Abstract
Objective:
This study determined the incidence rates for obesity among adult patients ages 20 and older empaneled in primary care practice in Midwest United States to potentially identify an optimum timeframe for initiating intervention.
Background:
Primary care practice patients are likely to reflect underlying community trends in overweight and obesity; however, data on overweight and obesity in primary care patients is limited. While childhood incidence rates of obesity have been well reported, there is still a paucity of data on the incidence of obesity among adult population; literature has mainly focused on its prevalence.
Methods:
Medical record review of identified cohort with BMI data was conducted. Population was stratified by age and sex and overweight category was subdivided into tertiles.
Results:
Majority of 40 390 individuals who comprised the final population and had follow-up data, consisted of adults ages 40 to 69 years (47.5%), female (59.8%) of non-Hispanic ethnicity (95.9%) with 21 379 (52.8%) falling in weight category of overweight. Incidence of obesity was 7% at 1 year and 16% at 3 years follow-up. Highest percentages of individuals who became obese at 1 and 3 years were in age category of 40 to 69 years among men and 20 to 39 years among women. In Cox regression analysis, there was statistically significant association to developing obesity among all tertile groups in the overweight category. Age and particularly gender appeared to be modifying factors to likelihood of developing obesity.
Conclusion:
Study results suggest that while obesity incidence is higher among certain age groups in both genders, middle-aged women, and men in all tertiles of overweight category are at highest risk and may be the optimum population to target for weight loss interventions. Findings support the initiation of population-based interventions before onset of obesity.
Keywords: obesity, incidence, primary care, adults, population health
Background
The worldwide prevalence of obesity has nearly tripled between 1975 and 2016. 1 About 13% of the world’s adult population was obese in 2016. 2 Compared to these numbers, the United States had a three-fold higher rate for obesity among adults (42.4% of adults aged 20 and over) from 2017 to 2018. 3 In the state of Minnesota, adult obesity prevalence in 2018 was 30.1%. 4
Obesity has been associated with at least 60 chronic health conditions including heart disease, stroke, diabetes mellitus type 2, obstructive sleep apnea, and certain cancers.5,6
It has also been associated with an increased risk for death, particularly among adults younger than 65 years. The United States Preventive Services Task Force (USPSTF) has therefore recommended that clinicians offer or refer adults with a body mass index (BMI) of 30 or higher (calculated as weight in kilograms divided by height in meters squared) to intensive, multicomponent behavioral interventions. 7
Primary care practice patients are likely to reflect underlying community trends in overweight and obesity; however, data on overweight and obesity in primary care patients is limited. Between 1999 and 2001, over 60% of patients seen in any primary care practice had either overweight or obesity. 8 Along with the rising prevalence of obesity nationwide, this percentage is expected to have increased in recent years. While childhood incidence rates of obesity have been well reported, there is still a paucity of data on the incidence of obesity among adult population particularly in primary care setting; literature has mainly focused on its prevalence.9,10 Since incidence describes how quickly a condition or disease occur in a population, it is a more useful indicator in influencing decision making and identifying what public health interventions should be adopted. Studies of childhood obesity have also shown a declining incidence with age 9 ; the trend among adults is not largely known.
Mayo Clinic Employee and Community Health (ECH) practice which has over 80 000 empaneled adult patients served in its primary care clinics, has no structured weight management program in place. Several evidence-based interventions such as the IBT (Intensive Behavioral Therapy), DPP (Diabetes Prevention Program), motivational interviewing, and comprehensive lifestyle modification programs, have been showed to be effective for obesity management in primary care.11-13 Using an App to deliver obesity treatment in socioeconomically disadvantaged patients had shown promise. 14 These are all management strategies that can potentially be adopted in the practice. As an initial step in designing a patient centered weight management program in primary care, it was important to define the characteristics of the community served by the practice. This study therefore aimed to determine the prevalence of overweight and obesity among adult patients ages 20 and older empaneled in ECH in 2015, as well as the 1- and 3-year incidence of obesity in this population group in order to potentially identify an optimum timeframe for initiating weight loss intervention.
