Abstract
Objectives:
The study examined the differentials in prevalence and correlates on the uptake of tetanus toxoid and intermittent preventive treatment of malaria among pregnant women in The Gambia.
Methods:
The 2018 data from The Gambia Multiple Indicators Cluster Survey were analyzed. Data from 6143 women of reproductive age who have given birth were extracted for the analysis. Percentages and Chi-square tests were used. In addition, a multivariable logistic regression model was used to calculate the adjusted odds ratios (with a corresponding 95% confidence interval). The level of significance was set at p < 0.05.
Results:
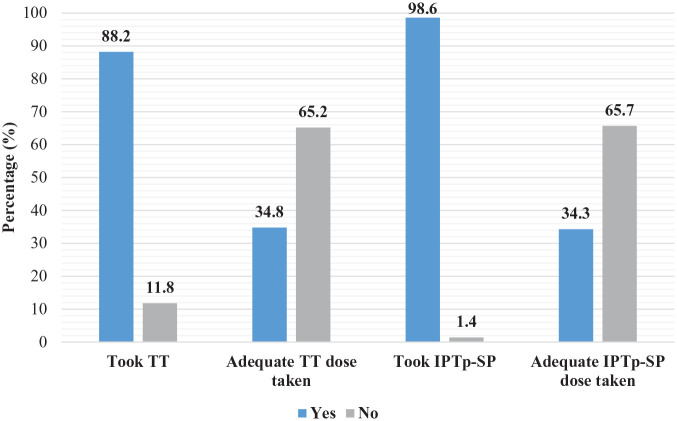
The prevalence of tetanus toxoid uptake among women in The Gambia was 88.2%, while that of the adequate tetanus toxoid doses was 34.8%. The prevalence of intermittent preventive treatment with sulfadoxine-pyrimethamine uptake among maternal women in The Gambia was 98.6%, while that of the adequate intermittent preventive treatment with sulfadoxine-pyrimethamine doses taken was 34.3%. The identified statistically significant covariates of tetanus toxoid immunization and intermittent preventive treatment with sulfadoxine-pyrimethamine uptake includes women’s age, local government areas, parity, use of radio, use of newspaper, and antenatal care visits.
Conclusion:
The current utilization rate for adequate intermittent preventive treatment with sulfadoxine-pyrimethamine and tetanus toxoid immunization during pregnancy in The Gambia is very low and even below universal levels. The country needs to strengthen more and effective mass media advocacy programs that would target both rural and urban populace, and motivate maternal women to ensure adequate vaccination against malaria and tetanus.
Keywords: Malaria, Gambia, immunization, intermittent preventive treatment with sulfadoxine-pyrimethamine, pregnant women
Introduction
Malaria remains a huge public health challenge for the existing healthcare systems, which results in an escalated burden of maternal and under-5 years morbidities and mortalities in sub-Saharan Africa.1–3 The five common Plasmodium species that caused malaria through the bites of infected female anopheles mosquitoes in humans include Plasmodium falciparum, Plasmodium ovale, Plasmodium vivax, Plasmodium knowlesi and Plasmodium malariae.4,5 Malaria is a parasitic infection transmitted by mosquitoes and is relatively the most fatal infectious disease with yearly mortalities of more than one million. 6 Globally, an estimated 228 million cases of malaria occurred in 2018 as compared with 251 million cases in 2010 and 231 million cases in 2017. 5 According to World Health Organization (WHO), 5 the African region constituted approximately 213 million or 93% of the total malaria cases, and 94% of global malaria deaths in 2018, with Nigeria and the Democratic Republic of Congo, accounted for 25% and 15%, respectively. Evidence from epidemiological studies suggested that malaria and tetanus in pregnancy remain a public health concern for decades causing maternal, fetal, and infant morbidities and mortalities, especially in low- and middle-income countries (LMICs).7–11 Approximately 125 million pregnancies occur globally and are at risk of malarial infection each year. 8
Susceptibility to malaria is higher in antenatals than the general population and are more likely to be infected, recur, causing severe complications, and to die as a result of the disease. 6 Some of the documented complications of malaria during pregnancy include anemia, fetal growth retardation, intrauterine death, miscarriages, low-birth-weight neonates, neonatal death, premature delivery, severe anemia, hypoglycemia, fetal distress, premature labor, acute pulmonary edema, spontaneous abortions, and maternal death.7,9 Thus, pregnant women are the most affected groups accounting for about 11 million cases and 16% (872,000) children with low birth weight at delivery due to malaria in West Africa. 5
To prevent, protect, and reduce women transmission of malaria in Africa, WHO recommended interventions that include sleeping under insecticide-treated bednets (ITNs), 12 prompt diagnosis and treatment of confirmed infection, indoor residual spray with insecticides, 13 and use of at least three doses of intermittent preventive treatment in pregnancy with sulfadoxine-pyrimethamine (IPTp-SP) from the second trimester (first antenatal care (ANC) visit) until delivery.5,14 Countries including The Gambia that experience stable malaria transmission were recommended by WHO to adopt the policy on the use of IPTp-SP prophylactic treatment to help mitigate the complications of malaria during pregnancy.15,16 In 2016, across the 23 African countries surveyed on IPTp coverage levels, an estimated 19% of eligible antenatal mothers reported receiving the WHO recommended three or more doses of IPTp, compared with 18% in 2015 and 13% in 2014. 17 Many countries, including The Gambia, have adopted this policy and poor implementation was observed in some studies.12,13,16,18
In the 1970s, WHO recommended the introduction of tetanus toxoid (TT) vaccination in the expanded program immunization services with the motive of protecting pregnant mothers and their unborn fetuses against tetanus.19,20 The initial global target to eliminate tetanus by 2005 set by WHO was not attained since the burden in the number of maternal and neonatal mortality continues to increase worldwide. 21 Tetanus-related mortality accounted for 180,000 lives each year, while neonatal tetanus (NT) accounted for 14% of the neonatal deaths and maternal tetanus (MT) constituted 5% of maternal deaths in LMICs. It was also estimated that 15,000–30,000 women die annually as a result of contracted tetanus during or immediately after pregnancy mostly in Africa, East, and Southern Asia.21,22 Studies have suggested that the uptake of TT and IPTp-SP is influenced by women’s level of education, age, residency, wealth index, timing of initial ANC visits, parity, mass media use, stockouts of commodity, and proximity to health facilities from home, and there is no natural immunity against tetanus.6,22–25 In rural areas where most deliveries take place under unsanitary conditions and in homes where substandard prenatal and postnatal child care prevails, NT is particularly frequent and dangerous. Most infected children do not survive or have profoundly weakening results. 26
In The Gambia, 97.4% of maternal women attend ANC at least once during pregnancy. 27 Almost half of the pregnant women visit at least 4 times and about 25% reported having their first ANC visits before 20 weeks of their pregnancy.28–30 Despite this high level of contact with health facilities and the provision of free IPTp, coverage for two or more IPTp doses among women aged 15–49 was 75.2%, with little difference between urban and rural areas. 27 We extracted secondary data from the latest multiple indicator cluster survey (MICS), which was conducted in The Gambia in 2018. There is little evidence on the known factors that influence the utilization of IPTp-SP and TT while seeking ANC services among pregnant women in The Gambia. Thus, this article would have a considerable influence in guiding policymaking on the prevention and control of malaria in pregnancy. This study’s objective was, therefore, to assess the prevalence and correlates of IPTp-SP and TT immunization uptake with ANC use among pregnant women in The Gambia.
