Abstract
Mild cognitive impairment (MCI) or dementia often leads to behavioral and psychiatric symptoms of dementia (BPSD). Sensory processing abnormalities may be associated with BPSD. The purpose of this study was to explore relationships among sensory processing, behavior, and environmental features within the homes of people with MCI or dementia. This project used mixed methods to assess participants’ sensory processing, care partner perspectives on behaviors, and in situ observations of the home environment. Nine participants with cognitive impairment (MCI n = 8, early dementia = 1) and their care partners were included. Seven participants with cognitive impairment were reported to have abnormal sensory processing. Findings suggest that unique environmental adaptations, tailored to personal and sensory preferences for each participant, were associated with a decreased level of behavioral disruption during the observation periods. Implementing sensory-based approaches to maximize environment adaptation may be beneficial in reducing disruptive behaviors for adults with cognitive impairment.
Introduction
One in nine individuals over the age of 65 have mild cognitive impairment (MCI) or Alzheimer’s disease or related dementias (ADRD), and as many as one in three over the age of 85 have these conditions (Alzheimer’s Association, 2020). Including persons with MCI, nearly 90% of individuals with these diagnoses demonstrate behavioral and psychiatric symptoms of dementia (BPSD) (Gerlach & Kales, 2020; Zhao et al., 2016). Often BPSD, such as agitation, anxiety, apathy, and depression, present in early stages of cognitive impairment including MCI and can be a precursor to severity of ADRD (Sun et al., 2021; Wise et al., 2019; Zhao et al., 2016). These symptoms interfere with optimal care provision, decrease functional independence, result in inappropriate use of antipsychotic medications, and reduce quality of life for both persons with cognitive impairment and their care partners (Kales et al., 2014).
The Science of Behavior Change program (Nielsen et al., 2018), endorsed by the National Institutes of Health, suggests that behavioral scientists need to identify mechanisms of action which influence behavior and to determine appropriate assessment of such mechanisms. Identification of underlying mechanisms contributing to BPSD is needed to improve care and behavior science (Topaz et al., 2020; Nielsen et al., 2018). National and international agencies recognize a strong need for nonpharmacological interventions, including environmental assessment and modification, as first-line treatment for BPSD in ADRD (Gitlin et al., 2012; Zeisel et al., 2003). However, lack of assessments and interventions to guide and apply such approaches severely limit real-world implementation (Padilla, 2011). To fill this gap, innovative methodologies are needed to define mechanisms of BPSD.
The current study was influenced by mechanisms established by environmental gerontologists who have long recognized behavior as a product of environmental interaction. In 1936, Lewin defined (B)ehavior as a (f)unction of the (P)erson and (E)nvironment: B = f (P, E) (Lewin, 1936). Building on this, Lawton and Nahemow (1973) developed the Ecological Model of Aging which depicts zones of adaptive behavior when environmental factors/demands are aligned with a person’s capability. This model identifies zones of maximum comfort and performance when environmental factors are consonant with individual ability. Person-environment fit, as identified in this model, informs pragmatic development of assessment and intervention for community-residing adults with ADRD. However, there is sparse evidence for the combined effects of environmental factors on behavioral regulation and performance for people with ADRD (Jensen & Padilla, 2017; Magasi et al., 2015).
Neurobehavioral disruptions, including BPSD, may be a manifestation of sensory impairment and/or sensory processing abnormalities (Gerlach & Kales, 2020; Luo et al., 2018; Pinto et al., 2017; Sánchez et al., 2016). For example, agitation may occur in response to overstimulation, and wandering may be a self-initiated attempt to increase sensory stimulation (Ravn et al., 2018). Behaviors related to sensory processing are unique to the individual and reflect personal preferences, prior experiences, and neurological needs (Dunn, 1997; Kovach et al., 2004). Such behaviors have been described as patterns which reflect sensory processing abilities and have been classified within four categories: low registration; sensation seeking; sensory sensitivity; and sensation avoiding (see Table 1) (Brown & Dunn, 2002; Dunn, 1997).
Table 1.
Adult Sensory Profile Questionnaire Domains, Behaviors, and Examples.
| Sensory Domain | Associated Behavior | Sample Statements from ASP |
|---|---|---|
| Low registration | Decreased awareness to sensory information and need for high intensity stimulation | I trip or bump into things. |
| I do not seem to notice when my face or hands are dirty. | ||
| Sensory seeking | Behaviors that seek out sensory stimuli | I add spice/herbs to my food. |
| I wear colorful clothing. | ||
| Sensory sensitivity | Likely to respond and be sensitive to low levels of sensory stimuli | I feel dizzy easily. |
| I am distracted when there is a lot of noise around. | ||
| Sensation avoiding | Tendency to control or avoid overwhelming sensory stimuli | I only eat familiar foods. |
| I stay away from crowds. |
Utilization of sensory processing considered in environmental context as an innovative approach for understanding BSPD may be appropriate and effective for persons with ADRD and their caregivers (Champagne, 2018; Ravn et al., 2018).
The aim of this study was to assess the presence of sensory processing abnormalities in older adults with cognitive impairment and evaluate the relationship among these abnormalities, environmental features, and behavior in their home environment.