Methods
In this retrospective cohort study, we identified adult community dwelling patients 20 years or older, empaneled with ECH (comprised of Family Medicine practice and Community Internal Medicine practice) in 2015, who had at least 1 BMI data available within a 5-year range (1/2010-1/2015) and who gave permission for their medical records to be used for research. For those with multiple BMI measurements, the BMI measurement closest to January 1, 2015 was used. BMI is a person’s weight in kilogram divided by the square of height in meters and is the most commonly used measure in population assessment of overweight and obesity. 15 Based on BMI, overweight is categorized as BMI of 25 to 29.9, Class 1 Obesity: 30 to 34.9, Class II Obesity: 35 to 39.9, and Class III Obesity: 40 and above. The tertile categorization was chosen to allow for as closely even distribution of individuals who have overweight.
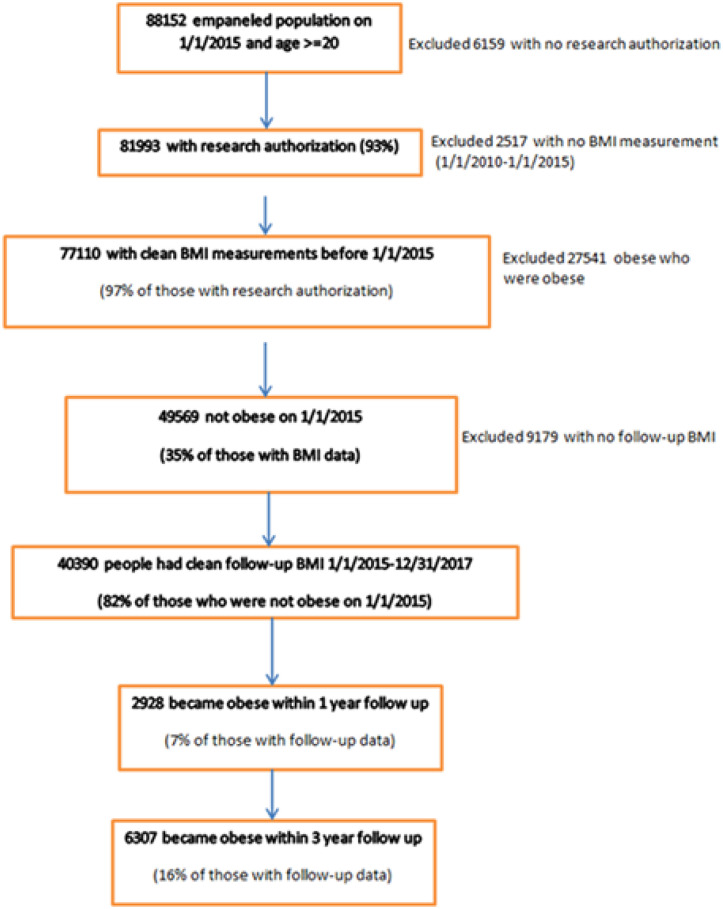
As of January 1, 2015, ECH had 88 152 empaneled patients aged 20 years and older; 93% (N = 81 993) had given authorization for their records to be accessed for research. After excluding those who had obesity or had no BMI measurement as well as those with no follow-up BMI data and outliers, the final number of people with follow-up data was 40 390. There was no difference in demographic characteristics between those who had obesity and therefore were excluded and those who were included in incidence analysis. We then determined the 1 and 3 years incidence rates of developing obesity in this population based on BMI data of individuals measured within a year from 1/1/2015 and from those measured within 3 years, but not necessarily within a year from baseline (Figure 1). We further stratified the population by age and sex to see if certain demographic characteristics were associated with rate of progression from being overweight to obesity. We used tertiles for the following BMI distributions: overweight 1: 25 ≤ BMI < 26.7; overweight 2: 26.7 ≤ BMI < 28.3; overweight 3: 28.3 ≤ BMI < 30. The study was reviewed and approved by the Mayo Clinic Institutional Review Board (IRB).
