Abstract
The ongoing novel coronavirus (COVID-19) pandemic has highlighted the need for individuals to have easy access to healthcare facilities for treatment as well as vaccinations. The surge in COVID-19 hospitalizations during 2020 also underscored the fact that accessibility to nearby hospitals for testing, treatment and vaccination sites is crucial for patients with fever or respiratory symptoms. Although necessary, quantifying healthcare access is challenging as it depends on a complex interaction between underlying socioeconomic and physical factors. In this case study, we deployed a Multi Criteria Decision Analysis (MCDA) approach to uncover the barriers and their effect on healthcare access. Using a least cost path (LCP) analysis we quantified the costs associated with healthcare access from each census block group in the Los Angeles metropolitan area (LA Metro) to the nearest hospital. Social vulnerability reported by the Centers for Disease Control and Prevention (CDC), the daily number of COVID-19 cases from the Los Angeles open data portal and built environment characteristics (slope of the street, car ownership, population density distribution, walkability, traffic collision density, and speed limit) were used to quantify overall accessibility index for the entire study area. Our results showed that the census block groups with a social vulnerability index above 0.75 (high vulnerability) had low accessibility owing to the higher cost of access to nearby hospitals. These areas were also coincident with the hotspots for COVID-19 cases and deaths which highlighted the inequitable exposure of socially disadvantaged populations to COVID-19 infections and how the pandemic impacts were exacerbated by the synergistic effect of socioeconomic status and built environment characteristics of the locations where the disadvantaged populations resided. The framework proposed herein could be adapted to geo-target testing/vaccination sites and improve accessibility to healthcare facilities in general and more specifically among the socially vulnerable populations residing in urban areas to reduce their overall health risks during future pandemic outbreaks.
Keywords: CDC, Centers for Disease Control and Prevention; LA, Los Angeles; LADOT, Los Angeles Department of Transportation; LA Metro, Los Angeles Metropolitan Area; LCP, Least Cost Path; MCDA, Multi Criteria Decision Analysis; 2SFCA, Two-step Floating Catchment; SVI, Social Vulnerability Index; WHO, World Health Organization
Keywords: Healthcare accessibility, COVID-19, Least cost path, MCDA, Social vulnerability
1. Introduction
Access to healthcare is a necessity for equitable distribution of amenities in the face of a pandemic such as the 2019 novel coronavirus (COVID-19) (WHO, 2021). Inequitable access to healthcare has been recognized as a strong indicator of discrepancies in the spread of COVID-19 (Berger et al., 2020; Gray et al., 2020; Chin et al., 2020) in the United States (US). Previous research has shown that the skewed access to healthcare facilities between the urban and rural populations in the US (Rosenblatt and Lishner, 1991; Lovett et al., 2002) is due to (i) transportation barrier, a result of limited access to a vehicle and limited network connectivity between population centers and healthcare facilities (such as hospitals), and (ii) uneven distribution of healthcare facilities. The limited access to healthcare facilities tends to pose a critical challenge to regional health planning and interventions (Todd et al., 1991; Wang, 2012).
The COVID-19 pandemic underscored the health disparities in the US (Shadmi et al., 2020), specifically, regarding access to testing sites, hospitals, and potential vaccination sites (Shen et al., 2021). The African Americans, Hispanics, and Native Americans were found to have experienced a disproportionate burden of COVID-19 related infections and deaths (Hooper et al., 2020). These population groups are not only financially disadvantaged but also tend to work in the service industry which prevented them from working from home, thereby increasing their potential exposure to COVID-19. These groups also tend to have underlying health conditions such as obesity, diabetes, and cardiovascular diseases that exacerbated the impacts of COVID-19. Hence, improved access to testing facilities, hospitals, and vaccinations sites is crucial to control the spread of COVID-19 in general and specifically, among these socio-economically vulnerable populations. It is essential for policy and decision-makers to ensure that every community has equitable access to healthcare services (Kang et al., 2020) to control the spread and adverse impacts of COVID-19 among underserved populations.
Access to healthcare facilities can be measured based on several dimensions, such as availability (i.e., adequate healthcare facilities and services), geographic/spatial accessibility (i.e., travel impedance between patients and providers), and accommodation (i.e., number of beds available at a particular hospital - an indicator of the hospitals where patients could be treated if needed during life-threatening situations. Spatial accessibility refers to the ease with which healthcare facilities (e.g hospitals, medical centers etc.) can be reached from a location and/or by an individual irrespective of his/her socio-economic condition(s) (Hansen, 1959; Kwan, 1998, 1999; Luo and Wang, 2003; Kwan and Weber, 2008). Having easy access to healthcare facilities by every individual can reduce the spread and impact of COVID-19 among communities. Thus, accurate and reliable methods for identifying deficiencies in accessibility to health services is essential for local authorities (McGrail and Humphreys, 2009, 2014; Luo and Qi, 2009).
Previous studies have examined the significance of spatial access to primary care (Luo and Wang, 2003; Khan, 1992) in terms of linear distance to physicians, number or size of health care facilities relative to the population centers in need of healthcare as well as the importance of aspatial factors like the Index of Relative Disadvantage (IRD), social factors like ethnic diversity and income levels (Carr-Hill et al., 1994; Field, 2000; Bissonnette et al., 2012), among others. Wang and Luo (Wang and Luo, 2005) integrated spatial and aspatial factors to measure accessibility to healthcare facilities but did not consider the vulnerability of geographic regions (i.e., limited access to transportation networks) and socioeconomic factors that can and do influence access. Previous studies have also identified distance as a major factor that impacts accessibility (Pagano et al., 2007; Exworthy and Peckham, 2006), but the distance does not fully explain accessibility, since the interactions between transportation and mobility also pose barriers to health care. Travel time instead of distance is a better representation of accessibility during an epidemic as individuals can suddenly fall ill and need immediate medical assistance. Essentially, both spatial and aspatial factors influence healthcare access among different demographic groups.
Decision problems, especially those of a spatial nature, such as the spread of infectious diseases like COVID-19, involve a complex interaction of numerous interrelated social, economic, and environmental criteria. Exploring the overarching effect of such combinations of factors on accessibility is a challenge faced by researchers. With the availability of a large volume of data from disparate sources, novel decision analysis approaches can now be applied to understand spatial problems like accessibility. Existing methods like the two-step floating catchment (2SFCA) methods use a top-down approach where predetermined catchment areas are generated to understand accessibility. The 2SFCA method is a form of the gravity model (Luo and Whippo, 2012) and involves service to population ratio within predetermined catchments of the service location.
While determining the percent population served by a specific healthcare facility is crucial, the COVID-19 pandemic underscored the significance of having access to a healthcare facility to receive testing and treatments. However, there is a gap in available methods which combine both geographic and socioeconomic factors to assess healthcare facility accessibility in the face of COVID-19 based on travel time considerations (Rader et al., 2020). Without prior knowledge about the catchments, in this study, we implemented a data-driven Multi-Criteria Decision Analysis (MCDA) approach to examine spatial accessibility of individuals susceptible to COVID-19 spread by considering their socioeconomic conditions and exposure which influence the overall cost of accessing healthcare facilities. We also compared our results with a 2-SFCA method.
MCDA is widely used in decision-making processes to identify the best choice from a set of contradicting alternatives. Primarily, MCDA enables the ranking of alternatives based on a set of decision criteria, which requires the weighting of each criterion based on specific constraints (Jacquet-Lagreze and Yannis, 2001). Several forms of MCDA, such as Analytic Hierarchy Process (AHP) (Saaty, 1990), preference ranking organization method for enrichment evaluations (Oberschmidt et al., 2010), elimination and choice expressing reality (Wang et al., 2009), and Multi-Attribute Utility Theory (Wang et al., 2009) have been developed that account for the impact of criteria selection and weights on final decisions (Brugha, 1998; Cervantes and Lorenz, 2009).
