Abstract
Background:
A Community-Based Essential Newborn Care is a national initiative that incorporates a newborn care program into the continuum of maternal and child health care through enhancing community participation to reduce child morbidity and mortality and encourage healthy growth and development. This study aimed at assessing the level of Community-Based Essential Newborn Care service uptake and its associated factors among rural women in the Guraghe zone, Southern Ethiopia, 2020.
Methods:
A community-based cross-sectional study was conducted in the rural districts of Southern Ethiopia, from 1 to 31 May 2020. A multistage sampling technique was applied. Using a systematic random sampling technique, a total of 818 respondents were selected. The data collected by a pretested structured questionnaire were entered into EpiData 3.1 and exported to the Statistical Package for Social Sciences (Version 23) for analysis. To identify significant predictors of Community-Based Essential Newborn Care utilization, a multivariable logistic regression analysis was fitted. Adjusted odds ratios with 95% confidence intervals were used to estimate the strength of associations, and statistical significance was declared at a p value <0.05.
Results:
One-third, 269 (33.1%) (95% confidence interval = 30.0–36.2), of women and their newborns got the entire packages of the Community-Based Essential Newborn Care program. Desire on the last pregnancy (adjusted odds ratio = 2.66, 95% confidence interval = 1.56–4.51), birth preparedness and complication readiness plan (adjusted odds ratio = 4.82, 95% confidence interval = 3.26–7.12), timing of the postpartum visit (adjusted odds ratio = 3,56, 95% confidence interval = 2.00–6.34), attending monthly pregnant women conference (adjusted odds ratio = 3.01, 95% confidence interval = 1.99–4.57), and being a certified model household (adjusted odds ratio = 1.88, 95% confidence interval = 1.24–2.85) were identified as key predictors of Community-Based Essential Newborn Care utilization.
Conclusion:
The uptake of the full Community-Based Essential Newborn Care packages in the study area was low. Health care providers at the health institution and community level should give due emphasis to improve contraceptive service delivery. Besides, health extension workers at the community level should work on providing immediate postpartum visits, creating model households, and strengthening pregnant women conferences.
Keywords: Community-Based Essential Newborn Care, determinants, Southern Ethiopia
Introduction
Children continue to face widespread geographical inequalities in their chances of survival. According to a World Bank report of 2017, for every 1000 children born, 43 die before their fifth birthday, with the majority dying in developing countries. 1 The United Nations Children’s Fund and World Health Organization (WHO) reports of 2019 revealed that 5.2 million under-five children have died globally, and of these, 2.4 million (47%) occur in the first month of life, 1.5 million (28%) occur between 1 and 11 months, and 1.3 million (25%) occur between the ages of 1 and 4 years. 2 Current estimates show that developing countries are still far from reaching the Sustainable Development Goal (SDG) 3.2 (i.e. ending preventable deaths of newborns and children under the age of 5, at least 12 deaths per 1000 live births by 2030).2,3 Sub-Saharan Africa reagion has the highest child mortality rate in the world, with neonatal and under-five mortality rates of 27 and 76 deaths per 1000 live births, respectively.2–4
Community-Based Essential Newborn Care (CBENC) is a national initiative that integrates a newborn care program into the maternity and child health care continuum.5–7 It is about providing vital maternal and newborn care by increasing household and community engagement to minimize child mortality and promote stable early childhood growth and development.6,8 Its concept was based on global evidence of successful interventions in newborn care service package efficiency trials through the 4Cs: contact, case identification, care, and completion of treatment.6,9–12
The core components of CBENC are early identification of pregnancy; provision of focused antenatal care (ANC); promotion of institutional delivery; provision of immediate postnatal care (PNC); promotion of Exclusive breastfeeding (EBF); counseling on detection of danger signs; safe cord care (i.e. the application of chlorhexidine to the cord), hypothermia prevention (thermal care), and eyecare; and counseling on danger signs.6–8 An additional item incorporated in the program is the management of neonatal sepsis/very serious disease at the community level. 6
Globally, premature births, intrapartum complications, hypothermia, and infection are the leading causes of neonatal deaths, which together account for over 85% of all neonatal deaths.13,14 Although 70% of infant deaths occur in the first month of life, neonatal care was ignored by policy makers and health professionals in low- and middle-income countries. 14 The lack of postnatal facilities, lack of access to skilled delivery services (SDS), and delayed breastfeeding contributed to high rates of newborn mortality.15,16 Proper implementation of CBENC packages results in a 10% to 40% reduction in Neonatal Mortality Rate (NMR).11,17 Outreach programs such as ANC alone reduce NMR by about 10%. But an additional 30% reduction in NMR in Ethiopia is expected when combined with family packages using community health promoters.5,18
The reports of the mini Ethiopian Demographic Health Survey (EDHS) 2019 indicate that 74%, 48%, and 34% of women received at least one ANC visit, SDS, and PNC service from health care providers, respectively. 19 The neonatal, post-neonatal, and infant mortality rates were 30, 13, and 43 deaths per 1000 live births, respectively. 19 Compared to the 2016 EDHS report, infant and under-five mortality continue to decline, but neonatal mortality has remained constant from 29 20 to 30 19 per 1000 live births.
Health care providers in Ethiopia, as one of the developing countries, lack the resources to provide reliable and comprehensive neonatal care, particularly in rural settings. 8 Understanding the severity of the conditions, the Federal Ministry of Health of Ethiopia developed evidence-based, cost-effective initiatives called CBENC at the community level to improve neonatal outcomes.6–8 The CBENC initiative is essential to address the pressing need for affordable, efficient, and sustainable neonatal care at the community level.6,8
Despite the country, Ethiopia, has implemented a CBENC program to achieve the SDG of reducing child and infant mortality to 25 and 12 per 1000 live births, respectively,21,22 newborns face various barriers to access to health care. Some of these are due to traditions and access to health care services over long physical distances. 6 According to studies conducted elsewhere in Ethiopia, the level of CBENC uptake is between 23% and 40.7%, suggesting that the government needs to put in more effort.23–26 Educational status, postpartum visits (PPVs), knowledge of newborn danger signs, ANC usage, and place of delivery were all found to be predictors of CBENC service utilization.23–26 However, most of the previously conducted studies have failed to thoroughly investigate the influence of some of the health system–related factors such as attending a pregnant women conference (PWC) and birth preparedness and complication readiness (BPCR) plan on CBENC uptake.
