Abstract
Objective/background
To describe and characterize insomnia symptoms and nightmare profiles in Portugal during the first six weeks of a national lockdown due to COVID-19.
Patients/methods
An open cohort study was conducted to collect information of the general population during the first wave of SARS-CoV-2/COVID-19 pandemic in Portugal. We analyzed data from 5011 participants (≥16 years) who answered a weekly questionnaire about their well-being. Two questions about the frequency of insomnia and nightmares about COVID-19 were consecutively applied during six weeks (March–May 2020). Latent class analysis was conducted and different insomnia and nightmare profiles were identified. Associations between individual characteristics and both profiles were estimated using odds ratios (ORs) and 95% confidence intervals (CI).
Results
Five insomnia (No insomnia, Stable-mild, Decreasing-moderate, Stable-severe, Increasing-severe) and three nightmares profiles (Stable-mild, Stable-moderate, Stable-severe) were identified. Being female, younger, perceiving their income as insufficient and feelings of fear towards COVID-19 were associated with higher odds of insomnia (Women: OR = 6.98 95%CI: 4.18–11.64; ≥60 years: OR = 0.30 95%CI: 0.18–0.53; Insufficient income: adjusted OR (aOR) = 8.413 95%CI: 3.93–16.84; Often presenting fear of being infected with SARS-CoV-2 infection: aOR = 9.13 95%CI: 6.36–13.11), and nightmares (Women: OR = 2.60 95%CI: 1.74–3.86; ≥60 years: OR = 0.45 95%CI: 0.28–0.74; Insufficient income: aOR = 2.60 95%CI: 1.20–5.20; Often/almost always presenting fear of being infected with SARS-CoV-2 infection: aOR = 6.62 95%CI: 5.01–8.74). Having a diagnosis of SARS-CoV-2 virus infection was associated with worse patterns of nightmares about the pandemic.
Conclusions
Social and psychological individual factors are important characteristics to consider in the development of therapeutic strategies to support people with sleep problems during the COVID-19 pandemic.
Keywords: COVID-19, SARS-CoV-2, Nightmares, Insomnia symptoms, Portugal, Prospective studies
1. Introduction
By the end of 2019 and the beginning of 2020, the world experienced a highly pathogenic viral infection caused by SARS-CoV-2 generating the COVID-19 pandemic [1]. The fear of infection, the changes in social relationships characterized by social distance, the financial loss and the uncertainty about the future spread worldwide [2]. To reduce the transmission of the infection and the pressure on the Portuguese National Health System, Portugal decreed the state of emergency and later of calamity to frame national lockdown that included a “stay-at-home” order from March 19th to May 3rd, 2020 [3].
In past lockdowns experiences, during SARS-CoV in 2003 and Ebola in 2014, high levels of anxiety, acute stress disorders, psychological distress, depressive and insomnia symptoms were observed [2]. During the COVID-19 pandemic, besides insomnia symptoms, that was reported in 20–45% general population worldwide [4], oneiric activity has been strongly influenced by the lockdown, characterized by a marked increase of dream frequency, as well as a change in dream qualitative features [5]. This fact is in line with the “continuity hypothesis”: dreams reflect waking experience and in particular the emotional characteristics of daily mental activity [6]. Additionally, nightmares related to traumatic events can also emerge in these periods and outlast for a long period of time [7,8]. Poor sleep is also a predisposing factor for mental health problems, namely depression, anxiety, alcohol abuse, and psychosis [9], but is often underrecognized as a public health issue [10].
Studies conducted in Southern European countries suggest that insomnia and poor sleep quality have been widespread complaints among adults during the COVID-19 pandemic [11]. In Greece, a web-based study performed during April 2020, three weeks after the lockdown, showed that 37.6% of the adult participants reported insomnia [12], suggesting an exacerbation of sleep disturbances during this period. In Italy, another online survey with 2291 participants revealed that 57.1% of participants reported poor sleep quality, 32.1% high anxiety, 41.8% high distress, and 7.6% reported post-traumatic stress disorder symptomatology linked to the COVID-19 pandemic [13]. Moreover, during this period in China, in addition to the occurrence of new insomnia complaints, a 37% increase in the rates of clinical insomnia was observed, compared to before the peak of the COVID-19 pandemic [14], suggesting that the pandemic may have aggravated preexisting sleep problems.
Furthermore, particularly during the COVID-19 pandemic, it should be noted that age and gender are two important features associated with oneiric activity and insomnia, with women presenting higher dream recall rate, higher negative emotions [15] and, together with young adults, presented higher probability of severe insomnia [14,16], but more characteristics, namely regarding the SARS-CoV-2 infection need to be studied.
Since sleep is a dynamic process that changes throughout time [11], it is expected that fluctuations in its quality might occur during the pandemic. At the same time, there have been reports of sleep changes from many countries around the world, but there appears to be no single universal response that applies to all people: some have experienced improvements, others have had more complaints, and many individuals have exhibited little or no change [17]. Thus, monitoring sleep and dream-related aspects over time seems to be of high relevance, not only because it allows a more complete description of individual sleep profiles and a better characterization of sleep patterns, but also because it will contribute to the development of more tailored interventions to support people with sleep problems during the COVID-19 pandemic. Also, better identifying population subgroups with higher chances of presenting unhealthy sleep trajectories could help to delineate prevention measures targeting specific strata within the general population. Therefore, this longitudinal study aimed to characterize insomnia symptoms and nightmare profiles and the associated factors in the Portuguese population throughout the first six weeks of lockdown due to the COVID-19 pandemic.