Exploring the conditions that lead to the spread of COVID-19 in urban areas can be challenging as they often manifest local variations arising from spatially heterogeneous interactions (Thomas et al., 2020) of several underlying socioeconomic and built environment factors. Since MCDA allows fragmenting a complex problem into smaller subparts, analysis of each subpart, and their integration into a desirable solution, it has been utilized in several interdisciplinary applications, such as in finance (Zopounidis and Doumpos, 2002), public policy (Mladineo et al., 1992), resource management (Bonila et al., 2016), siting of emergency shelters (Kar and Hodgson, 2008), land use (Chen, 2014), urban planning (Al-Shalabi et al., 2006), ecology (Bunruamkaew and Murayam, 2011; Zhang et al., 2015), humanitarian assistance (Curran et al., 2014) as well as in siting of energy infrastructures (Kotikot et al., 2020). MCDA allows spatialization of decision criteria (Ligmann-Zielinska and Jankowski (2012); Rinner and Heppleston (2006) and sensitivity analysis (Feick and Hall, 2004; Rinner and Heppleston, 2006) to capture local variants of certain decision rules (Carter and Rinner, 2014; Malczewski, 2011; Malczewski and Liu, 2014; Qin, 2013; Şalap-Ayça and Jankowski, 2016). Therefore, MCDA has gained popularity among researchers in terms of applications in urban equity studies (Obadia and Rinner, 2021). From a public health perspective, MCDA is useful in identifying interventions and evaluation criteria, measuring the interventions against those criteria, and combining the scores for each criterion to produce an overall assessment of each intervention (Marsh et al., 2013).
Using the Los Angeles (LA) metropolitan area as a case study site (one of the COVID-19 epicenters), we implemented MCDA to integrate built environment (i.e., land use type, road networks), socioeconomic characteristics, and mobility patterns to generate an accessibility index. The accessibility index represents the ease of commuting to a healthcare facility (e.g. hospitals) from different census block groups. We used the accessibility index in conjunction with social vulnerability indices developed by CDC to answer the following questions:
-
(i)
How does the accessibility index vary across census block groups based on their underlying socioeconomic and built environment characteristics w.r.t nearest hospitals? and,
-
(ii)
What is the optimal service area of a specific hospital w.r.t census block groups with a high incidence of COVID-19?
As discussed above, socioeconomic factors affected the contact rates among individuals across the US. Roy and Kar (2020) also found that social distancing was less likely to be maintained among socially disadvantaged communities. The purpose of this study is to quantify an accessibility metric for COVID-19 spread based on natural and built environment characteristics. By deploying a stratified approach that combines multiple criteria, this study generated a deeper understanding of parameters that contribute to the lack of social distancing and higher contact rates but were not previously used in forecasting COVID-19 spread.
2. Data & methods
The study area, LA Metro, is the second most populous metropolitan area in the US and within the Los Angeles (LA) county. The scope of the study includes the city of Los Angeles, Long Beach, and Beverly Hills, which is referred to as the “LA metro”. The findings correspond to the LA metro region beyond the city of LA. The LA Metro is also home to about 10 million people and more than 3.5 million households (US Census Bureau, 2016) as of 2016. In 2000, the city was occupied by ∼3.7 million people (1/3rd of the current population) and was the second-largest city in the nation (US Census Bureau, 2016). The distribution of neighborhoods based on poverty level forms a distinctive geographic pattern in the city (Fig. 1 ). Evidently, the poorest neighborhoods are concentrated near the downtown area, specifically, in South-Central and East LA, but there are other economically disadvantaged neighborhoods spread out sporadically throughout LA Metro. The affluent neighborhoods are concentrated along the coastal areas and in Santa Monica Mountains. Although a majority of hospitals are located closer to poorer neighborhoods (Fig. 1), the accessibility to these facilities may not be comparable to their locations. Additional analysis is required to understand the drivers of lower access (i.e., number of beds available, access to cars, etc.) which probably influenced the spread of COVID in these areas despite the increased availability of hospitals. We utilized locations of major hospitals in the LA Metro along with the number of available beds as primary healthcare facilities for this study.
Fig. 1.
Spatial distribution of hospitals with respect to income levels in the Los Angeles metropolitan area.
*Note: The boundary shapefile was obtained from the Los Angeles city planning map gallery (https://planning.lacity.org/odocument/0541e9db-ddb3-4279-a1d8-a271048fcc9d).
As of July 24th, 2021, the LA County Public Health Department had identified 173,995 positive cases of COVID-19 and a total of 4360 deaths across LA County (CDC, 2020). Of those who died, information about race and ethnicity was available for 4069 people (LA Public Health Dept., 2020). From the 4069 deaths, 48% of deaths occurred among Hispanic residents, 25% among White residents, 15% among Asian residents, 11% among African American/Black residents, less than 1% among Native Hawaiian/Pacific Islander residents, and 1% among residents identifying with other races (LA County Public Health Dept., 2020). According to the LA County Public Health Department, the death rates (number of deaths/100,000) were disproportionately higher in some neighborhoods, specifically, those present in the northeastern part and near the downtown area of LA city (Fig. 1).
For this study, we used the following social and built environment criteria – demographic, economic, number of COVID-19 cases, and built environment characteristics (slope of the street, transit stop density, proximity to busy intersections, walkability of neighborhoods) for the 4263 census block groups in LA Metro as listed in Table 1 . We obtained the socio-economic data (representing demographic characteristics and income) and social vulnerability characteristics from the US Census Bureau and the Centers for Disease Control and Prevention (CDC), respectively. We obtained data sets on transportation (i.e., traffic collision density, transit stop density) and road characteristics (i.e., speed limit, walkable conditions) from the LA County open data portal, LA County Department of Transportation (LA DOT, 2020), and Open Street Map road network.
Table 1.
List of all variables used to compute the overall cost to access the hospitals.
| Category | Variable | Source | Year |
|---|---|---|---|
| COVID-19 | Number of daily COVID-19 cases and deaths | LA County Public Health Department | 2020 (March 1st – July 31st) |
| Social Vulnerability | Social Vulnerability Index | Centers for Disease Control and Prevention | 2020 (Jan 1st – Dec 31st) |
| Healthcare facilities | Hospital locations | LA County Location Management System | 2017 |
| Built Environment | The slope of the street, Residential areas, % Green spaces, Population near busy streets, Car ownership | USGS, LA County open data portal , US Census Bureau | 2016 |
| Transportation | Walkable neighborhoods, Transit Stop Density, Speed limit, Traffic collision density | LA Department of Transportation | 2017 |
The datasets that were obtained in Excel or CSV format were converted to point layers using latitude and longitude information. We created density layers using the point data sets to depict the concentration of collisions and transit stops across the city. The remaining data layers were converted to 30 m × 30 m grids represented as raster layers for ease of comparison and analysis. The layers were also spatially referenced to UTM Zone 9N and the 1983 North American Datum for co-registration. We used the raster layers to assess the accessibility to 44 hospitals in the City of Los Angeles using the MCDA framework.