Methods
Design
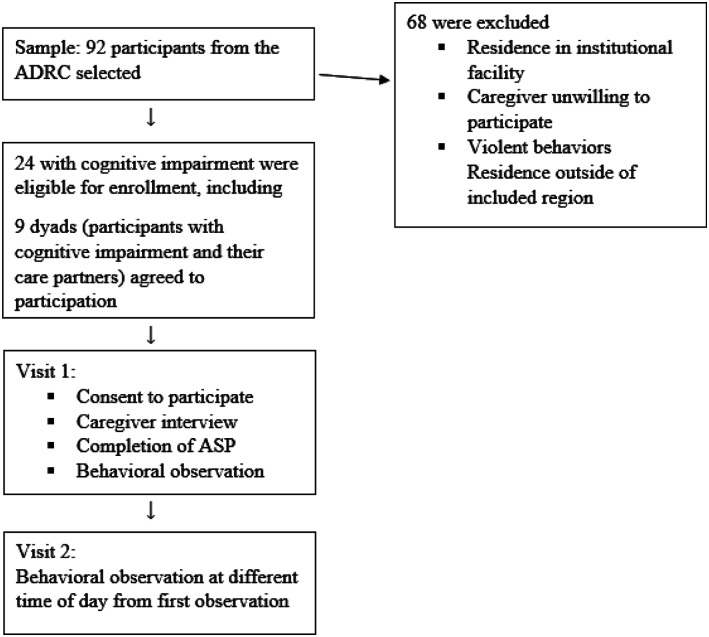
We used a mixed method approach involving descriptive quantitative evaluation of cognition and sensory processing and qualitative exploration of community-dwelling older adults with cognitive impairment through interviews with caregivers and in situ observation of behavior and environmental features in the home setting (see Figure 1). This approach was selected due to the complexity of the situational context. Using these methods increases rigor through triangulation of data sources and provides a pragmatic approach to investigating and interpretation of behavior in the context of which it occurs (Creswell, 2013; Morgan, 2007). Written consent for participation was obtained from care partners and the legally authorized representative of the person with cognitive impairment. Verbal assent for participation was obtained from those with cognitive impairment. All procedures were approved by the University Institutional Review Board.
Figure 1.
Recruitment and data collection.
Participants
All participants were enrolled in an Alzheimer’s Disease Research Center (ADRC) cohort (Schmitt et al., 2012). Purposeful sampling was used to recruit participants from the ADRC if they had a clinical diagnosis of MCI or dementia, were aged 65 years or older, were deemed appropriate for participation by a medical clinician or social worker from the ADRC, lived at home with a care partner who was willing to participate in this study, were able to speak and understand English, and resided in the same county as the research institution. Residence in the same county of the research institution was necessary to maintain feasible travel for in-home observations.
Diagnosis
The diagnosis of MCI was determined according to the consensus guidelines developed by the Second International Working Group on MCI (Winblad et al., 2004) and adopted by the National Institute on Aging-Alzheimer’s Association Workgroup on Diagnostic Guidelines for Alzheimer’s Disease as follows: (1) a cognitive complaint by the subject or informant, or evidence for longitudinal decline on cognitive test performance (at least 1.5 standard deviation decline); (2) generally intact global cognition; (3) no or minimal functional impairment; and (4) not demented according to DSM-IV criteria. Diagnosis of dementia was based on criteria set forth by the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) (American Psychiatric Association, 2013). Additional guidance by the National Institute for Aging and the Alzheimer’s Association (Albert et al., 2011) was used for MCI and ADRD diagnoses. All participants’ diagnoses were confirmed with a neurologist.
Quantitative Data Collection
Quantitative data was assembled from cross-sectional cognitive test scores and measurement of sensory processing. Cognitive test scores were collected from the ADRC database (test date within 24 months of observation) to supplement clinical diagnoses with methods described elsewhere (Schmitt et al., 2012). Measurement of sensory processing was collected at the time of participant observation. These descriptive quantitative measures are presented to provide a diagnostic description of the participants; statistical analyses, including power analysis and sample size calculation, were not conducted.
Cognitive assessment
The Clinical Dementia Rating (CDR) (Morris, 1993) scores from the most recent ADRC annual visit of each participant were extracted from the ADRC database and used to identify cognitive impairment severity to supplement the clinical diagnosis. CDR scores reflect participants’ status at the most recent ADRC visit (within 24 months) from the date of study enrollment. The CDR has high reliability and validity for assessment of cognitive function and serves as a primary tool in psychometric analysis of functional cognition of ADRD (Hughes et al., 1982; Morris, 1993). Six cognitive domains were assessed via caregiver interview during the CDR (memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care). Following the interview, each domain is rated on a 5-point scale indicating the level of impairment (0 = none, 0.5 = questionable, 1 = mild, 2 = moderate, and 3 = severe) based on standard rules.
Sensory processing
The Adult Sensory Profile (ASP) questionnaire was used to measure sensory processing (Brown et al., 2001). Participants or their primary care partner completed the 60-item ASP questionnaire, which is validated and reliable for use in older adults, including those with MCI and dementia (Chung, 2006; Engel-Yeger & Rosenblum, 2021). Each item describes a behavior attributed to sensory processing and results present sensory processing abilities among four categories (see Table 1). For the respondent, the ASP items are presented in groups, by sensory system (number of items): gustatory/olfactory (8), proprioceptive (8), visual (10), haptic (13), and auditory (11). The 10 remaining items are classified as activity level. Participants rate the frequency with which they engage in each behavior or they observe it in the participant, in the case of caregivers responding. Ratings for all items are summed within each sensory processing pattern to obtain summary scores (Brown et al., 2001). The summary score of each category is compared to normative data established via a national sample of same-aged adults (Dunn & Westman, 1997). Identification of more than one category outside of normative results was indicative of sensory processing abnormalities.
Qualitative Data Collection
A qualitative descriptive approach was used to describe the situation of each study participant. Prior to data collection, the first author used principles of bracketing and reflexivity to acknowledge their background as an occupational therapist which may introduce biases, such as emphasis on occupations and functional behaviors (Creswell, 2013). Avenues to ensure trustworthiness and consistency of findings included peer debriefing with AD researchers, constant comparison of emergent findings, and triangulation (Creswell, 2013).
Care partner interviews
Semi-structured interviews took place with the primary care partner (interview prompts included in Supplementary file). These interviews were designed to gain information regarding care partner observations of behaviors and environmental interaction. All interviews were audio recorded and transcribed verbatim by the first author.
Behavioral observation
In-home observations were undertaken after semi-structured interviews with care partners to discuss their perceptions of behaviors and interactions within the home environment by the person with cognitive impairment. The first author acted as a participant-observer, meaning that verbal interaction between the participant and observer occurred, if appropriate, but was not solicited. Second home visits were observation-only and were conducted at a different time of day than the first visit (morning vs. afternoon) to promote representation of behaviors throughout daylight hours.