2. Methods
2.1. Study design, participants and definition of variables
The Institute of Public Health of the University of Porto (ISPUP) and the Institute of Systems and Computers Engineering, Technology and Science (INESC TEC) designed an internet-based open cohort study (Diários de uma Pandemia, in English, Diaries of a Pandemic) that aimed to collect daily information on different aspects of the life of the Portuguese population during the first wave of SARS-CoV-2/COVID-19 pandemic in Portugal. We used a dynamic cohort design, participants being allowed to enter and leave the study at any time during follow-up and fill in any number of questionnaires, with any periodicity. The study was primarily designed for residents in Portugal, even though a minority (n = 59) of Portuguese nationals living in other countries were also included. A non-probabilistic sampling method was used, where the dissemination of the survey and a call for participation were made primarily through a national daily newspaper (PÚBLICO), which published several news pieces on the study and posted a temporary banner on their website, as well as through the institutional websites of ISPUP and INESC TEC, their social network accounts, and mailing lists. In addition, key opinion leaders were contacted to contribute to the dissemination through their own networks.
Persons aged 16 years or more were eligible to participate. Potential participants were asked to provide an email address which was used to generate a unique pseudonymized token that directed them to an informed consent page. Participation was considered valid only if the respondent had scrolled through the whole privacy policy and consent document. Each participant was re-sent their unique token every day as part of a reminder to fill in that day's questionnaire.
Besides the daily survey, between 26th of March and first of May (six weeks), participants received a weekly questionnaire in order to characterize their well-being and the impact that the pandemic might have on their daily life. Specifically, insomnia symptoms and nightmares were assessed in the weekly module through the questions “During the past week, did you experience difficulties falling asleep or staying asleep?” and “During the past week, did you have any nightmares about the current situation?”, respectively. For both questions, the answer options were “never/almost never”, “occasionally”, “often”, “always/almost always”. These questions were applied weekly during six weeks. During the same weeks and using the same answer options, participants were inquired about the frequency of feeling fear of being infected with SARS-CoV-2. Since these answers were considerably stable over time, we used only the information collected at baseline. A confirmed infection by SARS-CoV-2 (yes/no) was also registered every day.
At the beginning of the study, participants were asked to fill in a short module on sociodemographic characteristics, comprising gender, age, household size, household composition, educational attainment, and perceived income adequacy, by asking respondents the following question: “How do you consider your household income. The answer options were a) insufficient, b) cautious with expenses, c) enough to make ends meet, and d) comfortable.
For this particular analysis, we considered information retrieved from 5011 participants that provided information about insomnia symptoms and nightmares in three or more time points throughout the six weeks and their characteristics are depicted in Table 1 . Among the participants who provided information during the six weeks of the study, 73.4% were women, 68.3% had less than 50 years of age, 81.3% had a University degree, 82.3% were not living alone, and the majority did not have any child (80.0%) or a person with a chronic disease (58.7%) in their household. A quarter of this sample considered their household income as insufficient or reported the need to be cautious with expenses. During the study period, 3% of the sample was diagnosed with SARS-CoV-2 infection and 23.8% reported to often/almost always/always feel fear of getting infected (Table 1).
Table 1.
Participants' sociodemographic characteristics (n = 5011).
| n (%) | |
|---|---|
| Gender | |
| Men | 1303 (26.6) |
| Women | 3592 (73.4) |
| Age (years) | |
| 16-39 | 2058 (42.1) |
| 40-49 | 1284 (26.2) |
| 50-59 | 885 (18.1) |
| ≥ 60 | 665 (13.6) |
| Education level | |
| University | 3980 (81.3) |
| High school | 793 (16.2) |
| ≤ Elementary | 124 (2.5) |
| Living alone | |
| No | 4038 (82.3) |
| Yes | 868 (17.7) |
| Household with ≥ 1 child | |
| No | 3926 (80.0) |
| Yes | 980 (20.0) |
| Household with ≥ 1 person with chronic disease | |
| No | 2878 (58.7) |
| Yes | 2028 (41.3) |
| Perceived income adequacy | |
| Comfortable | 1643 (33.5) |
| Enough to make ends meet | 1970 (40.2) |
| Cautious with expenses | 1151 (23.5) |
| Insufficient | 134 (2.7) |
| Fear of SARS-CoV-2 infection | |
| Never/occasionally | 3920 (78.2) |
| Often/almost always/always | 1191 (23.8) |
| SARS-CoV-2 infection | 152 (3.0) |
Note: In each variable, the total may not add up to 5011 due to missing data.
2.2. Statistical analysis
Insomnia symptoms and nightmare profiles were obtained using latent class analysis based on the answers given to the two questions previously described, during six consecutively weeks. The Bayesian information criterion (BIC) was used for model selection. For both insomnia symptoms and nightmare profiles, we started by considering a one-class model, increasing the number of classes at each step up to six, searching for the lowest BIC value. Individuals were classified according to their probability of being in each latent class and each individual was assigned to the class with the highest probability. The best models obtained for insomnia symptoms and nightmare profiles were a five-class and three-class model, respectively (Supplementary file, Table S1).
The associations between sociodemographic factors and profiles of insomnia symptoms or nightmares were assessed using multinomial logistic regressions, and crude (OR) and adjusted odds ratio (aOR) with the respective 95% confidence intervals (95%CI) were computed. The sociodemographic factors considered were gender, age group, educational level, living alone, living in a household with children, living in a household with people with chronic diseases, and perceived income adequacy. Multivariate models were adjusted for potential confounders theoretically defined as documented causes of each exposure variable as well as of sleep problems (insomnia symptoms and nightmares), and that are not likely to mediate the main association. Thus, we built distinct multivariate models, for the relation of each potential determinant and sleep. For gender and age, only crude models are presented.
Statistical analyses were performed using R software [18] version 3·6.3 for Windows.
2.3. Ethics
The study received ethical approval by the Ethics Committee of the Institute of Public Health of the University of Porto (ref: CE20142). A Data Protection Officer was designated by the institutions involved and a formal Data Protection Impact Assessment was carried out.