Methods
Data extraction
Secondary data from The Gambia MICS 2018 were used. 27 The data from 6143 women of reproductive age who have given birth were extracted for the analysis with a response rate of 95.4% of the original survey size of 13,640 women (age 15–49 years). 27 The Gambia MICS carried out in 2018 provided the opportunity to strengthen the national statistical capacity by providing technical guidance on the quality of survey information, statistical tracking, as well as data collation and analysis. The MICS ensures the measurement of key pointers which countries depend upon to generate data that are used in policy formulations and program planning to monitor their progress in achieving the sustainable development goals, as well as the national development plan (NDP) of The Gambia and other international commitments which the country is a signatory to. The contribution of the MICS on the strengthening of The Gambian’s improvement on data and systems monitoring and the provision of technical expertise in the design, implementation, and analysis of such systems. The major reason for the development of the MICS program by the United Nations Children’s Fund (UNICEF) was to assist countries in internationally comparable data collection on an extensive variety of indicators ranging from data on children to that of women.
Study design and sampling strategy
The Gambia MICS 2018 is a cross-sectional stratified survey designed to provide nationally representative estimates for children and women across local government areas (LGAs): Banjul, Kanifing, Brikama, Mansakonko, Kerewan, Kuntaur, Janjanbureh, and Basse. The urban and rural areas in each LGA have been designated as the principal sampling stratum. A two-stage sampling technique for the systemic selection of households was applied. The first step randomly selected enumeration areas (EAs), and clusters from each substratum were probability proportionate to the size of the 390 EAs identified in the MICS. 27 A systemic sample of 20 households was obtained in each enumeration area following household listing in the designated enumeration areas. During the fieldwork period, all the selected EAs were visited.
This was the sixth round of MICS for The Gambia conducted by The Gambia Bureau of Statistics with technical support from UNICEF. A comprehensive sampling frame, error estimates, and allocation in their weighted forms as clearly presented in Appendix A of The Gambia MICS 2018 report from page 424 to 431. 27 Several other published articles only and briefly described the section as shown in several studies in The Gambia.31–33
Variable selection and measurement
Outcome variables
The two dependent variables used for this study are not in variance with the previous study. 6 These two variables were uptake of TT and Fansidar (SP) during their last pregnancy. The question that participants were asked was whether or not they took TT vaccination and used IPTp-SP during their last pregnancy. Based on WHO recommendation, a minimum of (at least two doses) of TT was defined as adequate, and (at least three doses) of IPTp-SP were also determined as adequate. Below those values are regarded as inadequate doses for both IPTp-SP and TT. Thus, doses that are less than those stated above were considered inadequate.
Explanatory variables
The maternal age was grouped as (15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49 years); residency: urban versus rural; LGA: Banjul, Kanifing, Brikama, Mansakonko, Kerewan, Kuntaur, Janjanbureh, Basse; education level: none, primary, secondary+; ethnicity: Mandinka, Wollof, Fula, Jola, Sarehule, Others, Non-Gambian; household wealth status: poorest, second, middle, fourth, richest; parity: 0–3, 4, and above; reading newspaper: do not use, few days a week, almost every day; listening to the radio: do not use, few days a week, almost every day; watching TV: do not use, few days a week, almost every day; ANC visits: less than five, five, and above; and currently pregnant: yes versus no. These inclusions of variables were as a result of the examined factors associated with the utilization of IPTp-SP and TT vaccination in previous studies.6,23
Ethical consideration
The original survey was conducted after being ethically approved by The Gambia Government Joint Research Ethics Committee (Ref. No: SCC1570v1.1). Before analysis, we obtained permission from The Gambia Bureau of Statistics and MICS program to access the dataset. The issue of privacy of the respondents was considered such that exclusive information such as respondents’ locations and their names as collected during the MICS interviews were consciously removed from datasets. It is also on record that participants’ consent was obtained either through signing or thumbprinted before their participation in the survey. For underage children, the adult’s consent was gotten in advance of the child’s assent.
Statistical analyses
Prevalence rates of taking TT vaccination and IPTp-SP for each explanatory variable were shown as percentages in their weighted forms. The collinearity testing method was adopted in the correlation analysis to distinguish the interdependencies that exist between variables. To examine the multicollinearity that causes major concerns, a cutoff of 0.7 was used. 34 No variable from the correlation matrix was removed in the model as a result of a lack of multicollinearity. Chi-square bivariate tests were used to examine the association at p value <0.05. Controlled variables that showed p value <0.15 including those that had significant associations in the bivariate tests were included in the multivariable logistic regression model to compute the adjusted odds ratios with corresponding 95% confidence interval (CI) of the factors (covariates) associated with taking TT vaccinations and IPTp-SP. Statistical significance was set at a p value of <0.05 for all analyses. Data analysis was performed using IBM SPSS version 25.
Results
The study included a total of 6143 maternal women of childbearing age who were ever pregnant at least once in their lifetime before the survey. The mean age was 28.0 years with a standard deviation of ±9.2. The study revealed that 27.5% and 30.5% of the women aged 20–24 years had received TT immunization and adequate TT doses (at least two doses), respectively. About 25.7% of maternal women aged 25–29 years were found to receive IPTp-SP antimalarial drugs. In contrast, one-fourth of those aged 20–24 years had had the highest proportion to receive adequate IPTp-SP (at least three doses) antimalarial drugs as shown in Table 1. Three-fourths of these women were residing in rural areas; Basse LGA recorded the highest in the use of IPTp-SP and TT immunization at 20.3% and 19.2%, respectively.
Table 1.
Participants’ sociodemographic characteristics (n = 6143).
