Abstract
Following the growing evidence that personality is related to various health behaviors, we examined whether personality traits were related to compliance with COVID-19 protective measures and evaluated the extent to which associations were moderated by age, gender, or race/ethnicity among older adults during a summer 2020 surge of COVID-19 cases in the United States. Data were from the 2020 Health and Retirement Study COVID-19 module. Multivariate ordinary least squares regression analyses were computed adjusting for health, psychosocial, and sociodemographic factors. Results indicated the significant associations between personality traits and compliance with COVID-19 measures varied by age, gender, and race/ethnicity. Specifically, the associations of agreeableness with wearing a mask and frequent handwashing were less pronounced among older compared with younger individuals. The association between extraversion and wearing masks was stronger for men than for women. The associations of agreeableness with handwashing and physical distancing were weaker for Hispanic older adults, whereas the associations of extraversion with physical distancing and using sanitizers were stronger for Hispanic older adults than for their non-Hispanic White counterparts. Implications regarding behavioral science underlying the current pandemic and future public health crises are discussed.
Keywords: Age, COVID-19 prevention, Gender, Personality, Race/ethnicity
1. Introduction
Since the start of the COVID-19 pandemic in December 2019, many countries worldwide have implemented preventive measures to limit the transmission of COVID-19 (Campos-Mercade et al., 2021), and people have adapted their lives in many ways. To slow the spread of coronavirus, the pandemic has led to a global public health campaign promoting wearing a mask in public, physical distancing, and handwashing (Van Bavel et al., 2020). A growing body of literature documents that personality, biopsychosocial characteristics, and behavior patterns are reliable predictors of health behaviors (Smith, 2006). Previous research has shown that personality is related to various preventive health behaviors (Milad & Bogg, 2021) and health outcomes (Chapman et al., 2009), as well as well-being and coping (Hudson et al., 2021). For example, researchers established conscientiousness as a predictor of better health outcomes across the life span, whereas neuroticism is a risk factor for worse health (Smith, 2006). Health behaviors during a pandemic may be more driven by fear than diligence, and extraversion and openness may be specifically relevant when social distancing is recommended.1 Neuroticism also emerges as the most relevant predictor of health behaviors concerning anxiety and fear during the COVID-19 pandemic (Nikčević et al., 2021).
Several studies indicated that demographic and socioeconomic factors are related to COVID-19 preventive health behaviors. Specifically, associations of age (Dai et al., 2020), gender (Griffith et al., 2020), and race/ethnicity (Barber & Kim, 2021) with COVID-19 protective measures have been explored. Chapman et al. (2009) suggested that while broad group differences in inflammation between gender and race/ethnicity exist, personality has been identified as a vital source of individual differences in health outcomes within groups. However, few studies thus far have investigated the interactions of these factors in predicting virus-mitigating preventive health behaviors. Building on this, we examined the associations between personality traits and compliance with COVID-19 protective measures among older Americans. Furthermore, we evaluated the extent to which associations were moderated by age, gender, and race/ethnicity using a nationally representative population-based panel data.
1.1. Theoretical background
1.1.1. Personality and health behaviors
Guided by the five-factor model of personality (McCrae & John, 1992; Soto & John, 2017) in predicting health behaviors (Willroth et al., 2021), we posited that particular personality traits might contribute to compliance with COVID-19 protective measures. Whether individuals engage in health behaviors may depend on their personality dispositions. Several studies have linked these traits with desirable or undesirable health behaviors (Marshall et al., 1994). For example, higher neuroticism was related to smoking (Terracciano & Costa, 2004) and alcohol and substance abuse (Turiano et al., 2012). Personality traits have also been associated with medication non-adherence among older adults (Jerant et al., 2011). High levels of conscientiousness and openness and low levels of agreeableness and neuroticism were associated with preferring active patient decision-making styles concerning health outcomes (Flynn & Smith, 2007). Furthermore, there is evidence of mediation, indicating that traits like conscientiousness predict health behaviors which in turn influence physical health and mortality (Bogg & Roberts, 2004; Smith, 2006). Although the evidence linking personality with health behaviors appears strongest for conscientiousness, the role of other personality traits during a pandemic has remained unclear. Typically, all five traits are included in studies linking personality with health-promoting behaviors. Regarding the COVID-19 pandemic, recent studies leveraged long-standing theories of personality in predicting health behaviors (Willroth et al., 2021). Conscientiousness, agreeableness, and openness have been identified as important predictors of behavioral responses to the COVID-19 pandemic and engagement in preventive health behaviors (Aschwanden et al., 2021; Milad & Bogg, 2021; Willroth et al., 2021). More specifically, Milad and Bogg (2021) indicated a positive relationship between higher openness and more frequent mask wearing. Willroth et al. (2021) found that higher agreeableness was associated with greater compliance with COVID-19 measures. Aschwanden et al. (2021) demonstrated that higher neuroticism was associated with more concerns but was not related to face masking. These earlier studies included all five personality traits.