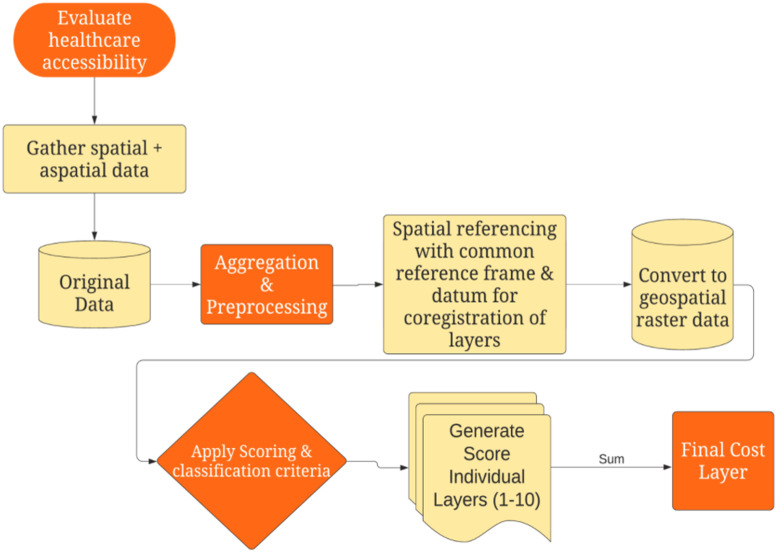
2.1. Developing the MCDA workflow
Based on previous research (Kotikot et al., 2020; Thokala et al., 2016, Dell’Ovo et al., 2018), we used an MCDA approach to integrate socio-economic characteristics, physical characteristics (topography - slope), and built environment characteristics (population density and transportation characteristics) to determine the least-cost path to a healthcare facility from each census block group centroid within LA Metro. We used the final cost layer generated from using MCDA (Fig. 2 ) to determine the least-cost path to the hospitals from each census block group. This helped us determine the accessibility cost associated with a block group based on the number of COVID-19 cases, and concentration of vulnerable population groups, which included low-income population, population with low accessibility to vehicles, elderly population above 65 years of age, and racial distribution (CDC, 2020; Flanagan et al., 2011).
Fig. 2.
A workflow describing the MCDA framework for healthcare accessibility.
2.2. Scoring mechanism for cost layer generation
MCDA is used to rank m alternatives based on n decision criteria. Each alternative A i (where i = 1, 2, …, m) is influenced by all the criteria C j (where j = 1, 2, …, n), and each criterion has a set of normalized value scores V k (where k = 1, 2, …, m). Typically, high scores imply high importance for a criterion. Once the criteria and their corresponding value scores are determined, the next step in MCDA is aggregation, which provides an overall value for each alternative based on all criteria and their corresponding weights. The aggregation results in a decision matrix given by, D, in the real Euclidean space R m x n, in which each decision a ij corresponds to an alternative A i, which is evaluated by the sum of the value scores for each criterion. The simplest form of MCDA is the linear sum model (LSM), which implements an addition function such that each alternative A i is derived by adding the multiplied output of a criterion C j and its corresponding value score V k given by Equation (1).
| (1) |
Typically, the MCDA criterion C j requires a weighting mechanism to highlight the importance of one criterion over the others. Assigning a weight to each criterion was challenging because there are no specific guidelines or prior studies in the context of COVID-19 that could be leveraged and conducting a survey of subject matter experts to determine weights was beyond the scope of the current research. Hence, we used an equal weighting approach with weight for each criterion was set to “1”.
2.3. Quantifying accessibility metric for hospitals
All the data layers were first resolved to the census block group boundary and then rasterized. The spatial overlay was used to match the COVID-19 cases at the census block group, and the data were apportioned using the population weighting scheme such that a block group's entire population was counted if it existed within the overlay polygon. Given the nature of the pandemic, the cost of accessing a healthcare facility was assumed to be influenced by travel time, which is subsequently influenced by traffic collisions, speed limit, and slope/topography of the transportation network connecting a healthcare facility with census block groups.
Each of these criteria was classified into 10 categories (Table 2 ) using Jenks natural breaks classification (Jenks and Caspall, 1971). The classified layers were combined using the equal weighting approach discussed above to generate the total cost layer. The value within each cell in the cost layer represents the cost per unit distance for moving through the cell to reach a healthcare facility. The cost layer was then used to compute a cost metric which was used to determine the overall accessibility to the nearest healthcare facility from each census block group. The lease cost path is also influenced by the direction of travel from a source (i.e., the centroid of a census block group) to reach a destination (i.e., the healthcare facility). Hence, we multiplied each cell value with the cell resolution while compensating for diagonal movement to obtain the total cost of passing through the cell.
Table 2.
Classification criteria to determine rank normalized value score of each layer.
| Scores |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Category | Very Low | Low | Medium | High | Very High | |||||
| Green Spaces (%) | 2.8–13.0 | 13.1–22.5 | 22.6–30.1 | 30.2–37.7 | 37.8–46.8 | 46.9–57.1 | 57.2–65.8 | 65.9–75.6 | 75.7–85.1 | 85.2–96.1 |
| Population near busy roads (%) | 0–338 | 338–794 | 794–1139 | 1139–1502 | 1502–1910 | 1910–2359 | 2359–2888 | 2888–3625 | 3625–5421 | 5421–8072 |
| Slope (degrees) | <3.7 | 3.7–8.8 | 8.8–14.9 | 14.9–20.3 | 20.3–25.1 | 25.1–29.8 | 29.8–34.3 | 34.3–39.4 | 39.4–46.9 | >46.9 |
| Speed Limit (km/hr) | <15 | 15–25 | 25–40 | 40–45 | 45–55 | 55–65 | 65–70 | 70–75 | 75–80 | >80 |
| Traffic Collisions density (per km) | <0.1 | 0.1–0.2 | 0.2–0.3 | 0.3–0.5 | 0.5–0.6 | 0.6–0.8 | 0.8–1.0 | 1.0–1.2 | 1.2–1.5 | >1.5 |
| Vehicles Owned | 0.36–0.86 | 0.87–1.25 | 1.26–1.56 | 1.57–1.84 | 1.85–2.06 | 2.07–2.30 | 2.31–2.88 | 2.89–3.74 | 3.75–4.43 | 4.44–4.76 |
| Walkable neighborhoods (%) | 0.44–0.47 | 0.48–0.52 | 0.53–0.57 | 0.58–0.60 | 0.61–0.65 | 0.99–0.70 | 0.71–0.73 | 0.74–0.78 | 0.79–0.83 | 0.84–0.87 |
| Transit Stop Density (KDE) | 0–71.17 | 71.18–213.52 | 213.53–403.32 | 403.33–664.30 | 664.31–1067.63 | 1067.63–1660.75 | 1660.76–2372.50 | 2372.51–3297.77 | 3297.78–4555.20 | 4555.21–6073.60 |
The LCP represented the shortest path (lowest travel time or highest accessibility) to a healthcare facility based on the cumulative cost over the entire cost surface from each census block group. The LCP i length was used to calculate the final accessibility metric, which is a measure of travel access to the nearest healthcare facility from a census block group normalized by the Social Vulnerability Index and the total number of COVID-19 cases (as of November 30th, 2020) as well the number of hospital beds available in destination hospitals.
To compare the MCDA method to well-acknowledged spatial accessibility measures in the transportation literature, we compared our results to the two-step floating catchment method. We determined the catchment areas based on a 10-mile radius around hospitals which is comparable to a 30-min driving time from a particular healthcare facility using the method proposed by Vo et al. (2015). For each catchment, we estimated the total population that the healthcare provider can reach within that drive time and computed a provider-to-population ratio (i.e., hospital capacity to total population within the catchment being served) as the first step. In the second step, we obtained the provider-to-population ratio of each healthcare facility based on a 30-min drive time and summed up the provider-to-population ratios of all hospitals. We used the maximum number of beds available for each hospital as the capacity of each hospital to admit patients infected by COVID-19 and requiring medical attention.
