Abstract
Background and aims
Worldwide the COVID-19 pandemic has accelerated sufferings of mental health and behaviour attitudes of people. Many countries, including Bangladesh, reported suicide as extreme consequences of the psychological burden influenced by COVID-19. The present study explores human stress and its factor influenced by COVID-19 in Bangladesh, which significantly affect the quality of life.
Methods
An online-based questionnaire survey was conducted among 651 adult Bangladeshi populations by capturing socio-demographic information, possible human stress, and consequences of the pandemic. A set of statistical tools such as Pearson's Correlation Matrix (PCM), T-test, Principal Component Analysis (PCA) and Hierarchical Cluster Analysis (HCA) were applied to identify the relationship between different factors and influential factors increasing human stress.
Results
More than 83% of the participants are facing COVID-19 related mental stress, which results in short temper, sleep disorder, and family chaos. PCA and HCA outcomes indicated a significant relationship between the respondents' opinions and human stress factors, which harmonized with the country's existing scenario. PCM results enlighten the relationship between human stress factors and found financial hardship, cutting back daily spending, and food crisis are interconnected together causes stress. Also, hampering students' formal education and future career plans significantly contribute to mental stress.
Conclusion
Based on the above findings, it's crucial to introduce a time-oriented strategy and implement precaution monitoring plans for Bangladesh. The rescue plan will help people to manage the pandemic and improve mental health to fight against psychological challenges related to COVID-19 and future pandemics.
Keywords: COVID-19, Public health, Stress, Psychology, Mental health
1. Introduction
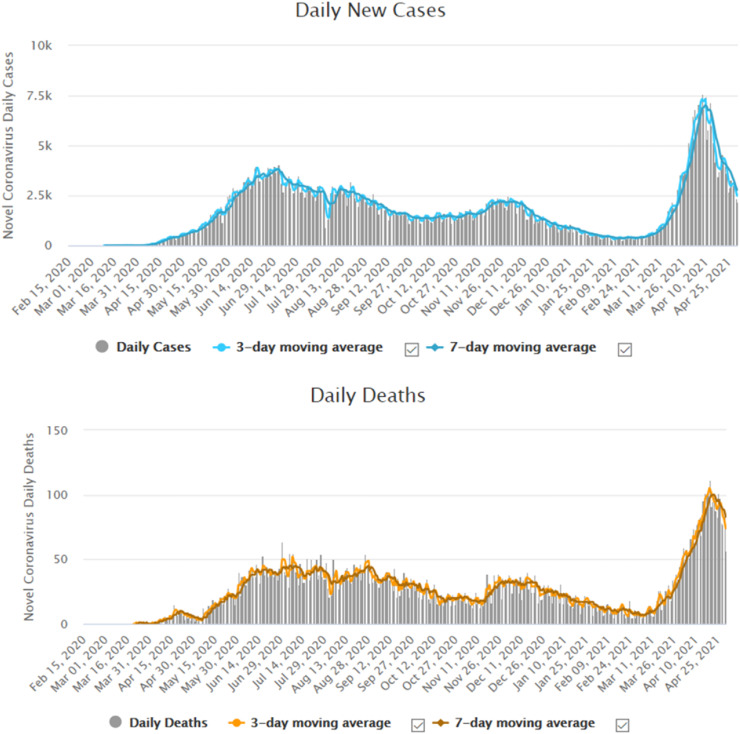
The COVID-19, officially known as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), (coronavirus disease) pandemic originating from the epicentre, Wuhan, China, started to spread rapidly across the world in December 2019 [1,2]. Fatigue, dry cough, fever, myalgia, and dyspnea may appear within 2–14 days of infection due to respiratory droplets and close contact with COVID-19 infected patients [[2], [3], [4], [5], [6]]. The World Health Organization (WHO) had to declare it a pandemic in early March 2020 due to its rapid global spread and challenges. A total of 146, 067, 511 active cases with 3,092,497 deaths were confirmed worldwide as of April 25, 2021, affecting all countries and territories [7]. The first COVID-19 case was reported in Bangladesh on March 8, 2020 [8,9], and the virus spread slowly at first, though a rapid case increase began in April 2020. According to the COVID-19 website launched by the Government of Bangladesh, till April 30, 2021, the virus had infected 759,132 people in the country, resulting in 11,450 deaths (Fig. 1 ). The country enforces lockdown as named public holidays from March 26 to May 31, 2020, likely in line with a global trend aimed at social distancing without emergencies [8,10].
Fig. 1.
COVID-19 active cases and deaths in Bangladesh till April 30, 2021 (Source: https://www.worldometers.info/coronavirus/country/bangladesh/).
The world has arguably failed to combat the COVID-19 induced physical treatments, and the mental health component has been neglected or overlooked [[11], [12], [13]]. COVID-19 studies have found amplified psychological problems and worse quality of life across countries and occupations (e.g., healthcare professionals to the general public), reflecting the risky people's upcoming worst mental and physical health situations [2,[14], [15], [16]]. Furthermore, most of the worldwide COVID-19 research concentrated on infection control, effective vaccine, and treatment, as well as the disease's spread and forecasting [12,15,[17], [18], [19]]. Thus, the psychological characteristics must be explored in a country like Bangladesh, whereas a limited number of studies are conducted to the authors best knowledge [[20], [21], [22]]. Although mental health strategies are not focused in the country, the government of Bangladesh launched an extensive campaign on public health awareness and announced a stimulus package worth $11.90 billion to be distributed across various sectors [23]. Besides, because the Bangladeshi people were in lockdown, quarantine, or social distance from March to May 2020, it is expected that direct or indirect psychiatric and economic suffering have increased during this time, as evidenced by COVID-19-related suicides in the country [17,24].
Thus, the present study tried to investigate the associations between COVID-19 stress with demographic characteristics, financial and food risk, mental/physical threat, health insecurity, and education and career uncertainty variables, which can aid in developing mental health strategies to combat the COVID-19 crisis.
