Abstract
Positive Psychological (PP) constructs (e.g., optimism and gratitude) may impact the adherence to healthy behaviors, including diet, though prior studies have shown mixed findings. This qualitative study explored the relationships between PP constructs and dietary behaviors among 21 adults with metabolic syndrome through semi-structured interviews. Directed content analysis led to five themes: eating healthfully leads to PP constructs, PP constructs lead to eating healthfully, eating healthfully prevents negative emotions, healthy behaviors associated with diet, and an upward healthy spiral. Given the close relationship between PP constructs and diet, these may be targeted to improve diet in risk populations through interventions that promote well-being.
Keywords: positive emotions, positive psychology, diet, obesity, qualitative research
Introduction
Metabolic syndrome (MetS) is a cluster of risk factors such as obesity, elevated blood pressure, and dyslipidemia affecting 35% of US adults (Alberti et al., 2009; Hirode and Wong, 2020; Sperling et al., 2015). It increases the risk of developing chronic diseases such as type 2 diabetes and cardiovascular disease (Alberti et al., 2009; Hirode and Wong, 2020; Sperling et al., 2015). Health behaviors, like following a healthy diet and maintaining a healthy weight, are critical for preventing progression to these chronic diseases. However, most people with MetS struggle to follow and maintain a healthy lifestyle (Fappa et al., 2008; Lakka and Laaksonen, 2007). Dietary recommendations for MetS and chronic disease prevention emphasize the consumption of fruits, vegetables, and lean proteins, as well as reduced consumption of sugar-sweetened beverages, processed foods, and fried foods (American Heart Association, 2016; Falk et al., 2001). Adherence to diets such as the plant-forward Mediterranean diet is inversely associated with the development of MetS and diabetes (Babio et al., 2009; Rodríguez-Monforte et al., 2017). Some people with chronic diseases may have a healthier diet, but one study showed that only 1.7% of people with chronic diseases consumed a high-quality diet (Chen et al., 2011). Thus, understanding factors that lead to a healthy diet and ultimately weight loss may help inform the development of effective dietary interventions for people at risk of developing chronic diseases.
Psychological factors have an important and complex influence on people’s adherence to healthy dietary behaviors (Firth et al., 2020; Macht, 2008). There are bidirectional relationships between emotional states and eating behavior (Bongers et al., 2013; Fedorikhin and Patrick, 2010; Jacka et al., 2017; White et al., 2013), with the majority of research focusing on negative psychological constructs. For example, it has been shown that people tend to overeat and eat more unhealthy food when experiencing negative psychological states such as stress or pessimism (Giltay et al., 2007; Pänkäläinen et al., 2018). Conversely, lower levels of stress are associated with higher consumption of healthy food (Whatnall et al., 2019).
However, the association between eating behaviors and PP constructs such as positive affect (experiencing positive emotions), optimism (positive expectations of the future), or life satisfaction, has received much less scientific attention (Firth et al., 2020), and the existing literature shows different results. On the one hand, some research has shown that healthy eating is associated with increased PP constructs. For example, healthy eating has been associated with improved mood, reduced stress, and may be associated with lower incidence of depression (Firth et al., 2020; White et al., 2013), and the consumption of fruit and vegetables seems to predict next-day positive affect in young adults (White et al., 2013). Other positive constructs such as optimism and resilience have been found to be positively associated with a healthy body weight, improved diet quality, less snacking, or higher consumption of healthy food such as fruits and vegetables (Ait-hadad et al., 2020; Hingle et al., 2014; Pänkäläinen et al., 2018).
Conversely, other studies have found that positive emotions and positive emotional states are associated with increased caloric intake; for example, in the context of socializing or celebration, which has implications for poorer diet quality (Bongers et al., 2013; Cardi et al., 2015; Evers et al., 2013, 2018). Given the differences in findings between PP constructs and diet (Evers et al., 2013), qualitative approaches are needed to help elucidate these different associations in greater depth.