This study replicates and extends previous research by examining whether personality traits were related to compliance with COVID-19 protective measures and, further, evaluated the extent to which associations were moderated by age, gender, and race/ethnicity among older adults during a summer 2020 surge of COVID-19 cases in the United States.
1.2. Factors associated with preventive health behaviors
Sociodemographic, health, and psychosocial factors have been shown to be important predictors of engagement in preventive health behaviors. Researchers found mixed results on the association between age and preventive health behaviors, including mask wearing, frequent handwashing, keeping distance, and using sanitizers. Some researchers concluded that older people reported more intention of complying with preventive health behaviors (Dai et al., 2020). On the other hand, contrary findings demonstrated that engagement in preventive behaviors declined with advancing age (Barber & Kim, 2021). Most studies reported that women intended to comply more with preventive behaviors than men (Barber & Kim, 2021; Dai et al., 2020). Racial differences were found in adopting preventive behaviors during COVID-19 (Breakwell et al., 2021). Also, Breakwell et al. (2021) found that race/ethnicity directly affected preventive behaviors and indirectly affected them through political trust, ingroup power, COVID-19 risk, and trust in science. Black, Asian, and minority ethnic groups were more likely to adopt preventive behaviors than the White British group (Breakwell et al., 2021).
As Chapman et al. (2009) suggested, age, gender, and race/ethnicity, along with individual differences in personality, have been critical sources of variation in both biological and psychosocial attributes. Older persons, women, and racial/ethnic minorities may be more cautious about recommended COVID-19 protective measures and health practices because they have been far more likely to experience severe health consequences (Dai et al., 2020). This may stand in contrast to other research indicating that the link between conscientiousness and health behaviors is greater among younger than older adults (Bogg & Roberts, 2004). However, the health behaviors typically studied are alcohol use, drug use, or unhealthy eating. These behaviors may be more relevant for younger adults, whereas poor health behaviors may be more relevant for older adults. Thus, it is important to further evaluate the extent to which associations were moderated by age, gender, and race/ethnicity.
1.3. Hypotheses
Based on prior empirical and theoretical studies, we predicted that personality traits would be related to engagement in COVID-19 protective measures, including mask wearing, frequent handwashing, keeping distance, and using sanitizers. We hypothesized that those with higher levels of emotional stability (i.e., the opposite of neuroticism), extraversion, openness, agreeableness, and conscientiousness would be more likely to comply with COVID-19 protective measures among U.S. older adults. We hypothesized that age would moderate these associations between these personality traits and compliance with COVID-19 protective measures, such that these associations would be stronger for the older age group than the relatively younger age group. Also gender would moderate these associations, such that these associations would be stronger for older women than their men counterparts. Finally, we hypothesized that race/ethnicity would moderate these associations, such that these associations would be stronger for older racial/ethnic minorities than their non-Hispanic White counterparts. In addition to personality traits, we explored the relations of health (self-rated memory, COVID-19 diagnosis, self-rated health, comorbidity, and depressive symptoms), psychosocial (religious beliefs and social support), and sociodemographic factors (marital status, years of education, employment status, the number of living children and siblings, and log of total household income and wealth) to compliance with COVID-19 protective measures.
2. Material and methods
2.1. Data and sample
This study used data from the HRS, a nationally representative longitudinal panel survey of Americans aged 51 and older conducted biennially. Participants were drawn from the 2020 HRS COVID-19 module. Beginning June 2020, a COVID-19 module was administered to a 50% random sample of the HRS. More details are described in Health and Retirement Study (2020).
