (CDC, 2020).
Within the challenging environment engendered by the COVID-19 pandemic, telemedicine services provide comfort, safety, and flexibility to patients in taking their timely consultation from clinicians while being at home. Nevertheless, telemedicine services do come with quite a few plaguing challenges, especially for regulatory bodies, hospital administration, medical staff, and patients themselves. We, through this study, explore a few key success factors that significantly enhance their role in adapting telemedicine services both by patients and clinicians while proposing a few solutions in overcoming the hurdles posed by these challenges. The research objectives and key contributions of this study are as follows:
Research objectives
First, we identify some key success factors of telemedicine services with the help of a literature review. We cross-verify and group them after brainstorming with domain experts. Second, we reveal the causal relationship among the seven grouped criteria of telemedicine services using the DEMATEL method to understand the nature of each criterion. Third, we compute the relative importance (weights) of criteria for evaluating hospitals’ telemedicine services with the help of the Bayesian BWM method. Last, we rank the telemedicine services of the hospitals studied, using the VIKOR method for assisting patients in their decision-making, while they select a hospital for availing healthcare services.
Key contributions
This study significantly contributes to proposing a decision-making framework for the administrative body of healthcare facilities. We also contribute to identifying 37 key success factors, along with their contextual groupings, under seven criteria for rendering successful telemedicine services in India during the COVID-19 pandemic. Furthermore, we develop a causal relationship model depicting the relationships among criteria, thereby revealing their importance in decision-making. Notably, we believe that our proposed evaluation model can help in assessing the telemedicine services of hospitals.
The remainder of the paper is structured as follows: Section 2 provides a detailed literature review on digital healthcare, e-health, and telemedicine services for identifying key success factors. Section 3 encompasses the research methodology, including the DEMATEL, Bayesian BWM, and VIKOR methods. Section 4 discusses the application of the proposed model, followed by the results and a discussion of the findings. Section 5 covers the implications, limitations, and future research directions, while Section 6 concludes the study.
2. Literature review
A few researchers in the past have looked at the behavioral and operational challenges encountered by healthcare facilities in implementing smart health services. Pan et al. (2019), for instance, studied the adoption of these services and highlighted challenges, such as the intention of clinicians and nonclinicians to adopt smart healthcare systems. However, the enhancement of resiliency in the behavior of healthcare teams has been noticed after adopting digital health technology platforms (Papa et al., 2020; Rubbio et al., 2020). Martínez-Caro et al. (2018) found that the training of healthcare professionals is very important in using ICT tools and effective implementation of e-health services. Sims (2018) and Liu et al. (2020) emphasized the development of a sustainable healthcare expert community, which could use virtual platforms and engage physicians through gamification.
Digital health services do improve the efficiency of the entire healthcare system with enhanced service quality, decreased response time, and an improvised post discharge schedule, resulting in the satisfaction of patients, clinicians, and hospitals (Laurenza et al., 2018; Liu et al., 2018; Lu et al., 2021; Miao et al., 2017; Senot et al., 2016). A few other studies discussed the importance of healthcare information technologies in the collection, safety, privacy, and analysis of the huge healthcare data generated in discharging e-health and telemedicine services (Vesselkov et al., 2018; Villalba-Mora. et al., 2015; Wang et al., 2018).
Telemedicine uses ICT in safely consulting, analyzing, and transferring the patients’ healthcare data through videos, photographs, sounds, messages, and various other means of illness diagnosis (Cobelli et al., 2021). Both the implementation and adoption of the telemedicine system across the globe is the dual responsibility of policy-makers and healthcare facilities (Adenuga et al., 2017; Al-Samarraie et al., 2020; Cobelli et al., 2021). Lee and Lee (2021) carried out interesting work that revealed the opportunities and challenges in providing medical services in a contactless manner, such as in the case of telemedicine. Recently, Cobelli et al. (2021) conducted a study to understand the factors that impact the choices of adoption or non-adoption for telemedicine by community pharmacists in Italy during COVID-19. Baudier et al. (2021) studied the perception of patients about teleconsultation during COVID-19. Kaplan (2020) revisited the ethical, social, technological, privacy, and legal issues of telemedicine services at the time of the COVID-19 outbreak and proposed a framework. Similarly, Rezaei et al. (2021) specifically examined the ethical challenges in adopting telemedicine services based on key indicators, such as privacy, security, and autonomy.
Despite its benefits, telemedicine services have received limited attention, especially in emerging economies, for various reasons. Some of them include technological limitations, privacy, the familiarity of clinicians, and patients’ perception during COVID-19 (Al-Samarraie et al., 2020; Armfield et al., 2015; Baudier et al., 2021; Chandwani et al., 2018; Gamus et al., 2019; Lee and Lee, 2021). Some of the major issues in adopting telemedicine services have been experienced, such as the intention and willingness of clinicians (Adenuga et al., 2017; Cobelli et al., 2021; Rho et al., 2014); loss of autonomy, fear, and cost of technology (Xue et al., 2015); lack of technology and technical aptness of the staff, age and education level of patient (Scott Kruse et al., 2018); lack of trust and acceptance of patients (Jensen and Nielsen, 2001; Velsen et al., 2017); and the legal implications and liability (Parimbelli et al., 2018).
Jansen-Kosterink et al. (2019) suggested finding more contextual factors for the successful implementation of telemedicine services. Rezaei et al. (2021) recommended that researchers carry out further studies based on sociolegal dimensions coupled with regulatory challenges in adopting telemedicine services and digital healthcare. Some studies have specifically emphasized the identification of challenges in adopting telemedicine services by hospitals and clinicians (Cegarra-Sánchez et al., 2020; Chowdhury et al., 2021; Lee and Lee, 2021; Oderanti et al., 2021). Chandwani et al. (2018) recommended studying causal relationships among the key success factors of telemedicine services in diverse contexts. Lu et al. (2021) suggested conducting a study on the dimensions of patient satisfaction and economic aspects of telemedicine services.
Based on our extensive literature review, we did find some interesting research questions:
RQ1. What are the key success factors and their contextual dimensions (criteria) for adapting telemedicine services in India during COVID-19?
RQ2. How do the causal relationships among the criteria impact the adaptation of telemedicine services?
RQ3. What is the relative importance (weights) of criteria in comparison with one another for evaluating telemedicine services, especially during the ongoing pandemic?
RQ4. What is the rank attained by our studied hospitals based on telemedicine services that are being provided to patients?