In-home observations were documented via field notes and observation charts (see Table 2). These charts were developed from select items of the Neuropsychiatric Inventory (NPI) (Cummings, 1997) and In-Home Occupational Performance Evaluation (I-HOPE) (Stark et al., 2010). Items from the NPI were used to identify behaviors specific to cognitive impairment, including observation of the sleeping environment which might have contributed to nighttime behaviors. The NPI is a commonly used behavior assessment tool for persons with cognitive impairment (Cummings, 1997). Items from the I-HOPE were selected for observation data acquisition of environmental features that might influence behaviors.
Table 2.
Observation Chart Prompts Used for Data Collection.
| Assessment | Behavioral Signs |
|---|---|
| Neuropsychiatric Inventory (NPI) | Delusions/hallucinations, irritability, anxiety/agitation, depression/apathy, disinhibition, aberrant motor behaviors, appetite/eating changes, nighttime behaviors |
| In-Home Occupational Performance Evaluation (I-HOPE) | Lighting/sounds, smells/temperature, visual aids/distractions, position (seated/standing/mobile), inside/outside, time of day, access within and surrounding home, performance within environment (including decision making) |
| Social context | Caregiver present, interactions (empathy, theory of mind, facial recognition), lives with, alertness, communication (figurative language, nonverbal), response to social contact, participant’s mood, routine interactions |
Analysis
Mixed methods were used for data analysis. Quantitative measures were scored and used for descriptive purposes in combination with qualitative findings. Qualitative analyses used descriptive, case study analysis allowing for illustration of the situational context of the participants’ living environment in relation to their sensory processing and behavior. Data analysis began following the first interview and used a constant comparison approach with appropriate modifications following each field visit (Boeije, 2002). Peer debriefing with ADRC researchers and expert consulting with the ADRC clinical director (senior author) was used during data collection and analysis to ensure validity and rigor of data. Transcriptions were coded using HyperResearch 4.0.2 (Researchware, 2018).
Findings
Twenty-four individuals with cognitive impairment who were enrolled in the ADRC met inclusion criteria and were selected for recruitment. Of these, 11 were unable to be contacted and four declined participation. Common reasons for exclusion of potential participants included: recent move into facility-based care, death, and care partners’ refusal to participate.
Nine participants with cognitive impairment and their care partners agreed to study enrollment (Table 3; pseudonyms are used). All participants were in stable condition at the time of study participation without recent (4 weeks) exacerbations or onset of cognitive, behavioral, or medical conditions. Two participants (Charlotte and Ronald) were married, both with diagnosis of MCI, and both participated as cognitively impaired participants and simultaneously responded as one another’s care partner. Both were legally and cognitively able to make consent decisions for this study, and their family was aware of their participation. For purposes of data collection and presentation of findings, their personal experiences as a participant with cognitive impairment as well as insights from a care partner perspective were collected, and observations occurred simultaneously.
Table 3.
Participant Characteristics.
| Name | Age | Sex | Education (Years) | Race | Diagnosis | Global CDR | Care Partner | Length of Relationship (Years) |
|---|---|---|---|---|---|---|---|---|
| Betty | 73 | F | 18 | White | MCI | 0 | Samuel | 50 |
| Chris | 93 | M | 21 | White | MCI | 0 | Karen | 50 |
| Walter | 82 | M | 21 | Black | MCI | 0.5 | Laura | 48 |
| Charlotte | 88 | F | 13 | White | MCI | 0.5 | Ronald | 58 |
| Ronald | 83 | M | 13 | White | MCI | 0.5 | Charlotte | 58 |
| Adam | 85 | M | 21 | White | MCI | 0.5 | Ellen | 20 |
| Pamela | 67 | F | 12 | Black | MCI | 0.5 | Alex | 50 |
| Ricky | 81 | M | 16 | White | MCI | 0.5 | Janelle | 10 |
| Vicky | 81 | F | 12 | White | Dementia | 1 | John | 61 |
Notes. M = male; F = female; MCI = mild cognitive impairment; CDR = cognitive dementia rating.
Sixteen observations took place within participants’ homes. ASP summary scores indicated at least one sensory processing category deviated from the normative data of older adults for all nine participants (Table 4). Seven of the nine participants had two categories outside of normative data. Abnormalities with low registration were reported most frequently in 78% of participants (n = 7). Scores outside of normal range were also common in sensory avoiding, noted in 56% of participants (n = 5).
Table 4.
Adult Sensory Profile results for participants with cognitive impairment compared to normative data for persons aged 65 years and older.
| Participant | Low Registration | Sensation Seeking | Sensory Sensitivity | Sensation Avoiding |
|---|---|---|---|---|
| Ronald | + | = | = | + |
| Pamela | + | = | = | = |
| Walter | + | = | = | = |
| Charlotte | + | = | + | + |
| Vicky | = | + | − | = |
| Adam | + | = | = | ++ |
| Betty | + | = | = | + |
| Ricky | + | + | = | = |
| Chris | = | − | = | − |
Notes. Symbols representative of normative data for specific age group as reported on the Adult Sensory Profile:19 (−) Less than most people; (=) similar to most people; (+) more than most people; (++) much more than most people.
During interviews, all participants and their care partners described elements of their environment associated with their sensory processing patterns and behavior. These responses were unique for each participant. Some described self-initiated modifications of the environment to adjust sensory stimuli in the home. Vignettes below describe participants’ sensory profiles, care partner discussion of behavioral symptoms, and environmental features to illustrate interrelationships among sensory processing, home environment elements, and behavior, whereby illustrating the potential mechanism of action related to behavioral expression for this population.
Chris
Chris, age 93 had a diagnosis of MCI, and lived with his wife, Karen. She described his temperament as very laid-back. He went with the flow of the day and said he was not bothered by anything within his environment. He enjoyed weekly outings to have coffee with the “guys” and to exercise at a local boxing club.