To investigate compliance with COVID-19 protective measures among older adults, of 3266 respondents, we excluded 54 respondents under 50 years old, so the potential sample for the present study became 3212 respondents. The analyses were limited to those who completed the HRS Leave-Behind Questionnaire (LBQ), which contained questions on personality traits. We excluded those who did not participate in the LBQ from the analyses. The final analytic sample had 1006 respondents. All participants provided informed consent with study approval from the University of Michigan Institutional Review Board. The sample characteristics are presented in Supplementary Table 1.
2.2. Measurements
2.2.1. Compliance with COVID-19 protective measures
Four types of COVID-19 protective measures were assessed with the questions, “Since the coronavirus pandemic, have you (a) worn a mask around other people outside your home (e.g., in shops)?; (b) washed your hands with soap more frequently?; (c) kept a distance from others when you went outside your home?; and (d) used special hand sanitizers or disinfectants?” We reverse-coded and higher scores represented more frequent engagement in preventive health behaviors (1 = never; 2 = sometimes; 3 = always).
2.2.2. Personality traits
Participants completed the Midlife Development Inventory (MIDI) Personality Scale (Lachman & Weaver, 1997) as part of the LBQ. The Big Five personality traits were assessed with 31 items: (a) neuroticism (α = 0.71), (b) extraversion (α = 0.75), (c) openness to experience (α = 0.80), (d) agreeableness (α = 0.79), and (e) conscientiousness (α = 0.71). Items were rated on a scale from 1 (a lot) to 4 (not at all) and reverse-coded in the direction of the trait label. Each trait's mean was calculated.
2.2.3. Moderators
Potential moderators included age (50–59 (reference); 60–69; 70–79; 80+), gender (men (reference); women), and race/ethnicity (non-Hispanic White (reference); non-Hispanic Black; Hispanic of any race; non-Hispanic other race).
2.2.4. Covariates
We adjusted for health, sociodemographic, and psychosocial factors that may confound the association between personality traits and preventive health behaviors. Details of covariate measures are included in Supplementary material.
2.3. Statistical analysis
Descriptive statistics were computed for all variables. We conducted moderated hierarchical multiple regression analyses to test the associations between personality traits and COVID-19 protective measures and evaluated the extent to which associations were moderated by age, gender, or race/ethnicity. We separately evaluated each two-way interaction term in the fully adjusted models. Supplementary Tables 2 and 3 present the results from hierarchical multiple regression models that included the main effects of personality traits (Model 1), age, gender, and race/ethnicity (Model 2), and each two-way interaction effect (Models 3, 4, and 5).
3. Results
Older Americans who had higher levels of extraversion were significantly less likely to wear masks (β = −0.128, p < .01), whereas those who had higher levels of openness were more likely to wear masks (β = 0.131, p < .001) and keep distancing (β = 0.073, p < .10). Higher agreeableness was significantly associated with greater compliance with COVID-19 protective measures of frequent handwashing (β = 0.130, p < .001) and using hand sanitizers (β = 0.103, p < .01). Higher conscientiousness was significantly associated with greater compliance with COVID-19 protective measures of keeping distancing (β = 0.080, p < .05) and using hand sanitizers (β = 0.097, p < .01).
Compared with adults aged 50–59 years old, individuals aged 60–69 years old were more likely to wash hands frequently (β = 0.093, p < .05) and use sanitizers (β = 0.081, p < .10). Adults aged 70–79 years old (β = 0.082, p < .10) and oldest-old adults (aged 80 and older, β = 0.063, p < .10) were marginally more likely to engage in preventive health measures, particularly wearing a mask than their adults aged 50–59 counterparts. Women were significantly more likely to report taking precautionary protective measures than men. Being a woman was significantly associated with greater compliance with all COVID-19 protective measures of wearing a mask (β = 0.133, p < .001), frequent handwashing (β = 0.119, p < .001), keeping distancing (β = 0.105, p < .01), and using sanitizers (β = 0.137, p < .001) in Model 2. Regarding race/ethnicity, overall, non-Hispanic Black, Hispanic, and non-Hispanic other race older adults were significantly more likely to comply with COVID-19 protective measures than their non-Hispanic White counterparts.