Despite nearly all health extension workers (HEWs) have been trained to treat serious infections in newborns in the CBENC program, relatively few ill newborns in the country have been diagnosed and treated.5,18 It is important to assess the extent of CBENC service uptake at the community level to design interventions to reduce morbidity and mortality in newborns and achieve the target SDG3. 3 Despite a few studies24,25 conducted in CBENC, core components of care were not assessed comprehensively. Hence, this study was aimed at assessing the magnitude of CBENC service utilization and its associated factors among rural women based on the updated CBENC implementation guideline of 2013.6,7 The findings of this study may be used to inform health professionals, policy makers, and local administrative authorities about the extent of the CBENC program implementation in the study area. The findings of this study could aid in the careful design of ongoing health systems by strengthening community-based interventions that improve newborn care quality, resulting in reduced neonatal and maternal morbidity and mortality.
Materials and methods
Study setting and design
A community-based cross-sectional study was conducted in the rural districts of the Guraghe zone, Southern Ethiopia, from 1 to 31 May 2020. The area is located 158 km from Addis Ababa (Ethiopia’s capital city) and 337 km from Hawassa (capital of Southern Ethiopia region). Administratively, the zone is divided into 11 districts, encompassing 174 rural kebeles (kebele: the smallest administrative unit next to the district). For the fiscal year 2020, the total population of the district was 1,835,110, of which 1,515,801 (86.28%) lived in rural areas and 19.84% belonged to women in the reproductive age group (15–49 years old). Expected live births in the zone were 63,495 per year. There are 527 health facilities, comprising 74 health centers, 9 hospitals, and 444 health posts. 27
The population of the study
All women who had infants less than 6 months of age were the source population, and those selected women in the selected districts during the data collection period were considered to be the study population. Women who had infants under 6 months of age were included. Those mothers with a fetal death or stillbirth, who were living in the study area for less than 6 months, and were seriously ill during the data collection period were excluded from the study.
Sample size determination
The sample size for the study was determined by using a single population proportion formula by using the estimated prevalence of CBENC service uptake of 40.7% taken from a related study carried out in Northern Ethiopia, 24 95% confidence interval (CI), and 5% margin of error
After consideration of a 10% non-response rate and a design effect of 2, the total sample size was 818 women.
Sampling procedures
To recruit study participants, a multistage sampling technique was applied. At stage 1, out of 11 rural districts, 4 districts were randomly selected, namely, Ezha (with 24 kebeles), Cheha (with 12 kebeles), MihurAkilil (with 12 kebeles), and Soddo (11 kebeles). In stage 2, 24 kebeles were randomly selected out of a total of 59 kebeles of the four above-mentioned districts. The overall sample size was then allocated proportionally to each selected kebele. The list of women who gave birth within the last 6 months was obtained from the delivery registration book at the health post level, and a sampling frame was formed. The HEWs who work at the community level registered every mother within 24 h of delivery. Eligible women in each of the selected Kebeles were counted and reassured by HEWs for their presence. Codes/numbers were then provided for homes with eligible study participants, and a sampling frame had been developed for each kebele. Finally, study participants were chosen at random from the sampling frame by using a computer-generated random number and interviewed at their homes. If more than one eligible woman lives in the same house, the lottery method was used to select only one.
Data collection tools, methods, and personnel
Data were collected through a face-to-face interview using pretested structured questionnaires. Eight diploma nurses and three BSc (Bachelor of Science) public health professionals who have experience in data collection were recruited as data collectors and supervisors, respectively. The tool for data collection was developed by reviewing related literature in the field of interest.5,6,24,25,28 Household socioeconomic status was assessed by using a tool adapted from EDHS 2016, composed of multiple items like household assets, livestock ownership, crop production in quintals, average estimated monthly income, having agricultural land in hectares, and residential home with its infrastructures. 20 Sociodemographic variables, obstetric variables, use of maternal health services, level of BPCR, mothers’ knowledge of newborn danger signs, health system–related characteristics, and male involvement have been incorporated into the questionnaire. Women were contacted with the guidance of local community health workers (CHWs) in each kebele. The list of selected women in each kebele was provided in advance to the data collectors. The data were collected on a house-to-house basis.
Data quality management
Initially, the questionnaire used to collect data was prepared in English and translated into the local language (Amharic) by experts in that language, and finally re-translated into English to verify its consistency. A 1 day training was provided to both data collectors and supervisors on the objectives of the study, the content of the questionnaire, and the issues related to ethical issues during data collection. A pretest was carried out in the Mareko district, on 5% of the sample size (41 respondents), and necessary corrections were made before the actual data collection. The reliability of the questionnaires was assessed, and the reliability index for practical questions (Cronbach’s alpha) was 0.79. The potential of recall bias related to the time elapsed between the event and data collection time should also be considered even though respondents were allowed as much time as they needed for an adequate recall of long-term memory. In addition, concerning the questionnaire/interview design, the research team did its best to formulate questions that are clear and precise to reduce variation in comprehension ability. Inquiries were made following an ordered sequence of events; starting with the present and thinking back to a point in time. Moreover, memory aids, such as personal diaries, and probes, such as follow-up questions on a specific utilization event, were also used to enhance recall and reduce the risk of under-reporting. A day-to-day follow-up during the data collection period was carried out by the principal investigator and supervisors. Every completed questionnaire was checked for completeness. Unfilled and partially filled questionnaires were excluded before analysis. To minimize social desirability bias, study participants were interviewed privately.