3. Results
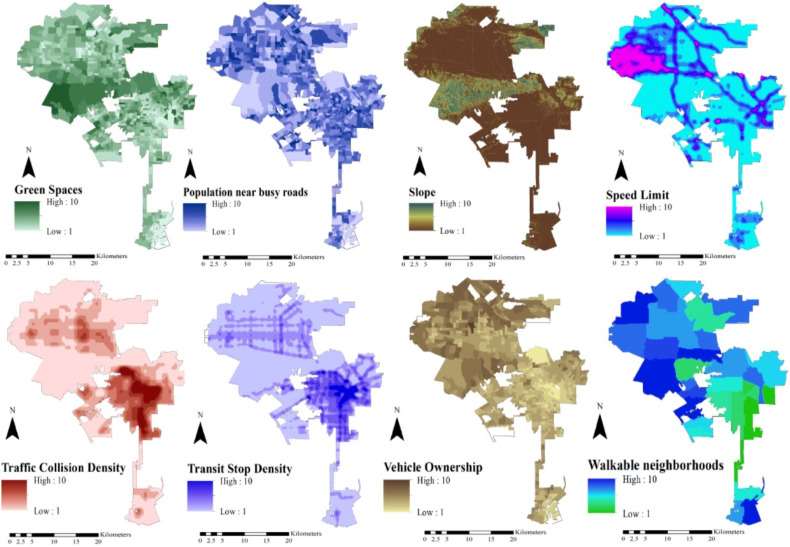
We used the criteria listed in Table 2 to quantify the spread of COVID-19 infections and deaths in LA Metro. For instance, the availability of green spaces and walkable neighborhoods ensure that people can maintain social distancing guidelines provided by the CDC thereby reducing exposure to the virus. Likewise, neighborhoods with a high volume of transit stops, reduced traffic collisions, and speed limits ensure the safe travel of residents to hospitals using public transit options even if they lack personal vehicles. The topography of a neighborhood, such as the slope of the road, contributes to the ease of driving to a healthcare facility as well as the travel time. Likewise, vehicle ownership ensures a resident can travel to a hospital based on personal needs, which may not be possible for residents who rely on public transit systems. The social and built environment criteria jointly contribute to the overall cost of accessing hospitals in LA Metro. We generated a cost layer using the MCDA workflow (Fig. 2) and eight variables corresponding to the demographic, built environment, safety, and vulnerability criteria (Fig. 3 ).
Fig. 3.
Normalized ranks of spatial layers for all factors considered important for accessibility.
The cost layer shown in Fig. 4 represents the total cost associated with accessing a healthcare facility throughout LA Metro. Using an equal weighting approach, the total cost was calculated by aggregating all the evaluated factors in Fig. 3 and using the linear sum approach based on values listed in Table 2.
Fig. 4.
A cost weighted distance layer for Los Angeles derived from MCDA to measure accessibility.
The summation of all the ranked layers resulted in total cost ranging between 12 and 44. The final layer shown in Fig. 4 represents the cost of traveling from the centroid of a census block group to any healthcare facility in LA Metro. Evidently, the cost is higher for residents in the LA downtown area as opposed to those residing in the surrounding block groups. The higher score represents lower access to hospitals and those regions need more attention from local authorities to facilitate more testing and vaccinations. The cost layer was used to generate the LCP from the centroid of each census block group (source) to the nearest healthcare facility (destination) which accounts for barriers to access (the criteria used in MCDA - Fig. 1).
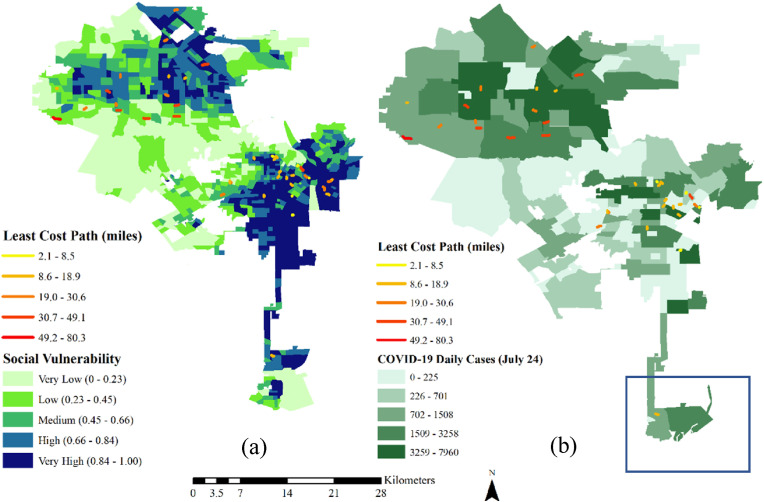
The length of the potential LCPs ranged from a minimum of 2.1 miles to a maximum of 80.3 miles across LA Metro (Fig. 5 ). The LCP was found to be higher in the LA downtown and Westfield area where the Social Vulnerability Indices for the block groups are also very high (Fig. 5). These areas have a disproportionately higher number of low-income neighborhoods, a high density of Hispanic and African American population as well as an increased number of COVID-19 cases. Fig. 5 depicts the overall spatial distribution of the Social Vulnerability Index (CDC, 2020) (SVI) generated by CDC for each census block group along with the LCPs. The SVI combines social, economic, and demographic indicators to identify the most socially vulnerable populations in each census block group. The SVI also accounts for a high unemployment rate, population below poverty levels, lower educational levels (i.e., below high school diploma), and a lack of homeownership.
Fig. 5.
Maps showing the least-cost path to each hospital along with (a) number of confirmed daily COVID-19 cases and (b) Social Vulnerability Indices.
According to Fig. 5a and b, the higher number of COVID-19 cases appear to be occurring in areas with SVI above 0.75 and these areas have a high elderly population (aged 65 or older), low income (poor neighborhoods), and less access to private motor vehicles. The social, economic, and demographic factors that contribute to a high Social Vulnerability Index are determined from the scoring mechanism defined by Flanagan et al. (2011). Using the total number of COVID-19 cases and SVI in each census block group, we derived the final weighted normalized accessibility index (Table 4) to hospitals in LA Metro and mapped the overall MCDA accessibility across LA Metro (Fig. 6 a), and compared it with spatial accessibility using 2SFCA (Fig. 6b).
Table 4.
List of Accessibility index along with least cost path, SVI, and COVID-19 cases.
| Variable | Values | Accessibility Index (Ai) |
Least Cost Path (LCPi) |
||
|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | ||
| COVID-19 Daily Cases | Very Low | 0.13 | 0.10 | 19.24 | 9.38 |
| Low | 0.34 | 0.40 | 26.49 | 11.79 | |
| Medium | 0.22 | 0.27 | 22.38 | 13.35 | |
| High | 0.09 | 0.07 | 21.59 | 14.40 | |
| Very High | 0.06 | 0.04 | 16.12 | 5.49 | |
| Social Vulnerability Index | Very Low | 0.62 | 0.46 | 31.91 | 15.71 |
| Low | 0.20 | 0.12 | 24.38 | 11.07 | |
| Medium | 0.16 | 0.03 | 28.08 | 9.13 | |
| High | 0.08 | 0.04 | 18.63 | 5.13 | |
| Very High | 0.09 | 0.10 | 16.82 | 10.73 | |
Fig. 6.
Map showing (a) MCDA accessibility indices and (b) spatial accessibility using 2SFCA associated with the hospitals in the LA Metro area.
The accessibility index was computed as a normalized value from 0 to 1 by applying a second level of MCDA by combining the LCP, the number of available beds in each hospital, the total number of confirmed COVID-19 cases, and the Social Vulnerability Index at the census block group level using a linear sum of scores from 1 to 10 (Table 3 ). Fig. 5, Fig. 6 jointly highlight some of the underlying factors influencing lower accessibility to hospitals in the South-Central part of LA. The variability in accessibility indices across all 44 facilities revealed that the higher Social Vulnerability is directly related to low access to healthcare. The findings revealed that the most accessible areas where people have easy access to hospitals are in Panorama City as well as in a small section of downtown and central part of LA city. It is also evident that the following neighborhoods - Encino, Woodland Hills, Westwood, Del Rey. Harbor City, Elysian Park, and Echo Park have the least access to hospitals.
Table 3.