Figure 1.
Flow Diagram.
Statistical Analysis
Demographic characteristics were reported as number (percent) for the final cohort with 3 years of BMI follow-up data (N = 40 390). The age/sex specific incidence of becoming obese in 1 (or 3) years was determined by dividing the number who became obese in the age (20-39, 40-69, 70+) group/sex in 1 (or 3) years by the corresponding age group/sex total population. Because the hazard ratios (HRs) were heterogeneous across age/sex groups, separate cox proportional hazard regression were fit on subsets of the population grouped by sex and age on January 1, 2015. Predictors in the model were race (White, Black, Asian, Other/Unknown), ethnicity (Hispanic, Not Hispanic), and BMI (Underweight/Normal Weight, Overweight tertiles (25 ≤ BMI < 26.7, 26.7 ≤ BMI < 28.3, and 28.3 ≤ BMI < 30). Follow-up began January 1, 2015 and continued until death, last clinical encounter, or 1 (or 3) years of follow-up, whichever came first. Analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, NC).
Results
At baseline 27 541 adult patients empaneled to ECH (35% of those with BMI data) had a BMI of ≥30 and were therefore categorized to have obesity, its prevalence in this population. These individuals were excluded in the determination of incidence rates. Overall, 40 390 individuals had follow-up data and comprised the final study population. Majority of this population consisted of adults ages 40 to 69 years (47.5%), female (59.8%) of non-Hispanic ethnicity (95.9%) with 21 379 (52.8%) falling in the weight category of overweight (Table 1).
Table 1.
Demographics.
| Final number of people (%) with follow up data N = 40 390 | |
|---|---|
| Age | |
| 20-39 | 13 622 (33.73%) |
| 40-69 | 19 201 (47.54%) |
| 70+ | 7567 (18.73%) |
| Sex | |
| Male | 16 241 (40.21%) |
| Female | 24 149 (59.79%) |
| Race | |
| White | 35 892 (88.86%) |
| Black | 1151 (2.85%) |
| Asian | 1863 (4.61%) |
| Other/Unknown | 1484 (3.67%) |
| Ethnicity | |
| Not Hispanic | 38 729 (95.89%) |
| Hispanic | 700 (1.73%) |
| Unknown | 961 (2.38%) |
| BMI | |
| Underweight/Normal weight | 19 011 (47.07%) |
| Overweight tertile1* | 7377 (18.26%) |
| Overweight tertile2* | 7191 (17.80%) |
| Overweight tertile3* | 6811 (16.86%) |
Cut points of overweight 1, 2, 3 are based on tertiles of the follow-up distributions:
overweight 1: 25 ≤ BMI < 26.7; overweight 2: 26.7 ≤ BMI < 28.3; overweight 3: 28.3 ≤ BMI < 30.
At 1 year follow up, 2928 individuals (7%) had developed obesity and 6307 (16%) had developed obesity within 3 years of follow up (Figure 1). The highest percentages of individuals who became obese at 1 and 3 years follow-up were in the age category of 40 to 69 years among men and 20 to 39 years among women (Table 2).
Table 2.
Counts and Incidence Rates for Number Who Become Obese Stratified by Age and Sex.
| Men 20-39 | Men 40-69 | Men 70+ | Women 20-39 | Women 40-69 | Women 70+ | |
|---|---|---|---|---|---|---|
| 1 year follow-up | ||||||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Became obese | 304 (9.73%) | 666 (12%) | 327 (11.8%) | 591 (9.52%) | 717 (8.59%) | 323 (8.35%) |
| 3-year follow-up | ||||||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Became obese | 735 (14.53%) | 1476 (18.38%) | 586 (18.57%) | 1302 (15.20%) | 1573 (14.08%) | 635 (14.40%) |
There was a significantly increased likelihood of developing obesity at 1 and 3 years among those who had overweight at baseline, with 1-year unadjusted hazard ratio (HR) of 13.4 (CI: 11.48-15.49) and 3-year HR of 11.9 (CI: 10.87-13.14) using WALD test. Persons of Black racial background were at increased risk of becoming obese (HR: 1.3 and 1.2 at 1 and 3 years, unadjusted). In contrast, there was decreased likelihood of developing obesity among those of Asian race (unadjusted HR: 0.4 and 0.5 at 1 and 3 years) (Data available upon request).