To cater to these RQs, we first identified and prepared an exhaustive list of 37 key success factors (subcriteria) after reviewing the extant literature, along with a field survey. Furthermore, we classified them under 7 contextual dimensions (criteria) with the help of experts who participated in focused group discussions (FGDs). The key success factors along with criteria are provided with a brief description in Table 1 .
Table 1.
Description and source of key success factors.
| Contextualized dimension (Criteria) | Key success factor | Description | Source | |
|---|---|---|---|---|
| 1 | Social (C | Emotional maturity of patient | Visiting a clinician in person gives psychological strength to many patients. In the case of telemedicine services, it is absent as physical visits do not happen. Hence, the emotional maturity of a patient becomes important in his availing of telemedicine services. | (Chowdhury et al., 2021) |
| 2 | Education level and type of disease | The education plays a vital role in availing the telemedicine service and overcoming many related issues such as usage of technology and performing preliminary tests at home. | (Al-Samarraie et al., 2020; Armfield et al., 2015; Scott Kruse et al., 2018) | |
| 3 | Patient age and family background | The age of patient, i.e., child, teenager, adult or old; and his family background, such as educated family, urban/rural, rich/poor, etc. | (Oderanti et al., 2021; Scott Kruse et al., 2018) | |
| 4 | Trust in Telemedicine | This shows the trust of a patient and his social circle in telemedicine services. Trust is important for patient's acceptance of telemedicine services and helps in recovery. | (Al-Samarraie et al., 2020; Parimbelli et al., 2018; Velsen et al., 2017) | |
| 5 | Readability of prescription report | The medical examination report can be read by a patient and his caretakers or not. | This study | |
| 6 | Distance of healthcare facility | The patients from rural area must travel miles to reach to a healthcare facility which might exhaust the patient and deteriorate his condition; therefore, in such cases adoption of telemedicine services brings value to them. | (Cobelli et al., 2021; Jansen-Kosterink et al., 2019) | |
| 7 | Availability of public/private transportation | The availability of private or public transportation is required to visit a healthcare facility. In cases like the COVID-19 pandemic, due to transmission of coronavirus, public transport was halted in many countries and private vehicles were not allowed due to lockdown. | (Jansen-Kosterink et al., 2019; Scott Kruse et al., 2018) | |
| 8 | Cost of transportation | The patients who are indifferent to the mode of medicine service they use generally do a cost–benefit analysis. Hence, if the cost of transportation is very high, for example, then visiting a hospital in another area may significantly cost. | (Jansen-Kosterink et al., 2019; Scott Kruse et al., 2018) | |
| 9 | Digital literacy (e-skills) | To avail telemedicine services, e-skills and digital literacy are extremely important. Patients should know how to operate a mobile and laptop and how to download medical examination and prescription reports. | (Al-Samarraie et al., 2020; Chowdhury et al., 2021; Jansen-Kosterink et al., 2019) | |
| 10 | Availability of basic medical kit at home | Basic medical equipment, such as thermometers, doppler fetal monitors and sphygmomanometers are required for initial diagnosis, which must be performed at home. Based on these reports and other symptoms, clinicians can easily provide their prescription reports for further treatment. |
(Portnoy et al., 2020) |
|
| 11 | Environmental (C2) | Probability of catching COVID-19 infection in visiting hospital | If a pandemic like COVID-19 is occurring, then it becomes extremely risky to travel to a hospital for minor things such as fever, headache, and regular check-ups. This may be especially harmful for old age people and pregnant women. | (Hollander and Carr, 2020) |
| 12 | Availability of prescribed medicine in medical stores | If the drugs prescribed by a clinician during telemedicine consultation are available in nearby pharmacies, then it becomes easy for them to continue with telemedicine services in the future. | This study | |
| 13 | Weather condition |
In extreme weather conditions such as heavy rain, extreme hot or chilling cold, patients’ conditions may deteriorate during travel; therefore, telemedicine services can be an easy and comfortable choice for them. | This study | |
| 14 | Economic (C3) | Affordability | For utilizing telemedicine services, smart electronic gadgets and internet are essential, which might be a one-time fixed investment for many poor patients and might not suit their economic condition. | (Al-Samarraie et al., 2020) |
| 15 | Availability of bank account and payment apps | The payment in telemedicine services is accepted online,therefore patient must have access to a bank account, payment app or internet banking. | This study | |
| 16 | Technological (C4) | Availability of ICT device with doctor and patient | For seeking and giving consultation, both patient and clinician need electronic gadgets such as smartphones and laptops. | (Calton et al., 2020; Scott Kruse et al., 2018) |
| 17 | Doctor and Patient's familiarity with ICT devices | The clinician and patient must be familiar in using smart ICT devices. Video calls are one of the best considered methods for examining a patient online, as they provide the scope necessary to learning the patient and understanding their psychological condition. | (Calton et al., 2020; Jansen-Kosterink et al., 2019; Laurenza et al., 2018; Scott Kruse et al., 2018) | |
| 18 | Speed and Availability of internet | If internet speed is poor, then patient and clinician interaction cannot be performed well; therefore, having a good internet connection is extremely important for telemedicine services. | (Calton et al., 2020; Chowdhury et al., 2021; Scott Kruse et al., 2018) | |
| 19 | Digital platform usage for audio and video communication | There are various digital platforms for video calling, i.e., Skype, Google Meet, Zoom, Microsoft team, and WhatsApp. | (Armfield et al., 2015; Calton et al., 2020) | |
| 20 | Digital payment methods familiarity | Familiarity with the methods of online payment, such as apps, debit and credit cards and net-banking removes the obstacle of taking consultation through telemedicine. | This study | |
| 21 | Electronic record keeping | The electronic record keeping of videos, audios and images aids in referencing the data for patient progress. | (Wani and Malhotra, 2018) | |
| 22 | Smart e-infrastructure | The effective delivery of telemedicine services requires many investment in rather sophisticated and advanced electronic equipment. | (Adenuga et al., 2017; Al-Samarraie et al., 2020; Calton et al., 2020; Lolich et al., 2019) | |