| Variables | Took TT | Adequate TT dose | Took IPTp-SP | Adequate IPTp-SP dose | ||||
|---|---|---|---|---|---|---|---|---|
| Yes (88.2) | No (11.8) | Yes (34.8) | No (65.2) | Yes (96.6) | No (3.4) | Yes (34.3) | No (65.7) | |
| Age of participants, years | ||||||||
| 15–19 | 8.9 | 3.9 | 13.9 | 6.2 | 8.1 | 11.9 | 8.8 | 7.8 |
| 20–24 | 27.5 | 8.4 | 30.5 | 25.9 | 25.1 | 36.9 | 25.2 | 25.0 |
| 25–29 | 26.7 | 16.5 | 25.1 | 27.7 | 25.7 | 13.1 | 24.5 | 26.4 |
| 30–34 | 20.2 | 28.1 | 17.6 | 21.7 | 21.2 | 19.0 | 22.4 | 20.6 |
| 35–39 | 11.7 | 29.4 | 9.3 | 13.0 | 13.9 | 11.9 | 14.2 | 13.8 |
| 40–44 | 3.8 | 12.5 | 2.5 | 4.3 | 4.8 | 4.8 | 4.1 | 5.1 |
| 45–49 | 1.2 | 1.2 | 1.1 | 1.2 | 1.2 | 2.4 | 0.8 | 1.3 |
| p value | <0.0001* | <0.0001* | 0.047* | 0.071 | ||||
| Residence | ||||||||
| Urban | 23.2 | 20.8 | 24.4 | 22.5 | 22.7 | 31.0 | 24.9 | 21.5 |
| Rural | 76.8 | 79.2 | 75.6 | 77.5 | 77.3 | 69.0 | 75.1 | 78.5 |
| p value | 0.146 | 0.120 | 0.087 | 0.003* | ||||
| Local government area | ||||||||
| Banjul | 3.2 | 1.5 | 3.5 | 3.1 | 3.1 | 6.0 | 2.1 | 3.5 |
| Kanifing | 5.8 | 4.8 | 6.1 | 5.6 | 5.6 | 9.5 | 5.8 | 5.5 |
| Brikama | 8.8 | 6.6 | 10.9 | 7.7 | 8.4 | 13.1 | 11.4 | 6.9 |
| Mansankonko | 13.2 | 8.0 | 15.7 | 11.7 | 12.6 | 7.1 | 15.8 | 11.1 |
| Kerewan | 14.8 | 18.8 | 12.4 | 15.9 | 15.3 | 10.7 | 13.6 | 16.1 |
| Kuntaur | 19.2 | 22.1 | 17.4 | 20.2 | 19.7 | 11.9 | 18.0 | 20.5 |
| Janjanbureh | 15.6 | 15.1 | 14.8 | 16.2 | 15.4 | 25.0 | 13.0 | 16.7 |
| Basse | 19.4 | 23.1 | 19.2 | 19.6 | 19.9 | 16.7 | 20.3 | 19.7 |
| p value | <0.0001* | <0.001* | 0.014* | <0.0001* | ||||
| Educational level | ||||||||
| None | 56.2 | 72.6 | 52.0 | 58.7 | 58.3 | 56.0 | 58.0 | 58.4 |
| Primary | 19.5 | 16.5 | 20.1 | 19.1 | 19.1 | 22.6 | 18.8 | 19.3 |
| Secondary+ | 24.3 | 10.9 | 27.9 | 22.2 | 22.6 | 21.4 | 23.2 | 22.3 |
| p value | <0.0001* | <0.0001* | 0.719 | 0.714 | ||||
| Ethnicity | ||||||||
| Mandinka | 27.9 | 32.3 | 29.7 | 26.9 | 28.5 | 33.3 | 27.2 | 29.1 |
| Wollof | 20.5 | 16.5 | 20.0 | 20.9 | 20.0 | 21.4 | 18.8 | 20.7 |
| Fula | 27.1 | 25.6 | 25.0 | 28.3 | 26.8 | 29.8 | 28.0 | 26.2 |
| Jola | 3.1 | 2.1 | 3.4 | 2.8 | 2.8 | 4.7 | 3.6 | 2.5 |
| Serahule | 10.2 | 11.3 | 9.8 | 10.5 | 10.4 | 4.8 | 10.8 | 10.2 |
| Others | 5.7 | 6.7 | 6.2 | 5.4 | 5.9 | 2.4 | 5.3 | 6.2 |
| Non-Gambian | 5.5 | 5.5 | 5.9 | 5.2 | 5.6 | 3.6 | 6.3 | 5.1 |
| p value | 0.031* | 0.045* | 0.323 | 0.014* | ||||
| Marital status | ||||||||
| Married | 95.8 | 96.3 | 94.4 | 96.6 | 96.1 | 94.0 | 96.0 | 96.1 |
| Widow/divorce | 2.3 | 1.5 | 2.4 | 2.1 | 2.1 | 2.4 | 2.0 | 2.2 |
| Single | 1.9 | 2.2 | 3.2 | 1.3 | 1.8 | 3.6 | 2.0 | 1.7 |
| p value | 0.504 | <0.0001* | 0.572 | 0.775 | ||||
| Wealth index | ||||||||
| Poorest | 42.3 | 46.9 | 42 | 42.6 | 42.9 | 40.7 | 41.6 | 43.6 |
| Second | 25.9 | 23.8 | 27.2 | 25.2 | 25.7 | 23.8 | 26.1 | 25.6 |
| Middle | 16.4 | 17.1 | 14.8 | 17.0 | 16.4 | 12.9 | 16.3 | 16.5 |
| Fourth | 8.9 | 7.2 | 8.6 | 9.2 | 8.7 | 11.9 | 9.2 | 8.4 |
| Richest | 6.5 | 5.0 | 7.4 | 6.0 | 6.2 | 10.7 | 6.8 | 5.9 |
| p value | 0.065 | 0.033* | 0.301 | 0.347 | ||||
| Parity | ||||||||
| 0–3 | 56.8 | 19.0 | 66.5 | 51.4 | 52.0 | 63.1 | 54.3 | 50.8 |
| 4 and above | 43.2 | 81.0 | 33.5 | 48.6 | 48.0 | 36.9 | 45.7 | 49.2 |
| p value | <0.0001* | <0.0001* | 0.048* | 0.011* | ||||
| Newspaper | ||||||||
| Do not use | 95.7 | 97.1 | 93.9 | 96.9 | 96.0 | 95.2 | 95.8 | 96.1 |
| Few days a week | 4.0 | 2.9 | 5.7 | 3.9 | 2.8 | 2.4 | 4.1 | 3.6 |
| Almost everyday | 0.3 | 0.0 | 0.4 | 0.2 | 0.2 | 2.4 | 0.1 | 0.3 |
| p value | 0.239 | <0.0001* | 0.005* | 0.348 | ||||
| Radio | ||||||||
| Do not listen | 20.5 | 19.8 | 17.6 | 22.1 | 20.4 | 22.6 | 21.3 | 19.9 |
| Few days a week | 44.9 | 42.0 | 47.3 | 43.5 | 44.4 | 44.1 | 42.0 | 45.7 |
| Almost everyday | 34.6 | 38.2 | 35.1 | 34.4 | 35.2 | 33.3 | 36.7 | 34.4 |
| p value | 0.194 | <0.0001* | 0.101 | 0.040* | ||||
| Television | ||||||||
| Do not watch | 51.8 | 52.8 | 52.4 | 51.6 | 52.1 | 48.8 | 51.4 | 52.4 |
| Less than once | 23.2 | 22.6 | 22.3 | 23.7 | 23.3 | 15.5 | 22.3 | 23.8 |
| Almost everyday | 25.0 | 24.6 | 25.3 | 24.7 | 24.6 | 35.7 | 26.3 | 23.8 |
| p value | 0.063 | 0.496 | 0.106 | 0.001* | ||||
| Antenatal visit | ||||||||
| <5 times | 47.2 | 54.8 | 43.2 | 49.5 | 47.9 | 63.1 | 40.0 | 52.0 |
| 5 times and above | 52.8 | 45.2 | 56.8 | 50.5 | 52.1 | 36.9 | 60.0 | 48.0 |
| p value | <0.0001* | <0.0001* | 0.006* | <0.0001* | ||||
| Current pregnancy | ||||||||
| Yes | 5.5 | 3.8 | 5.8 | 4.3 | 4.2 | 8.3 | 3.9 | 5.6 |
| No | 94.5 | 96.2 | 94.2 | 95.7 | 95.8 | 91.7 | 96.1 | 94.4 |
| p value | <0.0001* | 0.544 | 0.215 | 0.009* | ||||
TT: tetanus toxoid.