In cox regression analysis, after stratifying by age and sex, there remained a statistically significant association to developing obesity among the overweight tertile groups (P value <.0001) with the greatest association seen among those in the third tertile of overweight category regardless of age or sex (Figure 2). While the trajectory of the 2 plots were similar, the rates looked incongruent because of different denominators; there was 35% more individuals with BMI measured at 3-year incidence measurement than at 1 year. The positive association to likelihood of developing obesity was no longer statistically significant among Black men; in contrast, there remained an increased likelihood of developing obesity in Black women ages 40 to 69 years but only at 1 year (HR: 1.2; 95% CI: 1.02-2.25). At 3 years, this association was no longer significant. The association between being of Asian race and decreased likelihood of developing obesity was still present but no longer statistically significant except among Asian men ages 40 to 69 and Asian women ages 20 to 39 at 3 years follow-up. Using normal and underweight categories as reference, the highest risk of progression to obesity was seen in women ages 40 to 69 who were in the third overweight tertile (28.3 ≤ BMI < 30) with a HR of 62.3 (CI: 49.37-78.64). Since there were very few individuals in the underweight category, they were combined with those of normal body weight and used as reference (Table 3).
Figure 2.
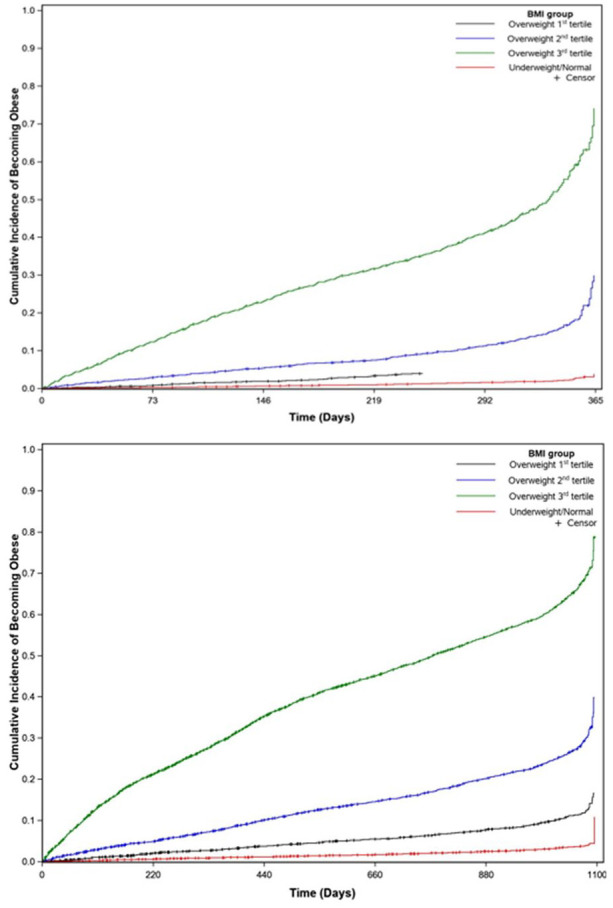
Obesity incidence association to weight tertile at 1 and 3 years follow-up.
Table 3.