2. Materials and method
2.1. Participants, procedures, and timeline of survey
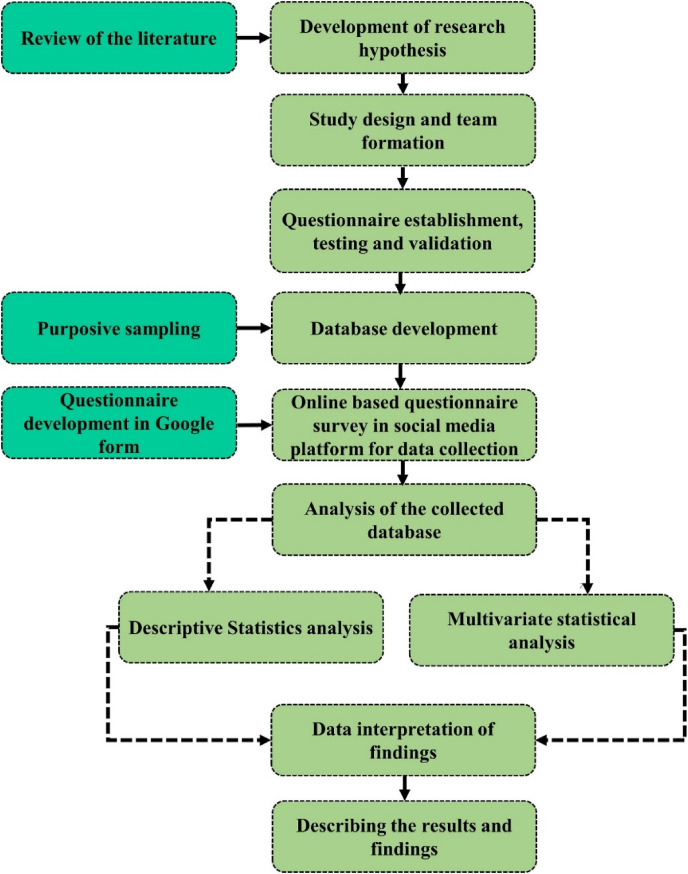
An online-based survey was conducted during the pick time of COVID -19 from May 10 to June 20, 2020, among the adult residents (20 years and above) of Bangladesh. An introductory paragraph describing the study's objective and ethical concerns of participating were shared with the respondents through social platforms, e.g., LinkedIn, Whatsapp, Twitter, Facebook, and Messenger. To ensure response from all the occupations, a research team was formed consisting of 20 members, and they were instructed to share the questionnaire survey link from their online platforms, where all age groups and professionals are exposed. The research team generated a database of target participants through social media screening based on their activities, education, occupation, knowledge and attitude associated with COVID-19. A total of 30 responses were collected from each team members based on the purposive sampling method. Total 750 participants were approached, and of these, 651 of them contributed to the online survey (63.80% male and mean age = 24.33 [±5.63] years). A flowchart describing the study methodology is demonstrated in Fig. 2 .
Fig. 2.
Flowchart of research methodology.
The respondent's consent was taken before the online survey, and they remained anonymous. Before starting to fill out the questionnaire, all contributors were informed of the study's specific objectives. Participants could only complete the survey once and able to terminate it whenever they wanted. The data's privacy and confidentiality were ensured.
2.2. Study mesures
In order to identify the human stresses associated with the COVID-19 pandemic in Bangladesh, a self-developed question was used. In addition, the questionnaire included basic socio-demographics (e.g., gender, age, occupation, and marital status), anxiety and fear related to COVID-19 (e.g., scared of taking treatment, healthcare facilities, concern for family members etc.), financial insecurities due to pandemic (e.g., job security, financial conditions, travel plan, and food supply) and effect on the education and future career plan after the lockdown.
2.3. Data analysis
The descriptive statistics, e.g., percentages, frequencies, and T-test were performed to understand respondents' basic characteristics. A set of established statistical methods, including Pearson Correlation Matrix (PCM), Principal Component Analysis (PCA), and Hierarchical Cluster Analysis (HCA) and T-test, were applied to identify the relationship between human stress-related studied factors. In large sample datasets, PCA is a data reduction tool that shows each potentiality of parameters and their confidence level. The Kaiser–Maier–Olkin (KMO) and Bartlett's Sphericity tests were used to confirm the PCA need before it was carried out. The KMO value results were 0.772, which is greater than 0.5 and the significance of Bartlett's sphericity test at p < 0.01 supported our datasets to be fitted for the PCA [[25], [26], [27]]. The number of factors was determined using Kaiser's Principle, which stipulated that only factors with eigenvalues greater than 1.0 be considered. In this study, Cronbach's alpha was used to assess the factor loadings' consistency and reliability. In social science research, Cronbach's alpha values greater than 0.6 (the Cronbach's alpha value was 0.83) are considered acceptable [[28], [29], [30]]. The PCA and the HCA are essential tools for detecting associations between studied factors. HCA helps to classify a population into various groups based on the same feature of a dataset, which may reveal causes, effects, and the source of any unidentified factors' relationships. In addition, HCA was used to estimate the number of clusters that might exist. The Statistical Package for the Social Sciences (SPSS) v. 25.0 was used to analyze the data in this study.
3. Result and discussion
3.1. Characteristics of the respondent
A total of 651 respondents contributed to the online survey, with 63.80% male and 36.20% female. The composition of age groups were 20 - <25 years (20.90%), 25 - <35 years (53.15%), 35 - <45 years (15.04%), 45 - <55 years (6.91%), and >55 years (3.99%) old. It was found that the frequency of young participants is higher than older and mid-age groups because of frequent use and access to social media. Among the respondents, 62% are single, 36.25% are married, and 1.75% are in an affair. However, more than half of the respondents were students in terms of occupation (52.64%), other groups such as private service holder (22.01%), businessman (5.96%), government service holder (4.26%), teacher (3.94%), unemployed (6.8%), and others (4.39%) participated in the study.