| 23 | Proficient IT-support staff for medical team and patients | The information technology (IT) staff needs to be very proficient at connecting patients with doctors and sorting out various issues during the process. | (Al-Samarraie et al., 2020; Calton et al., 2020; Lolich et al., 2019; Scott Kruse et al., 2018) | |
| 24 | Online payment acceptance through different modes | Rural and elderly patients may have only debit cards, whereas urban patients may have net-banking and payment apps; therefore, it is required that healthcare facilities have a variety of options to accept payment from customers in providing telemedicine services. | This study | |
| 25 | Legal and Regulatory (C5) | Implementation of Government guidelines | Guidelines for standard practices and procedures must be followed during telemedicine service delivery for the benefits of patients. | (Adenuga et al., 2017; Calton et al., 2020) |
| 26 | Patient consent and secrecy of diagnosis report | The consent of a patient and his diagnosis report shall be kept confidential by healthcare facility. | (Kaplan, 2020) | |
| 27 | Strict penalty mechanism for medical malpractice | Healthcare facility must also formulate rules and regulations for strict penalties on misusing of any type of content, including audio, video, and images. | (Al-Samarraie et al., 2020) | |
| 28 | Ethical (C6) | Patient data security and privacy of conversation | The safety and security of patient data encourages patients to use telemedicine consultation from a healthcare facility. | (Al-Samarraie et al., 2020; Calton et al., 2020; Gu et al., 2019; Jansen-Kosterink et al., 2019; Lolich et al., 2019) |
| 29 | Confidentiality of Patient history and treatment follow up | The confidentiality of patient history is important as they may have a disease which might make then self- conscious. Similarly, the follow up should be performed in a very confidential manner by well-trained and experienced medical staff. |
(Chowdhury et al., 2021; Jansen-Kosterink et al., 2019) |
|
| 30 | Organizational (C7) | Willingness/Resistance to change | Telemedicine is new to patients and clinicians both, especially in developing nations; therefore, significant efforts and zeal are needed to accept this new way of receiving and providing healthcare services. | (Adenuga et al., 2017; Laurenza et al., 2018; Lolich et al., 2019; Pan et al., 2019; Rho et al., 2014; Scott Kruse et al., 2018; Xue et al., 2015) |
| 31 | Location of healthcare facility | If a healthcare facility is in a heavy traffic area and consumes lots of energy and time, then patient may prefer to adopt telemedicine mode rather than using physical visits. | This study | |
| 32 | Capacity of patient waiting area | The availability of less seating capacity and walking area also discourages patients from visiting a healthcare facility and encourages the use of telemedicine services. | (Baudier et al., 2021) | |
| 33 | Encouraging patients for telemedicine | Healthcare facilities can encourage patients by reducing their consultation fees and appreciating by other means as well. During COVID-19, less patient visits to healthcare facilities helps both parties in keeping safe and stopping the transmission of the deadly virus. | (Chowdhury et al., 2021; Hollander and Carr, 2020; Portnoy et al., 2020) | |
| 34 | Incentives to clinicians and admin | In order to increase clinicians’ interest and encourage them to learn this novel way of providing consultation through an online medium, they may be incentivized by healthcare facilities for adopting the change and flexi hours of consultation. |
(Adenuga et al., 2017; Lolich et al., 2019; Rho et al., 2014) |
|
| 35 | Overall cost reduction in healthcare operations | Fewer visits to healthcare facilities puts less burden on its physical resources. Additionally, clinicians can increase their consultation time for providing telemedicine services to patients. | (Adenuga et al., 2017; Portnoy et al., 2020) | |
| 36 | Number of doctors and nursing staff available for patient care in hospital | A top-down thrust works effectively for adopting telemedicine services in a healthcare facility where the quality of clinicians is good, but there are fewer of them. Hence, delivering telemedicine services may help in gathering more patients. | (Adenuga et al., 2017; Hollander and Carr, 2020) | |
| 37 | Quality care | The quality of care extended by a healthcare facility and its clinicians is a very important factor for positively adopting and sustaining telemedicine services by a patient. | (Kaplan, 2020; Lolich et al., 2019; Senot et al., 2016) |
3. Research methodology
This study was carried out with the help of a comprehensive three-stage hybrid methodology of the DEMATEL, Bayesian BWM, and VIKOR methods. DEMATEL helps to reveal the causal relationships among the system of criteria in a study (Fontela and Gabus, 1976). In previous studies, DEMATEL had been applied in various research contexts, including vaccine supply chain management, hospital service quality assessment and medical tourism (Nilashi et al., 2019; Tanvir et al., 2021). Similarly, in our study, DEMATEL helped us explore the causal relations among seven criteria. Thereafter, the Bayesian BWM method is applied, which helps in identifying the importance of criteria in terms of their weights and provides a credal ranking order of the criteria (Mohammadi and Rezaei, 2019; Rezaei, 2015).
Our study is one of the first to apply Bayesian BWM since its introduction by Mohammadi and Rezaei (2019); however, BWM has been applied in a wider range of studies, including hospital performance evaluation and offshore outsourcing adoption for automotive companies (Liao et al., 2019; Yadav et al., 2018). Finally, the VIKOR method helps in achieving the compromised ranking of different alternatives with the help criteria weights under study (Opricovic and Tzeng, 2004). VIKOR has been applied in fields such as the online selection of doctors for medical consultation, green performance evaluation of airports and renewal energy project selection (Kumar et al., 2020; San Cristóbal, 2011; Yadav et al., 2018). Recently, frameworks with multimethod approaches have been proposed in studies such as technology acquisition for telecom companies and the selection of healthcare waste disposal firms (Chauhan and Singh, 2021; Dahooie et al., 2021). Our stepwise explanation of the research methods used in this study is given in Appendix A2 (DEMATEL method), Appendix A3 (Bayesian BWM method), and Appendix A5 (VIKOR method).
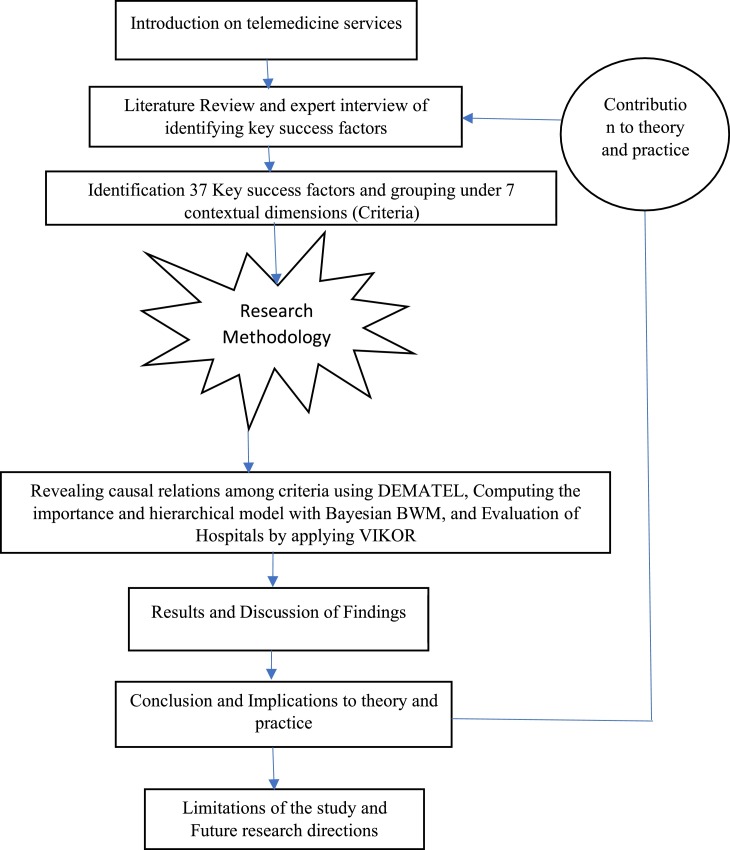
A brief description of the present study is provided in Fig. 1 .