3. Results
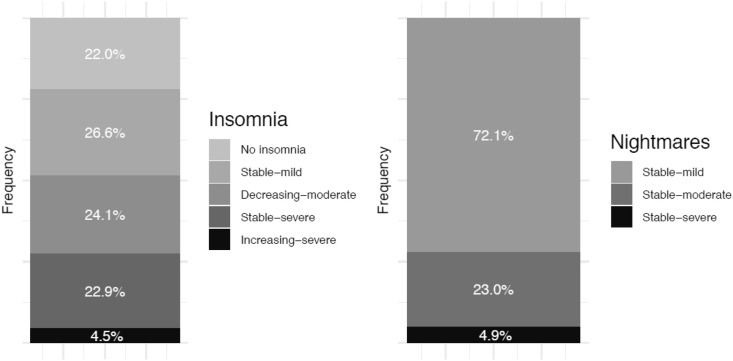
Five profiles of insomnia symptoms and three profiles of nightmares were identified. Insomnia symptoms' profiles were labelled as “No insomnia” (n = 1100, 22.0%), “Stable-mild” (n = 1334, 26.6%), “Decreasing-moderate” (n = 1207, 24.1%), “Stable-severe” (n = 1146, 22.9%) and “Increasing-severe” (n = 224, 4.5%). The three profiles that emerged for nightmares were named “Stable mild” (n = 3613, 72.1%), “Stable moderate” (n = 1153, 23.0%), and “Stable severe” (n = 245, 4.9%) (Fig. 1 ).
Fig. 1.
Description of the proportion of participants in each insomnia symptoms' and nightmare profiles.
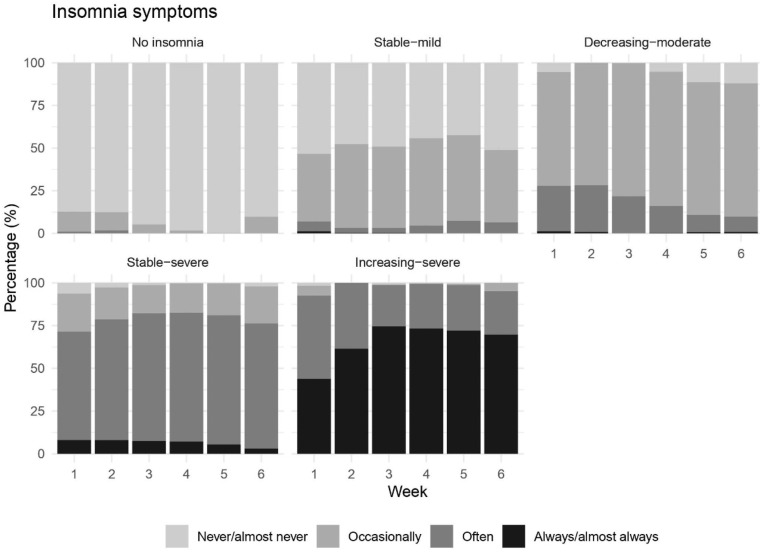
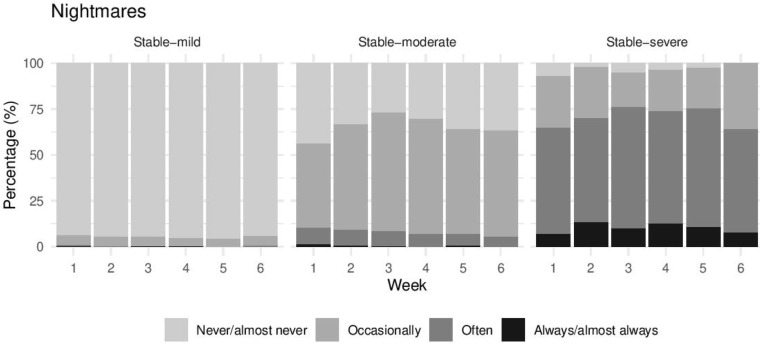
The “No insomnia” profile included mainly individuals stating that they never/almost never had difficulties to fall asleep or stay asleep throughout the study period, while half of the participants in “Stable-mild” profile occasionally presented insomnia symptoms during the six weeks. The profile entitled “Decreasing-moderate” included around a quarter of participants who referred to often experiencing insomnia symptoms but with decreasing frequency over time. The two profiles with the worst insomnia symptoms were “Stable-severe” and “Increasing-severe”. Most participants in both profiles reported to struggle to fall asleep or stay asleep recurrently with the latter presenting a worsening of symptoms over time (Fig. 2 and Table S2). Regarding nightmares, the three profiles had a stable trajectory over time, with “Stable-moderate” and “Stable-severe” presenting a slight worsening of symptoms in the middle weeks. Most participants in the “Stable-mild” profile never/almost never had nightmares about COVID-19 during the study period, while people in “Stable-moderate” and “Stable-severe” mostly referred to have them occasionally and often, respectively (Fig. 3 and Table S2).
Fig. 2.
Characterization of insomnia symptoms during the first wave of the COVID-19 pandemic.
Fig. 3.
Characterization of nightmares about COVID-19 during the first wave of COVID-19 pandemic.
In the crude analysis, being female, having less than 50 years of age, belonging to a household with at least 1 person with a chronic disease, perceiving their income as less favorable, often presenting fear of being infected with SARS-CoV-2 was associated with a higher likelihood of presenting a worse profile for insomnia symptoms and nightmares during the first wave of the pandemic. Lower education was associated with the “Increasing-severe” insomnia profile (High school: OR = 1.54, 95%CI 1.07–2.23), but not with the “Stable-severe” nightmare profile (High school: OR = 1.17, 95%CI 0.84–1.65). Inversely, having a child in the household and being diagnosed with SARS-CoV-2 infection was associated with a worse nightmare profile (Stable-severe: OR = 1.71, 95%CI: 1.27–2.29) but not with insomnia symptoms; living alone was not associated with any insomnia or nightmare profiles (Insomnia/increasing-severe: OR = 1.15, 95%CI: 0.80–1.66; Nightmares/stable-severe: OR = 1.18, 95%CI: 0.85–1.63) (Table 2, Table 3 ).
Table 2.