Measurement of variables of the study
Outcome variable
CBENC utilization was assessed when a woman and her newborn obtained all the recommended elements of the program. Services from the maternal side were as follows: early identification of pregnancy, provision of ANC, promotion of health facility delivery service, and counseling on detection of danger signs. Services from the newborn side were optimal breastfeeding, safe cord care, thermal care, and eyecare.6–8,24 Consequently, if all elements of the program were obtained by the mothers, we considered them as “Utilized = 1” the CBENC program, otherwise “Not utilized = 0”:23,24
Optimal breastfeeding: Initiation of breastfeeding within 1 h after delivery, no avoidance of colostrum, and no prelacteal feeding.7,29
Thermal care: Dry and wrap newborns in clean clothes, postpone bathing newborns for 24 h, and place the newborns in skin-to-skin contact with their mothers.7,24
Safe cord care: Use a clean instrument for cutting the umbilical cord with the application of chlorhexidine.23,29
Explanatory variables
Knowledge of mothers on neonatal danger signs
The total number of right answers to eight items (neonatal danger signals) with a minimum score of 0 and a maximum score of 8 was used to assess mothers’ knowledge of neonatal danger signs. Respondents were asked to mention neonatal danger signs without offering the alternative of respectable signs. Mothers who reported at least half (four) neonatal risk signs were considered to have good knowledge of neonatal danger signs, while mothers who mentioned less than half (<4) of neonatal danger signs were considered to have poor knowledge of neonatal danger signs. 30
BPCR plan
The BPCR plan can be described as having taken at least five of the eight measures recommended by WHO: ascertained birthplace, identified birth attendants, put money aside, established emergency transportation, identified labor and birth companion, identified nearby health facility, identified blood donors if necessary, and identified care provider for children at home when the mother was away.31,32
PWC attendant
When a woman took part in meetings held in each kebele monthly, under the leadership and coordination of the HEW, with the support from a midwife from the health center, and the kebele command post members, otherwise considered as non-attendant.33,34
Model households
Model households (MHHs) are those who have implemented all four components of the health extension packages (HEPs) and have received formal certification. Those HEPs encompass interventions that fall under four categories: Family Health Services (maternal and child health, family planning, immunization, adolescent reproductive health, and nutrition), Infectious Disease Prevention and Control (tuberculosis (TB), human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), sexually transmitted infection (STI), and malaria), Hygiene and Environmental Sanitation (excreta, solid and liquid waste disposal, water supply, food hygiene, housing, personal hygiene, vector, and rodent control), and Health Education and Communication. 35
Data analysis
The data were coded, entered, and cleaned via EpiData (Version 3.1), and exported to Statistical Package for Social Sciences (SPSS, Version 23) for analysis. Descriptive statistics like frequencies, percentages, mean, and standard deviation were computed to describe the respondents’ characteristics through relevant variables of the study. The wealth status of households was determined by applying principal components analysis (PCA). Initially, 32 items were used and grouped into six components, namely, crop production in quintal, household properties, the average estimated monthly income, livestock ownership, hectares of agricultural land, and housing conditions. The fulfillment of assumptions for PCA such as overall sampling adequacy, sampling adequacy of individual variables, and Bartlett’s Test of Sphericity was checked. In each step, these variables with communalities less than 0.5 and complex structures were removed before the criteria were met by the iterations. Finally, three components were extracted from the PCA that clarified the maximum explained variation, and the first component which took part in the maximum variation was used to rate the study participants’ household wealth status in quintiles. 20
Bivariable and multivariable binary logistic regression analyses were employed to identify factors associated with CBENC uptake. The Hosmer–Lemeshow goodness-of-fit tests and the Nagelkerke R 2 were used to test model fitness. Multicollinearity between the explanatory variables was checked using the variance inflation factor (VIF > 10). A variable in the bivariable binary logistic regression analysis at p value <0.25 was eligible for multivariable logistic regression analysis. The crude and adjusted odds ratios (AORs) together with their corresponding 95% CIs were computed to determine the direction and strength of association of each explanatory variable with the outcome variable. Finally, variables with a p value less than 0.05 in a multivariable logistic regression were declared as significant determinants of CBENC uptake.
Results
Sociodemographic characteristics of the respondents
Of the total 818 sampled women for the study, 812 were actively involved in the study and yielded a response rate of 99.3%. The mean (±SD) age of respondents was 28.9 (±5.3) years, with the majority of women (78.1%) belonging to the age group 20 to 34 years. Most of the respondents were in marital unions (95.8%), housewives (71.7%), and had no formal education (43.3%). About half (50.7%) of the respondents were Orthodox followers by religion, and almost all (97.1%) of the respondents belonged to the Guraghe ethnicity (Table 1).
Table 1.
Sociodemographic characteristics of women in rural districts of Guraghe zone, Southern Ethiopia, 1 to 30 February 2020.
| Variables | Categories | Frequency | % |
|---|---|---|---|
| Age of mother in years (n = 812) | ⩾35 | 147 | 18.1 |
| 20–34 | 634 | 78.1 | |
| <20 | 31 | 3.8 | |
| Marital status (n = 812) | In marital relation | 778 | 95.8 |
| Not in marital relation a | 34 | 4.2 | |
| Religion (n = 812) | Orthodox | 412 | 50.7 |
| Muslim | 357 | 44.0 | |
| Protestant | 39 | 4.8 | |
| Catholic | 4 | 0.5 | |
| Ethnicity (n = 812) | Guraghe | 788 | 97.1 |
| Others b | 24 | 2.9 | |
| Mother’s educational level (n = 812) | No formal education | 352 | 43.3 |
| Primary education (1st–8th) | 285 | 35.1 | |
| Secondary education (9th–12th) | 147 | 18.1 | |
| College and above | 28 | 3.4 | |
| Mother’s occupation (n = 812) | Housewife | 582 | 71.7 |
| Merchant | 154 | 19.0 | |
| Daily laborer | 39 | 4.8 | |
| Farmer | 21 | 2.6 | |
| Government employee | 16 | 2.0 | |
| Husband’s educational level (n = 778) | No formal education | 302 | 38.8 |
| Primary education (1st–8th) | 267 | 34.3 | |
| Secondary education (9th–12th) | 170 | 21.9 | |
| College and above | 39 | 5.0 | |
| Husband’s occupation (n = 778) | Farmer | 546 | 67.2 |
| Merchant | 184 | 22.7 | |
| Government employee | 31 | 3.8 | |
| Daily laborer | 17 | 2.1 | |
| Wealth index (n = 812) | Highest | 162 | 20.0 |
| Fourth | 164 | 20.2 | |
| Middle | 161 | 19.8 | |
| Second | 164 | 20.2 | |
| Lowest | 161 | 19.8 | |
| Family size (n = 812) | <5 | 429 | 52.8 |
| ⩾5 | 383 | 47.2 |
Unmarried + divorced + widowed.
Other ethnicity = Amhara and Oromo.