Fig. 1.
Flow of the Study.
4. Application case
The 37 key success factors identified for telemedicine services are contextualized under 7 major dimensions (criteria): social, environmental, economic, technological, legal and regulatory, ethical, and organizational. Since we have adopted a three-step methodology, presented in Section 3, to conduct this study, our data collection has been done separately on each of the stages; please refer to Appendix A1. In the first stage, we collected data from medical practitioners in primary, secondary and tertiary healthcare settings. Three groups comprising 9 to 11 clinicians participated through video conferencing where they identified and cross-verified the key success factors of telemedicine services grouped under the previously mentioned 7 criteria; second, they participated in providing responses for the DEMATEL matrix.
In the second step, the clinicians were asked to provide their responses in groups of 3 for the BWM criteria response matrix. In total, 7 groups of clinicians and senior medical administrative staff members participated through video conferencing to provide their responses on the Saaty scale (Saaty, 1980). In the third step, the data collection was done from healthcare facilities of the clinicians who participated in the previous two stages; the confidentiality of the responses was maintained by disguising the names of healthcare facilities. These responses were recorded from the hospital's administrative unit supervisors against each of the 7 criteria for six participating hospitals, namely, Sunflag, CMI, Vardaan, Metro, Himalyan, and Holy.
4.1. Discussion of findings
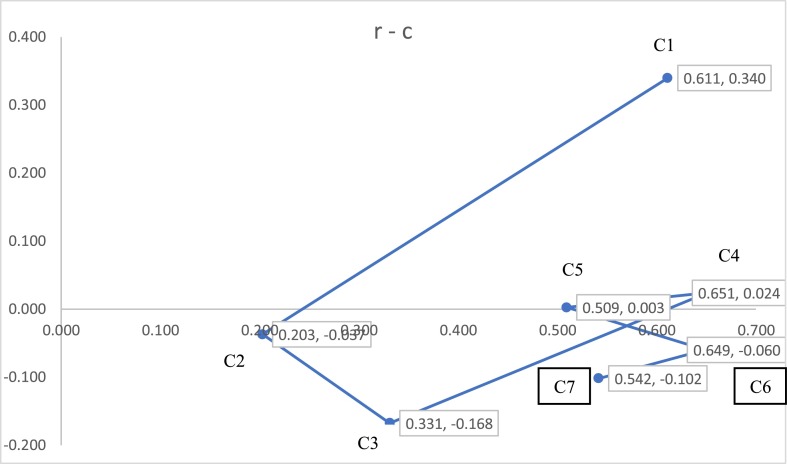
After analyzing the data with DEMATEL (in Appendix A2, refer to Table A2.1 and Table A2.9), the net causes and net receivers are presented in Table 2 . To show the impact of net causes and net receivers in the system, we have provided Fig. 2 for pictorial representation.
Table 2.
Cause-effect diagram table.
| r | c | r + c | r - c | |
|---|---|---|---|---|
| C1 | 0.475 | 0.136 | 0.611 | 0.340 |
| C2 | 0.083 | 0.120 | 0.203 | −0.037 |
| C3 | 0.082 | 0.249 | 0.331 | −0.168 |
| C4 | 0.338 | 0.314 | 0.651 | 0.024 |
| C5 | 0.256 | 0.253 | 0.509 | 0.003 |
| C6 | 0.295 | 0.354 | 0.649 | −0.060 |
| C7 | 0.220 | 0.322 | 0.542 | −0.102 |
r is the sum of a given row; c is the sum of a given column; r + c shows the intensity of the relationship among criteria; and r-c shows the intensity of the impact among criteria.
Fig. 2.
DEMATEL Causal relation diagram for criteria.
The data provided by groups of respondents are analyzed with the DEMATEL method using a four-step methodology. In Table 2, the criteria C4>C6>C1>C7>C5>C3>C2 can be ordered according to their importance in the entire system based on their r + c values, which shows that technological criteria with the value of 0.651 are the most important for the success of telemedicine services, whereas environmental criteria with the value of 0.203 are the least important for telemedicine services. The r-c value given in Table 2 shows the impact that a criterion can make on the entire system as a net cause (if it is positive); however, a negative value of r-c for a criterion makes it a net receiver despite a net cause.
We can observe in Table 2 that criteria C2, C3, C6, and C7 are net receivers, whereas criteria C1, C4, and C5 are net causes. Hence, as shown in the digraph given in Fig. 2, the social criterion (C1) is not influenced by other criteria, but it influences the environmental criterion (C2) directly. Most criteria mutually influence each other, acting as a net cause or net effect. Hence, the digraph shown in Fig. 2 depicts a causal relationship diagram among the criteria for successful adoption of telemedicine services in India.
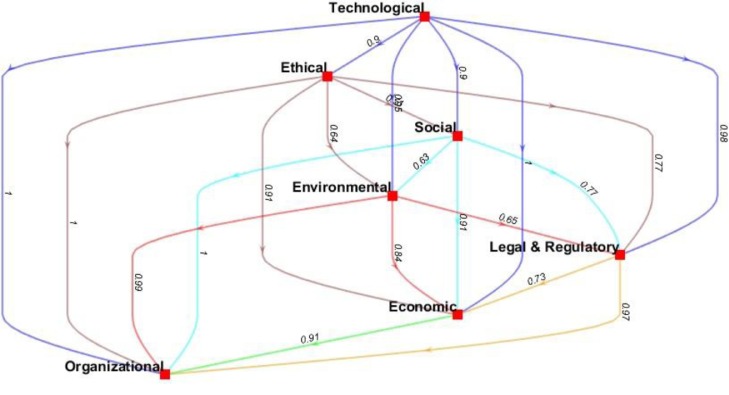
The results are obtained after analyzing the respondents’ responses (please refer to Appendix A3, Table A3.1 and Table A3.2) using the Bayesian BWM method. We have also presented the Bayesian hierarchical model given in Fig. 3 and obtained with the help of MATLAB code (provided in Appendix A4).