Statistically significant at p < 0.05.
In this study, slightly more than half of the women (52.0%) had never been to school, at least 2 in every 10 maternal women (26.9%) were found to be Mandinka by ethnicity and at least 94.0% were currently married at the time of the study. The study revealed that at least 40.7% of that used IPTp-SP and TT were from the poorest household’s wealth index with a mean parity of 2.9 with a standard deviation of ±2.9. Slightly more than half of these women (51.4%) were within a parity range of 0–3. In terms of frequency of reading newspapers, at least 93.9% do not use newspapers and only one-third (35.1%) of these women reported to listen to the radio almost every day. One in every four women (24.6%) was found to watch television almost every day, and more than half (56.8%) reported having had at least 5 times antenatal visits during their previous pregnancies. The mean number of antenatal visits was 4.9 times with a standard deviation of 5.3. Only 5.8% of those currently pregnant had received adequate TT immunization and 3.9% received at least three doses of IPTp-SP antimalarial drug at the time of the study.
The study revealed that 88.2% of maternal women took TT immunization, while 34.8% had had at least two doses of TT immunization as shown in Figure 1. About 98.6% of the participants received IPTp-SP antimalarial drugs, while 34.3% of the women received at least three doses of IPTp-SP antimalarial drugs.
Figure 1.
A bar chart showing the prevalence of maternal mothers’ utilization of IPTp-SP drugs and TT immunization.
TT: tetanus toxoid.
Table 2 shows the results of the logistic regression model in determining the correlates of IPTp-SP antimalarial drug utilization among maternal women in The Gambia. Having adjusted the predictor variables for possible confounders, frequency of reading newspapers, and ANC visits were found to be significantly associated with taking IPTp-SP drugs during pregnancy. With regard to determinants for adequate IPTp-SP antimalarial drugs, the findings show that women’s LGA of residence, ethnicity, parity, frequency of listening to the radio, and the number of ANC visits were found to be statistically associated. Women who read newspapers almost every day were 89.7% (odds ratio (OR) = 0.103, 95% CI = 0.020–0.523) less likely to receive IPTp-SP antimalarial drugs compared to those who do not read newspapers. Women with less than 5 times ANC visits were 50.0% (OR = 0.500, 95% CI = 0.317–0.789) less likely to IPTp-SP antimalarial drugs compared to those with at least 5 times ANC visits.
Table 2.
Correlates on the utilization of IPTp-SP drugs among pregnant women in The Gambia.
| Model I—IPTp-SP taken | Model II—Adequate IPTp-SP dose | |||||||
|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI for OR | p value | aOR | 95% CI for OR | p value | |||
| LB | UB | LB | UB | |||||
| Age (ref: 45–49), years | 0.138 | 0.074 | ||||||
| 15–19 | 1.740 | 0.325 | 9.313 | 0.517 | 1.343 | 0.735 | 2.456 | 0.338 |
| 20–24 | 1.662 | 0.344 | 8.025 | 0.527 | 1.196 | 0.669 | 2.137 | 0.546 |
| 25–29 | 4.663 | 0.956 | 22.735 | 0.057 | 1.163 | 0.656 | 2.061 | 0.605 |
| 30–34 | 2.421 | 0.535 | 10.962 | 0.251 | 1.444 | 0.817 | 2.551 | 0.206 |
| 35–39 | 2.406 | 0.511 | 11.317 | 0.267 | 1.445 | 0.813 | 2.566 | 0.209 |
| 40–44 | 2.122 | 0.376 | 11.973 | 0.394 | 1.149 | 0.623 | 2.119 | 0.657 |
| Residence (ref: rural) | ||||||||
| Urban | 1.160 | 0.506 | 2.663 | 0.726 | 1.094 | 0.892 | 1.342 | 0.388 |
| Local government area (ref: Basse) | 0.070 | 0.000 | ||||||
| Banjul | 0.370 | 0.104 | 1.317 | 0.125 | 0.439 | 0.288 | 0.668 | 0.000*** |
| Kanifing | 0.442 | 0.137 | 1.425 | 0.172 | 0.838 | 0.607 | 1.157 | 0.283 |
| Brikama | 0.500 | 0.187 | 1.331 | 0.165 | 1.481 | 1.121 | 1.958 | 0.006** |
| Mansakonko | 1.428 | 0.542 | 3.761 | 0.471 | 1.419 | 1.164 | 1.731 | 0.001** |
| Kerewan | 1.262 | 0.538 | 2.959 | 0.593 | 0.854 | 0.691 | 1.055 | 0.143 |
| Kuntaur | 1.562 | 0.681 | 3.582 | 0.293 | 0.888 | 0.727 | 1.084 | 0.243 |
| Janjanbureh | 0.552 | 0.276 | 1.104 | 0.093 | 0.726 | 0.592 | 0.892 | 0.002** |
| Ethnicity (ref: non-Gambian) | 0.006 | |||||||
| Mandinka | 0.694 | 0.536 | 0.898 | 0.005** | ||||
| Wollof | 0.907 | 0.689 | 1.192 | 0.483 | ||||
| Fula | 0.897 | 0.690 | 1.165 | 0.414 | ||||
| Jola | 0.802 | 0.537 | 1.198 | 0.281 | ||||
| Sarahule | 0.783 | 0.580 | 1.057 | 0.111 | ||||
| Other | 0.730 | 0.526 | 1.013 | 0.060 | ||||
| Parity (ref: 4 and above) | ||||||||
| 0–3 | 1.285 | 0.660 | 2.500 | 0.460 | 1.216 | 1.047 | 1.412 | 0.010* |
| Newspaper (ref: do not use) | 0.014 | |||||||
| Few days a week | 1.832 | 0.432 | 7.773 | 0.412 | ||||
| Almost everyday | 0.103 | 0.020 | 0.523 | 0.006** | ||||
| Radio (ref: do not use) | 0.913 | 0.003 | ||||||
| Few days a week | 1.120 | 0.635 | 1.977 | 0.695 | 0.860 | 0.578 | 1.279 | 0.456 |
| Almost everyday | 1.124 | 0.615 | 2.055 | 0.704 | 1.108 | 1.032 | 1.190 | 0.005** |
| Antenatal visits (ref: 5 and above) | ||||||||
| Less than 5 times | 0.500 | 0.317 | 0.789 | 0.003** | 0.618 | 0.553 | 0.691 | 0.000*** |
| Constant | 33.351 | 0.001 | 0.521 | 0.667 | ||||
aOR: adjusted odds ratio (exponentiated coefficients); CI: confidence interval; IPTp-SP: intermittent preventive treatment with sulfadoxine-pyrimethamine; LB: lower boundary; LGA: local government area; OR: odds ratio; ref: reference category; UB: upper boundary.
Model I—Took IPTp-SP: adjusted for age, residence, LGA, parity, newspaper, radio, and antenatal visits.
Model II—Took adequate IPTp-SP: adjusted for age, residence, ethnicity, LGA, parity, radio, and antenatal visits.
p < 0.055; **p < 0.01; ***p < 0.001.