Sensory profile
Chris was “less than most” in sensation seeking and sensation avoiding, meaning his sensory processing system sought out sensory stimulation less than others of his age, and he also actively avoided stimulation less than others. That behaviors were passive in relation to environmental stimuli was evident by minimal influence from the environment impacting his behavioral state. A sensory profile indicating passivity in behavioral reactions to stimulation correlates with his self-described laid-back personality. For example, he was indifferent regarding the noise level in their home when friends or family visited, and he did not actively attempt to clean or reorganize their belongings as Karen packed things to donate.
Environment
Chris and Karen’s home was quiet, well-lit, and without clutter. Chris stayed on the primary floor, rather than descending stairs to the basement. For this reason, Karen completed the laundry. Chris slept in the living room in an electric, reclining chair. Karen helped him with bathing and dressing, but she said the bathrooms were well-equipped with grab bars and bathroom stools to support his decreased balance. In addition to Karen, Chris had regular help with transportation from friends and neighbors. Their children visited monthly.
Behavior
Chris’ sensory profile and home environment characteristics appeared to be a good match as Chris did not present with negative behaviors or limited accessibility within his home. While he did describe some frustration with any clutter of mail and/or and medicine bottles on the dining room table which caused him to have difficulty differentiating or remembering which medicine to take, he had no other comments or complaints of discomfort within the home.
Ricky
Ricky, age 81 with a diagnosis of MCI, lived with his wife of 10 years, Janelle. He described himself as the shopper for the family because he enjoyed going to the grocery store and driving his car.
Sensory profile
Ricky’s sensory profile revealed he was “more than most” in areas of low registration and sensation seeking. More than most in low registration indicates a difficulty with sensory discrimination and a need for increased intensity of sensory stimulation for perception. More than most in sensation seeking indicates a drive to seek out sensory stimulation, such as driving or seeking a cluttered space. His sensory profile scores correspond with his interest in shopping, driving, and need for high levels of visual stimulation in his office.
Environment
Ricky’s home was well-kept with one room dedicated as his office. In his office, the walls were covered with pictures and shelves were filled with books. He mentioned he felt comfortable in this space with his belongings. They had moved into their patio home in a small retirement community a few years prior to the interview. Ricky and his wife describe a rich social life with their neighbors, including frequent visits from friends, neighborhood socials, and game night with friends.
Behavior
Ricky was pleasant and friendly throughout observations. He appeared to have good environmental fit within his home, as it was clean with limited distractions to the completion of tasks. He and his wife described times of agitation and frustration when he was cognitively challenged. For example, Ricky asked Janelle to make decisions regularly. When in the community, she navigated as he drove; she made the grocery list and weekly meals, and he shopped. When he did not have her guidance in making decisions, he became overwhelmed and agitated. They were both close with their church leadership and described church support groups which aided Ricky’s ability to manage his agitation.
Betty
Betty, age 73 with a diagnosis of MCI, was an active member of her community and church as a volunteer. She lived with her husband, Samuel, in a home where they had lived for the majority of their adulthood.
Sensory profile
Betty’s ASP results identified her as “more than most” in areas of low registration and sensation avoiding. More than most in low registration indicates a need for increased intensity in stimulation for perception. Also, more than most in sensation avoiding indicates a tendency to avoid unpredictable sensory environments. These are evident by her need for increased attention to detail and self-report of need to control aspects of her environment. Those who are sensory avoiding are often more accepting of environmental stimuli they can control. For example, Betty said she loved to sing but often avoided loud sounds. She slept in a separate room from her husband due to his loud snoring.
Environment
Betty and Samuel lived in a two-story home which had undergone major renovation and expansion to accommodate their needs as they aged. They were committed to living in their home for as long as possible. She and her husband laughed about her desire to organize everything in their home and keen attention to details in all her activities.
Behavior
Betty was friendly and inviting during observations. She and Samuel had no concerns regarding her behaviors and moods. She did discuss the need to decrease her involvement in community organizations in preparation for worsening cognition in the coming years, but she was accepting of this transition and had adapted her home and daily routines to support her needs.
Adam
Adam, aged 85 with a diagnosis of MCI, had lived in his home for decades, and he and his wife planned renovations to their home to enhance access and safety.
Sensory profile
Adam’s profile indicated that he was considered “more than most” others of his age in the area of low registration. This indicated that he needed a higher level of sensory input to perceive stimuli. His wife accommodated this by adding large signs in their home to remind him to drink water and find his keys.
Environment
Adam described times when he felt overwhelmed by sensory stimuli from his environment which caused some avoidant and agitated behaviors. He preferred a quiet environment and actively sought out decreasing the volume when it was too high. He also required control over stimulation. For example, he enjoyed bright lights as long as he was in control of when they were on and where. He gave examples of becoming agitated when there was too much stimulation in his environment. His wife told a story of a time when he was asked to leave a grocery store because he felt out of control of the noise level in the store and had lashed out at store staff.
Behavior
Adam demonstrated persistent behaviors to align his environment with his sensory preferences. He and his wife shared examples of increased stress and agitation when he was not able to accommodate his environment to meet his sensory preferences and processing abilities, for example, he became agitated when the television was on while he talked on the phone, or he was restless when the lighting was not as he preferred when falling asleep. However, he was active in adjusting elements of the environment as needed (i.e., turning the television off).
Vicky
Vicky, aged 81 with a diagnosis of dementia, lived with her husband of 61 years. She enjoyed looking at family photos and visiting with her children and grandchildren.
Sensory profile
Vicky’s ASP indicated that she sought sensation “more than most” and had sensory sensitivity “less than most” others within the normative data. These indicate that she preferred sensory stimuli and tolerated higher levels of sensory stimuli. These were evident in her desire for regular car rides and pictures covering the majority of the wall space within her home.