Most prior research on PP constructs and diet have focused only on broad or general PP states (e.g., positive affect, resilience, or well-being) instead of specific positive experiences or emotions and often only in the general population (Blanchflower et al., 2013; Cardi et al., 2015; Evers et al., 2018; White et al., 2013). There have been no studies of specific PP constructs and diet in a chronic disease prevention context. Thus, there is a gap in the knowledge on how specific positive cognitions and emotions are related to diet and eating in people in a pre-disease state, as it would help to advance the understanding of chronic disease prevention interventions.
This study aims to expand the depth of knowledge about how PP constructs are associated with a healthy diet through a qualitative analysis among adults with MetS. It was expected that participants would share their experiences about their positive emotional experiences, draw associations between healthy diet and PP constructs, and identify emotion-based motivation for healthy eating.
Methods
Study criteria and recruitment
This was a qualitative analysis completed as part of the first phase of a multi-phase study to develop a positive psychology intervention for health behaviors in metabolic syndrome (Millstein et al., 2020b). A detailed description of recruitment and data collection methods have been previously published (Millstein et al., 2020a). Briefly, eligible patients were recruited from May 2017 to November 2017. Participants were primary care patients from outpatient clinics of an academic medical center who were willing to be contacted about research studies. Inclusion criteria were English-speaking adults with at least three risk factors for MetS based on the 2009 NCEP guidelines (Alberti et al., 2009) who did not meet US physical activity recommendations [<150 min of moderate to vigorous physical activity in the last week (Piercy et al., 2018)] measured by the International Physical Activity Questionnaire-Short Form [IPAQ-SF (Lee et al., 2011)]. Exclusion criteria were having cognitive deficits measured by a 6-item screener (Callahan et al., 2002), having a physical condition likely to lead to death within the next 6 months, and not having access to a telephone. Gender was used as the stratified sampling variable to represent the distribution of MetS prevalence (50% men and women). Interviews were conducted until thematic saturation was reached within each gender stratum, which determined the sample size (Saunders et al., 2018). All contact with participants was done by phone, including the interviews.
Purposeful sampling (Palinkas et al., 2015) was used to identify people who were willing to share their opinions and experience of their chronic conditions. Of the 72 opt-out letters sent, 32 participants were reached and screened by phone. Of those screened, 27 were eligible, and 23 were interested in proceeding. Of the 23 scheduled interviews, two participants dropped out, for a final sample of 21 completed interviews. All participants signed an informed consent form. All study procedures were approved by the healthcare system’s Institutional Review Board.
Qualitative interviews
Semi-structured interviews were designed to ask participants about their perceptions of health behaviors including diet, PP constructs, and the relationship between the two. We aimed at eliciting and identifying the perceptions of this population about specific PP constructs and to explore perceptions of the directionality of the relationships between those constructs and healthy eating (e.g., Does healthy eating lead to an increase in PP constructs? Do PP constructs lead to following a healthier diet?). All interviews were conducted by telephone, a common method of data collection (Drabble et al., 2016) by the principal investigator (RM) from June through November 2017. A semi-structured interview guide was created prior to beginning the interviews, based on the goals of the study and prior qualitative research on PP constructs in chronic disease populations (Huffman et al., 2016). The interview guide was refined based on input from the study’s qualitative research expert (EP). The interview asked participants about their experiences with their chronic conditions, including their perceptions of how positive and negative emotions affected their health and health behaviors [see (Millstein et al., 2020a) for additional details]. For the present analysis, we focused on emotions related to diet and eating behaviors. Participants were asked pre-specified interview questions related to their emotional experiences and eating behaviors and were asked additional questions (probes) about specific positive emotions when needed to clarify responses.
The interviews were 45–60 minutes long and were audiotaped and then professionally transcribed. Transcripts were reviewed by the principal investigator for accuracy and completeness. Participants were paid US$100 to complete the interview and self-report questionnaires (not included in the present analysis).