The study revealed that women from Banjul and Janjanbureh LGAs were 46.1% (OR = 0.439, 95% CI = 0.288–0.668) and 27.4% (OR = 0.726, 95% CI = 0.592–0.892) less likely to receive adequate IPTp-SP antimalarial drugs, respectively, compared to those from Basse LGA. The likelihood of women from Brikama and Mansakonko LGAs to receive adequate IPTp-SP antimalarial drugs increased by 48.1% (OR = 1.481, 95% CI = 1.121–1.958) and 41.9% (OR = 1.419, 95% CI = 1.164–0.731). Women who are Mandinkas were 30.6% (OR = 0.694, 95% CI = 0.536–0.898) less likely to receive adequate IPTp-SP antimalarial drugs compared to those that are non-Gambians. Women of parity 0–3 had higher odds (OR = 1.216, 95% CI = 1.047–1.412) of receiving adequate IPTp-SP antimalarial drugs compared to those with parity four and above. The significant positive association between frequency of listening to the radio and receiving adequate antimalarial drugs was true for women who listen to the radio almost every day (OR = 1.108, 95% CI = 1.032–0.190) compared to those who do not listen to the radio. Maternal women’s ANC visits were found to be associated with receiving adequate IPTp-SP antimalarial drugs (OR = 0.618, 95% CI = 0.553–0.691).
Table 3 shows the results of the logistic regression model on the correlates of TT immunization among maternal women in The Gambia. Covariates such as age, educational level, ethnicity, parity, current pregnancy status, and ANC visits were found to be significantly associated with TT immunization. The model, having been adjusted for confounders, covariates that include LGA of residence, ethnicity, parity, listening to the radio, reading newspapers, and ANC visits were significantly associated with the odds of receiving adequate doses of TT immunization. The likelihood of women aged 35–39 years (OR = 0.382, 95% CI = 0.185–0.789) and 40–44 years (OR = 0.333, 95% CI = 0.157–0.706) on using TT immunization was significantly lowered compared to those are 45–49 years old. Maternal who never been to school (OR = 0.503, 95% CI = 0.377–0.670) and those with a primary level of education (OR = 0.583, 95% CI = 0.420–0.809) have lower odds of receiving TT immunization compared to those with a secondary level of education or more. The model predicted that women who are Wollof by ethnicity (OR = 1.642, 95% CI = 1.070–2.519) have higher odds of receiving TT immunization compared to non-Gambians. Women with parity 0–3 are more likely to use TT immunization by a factor of 3.074 (OR = 3.074, 95% CI = 2.341–4.037) compared to those with higher parity (⩾4). The currently pregnant women were 3.747 times (OR = 3.747, 95% CI = 1.519–9.240). The ANC visits were significantly associated with a lower odds of receiving TT immunization (OR = 0.683, 95% CI = 0.576–0.809).
Table 3.
Correlates on the utilization of TT among pregnant women in The Gambia.
| Model III—TT took | Model IV—Adequate TT dose | |||||||
|---|---|---|---|---|---|---|---|---|
| 95% CI for OR | 95% CI for OR | |||||||
| aOR | LB | UB | p value | aOR | LB | UB | p value | |
| Age (ref: 45–49), years | 0.000 | 0.000 | ||||||
| 15–19 | 0.977 | 0.406 | 2.356 | 0.959 | 1.750 | 0.969 | 3.158 | 0.063 |
| 20–24 | 1.316 | 0.601 | 2.882 | 0.492 | 0.903 | 0.512 | 1.592 | 0.723 |
| 25–29 | 0.958 | 0.459 | 2.003 | 0.910 | 0.775 | 0.444 | 1.356 | 0.372 |
| 30–34 | 0.596 | 0.289 | 1.230 | 0.162 | 0.758 | 0.434 | 1.323 | 0.329 |
| 35–39 | 0.382 | 0.185 | 0.789 | 0.009** | 0.734 | 0.416 | 1.294 | 0.285 |
| 40–44 | 0.333 | 0.157 | 0.706 | 0.004** | 0.639 | 0.341 | 1.197 | 0.162 |
| Residence (ref: rural) | ||||||||
| Urban | 0.969 | 0.728 | 1.290 | 0.828 | 0.920 | 0.727 | 1.164 | 0.487 |
| Education (ref: secondary+) | 0.000 | |||||||
| None | 0.503 | 0.377 | 0.670 | 0.000*** | ||||
| Primary | 0.583 | 0.420 | 0.809 | 0.001** | ||||
| Local government area (ref: Basse) | 0.000 | |||||||
| Banjul | 1.350 | 0.862 | 2.113 | 0.190 | ||||
| Kanifing | 1.268 | 0.865 | 1.859 | 0.224 | ||||
| Brikama | 1.689 | 1.244 | 2.293 | 0.001** | ||||
| Mansakonko | 1.321 | 1.067 | 1.635 | 0.011** | ||||
| Kerewan | 0.753 | 0.598 | 0.948 | 0.016** | ||||
| Kuntaur | 0.825 | 0.662 | 1.028 | 0.087 | ||||
| Janjanbureh | 0.892 | 0.717 | 1.109 | 0.304 | ||||
| Ethnicity (ref: non-Gambian) | 0.000 | 0.007 | ||||||
| Mandinka | 0.860 | 0.578 | 1.279 | 0.456 | 0.922 | 0.698 | 1.219 | 0.570 |
| Wollof | 1.642 | 1.070 | 2.519 | 0.023* | 0.952 | 0.708 | 1.280 | 0.745 |
| Fula | 1.176 | 0.781 | 1.771 | 0.438 | 0.719 | 0.541 | 0.956 | 0.023* |
| Jola | 1.545 | 0.774 | 3.082 | 0.217 | 0.764 | 0.499 | 1.170 | 0.216 |
| Sarahule | 0.965 | 0.618 | 1.507 | 0.876 | 0.979 | 0.703 | 1.363 | 0.898 |
| Other | 0.824 | 0.506 | 1.342 | 0.437 | 1.065 | 0.750 | 1.510 | 0.726 |
| Wealth index (ref: richest) | 0.647 | 0.006 | ||||||
| Poorest | 1.061 | 0.649 | 1.736 | 0.814 | 1.369 | 0.957 | 1.958 | 0.086 |
| Second | 1.206 | 0.742 | 1.961 | 0.451 | 1.337 | 0.941 | 1.899 | 0.105 |
| Middle | 1.099 | 0.688 | 1.756 | 0.691 | 0.996 | 0.709 | 1.399 | 0.981 |
| Fourth | 1.28 | 0.781 | 2.098 | 0.327 | 0.906 | 0.663 | 1.239 | 0.538 |
| Parity (ref: 4 and above) | ||||||||
| 0–3 | 3.074 | 2.341 | 4.037 | 0.000*** | 1.492 | 1.273 | 1.750 | 0.000*** |
| Radio (ref: do not use) | ||||||||
| Few days a week | 0.922 | 0.698 | 1.219 | 0.570 | 0.884 | 0.819 | 0.954 | 0.002** |
| Almost everyday | 0.981 | 0.879 | 1.094 | 0.725 | 1.832 | 0.432 | 7.773 | 0.412 |
| Newspaper (ref: do not use) | 0.000 | |||||||
| Few days a week | 1.899 | 1.412 | 2.554 | 0.000*** | ||||
| Almost everyday | 1.480 | 0.505 | 4.339 | 0.475 | ||||
| Currently pregnant (ref: yes) | 0.011 | |||||||
| None | 3.747 | 1.519 | 9.240 | 0.004** | ||||
| Antenatal visits (ref: 5 and above) | ||||||||
| Less than 5 times | 0.683 | 0.576 | 0.809 | 0.000*** | 0.791 | 0.703 | 0.890 | 0.000*** |
| Constant | 8.002 | 0.001 | 0.614 | 0.193 | ||||
ANC: antenatal care; aOR: adjusted odds ratio (exponentiated coefficients); CI: confidence interval; IPTp-SP: intermittent preventive treatment with sulfadoxine-pyrimethamine; LGA: local government area; OR: odds ratio; ref: reference category; TT: tetanus toxoid; LB: lower boundary; UB: upper boundary.