3.2. COVID – 19 influence on socioeconomic and psychological stress
COVID-19 infection rate is rising in Bangladesh through community transmission like in other parts of the world. Among the 651 respondents, 45.20% (n = 294) claimed that active COVID-19 case was identified in their community. The government has taken necessary steps to control the spread of the virus, fear of infection and help people minimise their anxiety and physiological stress like other developing countries [11,31]. However, 83.56% (n = 544) of the total respondents from the total sample reported being stressed due to the COVID-19 outbreak, which was determined by a simple question. Consistent with other studies, the COVID-19 stress is arbitrating factors included – (i) fear and tension of personal and family members life ii) feeling concern in taking any kind of health treatment or facilities iii) significant impact on travel plans iv) economic stress increase because of the probability of losing job or loss in the business v) economic status creat impact on food security for the upcoming days vi) hamper on formal education vii) creat concern on upcoming career viii) hamper in sleep due to mental stress ix) mental stress reduces working efficiency x) mental pressure creating short temper and chaos between family members and so on [[32], [33], [34], [35], [36], [37]].
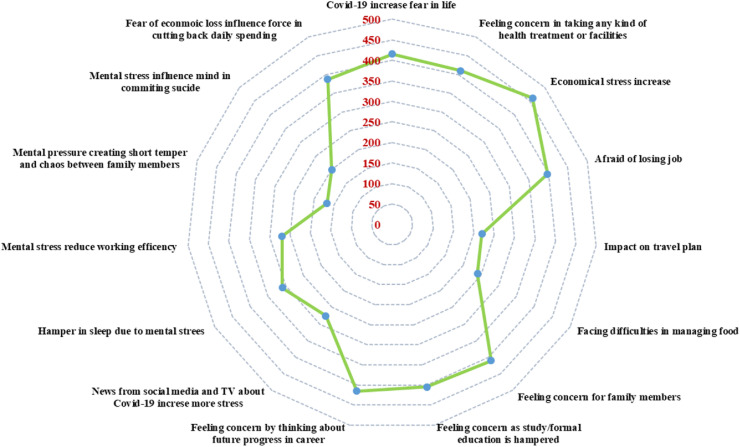
However, most of the respondents claimed COVID-19 significantly hamper their economic stability, creating health concerns, hindering scheduled study plans and future careers as the leading causes of stress (Fig. 3 ). Because of no family responsibilities or other issues to cause mental stress,103 (15.80%) respondents reported no stress. Less stressed people also indicated that they tend to take things easier, for example, being more resilient to traumatic events or not being aware enough of the consequences of COVID-19 related global threat status and finding happiness in every situation rather than being stressed out.
Fig. 3.
Spider diagram illustrates the perception of participants' causes of stress during the COVID-19 pandemic.
However, Table 1 reveals the descriptive statistics of the studied human stress factors and effects induced by COVID-19. It is established that COVID-19 created concern in most of the respondent's life (S2) for taking any kind of health treatment, with a mean value of 8.06 on the scale of 1–8 (1 indicating not applicable to 8 signifying highly agree). Most of the respondents agreed that COVID-19 increases fear in life (S1), with a second highest mean value of 7.06. The mean value of reason for stress and fear S3–S9 and S15 ranging from 3.71 to 6.51 indicates highly agree with the statement. Respondents claimed that getting updated news of COVID-19 from social media and television also aggravates stress (5.02). The stress of COVID-19 (S11–S14) hampers working efficiency (5.53), sound sleep (5.37), creating short temper and chaos between family members (3.99), and sometimes a group of people is feeling distressed with the situation, and their mind influences them in committing suicide (3.84). The COVID-19 pandemic worsened psychological issues, particularly depression, post-traumatic stress disorder, adjustment disorder, and fear, which are among the most common causes of suicide [3,38]. Financial stress related to the COVID-19 crisis, such as increasing poverty, economic stagnation, unemployment rate, and aggregate mental instabilities leading to suicide occurrences [19,26,31]; these occurrences have been reported in Bangladesh and neighbouring countries India and Pakistan [18,20,24,38,39]. Similar outcomes are also stated by Cellini et al. (2020) for Italy.
Table 1.
Descriptive Statistics of Factors affecting COVID-19 stress (n = 651).
| Impacts of COVID-19 | Mean | Std. error of mean | Median | Mode | Std. Dev. | Variance | Skewness | Kurtosis | Min. | Max |
|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19 increase fear in life (S1) 2 | 7.06 | −0.86 | 7 | 7 | 2.01 | 4.2 | −0.38 | −0.38 | 1 | 8 |
| Feeling concern in taking any kind of health treatment or facilities (S2) 1 | 7.42 | 0.44 | 7 | 8 | 2.29 | 3.71 | −0.7 | 0.31 | 1 | 8 |
| Economical stress increase (S3) 3 | 6.51 | 0.45 | 5 | 3 | 2.58 | 4.75 | 0.36 | −0.81 | 1 | 8 |
| Afraid of losing job (S4) 4 | 5.74 | 0.44 | 6 | 7 | 2.34 | 3.88 | −0.27 | −0.38 | 1 | 8 |
| Impact on travel plan (S5) | 4.97 | 0.41 | 8 | 8 | 1.76 | 2.24 | −1.65 | 4.3 | 1 | 8 |
| Facing difficulties in managing food (S6) | 3.71 | 0.43 | 7 | 7 | 2.08 | 3.06 | −0.95 | 1.15 | 1 | 8 |
| Feeling concern for family members (S7) 5 | 5.71 | −0.86 | 7 | 7 | 2.01 | 4.2 | −0.38 | −0.38 | 1 | 8 |
| Feeling concern as study/formal education is hampered (S8) 6 | 5.61 | 0.46 | 7 | 8 | 2.59 | 4.76 | −0.35 | −0.57 | 1 | 8 |
| Feeling concern by thinking about future progress in career (S9) 8 | 5.45 | 0.44 | 7 | 8 | 2.23 | 3.51 | −1.08 | 1.15 | 1 | 8 |
| News from social media and TV about COVID-19 increse more stress (S10) | 5.02 | 0.47 | 6 | 9 | 1.99 | 4.66 | −0.83 | −0.31 | 1 | 8 |
| Hamper in sleep due to mental strees (S11) | 5.37 | 0.44 | 6 | 8 | 2.39 | 4.04 | 0.03 | −0.53 | 1 | 8 |
| Mental stress reduce working efficency (S12) 7 | 5.53 | 0.45 | 6 | 8 | 2.46 | 4.29 | −0.1 | −0.58 | 1 | 8 |
| Mental pressure creating short temper and chaos between family members (S13) | 3.99 | 0.44 | 5 | 3 | 2.36 | 3.94 | 0.3 | −0.52 | 1 | 8 |
| Mental stress influence mind in commiting sucide (S14) | 3.84 | 0.42 | 4 | 3 | 2.02 | 2.88 | 1.48 | 1.67 | 1 | 8 |
| Fear of econmoic loss influence force in cutting back daily spending (S15) | 5.86 | −0.86 | 7 | 7 | 2.01 | 4.2 | −0.38 | −0.38 | 1 | 8 |
3.3. Factors affecting COVID-19 related stress: statistical analysis and results
3.3.1. Pearson correlation matrix (PCM) assessment
In this study, PCM is used to designate the relationship between the studied human stress factors (Table 2 ). A significant strong correlation was found among the statements S3, S4 and S15, indicating economic crisis, losing job is linked together, and fear of economic loss force in cutting back daily spending are linked which creates psychological stress of the respondents. A strong correlation is also found between S8 and S9 factors, which illustrates the association between formal education and future career. Formal education is hampered, which creates substantial stress to the young age respondent's life as they are worried about their future career. Again, a substantial positive correlation is found within S11 and S12, S13 and S14, and S1 and S2 linked with the effects of stress and health issues. Mental stress caused by a lack of sleep leads to irritability and chaos in the family and social life. Lockdown and fear of COVID-19 cause mental stress, which leads to sleep deprivation, irritability, and chaos in the family [15,40,41].