Qualitative analysis
Transcribed interviews were uploaded into Dedoose, a web-based qualitative research program, for data management and content analysis. Prior to conducting the analysis, a coding framework was developed and iteratively refined based on input from the team’s qualitative research expert (EP), participant data, and coders’ feedback. The framework and data analysis were based on directed content analysis following the Consolidated Criteria for Reporting Qualitative Research (COREQ) framework (Tong et al., 2007). Directed content analysis uses a framework derived from research literature and theory but allows for themes to emerge from the data during coding (Elo and Kyngäs, 2008). Coding was conducted using inductive and deductive methods. Codes were developed based on prior literature, and new themes were added based on the raw data during coding and team consensus. Two different trained raters (AC, EF, and LH) coded each interview independently using the codebook, with oversight from the principal investigator (RM). Weekly meetings from May 2020 to July 2020 with raters and the principal investigator were held to discuss emerging themes and resolve any coding discrepancies. Discrepancies were resolved together with the coders and the principal investigator. The present analysis focuses on one of the interview’s domains: PP constructs associated with a healthy diet and their bidirectional relationships. Results from other interview domains have been previously published (Millstein et al., 2020a). Within the domain of “diet and emotions,” there were eight primary (parent) themes in the codebook and 11 child nodes.
Results
Descriptive statistics
Twenty-one interviews were completed. Participants were mostly older adults (mean age 63.1, SD: 9.7), and over half (62%) were female. All of them had obesity (mean BMI 33.5 m/kg2, SD: 2.8), 90.4% had hyperlipidemia, 66.7% had insulin resistance, and 90.4% had hypertension. See (Millstein et al., 2020a) for additional sample descriptive statistics.
Qualitative results
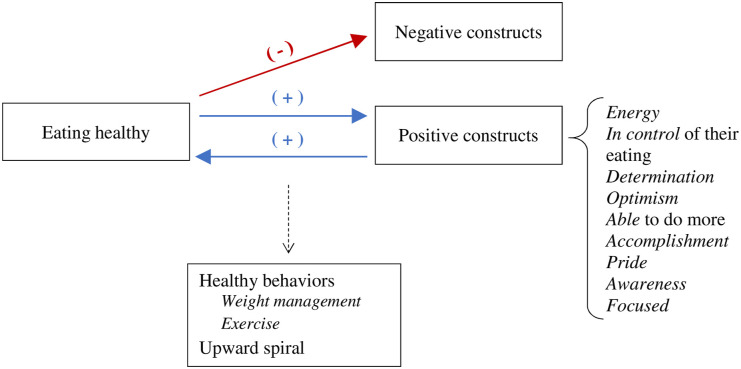
Results emerged in four main themes, which are detailed below: (1) eating a healthy diet leads to PP constructs, (2) PP constructs lead to eating more healthfully, (3) eating a healthy diet prevents negative emotions, (4) healthy behaviors (weight management and exercise) that participants associate with diet, and (5) the presence of an upward healthy spiral of behaviors can help participants follow a healthy diet. Main results are summarized in Figure 1.
Figure 1.
Schematic diagram of the overall qualitative results depicting the relationships between eating healthfully and emotional experiences, and their bidirectional relationships.
Theme 1. Eating a healthy diet leads to PP constructs. Most participants expressed a connection between diet and PP constructs, and in particular, a directional relationship such that eating more healthfully led to PP constructs. Participants noted that eating healthier helped them to feel better overall. For example, “I feel like for the most part it was eating better that brought about the positive emotions.” (female, 60), and “I felt pretty terrific [when I ate better…] and things were good.” (female, 55). These general mentions of positive emotions or feeling better often led to a more in-depth discussion of specific positive emotions experienced in the context of eating better or trying to change one’s diet.