Fig. 3.
Bayesian BWM Hierarchical Model.
After revealing the nature of the criteria and their overall impact on the decision-making of telemedicine service adoption, the weights of these criteria are computed using the Bayesian BWM method from the inputs received from clinicians of 7 groups. The Bayesian BWM helps in providing the weights and the confidence associated with it, i.e., ; criterion X is more important than Y with confidence t. This can be easily observed in the credal ranking (hierarchical model) provided in Fig. 3, which shows that a technological criterion is more important than an ethical criterion with a confidence of 0.90. Similarly, the social criterion is more important than the economic criterion, and the ethical criterion is more important than the organizational criterion, with confidence levels of 0.91 and 0.99, respectively. Interestingly, it can be noted from the hierarchical model that ethical, social and environmental criteria are more important than legal and regulatory criteria, with confidence levels of 0.77, 0.77 and 0.65, respectively, which are low for generalization. However, it indicates that in the case of telemedicine services, considering ethical, social, and environmental criteria may be sufficient and strong, but it may be insufficient and weak in any other problem. The weights obtained through the Bayesian BWM given in Table 3 are 0.205, 0.157, 0.156, 0.145, 0.134, 0.117, and 0.087 for technological, ethical, social, environmental, legal and regulatory, economic, and organizational criteria, respectively. The higher weight of a criterion represents its importance in the adoption of telemedicine services by different stakeholders. The MATLAB code for Bayesian BWM is given Appendix A4.
Table 3.
Bayesian BWM criteria weights.
| Criteria | Social (C1) | Environmental (C2) | Economic (C3) | Technological (C4) | Legal & regulatory (C5) | Ethical (C6) | Organizational (C7) |
|---|---|---|---|---|---|---|---|
| Weights | 0.156 | 0.145 | 0.117 | 0.205 | 0.134 | 0.157 | 0.087 |
The criteria-alternatives matrix obtained from the respondents and analyzed (please refer Appendix A5, Table A5.1 to Table A5.4) with the help of the VIKOR method. The ranking of the hospitals based on their final Sj, Rj, and Qj scores is given in Table 4 .
Table 4.
Ranking order based on Sj, Rj & Qj.
| Hospitals rank | Sj | Hospitals rank | Rj | Hospitals rank | Qj | ||
|---|---|---|---|---|---|---|---|
| H1 | 0.369 | H2 | 0.137 | H2 | 0.013 | ||
| H2 | 0.372 | H3 | 0.137 | H1 | 0.024 | ||
| H3 | 0.447 | H1 | 0.145 | H3 | 0.282 | ||
| H6 | 0.563 | H6 | 0.205 | H6 | 0.903 | ||
| H4 | 0.573 | H4 | 0.205 | H4 | 0.939 | ||
| H5 | 0.590 | H5 | 0.205 | H5 | 1.000 |
With the help of the inputs received from the Bayesian BWM, the telemedicine services provided by six hospitals, namely, Himalayan (H1), Holy (H2), Vardaan (H3), Metro (H4), CMI (H5), and Sunflag, are ranked using the VIKOR method. The values are used to rank these hospitals, for which the ranking is given in Table 4. Since it is evident from Table 4 that the ranking for hospitals is different in the case of , a compromised ranking is achieved through the process as described in the methodology section of VIKOR.
After satisfying Condition 1 and Condition 2, we find that Himalayan Hospital (H1) attains rank 1 in providing telemedicine services to patients. According to Condition 1, is the alternative with second position in the ranking list prepared using Q value; ; and J is the number of alternatives. For the second condition to be satisfied, the alternative must have been ranked 1st either or both. Hence, in our case, , which is less than and does not satisfy the required condition; however, , and alternative 1 (H1) is also ranked 1st by , which satisfies the second condition. Therefore, after compromised ranking, Himalayan hospitals (H1) are ranked 1st in providing telemedicine services. Tables A4.1 and A4.2 in Appendix A6 provide a detailed analysis of the compromised ranking.
The framework proposed in this study overcomes the limitations of the theoretical modeling of barriers conducted by Al-Samarraie et al. (2020). Their proposed fishbone model classified the barriers under contextual dimensions of challenges in adopting telemedicine services wherein our proposed decision-making framework helps in quantifying the importance of criteria and ranks the telemedicine services of hospitals for the benefit of patients and other stakeholders.
5. Implications and future research directions
5.1. Implications of the study
5.1.1. Theoretical implications
A setting for the successful adoption of telemedicine services is a novel contribution of this study to the theory of telemedicine services (Al-Samarraie et al., 2020; CDC, 2020). Several key success factors within contextual dimensions (criteria), which facilitate the adoption of telemedicine services during the COVID-19 pandemic, were included in this study. Key success factors, such as emotional maturity, readability of doctors’ prescription reports, availability of basic medical kits at home, probability of catching COVID-19 infection in visiting hospitals, availability of prescribed medicines at pharmacies, bank accounts and payment apps, and digital payment method familiarity, are important factors that drive patients’ intention to adopt telemedicine services during pandemic times. Similarly, key success factors, such as the capacity of the patient waiting area, online payment acceptance by hospitals and clinicians, confidentiality of patient history and treatment follow-up, and encouraging patients to avail themselves of telemedicine services, are some of the important factors that require hospital and government attention to create a convenient environment to motivate patients to adopt telemedicine services. The successful adoption of telemedicine services during a pandemic scenario such as COVID-19 may significantly reduce new infections due to the absence of physical contact and help noncritical patients with various diseases to recover at home.
5.1.2. Managerial and policy implications
The triple method-based hybrid model proposed in this study may help hospitals work upon the key criteria for making their telemedicine services more acceptable to patients, hospitals, and clinicians. DEMATEL- and Bayesian BWM-based causal and hierarchical analyses revealed that technological, social, and ethical criteria were more important than environmental, economic, legal and regulatory criteria and organizational criteria for enhancing the adoption of telemedicine services during the pandemic crisis. Hence, hospitals and governments can work upon these criteria for the successful implementation of telemedicine services in hospitals. Government policymakers can evaluate the comparative performance of telemedicine services providing hospitals and assist patients in selecting the best hospitals from their vicinity using our hybrid model. Government bodies may devise robust legal and regulatory policies for patient and hospital security from cybercrime (Jercich, 2020) in addition to the other important criteria proposed in our study for enhancing the adoption of telemedicine services across the world during and after the COVID-19 pandemic.