Crude and multivariate-adjusted odds ratio for the association between individual characteristics and insomnia symptoms' profiles during the first wave of the COVID-19 pandemic.
| Insomnia symptoms |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Crude ORa (95%CI) |
Adjusted ORa (95%CI) |
||||||||
| Stable mild | Decreasing moderate | Stable severe | Increasing severe | Stable mild | Decreasing moderate | Stable severe | Increasing severe | ||
| Gender | |||||||||
| Men | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Women | 1.52 (1.28–1.80) | 2.07 (1.72–2.48) | 3.08 (2.53–3.75) | 7.33 (4.46-12.05) | – | – | – | – | |
| Age (years) | |||||||||
| 16-39 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| 40-49 | 0.98 (0.80–1.21) | 1.09 (0.88–1.35) | 1.21 (0.98–1.26) | 0.84 (0.59–1.19) | – | – | – | – | |
| 50-59 | 0.93 (0.74–1.16) | 0.93 (0.73–1.17) | 0.92 (0.73–1.16) | 0.44 (0.28–0.69) | – | – | – | – | |
| ≥ 60 | 0.76 (0.60–0.97) | 0.83 (0.65–1.06) | 0.51 (0.39–0.67) | 0.30 (0.18–0.53) | – | – | – | – | |
| Education levelb | |||||||||
| University | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| High school | 1.14 (0.91–1.43) | 1.07 (0.85–1.35) | 1.21 (0.96–1.52) | 1.54 (1.07–2.23) | 1.21 (0.97–1.52) | 1.19 (0.94–1.51) | 1.40 (1.10–1.77) | 1.90 (1.35–2.77) | |
| ≤ Elementary | 1.25 (0.69–2.25) | 1.83 (1.04–3.20) | 1.68 (0.94–2.98) | 2.25 (0.97–5.22) | 1.46 (0.80–2.64) | 2.24 (1.27–3.97) | 2.35 (1.29–4.26) | 4.20 (1.75–10.05) | |
| Living aloneb | |||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Yes | 1.06 (0.86–1.30) | 0.95 (0.76–1.18) | 0.97 (0.78–1.21) | 1.15 (0.80–1.66) | 1.06 (0.86–1.32) | 0.93 (0.74–1.16) | 0.99 (0.79–1.25) | 1.21 (0.83–1.76) | |
| Household with ≥ 1 childc | |||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Yes | 0.94 (0.76–1.15) | 1.02 (0.83–1.26) | 1.11 (0.90–1.36) | 0.97 (0.68–1.40) | 0.88 (0.71–1.09) | 0.94 (0.76–1.18) | 0.96 (0.77–1.19) | 0.76 (0.52–1.11) | |
| Household with ≥ 1 person with chronic diseasec | |||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Yes | 1.22 (1.03–1.44) | 1.32 (1.12–1.57) | 1.32 (1.11–1.56) | 1.59 (1.19–2.13) | 1.26 (1.06–1.49) | 1.36 (1.15–1.62) | 1.39 (1.17–1.67) | 1.77 (1.31–2.38) | |
| Perceived income adequacyd | |||||||||
| Comfortable | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Enough to make ends meet | 1.21 (1.01–1.45) | 1.29 (1.06–1.55) | 1.56 (1.29–1.90) | 1.44 (0.98–2.10) | 1.19 (0.99–1.43) | 1.27 (1.04–1.54) | 1.50 (1.23–1.83) | 1.32 (0.90–1.94) | |
| Cautious with expenses | 1.43 (1.14–1.79) | 1.81 (1.44–2.28) | 2.49 (1.97–3.14) | 3.62 (2.45–5.34) | 1.37 (1.09–1.74) | 1.79 (1.41–2.27) | 2.28 (1.79–2.91) | 3.31 (2.21–4.94) | |
| Insufficient | 1.35 (0.75–2.42) | 1.87 (1.05–3.32) | 2.53 (1.43–4.46) | 8.09 (4.06–16.14) | 1.40 (0.76–2.55) | 1.99 (1.10–3.61) | 2.60 (1.44–4.70) | 8.13 (3.93–16.84) | |
| Fear of SARS-CoV-2 infectione | |||||||||
| Never/occasionally | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Often/almost always/always | 2.11 (1.60–2.79) | 4.55 (3.49–5.92) | 7.47 (5.76-9.68) | 10.76 (7.59–15.26) | 2.03 (1.53–2.68) | 4.20 (3.21–5.49) | 6.60 (5.06–8.62) | 9.13 (6.36–13.11) | |
| SARS-CoV-2 infectionf | |||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Yes | 0.72 (0.43–1.19) | 1.11 (0.69–1.77) | 1.20 (0.75–1.91) | 1.35 (0.64–2.87) | 0.65 (0.39–1.10) | 1.06 (0.66–1.72) | 1.19 (0.73–1.93) | 1.29 (0.57–2.89) | |
95%CI, 95% confidence interval, OR, odds ratio.
No insomnia as the reference category.
Multivariate model adjusted for gender and age.
Multivariate model adjusted for gender, age and education.
Multivariate model adjusted for gender, age, education and living alone.
Multivariate model adjusted for gender, age, education, household with ≥ 1 child; household with ≥1 person with chronic disease, perceived income adequacy and SARS-CoV-2 infection.
Multivariate model adjusted for gender, age, education, perceived income adequacy and living alone.
Table 3.
