Abstract
Background
The novel 2019 coronavirus disease (COVID-19), which is caused by infection with the severe acute respiratory syndrome coronavirus 2, has spread rapidly around the world and has caused many deaths. COVID-19 involves a systemic hypercoagulable state and arterial/venous thrombosis which induces unfavorable prognosis. Herein, we present a first case in East Asia where an acute superior mesenteric artery (SMA) occlusion associated with COVID-19 pneumonia was successfully treated by surgical intervention.
Case presentation
A 70-year-old man presented to his local physician with a 3-day history of cough and diarrhea. A real-time reverse transcriptase-polymerase chain reaction test showed positive for COVID-19, and he was admitted to the source hospital with the diagnosis of moderate COVID-19 pneumonia. Eight days later, acute onset of severe abdominal pain appeared with worsening respiratory condition. Contrast CT showed that bilateral lower lobe/middle lobe and lingula ground glass opacification with distribution suggestive of COVID-19 pneumonia and right renal infarction. In addition, it demonstrated SMA occlusion with intestinal ischemia suggesting extensive necrosis from the jejunum to the transverse colon. The patient underwent an emergency exploratory laparotomy with implementing institutional COVID-19 precaution guideline. Upon exploration, the intestine from jejunum at 100 cm from Treitz ligament to middle of transverse colon appeared necrotic. Necrotic bowel resection was performed with constructing jejunostomy and transverse colon mucous fistula. We performed second surgery to close the jejunostomy and transverse colon mucous fistula with end-to-end anastomosis on postoperative day 22. The postoperative course was uneventful and he moved to another hospital for rehabilitation to improve activities of daily living (ADLs) on postoperative day 45. As of 6 months after the surgery, his ADLs have completely improved and he has returned to social life without any intravenous nutritional supports.
Conclusions
Intensive treatment including surgical procedures allowed the patient with SMA occlusion in COVID-19 pneumonia to return to social life with completely independent ADLs. Although treatment for COVID-19 involves many challenges, including securing medical resources and controlling the spread of infection, when severe abdominal pain occurs in patients with COVID-19, physicians should consider SMA occlusion and treat promptly for life-saving from this deadly combination.
Keywords: Superior mesenteric artery occlusion, COVID-19, SARS-CoV-2
Background
The novel 2019 coronavirus disease (COVID-19), which is caused by infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread rapidly around the world and has caused many deaths [1]. Although efforts to recognize and manage COVID-19 have been focused on elucidating the respiratory complications, it has now become clear that COVID-19 infection occasionally involves atypical presentations, such as gastrointestinal manifestation and thromboembolic complications [2, 3]. COVID-19 may predispose to both venous and arterial thromboembolism including stroke, myocardial infarction, acute limb ischemia, mesenteric ischemia, deep venous thrombosis, and pulmonary embolism, due to excessive inflammation, hypoxia, immobilization and diffuse intravascular coagulation [2–7].
Acute mesenteric ischemia, especially superior mesenteric artery (SMA) occlusion, is a critical condition with a high mortality rate of 60–80% which requires urgent diagnosis and treatment [8, 9]. COVID-19 and acute SMA occlusion seem to be a very deadly combination knowing the destructive nature of both alone [9]. To date, limited cases of these lethal patient subgroup have been reported in the world. Herein, we report a first case of SMA occlusion in patient with COVID-19 pneumonia successfully treated by surgical intervention in East Asia.
Case presentation
A 70-year-old man, who had been taking with aspirin, dabigatran and other medication for atrial fibrillation, hypertension, type 2 diabetes mellitus and dyslipidemia, presented to his local physician with a 3-day history of cough and diarrhea. A real-time reverse transcriptase-polymerase chain reaction test of his nasopharyngeal swab specimen showed positive for SARS-CoV-2 nucleic acid, and he was admitted to the source hospital with the diagnosis of moderate COVID-19 pneumonia. He had been administered one liter of supplemental oxygen via nasal cannula and treated by remdesivir and dexamethasone. Antithrombotic therapy with dabigatran and aspirin for comorbidities was continued after his admission.