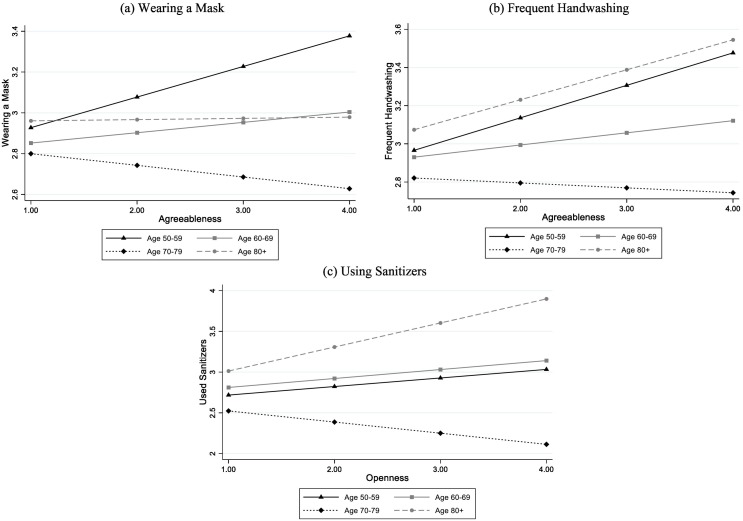
Multiple moderation analyses indicated that the associations between personality traits and compliance with COVID-19 protective measures varied by age group. The associations of agreeableness with wearing a mask and frequent handwashing were less pronounced among individuals aged 70–79 years old than the youngest age group (50–59 years old) (β = −0.125, p < .05; β = −0.128, p < .05, respectively, Model 3 in Supplementary Table 2). As the levels of agreeableness increased, compliance with COVID-19 measures increased among individuals aged 50–59 years old, and the patterns were similar in other age groups (i.e., 60–69 and 80+ groups), however, decreased compliance with COVID-19 measures was observed among individuals aged 70–79 years old. The association between openness and using sanitizers also differed by age groups. As the levels of openness increased, adults aged 50–59 tended to use sanitizers more often, whereas adults aged 70–79 years old were less likely to use sanitizers (β = −0.121, p < .05). Fig. 1 shows the significant interaction effects of age on the associations between personality traits and compliance with COVID-19 protective measures.
Fig. 1.
Moderating effect of age on the association between personality and compliance with COVID-19 protective measures.
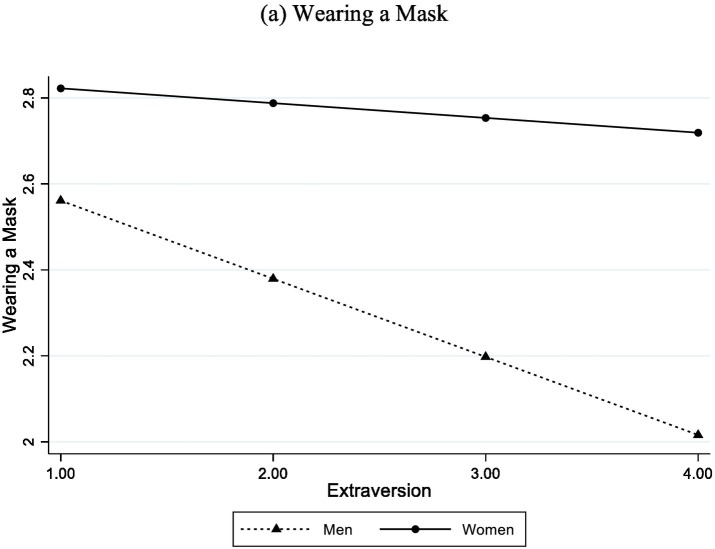
As shown in Fig. 2 , results indicated a significant moderating effect of gender on the association between personality and COVID-19 preventive measures. Specifically, the slope of the association between extraversion and mask wearing was steeper among men than women. That is, older men with high in extraversion were much less likely to wear a mask (a steeper slope), whereas older women showed relatively high engagement in mask wearing regardless of the level of extraversion (a gentler slope) (β = 0.152, p < .05, Model 4 in Supplementary Table 2).
Fig. 2.
Moderating effect of gender on the association between personality and compliance with COVID-19 protective measures.