Table 2.
Pearson correlation matrix of the considered factors increasing COVID -19 related human stress (significant values (>0.5) are bold values).
| Factors | S1 | S2 | S3 | S4 | S5 | S6 | S7 | S8 | S9 | S10 | S11 | S12 | S13 | S14 | S15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S1 | 1 | ||||||||||||||
| S2 | 0.497∗∗ | 1 | |||||||||||||
| S3 | 0.135∗∗ | 0.121∗∗ | 1 | ||||||||||||
| S4 | 0.201∗∗ | 0.112∗∗ | .560∗∗ | 1 | |||||||||||
| S5 | 0.231∗∗ | 0.175∗∗ | 0.257∗∗ | 0.331∗∗ | 1 | ||||||||||
| S6 | 0.130∗∗ | 0.107∗∗ | .398∗∗ | 0.230∗∗ | 0.101∗∗ | 1 | |||||||||
| S7 | 0.367∗ | 0.501∗ | 0.204∗ | 0 | 0 | 0.098∗∗ | 1 | ||||||||
| S8 | 0.056∗∗ | 0.208∗ | 0.045∗∗ | 0.231∗∗ | 0.034∗∗ | 0.01∗∗ | 0.132∗∗ | 1 | |||||||
| S9 | 0.210∗∗ | 0.102∗∗ | 0.217∗∗ | 0 | 0.213∗∗ | 0.034∗∗ | 0 | 0.201∗∗ | 1 | ||||||
| S10 | 0.267∗∗ | 0.067∗∗ | 0.045∗∗ | 0.105∗∗ | 0.073∗∗ | 0.56∗∗ | 0.249∗∗ | 0.147∗∗ | 0.169∗∗ | 1 | |||||
| S11 | 0.360∗∗ | 0.203∗∗ | 0.487∗∗ | 0.490∗∗ | 0.032∗∗ | 0.022∗∗ | 0.110∗∗ | 0.390∗∗ | 0.521∗∗ | 0.301∗∗ | 1 | ||||
| S12 | 0.307∗∗ | 0.284∗∗ | 0.430∗∗ | 0.520∗∗ | 0 | 0.044∗ | 0.421∗∗ | 0.089∗ | 0.218∗∗ | 0.350∗∗ | 0.543∗∗ | 1 | |||
| S13 | 0.177∗∗ | 0.185∗∗ | 0.133∗ | 0.213∗∗ | 0.179∗∗ | 0 | 0.291∗∗ | 0.221∗∗ | 0.399∗∗ | 0.233∗∗ | 0.504∗∗ | 0.526∗∗ | 1 | ||
| S14 | 0.113∗ | 0.01∗ | 0.443∗∗ | 0.132∗ | 0 | 0 | 0.05∗ | 0.03∗ | 0.345∗∗ | 0.01∗ | 0.166∗∗ | 0.130∗∗ | 0.536∗∗ | 1 | |
| S15 | 0.239∗∗ | 0.06∗∗ | 0.533∗∗ | 0.545∗∗ | 0.332∗∗ | 0.210∗∗ | 0 | 0 | 0.115∗∗ | 0.04∗∗ | 0.07∗∗ | 0.224∗∗ | 0.06∗∗ | 0 | 1 |
3.3.2. Assessment of T-test
The T-test was performed to evaluate the relationship between stress factors and the demographic characteristics of the respondents. The T-test revealed that demographic factors such as age, gender, occupation, and marital status significantly impact mental stress (Table 3 ). Occupation is a significant factor in regulating human stress. For example, S3 and S4 statements discussed economic or financial stress and stress related to the fear of losing a job, both of which are closely related to the respondent's occupation. Unemployment, workforce reduction, and salary minimization are directly linked to stress syndromes, anxiety, depression, dysthymia, and even suicide [26,28].
Table 3.
T-test results indicating the relationship between COVID-19 induced factors and socio-demographic parameters.