Eight days later, acute onset of severe abdominal pain appeared, and he was diagnosed as right renal infarction by contrast computed tomography (CT) at that time. Although heparinization was administered immediately, his clinical course was complicated with worsening abdominal pain and respiratory condition. On the next day, he was transferred to our hospital with severe general condition, and intubated immediately. Contrast CT in our hospital showed that bilateral lower lobe/middle lobe and lingula ground glass opacification with distribution suggestive of COVID-19 pneumonia and right renal infarction. In addition, it demonstrated SMA occlusion with intestinal ischemia suggesting extensive necrosis from the jejunum to the transverse colon (Fig. 1a–c). A retrospective re-review of the CT at the previous hospital showed SMA occlusion was already presented at that time. After consultation with surgery departments, the patient underwent an emergency exploratory laparotomy. During operation, institutional COVID-19 precaution guideline was implemented with appropriate personal protective equipment. Upon exploration, the intestine from jejunum at 100 cm from Treitz ligament to middle of transverse colon appeared clearly necrotic. We resected necrotic bowel and evaluated the blood flow in the preserved intestine by utilizing an indocyanine green fluorescence imaging device, photodynamic eye camera. Although intestinal blood flow was confirmed by the system, considering severe general condition of the patient, we constructed jejunostomy and transverse colon mucous fistula without primary anastomosis.
Fig. 1.
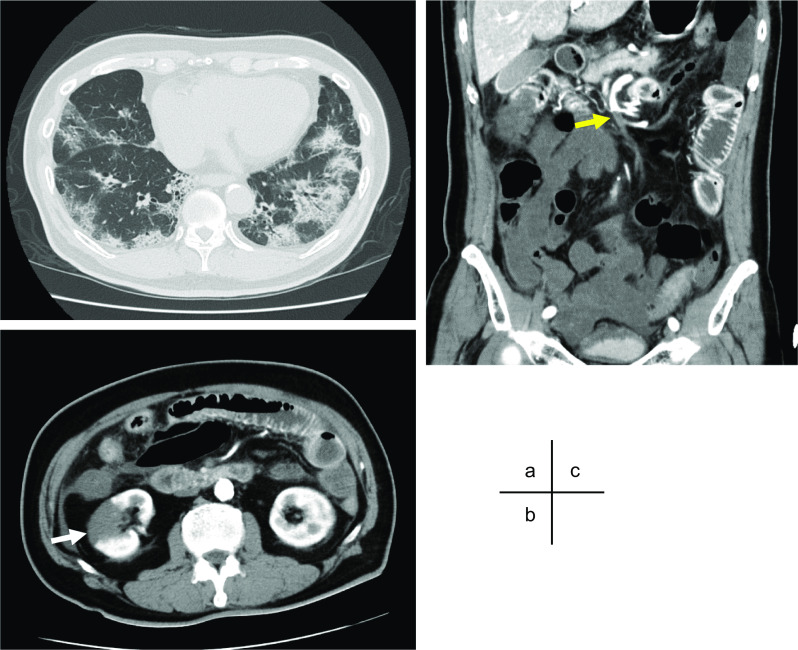
Contrast computed tomography (CT). Contrast CT revealed ground glass opacification with distribution suggestive of COVID-19 pneumonia (a), right renal infarction (b, white arrow), and superior mesenteric artery occlusion (yellow arrow) with intestinal ischemia suggesting extensive necrosis from the jejunum to the transverse colon (c)
He was extubated the next day of the surgery and out of intensive care unit on postoperative day 2. The jejunostomy and transverse colon mucous fistula had revealed favorable color with no signs of necrosis. After surgery, the patient was continued on heparinization, and then transitioned to apixaban on postoperative day 11. We performed second surgery to close the jejunostomy and transverse colon mucous fistula with end-to-end anastomosis on postoperative day 22. The postoperative course was uneventful and he required no nutritional treatment despite having only 100 cm small bowel. He moved to another hospital for rehabilitation to improve activities of daily living (ADLs) on postoperative day 45. As of 6 months after the surgery, his ADLs have completely improved and he has returned to social life without any intravenous nutritional supports for short bowel syndrome.
Discussion
SARS-CoV-2 infection and its disease, COVID-19, have spread rapidly and led the pandemic around the world. COVID-19 has been known a respiratory disease, mainly pneumonia, but also it causes a variety of organ damage [10]. It has been reported worldwide that COVID-19 causes abnormal coagulation from a systemic inflammatory immune response and induces thrombosis-related complications, which is mostly venous thrombosis [5, 6]. Arterial occlusion is less common complication of this disease, but it can involve fatal prognosis [3, 5]. In our literature review on PubMed, total 17 cases (including our case) of SMA occlusion in COVID-19 have been reported from over the world (Table 1) [3, 7, 9–22]. Out of the 14 cases with a description about detailed prognosis in the papers, 5 had died in hospital.
Table 1.
