Abstract
Objective
This multicenter study investigated clinical risk factors associated with the number of long-term symptoms after COVID.
Methods
Clinical features, symptoms at hospital admission, hospitalization data, and the number of symptoms after COVID was systematically assessed for patients who recovered from COVID-19 in 4 hospitals in Madrid (Spain) from February 20 to May 31, 2020.
Results
Overall, 1,969 patients (46.5% women, age: 61, SD: 16 years) were randomly assessed 8.4 months (SD 1.5) after hospital discharge. Female gender (odds ratio [OR] 1.82, 95% confidence interval [CI] 1.57-2.10), number of morbidities (OR 1.182, 95% CI 1.08-1.29), number of symptoms at hospital admission (OR 1.309, 95% CI 1.15-1.49) and days at the hospital (OR 1.01, 95% CI 1.007-1.017) were associated (all, p <0.001) with more long-term symptoms after COVID. Further, vomiting (OR 1.78, 95% CI 1.26-2.52), throat pain (OR 1.36, 95% CI 1.02-1.81), diarrhea (OR 1.51, 95% CI 1.25-1.82), dyspnea (OR 1.20, 95% CI 1.01-1.41), or headache (OR 1.50, 95% CI 1.28-1.75) as symptoms at hospital admission were also associated (all, p <0.01) with a higher number of symptoms after COVID.
Conclusion
This multicenter study found that a higher number of symptoms at hospital admission were the most relevant risk factor for developing more symptoms after COVID, supporting the assumption that a higher symptom load at the acute phase is associated with a greater likelihood of long-term symptoms after COVID.
Keywords: COVID-19, persistent, symptoms, risk factors, acute phase
Introduction
The presence of symptoms after COVID range from 35% to 60% (Fernández-de-las-Peñas et al., 2021). Identification of risk factors is needed for early monitoring of individuals at a high risk of developing symptoms after COVID, yet present data are still limited (Iqbal et al., 2021). Potential identified risk factors described in former literature include female gender, more onset symptoms (higher symptom load), older age, longer hospital stay, and a higher number of co-morbidities (Yong et al., 2021). Nevertheless, contradictory results are also observed between studies. Further, most of the studies included samples of <300 patients and were recruited from single centers (Iqbal et al., 2021). A study including a large number of COVID-19 patients reported a prevalence of long-term sick leave from work of 5.8% (Jacobs et al., 2021). These authors found that female gender, older age, and co-morbid medical conditions were significantly associated with long-term sick leave (Jacobs et al., 2021). We describe here a large multicenter study investigating clinical risk factors related to hospitalization associated with the number of long-term symptoms after COVID in a large population sample.
Methods
The LONG-COVID-EXP-CM is a multicenter cohort study including individuals hospitalized with a diagnosis of SARS-CoV-2 during the first wave of the pandemic in 5 public hospitals in Madrid (Spain). A sample of 400 individuals from each hospital was randomly selected. All Local Ethics Committees approved the study (HCSC20/495E, HSO25112020, HUFA 20/126, HUIL/092-20, HUF/EC1517). Informed consent was obtained from all participants. Participants were scheduled for a telephone interview conducted by experienced healthcare professionals, were systematically asked about a list of symptoms after COVID (multiple symptoms could be selected by the same patient), but were free to report any additional symptom that they experienced at the time of the study. Clinical data (i.e., gender, age, height, weight, co-morbidities), COVID-19 symptoms at hospital admission, and hospitalization (i.e., days at hospital, intensive care unit admission) data were collected from medical records.
Mean and SD or percentages were calculated. Missing values were imputed using median imputation. Multivariate logistic regressions were conducted to analyze associations between clinical and hospitalization variables with the number of symptoms after COVID (dependent variable) using Python library statsmodels 0.11.1. Adjusted odds ratio (OR) and confidence intervals (95% CI) were calculated.
Results
From 2,000 patients randomly selected and invited to participate, a total of 1,969 (46.5% women, age: 61, SD: 16 years) participated. The most prevalent symptoms at hospital admission were fever (74.6%), dyspnea (31.5%), and myalgia (30.7%). Almost 57.5% of the individuals (n = 1,133) reported at least one co-morbidity. Participants were assessed 8.4 months (SD 1.5) after hospital discharge. Almost 1 out of 5 patients (n = 367, 18.7%) were free of symptoms after COVID, whereas 34.4% (n = 679) experienced ≥3 symptoms after COVID. The mean number of symptoms after COVID was 1.9 (SD 1.4). The most frequent long-term symptoms after COVID included fatigue (61.3%) and dyspnea (23.3%).