When they were asked about their emotional experiences related to healthy eating, participants expressed a diversity of specific PP constructs. Most commonly, they stated that healthy eating led them to feel more energy. For example, “I like the energy it gives me. I like the fact that I can jump around a lot more and play with my dog a lot more.” (female, 79). Next most commonly mentioned was the feeling of being in control of their eating: “I like the way it makes me feel. And when I’m in control, really good control. […] That’s a good, good feeling physically and mentally too.” (female, 79). Determination to have a healthy diet was another positive construct that emerged; for example, “I want to be healthy. And I want to be functioning as a normal human being. And I don't want to be in any way affected by diabetes or by anything else. So, this is my time to do it. It’s what I want to do, and I’m going to do it.” (female, 69). Optimism also came up as a positive construct that was associated with healthy eating; for example, “I’m optimistic that I’m going to beat this [metabolic syndrome]. I am.” (male, 70). The idea of being able to do more as a consequence of eating better was also a positive construct for some participants, such as, “I feel better. […] Able to do more things. Keep up with my young grandchildren.” (female, 72). Additional positive emotional experiences were expressed by fewer participants. Accomplishment: “Well, it feels good to make that selection, eat it, and know you made a healthy choice. It’s a sense of accomplishment […] (male, 64). Pride in sticking with one’s diet goals: “I think I’m on my way to doing it right for about the first time. I mean, I didn’t cheat ever, even if we went out.” (female, 69). Awareness: “Yeah, definitely the awareness, and knowing what’s going on, and knowing doing this will prevent this or eating this kind of food will help with this.” (male, 47). Finally, for the construct of focus, which in this case was also related to having energy: “But I noticed that when I have just good stuff [food] that maybe a little more energy, a little more focused.” (male, 47).
Theme 2: PP constructs lead to eating more healthfully. Almost half of participants stated a clear directionality such that they experienced positive emotions as leading to eating more healthfully. These participants expressed that feeling positive constructs led them to eat healthier or prepare healthy food. One participant connected positive emotions with healthy eating via cooking: “And when you’re in a positive mood, you’re in the mood to cook and make things the way they should be made.” (female, 69). Another mentioned a general positive directional association: “Yeah. If I’m feeling great, chances are I’ll eat better.” (male, 62). One participant contrasted her experiences of negative versus positive emotional experiences with respect to awareness of healthy eating: “Oh, sure. When you’re negative, you tend to reach for that ice cream [laughter]. But when you’re positive, you’re kind of more aware of what you’re eating.” (female, 72). And yet another noted that feeling more positively allowed for greater ease in making healthy choices: “And when I am feeling good or positive, it is a little bit easier to make healthy choices. Like obviously, when you’re feeling good, you might have a drink when you go out or you might have a dessert, but not like bingeing on something.” (female, 39).
In these quotes, participants were able to describe their perceptions of the role of positive emotions in helping them make healthy choices with regard to their eating, preparing healthy food, or staying in control when faced with potentially challenging eating situations. Not everyone made this connection with directionality, and it was less common than the direction of eating well leading to positive emotions. It emerged more commonly in response to a probe than spontaneously, indicating that people are less aware of this direction of the relationship between emotions and healthy eating.
Theme 3. Eating a healthy diet prevents negative emotions. Even when asked specifically about positive emotions, participants frequently mentioned negative emotions—or the avoidance of them—in relation to eating. For example, when they were asked whether feeling better helped them to eat more healthfully, a participant stated, “It does. [It seems] to kick in the memory of not feeling good, quicker and to not just go into automatic pilot again.” (female, 79). Another said, “I think so. I mean, to me, it’s always been positive feedback until something interrupts that. Whether it’s an illness, or stress.” (female, 39). More specifically, some participants talked about how following a healthy diet might lead them to avoid feeling negative emotions such as shame or self-incrimination around eating. Some examples about how eating healthfully might prevent the negative emotion of guilt are: (Q: What do you like about eating healthier?) “Well, probably the lack of guilt about eating badly [laughter] would be one thing.” (male, 59), and “I don't feel like I ran around being guilty a lot, you know. Because I certainly don't forbid myself of things but I don't gorge on things […].” (male, 57). As displayed by these quotes, we can see that often participants’ first response to the idea of eating healthier is that it prevents guilt or associated negative emotions, or that a negative event set them off course with their eating. This is notable because the questions did not include the concept of negative emotions around eating, but they appear to be highly salient for some participants.