Literature review: summary of the case reports of SMA thrombosis with COVID-19 infection
| Case no. | Authors | Year | Country | Age | Sex | Medical history | Preventive anti-thrombotic therapy | Treatment | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Amaravathi et al. | 2020 | India | 45 | M | None | Missing | Thrombectomy and laparotomy | Unknown |
| 2 | Azouz et al. | 2020 | France | 56 | M | Missing | Missing | Endovascular thrombectomy/laparotomy | Unknown |
| 3 | Bannazadeh et al. | 2020 | USA | 55 | M | HT, hyperthyroidism | Heparin | Laparotomy | Alive |
| 4 | Barry et al. | 2020 | France | 79 | F | None | None | Thrombectomy and laparotomy | Dead |
| 5 | Beccara et al. | 2020 | Italy | 52 | M | Missing | Heparin | Thrombectomy and laparotomy | Alive |
| 6 | Cheung et al. | 2020 | USA | 55 | M | HT | Missing | Thrombectomy and laparotomy | Alive |
| 7 | Karna et al. | 2020 | India | 61 | F | DM, HT | Enoxaparin | Laparotomy | Dead |
| 8 | Krothapalli et al. | 2020 | USA | 76 | F | Af, CAD, DM, HF, HT | Apixaban | Conservative management | Dead |
| 9 | Ucpinar et al. | 2020 | Turkey | 82 | F | Af, CKD, HT | Enoxaparin | Conservative management | Dead |
| 10 | Vulliamy et al. | 2020 | UK | 75 | M | None | None | Thrombectomy and laparotomy | Unknown |
| 11 | Balani et al. | 2021 | India | 37 | M | None | None | Thrombolysis and thrombectomy | Alive |
| 12 | Chaubal et al. | 2021 | India | 9 | M | Missing | Missing | Laparotomy | Alive |
| 13 | Dinoto et al. | 2021 | Italy | 84 | F | CKD, DM, HT | Aspirin | Endovascular thrombectomy | Dead |
| 14 | Hanif et al. | 2021 | Pakistan | 20 | F | None | None | Laparotomy | Alive |
| 15 | Mahrugi et al. | 2021 | Oman | 51 | M | Missing | Missing | Thrombectomy and laparotomy | Alive |
| 16 | Mitchell et al. | 2021 | USA | 69 | M | Missing | None | Thrombectomy and laparotomy | Alive |
| 17 | Current case | 2021 | Japan | 71 | M | Af, DM, HT | Dabigatran + aspirin | Laparotomy | Alive |
SMA superior mesenteric artery, USA United States of America, UK United Kingdom, Af atrial fibrillation, CAD coronary artery disease, CKD chronic kidney disease, DM diabetes mellitus, HF heart failure, HT hypertension
This present case is a first report from East Asia about acute SMA occlusion associated with COVID-19 pneumonia. This is presumably because the distribution of COVID-19 epidemics varies among regions in the world, and the situation of the pandemic revealed relatively stable in East Asia, including Japan, compared to other regions. It suggests that if patients with COVID-19 will increase from the current level, it will be necessary to pay attention to this lethal complication even in areas where the pandemic situation has been currently stable.
Acute mesenteric arterial occlusion most commonly results from thrombosis based on atherosclerotic disease, or embolism where the embolus originates from the left atrium as a consequence of atrial fibrillation [23, 24]. Interestingly, in our literature review, SMA occlusion also occurred in COVID-19 patients who had no risk factors for thromboembolic diseases, which is consistent with previous review [25]. The mechanisms of arterial occlusion in patients with COVID-19 are still unclear. Emerging evidence suggests that COVID-19 is associated with (1) endotheliitis by diffuse endothelial damage and infiltration of inflammatory cells, and (2) a systemic hypercoagulable state caused by hyperinflammation and hypercytokinemia [25–27]. These factors of COVID-19 patients can provide a plausible explanation for the mechanisms of arterial occlusion; highlighting the impact of COVID-19 infection on both thrombosis and embolism. Further fundamental researches to elucidate the mechanism are essential to establish anticoagulation/antiplatelet therapy for preventing this lethal complication.
In our case, due to his medical history of atrial fibrillation, he had been managed with dabigatran since before the thromboembolic complication developed. However, he had multi-site thromboembolism, SMA occlusion and renal infarction. In our literature review, 3 out of 12 patients with a detailed description of their medical history had atrial fibrillation (Table 1). Recently, anticoagulation therapy with heparin and low molecular weight heparin has been reported to be useful for prevention of thrombotic complication with COVID-19 infection [28]. Importantly, despite 7 patients (6 of them had high risk factors for thromboembolic diseases such as atrial fibrillation, diabetes mellitus, hypertension, and dyslipidemia) were maintained with preventive anticoagulation therapy by heparin/low molecular weight heparin or direct oral anticoagulants, they developed SMA occlusion. These results suggest that COVID-19 patients with thromboembolic risk factors are categorized as a high-risk subgroup for SMA occlusion, and stronger anticoagulation, possibly including antiplatelet therapies, may be necessary for those patients, as in our case. In order to establish the preventive strategies for arterial occlusion in COVID-19, further clinical/basic studies using large patient cohorts are required.