Environment
Vicky and her husband described a daily routine with prayer in the morning, television shows mid-morning, a drive and eating lunch out of the home, resting in the afternoon and a light meal for an early dinner each day. Vicky’s husband described her desire to look through photo albums daily and routine requests to go out for a drive with him. He easily accommodated these requests and did not report any concerns regarding her behavior. She was pleasant and quiet throughout the interview and observations. Vicky said she liked to sweep and help in the kitchen, but her husband stated he preferred she did not do these tasks due to previous lower extremity joint replacements and back pain.
Behavior
Vicky was soft-spoken and kind throughout observations. Her husband described her as a wonderful wife and stated that she never acted out or had difficulty with behaviors. She navigated her home environment with ease and appeared to have good environmental fit within her home.
Charlotte
Charlotte, aged 88 with a diagnosis of MCI, was a care provider for her husband, Ronald, described below.
Sensory profile
Her ASP results indicated that she had sensory sensitivity, low registration, and sensation avoidance “more than most” for her age. Similar to Betty, Charlotte needed to be in control of her environment to help accommodate a need to avoid sensation. She said she often spent an entire day in bed after a busy day prior, which may be related to sensory sensitivity and sensation avoiding tendencies. She also described situations, such as trouble with cooking and bumping into things, which are evident in those with low registration.
Environment
Charlotte said she enjoyed rearranging her home but felt that care for the home was beginning to be burdensome. She discussed increasing reliance on supports within her environment such as needing assistance for shopping trips and new troubles related to cooking (i.e., burning food and improper seasoning). She mentioned that she frequently bumped into items in her home and needed extra equipment (shower chair and grab bars) in the bathroom for stability. Charlotte required continual oxygen through a nasal canula and had long electrical cords throughout her living space.
Behavior
She described bouts of depression and explained that she would spend days in bed. She said she felt depressed and lonely and had little enthusiasm to do things outside of her home. Her husband described her as a social person, but she no longer had regular contact with her friends.
Ronald
Ronald, aged 83 with a diagnosis of MCI, the husband of Charlotte, was a retired salesman who enjoyed driving.
Sensory profile
Ronald’s sensory profile indicated three domains that were different than most others his age. He had low registration “less than most,” sensory sensitivity “less than most,” and sensation avoiding “much more than most.” Low registration indicates a need for increased sensory stimuli for perception. Lowered sensory sensitivity also indicates that he is not sensitive to increased sensory input. These are consistent with a tendency to interrupt in conversation and speak loudly despite normal hearing. Despite these areas being lowered, he has increased tendencies to be sensory avoiding, which indicated he did not prefer high amounts of stimuli. This was evident in his reluctance to grocery shop, resistance to moving or trying new situations, and a work history of traveling alone.
Environment
Ronald is happy in his home and hopes to remain living there for as long as possible. He said he was satisfied with the home and did not want to make changes to this living environment. Socially, he participated in several community activities, including a weekly breakfast with the guys at McDonalds, YMCA exercise classes, church, and offering transportation to disabled friends. Ronald continues to enjoy driving, an activity he did throughout his career as a regional sales representative which he reports would cause him to be away from home at least three nights per week. Because of his love for driving, he would often help his friends if they needed transportation. For tasks in their home, Charlotte managed all finances, grocery shopping, and cooking. Ronald drove for the couple, did the laundry, and had a decreasing role in outside yard work, as they hired additional help.
Behavior
Ronald was welcoming and open during observations. He did tend to dominate conversations, and was, at times insistent that he was correct. Charlotte said they often bickered back and forth but got along, overall. He did describe times of becoming agitated when in highly stimulating environments, such as the grocery store, and so he avoided such places. Ronald was able to maintain appropriate environmental contexts to meet his needs and sensory preferences.
Pamela
Pamela was an active 67-year-old living with MCI. She lived with Alex, her husband of 50 years. She enjoyed community service and housework.
Sensory profile
Pamela’s sensory profile results indicated that she has low registration “more than most” others her age, and the other three domains were “similar to most” others of her age group. During observation, she talked about the need for strong sensory input, including her desire to have candles in her home and preference to have the television on for sound. Her craft room was also full of supplies but organized. She discussed avoidance of large box stores, and she frequently stays home while her husband runs errands.
Environment
Pamela and Alex had lived in their current home for most of their marriage. Pamela said she felt safe in her home, and that she enjoyed working on projects in her space. They participated in regular exercise together three to 4 days per week. Pamela and Alex engaged in weekly volunteering with meal delivery for their church. Pamela said she liked to help navigate, and her husband drives. They both attend the local senior citizen’s center for social engagement. Alex manages all finances and grocery shopping, and Pamela helps with cooking, cleaning, and other housework.
Behavior
Pamela was friendly and inviting during observations. She presented with some perseveration during conversation and daily tasks, but this did not seem to interfere with her daily function. Pamela described a lifetime of challenges with psychiatric conditions that often caused her “fly off the handle.” She said she often became agitated and anxious over minute details. Her husband stated that he remained calm and “let her blow off steam.” These abrupt changes may have been related to lack of environmental fit or her inability to maintain a good fit as elements of her environment changed, such as noise level or disorganization.
Walter
Walter, age 82 with a diagnosis of MCI, lives with Laura, his wife of 48 years.
Sensory profile
Low registration was “more than most” others his age. All other areas of sensory processing and patterns were reported as “similar to most” others. Low registration is evident by his tolerance of clutter throughout his home and yard, along with frequent small car accidents, as he may not register all needed environmental precautions while driving.
Environment
Walter and Laura lived in a large three-story home. They had limited outside support or help from their family or social groups. The home was cluttered and needed home improvements, such as painting and small repairs. They both agreed that the house had become difficult to care for and maintain. There was clutter throughout the house that presented numerous tripping hazards. Laura said Walter liked to get started on house projects but was not likely to finish or often made bigger problems in the home. She gave the example of when he attempted to re-tile the bathroom wall, and she had to call in a contractor to repair damage he inadvertently caused.
Behavior
Walter had a passion for cars and driving, despite recent accidents and growing concerns from Laura for his safety. She talked about struggles in their partnership in terms of communication. During observations, he talked loudly, often over Laura, was agitated, and had difficulty with transition between topics. Laura said he became aggressive at times. Walter’s situation is an example of an environment not supporting his needs and preferences, whereby impacting his behavior.