Crude and multivariate-adjusted odds ratio for the association between individual characteristics and nightmare' profiles during the first wave of COVID-19 pandemic.
| Nightmares |
||||
|---|---|---|---|---|
| Crude ORa (95%CI) |
Adjusted ORa (95%CI) |
|||
| Stable moderate | Stable severe | Stable moderate | Stable severe | |
| Gender | ||||
| Men | 1 | 1 | 1 | 1 |
| Women | 2.29 (1.92–2.72) | 3.04 (2.07–4.46) | – | – |
| Age (years) | ||||
| 16-39 | 1 | 1 | 1 | 1 |
| 40-49 | 1.03 (0.88–1.21) | 0.90 (0.66–1.23) | – | – |
| 50-59 | 0.69 (0.57–0.84) | 0.62 (0.42–0.91) | – | – |
| ≥ 60 | 0.61 (0.49–0.77) | 0.45 (0.28–0.74) | – | – |
| Education levelb | ||||
| University | 1 | 1 | 1 | 1 |
| High school | 0.94 (0.78–1.13) | 1.17 (0.84–1.65) | 1.02 (0.84–1.23) | 1.28 (0.91–1.80) |
| ≤ Elementary | 0.87 (0.56–1.36) | 0.98 (0.42–2.26) | 1.06 (0.67–1.67) | 1.35 (0.58–3.16) |
| Living aloneb | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.95 (0.80–1.14) | 1.18 (0.85–1.63) | 0.97 (0.81–1.17) | 1.23 (0.88–1.71) |
| Household with ≥ 1 childc | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.37 (1.16–1.61) | 1.71 (1.27–2.29) | 1.21 (1.02–1.44) | 1.50 (1.10–2.04) |
| Household with ≥ 1 person with chronic diseasec | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.16 (1.01–1.33) | 1.07 (0.82–1.40) | 1.23 (1.07–1.42) | 1.14 (0.87–1.49) |
| Perceived income adequacyd | ||||
| Comfortable | 1 | 1 | 1 | 1 |
| Enough to make ends meet | 1.27 (1.09–1.50) | 1.37 (0.98–1.91) | 1.25 (1.06–1.47) | 1.30 (0.93–1.82) |
| Cautious with expenses | 1.47 (1.23–1.76) | 2.13 (1.51–3.02) | 1.44 (1.19–1.74) | 2.01 (1.40–2.87) |
| Insufficient | 1.59 (1.06–2.39) | 2.65 (1.34–5.22) | 1.66 (1.10–2.53) | 2.60 (1.30–5.20) |
| Fear of SARS-CoV-2 infectione | ||||
| Never/occasionally | 1 | 1 | 1 | 1 |
| Often/almost always/always | 2.60 (2.24–3.03) | 7.09 (5.42–9.27) | 2.48 (2.12–2.91) | 6.62 (5.01–8.74) |
| SARS-CoV-2 infectionf | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.54 (1.06–2.21) | 2.89 (1.69–4.93) | 1.73 (1.19–2.53) | 3.09 (1.76–5.43) |
95%CI, 95% confidence interval, OR, odds ratio.
Stable-mild as the reference category.
Multivariate model adjusted for gender and age.
Multivariate model adjusted for gender, age and education.
Multivariate model adjusted for gender, age, education and living alone.
Multivariate model adjusted for gender, age, education, household with ≥ 1 child; household with ≥1 person with chronic disease, perceived income adequacy and SARS-CoV-2 infection.
Multivariate model adjusted for gender, age, education, perceived income adequacy and living alone.
In a multivariate model, and after adjusting for potential confounders theoretically defined as documented causes of each exposure variable and sleep problems, dose–response direct associations were found between insomnia symptoms or nightmares and, household with at least one person with chronic disease, perceived income adequacy and the fear of being infected with SARS-CoV-2. Those who perceived their income as insufficient and those who often felt fear about being infected with SARS-CoV-2 were the ones with higher chances of presenting the most severe profiles of insomnia symptoms (Insufficient income: aOR = 8.13 95%CI: 3.93–16.84; Often/almost always/always presenting fear of being infected with SARS-CoV-2 infection: aOR = 9.13 95%CI: 6.36–13.11) and nightmares (Insufficient income: aOR = 2.60 95%CI: 1.30–5.20; Often/almost always/always presenting fear of being infected with SARS-CoV-2 infection: aOR = 6.62 95%CI: 5.01–8.74). Having a diagnosis of SARS-CoV-2 virus infection was associated with worse patterns of nightmares about the pandemic (Table 2, Table 3).
4. Discussion
During the first six weeks of lockdown, we identified five insomnia and three nightmare profiles in the adult population of Portugal. Those profiles showed considerable heterogeneity between individuals in relation to insomnia symptoms and nightmares about the pandemic, varying in severity and over time.
Women, younger individuals and those who perceived their income as insufficient had higher chances of presenting the most severe sleep profiles. Besides the sociodemographic characteristics, the fear of getting the SARS-CoV-2 infection influenced the observed patterns of insomnia symptoms and nightmares about the COVID-19 pandemic during lockdown.
Even though the sleep profiles that emerged from this particular work cannot be directly compared with other studies, we were able to show that more than a quarter of our sample stated that they often or always had difficulties falling asleep or staying asleep during the study period, making them part of the two most severe insomnia profiles. A study published in Portugal in 2005 already presented a similar proportion of insomnia symptoms at least three nights per week, being reported by 28.1% of the general adult population [19].
In Europe, specifically during the COVID-19 pandemic, the prevalence of insomnia varied between 17.4% and 52.4% in Italy [11,20] and 37.6% in Greece [12]. In China, it was observed not only the occurrence of new insomnia complaints but also a 37% increase in the rates of clinical insomnia compared to before the peak of the COVID-19 pandemic [14]. Even though a comparison between studies is a challenging task, since each study referred to different time periods, used different measurement tools and had samples with different age ranges, all of them underline the high prevalence of insomnia symptoms worldwide, not only during the COVID-19 pandemic but also before that period and highlights that sleep problems are a major public health concern.
According to our findings, five percent of the participants reported to have nightmares about COVID-19 pandemic often, almost always or always. In a Brazilian study, they observed almost a three-fold increase in the number of participants reporting nightmares “once a week or more” comparing the periods before and after the pandemic and over two thirds of these participants described nightmares with a pandemic content [21], which is considerably higher compared to our present findings. Previous theoretical conceptualizations reported dreams and nightmares as adaptive biological responses with an adjustment function [22] that have been shown to be associated with psychopathology [23]. Additionally, an association between the frequency of nightmares and the chance of suicidal ideation was found during the pandemic [21]. Insomnia and nightmares triggered by stressful life events are frequent symptoms of psychiatric disorders that can persist over time [7]. Therefore, individuals who develop insomnia and nightmares during the COVID-19 pandemic may be at a greater risk for long-term psychiatric disorders, as it was observed in the prior SARS-CoV-1 epidemic [24] and could indicate the need for preventive public health interventions [25]. Moreover, these nightmare patterns were relative stable over time, contrasting with other studies showing an increase in dream recall and nightmares along the pandemic [15]. One possible explanation for our results could be the short study period at an early stage of the pandemic.