Theme 4. Healthy behaviors. Even when participants were only asked about diet and emotions, closely related topics like exercise and weight management emerged in their responses. Participants expressed how emotions and a healthy diet were related through third (interrelated) variables. With regard to weight, participants often spoke about the topics of diet and weight simultaneously. Some participants mentioned that eating healthfully would result in better or worse weight management, which in turn, would produce positive or negative emotions. Some examples are “Yeah. I mean, if you stick to your diet and you’re doing well and you’re losing weight, it’s fabulous. It’s great. You’re on the road and you’re on your way to achieving your goal. What the frustrating thing is that even when you’re—[…]. I weigh myself every morning. So when you’ve lost the weight, it’s great. Even though you’re being good and you didn’t lose the weight that particular day, it’s either a neutral or a little bit of a downer.” (female, 76), and “I know that if I didn’t do carrying on a good diet, my weight would become a problem. And then, that, mentally, that would definitely become depressing for me. If I really start to put on a lot-- if I didn’t watch my diet and I really start to put on a lot of weight, to me, that would just be depressing. To me, that would constitute failure.” (male, 54). Related to exercise, some participants expressed that the relationship between diet and emotions was mediated by or co-occurred with exercise: they felt more positively as a consequence of doing exercise, and this, in turn, led to following a healthier diet. This can be seen in examples such as “Once I start doing a kind of exercise routine […], my whole eating habits changed to a healthier side without consciously saying, ‘I need to eat better to lose weight’. […] I tend to eat better when I do some form of exercise regularly. I even crave different kinds of food. So I will crave salads more. I’ll look for a piece of fish and not a piece of steak just from doing the exercise.” (male, 64), and “In other words, if I had done a lot of exercise, I wouldn’t want to go and eat something really unhealthy and undo the positive.” (male, 59)
Theme 5. Starting an upward spiral of healthy behaviors. In terms of how positive emotions may lead to a better diet, some participants talked about how eating healthfully was easier once they were already in a healthy cycle or routine. That is, instead of being triggered by a positive state, a behavioral cycle or having momentum helped them to adhere to a healthier diet. Some examples are “If I can screw my brain in right. I mean, if I can focus properly. Right now I’m in a very good place. So every morning I have toast and coffee. Then I come to the beach where I am right now and I walk. If I do that every day, if I can discipline myself to do that every day, I’d be a thin person. […].” (female, 76), and “Oh, I felt better. I slept better at night. It’s everything. Your whole life is different. You’re more active, you can-- if you’re sitting down and you’ve got to get up, you just jump up.” (male, 70). When discussing healthy eating, these participants noted that they experience behavioral bundling, such that their lifestyle improvements happen together and allow them to continue to eat in a way that can improve their health.
Discussion
This qualitative study explored how people at high risk of developing chronic diseases perceived PP constructs to be associated with eating, and vice-versa. When sharing their personal experiences, most participants stated that eating healthy made them feel better in some way (e.g., feeling better overall, having more energy, optimism, or determination). Though less readily accessible, some participants articulated how feeling more positively led to eating better. For many, even when asked about positive experiences, negative emotions were easier to access, and diet or weight were very closely related to negative emotions. We also found that in the context of considering their diets, participants concurrently thought about the role of physical activity, weight, and health behaviors overall. This finding speaks to the idea of behavioral bundling or complementary behaviors, in a way in which participants can initiate or maintain chains of health behaviors together, including following a healthy diet.
When it came to the relationship between eating a healthy diet and positive emotions, our findings are in line with prior literature in the direction that eating healthy food such as vegetables and fruits is associated with positive constructs such as positive affect, happiness or vitality (Conner et al., 2017; Mujcic and Oswald, 2016). However, there is a limited body of literature on the association between eating healthfully and specific associated PP constructs, and on how these relationships may be working in people with MetS. This study adds a nuanced perspective on the different types of PP constructs that people feel when following a healthy diet. We specifically derived themes of PP constructs like energy, determination, feeling in control of their eating, optimism, being able to do more, accomplishment, pride, awareness, and focus. As previously stated, emotions have an impact on one’s habits and adherence to health behaviors (Evers et al., 2013), and especially for people with MetS, prevention in the form of health behavior adherence is particularly important. Here we demonstrate that healthy eating is associated with many specific positive emotions and that positive emotions can start or be part of a chain of healthy behaviors including eating. This is noteworthy as, in research, positive emotions receive less attention than negative emotions, and people can describe negative emotions more easily than the positive ones (Baumeister et al., 2001).