Obstetric characteristics of respondents
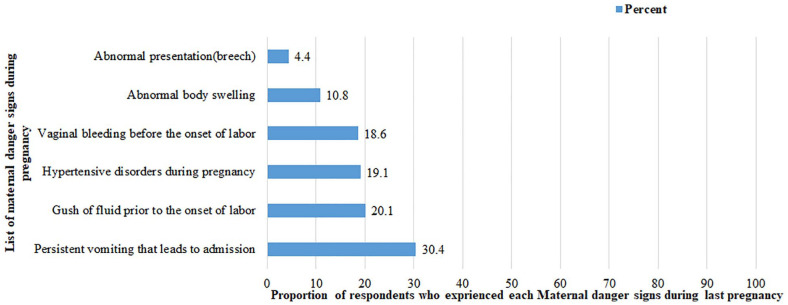
Four hundred twenty-two (52.0%), 286 (35.2%), and 104 (12.8%) respondents were multigravida, paragravida, and primigravida, respectively. More than half, 436 (53.7%), of respondents were multipara (have two to four children). The remaining 131 (16.1%) and 245 (30.2%) were primipara (have only one child) and grand multiparas (have five and more children), respectively. The last pregnancy was unplanned for more than one-fifth, 182 (22.4%), of respondents. Sixty-six (8.1%) respondents had a history of neonatal death. In one-quarter (25.1%) of respondents, the course of the last pregnancy was complicated, with at least one danger sign experienced. The main complaints reported were persistent vomiting leading to admission, 62 (30.4%), and fluid gush before the commencement of labor, 41 (20.1%) (Figure 1).
Figure 1.
Danger signs experienced by respondents during their last pregnancy in rural districts of Guraghe zone, Southern Ethiopia, 2020 (n = 204).
Maternal health service–related characteristics of respondents
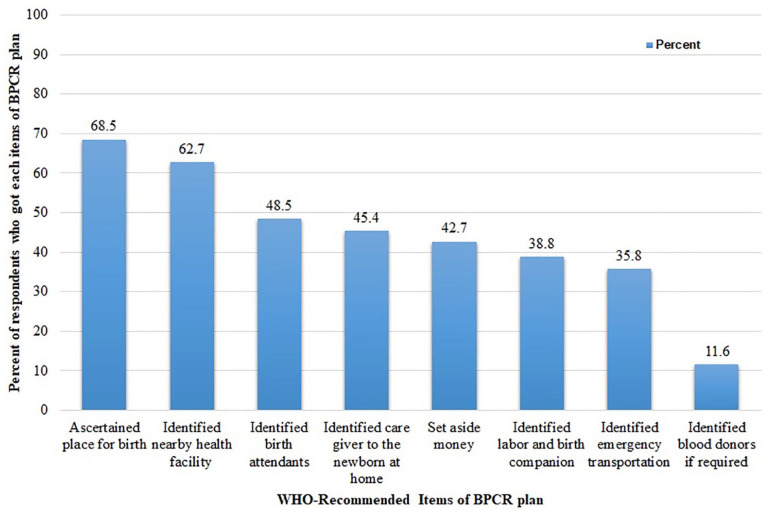
For their last pregnancy, 706 (86.9%) of respondents received at least one ANC visit and 274 (33.7%) of them received four and more visits. About the place of delivery, 652 (80.3%) women gave their last birth at a health institution. The majority, 683 (84.1%), of respondents got at least one PPV, and of them, 422 (61.8%) received their first visit within the first 24 h of birth. Two hundred sixty-five (32.6%) respondents attended the monthly PWC at the health post level (Table 2). Concerning BPCR plans, 274 (33.7%) respondents were well prepared for their last birth. Nearly 7 out of 10 mothers have ascertained a place of birth (68.5%; Figure 2).
Table 2.
Maternal health service–related characteristics of women in rural districts of Guraghe zone, Southern Ethiopia, 2020.
| Variable | Categories | Frequency | % |
|---|---|---|---|
| Number of ANC visits (n = 812) | No visit | 106 | 13.1 |
| 1 visit | 261 | 32.1 | |
| 2–3 visits | 171 | 21.1 | |
| ⩾4 visits | 274 | 33.7 | |
| ANC booking (n = 706) | Early booking (<12 weeks) | 352 | 43.3 |
| Late booking (⩾12 weeks) | 460 | 56.7 | |
| Attending PWC (n = 812) | Yes | 265 | 32.6 |
| No | 547 | 67.4 | |
| Place of last delivery (n = 812) | Health center | 509 | 62.7 |
| Hospital | 143 | 17.6 | |
| Home | 160 | 19.7 | |
| Mode of delivery (n = 812) | SVD | 679 | 83.6 |
| Instrumental delivery | 87 | 10.7 | |
| C/S | 46 | 5.7 | |
| Frequency of PPVs (n = 812) | No visits | 129 | 15.9 |
| 1 visit | 324 | 39.9 | |
| 2 visits | 195 | 24.0 | |
| ⩾3 visits | 164 | 20.2 | |
| The time when she got her first PPV (n = 683) | Within 24 h | 422 | 61.8 |
| On 3rd day | 130 | 19.0 | |
| On 7th day | 131 | 19.2 |
ANC: antenatal care, PWC: pregnant women conference; SVD: spontaneous vaginal delivery, C/S: cesarean section; PPVs: postpartum visits.
Figure 2.
The level of birth preparedness and complication readiness plan among respondents in rural districts of Guraghe zone, Southern Ethiopia, 2020.
Health system–related characteristics of respondents
The average time to reach the nearest health facility on foot was 51.7 min, and 547 (67.4%) of respondents reached the health facility within an hour. Concerning means of transport, 565 (69.6%) and 247 (30.4%) respondents traveled on foot and by vehicle, respectively. Six hundred sixty-one (81.4%) respondents reported that at least one HEW is available in the community. Three hundred seventy-nine (46.7%) respondents were accredited as an MHH for the successful implementation of HEPs launched by national health authorities. In the quest for maternal health services, more than three-fourths (76.4%) of respondents were autonomous.
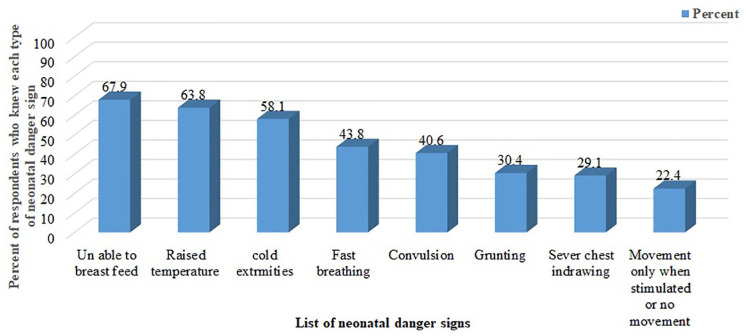
Respondent’s knowledge on neonatal danger signs
Nearly two-thirds of respondents (65.1%) had good knowledge of neonatal danger signs. Unable to breastfeed, 551 (67.9%); raised temperature, 518 (63.8%); and cold extremities, 472 (58.1%), were the common danger signs mentioned by respondents (Figure 3).