Model III—Took TT doses: adjusted for age, residence, educational level, ethnicity, wealth index, parity, radio, newspaper, currently pregnant, and ANC visits.
Model IV—Took adequate TT doses: adjusted for age, residence, LGA, ethnicity, wealth index, parity, newspaper, radio, and ANC visits.
p < 0.055; **p < 0.01; ***p < 0.001.
This study revealed that women from Brikama and Mansakonko LGAs were 1.689 times (OR = 1.689, 95% CI = 1.244–2.293) and 1.321 times (OR = 1.321, 95% CI = 1.067–1.635) more likely to receive adequate TT dose, while those from Kerewan LGA had lower odds (OR = 0.753, 95% CI = 0.598–0.948) of receiving adequate TT dose compared to those from Basse LGA. Furthermore, Fulas had lower odds of receiving adequate TT dose as compared to non-Gambians. Women with parity 0–3 are more likely to receive adequate doses of TT by a factor of 1.492 (OR = 1.492, 95% CI = 1.273–1.750) compared to those with high parity (⩾4). The study also revealed that women who listen to the radio a few days a week had lower odds (OR = 0.884, 95% CI = 0.819–0.954) of receiving adequate TT dose compared to those who do not listen to the radio. Reading newspapers a few days a week (OR = 1.899, 95% CI = 1.412–2.554) and ANC visits (OR = 0.791, 95% CI = 0.703–0.890) were found to be associated with receiving adequate doses of TT.
Discussion
The study examined the differentials in prevalence and correlates of utilizing TT and intermittent preventive treatment of malaria in pregnancy, using data from the MICS conducted in The Gambia in 2018. The findings of this study revealed that the overall prevalence of TT uptake among women in The Gambia was 88.2%. In comparison, the prevalence of maternal women who took at least two doses of TT was 34.8%. As shown in the regression analysis model, an increased women’s age was a significant indicator of the uptake of TT immunization. On the contrary, this finding is inconsistent with the study done in Ethiopia, showing a positive association between advanced age and taking TT immunization. 35 There is a possibility that women in advanced age groups have been exposed to multiple pregnancies and had previous experience in attending numerous ANC clinics where many factors such as the attitude of healthcare workers toward antenatal women and distance to access the services. Furthermore, quality of care and affordability of transportation could deter them from accessing the services, especially in rural and resource-poor settings.36–39
Furthermore, the study showed that the overall prevalence of IPTp-SP uptake among maternal women in The Gambia was 98.6%, while the prevalence of expectant women who took at least three doses of IPTp-SP was 34.3%. These findings are similar to the study done in Ghana at 98.5%, 40 Ivory Coast at 81.9%, 23 Tanzania at 96.0%, 41 and Sierra Leone at 94.8%. 6 This study is in variance with other studies that documented low rates of IPTp-SP antimalarial drugs among pregnant women.1,42–44 The study also documented that the prevalence of TT and IPTp-SP uptake tends to be higher in women aged 20–24 and 25–29 and rural residents, those from Kuntaur LGA with no educational background and of Mandinka ethnicity. Furthermore, the prevalence is still higher among women who are married, from the poorest households’ wealth index, with parity 0–3, and those who do not read the newspaper. Those who use radio a few days a week, do not watch TV, and made adequate ANC visits and were not pregnant at the time of the study were reported to be high in prevalence for TT and IPTp-SP. This is similar to previous studies.45,46 Therefore, the pivotal role of the community and opinion leaders, especially in deep-rooted cultural societies, should be integrated and strengthened in our maternal and child health programs.
The multivariate logistic regression model found that the controlled variables that had significantly higher odds of predicting IPTp-SP uptake in expectant mothers include women from Mansakonko LGA, women with parity 0–3, while other covariates that had significantly higher odds of predicting adequate IPTp-SP uptake includes women from Brikama and Mansakonko LGA, women with parity 0–3 and those who listen to the radio almost every day. These could be attributed to the consistent implementation of women-centered intervention programs such as the integrated routine reproductive and child health (RCH) services across the length and breadth of the country. Furthermore, the uptake of IPTp-SP could be more about accessibility than availability, based on the parts or regions of the country they are residing in during the course of their pregnancy. Most rural communities in The Gambia or non-primary health care villages may face barriers to accessing adequate IPTp-SP and even TT doses. Surprisingly, women with reduced ANC visits and almost everyday reading of newspapers had lower odds of taking IPTp-SP doses, while other correlates such as reduced ANC visits, women who are Mandinka by ethnicity, residents of Janjabureh, and Banjul LGA had lower odds of taking adequate IPTp-SP doses. This necessitates a strong collaboration between the healthcare workers and community leaders for the promotion of expectant women’s optimal ANC attendance and ensures that everyone receives the required dose of IPTp-SP.42,45
With regard to the update of adequate TT immunization, women with a reduced number of ANC visits were less likely to receive the required doses of TT compared to those with at least five ANC visits. These results were also supported by other studies.47–50 This could be attributed to the fact that women who usually attend ANC services are more likely to be informed about the relevance of TT immunization in protecting them from having tetanus. Thus, they would receive more TT doses than those who attended fewer ANC services. Furthermore, our study further revealed that women with lower parity had higher odds in the uptake of TT immunization compared to those of higher parity. These contradicted the findings from previous studies which reported that higher parity (>4 pregnancies) was a significant predictor of TT immunization.20,51 Women’s previous experience with the delivery, including the side effects of TT immunization, could be deterrent factors in their utilization of RCH services. The use of different health education and promotion tools and strategies provides choice and informed decision-making for maternal women in both rural and urban settings of resource-poor countries. 6 In general, women with an increased number of parity, education, and living in urban areas are more likely to be aware of health issues relating to pregnancy and utilization of RCH services, including antenatal and postnatal care.31,40,52,53
Strengths and limitations
The cross-sectional study design nature of the data used for this study prevented us from making any causal assumptions but instead showed associations between the study variables.54,55 The reported prevalence of IPTp-SP and TT use was self-reported, and therefore, this may lead to reporting bias. The authors could not establish the exact trimester the IPTp-SP and TT were administered. Furthermore, we worked within the scope of our objectives, and other covariates of IPTp-SP uptake could be examined in another study. There is a need for further studies that would look at the causal linkage between ANC attendance and TT vaccination/IPTp-SP coverage. As for strengths, due to the large sample size, the findings can be generalized for women aged 15–49 years in The Gambia.