In the opposite direction, some participants noted that positive emotions led to or were associated with eating healthier. Participants expressed that feeling more positively helped them eat more healthfully, which is in line with previous research (Ait-hadad et al., 2020; Hingle et al., 2014; Pänkäläinen et al., 2018; Whatnall et al., 2019). Optimism, in particular, has received special attention with regard to this topic, and it has been found that this construct is associated with the consumption of healthier food (Ait-hadad et al., 2020; Boehm et al., 2018; Hingle et al., 2014; Kelloniemi et al., 2005). It is possible that positive thoughts and feelings increase participants’ thought-action repertoires allowing them to build additional resources to eat healthfully (Fredrickson, 2004), such as cooking new recipes or shopping for healthy food. For example, participants who ate healthfully may have experienced greater feelings of self-efficacy and perceived control (e.g., the present themes of “feeling in control” and “accomplishment”), which then promoted self-monitoring and the use of active coping strategies (e.g., themes of “awareness” or feeling “focused”), enhanced their social interactions (through the theme of feeling more “energy” or body image/confidence to socialize), and increased their self-regulation and motivation (feelings of “accomplishment,” “optimism,” or “determination”), thus promoting adherence to a healthy diet (Huffman et al., 2016). Additionally, some participants expressed that being in an “upward spiral” of multiple healthy behaviors helped them to eat healthfully. This is consistent with prior research which has demonstrated that participants are more likely to maintain healthy habits (e.g., eating healthfully) when they perceive positive emotions during the activity (Van Cappellen et al., 2018). Our results show that, for some, this positive reinforcement can occur for eating but also broadly, across multiple health behaviors. For some participants, the relationship between diet and emotions seemed to co-occur with at least one of three variables: weight management, exercise, or being involved in a broader cycle or chain of healthy habits. It is noteworthy that participants were able to draw complex relationships between such variables without being prompted, among which the relationship between weight and negative emotions was prominent. Indeed, all of these variables could be related to self-regulating behaviors (Huffman et al., 2016).
Limitations
First, this qualitative study was designed to gain in-depth and nuanced perceptions from a small number of participants who were mostly white. As such, these results may not be generalizable to a larger and more heterogeneous population. However, next step studies can confirm these findings using larger quantitative analyses. Second, this analysis of the interviews was only focused on the positive experiences of the participants, which was the study objective. However, exploring negative emotional constructs was outside the scope of this analysis, and its exclusion could have left out some relevant emotional experiences related to diet.
Future directions
Helping people at high risk of developing chronic diseases recognize and cultivate positive emotions may help them improve their adherence to a healthy diet. In this context, PP interventions can be especially useful. Such interventions are comprised of relatively simple activities that are aimed at cultivating positive emotions, thoughts, and behaviors (Seligman et al., 2005). These interventions could help populations at risk of developing chronic diseases become more aware of and to be able to cultivate their positive emotions. This, in turn, could potentially have beneficial effects on their health behaviors (Huffman et al., 2016). Future studies should focus on bolstering specific psychological constructs as a way to help people improve their diet quality and self-perceptions related to diet, physical activity, and weight. As such, future studies should also focus on enhancing participants’ experiences of PP constructs when engaging in health behaviors including diet.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was registered at clinicaltrials.gov (NCT# 03160755). Funding for this study was provided by NIH award number K23HL135277 to (Rachel Millstein). Time for manuscript preparation was provided by NIH award number K23HL148017 to (Emily Feig).
Data availability: Data from this qualitative study may be shared upon request to the authors.