Figure 3.
Neonatal danger signs mentioned by respondents in rural districts of Guraghe zone, Southern Ethiopia, 2020.
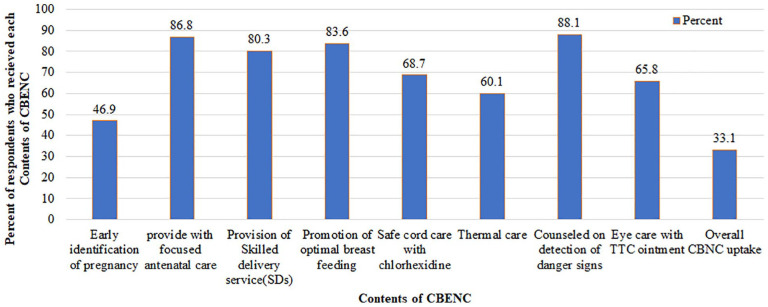
Uptake of CBENC
The adoption of the CBENC program was measured when all the recommended elements of the program were received by a woman and her newborn. Accordingly, 269 (33.1%) (95% CI = 30.0–36.2) women and their newborns got the entire packages of the CBENC program. Considering the individual components, the most common item received by 715 (88.1%) of mothers was counseling on the detection of danger signs, closely followed by focused ANC by 706 (86.9%). Early detection of pregnancy was comparatively the lowest service item obtained by the respondents, 381 (46.9%; Figure 4).
Figure 4.
Uptake of the contents of CBENC program among respondents in rural districts of Guraghe zone, Southern Ethiopia, 2020.
Factors associated with CBENC service utilization
Eleven variables showed association with CBENC utilization during a bivariable binary logistic regression analysis at a p value <0.25. After adjusting for those 11 variables using multivariable logistic regression, 5 variables—namely, desire on last pregnancy, BPCR plan, the timing of the PPV, being a certified MHH, and attending monthly PWC—were identified as significant predictors of CBENC utilization.
Women who planned for their recent pregnancy had 2.66 times higher odds of CBENC service uptake as compared to those who did not plan for their recent pregnancy (AOR = 2.66, 95% CI = 1.56–4.51). Having a BPCR plan was also identified as an important predictor of CBENC uptake. Those respondents who were well prepared for their last pregnancy were 4.6 times more likely than their counterparts to use CBENC (AOR = 4.82, 95% CI = 3.26–7.12).
The timing of the PPV in the current study showed a statistically significant association with CBENC experience. Those women who had received immediate PPV within 24 h of delivery were 3.56 times more likely to practice CBENC compared to those respondents who got their PPV on the 7th day and later (AOR = 3,56, 95% CI = 2.00–6.34). Those mothers who participated at the health post level in the monthly pregnant group meeting were 3 times more likely to practice CBENC as opposed to those who did not take part in the meeting (AOR = 3.01, 95% CI = 1.99–4.57). The odds of CBENC uptake among mothers from the MHH were almost 1.9 times higher compared to their counterparts (AOR = 1.88, 95% CI = 1.24–2.85; Table 3).
Table 3.
Determinants of CBENC service utilization among women in rural districts of Guraghe zone, Southern Ethiopia, 2020.
| Variables | Categories | CBENC utilization | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Yes (= 1) | No (= 0) | ||||
| Age in years (n = 812) | ⩾35 | 45 (16.8) | 102 (18.8) | 1 | 1 |
| 20–34 | 207 (76.9) | 427 (78.6) | 1.10 (0.74–1.62) | 0.93 (0.55–1.57) | |
| <20 | 17 (6.3) | 14 (2.6) | 2.75 (1.25–6.06)* | 1.96 (0.74–5.15) | |
| Mother’s educational level (n = 812) | No formal education | 107 (39.8) | 245 (45.1) | 1 | 1 |
| Primary education | 96 (35.7) | 189 (34.8) | 1.16 (0.83–1.62)* | 0.75 (0.47–1.18) | |
| Secondary education | 53 (19.7) | 94 (17.3) | 1.29 (0.86–1.94)* | 0.82 (0.47–1.42) | |
| College and above | 13 (4.8) | 15 (2.8) | 1.98 (0.91–4.31)* | 0.43 (0.14–1.29) | |
| Wealth index (n = 812) | Lowest | 50 (18.6) | 111 (20.2) | 1 | |
| Second | 59 (21.9) | 105 (19.4) | 1.25 (0.79–1.98) | ||
| Middle | 53 (19.7) | 108 (20.1) | 1.09 (0.68–1.74) | ||
| Fourth | 51 (18.9) | 113 (20.8) | 1.02 (0.63–1.60) | ||
| Highest | 56 (20.9) | 106 (19.5) | 1.17 (0.74–1.87) | ||
| Family size (n = 812) | ⩾5 | 116 (43.1) | 267 (49.2) | 1 | 1 |
| <5 | 153 (56.9) | 276 (50.8) | 1.28 (0.95–1.71)* | 1.01 (0.67–1.50) | |
| Parity (n = 812) | Grand multiparous | 71 (26.4) | 174 (32.1) | 1 | 1 |
| Multiparous | 148 (55.0) | 288 (53.0) | 1.26 (0.89–1.77)* | 1.42 (0.91–2.21) | |
| Primiparous | 50 (18.6) | 81 (14.9) | 1.51 (0.97–2.37)* | 1.63 (0.91–2.89) | |
| Desire on pregnancy | Unplanned | 31 (11.5) | 151 (27.8) | 1 | 1 |
| Planned | 238 (88.5) | 392 (72.2) | 2.96 (1.95–4.49) | 2.66 (1.56–4.51)** | |
| Level of BPCR plan (n = 812) | Not well prepared | 113 (42.0) | 425 (78.2) | 1 | 1 |
| Well prepared | 156 (58.0) | 118 (21.7) | 4.97 (3.62–6.82)* | 4.82 (3.26–7.12)** | |
| Mode of delivery (n = 812) | SVD | 219 (81.4) | 460 (84.7) | 1 | |
| Instrumental | 29 (10.8) | 58 (10.7) | 1.05 (0.65–1.69) | ||
| C/S | 21 (7.8) | 25 (4.6) | 1.76 (0.97–3.22)* | ||
| Timing of PPVs (n = 683) | On 7th day | 16 (6.8) | 115 (25.7) | 1 | 1 |
| On 3rd day | 42 (17.9) | 88 (19.6) | 2.65 (1.45–4.83)* | 2.72 (1.37–5.41)** | |
| Within 24 h | 177 (75.3) | 245 (54.7) | 3.85 (2.30–6.45)* | 3.56 (2.00–6.34)** | |
| Knowledge on danger sign | Not knowledgeable | 79 (29.4) | 204 (37.6) | 1 | 1 |
| Knowledgeable | 190 (70.6) | 339 (62.4) | 1.45 (1.06–1.98)* | 0.88 (0.59–1.32) | |
| Time to nearby health facility | Far (>1 h) | 82 (30.5) | 183 (33.7) | 1 | |
| Close (⩽1 h) | 187 (69.5) | 360 (66.3) | 1.16 (0.84–1.59) | ||
| Certified as MHHs (n = 812) | No | 108 (40.1) | 325 (59.9) | 1 | 1 |
| Yes | 161 (59.9) | 218 (40.1) | 2.22 (1.64–2.97)* | 1.88 (1.24–2.85)** | |
| Attending monthly PWC | No | 122 (45.3) | 425 (78.3) | 1 | 1 |
| Yes | 147 (54.7) | 118 (21.7) | 4.34 (3.17–5.95)* | 3.01 (1.99–4.54)** | |
CBENC: Community-Based Essential Newborn Care; COR: crude odds ratio; CI: confidence interval; AOR: adjusted odds ratio, BPCR: birth preparedness and complication readiness; SVD: spontaneous vaginal delivery; C/S: cesarean section; PPVs: postpartum visits; MHHs: model households; PWC: pregnant women conference. 1 = reference category.