Associations With Becoming Obese During Follow-Up Stratified by Age and Sex on January 1, 2015, in Separate Cox Regression Analysis at 1 and 3 years.
| Men 20-39 | Men 40-69 | Men 70+ | Women 20-39 | Women 40-69 | Women 70+ | |
|---|---|---|---|---|---|---|
| HR 95% CI | HR 95% CI | HR 95% CI | HR 95% CI | HR 95% CI | HR 95% CI | |
| 1 year follow-up | ||||||
| Race White | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 1.13 (0.67, 1.90) | 0.68 (0.38, 1.21) | 1.76 (0.78, 3.95) | 0.94 (0.67, 1.32) | 1.52 (1.02, 2.25) | 0.59 (0.08, 4.18) |
| Asian | 0.40 (0.16, 0.97) | 0.78 (0.47, 1.28) | 1.32 (0.49, 3.54) | 0.68 (0.41, 1.13) | 0.67 (0.40, 1.12) | 0.98 (0.36, 2.63) |
| Other/Unknown | 1.00 (0.57, 1.73) | 0.76 (0.42, 1.38) | 0.62 (0.19, 2.04) | 1.04 (0.71, 1.53) | 1.43 (0.90, 2.30) | 0.95 (0.24, 3.81) |
| Ethnicity | ||||||
| Hispanic | Ref | Ref | Ref | Ref | Ref | Ref |
| Not Hispanic | 1.01 (0.51, 1.97) | 1.80 (0.94, 3.47) | 2.23 (0.77, 6.42) | 0.74 (0.44, 1.24) | 0.79 (0.45, 1.41) | NA a |
| BMI b | ||||||
| Underweight/Normal | Ref | Ref | Ref | Ref | Ref | Ref |
| Overweight-1 | 2.67 (1.46, 4.89) | 2.09 (1.16, 3.75) | 1.10 (0.40, 3.05) | 4.60 (3.44, 6.16) | 3.31 (2.04, 5.36) | 5.22 (2.68, 10.16) |
| Overweight-2 | 8.75 (5.28, 14.51) | 6.46 (3.91, 10.68) | 7.78 (3.69, 16.40) | 7.96 (6.11, 10.37) | 13.52 (9.15, 19.99) | 12.12 (6.63, 22.14) |
| Overweight-3 | 36.56 (23.05, 57.98) | 37.17 (23.21, 59.55) | 46.99 (23.18, 95.25) | 22.06 (17.36, 28.02) | 61.83 (42.99, 88.91) | 63.89 (36.50, 111.82) |
| P-value c | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 |
| 3-year follow-up | ||||||
| Race White | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 1.10 (0.77, 1.56) | 0.90 (0.65, 1.25) | 1.37 (0.68, 2.76) | 1.09 (0.85, 1.39) | 1.10 (0.81, 1.49) | 0.80 (0.40, 1.61) |
| Asian | 0.64 (0.41, 1.01) | 0.63 (0.43, 0.93) | 1.43 (0.71, 2.89) | 0.56 (0.39, 0.79) | 0.76 (0.54, 1.05) | 0.60 (0.15, 2.41) |
| Other/Unknown | 1.28 (0.91, 1.82) | 0.82 (0.57, 1.20) | 1.28 (0.60, 2.70) | 1.07 (0.82, 1.39) | 1.19 (0.86, 1.63) | 0.95 (0.39, 2.32) |
| Ethnicity | ||||||
| Hispanic | Ref | Ref | Ref | Ref | Ref | Ref |
| Not Hispanic | 1.21 (0.79, 1.84) | 1.31 (0.84, 2.04) | 1.26 (0.48, 3.31) | 0.83 (0.57, 1.19) | 1.01 (0.69, 1.46) | 1.12 (0.35, 3.66) |
| BMI | ||||||
| Underweight/Normal | Ref | Ref | Ref | Ref | Ref | Ref |
| Overweight-1 | 2.47 (1.79, 3.43) | 2.34 (1.58, 3.46) | 1.75 (0.99, 3.09) | 5.16 (4.27, 6.24) | 4.87 (3.67, 6.47) | 3.06 (2.14, 4.39) |
| Overweight-2 | 8.37 (6.38, 11.00) | 8.38 (5.97, 11.77) | 7.07 (4.44, 11.25) | 10.19 (8.57, 12.13) | 17.06 (13.35, 21.80) | 6.82 (4.97, 9.35) |
| Overweight-3 | 25.30 (19.62, 32.63) | 40.73 (29.45, 56.33) | 33.85 (21.76, 52.66) | 21.76 (18.48, 25.63) | 62.31 (49.37, 78.64) | 28.78 (21.66, 38.23) |
| P-value | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 |
Limited number of events.