Discussion
This study explored sensory processing of community-dwelling adults with cognitive impairment as a potential mechanism to better understand behavioral presentation in the home environment. Seven of the nine cognitively impaired participants presented with sensory processing abnormalities. Several individuals employed self-identified environmental adaptations that were in line with their sensory processing preferences. These environmental adaptations led to greater behavioral regulation in the home context; a novel perspective for assessment and intervention for BPSD.
Findings of this study highlight the unique contributions of sensory processing as a potential mechanism of behavior for older adults with cognitive impairment (Kovach et al., 2004). Prevalence and implications of sensory processing impairment in older adults, especially those with cognitive impairment, has not been fully explored in existing literature (Champagne, 2018). However, evidence of sensory processing abnormalities creates a realm of assessment and interventions that may prove beneficial for BPSD in the earliest stages of cognitive impairment. For example, Adam often became agitated when overstimulated by sound. Without identification of this sensory preference, his behavioral response could manifest as a “problem behavior,” causing additional distress for him and his spouse and potentially leading to unnecessary or inappropriate intervention. Awareness of sensory processing abilities and preferences has the potential to inform small but significant modifications and adjustments to the environment to decrease behavioral symptoms for older adults with cognitive impairment (Crowe, 2014).
Several participants engaged in self-initiated and/or care partner–initiated environmental adaptations to accommodate for sensory processing ability and preference. Those who implemented environmental adaptations demonstrated and reported less behavioral disturbance in the home when compared to participants who did not engage in such adaptions (i.e., clutter throughout home, lack of control over noise volume). A person-centered approach toward tailoring environmental adaptation to support behavior may be most advantageous due to the unique complexities involved in the situational contexts of the home environment (Hung et al., 2016; Wang et al., 2019). Further, communication of such preference, if relocation to institutional care is warranted, may improve transition and integration into the new living environment (Ashbourne et al., 2021).
Use of sensory systems to regulate behavior involves identifying environment and sensory-based techniques to target behavior for persons with cognitive impairment (American Occupational Therapy Association, 2017). Expertise, such as that offered by occupational therapy, could provide support beyond what individuals can do on their own to adapt and facilitate a supportive home environment for management of BPSD over time (Dunn & Bennett, 2002). Despite practice guideline recommendations, there are limited clinical tools for rigorous assessment and intervention related to sensory processing and sensory modulation for persons with ADRD (Champagne, 2018).
Our findings add to growing evidence of the need for supporting sensory-based assessment and intervention in late-life neurodegenerative disorders as a potential mechanism of action in behavioral expression for persons with MCI, as well as need for increased methods for evaluation of the situational context related to BPSD (Butler et al., 2020; Gitlin et al., 2012). Although replication with larger, more diverse samples is necessary, these findings offer preliminary description of sensory processing as it relates to behavior in the home environment. Future studies are needed to understand the nature of sensory processing and subtleties of environmental adaption in relation to BPSD, as well as potential avenues for treatment, such as nonpharmacological, occupational therapy interventions, to improve quality of life and enable prolonged residence in familiar settings for older adults with cognitive impairment.
Limitations
This study has limitations. The authors attempted to recruit participants with a dementia diagnosis; however, care partners of those with advanced dementia declined to participate in the current study. This limited observation of the breadth of cognitive impairment provides continued opportunity for investigation. Future research is needed to confirm behavioral phenotypes and the relationship to sensory processing in later stages of cognitive impairment.
Conclusion
Onset and progression of altered sensory processing as a symptom of neurodegenerative cognitive impairment may have significant implications for behavior and environmental interaction. Findings of this study offer evidence of reduced sensory processing abilities as a potential mechanism of behavior in the home environment of adults with MCI. A rigorous, nonpharmacological, therapeutic approach to assessment and intervention of sensory processing as it relates to behaviors of individuals living with cognitive impairment could provide opportunity for improved quality of life for all individuals involved. Additional research is needed to define subtleties of environmental adaption to support older adults with MCI as they age in their home environment.
Supplemental Material
Supplemental Material, sj-pdf-1-ggm-10.1177_23337214211068290 for Sensory Processing Abnormalities in Community-Dwelling Older Adults with Cognitive Impairment: A Mixed Methods Study by Elizabeth K. Rhodus, Elizabeth G. Hunter, Graham D. Rowles, Shoshana H. Bardach, Kelly Parsons, Justin Barber, MaryEllen Thompson, and Gregory A. Jicha in Gerontology and Geriatric Medicine
Acknowledgments
This study utilized University of Kentucky Alzheimer’s Disease Research Center. The authors acknowledge and thank all participants.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for the longitudinal cohort is provided by NIH/NIA under Grant NIH/NIA P30 AG072946; and the first author is funded by the NIH under Grant NIH T32 AG057461: “Training in Translational Research in Alzheimer’s and Related Dementias (TRIAD).”
