Abstract
Kambô is a cleansing ritual involving the application of a toxin produced by the giant leaf frog (Phyllomedusa bicolor). The Kambô ritual has increasingly been adopted among cancer patients in Europe. Accumulating data indicate various adverse effects. We report another severe adverse reaction to Kambô, a systemic inflammatory response syndrome mimicking disease progression in a patient with cholangiocarcinoma. We describe a systemic reaction to Kambô, manifested as tachycardia, tachypnea, impaired liver cholestatic enzymes, and enlargement of lymphadenopathy mimicking disease progression. The clinical features and onset of symptoms, the rapid reaction, and the lack of other identified causes make the diagnosis of Kambô-induced SIRS highly probable. This case report calls for future studies examining standard oncological care such as chemotherapy, radiotherapy, and immunotherapy in conjunction with alternative therapy. Additionally, greater awareness and physician education should be promoted, encouraging inquiry of oncology patients’ administration of alternative, complementary, and integrative medicine.
Keywords: cholangiocarcinoma, kambu, integrative medicine, SIRS, physician’s education
Background
Kambô is a cleansing ritual performed among numerous indigenous South American cultures, involving the application of a toxin produced by the giant leaf frog (Phyllomedusa bicolor) as a remedy for chronic diseases of the mind and body. The toxin contains N-methyldecahydroquinolines, a class of alkaloids1,2 and has demonstrated anti-proliferative activity against cancer cells in vitro. 3 The Kambô ritual has increasingly been adopted among cancer patients in Europe. While not indicating therapeutic benefit, accumulating data demonstrate its various adverse effects, among them liver toxicity, 4 syndrome of inappropriate antidiuretic hormone secretion, 5 psychosis, 6 gastro-intestinal toxicity, 7 and even sudden death. 8 The toxin induces early onset activity within few days, and may manifest as tachycardia, vomiting, incontinence, euphoria, and sedation. 9
We report another severe adverse reaction to Kambô, systemic inflammatory response syndrome (SIRS) mimicking disease progression in a patient with cholangiocarcinoma. Signed consent for publication was obtained from the family of the patient, who is deceased, and is on file in the patient’s medical record.
Case Presentation
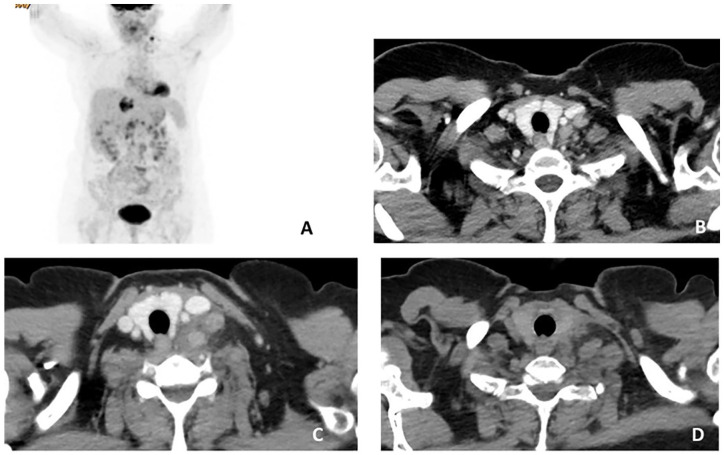
A 58 year old female was diagnosed with metastatic cholangiocarcinoma following workup for abdominal pain and weight loss. Her past medical history included polycythemia vera requiring intermittent phlebotomy, chronic obstructive pulmonary disease, and hyperlipidemia. Upon diagnosis, PET CT revealed metastatic disease including enlarged pathological peripancreatic, gastrohepatic, hepatoduodenal, and portocaval lymph nodes and a supraclavicular left mass (Figure 1A and B). Laboratory results reflected mildly increased ALT = 49 IU/L, complete blood count (CBC), comprehensive metabolic panel (CMP), and tumor markers CEA and CA19-9, which were unremarkable.
Figure 1.