From a viewpoint of infection prevention, in patients with COVID-19, even to perform usual clinical examinations and tests, more human and medical resources are required. This severe medical situation may cause exhaustion of medical staffs and inhibit cooperation between infectious disease specialists and abdominal specialists. In this case, it took about 24 h from the onset of abdominal pain to the diagnosis as SMA occlusion. In case that acute onset of severe abdominal pain occurs in patient with COVID-19, physicians should consider the possibility of SMA thrombosis and examine the patient by contrast CT immediately. Furthermore, it is important to collaborate between infectious disease and abdominal specialists to save their lives from this lethal disease.
Necrotic bowel resection is essential for saving lives in most cases of SMA occlusion. In our literature review, 13 cases underwent laparotomy with necrotic bowel resection. It had described the detail of surgical procedures in 9 cased, 4 out of 9 patients were reconstructed with primary anastomosis, and another 5 were constructed intestinal stomas. There were no reports that cases underwent second surgery for intestinal stoma closure. In our case, since the patient's general condition including respiratory function was stable after first surgery, we performed jejuno-transverse colon anastomosis on postoperative day 22. As a result, it was possible to discharge the patient on independent ADLs without intestinal stomas. The decision of whether to perform primary or secondary anastomosis and the optimal timing of secondary anastomosis should be determined, based on the intestinal and general condition, as well as the severity of COVID-19 pneumonia.
Conclusions
We have reported a first case of SMA occlusion in a patient with COVID-19 pneumonia in East Asia. Intensive treatment including surgical procedures allowed the patient to return to social life with completely independent ADLs. Although treatment for COVID-19 involves many challenges, including securing medical resources and controlling the spread of infection, when severe abdominal pain occurs in patients with COVID-19, physicians should consider SMA occlusion and treat promptly for life-saving from this deadly combination.
Acknowledgements
None.
Abbreviations
- COVID-19
Coronavirus disease 19
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- CT
Computed tomography
- SMA
Superior mesenteric artery
- ADLs
Activities of daily living
Authors' contributions
MS and SN wrote the manuscript and performed a literature search. MS reviewed and edited the manuscript. SN, MS, TT, HK, FK, KN, MN, and MS treated and observed the patient. All authors read and approved the final manuscript and agreed to be accountable for all aspects of the work.
Funding
None.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from the patient to publish this case report.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Masahiro Sukegawa, Email: msukegawa@naramed-u.ac.jp.
Satoshi Nishiwada, Email: s-nishiwada@naramed-u.ac.jp.
Taichi Terai, Email: t-taichi@naramed-u.ac.jp.
Hiroyuki Kuge, Email: kuge@naramed-u.ac.jp.
Fumikazu Koyama, Email: fkoyama@naramed-u.ac.jp.
Kenji Nakagawa, Email: k-nakagawa@naramed-u.ac.jp.
Minako Nagai, Email: 34nm@naramed-u.ac.jp.
Masayuki Sho, Email: m-sho@naramed-u.ac.jp.
References
- 1.Coronavirus disease (COVID-19) Pandemic. Geneva: World Health Organization. 2021. https://covid19.who.int. Accessed 13 Aug 2021.