5.2. Limitations and future research directions
The criteria studied in the present study are in groups that could not have brought the interrelations of key success factors within each criterion; therefore, in future work, each criterion can be studied separately to reveal the interrelationships within it. Second, this study covers the clinician's opinion from all types of healthcare settings, which makes it more acceptable but unspecific to one type of healthcare setting. Hence, in future studies, researchers can carry out work specifically in each type of healthcare setting. Finally, the clinicians who worked as experts in this study came from six states; therefore, increasing the versatility of responses with an increase in the number of states may bring minor changes to our findings; therefore, in the future, work can be carried out with the inclusion of more participating clinician states.
6. Conclusion
In the present study, 7 contextualized dimensions (criteria) were proposed based on 37 key success factors that help patients and clinicians adopt telemedicine services. We found that the causal digraph obtained with the help of the decision-making trial and evaluation laboratory method vividly classifies the seven criteria into net causes and net receivers. Social, technological, legal and regulatory factors were found to be net causes, whereas environmental, economic, ethical, and organizational factors evolved as net receivers in a system of criteria for healthcare service adoption. Furthermore, for evaluating the importance of each criterion, the application of the Bayesian best worst method resulted in a credal ranking (hierarchical model) order along with the confidence of a criterion being better than the others in telemedicine service adoption. The credal ranking revealed that technological criteria are most important, whereas organizational criteria are least important for patients and clinicians to adopt telemedicine services.
Henceforth, the criteria weights were used to rank the hospitals that provided telemedicine services to patients using the VIKOR method. Himalayan hospitals are found to be the best hospitals for providing telemedicine services to patients. Hence, this robust three-stage methodology provides a solution model for hospitals that can be used to make their healthcare services more comfortable to patients and clinicians. Specifically, during times of COVID-19, telemedicine services must be provided effectively to contain the virus, maintain social distancing, and reduce the burden on hospitals.
CRediT authorship contribution statement
Ankur Chauhan: Methodology, Investigation, Writing – original draft, Formal analysis. Suresh Kumar Jakhar: Conceptualization, Writing – review & editing. Charbel Jose Chiappetta Jabbour: Software, Validation, Supervision, Project administration.
Biographies
Ankur Chauhan: Dr. Ankur Chauhan is working as an Assistant Professor at Jaipuria Institute of Management Noida. Ankur is a PhD in the area of operations management from IIM Rohtak, India. In his thesis work, he has developed a decision support framework for healthcare waste management in India. Ankur has published 15 articles which incorporates 14 research articles and one book chapter on the issue waste management, agri-food supply chain, industry 4.0 and circular economy . His interest lies in the fields such as waste management, supply chain management, and reverse logistics.
Suresh Kumar Jakhar: Dr. Suresh K Jakhar is currently working as an Associate Professor at Operations Management Group at IIM Lucknow. He has been included in the Stanford University's ranking of the 2% most cited scientists globally (2021). At IIM Lucknow he is teaching courses like Revenue Management and Dynamic Pricing, Game Theory and Mechanism Design and Supply Chain Management. He has completed his M.Tech from IIT Delhi and PhD from IIT Roorkee. He has published more than 30 research papers in various international journals.
Charbel Jose Chiappetta Jabbour: Charbel Jose Chiappetta Jabbour is currently working as a Professor at Emlyon Business School, France. He has been included in the Stanford University's ranking of the 2% most cited scientists globally (2020). He is amongst the Top#10 most prolific researcher in 'Green Supply Chain Management' worldwide, according to SCOPUS (September 2020, C Jabbour/Chiappetta Jabbour). As one of the pioneers of 'Green Supply Chain Management' in emerging economies, his innovative research influenced the agenda on sustainable chains in Latin America. He is currently Principal Investigator of a Midlands Engine Research Project, and Co-Investigator of an Innovate UK large-scale project. With > 12,500 citations according to Google Scholar, H Index=55, and ranked in the top 2.5% globally for research impact according to ResearchGate score (September 2020), Professor Chiappetta Jabbour's interdisciplinary research focuses on pressing issues regarding sustainable supply chains, such as the role of industry 4.0 in unlocking sustainability in supply chains, critical human success factors for sustainable production, and innovative business models for the circular economy.
References
- Adenuga K.I., Iahad N.A., Miskon S. Towards reinforcing telemedicine adoption amongst clinicians in Nigeria. Int. J. Med. Inform. 2017;104:84–96. doi: 10.1016/j.ijmedinf.2017.05.008. [DOI] [PubMed] [Google Scholar]
- Al-Samarraie H., Ghazal S., Alzahrani A.I., Moody L. Telemedicine in Middle Eastern Countries: progress, barriers, and policy recommendations. Int. J. Med. Inform. 2020;141 doi: 10.1016/j.ijmedinf.2020.104232. [DOI] [PubMed] [Google Scholar]
- Armfield N.R., Bradford M., Bradford N.K. The clinical use of Skype—For which patients, with which problems and in which settings? A snapshot review of the literature. Int. J. Med. Inform. 2015;84:737–742. doi: 10.1016/j.ijmedinf.2015.06.006. [DOI] [PubMed] [Google Scholar]
- Baudier P., Kondrateva G., Ammi C., Chang V., Schiavone F. Patients’ perceptions of teleconsultation during COVID-19: a cross-national study. Technol. Forecast. Soc. Change. 2021;163 doi: 10.1016/j.techfore.2020.120510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calton B., Abedini N., Fratkin M. Telemedicine in the time of coronavirus. J. Pain Symptom Manage. 2020;60:e12–e14. doi: 10.1016/j.jpainsymman.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Uses of Telehealth during COVID-19 in Low Resource Non-U.S. Settings [WWW Document] Natl. Cent. Immun. Respir. Dis. 2020 https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/telehealth-covid19-nonUS.html URL. (accessed 8.11.20) [Google Scholar]
- Chandwani R., De R., Dwivedi Y.K. Telemedicine for low resource settings: exploring the generative mechanisms. Technol. Forecast. Soc. Change. 2018;127:177–187. doi: 10.1016/j.techfore.2017.06.014. [DOI] [Google Scholar]
- Chauhan A., Singh S.P. Selection of healthcare waste disposal firms using a multi-method approach. J. Environ. Manage. 2021;295 doi: 10.1016/j.jenvman.2021.113117. [DOI] [PubMed] [Google Scholar]
- Chowdhury S.R., Sunna T.C., Ahmed S. Telemedicine is an important aspect of healthcare services amid COVID-19 outbreak: its barriers in Bangladesh and strategies to overcome. Int. J. Health Plann. Manage. 2021;36:4–12. doi: 10.1002/hpm.3064. [DOI] [PubMed] [Google Scholar]
- Cobelli N., Cassia F., Burro R. Factors affecting the choices of adoption/non-adoption of future technologies during coronavirus pandemic. Technol. Forecast. Soc. Change. 2021;169 doi: 10.1016/j.techfore.2021.120814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahooie J.H., Qorbani A.R., Daim T. Providing a framework for selecting the appropriate method of technology acquisition considering uncertainty in hierarchical group decision-making: case Study: interactive television technology. Technol. Forecast. Soc. Change. 2021;168 doi: 10.1016/j.techfore.2021.120760. [DOI] [Google Scholar]
- Fontela, E., Gabus, A., 1976. The DEMATEL observer, DEMATEL 1976 Report Switzerland Geneva: Battelle Geneva Research Centre.