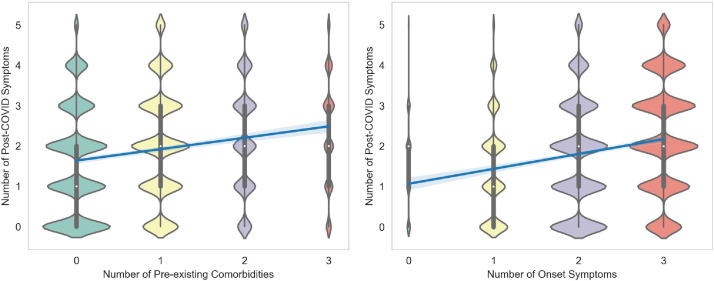
Female gender (OR 1.82, 95% CI 1.57-2.10), number of COVID-19 symptoms at hospital admission (OR 1.309, 95% CI 1.15-1.49), number of pre-existing medical co-morbidities (OR 1.182, 95% CI 1.08-1.29), and days at hospital (OR 1.01, 95% CI 1.007-1.017) were independently associated (all, p <0.001) with more long-term symptoms after COVID: the higher the number of COVID-19 onset symptoms or the higher the number of co-morbidities, the higher the number of symptoms after COVID (Figure ). No specific co-morbidity (e.g., obesity, hypertension) was associated with a greater number of symptoms after COVID. Some specific symptoms at the acute phase were also independently associated (all, p <0.01) with a higher number of long-term symptoms after COVID (Table ): vomiting (OR 1.78, 95% CI 1.26-2.52), throat pain (OR 1.36, 95% CI 1.02-1.81), diarrhea (OR 1.51, 95% CI 1.25-1.82), dyspnea (OR 1.20, 95% CI 1.01-1.41), or headache (OR 1.50, 95% CI 1.28-1.75).
Figure.
Positive associations between the number of long-term symptoms after COVID with the number of pre-existing co-morbidities (left) or the number of COVID-19 onset symptoms at hospital admission
Table.
Clinical/Hospitalization Data and Symptoms after COVID (n = 1,969)
| Age, mean (SD), years | 61 (16) |
| Gender, male/female (%) | 1,054 (53.5%) / 915 (46.5%) |
| Weight, mean (SD), kg. | 75 (15) |
| Height, mean (SD), cm. | 165 (16.5) |
| Main Symptoms at hospital admission, n (%)FeverDyspnoeaMyalgiaCoughHeadacheDiarrheaAnosmiaThroat PainAgeusiaVomiting | 1,469 (74.6%)620 (31.5%)604 (30.7%)549 (27.9%)332 (16.9%)210 (10.7%)167 (8.5%)102 (5.2%)66 (33.5%)55 (2.8%) |
| Number of medical co-morbidities, n (%)NoneOneTwo3 or more | 836 (42.5%)715 (36.3%)281 (14.2%)137 (7%) |
| Medical co-morbiditiesHypertensionDiabetesCardiovascular DiseaseAsmaObesityChronic Obstructive Pulmonary DiseaseStrokeRheumatological DiseaseOther (Cancer, Kidney Disease) | 514 (26.1%)236 (12.0%)234 (11.9%)126 (6.4%)88 (4.5%)77 (3.9%)38 (2.0%)31 (1.6%)332 (16.9%) |
| Stay at the hospital, mean (SD), days | 11.3 (11.4) |
| Intensive Care Unit (ICU) admissionYes/No, n (%) | 130 (6.6%) / 1,839 (93.4%) |
| Number of long-term symptoms after COVID, n (%)NoneOneTwo3 or more | 367 (18.7%)436 (22.1%)488 (24.8%)679 (34.4%) |
| Long-Term symptoms after COVID, n (%)FatigueDyspnoeaLoss memorySkin RashesBrain fogAttention DisordersPalpitationsGastrointestinal DisordersOcular/Vision DisordersAnosmiaAgeusiaThroat PainDiarrheaVoice Problems | 1,206 (61.3%)459 (23.3%)341 (17.3%)236 (12.0%)189 (9.5%)140 (7.1%)140 (7.1%)133 (6.7%)116 (5.9%)80 (4%)53 (2.7%)50 (2.55%)49 (2.5%)39 (2%) |
| COVID-19 Onset Symptom at Hospital Admission | Number Long-term Symptoms after COVID |
| *Dyspnoea (n=620)No Dyspnoea (n=1,349) | 2.1 (SD 1.3)1.8 (SD 1.4) |
| *Headache (n=332)No Headache (n=1,637) | 2.2 (SD 1.4)1.8 (SD 1.3) |
| *Diarrhea (n=210)No Diarrhea (n=1,759) | 2.25 (SD 1.4)1.8 (SD 1.4) |
| *Throat Pain (n=102)No Throat Pain (n=1,867) | 2.35 (SD 1.4)1.85 (SD 1.4) |
| *Vomiting (n=55)No Vomiting (n=1,914) | 2.5 (SD 1.4)1.85 (SD 1.3) |
Significant association in the multivariate analysis
Discussion