Cut-points of overweight 1, 2, 3 are based on tertiles of the follow-up distributions:
overweight 1: 25 ≤ BMI < 26.7; overweight 2: 26.7 ≤ BMI < 28.3; overweight 3: 28.3≤ BMI < 3.
P-value for test for trend across overweight groups.
Discussion
This study was conducted using a large U.S. based population cohort to determine the incidence rates among adults at 1 and 3 years of follow-up. To the authors’ knowledge, no similar studies had previously been reported. Of the 40 390 individuals who were not obese at their index date, the incidence of obesity was 7% at 1 year and 16% at 3 years follow-ups. These figures are higher when compared to childhood obesity incidence reported in the United States and elsewhere.9,16 In a systematic review of 19 childhood obesity incidence studies conducted in the United States, the median study-specific annual obesity incidences among studies using U.S. Centers for Disease Control and Prevention (CDC) growth charts were 4.0%, 3.2%, and 1.8% for preschool (2.0-4.9 years), school aged (5.0-12.9 years), and adolescence (13.0-18.0 years), respectively. 9 Also, in contrast to childhood obesity incidence which showed a downward trend from preschool to adolescence,9,10,16 adult obesity incidence in this study appeared to show an upward trend from 1 to 3 years. Using data from the Early Childhood Longitudinal Study, Cunningham et al 10 reported that the annual incidence of obesity decreased from 5.4% during kindergarten to 1.7% between fifth and eighth grade. Interestingly, that study showed that among children who became obese between the ages of 5 and 14 years, 75% had been above the 70th percentile for body-mass index at baseline, a similar observation seen in this study among adults in the third tertile group of overweight category.
When stratified by age and sex, some variations in incidence rate at 1 and 3 years were noted between men and women. Age and particularly sex appeared to be modifying factors to the likelihood of developing obesity; women who were overweight at baseline and in the age range of 40 to 69 years, were more likely to develop obesity at 1 and 3 years than men within the same age group. Women within this age range transition into menopause, a period in women’s life which has been associated with weight gain, and is a likely contributing factor to this observation. 17 This higher risk burden for obesity in females had been observed equally in both urban and rural settings. 18 Female gender, along with baseline BMI, had likewise been associated with higher odds of incident obesity phenotype among healthy non-obese individuals. 19 In contrast, analysis of epidemiological obesity among adults 20 years and older in European countries showed that the dynamics of obesity growth from 1999 to 2016 was greater for men than for women with rate of 3.09% per year in men compared to 1.92% per year in women. At this rate, more adult men were predicted to have obesity by 2030 than women in Europe. 20 Overall prevalence of overweight and obesity among a studied mid-eastern population was likewise higher in men compared to women. 21 In the United States, the highest prevalence of obesity among adults 20 years and older in 2017 to 2018 by age and sex was among men in the age category of 40 to 59 years. 3 Interestingly, this present study also showed a higher percentage of men than woman who developed obesity at 1 and 3 years, particularly in age category of 40 to 69 years (12% vs 8.6% and 18.4% vs 14.1% respectively) (Table 2). Hence, while the likelihood and risk of developing obesity among individuals who are overweight may be higher in women, the dynamics of obesity growth appeared to be faster among men leading to higher incidence rates of obesity in men. Further research may be needed to identify variables that would account for this paradoxical observation.
Overweight remained a major risk factor for developing obesity even after stratification by age and sex, with the greatest risk in the tertile of overweight 3: 28.3 ≤ BMI < 30. This observation has been reported in other studies; in particular, the association between higher BMI in childhood and adolescence with development of obesity in adulthood has previously been explored.16,22,23 Whether there is a difference in progression to various disease entities between overweight and obesity is less clearly delineated. Most studies had bundled overweight and obesity together in correlational analyses to morbidities such as cancer, chronic kidney disease, fatty liver disease, diabetes, and heart disease.24-26 Significant changes in lifestyle habits, that is, dietary pattern and physical activity, have been observed across the stages of obesity which appeared to alter the correlation to obesity associated chronic diseases; those at higher or severe stage of obesity had heavier chronic disease burden. 27 It would be interesting to determine if lifestyle behavior differs between individuals in overweight and obesity categories and if each weight category separately impact disease development.