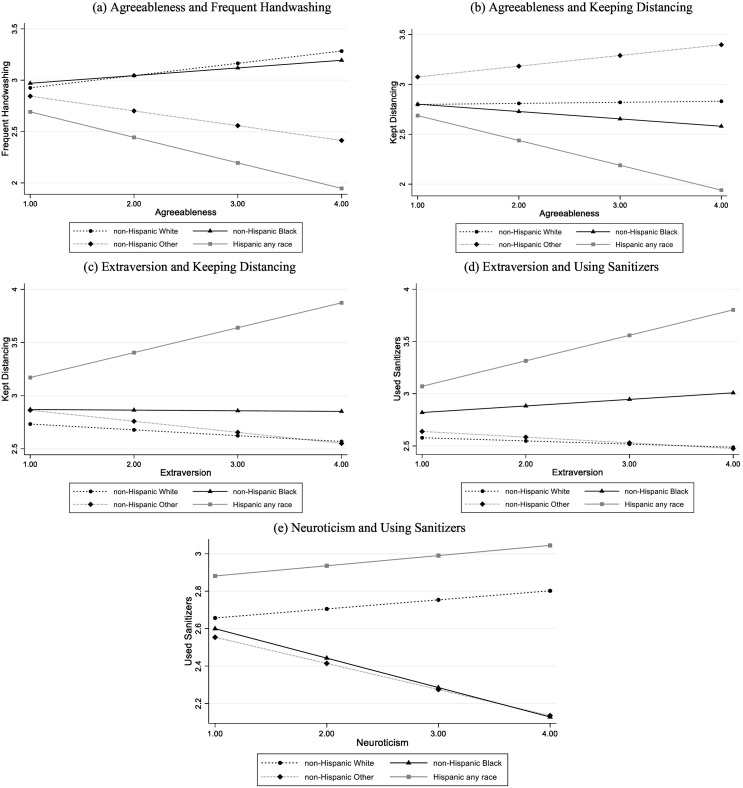
The associations between personality traits and compliance with COVID-19 protective measures also varied by race/ethnicity among U.S. older adults (Model 5 in Supplementary Tables 2 and 3, Fig. 3 ). For example, the associations of agreeableness with handwashing and physical distancing were weaker for Hispanic older adults (β = −0.156, p < .001; β = −0.104, p < .05, respectively), whereas the associations of extraversion with physical distancing and using sanitizers were stronger for Hispanic older adults than for their non-Hispanic White counterparts (β = 0.131, p < .01; β = 0.093, p < .05, respectively). As the levels of neuroticism increased, non-Hispanic White older adults tended to use sanitizers, whereas non-Hispanic Black older adults were less likely to use sanitizers (β = −0.090, p < .05).
Fig. 3.
Moderating effect of race/ethnicity on the association between personality and compliance with COVID-19 protective measures.
The associations of health, psychosocial, and sociodemographic characteristics with COVID-19 protective measures also warrant brief comments and the results were detailed in Supplementary material.
4. Discussion
This study demonstrates the importance of personality traits which are related to preventive health behaviors through their relationships to compliance with COVID-19 protective measures in a nationally representative sample of U.S. older adults. This study supports Willroth et al. (2021)'s approach underscoring the importance of incorporating both the individuals and the circumstances into the health behavior model of personality. Our results confirm recent studies indicating that conscientiousness, agreeableness, and openness to experience are associated with preventive health behaviors during the COVID-19 pandemic (Aschwanden et al., 2021; Milad & Bogg, 2021; Willroth et al., 2021).
However, our findings show that older adults high in extraversion are at higher risk for noncompliance with COVID-19 protective measures, particularly mask wearing. Prior studies have demonstrated that neuroticism predicts greater compliance (Willroth et al., 2021). Neuroticism, however, was not related to compliance with COVID-19 protective measures among U.S. older adults in the sample. Our findings also suggest that openness and extraversion predict virus-mitigating health behaviors within the context of the COVID-19 pandemic. Taken together, our results support the importance of the five-factor model as an important conceptual framework for predicting protective health behaviors during a pandemic.
Our findings indicating differential patterns of associations between personality traits and COVID-19 preventive measures by age, gender, and race/ethnicity are informative about individual personality characteristics in the context of the public health crisis. Three general interaction patterns emerged: age interacting with agreeableness and openness, gender interacting with extraversion, and race/ethnicity interacting with agreeableness, extraversion, and neuroticism.
First, the association between personality and protective health behaviors was moderated by age. The positive association between agreeableness and mask wearing was less pronounced among older (70–79 years old) compared with younger individuals (50–59 years old). Mask wearing is perhaps unfamiliar protective behavior for U.S. older individuals. Schroeter et al. (2021) discussed that mask wearing may impair recognition of emotions and interaction among people despite its justification for disease prevention. It is worse among older adults because they may have experienced some decline in social cognition (Schroeter et al., 2021). But younger and agreeable individuals may be more likely to see the benefits of this health behavior, particularly since they are more likely to be mobile in their community. As Noftle and Fleeson (2010) discussed, late midlife adults are more likely to act agreeably. Thus, public health campaigns, media, and communication may leverage social or peer pressure to comply with COVID-19 protective measures among agreeable late midlife adults who are in the workforce. Some studies also indicate that older adults have not had an adequate supply of and access to face masks and limited knowledge of the efficacy of face masking during the early stage of the COVID-19 pandemic (Kwan et al., 2021).