The scoring criteria for different variables used to generate the accessibility index.
| Scores |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Very Low | Low | Medium | High | Very High | |||||
| LCP (miles) | 0–4.71 | 4.72–13.5 | 13.6–22.3 | 22.4–30.7 | 30.8–39.5 | 39.6–46.4 | 46.5–53.9 | 54.0–64.6 | 64.7–74.9 | 75.0–80.3 |
| SVI | 0–0.05 | 0.05–0.14 | 0.14–0.24 | 0.2–0.35 | 0.35–0.46 | 0.46–0.57 | 0.57–0.68 | 0.68–0.79 | 0.79–0.89 | 0.89–1.00 |
| # Beds | 16–112 | 112–196 | 196–287 | 287–363 | 363–456 | 456–558 | 558–632 | 632–721 | 721–831 | 831–885 |
| #COVID Cases | 0–82 | 82–190 | 190–304 | 304–470 | 470–688 | 688–927 | 927–1207 | 1207–2617 | 2617–4934 | 4934–7960 |
Table 4 shows the overall variation in accessibility indices and least-cost paths based on SVI and COVID-19 case incidence. It is important to note that the socially disadvantaged neighborhoods not only lack appropriate access to hospitals but also had a high number of COVID-19 cases. Additionally, the distance to healthcare facility and Social Vulnerability Indices had direct correlations to the overall cost to access (Supplementary Fig. S1). The lowest accessibility between 0.08 and 0.09 occurs in the regions with high and very high SVI values indicating how social vulnerability adds to the overall cost of access.
Based on the 2-SFCA approach we found that the highest spatial accessibility was observed in the northern and central parts of LA Metro (Fig. 6b). The downtown area and southern parts of the LA Metro were prone to medium and low accessibility as hypothesized and shown by the MCDA approach as well. Hence our results proved to be conclusive in terms of identifying areas of lower access. However, MCDA further unfolds the underlying factors that might have contributed to the lack of access. The low to medium access areas are also densely populated and have a significantly high SVI between 0.40 and 0.70 on average. However, it is interesting to note that highly accessible areas also do overlap with high SVI values indicating that some portions of the socially vulnerable population do have more access than other areas.
A previous study by Chen et al. (2017) has defined accessibility as qualitative classes like low, medium-high based on accessibility scores. A study by Luo et al. (2003) has defined a range of accessibility scores specific to the study whereas other studies by Stentzel et al. (2018) and Brondeel et al. (2014) have defined travel times as a measure of accessibility based on the 2SFCA approach. However, there are no specified and well-defined qualitative classes to define accessibility. Based on these previous studies and to avoid subjective bias, in this study, we quantified accessibility based on MCDA scores and compared those with ranges from traditional 2SFCA approaches, and have developed a nomenclature that may be used in future work using a similar technique with five different categories namely Very Low, Low, Medium, High and Very High.
4. Discussion
The MCDA approach is a decision support technique that allows evaluating multiple alternatives with transparency and stakeholder participation using several quantitative and qualitative criteria (Hongoh et al., 2011). Our study highlights the usability of MCDA in assessing accessibility to hospitals based on transportation, built environment, and socio-economic indicators. Our results indicate that the cost associated with travel (Fig. 4) was the highest in and around downtown LA. Given the higher number of COVID-19 cases and mortality in this area, it can be concluded that the risk of getting infected by COVID-19 is elevated among the demographic groups that lack personal vehicles and are reliant on walking or using public transportation for their daily activities (Fig. 3). These areas are also hotspots for regular traffic collisions and are interspersed with freeways and arterials with considerably higher speed limits between 55 and 75 mph. The higher traffic collision density (Fig. 3) and high-speed limit (above 65 mph) in this area is also a contributor to the increased overall cost of reaching a healthcare facility by the low-income population groups residing in the downtown area (Fig. 3). By contrast, the areas resided by higher-income households with personal vehicles have higher accessibility to hospitals in general. These areas also overlap with regions of low COVID-19 cases as reported by the health department indicating a higher incidence of cases, which could be attributed to lower accessibility to hospitals and subsequent community spreading due to lack of treatment.
It is interesting to note that the 2SFCA and MCDA results (Fig. 6) are inverse since 2SFCA uses catchments based on travel times, which were derived using just speed limits and distances traveled without taking into account the socioeconomic factors (used to determine the distribution of vulnerable population groups) and immediate built environment characteristics (used to determine the accessibility constraints to hospitals) that contribute to additional barriers in access. The MCDA approach accounted for the underlying social, environmental and geographic context that adds to the overall cost of access. Hence, the MCDA approach allowed the identification of block groups that are closest to hospitals distance-wise but were homes to vulnerable populations (due to socio-economic conditions) with barriers to access owing to vehicle access, safety, or lack of walkability.
The low accessibility in the southern part of LA City (red box in Fig. 5) in 2SFCA indicates that given the presence of one hospital, the majority of the block groups within the box are farther away from the hospital to be reached within 30-min (travel time constraint used in this study). The cost of accessibility according to the MCDA (Fig. 4) based on socioeconomic and built environment constraints is moderate to low for majority of the block groups within the red box. According to Fig. 5, social vulnerability is high to moderate for block groups in the northern part but is very low to moderate in the block groups located in the southern part in the box. The block groups in the northern part have high traffic collisions, moderate to low vehicle ownership, are less walkable, and have low green space. Hence, despite their proximity to the hospital, these constraints reduced the accessibility of the block groups but increased the accessibility of the block groups located in the southern part. While 2SFCA provides a general picture of accessibility based on distance and travel time, MCDA provides the variation in accessibility within a region based on social and built environment characteristics.
Our results highlight the importance of social measures of access (Farrington and Farrington, 2005) that exacerbate the cost of accessing hospitals in addition to the geographic distance. The relationship between the cost and distance varies positively with each other (Supplementary Fig. S1) indicating that higher cost is associated with longer distances. The higher cost also relates to higher social vulnerability (Supplementary Fig. S1), which indicates that lower accessibility is pronounced in disadvantaged neighborhoods. Previous studies (Wang and Luo, 2005) have tried to capture the interactions among the social and economic indicators (McGrail and Humphreys, 2009) which add to the barriers to healthcare services beyond the typical geographic distance measure to quantify accessibility. Other than being in line with these studies, the results highlight the significance of accessibility for COVID-19 patients in terms of their social vulnerability, which determines the 'opportunity' to travel (Morris et al., 1979) to hospitals.
The socially vulnerable areas with SVI above 0.75 appear to have lower access to hospitals owing to the higher unemployment rate, low income, low education (i.e., below high school diploma), lower homeownership, and less access to personal vehicles. The LCP was predominantly higher in the census block groups with daily confirmed COVID-19 cases between 1000 and 5000 (Fig. 5). Although some census block groups have a low number of reported cases, the LCP for these tracts is higher due to a lack of a sufficient number of hospitals within a driving radius of 30 min. According to the accessibility index (Fig. 6), the most vulnerable areas were associated with very low access to hospitals as opposed to the less vulnerable populations residing in Northeast LA, Woodland Hills, and Encino areas. Although some areas with high accessibility also facilitate socially vulnerable populations (Fig. 7 b) there are existing inequities in the number and distribution of hospitals which further widens the gap of access in the context of pandemics like COVID-19. Policymakers should specifically work towards increasing the number of facilities in proportion to the population density and amount of socially vulnerable populations residing in areas with low and very low access – which are often neglected. These areas will not only need access to pharmacies and urgent care but more emergency facilities in case of COVID-like situations where the respiratory health of the vulnerable populations is severely affected. Both travel times as well as least-cost paths to healthcare facilities like hospitals as highlighted in this study can be effectively integrated into planning new sites for hospitals and emergency vans during a public health crisis.
Fig. 7.
Boxplots showing variability in (a) population density and (b) social vulnerability indices for each category of MCDA accessibility.
In areas with high social vulnerability more targeted efforts are required by the local authorities in terms of ensuring performing frequent testing. The health professionals could arrange for mobile testing vans and/or provide more number of ambulance services in case of severe respiratory conditions arising due to COVID-19.