Ethical Approval: University of Kentucky IRB Protocol: 46351.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Elizabeth K. Rhodus https://orcid.org/0000-0001-5108-0766
References
- Albert M. S., DeKosky S. T., Dickson D., Dubois B., Feldman H. H., Fox N. C., Gamst A., Holtzman D. M., Jagust W. J., Petersen R. C., Snyder P. J., Carrillo M. C., Thies B., Phelps C. H. (2011). The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 7(3), 270–279. 10.1016/j.jalz.2011.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer’s Association . (2020). 2020 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 16(3), 391–460. 10.1002/alz.12068 [DOI] [Google Scholar]
- American Occupational Therapy Association . (2017). Occupational therapy practice guidelines for adults with Alzheimer’s Disease and related major neurocognitive disorders. AOTA Press. [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. [Google Scholar]
- Ashbourne J., Boscart V., Meyer S., Tong C. E., Stolee P. (2021). Health care transitions for persons living with dementia and their caregivers. BMC Geriatrics, 21(1), 285. 10.1186/s12877-021-02235-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeije H. (2002). A purposeful approach to the constant comparative Method in the analysis of qualitative interviews. Quality and Quantity, 36(4), 391–409. 10.1023/A:1020909529486 [DOI] [Google Scholar]
- Brown C., Dunn W. (2002). Adolescent/Adult Sensory Profile user’s manual. Pearson. [Google Scholar]
- Brown C., Tollefson N., Dunn W., Cromwell R., Filion D. (2001). The adult sensory profile: Measuring patterns of sensory processing. American Journal of Occupational Therapy, 55(1), 75–82. 10.5014/ajot.55.1.75 [DOI] [PubMed] [Google Scholar]
- Butler M., Gaugler J., Talley K., Abdi H., Desai P., Duval S., Forte M., Nelson V., Ng W., Ouellette J., Ratner E., Saha J., Shippee T., Wagner B., Wilt T., Yeshi L. (2020). Care interventions for people living with dementia and their caregivers. Comparative Effectiveness Review No. 231. Agency for Healthcare Research and Quality. AHRQ Publication No. 20-EHC023 10.23970/AHRQEPCCER231 [DOI] [Google Scholar]
- Champagne T. (2018). Sensory modulation in dementia care: Assessment and activities for sensory enriched care. Jessica Kingsley Publishers. [Google Scholar]
- Chung J. C. (2006). Measuring sensory processing patterns of older Chinese people: Psychometric validation of the adult sensory profile. Aging & Mental Health, 10(6), 648–655. 10.1080/13607860600648080 [DOI] [PubMed] [Google Scholar]
- Creswell J. W. (2013). Qualitative inquiry & research design: Choosing among five approaches (3rd ed.). SAGE. [Google Scholar]
- Crowe J. (2014). Professional reasoning and occupational therapist’s use of a multi-sensory environment for clients with dementia. Physical & Occupational Therapy In Geriatrics, 32(3), 198–209. 10.3109/02703181.2014.927947 [DOI] [Google Scholar]
- Cummings J. L. (1997). The Neuropsychiatric Inventory: Assessing psychopathology in dementia patients. Neurology, 48(5 Suppl 6), S10–S16. 10.1212/wnl.48.5_suppl_6.10s [DOI] [PubMed] [Google Scholar]
- Dunn W. (1997). The impact of sensory processing abilities on the daily lives of young children and their families: A Conceptual Model. Infants & Young Children, 9(4), 23–35. 10.1097/00001163-199704000-00005 [DOI] [Google Scholar]
- Dunn W., Bennett D. (2002). Patterns of sensory processing in children with attention deficit hyperactivity disorder. OTJR: Occupation, Participation and Health, 22(1), 4–15. 10.1177/153944920202200102 [DOI] [Google Scholar]
- Dunn W., Westman K. (1997). The sensory profile: The performance of a national sample of children without disabilities. American Journal of Occupational Therapy, 51(1), 25–34. 10.5014/ajot.51.1.25 [DOI] [PubMed] [Google Scholar]
- Engel-Yeger B., Rosenblum S. (2021). Executive dysfunctions mediate between altered sensory processing and daily activity performance in older adults. BMC Geriatrics, 21(1), 132. 10.1186/s12877-021-02032-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerlach L. B., Kales H. C. (2020). Managing behavioral and psychological symptoms of dementia. Clinics in Geriatric Medicine, 36(2), 315–327. 10.1016/j.cger.2019.11.010 [DOI] [PubMed] [Google Scholar]
- Gitlin L. N., Kales H. C., Lyketsos C. G. (2012). Nonpharmacologic management of behavioral symptoms in dementia. JAMA, 308(19), 2020–2029. 10.1001/jama.2012.36918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes C. P., Berg L., Danziger W. L., Coben L. A., Martin R. L. (1982). A new clinical scale for the staging of dementia. British Journal of Psychiatry, 140, 566-572. 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- Hung L., Chaudhury H., Rust T. (2016). The effect of dining room physical environmental renovations on person-centered care practice and residents' dining experiences in long-term care facilities. Journal of Applied Gerontology, 35(12), 1279–1301. 10.1177/0733464815574094 [DOI] [PubMed] [Google Scholar]
- Jensen L., Padilla R. (2017). Effectiveness of environment-based interventions that address behavior, perception, and falls in people with Alzheimer’s disease and related major neurocognitive disorders: A systematic review. American Journal of Occupational Therapy, 71(5), 7105180030p7105180031–7105180030p7105180010. 10.5014/ajot.2017.027409 [DOI] [PubMed] [Google Scholar]
- Kales H. C., Gitlin L. N., Lyketsos C. G. (2014). Management of neuropsychiatric symptoms of dementia in clinical settings: Recommendations from a multidisciplinary expert panel. Journal of American Geriatric Society, 62(4), 762–769. 10.1111/jgs.12730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovach C. R., Taneli Y., Dohearty P., Schlidt A. M., Cashin S., Silva-Smith A. L. (2004). Effect of the BACE intervention on agitation of people with dementia. The Gerontologist, 44(6), 797–806. 10.1093/geront/44.6.797 [DOI] [PubMed] [Google Scholar]
- Lawton M. P., Nahemow L. (1973). Ecology and the aging process. In The psychology of adult development and aging. American Psychological Association. 10.1037/10044-020 [DOI] [Google Scholar]
- Lewin K. (1936). Principles of topological psychology. McGraw-Hill. [Google Scholar]