- Gu D., Li T., Wang X., Yang X., Yu Z. Visualizing the intellectual structure and evolution of electronic health and telemedicine research. Int. J. Med. Inform. 2019;130 doi: 10.1016/j.ijmedinf.2019.08.007. [DOI] [PubMed] [Google Scholar]
- Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- Jansen-Kosterink S., Dekker-van Weering M., van Velsen L. Patient acceptance of a telemedicine service for rehabilitation care: a focus group study. Int. J. Med. Inform. 2019;125:22–29. doi: 10.1016/j.ijmedinf.2019.01.011. [DOI] [PubMed] [Google Scholar]
- Jercich K. Cybercriminals seek to take advantage of rapid telehealth scale-up [WWW Document] Healthc. IT News. 2020 https://www.healthcareitnews.com/news/cybercriminals-seek-take-advantage-rapid-telehealth-scale URL. (accessed 9.4.21) [Google Scholar]
- Kalenzi C. Telemedicine can be a COVID-19 game-changer. Here's how [WWW Document] World Econ. Forum. 2020 https://www.weforum.org/agenda/2020/05/telemedicine-covid-19-game-changer/ URL. (accessed 8.11.20) [Google Scholar]
- Kaplan B. Revisiting health information technology ethical, legal, and social issues and evaluation: telehealth/telemedicine and COVID-19. Int. J. Med. Inform. 2020;104239 doi: 10.1016/j.ijmedinf.2020.104239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A., Aswin A., Gupta H. 2020. Evaluating green performance of the airports using hybrid BWM and VIKOR methodology. Tour. Manag. 2020;76 doi: 10.1016/j.tourman.2019.06.016. [DOI] [Google Scholar]
- Laurenza E., Quintano M., Schiavone F., Vrontis D. The effect of digital technologies adoption in healthcare industry: a case based analysis. Bus. Process Manag. J. 2018;24:1124–1144. doi: 10.1108/BPMJ-04-2017-0084. [DOI] [Google Scholar]
- Lee S.M., Lee D. Opportunities and challenges for contactless healthcare services in the post-COVID-19 Era. Technol. Forecast. Soc. Change. 2021;167 doi: 10.1016/j.techfore.2021.120712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao H., Mi X., Yu Q., Luo L. Hospital performance evaluation by a hesitant fuzzy linguistic best worst method with inconsistency repairing. J. Clean. Prod. 2019;232:657–671. doi: 10.1016/j.jclepro.2019.05.308. [DOI] [Google Scholar]
- Liu J., Zhang X., Meng F., Lai K.H. Deploying gamification to engage physicians in an online health community: an operational paradox. Int. J. Prod. Econ. 2020;228 doi: 10.1016/j.ijpe.2020.107847. [DOI] [Google Scholar]
- Liu X., Hu M., Helm J.E., Lavieri M.S., Skolarus T.A. Missed opportunities in preventing hospital readmissions: redesigning post-discharge checkup policies. Prod. Oper. Manag. 2018;27:2226–2250. doi: 10.1111/poms.12858. [DOI] [Google Scholar]
- Lolich L., Riccò I., Deusdad B., Timonen V. Embracing technology? Health and social care professionals’ attitudes to the deployment of e-Health initiatives in elder care services in Catalonia and Ireland. Technol. Forecast. Soc. Change. 2019;147:63–71. doi: 10.1016/j.techfore.2019.06.012. [DOI] [Google Scholar]
- Lu W., Hou H., Ma R., Chen H., Zhang R., Cui F., Zhang Q., Gao Y., Wang X., Bu C., Zhao J., Zhai Y. Influencing factors of patient satisfaction in teleconsultation: a cross-sectional study. Technol. Forecast. Soc. Change. 2021;168 doi: 10.1016/j.techfore.2021.120775. [DOI] [Google Scholar]
- Martínez-Caro E., Cegarra-Navarro J.G., García-Pérez A., Fait M. Healthcare service evolution towards the Internet of Things: an end-user perspective. Technol. Forecast. Soc. Change. 2018;136:268–276. doi: 10.1016/j.techfore.2018.03.025. [DOI] [Google Scholar]
- Miao R., Wu Q., Wang Z., Zhang X., Song Y., Zhang H., Sun Q., Jiang Z. Factors that influence users’ adoption intention of mobile health: a structural equation modeling approach. Int. J. Prod. Res. 2017;55:5801–5815. doi: 10.1080/00207543.2017.1336681. [DOI] [Google Scholar]
- Mohammadi M., Rezaei J. Bayesian best-worst method: a probabilistic group decision making model. Omega (Westport) 2019;96 doi: 10.1016/j.omega.2019.06.001. [DOI] [Google Scholar]
- Nilashi M., Samad S., Manaf A.A., Ahmadi H., Rashid T.A., Munshi A., Almukadi W., Ibrahim O., Ahmed O.H. Factors influencing medical tourism adoption in Malaysia: a DEMATEL-Fuzzy TOPSIS approach. Comput. Ind. Eng. 2019;139 doi: 10.1016/j.cie.2019.106005. [DOI] [Google Scholar]
- Oderanti F.O., Li F., Cubric M., Shi X. Business models for sustainable commercialisation of digital healthcare (eHealth) innovations for an increasingly ageing population:(A new business model for eHealth) Technol. Forecast. Soc. Change. 2021;171 doi: 10.1016/j.techfore.2021.120969. [DOI] [Google Scholar]
- Opricovic S., Tzeng G.H. Compromise solution by MCDM methods: a comparative analysis of VIKOR and TOPSIS. Eur. J. Oper. Res. 2004;156:445–455. doi: 10.1016/S0377-2217(03)00020-1. [DOI] [Google Scholar]
- Pan J., Ding S., Wu D., Yang S., Yang J. Exploring behavioural intentions toward smart healthcare services among medical practitioners: a technology transfer perspective. Int. J. Prod. Res. 2019;57:5801–5820. doi: 10.1080/00207543.2018.1550272. [DOI] [Google Scholar]