- 2.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amaravathi U, Balamurugan N, Muthu Pillai V, Ayyan SM. Superior mesenteric arterial and venous thrombosis in COVID-19. J Emerg Med. 2021;60(5):e103–e107. doi: 10.1016/j.jemermed.2020.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(23):2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beccara LA, Pacioni C, Ponton S, Francavilla S, Cuzzoli A. Arterial mesenteric thrombosis as a complication of SARS-CoV-2 infection. Eur J Case Rep Intern Med. 2020;7(5):001690. doi: 10.12890/2020_001690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yasuhara H. Acute mesenteric ischemia: the challenge of gastroenterology. Surg Today. 2005;35(3):185–195. doi: 10.1007/s00595-004-2924-0. [DOI] [PubMed] [Google Scholar]
- 9.Balani P, Bhuiyan AS, Dalal VN, Maheshwari GS. Early detection and successful management of acute mesenteric ischaemia in symptomatic COVID-19 patient. Indian J Surg. 2021 doi: 10.1007/s12262-021-02839-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung S, Quiwa JC, Pillai A, Onwu C, Tharayil ZJ, Gupta R. Superior mesenteric artery thrombosis and acute intestinal ischemia as a consequence of COVID-19 infection. Am J Case Rep. 2020;21:e925753. doi: 10.12659/AJCR.925753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al Mahruqi G, Stephen E, Abdelhedy I, Al Wahaibi K. Our early experience with mesenteric ischemia in COVID-19 positive patients. Ann Vasc Surg. 2021;73:129–132. doi: 10.1016/j.avsg.2021.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azouz E, Yang S, Monnier-Cholley L, Arrive L. Systemic arterial thrombosis and acute mesenteric ischemia in a patient with COVID-19. Intensive Care Med. 2020;46(7):1464–1465. doi: 10.1007/s00134-020-06079-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bannazadeh M, Tassiopoulos A, Koullias G. Acute superior mesenteric artery thrombosis seven days after discharge for novel coronavirus pneumonia. J Vasc Surg Cases Innov Tech. 2021;7(3):586–588. doi: 10.1016/j.jvscit.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chaubal G, Hatimi H, Nanavati A, Deshpande A, Andankar P, Biradar V, et al. Pediatric living donor intestine transplant following an atypical complication of COVID-19: a unique case report from India. Am J Transplant. 2021 doi: 10.1111/ajt.16798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Barry O, Mekki A, Diffre C, Seror M, El Hajjam M, Carlier RY. Arterial and venous abdominal thrombosis in a 79-year-old woman with COVID-19 pneumonia. Radiol Case Rep. 2020;15(7):1054–1057. doi: 10.1016/j.radcr.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dinoto E, Ferlito F, La Marca MA, Mirabella D, Bajardi G, Pecoraro F. Staged acute mesenteric and peripheral ischemia treatment in COVID-19 patient: case report. Int J Surg Case Rep. 2021;84:106105. doi: 10.1016/j.ijscr.2021.106105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanif M, Ahmad Z, Khan AW, Naz S, Sundas F. COVID-19-induced mesenteric thrombosis. Cureus. 2021;13(1):e12953. doi: 10.7759/cureus.12953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karna ST, Panda R, Maurya AP, Kumari S. Superior mesenteric artery thrombosis in COVID-19 pneumonia: an underestimated diagnosis-first case report in Asia. Indian J Surg. 2020 doi: 10.1007/s12262-020-02638-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krothapalli N, Jacob J. A rare case of acute mesenteric ischemia in the setting of COVID-19 infection. Cureus. 2021;13(3):e14174. doi: 10.7759/cureus.14174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell JM, Rakheja D, Gopal P. SARS-CoV-2-related hypercoagulable state leading to ischemic enteritis secondary to superior mesenteric artery thrombosis. Clin Gastroenterol Hepatol. 2021;19(11):e111. doi: 10.1016/j.cgh.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ucpinar BA, Sahin C. Superior mesenteric artery thrombosis in a patient with COVID-19: a unique presentation. J Coll Physicians Surg Pak. 2020;30(10):112–114. doi: 10.29271/jcpsp.2020.supp2.112. [DOI] [PubMed] [Google Scholar]
- 22.Vulliamy P, Jacob S, Davenport RA. Acute aorto-iliac and mesenteric arterial thromboses as presenting features of COVID-19. Br J Haematol. 2020;189(6):1053–1054. doi: 10.1111/bjh.16760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chou EL, Wang LJ, McLellan RM, Feldman ZM, Latz CA, LaMuraglia GM, et al. Evolution in the presentation, treatment, and outcomes of patients with acute mesenteric ischemia. Ann Vasc Surg. 2021;74:53–62. doi: 10.1016/j.avsg.2021.01.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Florim S, Almeida A, Rocha D, Portugal P. Acute mesenteric ischaemia: a pictorial review. Insights Imaging. 2018;9(5):673–682. doi: 10.1007/s13244-018-0641-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheruiyot I, Kipkorir V, Ngure B, Misiani M, Munguti J, Ogeng'o J. Arterial thrombosis in coronavirus disease 2019 patients: a rapid systematic review. Ann Vasc Surg. 2021;70:273–281. doi: 10.1016/j.avsg.2020.08.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20(6):355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020;58(7):1021–1028. doi: 10.1515/cclm-2020-0369. [DOI] [PubMed] [Google Scholar]
- 28.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