However, agreeableness was more strongly associated with frequent handwashing and sanitizing for the oldest and youngest age group. Perhaps older individuals see this as a relatively easier preventive measure than wearing masks. The media indicated that particularly oldest-old adults were more at risk, and for agreeable individuals, wearing masks and using sanitizers were simple preventive measures (Mueller et al., 2020).
Only one interaction was obtained with gender as a moderator, suggesting a stronger negative association between extraversion and wearing masks for men. The results may reflect gender roles and stereotypes, indicating that more outgoing men may not want to project any sign of vulnerability. Extraverted women, in contrast, may be more risk averse and may tend to respond to government recommendations for continued health. In general, women reported higher levels of perceived threats and fear of COVID-19 (Niño et al., 2021).
Finally, we obtained a number of ethnic differences moderating the effect of personality on protective health behaviors. The associations of agreeableness with frequent handwashing and keeping distance were less pronounced for Hispanic older adults. It would be expected that agreeable individuals of any age would be more likely to accept protective behaviors (Willroth et al., 2021), but perhaps the trait agreeableness for this subgroup reflects acceptance for the adverse health condition rather than the need for action. More research needs to be conducted to understand this strong negative association among Hispanic older adults, further, explicitly to test whether age and race/ethnicity, particularly Hispanic older adults' residential or work environment, is implicated in compliance with frequent handwashing and keeping distance. Conversely, there were positive associations between extraversion and keeping distance and using sanitizers among Hispanic older adults. It is possible that extraverted Hispanic older adults are more likely to interact with others, recognizing the importance of physical distance and sanitizing to stay healthy. Also, it should be noted that extraverted and neurotic African Americans and Hispanic older adults reported greater concerns about COVID-19 than non-Hispanic Whites (Aschwanden et al., 2021), which may be related to greater compliance with protective measures. Finally, the association between neuroticism and sanitizing was particularly relevant for non-Hispanic other race and non-Hispanic Black older adults, taking less advantage of using sanitizers. This result may be related to various societal factors such as working environment, frequency of using public transportation, cultural difference, easy access to sanitizing products, or disparities in health care and public health education (Lopez et al., 2021).
Taken together, the results suggest that not all demographic groups and not all individuals with specific personality traits react similarly to the pandemic by using the protective measures. Much of these behaviors need to be explained by the interaction of personality with demographic characteristics. Our findings underscore that exploring personality traits may be useful in designing more effective interventions during public health crises. For example, older adults who are high in extraversion and low in openness, agreeableness, and conscientiousness could benefit from personality-tailored interventions for preventive health behaviors. Health practitioners should be aware that older adults with these personality profiles are more difficult to reach when implementing health-promoting behaviors.
Policies and research should identify underlying mechanisms that promote preventive health behaviors during future public health crises for those living in the long-term health consequence of COVID-19. We indicate that men are significantly less likely to comply with COVID-19 protective measures. Our finding highlights the critical need for COVID-19 behavioral change interventions targeted at older men (Barber & Kim, 2021). For instance, health education programs aiming at improving self-protection rather than community-protection (Gandhi et al., 2020), particularly related to mask wearing, may be helpful to build up appropriate practices and reduce the risk of disease prevalence for men who are high in extraversion. The relationships between personality traits and preventive health behaviors are complex and other mechanisms such as health status, disability and its level of severity, access to health care, and types of residential settings, as well as engaging in social support behaviors may also play a part in compliance with COVID-19 protective measures. The associations between those mechanisms and preventive health behaviors are still unexplored. Thus, identifying the mechanisms is warranted in future studies.