- Luo Y., He P., Guo C., Chen G., Li N., Zheng X. (2018). Association between sensory impairment and dementia in older adults: Evidence from China. Journal of American Geriatric Soceity, 66(3), 480–486. 10.1111/jgs.15202 [DOI] [PubMed] [Google Scholar]
- Magasi S., Wong A., Gray D. B., Hammel J., Baum C., Wang C. C., Heinemann A. W. (2015). Theoretical foundations for the measurement of environmental factors and their impact on participation among people with disabilities. Archives of Physical Medicine and Rehabilitation, 96(4), 569–577. 10.1016/j.apmr.2014.12.002 [DOI] [PubMed] [Google Scholar]
- Morgan D. L. (2007). Paradigms lost and pragmatism regained: Methodological implications of combining qualitative and quantitative methods. Journal of Mixed Methods Research, 1(1), 48–76. 10.1177/2345678906292462 [DOI] [Google Scholar]
- Morris J. C. (1993, November). The clinical dementia rating (CDR): Current version and scoring rules. Neurology, 43(11), 2412–2414. 10.1212/wnl.43.11.2412-a [DOI] [PubMed] [Google Scholar]
- Nielsen L., Riddle M., King J. W., NIH Science of Behavior Change Implementation Team. Aklin W. M., Chen W., Clark D., Collier E., Czajkowski S., Esposito L., Ferrer R., Green P., Hunter C., Kehl K., King R., Onken L., Simmons J. M., Stoeckel L., Stoney C., Weber W. (2018). The NIH science of behavior change program: Transforming the science through a focus on mechanisms of change. Behaviour Research and Therapy, 101, 3–11. 10.1016/j.brat.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padilla R. (2011). Effectiveness of environment-based interventions for people with Alzheimer’s disease and related dementias. American Journal of Occupational Therapy, 65(5), 514–522. 10.5014/ajot.2011.002600 [DOI] [PubMed] [Google Scholar]
- Pinto J. M., Wroblewski K. E., Huisingh-Scheetz M., Correia C., Lopez K. J., Chen R. C., Kern D. W., Schumm P. L., Dale W., McClintock M. K. (2017). Global sensory impairment predicts morbidity and mortality in older U.S. adults. Journal of Amermican Geriatric Society, 65(12), 2587–2595. 10.1111/jgs.15031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravn M. B., Klingberg T., Petersen K. S. (2018). The Adult Sensory Profile™ in care homes targeting people diagnosed with dementia: A qualitative study from the care provider perspective. Rehabilitation research and practice, 2018, 5091643. 10.1155/2018/5091643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Researchware I. (2018). HyperRESEARCH 4.0.2. [Computer Software] http://www.researchware.com/ [Google Scholar]
- Sánchez A., Marante-Moar M. P., Sarabia C., de Labra C., Lorenzo T., Maseda A., Millán-Calenti J. C. (2016). Multisensory stimulation as an intervention strategy for elderly patients with severe dementia: A Pilot Randomized Controlled Trial. Am J Alzheimers Disease Other Dementias, 31(4), 341–350. 10.1177/1533317515618801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt F. A., Nelson P. T., Abner E., Scheff S., Jicha G. A., Smith C., Cooper G., Mendiondo M., Danner D. D., Van Eldik L. J., Caban-Holt A., Lovell M. A., Kryscio R. J. (2012). University of Kentucky Sanders-Brown healthy brain aging volunteers: donor characteristics, procedures and neuropathology. Current Alzheimer's Research, 9(6), 724–733. 10.2174/156720512801322591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark S. L., Somerville E. K., Morris J. C. (2010). In-home occupational performance evaluation (I-HOPE). American Occupational Therapy Association, 64(4), 580–589. 10.5014/ajot.2010.08065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Xu W., Chen K.-L., Shen X.-N., Tan L., Yu J.-T., the Alzheimer’s Disease Neuroimaging, I . (2021). Mild behavioral impairment correlates of cognitive impairments in older adults without dementia: Mediation by amyloid pathology. Translational Psychiatry, 11(1), 577. 10.1038/s41398-021-01675-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topaz M., Adams V., Wilson P., Woo K., Ryvicker M. (2020). Free-text documentation of dementia symptoms in home healthcare: A natural language processing study. Gerontology and Geriatric Medicine. 10.1177/2333721420959861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Wu B., Bowers B. J., Lepore M. J., Ding D., McConnell E. S., Corazzini K. N. (2019). Person-centered dementia care in China: A Bilingual literature review. Gerontology and Geriatric Medicine. 10.1177/2333721419844349\\. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winblad B., Palmer K., Kivipelto M., Jelic V., Fratiglioni L., Wahlund L.-O., Nordberg A., Bäckman L., Albert M., Almkvist O., Arai H., Basun H., Blennow K., de Leon M., DeCarli C., Erkinjuntti T., Giacobini E., Graff C., Hardy J., Petersen R. (2004). Mild cognitive impairment - Beyond controversies, towards a consensus: Report of the International working group on mild cognitive impairment. Journal of Internal Medicine, 256(3), 240–246. 10.1111/j.1365-2796.2004.01380.x [DOI] [PubMed] [Google Scholar]
- Wise E. A., Rosenberg P. B., Lyketsos C. G., Leoutsakos J. M. (2019). Time course of neuropsychiatric symptoms and cognitive diagnosis in National Alzheimer’s Coordinating Centers volunteers. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 11, 333–339. 10.1016/j.dadm.2019.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeisel J., Silverstein N. M., Hyde J., Levkoff S., Lawton M. P., Holmes W. (2003). Environmental correlates to behavioral health outcomes in Alzheimer’s special care units. The Gerontologist, 43(5), 697–711. 10.1093/geront/43.5.697 [DOI] [PubMed] [Google Scholar]
- Zhao Q. F., Tan L., Wang H. F., Jiang T., Tan M. S., Tan L., Xu W., Li J. Q., Wang J., Lai T. J., Yu J. T. (2016). The prevalence of neuropsychiatric symptoms in Alzheimer's disease: Systematic review and meta-analysis. Journal of Affective Disorders, 190, 264–271. 10.1016/j.jad.2015.09.069 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ggm-10.1177_23337214211068290 for Sensory Processing Abnormalities in Community-Dwelling Older Adults with Cognitive Impairment: A Mixed Methods Study by Elizabeth K. Rhodus, Elizabeth G. Hunter, Graham D. Rowles, Shoshana H. Bardach, Kelly Parsons, Justin Barber, MaryEllen Thompson, and Gregory A. Jicha in Gerontology and Geriatric Medicine