| 95% Confidence Interval of the Difference |
||||||
|---|---|---|---|---|---|---|
| Factors | t | df | Sig. 2 Tailed | Mean difference | Upper | Lower |
| Gender | 25.06 | 651 | 0.00 | 3.102 | 3.74 | 3.0571 |
| Age | 76.70 | 651 | 0.00 | 27.047 | 27.68 | 27.2363 |
| Occupation | 72.03 | 651 | 0.00 | 1.849 | 2.48 | 1.7228 |
| Matrital Status | 45.05 | 651 | 0.00 | 2.226 | 2.86 | 2.0988 |
| S1 | 56.05 | 651 | 0.00 | 2.077 | 2.71 | 1.9516 |
| S2 | 48.87 | 651 | 0.00 | 1.646 | 2.28 | 1.5126 |
| S3 | 81.34 | 651 | 0.00 | 5.228 | 5.86 | 5.1534 |
| S4 | 78.34 | 651 | 0.00 | 4.517 | 5.15 | 4.4598 |
| S5 | 18.56 | 651 | 0.00 | 5.024 | 5.66 | 4.9593 |
| S6 | 42.21 | 651 | 0.00 | 3.751 | 4.39 | 3.7019 |
| S7 | 70.79 | 651 | 0.00 | 4.438 | 5.07 | 4.3763 |
| S8 | 75.06 | 651 | 0.00 | 5.748 | 6.38 | 5.655 |
| S9 | 79.01 | 651 | 0.00 | 4.572 | 5.21 | 4.5228 |
| S10 | 20.09 | 651 | 0.00 | 5.317 | 5.95 | 5.2497 |
| S11 | 71.03 | 651 | 0.00 | 5.209 | 5.84 | 5.1338 |
| S12 | 77.45 | 651 | 0.00 | 4.199 | 4.83 | 4.1403 |
| S13 | 54.08 | 651 | 0.00 | 4.359 | 4.99 | 4.3035 |
| S14 | 51.33 | 651 | 0.00 | 3.816 | 4.45 | 3.7549 |
| S15 | 73.02 | 651 | 0.00 | 2.650 | 3.29 | 2.5709 |
Due to the COVID-19 lockdown, many people in Bangladesh have lost their jobs, particularly those from low-income families. For example, the extreme economic fallout among Bangladeshi people living in rural areas reported a 79% drop in per capita income and an 82% drop in slum people from February to early April [10,24]. This deteriorating financial crisis has resulted in multiple issues, including food scarcity, treatment, and poverty which significantly accelerates life-threatening situations in the country. Due to the financial crisis, one suicide is attributed in Bangladesh influenced by COVID-19 [4,29,42]. However, the S8 and S9 statements related to students who are stressed because their studies and future careers are being hampered. Because of the COVID-19 lockdown and the closure of educational institutions, students' graduation times will be delayed, which will impact their future careers. The respondents' age has a significant impact on statements S11 and S12 as well (Table 3). The early age group, which includes students and job seekers (more than half of the respondents), these young people are facing stress, which is affecting their institutional education and future career prospects. Gender differences in psychological stress have not been found to have any significant effects, but respondents' marital status has been linked to stress.
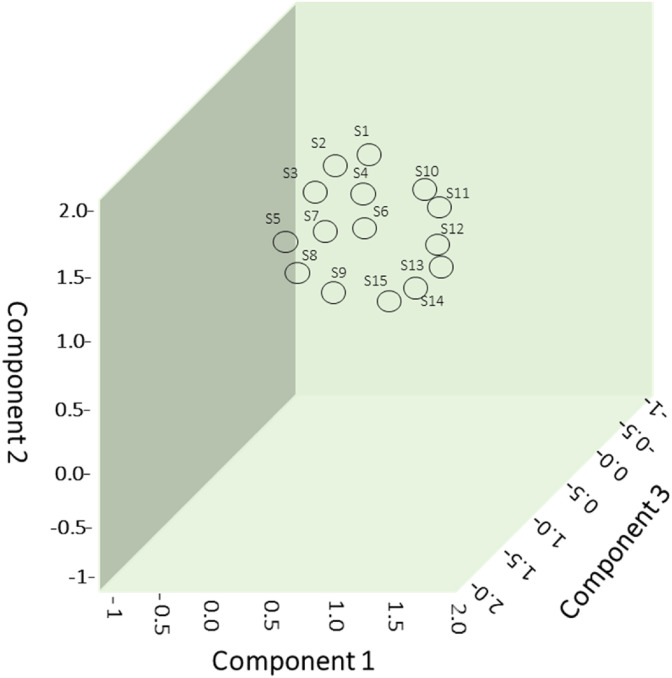
3.3.3. Consistency analysis of respondent's perception
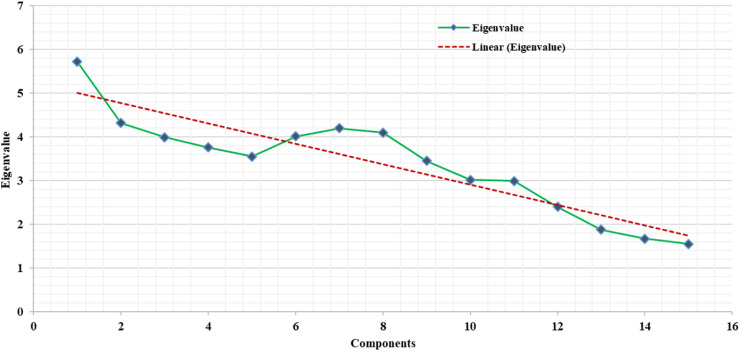
Multivariate statistical tools PCA and HCA were applied in this study to investigate the relationship between the respondent's perception and factors accountable for human stress. PCA was executed using Varimax rotation with Kaiser Normalization, which used to exploit the sum of variance of the factor coefficients [33,43,44], and better clarifies the potential causes of human stress (Ahmed et al., 2019; Bodrud-Doza et al., 2019, 2020b). Table 4 shows the calculated factor loadings, as well as the cumulative percentages and percentages of variance. PCA yielded a total of four factors, or principal components (PCs), accounting for 66.851% of the total variance. The plot of the rotation matrix was used to demonstrate the significant relationships between the studied variables (Fig. 5 ), while the scree plot determines the number of PCs to be retained in order to gain insight into the principal variable structure (Fig. 4). The loadings score generally divided into three categories: strong (>0.75), moderate (0.75–0.50), and weak (0.50–0.30) [2,12].
Table 4.