Significant in a bivariable analysis at a p value of less than 0.25. **Statistically significant at a p value of less than 0.05.
Discussion
This study was aimed at evaluating the practice of CBENC and its associated factors among women in rural districts of the Guraghe zone. The study found that one-third, 33.1% (95% CI = 30.0–36.2), of women and their newborns fully utilized CBENC. This finding is lower than documented studies conducted in the rural districts of Southern and Northern Ethiopia, in which 37.5% and 40.7% of respondents received full packages of the CBENC program, respectively.23,24 The disparity may be due to the variation in the study area in which the current study was limited to rural women, whereas the aforementioned studies were majorly encountered urban populations. On the contrary, the figure was higher than two studies conducted in Northern and Southern Ethiopia, in which the service was accessed by 23.1% and 29.0% of respondents and their newborns, respectively.25,26 The possible reason for this disparity may be the variation in the adoption of maternal and child health services, where most of those services were higher in the current study area than in the two studies mentioned above.25,26 Besides, one of the above studies conducted in Southern Ethiopia 26 was conducted among women who gave birth at home and this could lead to lower CBENC program practice, as certain components of CBENC may be missed by those mothers. Moreover, stronger and more resilient health systems focused on community-based service provisions, such as the health extension program in Ethiopia, may clarify some of the discrepancies in current and other results.36,37
Desire on the last pregnancy, BPCR plan, the timing of the PPV, being a certified MHH, and attending monthly PWC were identified as independent factors associated with the CBENC utilization.
One of the factors positively associated with CBENC use in the study was respondents’ desire for their most recent pregnancy. When compared to their counterparts, women with planned pregnancies had a higher chance of taking CBENC. Studies conducted elsewhere supported the current finding, in which those women with planned pregnancies have a higher tendency to use CBENC.38–40 This can be explained by the fact that just because an index pregnancy is planned, the mother and her family have adequate time from conception through birth and the postnatal period to pay due attention. As a result, the chances of receiving the CBENC program’s recommended elements increased.40,41 As a result, a concerted effort is needed to mitigate unplanned pregnancies by expanding contraceptive provision and improving CBENC services so that women and newborns can benefit fully from the spectrum of services provided.
The level of BPCR was also identified as a significant predictor of CBENC uptake. For those mothers who were well prepared, the likelihood of receiving CBENC was 4.7 times higher. Studies showed that having a good BPCR plan results in a good uptake of maternal newborn and child health (MNCH) services.25,26 This could be because those women with a good BPCR plan are less likely to be exposed to delays in seeking, reaching, and accessing MNCH services and this may lead to good compliance with the CBENC service items. This result may have a policy effect as BPCR is one of the 12 basic WHO recommendations for increasing the use of skilled maternity care and minimizing serious obstetric and neonatal complications by the well-timed use of facility care. 42 To enhance the BPCR strategy for the better achievement of the (MNCH) continuum of care, the enhanced effort is therefore needed from the family, the community, and health care providers.
The timing of the PPV has also been identified in this study as a factor affecting CBENC practice. Those women who received immediate PPV within 24 h of delivery were 3.5 times more likely to practice CBENC than those respondents who received their PPV on and after the 7th day. This result is in line with a study carried out in Northern Ethiopia. 24 It is known that the majority of contents of CBENC like promotion of optimal breastfeeding, clean cord care, and thermal care were provided during immediate postpartum periods. Therefore, when a woman gets PPV immediately after delivery, she has a high propensity to comply with all CBENC components. This is well supported by the finding of the current study in which those mothers who got early PPV experienced more than two-thirds (75.1%) of CBENC usage. In improving CBENC utilization, health care practitioners at the health facility and the community level should also give due emphasis to immediate PPV.
The likelihood of CBENC use has been greater among those mothers who attended the monthly PWC. Studies conducted in the Awabel district, Northern Ethiopia, and Northwest Ethiopia support this finding.25,33 The Ethiopian Ministry of Health initiated a community-based intervention called a “pregnant women conference” to raise awareness of obstetric dangers and the use of institutional skilled maternal health care services. 34 These monthly meetings are led by HEWs at the community level and midwives or replacement nurses when midwives are not available from the catchment health centers.33,34,43 These meetings in turn could increase uptake of CBENC by fostering a sense of peer support among women to pursue adequate ANC, planning for delivery at a health facility, following through with appropriate PNC, and promoting exclusive breastfeeding. 34 Health workers in the community and health facilities must therefore work actively to initiate and strengthen these conferences.