Our data suggest that there is a considerable heterogeneity between individuals in insomnia and nightmare profiles during lockdown as we identified five and three different profiles of insomnia and nightmares among Portuguese adults, respectively. These different profiles, that vary within- and between-persons, are in line with previous evidence showing that there is considerable night-to-night variability within the same person as well as significant heterogeneity between adults [26], and future research should explore long-term trajectories of such sleep variability. Independently of the lockdown, these results highlight the need to consider other factors which vary from day-to-day within older adults (eg, mood, daily demands, sleep environment) to better understand sleep variability. In any case, the fluctuation in insomnia and nightmare profiles during the pandemic is somehow expected, as sleep is a physiological process that depends on environment and social cues with a high variation according to the level of stress and the consequent physiological arousal over time [27,28].
In our study, being a female increased the odds of have a worse insomnia profile, which corroborates most of the studies conducted during lockdown [14,29]. A possible explanation is their higher propensity to stress related disorders and anxiety disorders [30], which could be due to biological and society-driven risk factors [31]. However, there are studies suggesting that men and women might have their sleep equally affected during the COVID-19 pandemic [32], which can also be explained by differences in study periods, contexts and sleep measurement methods.
Adults with less than 40 years of age were more likely to present worse insomnia symptoms and a higher frequency of nightmares about COVID-19 pandemic. These results can be, at least, partially explained by the high levels of mental health concerns in the younger population, namely due to the added stress of dealing with academic changes and a potential delay in their career due to the lockdown [33,34]. Additionally, the fact that young people are frequently engaged in precarious employments [35], and absorb a large amount of information from social media, can contribute to an increased stress level and lead to poor sleep [36]. Previous research has reported that a large proportion of college students already had poor sleep habits [37], and the COVID-19 pandemic has further worsened those sleep habits by allowing them to have less structured daily activities, including more hours free from school, staying up late, increase the use of mobile phone, and more frequent online games that were already recurrent [38].
Another important finding regarding social determinants was that participants that considered their income insufficient had higher chances of presenting the most severe profiles of insomnia symptoms and nightmares, independently of all other individual characteristics considered in the analysis. Socioeconomic disadvantage, which goes beyond objective measures of social position and encompasses the subjective perception of indicators of disadvantage, is known for its adverse impacts on health and has the potential to affect sleep [39]. The associations between poor sleep and low income are in line with previous evidence [39,40] and the COVID-19 pandemic does not change this robust association. Curiously, we did not find such a strong association between education and both types of sleep profiles, suggesting that the results regarding perceived income might reflect specific concerns and fear about losing the job and not having enough money for basic needs if confinement continues.
Fear is an adaptive response in the presence of a threat and, when that threat is uncertain and continuous like the current pandemic situation, it can become chronic and burdensome [41]. Therefore, it is somehow expected that this feeling can lead to sleep problems, as shown in the present results. Fear was also related to regular and social media use [41]. Considering the current level of online misinformation, a sufficient level of accurate information is imperative. Despite recent research suggesting that the COVID-19-related fear can be reversed to the level before the shutdown, generalized anxiety remains elevated over time [42], and therefore this fear should not be neglected.
Finally, a diagnosis of SARS-CoV-2 infection was significantly related to a more severe profile of nightmares about the virus. Daytime experiences with emotional content turn more easily into oneiric content therefore, a more severe profile of nightmares is expected with the increased ansiogenic context when experiencing the SARS-CoV-2 infection [43]. In addition, the absence of an association with insomnia symptoms might be due to the question format used to evaluate insomnia. We inquired about difficulties falling asleep or staying asleep during the past week, independently of being related to COVID-19 or not, while with nightmares the question was focused on the current context. Knowing that sleep disorders, including obstructive sleep apnea and insomnia, are common in patients hospitalized for SARS-CoV-2 infection [44], we would expect a more robust association with insomnia symptoms in our study if we had used more specific questions.
The question used to evaluate insomnia symptoms was not able to disentangle the specificities of insomnia subtypes: initial insomnia (difficulty in falling asleep at the beginning of the night), middle insomnia (difficulty in maintaining sleep) and terminal insomnia (early morning awakening) [45]. The question “During the past week, did you experience difficulties falling asleep or staying asleep?”, which is one of the most common questions used in surveys to measure insomnia [46], only covers information about initial and middle insomnia together. However, it was expected that the subtypes of sleep initiation and middle insomnia to be the most frequent subtypes of insomnia during the pandemic, as they are more related with a higher arousability due to the psychological distress experienced during the pandemic [13]. Knowing that insomnia subtypes might have differential effects in health [47], we recommend taking temporal effects of insomnia symptom subtypes into account in future investigations.
Some limitations should be highlighted. This sample was an opportunistic sample with limited representativeness of the general population. It comprises people with a comparatively high level of education and favorable income that may influence the prevalence estimates of insomnia and nightmares, ie, sleep problems might be underestimated. Moreover, this national study aimed to characterize a considerable number of health-related aspects of the Portuguese population during the first wave of the COVID-19 pandemic, and, for that reason, the questionnaire comprised a broader health characterization. In fact, sleep was not the primary outcome and, due to time constraints, it was not possible to apply a more complete and validated scale to measure sleep. As such, for a better sleep characterization, further studies should use validated scales such as Insomnia Severity Index or the Pittsburgh Sleep Quality Index for insomnia symptoms, and Nightmare Distress Questionnaire or Van Dream Anxiety Scale for nightmares. The improvement of these methodological aspects, will allow to assess other insomnia symptoms, such as early morning awakening with inability to return to sleep, daytime symptoms like attention, concentration, or memory problems and nightmares severity. Additionally, this internet-based open cohort was only stablished after the beginning of the pandemic and, for that reason, we were not able to collect information prior to the pandemic. This fact did not allow to disentangle the influence of the pandemic itself in this issues nor to assess important variables that could influence sleep patterns before the pandemic, such as depressive symptoms or anxiety. However, to the best of our knowledge, this is the first study characterizing, from a longitudinal perspective, insomnia symptoms and nightmare profiles among Portuguese population during the first weeks of the first national lockdown, allowing us to show the dynamics of those symptoms over time in this particular period.