Imaging studies before and after the Kambô ritual. PET-CT at presentation with FDG uptake in liver demonstrating primary cholangiocarcinoma, uptake in enlarged abdominal lymph nodes, and in a left supraclavicular mass (A). Neck and chest CT scan at presentation with small left supraclavicular lymph nodes and no airway compromise (B). Chest CT scan performed after the Kambo ritual demonstrating enlargement of a lymph node conglomerate in the left neck with deviation of the trachea and the left thyroid lobe (C). Partial spontaneous resolution of lymphadenopathy 3 months after Kambo ritual (D).
The patient received a single cycle of gemcitabine and oxaliplatin chemotherapy regimen and subsequently refused resumption of treatment due to general weakness attributed to the therapy.
Two months following administration of chemotherapy, the patient performed the Kambô ritual involving deliberate burns to the upper left arm and application of frog secretions to the burnt skin. Two days subsequent to the ritual, the patient presented at the oncology emergency department with acute enlargement of the known left supraclavicular mass, tachycardia, and shortness of breath. Physical examination revealed tachycardia of 96 bpm, tachypnea >15 breaths/minutes, oxygen saturation level of 96%, and a tender enlarged solid mass in her left lower neck. The laboratory results reveled an elevated CRP (from a baseline CRP level of 16 to 60), increased cholestatic enzymes (alkaline phosphatase increased from 66 to 137 U/L and GGT from 156 to 348 U/L), while the rest of the CMP and CBC was unremarkable.
A CT scan identified a new conglomerate of enlarged lymph nodes in the left neck extending to the left mediastinum constricting the jugular vein, carotid artery, trachea, and left lateral thyroid lobe. The size of the supraclavicular mass was 4 cm, which grew from 2.1 cm in a CT that was performed only 1 month earlier. (Figure 1C). Doppler ultrasound ruled out deep vein thrombosis. A biopsy from the supraclavicular mass was consistent with metastatic cholangiocarcinoma. Cardiac symptoms and shortness of breath were managed conservatively, with no administration of medications or oxygen. The patient refused radiotherapy and corticosteroids treatment. Within the next ten days the mass spontaneously diminished and respiratory symptoms resolved, physical examination revealed reduction of the mass, and blood tests returned to baseline values. A CT scan conducted 3 months following the acute presentation demonstrated that the supraclavicular lymphadenopathy subsided and the mass effect on the vasculature and trachea decreased to 3.1 cm.
Discussion
We describe a systemic reaction to Kambô, manifested as tachycardia, tachypnea, impaired liver cholestatic enzymes, and enlargement of lymphadenopathy mimicking disease progression. The clinical features and onset of symptoms, the rapid reaction, and the lack of other identified causes make the diagnosis of Kambô-induced SIRS highly probable. While the natural course of cholangiocarcinoma in the absence of therapy is progressive disease, the sudden onset of clinical symptoms, and radiological findings, concurrent with the Kambô ritual, together with the rapid resolution of lymphadenopathy and dyspnea suggests a clear causal relationship.
The reason for this unique localization of the lymphadenopathy is not clear, but is likely due to the application of the Kambô to the patient’s left arm, adjacent to the metastatic supraclavicular lymph nodes. Alternatively, Kambô may have provoked inflammation that is associated with the presence of tumor cells within the lymph node.