Varimax rotated Principal Component Analysis of the studied factors.
| Items | PC1 | PC2 | PC3 | PC4 |
|---|---|---|---|---|
| S1 | 0.297 | 0.778 | 0.699 | 0.193 |
| S2 | 0.178 | 0.316 | 0.789 | 0.098 |
| S3 | 0.893 | 0.309 | 0.584 | 0.242 |
| S4 | 0.687 | 0.229 | 0.43 | 0.208 |
| S5 | 0.241 | 0.775 | 0.271 | 0.101 |
| S6 | 0.275 | 0.742 | 0.288 | 0.55 |
| S7 | 0.199 | 0.145 | 0.443 | 0.455 |
| S8 | 0.117 | 0.157 | 0.852 | 0.062 |
| S9 | 0.469 | 0.677 | 0.758 | 0.439 |
| S10 | 0.027 | 0.305 | 0.562 | 0.248 |
| S11 | 0.707 | 0.675 | 0.178 | 0.152 |
| S12 | 0.857 | 0.655 | 0.295 | 0.136 |
| S13 | 0.511 | 0.725 | 0.254 | 0.823 |
| S14 | 0.257 | 0.245 | 0.259 | 0.756 |
| S15 | 0.787 | 0.365 | 0.439 | 0.319 |
| % of variance | 17.241 | 16.797 | 16.598 | 16.215 |
| Cumulative % | 17.241 | 34.038 | 50.636 | 66.851 |
Fig. 5.
Principal Component Analysis using component plot in rotated space.
Fig. 4.
Principal Component Analysis using the scree plot of the characteristic roots.
The first PC1 explained 17.241% of the total variance, with significant positive effects of mental stress caused by economic stress (S3: 0.893) and stress reduce working efficiency (S12:0.857) and moderate positive loading in insufficient sleep (S11: 0.707) (Table 4). Virus-prevention measures (such as lockdown, isolation, and social distancing) place a burden on the Bangladeshi people, people are stressed out because they are afraid of losing their jobs, as many companies have already begun to reduce staff and lower wages. The Asian Development Bank estimates that about nine million jobs will be lost in Bangladesh due to the ongoing COVID-19 lockdown, which will cost the country $3 billion in GDP [45].
Furthermore, PC2 explained 16.797% of the total variance, with strong positive loading of fear created in life as a result of the COVID-19 outbreak (S1: 0.778), as well as the impact on travel plan (S5: 0.775), and moderate positive loading on facing difficulties in managing food (S6: 0.742) (Table 4). Many people, particularly Bangladesh's low-income groups, are stressed about food management as a result of the slowdown in economic activities (e.g., transportation, industries, and business). Because of the distress of virus infection, the general public is now attempting to avoid going to hospitals and clinics unless it is an emergency. Also, due to the rapid transformation of the virus, all the travel plan is cancelled, which impacted people in business and students attempted for higher studies abroad. At the same time, due to fear of contracting the virus, Bangladeshi doctors and health care workers are refusing to treat patients without first ensuring that they are not infected with COVID-19. This adds burdens to the emergency patients' and may even put their lives at risk. For example, a recent Bangladeshi press report on a 40-year-old woman's suicide due to not receiving treatment for blood vomiting and throat pain illustrates how serious the issue of unnecessary public suffering becomes when seeking emergency treatment in hospitals [46,47].
PC3 explained 16.598% of the total variances, with strongly positive loadings of the hindrance of formal education (S8: 0.852), future progress in career (S9: 0.758), and taking any kind of health treatment (S2:0.789) during COVID-19, which significantly increase mental stress (Table 4). All educational institutions in Bangladesh are closed, and the education ministry plans to open the institutions in May 2021. E-learning and online class systems are not implemented due to the country's socioeconomic structure and limited access to internet facilities, which delays students' graduation process and causes mental stress. Although the country has not formally adopted the e-learning system, some institutes appear to have done so. However, students with fewer resources (e.g., high internet service costs, adequate internet connection availability in the residing village, having a device to connect to live classes, etc.) may be vulnerable to mental distress. For example, in China, a case of a middle-school student attempting suicide was reported due to a lack of digital device availability for online classes [16]. Besides, suicides (i.e., a mother-son suicide pact) have been reported in Bangladesh as a result of father-son issues with online schooling [42]. Finally, PC4 illustrates 16.215% of the total variance, with significant strong positive loading on mental pressure creating short temper and chaos between family members (S13:836) and influencing suicide (S14:756). The COVID-19 pandemic worsened psychological issues, particularly depression, post-traumatic stress disorder, adjustment disorder, and chaos between family members, which are among the most common causes of suicide [3,38].
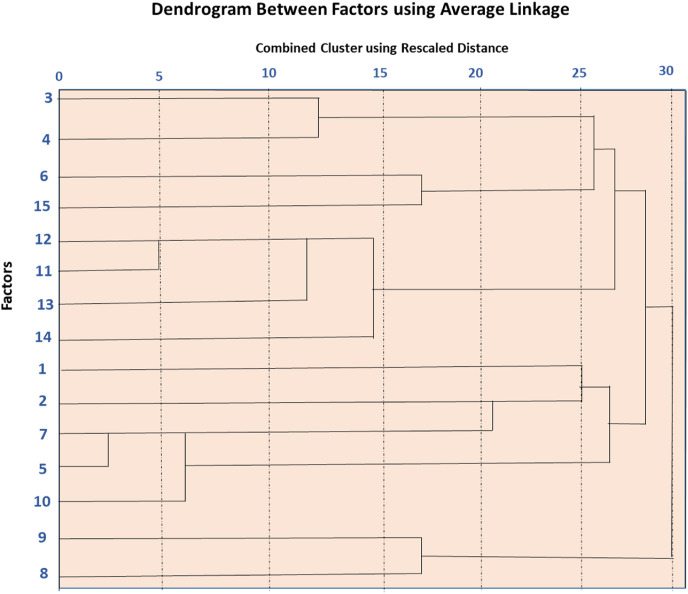
HCA was also used to describe how the studied variables affect human stress. HCA results were found to be highly correlated with PCA results and were classified into four major clusters or groups (Fig. 6 ). In general, each cluster has similar characteristics for the factors being studied. Statements S3–S4, S6, and S15 are related to the stress caused by the financial and food crises found in Cluster 1. On the other hand, Cluster 2 includes S11–S14 which are related to the physical and mental effects of stress similar to PCA 1. Cluster 3 delineates fear of COVID-19 virus infection and includes S1–S2, S5, S7, and S10. Cluster 3 is made up of statements S3–S5, all of which are related to the stress caused by the financial and food crises. Finally, statements S8 and S9 related to the stress of the young age group due to hindrance in education are found in cluster 4, similar to PCA3. Overall, statistical analysis results can be used effectively to describe Bangladesh's current situation.