5. Conclusion
The present study identified several different profiles of insomnia symptoms and nightmares during the first wave of the COVID-19 outbreak. We found strong social and psychological associated factors, namely age, gender, perceived income adequacy, a diagnosis of SARS-CoV-2 infection and the fear of a getting the infection influencing patterns of insomnia symptoms and nightmares about COVID-19 during lockdown.
Although some people will have only transient psychological and behavioral symptoms as a normal reaction to this traumatic event, if sleep problems persist over time, a pandemic of mental health problems might arise. With this work, we provide clues to early identify individuals at a higher risk of developing mental health problems triggered by poor sleep and help to act preventively.
Credit author statement
Each author participated sufficiently in the work to take public responsibility for its content and believes that the manuscript represents honest work. Gonçalves conducted the interpretation of the data and wrote the original draft of the article. Henriques, Costa and Lucas collaborated in the methodology of the study, reviewed and edited the article with important intellectual content. Severo and Correia collaborated in the formal analysis and interpretation of the data, and reviewed the article critically. Barros conceptualized the study and edited the article with important intellectual content.
Funding
This study was supported by national funding from the Foundation for Science and Technology – FCT (Portuguese Ministry of Science, Technology and Higher Education), under the projects UIDB/04750/2020 and LA/P/0064/2020. It is also acknowledged one Scientific Employment Stimulus contract to AH (CEECIND/01793/2017).
Footnotes
The authors declare that they have no conflict of interest.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.12.018.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleep.2021.12.018.
Contributor Information
the Task Force COVID-19 ISPUP – INESC TEC:
Ana Cristina Santos, Ana Isabel Ribeiro, Artur Rocha, Carla Lopes, Daniela Correia, Elisabete Ramos, Gonçalo Gonçalves, Henrique Barros, Joana Araújo, Makram Talih, Margarida Tavares, Milton Severo, Nuno Lunet, Paula Meireles, Raquel Duarte, Raquel Lucas, Rui Camacho, Sílvia Fraga, Sofia Correia, Susana Silva, and Teresa Leão
Conflict of interest
The following are the Supplementary data to this article:
Multimedia component 1
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020 Feb 20;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brooks S.K., Webster R.K., Smith L.E., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet (London, England) 2020 Mar 14;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mensagem do Presidente da República ao País sobre a declaração do estado de emergência (Palácio de Belém, 18 de março de 2020) Presidency of the Portuguese Republic; 18 March 2020. [Message of the President of the Republic to the Country on the declaration of a state of emergency] (in Portuguese). Retrieved 18 March 2020. [Google Scholar]
- 4.Becker S.P., Dvorsky M.R., Breaux R., et al. Prospective examination of adolescent sleep patterns and behaviors before and during COVID-19. Sleep. 2021 Aug 13;(8):44. doi: 10.1093/sleep/zsab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorgoni M., Scarpelli S., Alfonsi V., et al. Pandemic dreams: quantitative and qualitative features of the oneiric activity during the lockdown due to COVID-19 in Italy. Sleep Med. 2021 May;81:20–32. doi: 10.1016/j.sleep.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.2006;8:1e5. SM Factors affecting the continuity between waking and dreaming: emotional intensity and emotional tone of the waking-life event. Sleep Hypn. 2006;8:1–5. [Google Scholar]
- 7.Lavie P. Sleep disturbances in the wake of traumatic events. N Engl J Med. 2001 Dec 20;345(25):1825–1832. doi: 10.1056/NEJMra012893. [DOI] [PubMed] [Google Scholar]
- 8.Mellman T.A., Hipolito M.M. Sleep disturbances in the aftermath of trauma and posttraumatic stress disorder. CNS Spectr. 2006 Aug;11(8):611–615. doi: 10.1017/s1092852900013663. [DOI] [PubMed] [Google Scholar]
- 9.Hertenstein E., Feige B., Gmeiner T., et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019 Feb;43:96–105. doi: 10.1016/j.smrv.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Chattu V.K., Manzar M.D., Kumary S., et al. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel, Switzerland) 2018 Dec 20;7(1) doi: 10.3390/healthcare7010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cellini N., Canale N., Mioni G., et al. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020 Aug;29(4) doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voitsidis P., Gliatas I., Bairachtari V., et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatr Res. 2020 Jul;289:113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casagrande M., Favieri F., Tambelli R., et al. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020 Nov;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin L.Y., Wang J., Ou-Yang X.Y., et al. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021 Jan;77:348–354. doi: 10.1016/j.sleep.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scarpelli S., Gorgoni M., Alfonsi V., et al. The impact of the end of COVID confinement on pandemic dreams, as assessed by a weekly sleep diary: a longitudinal investigation in Italy. J Sleep Res. 2021 Jul 20 doi: 10.1111/jsr.13429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morin C.M., Carrier J. The acute effects of the COVID-19 pandemic on insomnia and psychological symptoms. Sleep Med. 2021 Jan;77:346–347. doi: 10.1016/j.sleep.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao C., Scullin M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020 Sep;73:1–10. doi: 10.1016/j.sleep.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Team R.C. R Foundation for Statistical Computing; Vienna, Austria: 2020. R: a language and environment for statistical computing. [Google Scholar]