Conclusion
Our study concludes that the overall uptake of TT immunization and IPTp-SP is low, with the prevalence slightly higher in rural areas than in urban areas. Factors such as LGA, ethnicity, parity, use of radio, use of newspaper, and ANC visits were found to be significantly associated with adequate IPTp-SP drugs and TT immunization, respectively. Therefore, the promotion of adequate antenatal care visits and vaccination by ensuring the availability of TT immunization and IPTp drugs should be regarded as an essential strategy to improve their utilization in The Gambia.
Acknowledgments
The authors’ appreciation goes to the MICS project for approval and access granted to the original data for this research.
Footnotes
Authors contributions: A.B., S.B., and A.J. conceived and designed the study. A.B., A.J., and S.B. performed data analysis and wrote the results. All authors discussed the results, reviewed, and approved the final article.
Availability of data and materials: The original survey was conducted after being ethically approved by the Gambia Government Joint Research Ethics Committee (ref. no. SCC1570v1.1). Before analysis, we obtained permission from the Gambia Bureau of Statistics and MICS program to access the data set. The issue of privacy of the respondents was considered such that exclusive information such as respondents’ locations, and their names as collected during the MICS interviews were consciously removed from data sets.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The original survey was conducted after being ethically approved by the Gambia Government Joint Research Ethics Committee (ref. no. SCC1570v1.1). Prior to analysis, we obtained permission from the Gambia Bureau of Statistics and MICS program to access the data set. The issue of privacy of the respondents was considered such that exclusive information such as respondents’ locations and their names as collected during the MICS interviews were consciously removed from data sets.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Not applicable/waived for secondary users of the MICS data.
ORCID iD: Amadou Barrow  https://orcid.org/0000-0002-6006-9355
https://orcid.org/0000-0002-6006-9355
References
- 1. Yaya S, Uthman OA, Amouzou A, et al. Use of intermittent preventive treatment among pregnant women in sub-Saharan Africa: evidence from malaria indicator surveys. Trop Med Infect Dis 2018; 3(1): 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bardají A, Sigauque B, Sanz S, et al. Impact of malaria at the end of pregnancy on infant mortality and morbidity. J Infect Dis 2011; 203(5): 691–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Moya-Alvarez V, Abellana R, Cot M. Pregnancy-associated malaria and malaria in infants: an old problem with present consequences. Malar J 2014; 13: 271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Antinori S, Galimberti L, Milazzo L, et al. Biology of human malaria plasmodia including Plasmodium knowlesi. Mediterr J Hematol Infect Dis 2012; 4(1): 4e2012013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. World malaria report 2019, https://www.who.Int/publications-detail-redirect/9789241565721 (accessed 10 August 2020).
- 6. Buh A, Kota K, Bishwajit G, et al. Prevalence and associated factors of taking intermittent preventive treatment in pregnancy in Sierra Leone. Trop Med Infect Dis 2019; 4(1): 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang H, Bhutta ZA, Coates MM, et al. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016: 388(10053): 1725–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Steketee RW, Nahlen BL, Parise ME, et al. The burden of malaria in pregnancy in malaria-endemic areas. Am J Trop Med Hyg 2001; 64(Suppl. 1–2): 28–35. [DOI] [PubMed] [Google Scholar]
- 9. Van Eijk AM, Hill J, Noor AM, et al. Prevalence of malaria infection in pregnant women compared with children for tracking malaria transmission in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health 2015; 3(10): e617–e628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Desai M, ter Kuile FO, Nosten F, et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis 2007; 7(2): 93–104. [DOI] [PubMed] [Google Scholar]
- 11. Goldenberg RL, McClure EM, Saleem S. Improving pregnancy outcomes in low- and middle-income countries. Reprod Health 2018; 15(Suppl. 1): 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Radeva-Petrova D, Kayentao K, ter Kuile FO, et al. Drugs for preventing malaria in pregnant women in endemic areas: any drug regimen versus placebo or no treatment. Cochrane Database Syst Rev 2014; 2014(10): CD000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dengela D, Seyoum A, Lucas B, et al. Multi-country assessment of residual bio-efficacy of insecticides used for indoor residual spraying in malaria control on different surface types: results from program monitoring in 17 PMI/USAID-supported IRS countries. Parasit Vectors 2018; 11(1): 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization. WHO evidence review group: intermittent preventive treatment of malaria in pregnancy (IPTp) with sulfadoxine-pyrimethamine (SP), 2012, https://www.who.int/malaria/mpac/sep2012/iptp_sp_erg_meeting_report_july2012.pdf
- 15. Orish VN, Onyeabor OS, Boampong JN, et al. Prevalence of intermittent preventive treatment with sulphadoxine-pyrimethamine (IPTp-SP) use during pregnancy and other associated factors in Sekondi-Takoradi, Ghana. Afr Health Sci 2015; 15(4): 1087–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Van Eijk AM, Larsen DA, Kayentao K, et al. Effect of Plasmodium falciparum sulfadoxine-pyrimethamine resistance on the effectiveness of intermittent preventive therapy for malaria in pregnancy in Africa: a systematic review and meta-analysis. Lancet Infect Dis 2019; 19(5): 546–556. [DOI] [PubMed] [Google Scholar]
- 17. World Health Organization. World malaria report 2017, http://www.who.Int/malaria/publications/world-malaria-report-2017/report/en/ (accessed 10 August 2020).
- 18. Iriemenam NC, Shah M, Gatei W, et al. Temporal trends of sulphadoxine-pyrimethamine (SP) drug-resistance molecular markers in Plasmodium falciparum parasites from pregnant women in western Kenya. Malar J 2012; 11: 134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Oladeinde BH, Omoregie R, Odia I, et al. Prevalence of malaria and anemia among pregnant women attending a traditional birth home in Benin City, Nigeria. Oman Med J 2012; 27(3): 232–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pathirana J, Nkambule J, Black S. Determinants of maternal immunization in developing countries. Vaccine 2015; 33(26): 2971–2977. [DOI] [PubMed] [Google Scholar]
- 21. Roman E, Andrejko K, Wolf K, et al. Determinants of uptake of intermittent preventive treatment during pregnancy: a review. Malar J 2019; 18(1): 372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aljedry ZAHS, Shaib AA, Al-Shamahy HAH, et al. Tetatnus immunization among pregnant women: coverage rate and rate of protection at time of delivery. Univ J Pharmaceut Res 2019; 4(1): 12–16. [Google Scholar]
- 23. Yaya S, Kota K, Buh A, et al. Antenatal visits are positively associated with uptake of tetanus toxoid and intermittent preventive treatment in pregnancy in Ivory Coast. BMC Public Health 2019; 19(1): 1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Anatea MD, Mekonnen TH, Dachew BA. Determinants and perceptions of the utilization of tetanus toxoid immunization among reproductive-age women in Dukem Town, Eastern Ethiopia: a community-based cross-sectional study. BMC Int Health Hum Rights 2018; 18(1): 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hill J, Hoyt J, van Eijk AM, et al. Factors affecting the delivery, access, and use of interventions to prevent malaria in pregnancy in sub-Saharan Africa: a systematic review and meta-analysis. PLoS Med 2013; 10(7): e1001488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sherley J, Newton S. The association between area of residence and sufficient antenatal tetanus vaccination in women ages 15–49 in Afghanistan: an analysis of the 2015 DHS dataset. Glob Health Res Policy 2020; 5(1): 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gambia Bureau of Statistics. The Gambia: multiple indicator cluster survey 2018: survey findings report, 2019, https://www.unicef.org/gambia/media/776/file/The%20Gambia%20Multiple%20Indicator%20Cluster%20Survey%202018.pdf (accessed 16 August 2020).