Our results also align with previous research conducted in the LA Metro region which have highlighted the social inequities which arise from the complex interactions of underlying factors like income (Oronce et al., 2020), transportation access (Chen et al., 2020), as well as housing affordability (Garde and Song, 2021) which have contributed to the low access to healthcare facilities. The factors explored in this study however add a new dimension to accessibility research in the context of COVID-19 and how the built environment and socioeconomic characteristics explored through MCDA could be leveraged to quantify the barriers to healthcare access among disadvantaged populations.
Although further analysis is required to examine the drivers of lower access in certain tracts, socio-economic conditions were major contributors to the spreading of COVID-19. Given the tracts with lower access have highly vulnerable population groups, it is crucial to identify those tracts before determining the barriers to access and developing strategies in terms of testing, future mobile vaccination, and basic healthcare support to reduce the spread and mortality from COVID-19. This information could also be used in case of other public health situations.
The primary focus of this study is to understand the rate of access to hospital beds among vulnerable communities. The pilot study conducted helps identify the factors which influence accessibility, and these factors can be used in the future for a predictive model. The current scope does not account for many other factors associated with the built environment, environmental conditions beyond social systems. We used only a subset of socioeconomic characteristics to understand the relationship between accessibility, COVID cases.
In the future, more qualitative analysis on top of the MCDA approach could be through questionnaires, interviews, and surveys to understand and prioritize the contributing factors that determine the overall cost of access. Additional predictive modeling approaches will also be used to identify census block groups that may need more attention in terms of urgent care and life support for vulnerable populations. Using these efforts could help researchers come up with a more streamlined approach for determining weights associated with each layer – that can help come up with a more nuanced model for computing the LCP. Additionally, travel times could be used as an indicator of accessibility as well, however, due to the lack of such high resolution and accurate speed limit data, we were not able to integrate it in our study. In the future, it might be beneficial to have travel time-based factors as an additional layer to determine the overall cost.
5. Conclusion
The study highlights that accessibility is shaped by factors such as affordability (El-Geneidy et al., 2016), employment availability (Geurs and Wee, 2004), gender (Akyelken, 2017), age (Ryan et al., 2015) as well as disability (Casas, 2007). Additional analyses (Supplementary Figs. S2 and S3) also indicate that these areas have residents with co-morbidities due to asthma and diabetes. Such information is useful for local authorities to plan for resource allocation (i.e., testing and vaccination site location) to ensure equitable healthcare access to all demographic groups.
Nearly 33% of census block groups which are disproportionately non-white with Hispanic and African- American populations in LA Metro accounted for 87.6% of COVID-19 deaths in Los Angeles during the study duration (February to July 2020). These epidemic hot spots appear to be based on the socioeconomic divide and inequitable access to critical infrastructures (transportation and healthcare facilities). The lack of testing as well as increased traffic congestion and speed limit may have contributed to the increase in COVID-19 cases and deaths. Hence, more geo-targeted resource planning, such as public transportation, rideshare, and/or use of high-speed lanes for patients with severe respiratory symptoms and establishment of testing and vaccination sites, is essential for the socially disadvantaged populations.
A major contributor to this study is the framework that accounts for both spatial and aspatial factors to determine healthcare accessibility, which could be used by the local authorities for resource planning as discussed above. Given the susceptibility of certain demographic groups to COVID-19, this framework can also be used to identify potential areas of COVID-19 spread based on demography and social vulnerability information as well as for policy deployment, such as the opening of schools in certain locations. Future studies will focus on deploying this framework in other COVID-19 hotspots to examine if equity exists in terms of access to healthcare facilities among different population groups in terms of vaccinations and planning preventive measures for future outbreaks.
Data availability
The datasets generated and/or analyzed during the current study are available in the Figshare repository, using the link https://doi.org/10.6084/m9.figshare.13184906.v1.
Acknowledgments
This manuscript has been authored by UT-Battelle, LLC under Contract No. DE-AC05- 00OR22725 with the U.S. Department of Energy. The U.S. Government retains and the publisher, by accepting the article for publication, acknowledges that the U.S. Government retains a non-exclusive, paid-up, irrevocable, world-wide license to publish or reproduce the published form of this manuscript, or allow others to do so, for United States Government purposes. DOE will provide public access to these results of federally sponsored research in accordance with the DOE Public Access Plan (https://energy.gov/downloads/doe-public-access-plan). Avipsa Roy was also supported in part by an appointment with the National Science Foundation (NSF) Mathematical Sciences Graduate Internship (MSGI) Program sponsored by the NSF Division of Mathematical Sciences. This program is administered by the Oak Ridge Institution for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy (DOE) and NSF. ORISE is managed for DOE by ORAU. All opinions expressed in this paper are those of the authors and do not necessarily reflect the policies and views of NSF, ORAU/ORISE, or DOE.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jth.2022.101331.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Akyelken Nihan. Mobility-related economic exclusion: accessibility and commuting patterns in industrial zones in Turkey. Soc. Incl. 2017;5(4):175–182. [Google Scholar]
- Al-Shalabi Mohamed A., Shattri Bin Mansor, Nordin Bin Ahmed, Rashid Shiriff. XXIII FIG Congress, Shaping the Change. 2006. GIS based multicriteria approaches to housing site suitability assessment; pp. 8–13. Munich, Germany, October. [Google Scholar]
- Berger Zackary D., Evans Nicholas G., Phelan Alexandra L., Silverman Ross D. 2020. Covid-19: Control Measures Must be Equitable and Inclusive. [DOI] [PubMed] [Google Scholar]
- Bissonnette Laura, Wilson Kathi, Scott Bell, Tayyab Ikram Shah. Neighbourhoods and potential access to health care: the role of spatial and aspatial factors. Health Place. 2012;18(4):841–853. doi: 10.1016/j.healthplace.2012.03.007. [DOI] [PubMed] [Google Scholar]
- Bonilla Valverde, Pablo José, Blank Clemens, Roidt Mario, Schneider Lisa, Catalin Stefan. Application of a GIS multi-criteria decision analysis for the identification of intrinsic suitable sites in Costa Rica for the application of managed aquifer recharge (MAR) through spreading methods. Water. 2016;8(9):391. [Google Scholar]
- Brondeel R., Weill A., Thomas F., Chaix B. Use of healthcare services in the residence and workplace neighborhood: the effect of spatial accessibility to healthcare services. Health Place. 2014;30:127–133. doi: 10.1016/j.healthplace.2014.09.004. [DOI] [PubMed] [Google Scholar]
- Brugha Cathal M. Trends in Multicriteria Decision Making. Springer; Berlin, Heidelberg: 1998. Structuring and weighting criteria in multi criteria decision making (MCDM) pp. 229–242. [Google Scholar]