ORCID iDs
Emily H Feig https://orcid.org/0000-0001-6152-0526
Lauren E Harnedy https://orcid.org/0000-0002-3636-7088
Rachel A Millstein https://orcid.org/0000-0003-2196-4557
References
- American Heart Association (2016) Prevention and Treatment of Metabolic Syndrome. Available at: https://www.heart.org/en/health-topics/metabolic-syndrome/prevention-and-treatment-of-metabolic-syndrome
- Ait-hadad W, Bénard M, Shankland R, et al. (2020) Optimism is associated with diet quality, food group consumption and snacking behavior in a general population. Nutrition Journal 19(1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberti KG, Eckel RH, Grundy SM, et al. (2009) Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 120(16): 1640–1645. [DOI] [PubMed] [Google Scholar]
- Babio N, Bulló M, Basora J, et al. (2009) Adherence to the mediterranean diet and risk of metabolic syndrome and its components. Nutrition, Metabolism and Cardiovascular Diseases 19(8): 563–570. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Bratslavsky E, Finkenauer C, et al. (2001) Bad is Stronger than Good. Review of General Psychology 5(4): 323–370. [Google Scholar]
- Blanchflower DG, Oswald AJ, Stewart-Brown S. (2013) Is psychological well-being linked to the consumption of fruit and vegetables? Social Indicators Research 114(3): 785–801. [Google Scholar]
- Boehm JK, Chen Y, Koga H, et al. (2018) Is optimism associated with healthier cardiovascular-related behavior? Circulation Research 122(8): 1119–1134. [DOI] [PubMed] [Google Scholar]
- Bongers P, Jansen A, Havermans R, et al. (2013) Happy eating. the underestimated role of overeating in a positive mood. Appetite 67: 74–80. [DOI] [PubMed] [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, et al. (2002) Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care 40(9): 771–781. [DOI] [PubMed] [Google Scholar]
- Cardi V, Leppanen J, Treasure J. (2015) The effects of negative and positive mood induction on eating behaviour: a meta-analysis of laboratory studies in the healthy population and eating and weight disorders. Neuroscience and Biobehavioral Reviews 57: 299–309. [DOI] [PubMed] [Google Scholar]
- Chen X, Cheskin LJ, Shi L, et al. (2011) Americans with diet-related chronic diseases report higher diet quality than those without these diseases. The Journal of Nutrition 141(8): 1543–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner TS, Brookie KL, Carr AC, et al. (2017) Let them eat fruit! The effect of fruit and vegetable consumption on psychological well-being in young adults: a randomized controlled trial. Plos One 12(2): e0171206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drabble L, Trocki KF, Salcedo B, et al. (2016) Conducting qualitative interviews by telephone: lessons learned from a study of alcohol use among sexual minority and heterosexual women. Qualitative Social Work 15(1): 118–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo S, Kyngäs H. (2008) The qualitative content analysis process. Journal of Advanced Nursing 62(1): 107–115. [DOI] [PubMed] [Google Scholar]
- Evers C, Adriaanse M, de Ridder DTD, et al. (2013) Good mood food. positive emotion as a neglected trigger for food intake. Appetite 68: 1–7. [DOI] [PubMed] [Google Scholar]
- Evers C, Dingemans A, Junghans AF, et al. (2018) Feeling bad or feeling good, does emotion affect your consumption of food? A meta-analysis of the experimental evidence. Neuroscience and Biobehavioral Reviews 92: 195–208. [DOI] [PubMed] [Google Scholar]
- Falk LW, Sobal J, Bisogni CA, et al. (2001) Managing healthy eating: definitions, classifications, and strategies. Health Education & Behavior 28(4): 425–439. [DOI] [PubMed] [Google Scholar]
- Fappa E, Yannakoulia M, Pitsavos C, et al. (2008) Lifestyle intervention in the management of metabolic syndrome: could we improve adherence issues? Nutrition 24(3): 286–291. [DOI] [PubMed] [Google Scholar]
- Fedorikhin A, Patrick VM. (2010) positive mood and resistance to temptation: the interfering influence of elevated arousal. Journal of Consumer Research 37(4): 698–711. [Google Scholar]
- Firth J, Gangwisch JE, Borisini A, et al. (2020) Food and mood: how do diet and nutrition affect mental wellbeing? Bmj: British Medical Journal 369: m2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL. (2004) The broaden–and–build theory of positive emotions. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences 359(1449): 1367–1377. doi: 10.1098/rstb.2004.1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giltay EJ, Geleijnse JM, Zitman FG, et al. (2007) Lifestyle and dietary correlates of dispositional optimism in men: the Zutphen elderly study. Journal of Psychosomatic Research 63(5): 483–490. [DOI] [PubMed] [Google Scholar]