- 28. Brabin L, Stokes E, Dumbaya I, et al. Rural Gambian women’s reliance on health workers to deliver sulphadoxine—pyrimethamine as recommended intermittent preventive treatment for malaria in pregnancy. Malar J 2009; 8: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Anya SE, Hydara A, Jaiteh LE. Antenatal care in The Gambia: missed opportunity for information, education and communication. BMC Pregnancy Childbirth 2008; 8: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Barrow A, Jobe A, Onoh V, et al. Prevalence and factors associated with institutional-based delivery in The Gambia: further analysis of population-based cross-sectional data. Afr J Reprod Health 2020; 24(2): 176–186. [DOI] [PubMed] [Google Scholar]
- 31. Barrow A, Jobe A. Predictors of postnatal care service utilization among women of childbearing age in The Gambia: analysis of multiple indicators cluster survey. Int J Womens Health 2020; 12: 709–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ekholuenetale M, Onikan A, Ekholuenetale CE. Prevalence and determinants of mother and newborn skin-to-skin contact in The Gambia: a secondary data analysis. J Egypt Public Health Assoc 2020; 95(1): 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rerimoi AJ, Jasseh M, Agbla SC, et al. Under-five mortality in The Gambia: comparison of the results of the first demographic and health survey with those from existing inquiries. PLoS ONE 2019; 14(7): e0219919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Midi H, Sarkar SK, Rana S. Collinearity diagnostics of binary logistic regression model. J Interdiscip Math 2010; 13(3): 253–267. [Google Scholar]
- 35. Mamoro MD, Hanfore LK. Tetanus toxoid immunization status and associated factors among mothers in Damboya Woreda, Kembata Tembaro Zone, SNNP, Ethiopia. J Nutr Metab 2018; 2018: 2839579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Akowuah JA, Agyei-Baffour P, Awunyo-Vitor D. Determinants of antenatal healthcare utilisation by pregnant women in third trimester in Peri-urban Ghana. J Trop Med 2018; 2018: 1673517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Okedo-Alex IN, Akamike IC, Ezeanosike OB, et al. Determinants of antenatal care utilisation in sub-Saharan Africa: a systematic review. BMJ Open 2019: 9(10): e031890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Alanazy W, Brown A. Individual and healthcare system factors influencing antenatal care attendance in Saudi Arabia. BMC Health Serv Res 2020; 20(1): 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tekelab T, Chojenta C, Smith R, et al. Factors affecting utilization of antenatal care in Ethiopia: a systematic review and meta-analysis. PLoS ONE 2019; 14(4): e0214848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ibrahim H, Maya ET, Issah K, et al. Factors influencing uptake of intermittent preventive treatment of malaria in pregnancy using sulphadoxine pyrimethamine in Sunyani Municipality, Ghana. Pan Afr Med J 2017; 28: 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Protas J, Tarimo D, Moshiro C. Determinants of timely uptake of ITN and SP (IPT) and pregnancy time protected against malaria in Bukoba, Tanzania. BMC Res Notes 2016; 9: 318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Azizi SC, Chongwe G, Chipukuma H, et al. Uptake of intermittent preventive treatment for malaria during pregnancy with Sulphadoxine-Pyrimethamine (IPTp-SP) among postpartum women in Zomba District, Malawi: a cross-sectional study. BMC Pregnancy Childbirth 2018; 18(1): 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392(10159): 1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Arnaldo P, Rovira-Vallbona E, Langa JS, et al. Uptake of intermittent preventive treatment and pregnancy outcomes: health facilities and community surveys in Chókwè district, southern Mozambique. Malar J 2018; 17(1): 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ozodiegwu ID, Doctor HV, Quinn M, et al. Is the positive association between middle-income and rich household wealth and adult sub-Saharan African women’s overweight status modified by the level of education attainment? A cross-sectional study of 22 countries. BMC Public Health 2020; 20: 996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Adebowale SA, Adedini SA, Ibisomi LD, et al. Differential effect of wealth quintile on modern contraceptive use and fertility: evidence from Malawian women. BMC Womens Health 2014; 14(1): 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mihret MS, Limenih MA, Gudayu TW. The role of timely initiation of antenatal care on protective dose tetanus toxoid immunization: the case of northern Ethiopia post natal mothers. BMC Pregnancy Childbirth 2018; 18(1): 235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Naeem M, Khan MZ, Abbas SH, et al. Coverage and factors associated with tetanus toxoid vaccination among married women of reproductive age: a cross sectional study in Peshawar. J Ayub Med Coll Abbottabad 2010; 22(3): 136–140. [PubMed] [Google Scholar]
- 49. Haile ZT, Chertok IRA, Teweldeberhan AK. Determinants of utilization of sufficient tetanus toxoid immunization during pregnancy: evidence from the Kenya Demographic and Health Survey, 2008–2009. J Community Health 2013; 38(3): 492–499. [DOI] [PubMed] [Google Scholar]
- 50. Ekholuenetale M, Nzoputam CI, Barrow A. Prevalence and socioeconomic inequalities in eight or more antenatal care contacts in Ghana: findings from 2019 population-based data. Int J Womens Health 2021; 13: 349–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Maral I, Baykan Z, Aksakal FN, et al. Tetanus immunization in pregnant women: evaluation of maternal tetanus vaccination status and factors affecting rate of vaccination coverage. Public Health 2001; 115(5): 359–364. [DOI] [PubMed] [Google Scholar]
- 52. Karlsen S, Say L, Souza JP, et al. The relationship between maternal education and mortality among women giving birth in health care institutions: analysis of the cross sectional WHO Global Survey on Maternal and Perinatal Health. BMC Public Health 2011; 11: 606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ekholuenetale M, Nzoputam CI, Barrow A, et al. Women’s enlightenment and early antenatal care initiation are determining factors for the use of eight or more antenatal visits in Benin: further analysis of the Demographic and Health Survey. J Egypt Public Health Assoc 2020; 95: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Yaya S, Bishwajit G. Trends in the prevalence and care-seeking behaviour for acute respiratory infections among Ugandan infants. Glob Health Res Policy 2019; 4: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Yaya S, Oladimeji O, Oladimeji KE, et al. Determinants of prenatal care use and HIV testing during pregnancy: a population-based, cross-sectional study of 7080 women of reproductive age in Mozambique. BMC Pregnancy Childbirth 2019; 19(1): 354. [DOI] [PMC free article] [PubMed] [Google Scholar]