The current study revealed that, among women who were from a certified MHH, the odds of CBENC uptake were greater than their counterparts. This may be because, through training, support, and follow-up, HEWs invest a lot of time in capacity building for those selected to be role models in HEPs.35,44 Such successive training and follow-up may contribute to the improvement of skills in the practice of the recommended CBENC program packages relative to their counterparts. Findings from previous studies have shown that MNCH services are well utilized by those mothers from MHHs.45,46 This is well supported by the current study in which 59.9% of mothers who have received maximum CBENC service packages were from MHHs. HEWs must therefore put a great emphasis on the creation of MHHs.
There were both strengths and shortcomings of this study. The study focused on CBENC practice by emphasizing all service items based on the newly established CBENC guideline in 2013 by the Ministry of Health of Ethiopia.6,12 Thus, it could be used as an input at the local and policy levels. As this study is cross-sectional, no relationship was established between cause and effect. Even though respondents were given as much time as they needed for a good recall of long-term memory and more recent births have been considered, the likelihood of recall bias due to the time elapsed between the event and data collection time should be considered. In addition, inquiries were made, following an ordered sequence of events—starting with the present and thinking backward to a point in time to cope with the recall bias. Furthermore, the sample frame was based on secondary data, which may not have included all of the study’s eligible women. The study was limited to a small locality due to resource constraints, which may limit its generalizability to a larger population. Finally, the study was based on self-reports and this may have contributed to biases in social desirability.
Conclusion
CBENC service utilization in the study area was low. Desire on the last pregnancy, BPCR plan, the timing of the PPV, attending monthly PWC, and being a certified MHH were identified as significant predictors of CBENC utilization. Health care providers at the health institution and community level should give due emphasis to improve contraceptive service delivery. Besides, HEWs at the community level should work on providing immediate PPVs, creating MHHs, and strengthening PWCs.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211067690 for The level of Community-Based Essential Newborn Care utilization and associated factors among rural women in Southern Ethiopia, 2020: Based on the updated Community-Based Essential Newborn Care guideline by Aklilu Habte, Kaleegziabher Lukas and Temesgen Tamirat in SAGE Open Medicine
Acknowledgments
We are indebted to Wachemo University College of Medicine and Health Sciences, Department of Public Health, for giving ethical clearance to undertake the study. Our appreciation also goes to the managers and health care providers who worked in the selected District Health Office for their assistance and cooperation during the study. Finally, for their efforts, we want to thank our supervisors, data collectors, and study participants.
Footnotes
Author contributions: A.H. wrote the proposal, supervised the collection of data, the entry, and analysis of data, and finally engaged in the writing and examination of the manuscript. K.L. participated in the design, methodology, data analysis, and reviewing of the manuscript critically. T.T. participated in the data review and during the study provided critical and progressive suggestions. The final paper was read and approved by all authors.
Availability of data and materials: The data used to support the findings of the current study can be obtained from the corresponding author on reasonable request via akliluhabte57@gmail.com.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the Ethics Committee of Wachemo University, College of Medicine and Health Sciences with an approval ID of WCU/039/12.
Informed consent: Written informed consent was obtained from all subjects before the study. Besides, after explaining the study goals and procedures, written informed consent was taken from a parent or guardian using normal disclosure processes for those participants less than 18 years of age.
ORCID iDs: Aklilu Habte  https://orcid.org/0000-0002-5719-4294
https://orcid.org/0000-0002-5719-4294
Temesgen Tamirat  https://orcid.org/0000-0002-8079-3789
https://orcid.org/0000-0002-8079-3789
Supplemental material: Supplemental material for this article is available online.
References
- 1. World Bank. Mortality rate, under-5 (per 1000 live births) data. http://data.worldbank.org/indicator/SH.DYN.MORT/countries?display¼default (accessed 26 October 2017).
- 2. United Nations Children’s Fund, WHO, World Bank Group, United Nations Population Division. Levels and Trends in Child Mortality United Nations Inter-Agency Group for Child Mortality Estimation (UN IGME), report 2020. file:///F:/under20consideration/enbc/Levels-and-trends-in-child-mortality-IGME-English_2020.Pdf (accessed 9 September 2020). [Google Scholar]
- 3. United Nations: Sustainable Development Goals (SDGs). United Nations sustainable development summit 2015. New York: United Nations, 2015. [Google Scholar]
- 4. Amuka JI, et al. Neonatal deaths and challenges of public health: where do we need urgent intervention in developing countries? Health Care Women Int 2020; 41(2): 227–237. [DOI] [PubMed] [Google Scholar]
- 5. Mathewos B, et al. Community-Based Interventions for Newborns in Ethiopia (COMBINE): cost-effectiveness analysis. Health Policy Plan 2017; 32: 21–32. [DOI] [PubMed] [Google Scholar]
- 6. Federal Ministry of Health Ethiopia. Community based newborn care implementation guideline. https://ideas.lshtm.ac.uk/wp-content/uploads/2019/08/CBNCFinalReportExecSummary_FINAL.pdf
- 7. Berhanu D, Avan B. Community based newborn care programme in Ethiopia 2013–2017: final evaluation report, March 2019. London: IDEAS, London School of Hygiene & Tropical Medicine, 2019. [Google Scholar]
- 8. Mathewos B, et al. Community-based newborn care in Ethiopia: implementation strength and lessons learned. Ethiop Med J 2019; 3: 269–279. [Google Scholar]
- 9. Banteyerga H. Ethiopia’s health extension program: improving health through community involvement. MEDICC Rev 2014; 13: 46–49. [DOI] [PubMed] [Google Scholar]
- 10. Bang AT, et al. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet 1999; 354: 1955–1961. [DOI] [PubMed] [Google Scholar]
- 11. Baqui A, et al. Effect of community-based newborn care on cause-specific neonatal mortality in Sylhet district, Bangladesh: findings of a cluster-randomized controlled trial. J Perinatol 2016; 36(1): 71–76. [DOI] [PubMed] [Google Scholar]
- 12. Taylor ME. Community based newborn care in Ethiopia: introduction to the special issue. Ethiop Med J 2019; 3: 181–183. [Google Scholar]
- 13. Lawn JE, Simon C. 4 Million neonatal deaths: when? Where? Why? Lancet 2005; 365: 891–900. [DOI] [PubMed] [Google Scholar]