Our analyses have several limitations, including the use of data focusing on U.S. older adults during the early COVID-19 pandemic and its correlational design that does not reveal longer-term adaptations and consequences. As the impact of COVID-19 changes over time, future studies are required to understand the consequences of compliance with COVID-19 protective measures. In addition, as socially responsible behavior is critical for slowing the spread of the virus (Campos-Mercade et al., 2021), respondents might over- or under-report their compliance with each COVID-19 protective measure. Also, only three response options were available for the questionnaires of each COVID-19 protective measure. Lastly, due to data restrictions, we were unable to specify the geographical residence of respondents.
Despite these limitations, our findings confirm that personality is associated with compliance with COVID-19 protective measures. Furthermore, we found evidence that age, gender, and race/ethnicity moderate the relationships between personality traits and compliance with COVID-19 protective measures. Our findings provide important evidence for developing intervention programs and promoting older adults' health during a pandemic, as well as for policymakers to prepare plans in case of future public health crises. By evaluating how age, gender, and race/ethnicity interacted with personality traits and compliance with COVID-19 protective measures using a nationally representative sample of older Americans, our findings provide insights into how the five-factor model of personality plays out in the COVID-19 pandemic, giving guidance for public health services to develop personality-tailored programs and policies (Aschwanden et al., 2021; Willroth et al., 2021).
CRediT authorship contribution statement
Shinae L. Choi: Conceptualization, Formal analysis, Methodology, Writing - Original draft preparation, reviewing, revising, and editing.
Peter Martin: Conceptualization, Writing - Original draft preparation, reviewing, revising, and editing.
Jinmyoung Cho: Writing - Original draft preparation, reviewing, revising, and editing.
Yeon Ji Ryou: Writing - Original draft preparation, reviewing, revising, and editing.
Melinda Heinz: Writing - Original draft preparation, reviewing, revising, and editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This study used data from the Health and Retirement Study (HRS), a public use dataset produced and distributed by the University of Michigan with funding from the National Institute on Aging [grant number NIA U01AG009740].
Declaration of competing interest
None.
Footnotes
We thank an anonymous reviewer for this comment.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.paid.2022.111499.
Appendix A. Supplementary data
Supplementary material
References
- Aschwanden D., Strickhouser J.E., Sesker A.A., Lee J.H., Luchetti M., Stephan Y., Sutin A.R., Terracciano A. Psychological and behavioural responses to coronavirus disease 2019: The role of personality. European Journal of Personality. 2021;35(1):51–66. doi: 10.1002/per.2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber S.J., Kim H. COVID-19 worries and behavior changes in older and younger men and women. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2021;76(2):e17–e23. doi: 10.1093/geronb/gbaa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogg T., Roberts B.W. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130(6):887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Breakwell G.M., Fino E., Jaspal R. COVID-19 preventive behaviours in White British and Black, Asian and Minority Ethnic (BAME) people in the UK. Journal of Health Psychology. 2021 doi: 10.1177/13591053211017208. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos-Mercade P., Meier A.N., Schneider F.H., Wengström E. Prosociality predicts health behaviors during the COVID-19 pandemic. Journal of Public Economics. 2021;195 doi: 10.1016/j.jpubeco.2021.104367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman B.P., Khan A., Harper M., Stockman D., Fiscella K., Walton J., Duberstein P., Talbot N., Lyness J.M., Moynihan J. Gender, race/ethnicity, personality, and interleukin-6 in urban primary care patients. Brain, Behavior, and Immunity. 2009;23(5):636–642. doi: 10.1016/j.bbi.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai B., Fu D., Meng G., Liu B., Li Q., Liu X. The effects of governmental and individual predictors on COVID-19 protective behaviors in China: A path analysis model. Public Administration Review. 2020;80(5):797–804. doi: 10.1111/puar.13236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn K.E., Smith M.A. Personality and health care decision-making style. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62(5):P261–P267. doi: 10.1093/geronb/62.5.P261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi M., Beyrer C., Goosby E. Masks do more than protect others during COVID-19: Reducing the inoculum of SARS-CoV-2 to protect the wearer. Journal of General Internal Medicine. 2020;35(10):3063–3066. doi: 10.1007/s11606-020-06067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D.M., Sharma G., Holliday C.S., Enyia O.K., Valliere M., Semlow A.R., Stewart E.C., Blumenthal R.S. Men and COVID-19: A biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Preventing Chronic Disease. 2020;17 doi: 10.5888/pcd17.200247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study . 2020. 2020 HRS COVID-19 Project data description and usage.https://hrsdata.isr.umich.edu/sites/default/files/documentation/data-descriptions/2020COVID_DD_0.pdf [Google Scholar]