The disease and economic burden of obesity are no lightweight matter. 28 With overweight identified as the most significant independent risk factor to developing obesity, this study lend further support to initiating weight loss interventions at an earlier stage when they would be most beneficial and not wait until an individual develop obesity.
This study was conducted using a large primary care cohort to determine the incidence rates among adults at 1 and 3 years. While majority of the cohort were Caucasians and non-Hispanics, the minority groups had adequate representation which strengthens the generalizability of the findings. This study also showed the association of incidence rates with several demographic factors, particularly, which has not been examined before on a large scale. However, other potential variables that may affect incidence rates such as waist circumference, socio-economic status, medications, co-morbidities, and physical activity were not captured. Generalizability of findings to more heterogeneous, multi-cultural population may be limited. Incidence determination only covered a period of 3 years; a longer time frame might have yielded different results.
Summary
In this study, the prevalence of obesity among community dwelling adults ages 20 and above is 35%. At 1 and 3 years, the incidence rates for obesity were 7% and 16% respectively. There was a statistically significant association to developing obesity among the overweight tertile groups (P value <.0001) with the greatest association seen among those in the third tertile of overweight category even after stratifying by age and sex. Gender, in particular, appeared to be a modifying factor to the likelihood of developing obesity; higher risk burden for obesity was seen in females than males yet the percentage of men who developed obesity at 1 and 3 years was higher than women. Hence, while the likelihood of developing obesity among individuals who are overweight may be higher in women, the dynamics of obesity growth appeared to be faster among men. Additional large, population-based studies will help elucidate further the gender differences in obesity risk. Data from this study suggests that middle aged women and men in all tertiles but particularly in the third tertile of overweight category may be the optimum population to target for weight loss interventions and implies that weight loss intervention may be best initiated prior to onset of obesity.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by funding from the Population Health Scholar Program of the Robert D. and Patricia E. Kern Center of the Science of Health Care Delivery. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Robert D. and Patricia E. Kern Center of the Science of Health Care Delivery.
Ethical Consideration: Only the medical records of eligible subjects who gave consent to have their records accessed for research purposed were reviewed.
ORCID iDs: Ramona S. DeJesus  https://orcid.org/0000-0003-0216-5223
https://orcid.org/0000-0003-0216-5223
Ivana T. Croghan  https://orcid.org/0000-0003-3464-3525
https://orcid.org/0000-0003-3464-3525
References
- 1. NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387:1377-1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization (WHO). Obesity and overweight fact sheet. 2020. Accessed October 12, 2021. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- 3. Center for Disease Control. Adult obesity facts. 2020. Accessed October 12, 2021. http://www.cdc.gov/obesity/data/adult.html
- 4. Minnesota Department of Health. Obesity quick facts. 2018. Accessed October 12, 2021. https://www.health.state.mn.us/people/obesity/docs/obesitydata2018.pdf
- 5. Torres-de la, Roche LA, Steljes I, Janni W, Friedl TWP, De Wilde RL. The association between obesity and premenopausal breast cancer according to intrinsic subtypes – a systematic review. Geburtshilfe Frauenheilkd. 2020;80:601-610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bendor CD, Bardugo A, Pinhas-Hamiel O, Afek A, Twig G. Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc Diabetol. 2020;19:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. United States Preventive Services Task Force (USPSTF). Weight loss to prevent obesity-related morbidity and mortality in adults: behavioral interventions. 2018. Accessed November 6, 2020. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/obesity-in-adults-interventions