This multicenter study found that female gender, a greater number of symptoms at hospital admission, a greater number of pre-existing medical co-morbidities, and a longer stay at the hospital were risk factors for developing more long-term symptoms after COVID. In all these risk factors, it seems that a higher number of symptoms at hospital admission was the most relevant for developing more symptoms after COVID. The presence of some specific symptoms at hospital admission such as vomiting, throat pain, diarrhea, dyspnea, or headache was also associated with long-term symptoms after COVID. No specific medical co-morbidity was associated with a greater number of long-term symptoms after COVID. Our data support previous assumptions that a higher symptom load at the acute phase is associated with a greater likelihood of long-term symptoms after COVID (Iqbal et al., 2021; Yong, 2021). The role of previous medical co-morbidities as a risk factor for symptoms after COVID needs further studies. We also observed that the female gender was a potential risk factor for symptoms after COVID, in agreement with previous assumptions (Iqbal et al., 2021). Specific studies investigating gender differences are needed.
Our results should be considered according to some potential weaknesses. First of all, only hospitalized patients participated. Second, we did not collect objective data on COVID-19 disease. Third, the cross-sectional design did not permit the determination of cause-and-effect associations.
Author Contributions
Dr Fernández-de-las-Peñas and Dr. Palacios-Ceña had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: All authors. Drafting of the manuscript: All authors. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Dr. Pellicer-Valero. Supervision: Dr. Martín-Guerrero
Declaration of interests
No conflict of interest is declared by any of the authors
Acknowledgments
We want to acknowledge all participants with COVID-19 of this study for their attention
Role of the Funding Source
. The LONG-COVID-EXP-CM is supported by a grant of Comunidad de Madrid y la Unión Europea, a través del Fondo Europeo de Desarrollo Regional (FEDER), Recursos REACT-UE del Programa Operativo de Madrid 2014-2020, financiado como parte de la respuesta de la Unión a la pandemia de COVID-19. The sponsor had no role in the design, collection, management, analysis, or interpretation of the data, draft, review, or approval of the manuscript, or its content. The authors were responsible for the decision to submit the manuscript for publication, and the sponsor did not participate in this decision.
References
- Fernández-de-las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Florencio LL, Cuadrado ML, Plaza-Manzano G, Navarro-Santana M. Prevalence of Post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur J Int Med. 2021;92:55–70. doi: 10.1016/j.ejim.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal FM, Lam K, Sounderajah V, Clarke JM, Ashrafian H, Darzi A. Characteristics and predictors of acute and chronic post-COVID syndrome: A systematic review and meta-analysis. EClinicalMedicine. 2021;36 doi: 10.1016/j.eclinm.2021.100899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs L, Koyanagi AI, Smith L, Tanislav C, Konrad M, van der Beck S, Kostev K. Prevalence of and factors associated with long-term COVID-19 sick leave in working-age patients followed in general practices in Germany. Int J Infectious Diseases. 2021 doi: 10.1016/j.ijid.2021.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis. 2021 doi: 10.1080/23744235.2021.192439. [DOI] [PMC free article] [PubMed] [Google Scholar]