- Hudson J., Kuroda Y., Morel P. Personality and motivational predictors of well-being and coping during COVID-19: A reversal theory analysis. Personality and Individual Differences. 2021;175 doi: 10.1016/j.paid.2021.110703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerant A., Chapman B., Duberstein P., Robbins J., Franks P. Personality and medication non-adherence among older adults enrolled in a six-year trial. British Journal of Health Psychology. 2011;16(1):151–169. doi: 10.1348/135910710X524219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan R., Lee P.H., Cheung D., Lam S.C. Face mask wearing behaviors, depressive symptoms, and health beliefs among older people during the COVID-19 pandemic. Frontiers in Medicine. 2021;8 doi: 10.3389/fmed.2021.590936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman M.E., Weaver S.L. 1997. The Midlife Development Inventory (MIDI) Personality Scales: Scale construction and scoring.https://www.brandeis.edu/psychology/lachman/pdfs/midi-personality-scales.pdf Retrieved from. [Google Scholar]
- Lopez L., Hart L.H., Katz M.H. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325(8):719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- Marshall G.N., Wortman C.B., Vickers R.R., Kusulas J.W., Hervig L.K. The five-factor model of personality as a framework for personality-health research. Journal of Personality and Social Psychology. 1994;67(2):278–286. doi: 10.1037/0022-3514.67.2.278. [DOI] [PubMed] [Google Scholar]
- McCrae R.R., John O.P. An introduction to the five-factor model and its applications. Journal of Personality. 1992;60(2):175–215. doi: 10.1111/j.1467-6494.1992.tb00970.x. [DOI] [PubMed] [Google Scholar]
- Milad E., Bogg T. Spring 2020 COVID-19 surge: Prospective relations between demographic factors, personality traits, social cognitions and guideline adherence, mask wearing, and symptoms in a US sample. Annals of Behavioral Medicine. 2021;55(7):665–676. doi: 10.1093/abm/kaab039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller A.L., McNamara M.S., Sinclair D.A. Why does COVID-19 disproportionately affect older people? Aging (Albany NY) 2020;12(10):9959–9981. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikčević A.V., Marino C., Kolubinski D.C., Leach D., Spada M.M. Modelling the contribution of the big five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. Journal of Affective Disorders. 2021;279:578–584. doi: 10.1016/j.jad.2020.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niño M., Harris C., Drawve G., Fitzpatrick K.M. Race and ethnicity, gender, and age on perceived threats and fear of COVID-19: Evidence from two national data sources. SSM - Population Health. 2021;13 doi: 10.1016/j.ssmph.2020.100717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noftle E.E., Fleeson W. Age differences in big five behavior averages and variabilities across the adult life span: Moving beyond retrospective, global summary accounts of personality. Psychology and Aging. 2010;25(1):95–107. doi: 10.1037/a0018199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeter M.L., Kynast J., Villringer A., Baron-Cohen S. Face masks protect from infection but may impair social cognition in older adults and people with dementia. Frontiers in Psychology. 2021;12 doi: 10.3389/fpsyg.2021.640548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T.W. Personality as risk and resilience in physical health. Current Directions in Psychological Science. 2006;15(5):227–231. doi: 10.1111/j.1467-8721.2006.00441.x. [DOI] [Google Scholar]
- Soto C.J., John O.P. Short and extra-short forms of the big five Inventory–2: The BFI-2-S and BFI-2-XS. Journal of Research in Personality. 2017;68:69–81. [Google Scholar]
- Terracciano A., Costa P.T., Jr. Smoking and the five-factor model of personality. Addiction (Abingdon, England) 2004;99(4):472–481. doi: 10.1111/j.1360-0443.2004.00687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano N.A., Whiteman S.D., Hampson S.E., Roberts B.W., Mroczek D.K. Personality and substance use in midlife: Conscientiousness as a moderator and the effects of trait change. Journal of Research in Personality. 2012;46(3):295–305. doi: 10.1016/j.jrp.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Crockett M.J., Crum A.J., Douglas K.M., Druckman J.N. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020;4(5):460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Willroth E.C., Smith A.M., Shallcross A.J., Graham E.K., Mroczek D.K., Ford B.Q. The health behavior model of personality in the context of a public health crisis. Psychosomatic Medicine. 2021;83(4):363–367. doi: 10.1097/PSY.0000000000000937. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material