- Bunruamkaew Khwanruthai, Murayam Yuji. Site suitability evaluation for ecotourism using GIS & AHP: a case study of Surat Thani province, Thailand. Proc. Soc. Behav. Sci. 2011;21:269–278. [Google Scholar]
- Carr-Hill Roy A., Sheldon Trevor A., Smith Peter, Martin Stephen, Peacock Stuart, Hardman Geoff. Allocating resources to health authorities: development of method for small area analysis of use of inpatient services. BMJ Br. Med. J. (Clin. Res. Ed.) 1994;309(6961):1046. doi: 10.1136/bmj.309.6961.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter B., Rinner C. Locally weighted linear combination in a vector geographic information system. J. Geogr. Syst. 2014;16(3):343–361. [Google Scholar]
- Casas Irene. Social exclusion and the disabled: an accessibility approach. Prof. Geogr. 2007;59(4):463–477. [Google Scholar]
- CDC’s Social Vulnerability Index SVI . 2020. Centers for Disease Control and Prevention.https://www.atsdr.cdc.gov/placeandhealth/svi/index.html [Google Scholar]
- Cervantes Arturo, Biegler Lorenz T. Optimization strategies for dynamic systems. Encycl. Optim. 2009;4:216–227. [Google Scholar]
- Chen Jiapei. GIS-based multi-criteria analysis for land use suitability assessment in City of Regina. Environ. Syst. Res. 2014;3(1):13. [Google Scholar]
- Chen J., Ni J., Xi C., Li S., Wang J. Determining intra-urban spatial accessibility disparities in multimodal public transport networks. J. Transport Geogr. 2017;65:123–133. [Google Scholar]
- Chen K.L., Brozen M., Rollman J.E., Ward T., Norris K., Gregory K.D., Zimmerman F.J. 2020. Transportation Access to Health Care during the COVID-19 Pandemic: Trends and Implications for Significant Patient Populations and Health Care Needs. [Google Scholar]
- Chin Taylor, Kahn Rebecca, Li Ruoran, Chen Jarvis T., Krieger Nancy, Buckee Caroline O., Balsari Satchit, Kiang Mathew V. medRxiv; 2020. US County-Level Characteristics to Inform Equitable COVID-19 Response. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran Richard W., Bates Matthew E., Bell Heather M. Multi-criteria decision analysis approach to site suitability of US Department of Defense humanitarian assistance projects. Procedia Eng. 2014;78:59–63. [Google Scholar]
- Dell'Ovo Marta, Capolongo Stefano, Oppio Alessandra. Combining spatial analysis with MCDA for the siting of healthcare facilities. Land Use Pol. 2018;76:634–644. [Google Scholar]
- Department of Transportation L: Los Angeles Department of Transportation. https://ladot.lacity.org/
- El-Geneidy Ahmed, Levinson David, Diab Ehab, Boisjoly Genevieve, Verbich David, Loong Charis. The cost of equity: assessing transit accessibility and social disparity using total travel cost. Transport. Res. Pol. Pract. 2016;91:302–316. [Google Scholar]
- Exworthy Mark, Peckham Stephen. Access, choice and travel: implications for health policy. Soc. Pol. Adm. 2006;40(3):267–287. [Google Scholar]
- Farrington John, Farrington Conor. Rural accessibility, social inclusion and social justice: towards conceptualisation. J. Transport Geogr. 2005;13(1):1–12. [Google Scholar]
- Feick R., Hall B. A method for examining the spatial dimension of multi-criteria weight sensitivity. Int. J. Geogr. Inf. Sci. 2004;18(8):815–840. [Google Scholar]
- Field Ken. Measuring the need for primary health care: an index of relative disadvantage. Appl. Geogr. 2000;20(4):305–332. [Google Scholar]
- Flanagan Barry E., Gregory Edward W., Hallisey Elaine J., Heitgerd Janet L., Lewis Brian. A social vulnerability index for disaster management. J. Homel. Secur. Emerg. Manag. 2011;8:1. [Google Scholar]
- Garde A., Song Q. Housing affordability crisis and inequities of land use change: insights from cities in the southern California region. J. Am. Plann. Assoc. 2021:1–16. [Google Scholar]
- Geurs Karst T., Bert Van Wee. Accessibility evaluation of land-use and transport strategies: review and research directions. J. Transport Geogr. 2004;12(2):127–140. [Google Scholar]
- Hansen Walter G. How accessibility shapes land use. J. Am. Inst. Plan. 1959;25(2):73–76. [Google Scholar]
- Hongoh Valerie, Anne Gatewood Hoen, Aenishaenslin Cécile, Waaub Jean-Philippe, Bélanger Denise, Michel Pascal. Spatially explicit multi-criteria decision analysis for managing vector-borne diseases. Int. J. Health Geogr. 2011;10(1):70. doi: 10.1186/1476-072X-10-70. Lyme-MCDA Consortium. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper Monica Webb, Anna María Nápoles, Pérez-Stable Eliseo J. COVID-19 and racial/ethnic disparities. JAMA. 2020 [Google Scholar]
- Jacquet-Lagreze Eric, Siskos Yannis. Preference disaggregation: 20 years of MCDA experience. Eur. J. Oper. Res. 2001;130(2):233–245. [Google Scholar]
- Jenks G.F., Caspall F.C. Error on choroplethic maps: definition, measurement, reduction. Ann. Assoc. Am. Geogr. 1971;61(2):217–244. [Google Scholar]
- Kang Jeon-Young, Michels Alexander, Lyu Fangzheng, Wang Shaohua, Agbodo Nelson, Freeman Vincent L., Wang Shaowen. Rapidly measuring spatial accessibility of COVID-19 healthcare resources: a case study of Illinois, USA. Int. J. Health Geogr. 2020;19(1):1–17. doi: 10.1186/s12942-020-00229-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kar Bandana, Hodgson Michael E. A GIS‐based model to determine site suitability of emergency evacuation shelters. Trans. GIS. 2008;12(2):227–248. [Google Scholar]
- Khan Abdullah A. An integrated approach to measuring potential spatial access to health care services. Soc. Econ. Plann. Sci. 1992;26(4):275–287. doi: 10.1016/0038-0121(92)90004-o. [DOI] [PubMed] [Google Scholar]
- Kotikot Susan M., Kar Bandana, Omitaomu Olufemi A. A geospatial framework using multicriteria decision analysis for strategic placement of reserve generators in Puerto Rico. IEEE Trans. Eng. Manag. 2020 [Google Scholar]
- Kwan Mei‐Po. Space‐time and integral measures of individual accessibility: a comparative analysis using a point‐based framework. Geogr. Anal. 1998;30(3):191–216. [Google Scholar]
- Kwan Mei‐Po. Gender and individual access to urban opportunities: a study using space–time measures. Prof. Geogr. 1999;51(no. 2):210–227. [Google Scholar]
- Kwan Mei-Po, Weber Joe. Scale and accessibility: implications for the analysis of land use–travel interaction. Appl. Geogr. 2008;28(2):110–123. [Google Scholar]
- Ligmann-Zielinska A., Jankowski P. Impact of proximity-adjusted preferences on rank-order stability in geographical multicriteria decision analysis. J. Geogr. Syst. 2012;14(2):167–187. [Google Scholar]
- Lovett Andrew, Haynes Robin, Sünnenberg Gisela, Gale Susan. Car travel time and accessibility by bus to general practitioner services: a study using patient registers and GIS. Soc. Sci. Med. 2002;55(1):97–111. doi: 10.1016/s0277-9536(01)00212-x. [DOI] [PubMed] [Google Scholar]
- Luo Wei, Qi Yi. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place. 2009;15(4):1100–1107. doi: 10.1016/j.healthplace.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Luo W., Wang F. Measures of spatial accessibility to health care in a GIS environment: synthesis and a case study in the Chicago region. Environ. Plann. Plann. Des. 2003;30(6):865–884. doi: 10.1068/b29120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Wei, Wang Fahui. Measures of spatial accessibility to health care in a GIS environment: synthesis and a case study in the Chicago region. Environ. Plann. Plann. Des. 2003;30(6):865–884. doi: 10.1068/b29120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo W., Whippo T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place. 2012;18(4):789–795. doi: 10.1016/j.healthplace.2012.04.002. [DOI] [PubMed] [Google Scholar]
- Malczewski J. Local weighted linear combination. Trans. GIS. 2011;15(4):439–455. [Google Scholar]
- Malczewski J., Liu X. Local ordered weighted averaging in GIS-based multicriteria analysis. Spatial Sci. 2014;20(2):117–129. [Google Scholar]