Fig. 6.
Dendrogram showing the Hierarchical Cluster Analysis of the analyzed factors.
4. Limitations of the study
The current research has some limitations, including being a cross-sectional study with a non-representative sample and overwhelming feedback from students and jobholders. The COVID-19 associated human stress valuation may be inadequate by the lack of validated tools, despite the use of self-developed questions that took into account factors applicable for Bangladesh's perspective affected by the pandemic. Despite its flaws, the current study offers effective insights into human stress and its interactions with other factors.
5. Conclusion
The COVID-19 pandemic produces fear and stress on Bangladeshi citizens. The study found that stress associated with COVID-19 significantly impacts financial stability creates short temper, hamper sound sleep, reduces work efficiency, generates chaos in the family, and sometimes turns people to conduct suicide. Several effective statistical applications were used in this study to demarcate the causes and factors controlling human stress. The correlation matrix results illustrate the linkage between economic difficulties and food scarcity and the association between the stoppage of formal education and future career plan causes stress in students and job seekers. Overall, lockdown significantly impacted mass people's socioeconomic conditions, and they fail to meet basic human needs. In addition, poor governance, communication, infrastructure, and inadequate healthcare facilities cause anxiety and disrupt human life. As a result, it is critical to implement a time-oriented policy that is accompanied by care monitoring in order to manage the pandemic condition and promote the healthy mental health of the citizens.
Authors contribution
Sajit Amit, conceived and designed the experiments, performed the experiments; Lumbini Barua, analyzed and interpreted the data; Abdulla – Al Kafy, contributed reagents, materials, analysis tools and data; wrote the paper.
Funding
This research doesn't receive any funding
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We want to express our heartiest gratitude to all the participants for their inputs in conducting this study. The authors also like to express their gratitude to the experts of DIGON, a consultancy firm for Research and Publication, for proofreading the manuscript.
References
- 1.Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int J Environ Res Publ Health. 2020;17:2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Y., Di Y., Ye J., Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2021;26:13–22. doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- 3.Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29 doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jahan S., Araf K., Gozal D., Griffiths M., Mamun M.A. Depression and suicidal behaviors among Bangladeshi mothers of children with Autistic Spectrum Disorder: a comparative study. Asian journal of psychiatry. 2020 doi: 10.1016/j.ajp.2020.101994. [DOI] [PubMed] [Google Scholar]
- 5.Pakpour A.H., Griffiths M.D., Lin C.-Y. Assessing the psychological response to the COVID-19: a response to Bitan et al.“Fear of COVID-19 scale: psychometric characteristics, reliability and validity in the Israeli population”. Psychiatr Res. 2020 doi: 10.1016/j.psychres.2020.113127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I., et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain and behavior. 2020;10 doi: 10.1002/brb3.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Who Situation report. March, 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports2021
- 8.Mamun M.A., Sakib N., Gozal D., Bhuiyan A.I., Hossain S., Bodrud-Doza M., et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J Affect Disord. 2021;279:462–472. doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Satu M., Howlader K.C., Islam S.M.S. 2020. "Machine learning-based approaches for forecasting covid-19 cases in Bangladesh," machine learning-based approaches for forecasting COVID-19 cases in Bangladesh (may 30, 2020) [Google Scholar]
- 10.Kamruzzaman M. BRAC Institute of Governance and Development; 2020. Coronavirus: poor income drops 80% in Bangladesh. [Google Scholar]
- 11.Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addiction. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trotogott R.L. A comparative analysis of data privacy impacted by COVID-19 contact tracing in the European union, the United States, and Israel: sacrificing civil liberties for a public health emergency. ILSA J. Int'l & Comp. L. 2020;27:55. [Google Scholar]
- 13.Gorzycki M. Wipf and Stock Publishers; 2020. Teaching for apocalypse: COVID-19's message to educators and those they serve. [Google Scholar]
- 14.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Restubog S.L.D., Ocampo A.C.G., Wang L. Elsevier; 2020. Taking control amidst the chaos: emotion regulation during the COVID-19 pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liao S., Zhou Y., Liu Y., Wang R. Variety, frequency, and type of Internet use and its association with risk of depression in middle-and older-aged Chinese: a cross-sectional study. J Affect Disord. 2020;273:280–290. doi: 10.1016/j.jad.2020.04.022. [DOI] [PubMed] [Google Scholar]
- 17.Mamun M.A., Bodrud-Doza M., Griffiths M.D. Hospital suicide due to non-treatment by healthcare staff fearing COVID-19 infection in Bangladesh? Asian journal of psychiatry. 2020;54:102295. doi: 10.1016/j.ajp.2020.102295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dsouza D.D., Quadros S., Hyderabadwala Z.J., Mamun M.A. Aggregated COVID-19 suicide incidences in India: fear of COVID-19 infection is the prominent causative factor. Psychiatr Res. 2020;290:113145. doi: 10.1016/j.psychres.2020.113145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Griffiths M.D., Mamun M.A. COVID-19 suicidal behavior among couples and suicide pacts: case study evidence from press reports. Psychiatr Res. 2020;289:113105. doi: 10.1016/j.psychres.2020.113105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bodrud-Doza M., Shammi M., Bahlman L., Islam A.R.M., Rahman M. Psychosocial and socio-economic crisis in Bangladesh due to COVID-19 pandemic: a perception-based assessment. Frontiers in public health. 2020;8:341. doi: 10.3389/fpubh.2020.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hossain M.M., Tasnim S., Sultana A., Faizah F., Mazumder H., Zou L., et al. Epidemiology of mental health problems in COVID-19: a review. F1000Research. 2020;9 doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mamun M.A., Akter T., Zohra F., Sakib N., Bhuiyan A.I., Banik P.C., et al. Prevalence and risk factors of COVID-19 suicidal behavior in Bangladeshi population: are healthcare professionals at greater risk? Heliyon. 2020;6 doi: 10.1016/j.heliyon.2020.e05259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The-Financial-Express . The financial express. 2020. COVID-19: govt so far announces $11.90b stimulus packages.https://thefinancialexpress.com.bd/economy/bangladesh/covid-19-govt-so-far-announces-1190b-stimulus-packages-1590759538 [Google Scholar]