- 8. Stecker T, Sparks S. Prevalence of obese patients in a primary care setting. Obesity. 2006;14:373-376. [DOI] [PubMed] [Google Scholar]
- 9. Cheung PC, Cunningham SA, Narayan KM, Kramer MR. Childhood obesity incidence in the United States: a systematic review. Child Obes. 2016;12:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370:403-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Semlitsch T, Stigler FL, Jeitler K, Horvath K, Siebenhofer A. Management of overweight and obesity in primary care-a systematic overview of international evidence-based guidelines. Obes Rev. 2019;20:1218-1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wadden TA, Tsai AG, Tronieri JS. A protocol to deliver intensive behavioral therapy (IBT) for obesity in primary care settings: the MODEL-IBT program. Obesity. 2019;27:1562-1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barnes RD, Ivezaj V. A systematic review of motivational interviewing for weight loss among adults in primary care. Obes Rev. 2015;16(4):304-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bennett GG, Steinberg D, Askew S, et al. Effectiveness of an app and provider counseling for obesity treatment in primary care. Am J Prev Med. 2018;55:777-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Center for Disease Control. Healthy weight. 2020. https://www.cdc.gov/healthyweight/assessing/index.html
- 16. Ikeda N, Nishi N. First incidence and associated factors of overweight and obesity from preschool to primary school: longitudinal analysis of a national cohort in Japan. Int J Obes. 2019;43:751-760. [DOI] [PubMed] [Google Scholar]
- 17. Al-Safi ZA, Polotsky AJ. Obesity and menopause. Best Pract Res Clin Obstet Gynaecol. 2015;29:548-553. [DOI] [PubMed] [Google Scholar]
- 18. Nansseu JR, Noubiap JJ, Bigna JJ. Epidemiology of overweight and obesity in adults living in Cameroon: a systematic review and meta-analysis. Obesity. 2019;27:1682-1692. [DOI] [PubMed] [Google Scholar]
- 19. Eftekharzadeh A, Asghari G, Serahati S, et al. Predictors of incident obesity phenotype in nonobese healthy adults. Eur J Clin Invest. 2017;47:357-365. [DOI] [PubMed] [Google Scholar]
- 20. Krzysztoszek J, Laudańska-Krzemińska I, Bronikowski M. Assessment of epidemiological obesity among adults in EU countries. Ann Agric Environ Med. 2019;26:341-349. [DOI] [PubMed] [Google Scholar]
- 21. Al-Qahtani AM. Prevalence and predictors of obesity and overweight among adults visiting primary care settings in the southwestern region, Saudi Arabia. Biomed Res Int. 2019;2019:8073057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kartiosuo N, Ramakrishnan R, Lemeshow S, et al. Predicting overweight and obesity in young adulthood from childhood body-mass index: comparison of cutoffs derived from longitudinal and cross-sectional data. Lancet Child Adolesc Health. 2019;3:795-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ryder JR, Jacobs DR, Jr, Sinaiko AR, Kornblum AP, Steinberger J. Longitudinal changes in weight status from childhood and adolescence to adulthood. J Pediatr. 2019;214:187-192.e2. [DOI] [PubMed] [Google Scholar]
- 24. Nowak KL, You Z, Gitomer B, et al. Overweight and obesity are predictors of progression in early autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2018;29:571-578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Middeldorp ME, Pathak RK, Meredith M, et al. PREVEntion and regReSsive effect of weight-loss and risk factor modification on atrial fibrillation: the REVERSE-AF study. Europace. 2018;20:1929-1935. [DOI] [PubMed] [Google Scholar]
- 26. Argolo DF, Hudis CA, Iyengar NM. The impact of obesity on breast cancer. Curr Oncol Rep. 2018;20:47. [DOI] [PubMed] [Google Scholar]
- 27. Cha E, Akazawa MK, Kim KH, et al. Lifestyle habits and obesity progression in overweight and obese American young adults: lessons for promoting cardiometabolic health. Nurs Health Sci. 2015;17(4):467-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tremmel M, Gerdtham UG, Nilsson PM, Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14:435. [DOI] [PMC free article] [PubMed] [Google Scholar]