- Papa A., Mital M., Pisano P., Del Giudice M. E-health and wellbeing monitoring using smart healthcare devices: an empirical investigation. Technol. Forecast. Soc. Change. 2020;153 doi: 10.1016/j.techfore.2018.02.018. [DOI] [Google Scholar]
- Parimbelli E., Bottalico B., Losiouk E., Tomasi M., Santosuosso A., Lanzola G., Quaglini S., Bellazzi R. Trusting telemedicine: a discussion on risks, safety, legal implications and liability of involved stakeholders. Int. J. Med. Inform. 2018;112:90–98. doi: 10.1016/j.ijmedinf.2018.01.012. [DOI] [PubMed] [Google Scholar]
- Portnoy J., Waller M., Elliott T. Telemedicine in the Era of COVID-19. J. Allergy Clin. Immunol. Pract. 2020;8:1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezaei J. Best-worst multi-criteria decision-making method. Omega (Westport) 2015;53:49–57. doi: 10.1016/j.omega.2014.11.009. [DOI] [Google Scholar]
- Rezaei M., Jafari-Sadeghi V., Cao D., Mahdiraji H.A. Key indicators of ethical challenges in digital healthcare: a combined Delphi exploration and confirmative factor analysis approach with evidence from Khorasan province in Iran. Technol. Forecast. Soc. Change. 2021;167 doi: 10.1016/j.techfore.2021.120724. [DOI] [Google Scholar]
- Rho M.J., Choi I., young Lee, J. Predictive factors of telemedicine service acceptance and behavioral intention of physicians. Int. J. Med. Inform. 2014;83:559–571. doi: 10.1016/j.ijmedinf.2014.05.005. [DOI] [PubMed] [Google Scholar]
- Rubbio I., Bruccoleri M., Pietrosi A., Ragonese B. Digital health technology enhances resilient behaviour: evidence from the ward. Int. J. Oper. Prod. Manag. 2020;40:34–67. doi: 10.1108/IJOPM-02-2018-0057. [DOI] [Google Scholar]
- Saaty, T.L., 1980. The analytic hierarchy process: planning, priority setting, resources allocation, 1st ed., McGraw-Hill, New York, NY, 1980.
- San Cristóbal J.R. Multi-criteria decision-making in the selection of a renewable energy project in spain: the Vikor method. Renew. energy. 2011;36:498–502. doi: 10.1016/j.renene.2010.07.031. [DOI] [Google Scholar]
- Scott Kruse C., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J. Telemed. Telecare. 2018;24:4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senot C., Chandrasekaran A., Ward P.T. Collaboration between service professionals during the delivery of health care: evidence from a multiple-case study in US hospitals. J. Oper. Manag. 2016;42:67–79. doi: 10.1016/j.jom.2016.03.004. [DOI] [Google Scholar]
- Sims J.M. Communities of practice: telemedicine and online medical communities. Technol. Forecast. Soc. Change. 2018;126:53–63. doi: 10.1016/j.techfore.2016.08.030. [DOI] [Google Scholar]
- Siwicki B. Telemedicine during COVID-19: benefits, limitations, burdens, adaptation [WWW Document] Healthc. IT News. 2020 https://www.healthcareitnews.com/news/telemedicine-during-covid-19-benefits-limitations-burdens-adaptation URL. (accessed 8.11.20) [Google Scholar]
- Tanvir S., Ahmed S., Mithun S., Sarker S., Kabir G. International journal of production economics challenges to COVID-19 vaccine supply chain : implications for sustainable development goals. Int. J. Prod. Econ. 2021;239 doi: 10.1016/j.ijpe.2021.108193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velsen L.van, Tabak M., Hermens H. Measuring patient trust in telemedicine services: development of a survey instrument and its validation for an anticoagulation web-service. Int. J. Med. Inform. 2017;97:52–58. doi: 10.1016/j.ijmedinf.2016.09.009. [DOI] [PubMed] [Google Scholar]
- Vesselkov A., Hämmäinen H., Töyli J. Technology and value network evolution in telehealth. Technol. Forecast. Soc. Change. 2018;134:207–222. doi: 10.1016/j.techfore.2018.06.011. [DOI] [Google Scholar]
- Villalba-Mora E., C I., V F.L., M I. Adoption of health information technologies by physicians for clinical practice: the Andalusian case. Int. J. Med. Inform. 2015;84:477–485. doi: 10.1016/j.ijmedinf.2015.03.002. [DOI] [PubMed] [Google Scholar]
- Wang X., Zhang Z., Yang L., Zhao J. Price and capacity decisions in a telemedicine service system under government subsidy policy. Int. J. Prod. Res. 2020:1–14. doi: 10.1080/00207543.2020.1774090. [DOI] [Google Scholar]
- Wang Y., Kung L., Byrd T.A. Big data analytics: understanding its capabilities and potential benefits for healthcare organizations. Technol. Forecast. Soc. Change. 2018;126:3–13. doi: 10.1016/j.techfore.2015.12.019. [DOI] [Google Scholar]
- Wani D., Malhotra M. Does the meaningful use of electronic health records improve patient outcomes? J. Oper. Manag. 2018;60:1–18. doi: 10.1016/j.jom.2018.06.003. [DOI] [Google Scholar]
- Xue Y., Liang H., Mbarika V., Hauser R., Schwager P., Getahun M.K. Investigating the resistance to telemedicine in Ethiopia. Int. J. Med. Inform. 2015;84:537–547. doi: 10.1016/j.ijmedinf.2015.04.005. [DOI] [PubMed] [Google Scholar]
- Yadav G., Mangla S.K., Luthra S., Jakhar S. Hybrid BWM-ELECTRE-based decision framework for effective offshore outsourcing adoption: a case study. Int. J. Prod. Res. 2018;56:6259–6278. doi: 10.1080/00207543.2018.1472406. [DOI] [Google Scholar]