- 24.Bhuiyan A.I., Sakib N., Pakpour A.H., Griffiths M.D., Mamun M.A. COVID-19-related suicides in Bangladesh due to lockdown and economic factors: case study evidence from media reports. Int J Ment Health Addiction. 2020:1–6. doi: 10.1007/s11469-020-00307-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bodrud-Doza M., Islam A.T., Ahmed F., Das S., Saha N., Rahman M.S. Characterization of groundwater quality using water evaluation indices, multivariate statistics and geostatistics in central Bangladesh. Water Science. 2016;30:19–40. [Google Scholar]
- 26.Mucci N., Giorgi G., Roncaioli M., Perez J.F., Arcangeli G. The correlation between stress and economic crisis: a systematic review. Neuropsychiatric Dis Treat. 2016;12:983. doi: 10.2147/NDT.S98525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kafy A.-A., Rahman M.S., Islam M., Al Rakib A., Islam M.A., Khan M.H.H., et al. Prediction of seasonal urban thermal field variance index using machine learning algorithms in Cumilla, Bangladesh. Sustainable Cities and Society. 2020;64:102542. [Google Scholar]
- 28.Shammi M., Bodrud-Doza M., Islam A.R.M.T., Rahman M.M. COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: a case from Bangladesh. Heliyon. 2020;6 doi: 10.1016/j.heliyon.2020.e04063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Banna M.H.A., Sayeed A., Kundu S., Christopher E., Hasan M.T., Begum M.R., et al. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. Int J Environ Health Res. 2020:1–12. doi: 10.1080/09603123.2020.1802409. [DOI] [PubMed] [Google Scholar]
- 30.Kafy A.-A., Naim M.N.H., Subramanyam G., Faisal A.-A., Ahmed N.U., Al Rakib A., et al. Cellular Automata approach in dynamic modeling of land cover changes using RapidEye images in Dhaka, Bangladesh. Environmental Challenges. 2021:100084. [Google Scholar]
- 31.Barkur G., Vibha G.B.K. Sentiment analysis of nationwide lockdown due to COVID 19 outbreak: evidence from India. Asian journal of psychiatry. 2020;51:102089. doi: 10.1016/j.ajp.2020.102089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahorsu D.K., Imani V., Lin C.-Y., Timpka T., Broström A., Updegraff J.A., et al. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: an actor-partner interdependence modelling. Int J Ment Health Addiction. 2020:1–15. doi: 10.1007/s11469-020-00340-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shammi M., Bodrud-Doza M., Islam A.R.M.T., Rahman M.M. Environment, Development and Sustainability; 2020. Strategic assessment of COVID-19 pandemic in Bangladesh: comparative lockdown scenario analysis, public perception, and management for sustainability; pp. 1–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Limongi J.E., de Oliveira S.V. vol. 8. 2020. pp. 139–149. ("COVID-19 e a abordagem One Health (Saúde Única): uma revisão sistemática," Vigilância Sanitária em Debate: sociedade, Ciência & Tecnologia (Health Surveillance under Debate: society, Science & Technology)–Visa em Debate). [Google Scholar]
- 36.Hossain A., Ali M., Khan H.R., Ahsan G. medRxiv; 2020. Mental wellbeing in the Bangladeshi healthy population during nationwide lockdown over COVID-19: an online cross-sectional survey. [Google Scholar]
- 37.Pakpour A.H., Griffiths M.D. The fear of COVID-19 and its role in preventive behaviors. Journal of Concurrent Disorders. 2020;2:58–63. [Google Scholar]
- 38.Mamun M.A., Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty?–The forthcoming economic challenges for a developing country. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shoib S., Nagendrappa S., Grigo O., Rehman S., Ransing R. Factors associated with COVID-19 outbreak-related suicides in India. Asian journal of psychiatry. 2020;53 doi: 10.1016/j.ajp.2020.102223. e102223-e102223. [DOI] [PubMed] [Google Scholar]
- 40.Jakovljevic M., Bjedov S., Jaksic N., Jakovljevic I. COVID-19 pandemia and public and global mental health from the perspective of global health security. Psychiatr Danub. 2020;32:6–14. doi: 10.24869/psyd.2020.6. [DOI] [PubMed] [Google Scholar]
- 41.Yeasmin S., Banik R., Hossain S., Hossain M.N., Mahumud R., Salma N., et al. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: a cross-sectional study. Child Youth Serv Rev. 2020;117:105277. doi: 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mamun M.A., Chandrima R.M., Griffiths M.D. Mother and son suicide pact due to COVID-19-related online learning issues in Bangladesh: an unusual case report. Int J Ment Health Addiction. 2020:1–4. doi: 10.1007/s11469-020-00362-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahmed N., Bodrud-Doza M., Islam S.D.-U., Choudhry M.A., Muhib M.I., Zahid A., et al. Hydrogeochemical evaluation and statistical analysis of groundwater of Sylhet, north-eastern Bangladesh. Acta Geochimica. 2019;38:440–455. [Google Scholar]
- 44.Bodrud-Doza M., Bhuiyan M.A.H., Islam S.D.-U., Rahman M.S., Haque M.M., Fatema K.J., et al. Hydrogeochemical investigation of groundwater in Dhaka City of Bangladesh using GIS and multivariate statistical techniques. Groundwater for Sustainable Development. 2019;8:226–244. [Google Scholar]
- 45.Begum M., Farid M.S., Alam M.J., Barua S. COVID-19 and Bangladesh: socio-economic analysis towards the future correspondence. Asian Journal of Agricultural Extension, Economics & Sociology. 2020:143–155. [Google Scholar]
- 46.Mamun M.A., Griffiths M.D. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian journal of psychiatry. 2020;51:102073. doi: 10.1016/j.ajp.2020.102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rahman M.S., Lassi Z.S., Islam S.M.S. Risks to Bangladeshi children and young people during covid-19 outbreak. BMJ. 2020;369 doi: 10.1136/bmj.m2299. [DOI] [PubMed] [Google Scholar]