- 14. Lawn JE, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet 2014; 384(9938): 189–205. [DOI] [PubMed] [Google Scholar]
- 15. Tinker A, et al. Advancing newborn health: the saving newborn lives initiative. Glob Public Health 2010; 5(1): 28–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. UNICEF. Target product profile for newborn care in low-resource settings, Consensus Meeting Report, March 2020. New York, NY: UNICEF, 2020. [Google Scholar]
- 17. Lassi ZS, Haider BA, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev 2010; 11: CD007754. [DOI] [PubMed] [Google Scholar]
- 18. Hailegebriel TD, et al. Effect on neonatal mortality of newborn infection management at health posts when referral is not possible: a cluster-randomized trial in rural Ethiopia. Glob Health Sci Pract 2017; 5(2): 202–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF. Ethiopia Mini Demographic and Health Survey 2019: key indicators. Rockville, MD: EPHI and ICF, 2019. [Google Scholar]
- 20. Central Statistical Agency (CSA). Ethiopia Demographic Health Survey 2016. https://dhsprogram.com/pubs/pdf/FR328/FR328
- 21. Taylor ME. Community based newborn care in Ethiopia: introduction to the special issue. Ethiop Med J 2019; 3: 181–183. [Google Scholar]
- 22. Semu Y, Tekle E, Bekele A, et al. Making community based newborn care sustainable in Ethiopia. Ethiop Med J 2019; 3: 281–285. [Google Scholar]
- 23. Gebremedhin T, Atnafu A, Dellie E. Community-based newborn care utilisation and associated factors in Geze Gofa rural district, South Ethiopia: a community-based cross-sectional study. BMJ Open 2020; 10(8): e037792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weldeargeawi GG, et al. Community-Based Essential Newborn Care practices and associated factors among women of Enderta, Tigray, Ethiopia, 2018. Int J Reprod Med 2020; 2020: 2590705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kokebie T. Community based essential newborn care practices and associated factors among women in the rural community of Awabel District, East Gojjam Zone, Amhara, Ethiopia, 2013. Int J Adv Sci Res 2015; 1: 1. [Google Scholar]
- 26. Agonafir M, et al. Community based essential newborn care practices and associated factors among women who gave birth at home in last twelve months in Amaro Woreda, Southern Ethiopia. Glob Pediatr Health 2019; 8: e1016151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Guraghe Zone Statistical Abstract, SNNPR, Wolkite, 2018–2019, 2020. [Google Scholar]
- 28. Tadesse L, et al. Modeling the potential reduction of newborn mortality with national scaling up of community-based newborn care in Ethiopia. Ethiop Med J 2019; Suppl 3. [Google Scholar]
- 29. Berhe M, et al. Essential neonatal care utilization and associated factors among mothers in public health facilities of Aksum Town, North Ethiopia, 2016. PLoS One 2017; 12(4): e0175902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jemberia MM, et al. Low level of knowledge about neonatal danger signs and its associated factors among postnatal mothers attending at Woldia General Hospital, Ethiopia. Matern Health Neonatol Perinatol 2018; 4(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Haile D, et al. Level of completion along continuum of care for maternal and newborn health services and factors associated with it among women in Arba Minch Zuria Woreda, Gamo zone, Southern Ethiopia: a community based cross-sectional study. PLoS One 2020; 15(6): e0221670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Belda SS, Gebremariam MB. Birth preparedness, complication readiness and other determinants of place of delivery among mothers in Goba District, Bale Zone, South East Ethiopia. BMC Pregnancy Childbirth 2016; 16(1): 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Asresie MB, Dagnew GW. Effect of attending pregnant women’s conference on institutional delivery Northwest Ethiopia: comparative cross-sectional study. BMC Pregnancy Childbirth 2019; 19: 353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Save the Children. Pregnant women conference best practice from Ethiopia. https://www.healthynewbornnetwork.org/hnn-content/uploads/Pregnant-Women-Conference.pdf (accessed 24 August 2017).
- 35. Wang H, Tesfaye RNV, Ramana G, et al. Ethiopia health extension program: an institutionalized community approach for universal health coverage. Washington, DC: The World Bank, 2016. [Google Scholar]
- 36. Fetene N, et al. The Ethiopian health extension program and variation in health systems performance: what matters? PLoS One 2016; 11(5): e0156438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Admasu K-B. Designing a resilient National health system in Ethiopia: the role of leadership. Health Syst Reform 2016; 2(3): 182–186. [DOI] [PubMed] [Google Scholar]
- 38. Alemu A, Eshete A. Newborn care practices and associated factors among lactating mothers at home in the Rural Districts of Gedeo Zone, Southern Ethiopia. Pediatr Health Med Ther 2020; 11: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Waiswa P, et al. Poor newborn care practices—a population based survey in eastern Uganda. BMC Pregnancy Childbirth 2010; 10(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ayiasi RM, et al. Is antenatal care preparing mothers to care for their newborns? A community-based cross-sectional study among lactating women in Masindi, Uganda. BMC Pregnancy Childbirth 2014; 14(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hajizadeh M, Nghiem S. Does unwanted pregnancy lead to adverse health and healthcare utilization for mother and child? Evidence from low- and middle-income countries. Int J Public Health 2020; 65(4): 457–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. World Health Organization. WHO and recommendations on health promotion interventions for maternal newborn health 2015. Geneva: World Health Organization, 2015. [PubMed] [Google Scholar]
- 43. Turan JM, Tesfagiorghis M, Polan ML. Evaluation of a community intervention for the promotion of safe motherhood in Eritrea. J Midwifery Womens Health 2011; 56(1): 8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Desta SH, Basha SY. The role of health extension workers in primary health care in AsgedeTsi’mbla District: a case of Lim’at T’abya health post. Int J Soc Sci Manag 2017; 4(4): 248–266. [Google Scholar]
- 45. Karim AM, et al. Effect of Ethiopia’s health extension program on maternal and newborn health care practices in 101 rural districts: a dose-response study. PLoS One 2013; 8(6): e65160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Medhanyie A, et al. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res 2012; 12(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211067690 for The level of Community-Based Essential Newborn Care utilization and associated factors among rural women in Southern Ethiopia, 2020: Based on the updated Community-Based Essential Newborn Care guideline by Aklilu Habte, Kaleegziabher Lukas and Temesgen Tamirat in SAGE Open Medicine