- Marsh K., Dolan P., Kempster J., Lugon M. Prioritizing investments in public health: a multi-criteria decision analysis. J. Publ. Health. 2013;35(3):460–466. doi: 10.1093/pubmed/fds099. [DOI] [PubMed] [Google Scholar]
- McGrail Matthew R., Humphreys John S. Measuring spatial accessibility to primary care in rural areas: improving the effectiveness of the two-step floating catchment area method. Appl. Geogr. 2009;29(4):533–541. [Google Scholar]
- McGrail Matthew R., Humphreys John S. The index of rural access: an innovative integrated approach for measuring primary care access. BMC Health Serv. Res. 2009;9(1):124. doi: 10.1186/1472-6963-9-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrail Matthew R., Humphreys John S. Measuring spatial accessibility to primary health care services: utilising dynamic catchment sizes. Appl. Geogr. 2014;54:182–188. [Google Scholar]
- Mladineo Nenad, Lozić Ivo, Stošić Snježana, Mlinarić D., Radica Tonko. An evaluation of multicriteria analysis for DSS in public policy decision. Eur. J. Oper. Res. 1992;61(1–2):219–229. [Google Scholar]
- Morris Jennifer M., Dumble Peter L., Ramsay Wigan M. Accessibility indicators for transport planning. Transport. Res. Gen. 1979;13(2):91–109. [Google Scholar]
- Obadia M., Rinner C. Measuring Toronto’s vital signs–Comparing global and local ideal point analysis in an urban equity case study. Comput. Environ. Urban Syst. 2021;88:101634. [Google Scholar]
- Oberschmidt Julia, Geldermann Jutta, Ludwig Jens, Schmehl Meike. International Journal of Energy Sector Management. 2010. Modified PROMETHEE approach for assessing energy technologies. [Google Scholar]
- Oronce C.I.A., Scannell C.A., Kawachi I., Tsugawa Y. Association between state-level income inequality and COVID-19 cases and mortality in the USA. J. Gen. Intern. Med. 2020;35(9):2791–2793. doi: 10.1007/s11606-020-05971-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano Eva, Di Cuonzo Daniela, Bona Cristina, Baldi Ileana, Gabriele Pietro, Ricardi Umberto, Rotta Paolo, et al. Accessibility as a major determinant of radiotherapy underutilization: a population based study. Health Pol. 2007;80(3):483–491. doi: 10.1016/j.healthpol.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Public Health Reports 10 New Deaths and 1,703 New Cases of Confirmed COVID-19 in Los Angeles County system. http://publichealth.lacounty.gov/phcommon/public/media/mediapubhpdetail.cfm?prid=25332
- Qin X. 2013. Local Ideal Point Method for GIS-Based Multicriteria Analysis: A Case Study in London. Ontario. [Google Scholar]
- Rader Benjamin, Astley Christina M., Sy Karla Therese L., Kara Sewalk, Hswen Yulin, Brownstein John S., Kraemer Moritz UG. Geographic access to United States SARS-CoV-2 testing sites highlights healthcare disparities and may bias transmission estimates. J. Trav. Med. 2020 doi: 10.1093/jtm/taaa076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray Darrell M., Anyane-Yeboa Adjoa, Balzora Sophie, Issaka Rachel B., May Folasade P. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nat. Rev. Gastroenterol. Hepatol. 2020;17(9):520–522. doi: 10.1038/s41575-020-0330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinner C., Heppleston A. International Conference on Geographic Information Science. Springer; Berlin, Heidelberg: 2006. The spatial dimensions of multi-criteria evaluation–case study of a home buyer's spatial decision support system; pp. 338–352. September. [Google Scholar]
- Rosenblatt Roger A., Lishner Denise M. Surplus or shortage? Unraveling the physician supply conundrum. West. J. Med. 1991;154(1):43. [PMC free article] [PubMed] [Google Scholar]
- Roy Avipsa, Kar Bandana. Proceedings of the 3rd ACM SIGSPATIAL International Workshop on Advances in Resilient and Intelligent Cities. 2020. Characterizing the spread of COVID-19 from human mobility patterns and SocioDemographic indicators; pp. 39–48. [Google Scholar]
- Ryan Jean, Anders Wretstrand, Schmidt Steven M. Exploring public transport as an element of older persons' mobility: a Capability Approach perspective. J. Transport Geogr. 2015;48:105–114. [Google Scholar]
- Saaty Thomas L. How to make a decision: the analytic hierarchy process. Eur. J. Oper. Res. 1990;48(1):9–26. doi: 10.1016/0377-2217(90)90060-o. [DOI] [PubMed] [Google Scholar]
- Şalap-Ayça S., Jankowski P. Integrating local multi-criteria evaluation with spatially explicit uncertainty-sensitivity analysis. Spatial Cognit. Comput. 2016;16(2):106–132. [Google Scholar]
- Shadmi Efrat, Chen Yingyao, Dourado Inês, Faran-Perach Inbal, Furler John, Peter Hangoma, Hanvoravongchai Piya, et al. Health equity and COVID-19: global perspectives. Int. J. Equity Health. 2020;19(1):1–16. doi: 10.1186/s12939-020-01218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Angela K., Richard Hughes Iv, Erica DeWald, Sara Rosenbaum, Amy Pisani, Walt Orenstein. Ensuring equitable Access to COVID-19 vaccines in the US: current system challenges and opportunities: analysis examines ensuring equitable access to COVID-19 vaccines. Health Aff. 2021:10–1377. doi: 10.1377/hlthaff.2020.01554. [DOI] [PubMed] [Google Scholar]
- Stentzel U., Bahr J., Fredrich D., Piegsa J., Hoffmann W., van den Berg N. Is there an association between spatial accessibility of outpatient care and utilization? Analysis of gynecological and general care. BMC Health Serv. Res. 2018;18(1):1–11. doi: 10.1186/s12913-018-3143-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thokala Praveen, Devlin Nancy, Marsh Kevin, Baltussen Rob, Boysen Meindert, Kalo Zoltan, Longrenn Thomas, et al. Multiple criteria decision analysis for health care decision making—an introduction: report 1 of the ISPOR MCDA Emerging Good Practices Task Force. Value Health. 2016;19(1):1–13. doi: 10.1016/j.jval.2015.12.003. [DOI] [PubMed] [Google Scholar]
- Thomas L.J., Huang P., Yin F., Luo X.I., Almquist Z.W., Hipp J.R., Butts C.T. Spatial heterogeneity can lead to substantial local variations in COVID-19 timing and severity. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(39):24180–24187. doi: 10.1073/pnas.2011656117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd James S., Seekins Steven V., Krichbaum John A., Harvey Lynn K. Health access America—strengthening the US health care system. JAMA. 1991;265(19):2503–2506. [PubMed] [Google Scholar]
- U.S. Census Bureau Quickfacts: Los Angeles County, California. 2016. https://www.census.gov/quickfacts/fact/table/losangelescountycalifornia,CA/PST04521927 California.
- Vo A., Plachkinova M., Bhaskar R. 2015. Assessing healthcare accessibility algorithms: A comprehensive investigation of two-step floating catchment methodologies family. [Google Scholar]
- Wang Fahui. Measurement, optimization, and impact of health care accessibility: a methodological review. Ann. Assoc. Am. Geogr. 2012;102(5):1104–1112. doi: 10.1080/00045608.2012.657146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Fahui, Luo Wei. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place. 2005;11(2):131–146. doi: 10.1016/j.healthplace.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Wang Jiang-Jiang, Jing You-Yin, Zhang Chun-Fa, Zhao Jun-Hong. Review on multi-criteria decision analysis aid in sustainable energy decision-making. Renew. Sustain. Energy Rev. 2009;13(9):2263–2278. [Google Scholar]
- Wang F., Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place. 2005;11(2):131–146. doi: 10.1016/j.healthplace.2004.02.003. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2021. WHO. Retrieved January 21.https://www.who.int/ from. [Google Scholar]
- Zhang Xiaorui, Wang Zhenbo, Lin Jing. GIS based measurement and regulatory zoning of urban ecological vulnerability. Sustainability. 2015;7(8):9924–9942. [Google Scholar]
- Zopounidis Constantin, Michael Doumpos. Multi‐criteria decision aid in financial decision making: methodologies and literature review. J. Multi-Criteria Decis. Anal. 2002;11(4‐5):167–186. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the Figshare repository, using the link https://doi.org/10.6084/m9.figshare.13184906.v1.