- Hingle MD, Wertheim BC, Tindle HA, et al. (2014) Optimism and diet quality in the women’s health initiative. Journal of the Academy of Nutrition and Dietetics 114(7): 1036–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirode G, Wong RJ. (2020) Trends in the prevalence of metabolic syndrome in the United States, 2011-2016. Jsls: Journal of the Society of Laparoendoscopic Surgeons 323(24): 2526–2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, DuBois CM, Mastromauro CA, et al. (2016) Positive psychological states and health behaviors in acute coronary syndrome patients: a qualitative study. Journal of Health Psychology 21(6): 1026–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacka FN, O'Neil A, Opie R, et al. (2017) A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Medicine 15(1): 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelloniemi H, Ek E, Laitinen J. (2005) Optimism, dietary habits, body mass index and smoking among young finnish adults. Appetite 45(2): 169–176. [DOI] [PubMed] [Google Scholar]
- Lakka TA, Laaksonen DE. (2007) Physical activity in prevention and treatment of the metabolic syndrome. Applied Physiology, Nutrition, and Metabolism 32(1): 76–88. [DOI] [PubMed] [Google Scholar]
- Lee PH, Macfarlane DJ, Lam TH, et al. (2011) Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. International Journal of Behavioral Nutrition and Physical Activity 8: 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macht M. (2008) How emotions affect eating: a five-way model. Appetite 50(1): 1–11. [DOI] [PubMed] [Google Scholar]
- Millstein RA, Huffman JC, Thorndike AN, et al. (2020. a) How do positive psychological constructs affect physical activity engagement among individuals at high risk for chronic health conditions? A qualitative study. [Epub ahead of print 2020/09/06] Journal of Physical Activity & Health. DOI: 10.1123/jpah.2019-0295. 1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millstein RA, Thorndike AN, Kim S, et al. (2020. b) A community-based positive psychology group intervention to promote physical activity among people with metabolic syndrome: Proof of concept results to inform a pilot randomized controlled trial protocol. Contemporary Clinical Trials Communications 19: 100626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mujcic R, Oswald AJ. (2016) Evolution of well-being and happiness after increases in consumption of fruit and vegetables. American Journal of Public Health 106(8): 1504–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palinkas LA, Horwitz SM, Green CA, et al. (2015) Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health 42(5): 533–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pänkäläinen M, Fogelholm M, Valve R, et al. (2018) Pessimism, diet, and the ability to improve dietary habits: a three-year follow-up study among middle-aged and older finnish men and women. Nutrition Journal 17(1): 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piercy KL, Troiano RP, Ballard RM, et al. (2018) The physical activity guidelines for Americans. Jama 320(19): 2020–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Monforte M, Sánchez E, Barrio F, et al. (2017) Metabolic syndrome and dietary patterns: a systematic review and meta-analysis of observational studies. European Journal of Nutrition 56(3): 925–947. [DOI] [PubMed] [Google Scholar]
- Saunders B, Sim J, Kingstone T, et al. (2018) Saturation in qualitative research: exploring its conceptualization and operationalization. Quality & Quantity 52(4): 1893–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman ME, Steen TA, Park N, et al. (2005) Positive psychology progress: empirical validation of interventions. American Psychologist 60(5): 410–421. [DOI] [PubMed] [Google Scholar]
- Sperling LS, Mechanick JI, Neeland IJ, et al. (2015) the cardiometabolic health alliance. Journal of the American College of Cardiology 66(9): 1050–1067. [DOI] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, Craig J. (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care 19(6): 349–357. [DOI] [PubMed] [Google Scholar]
- Van Cappellen P, Rice EL, Catalino LI, et al. (2018) Positive affective processes underlie positive health behaviour change. Psychology & Health 33(1): 77–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whatnall MC, Patterson AJ, Burrows TL, et al. (2019) Higher diet quality in university students is associated with higher academic achievement: a cross‐sectional study. Journal of Human Nutrition and Dietetics 32(3): 321–328. [DOI] [PubMed] [Google Scholar]
- White BA, Horwath CC, Conner TS. (2013) Many apples a day keep the blues away - daily experiences of negative and positive affect and food consumption in young adults. British Journal of Health Psychology 18(4): 782–798. [DOI] [PubMed] [Google Scholar]