- 19.Ohayon M.M., Paiva T. Global sleep dissatisfaction for the assessment of insomnia severity in the general population of Portugal. Sleep Med. 2005 Sep;6(5):435–441. doi: 10.1016/j.sleep.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 20.Gualano M.R., Lo Moro G., Voglino G., et al. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Publ Health. 2020 Jul 2;17(13) doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Musse F.C.C., Castro L.S., Sousa K.M.M., et al. Mental violence: the COVID-19 nightmare. Front Psychiatr. 2020;11:579289. doi: 10.3389/fpsyt.2020.579289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Revonsuo A. The reinterpretation of dreams: an evolutionary hypothesis of the function of dreaming. Behav Brain Sci. 2000 Dec;23(6):877–901. doi: 10.1017/s0140525x00004015. discussion 4-1121. [DOI] [PubMed] [Google Scholar]
- 23.Ohayon M.M., Morselli P.L., Guilleminault C. Prevalence of nightmares and their relationship to psychopathology and daytime functioning in insomnia subjects. Sleep. 1997 May;20(5):340–348. doi: 10.1093/sleep/20.5.340. [DOI] [PubMed] [Google Scholar]
- 24.Peng E.Y., Lee M.B., Tsai S.T., et al. Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. J Formosan Med Assoc (Taiwan yi zhi) 2010 Jul;109(7):524–532. doi: 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020 Oct;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dillon H.R., Lichstein K.L., Dautovich N.D., et al. Variability in self-reported normal sleep across the adult age span. J Gerontol B Psychol Sci Soc Sci. 2015 Jan;70(1):46–56. doi: 10.1093/geronb/gbu035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fortunato V.J., J. H. Stress and sleep quality: the moderating role of negative affectivity. Pers Indiv Differ. 2006;41(5):825–836. [Google Scholar]
- 28.Kocevska D., Blanken T.F., Van Someren E.J.W., et al. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. 2020 Dec;76:86–88. doi: 10.1016/j.sleep.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang C., Yang L., Liu S., et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatr. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li S.H., Graham B.M. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatr. 2017 Jan;4(1):73–82. doi: 10.1016/S2215-0366(16)30358-3. [DOI] [PubMed] [Google Scholar]
- 31.Albert P.R. Why is depression more prevalent in women? J Psychiatr Neurosci. 2015 Jul;40(4):219–221. doi: 10.1503/jpn.150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr Res. 2020 Jun;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., et al. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saúde Pública. 2020;36(4) doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- 34.Yuan S., Liao Z., Huang H., et al. Comparison of the indicators of psychological stress in the population of Hubei province and non-endemic provinces in China during two weeks during the coronavirus disease 2019 (COVID-19) outbreak in February 2020. Med Sci Mon Int Med J Exp Clin Res. 2020 Apr 15;26 doi: 10.12659/MSM.923767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bert F., Lo Moro G., Corradi A., et al. Prevalence of depressive symptoms among Italian medical students: the multicentre cross-sectional "PRIMES" study. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gradisar M., Wolfson A.R., Harvey A.G., et al. The sleep and technology use of Americans: findings from the National Sleep Foundation's 2011 Sleep in America poll. J Clin Sleep Med: Off Pub Am Acad Sleep Med. 2013 Dec 15;9(12):1291–1299. doi: 10.5664/jcsm.3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sivertsen B., Øverland S., Pallesen S. Trends in timing of sleep in the general population of Norway: 1980 to 20001. Percept Mot Skills. 2011 Oct;113(2):509–518. doi: 10.2466/02.06.13.PMS.113.5.509-518. [DOI] [PubMed] [Google Scholar]
- 38.Gellis L.A., Park A., Stotsky M.T., et al. Associations between sleep hygiene and insomnia severity in college students: cross-sectional and prospective analyses. Behav Ther. 2014 Nov;45(6):806–816. doi: 10.1016/j.beth.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 39.Grandner M.A., Patel N.P., Gehrman P.R., et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010 May;11(5):470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arber S., Bote M., Meadows R. Gender and socio-economic patterning of self-reported sleep problems in Britain. Soc Sci Med. 2009 Jan;68(2):281–289. doi: 10.1016/j.socscimed.2008.10.016. (1982) [DOI] [PubMed] [Google Scholar]
- 41.Mertens G., Gerritsen L., Duijndam S., et al. Fear of the coronavirus (COVID-19): predictors in an online study conducted in March 2020. J Anxiety Disord. 2020 Aug;74:102258. doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hetkamp M., Schweda A., Bäuerle A., et al. Sleep disturbances, fear, and generalized anxiety during the COVID-19 shut down phase in Germany: relation to infection rates, deaths, and German stock index DAX. Sleep Med. 2020 Nov;75:350–353. doi: 10.1016/j.sleep.2020.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eichenlaub J.B., van Rijn E., Gaskell M.G., et al. Incorporation of recent waking-life experiences in dreams correlates with frontal theta activity in REM sleep. Soc Cognit Affect Neurosci. 2018 Jun 1;13(6):637–647. doi: 10.1093/scan/nsy041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goldstein C.A., Rizvydeen M., Conroy D.A., et al. The prevalence and impact of pre-existing sleep disorder diagnoses and objective sleep parameters in patients hospitalized for COVID-19. J Clin Sleep Med. 2021 May 1;17(5):1039–1050. doi: 10.5664/jcsm.9132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. xliv. American Psychiatric Publishing, Inc.; Arlington, VA, US: 2013. p. 947. [Google Scholar]
- 46.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med: Off Pub Am Acad Sleep Med. 2007 Aug 15;3(5 Suppl):S7–S10. [PMC free article] [PubMed] [Google Scholar]
- 47.Chen T.Y., Saito Y. Longitudinal effects of nocturnal insomnia symptom subtypes and nonrestorative sleep on the incidence of depression among community-dwelling older adults: results from the Health and Retirement Study. Sleep Med. 2021 Mar;79:155–163. doi: 10.1016/j.sleep.2021.01.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1