Nearly 35.9% (ranging from 14.8% to 73.1%) of European oncology patients have reported use of complementary and alternative medications, 10 yet half of all patients do not discuss alternative therapies with their physicians. 11 It appears that physicians play a small role in providing complementary and alternative medicine—related information. Patients often pursue these alternative regimens independently, in the absence of their oncologists’ guidance in weighing the potential side effects or medical interactions. These alternative therapies may cause adverse effects in 4.4% of patients. 10 Accordingly, the American Society of Clinical Oncology recommends integration of complementary medicine, such as acupuncture or mind-body techniques, for cancer patients experiencing pain or fatigue, but heeds against alternative agents which brand themselves are curative treatments of cancer.12,13
Patients should be encouraged to maintain an open dialogue with their clinicians regarding alternative or complementary treatments they may be considering. Moreover, oncologists must be aware and actively question patients regarding alternative therapies and weigh the benefits and potential harm. Additionally, physicians often encounter an absence of literature on alternative regimens. This case report calls for future studies examining standard oncological care such as chemotherapy, radiotherapy, and immunotherapy concurrent with alternative therapies. Additionally, greater awareness and physician education should be promoted, encouraging inquiry of oncology patients’ administration of alternative, complementary, and integrative medicine.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shira Peleg Hasson  https://orcid.org/0000-0002-3707-1107
https://orcid.org/0000-0002-3707-1107
Reference
- 1. Daly JW, Ware N, Saporito RA, Spande TF, Garraffo HM. N-methyldecahydroquinolines: an unexpected class of alkaloids from Amazonian poison frogs (Dendrobatidae). J Nat Prod. 2009;72:1110-1114. doi: 10.1021/np900094v [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lazarus LH, Attila M. The toad, ugly and venomous, wears yet a precious jewel in his skin. Progr Neurobiol. 1993;41:473-507. [DOI] [PubMed] [Google Scholar]
- 3. van Zoggel H, Hamma-Kourbali Y, Galanth C, et al. Antitumor and angiostatic peptides from frog skin secretions. Amino Acids. 2012;42:385-395. doi: 10.1007/s00726-010-0815-9 [DOI] [PubMed] [Google Scholar]
- 4. Pogorzelska J, Łapiński TW. Toxic hepatitis caused by the excretions of the Phyllomedusa bicolor frog – a case report. Clin Exp Hepatol. 2017;3:33-34. doi: 10.5114/ceh.2017.65228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Leban V, Kozelj G, Brvar M. The syndrome of inappropriate antidiuretic hormone secretion after giant leaf frog (Phyllomedusa bicolor) venom exposure. Toxicon. 2016;120:107-109. doi: 10.1016/j.toxicon.2016.07.007 [DOI] [PubMed] [Google Scholar]
- 6. Roy R, Baranwal A, Espiridion ED. Can overuse of Kambô cause psychosis? Cureus. 2018;10:e2770. doi: 10.7759/cureus.2770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li K, Horng H, Lynch K, Smollin CG. Prolonged toxicity from Kambo cleansing ritual. Clin Toxicol. 2018;56:1165-1166. doi: 10.1080/15563650.2018.1457153 [DOI] [PubMed] [Google Scholar]
- 8. Aquila I, Gratteri S, Sacco MA, et al. The biological effects of Kambo: is there a relationship between its administration and sudden death? J Forensic Sci. 2018;63:965-968. doi: 10.1111/1556-4029.13641 [DOI] [PubMed] [Google Scholar]
- 9. Daly JW, Caceres J, Moni RW, et al. Frog secretions and hunting magic in the upper Amazon: identification of a peptide that interacts with an adenosine receptor. Proc Nat Acad Sci. 1992;89:10960-10963. doi: 10.1073/pnas.89.22.10960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Molassiotis A, Fernández-Ortega P, Pud D, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16:655-663. doi: 10.1093/annonc/mdi110 [DOI] [PubMed] [Google Scholar]
- 11. Ambrosone CB, Zirpoli GR, Hutson AD, et al. Dietary supplement use during chemotherapy and survival outcomes of patients with breast cancer enrolled in a cooperative group clinical trial (SWOG S0221). J Clin Oncol. 2020;38:804-814. doi: 10.1200/JCO.19.01203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alternative vs. complementary medicine: navigating the difference. ASCO. Published November 2, 2017. Accessed September 22, 2020. https://www.asco.org/about-asco/press-center/cancer-perspectives/alternative-vs-complementary-medicine-navigating
- 13. Burstein HJ, Lacchetti C, Anderson H, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol. 2019;37:423-438. doi: 10.1200/JCO.18.01160 [DOI] [PubMed] [Google Scholar]