Abstract
Objectives:
To propose invasive cervical root resorption (ICRR) as an unrecognized and/or overlooked etiologic factor in the failure of response of an impacted tooth to orthodontic traction and to underline the importance of cone beam computerized tomography (CBCT) for early and accurate diagnosis of ICRR.
Materials and Methods:
Fourteen patients (age 13–21 years) with impacted canines (15 canines) that had failed to respond to orthodontic forces and that exhibited ICRR formed the case series for this investigation. The initial diagnosis, treatment, clinical and radiographic expression of failure, and adverse effects on adjacent teeth were analyzed.
Results:
Initial diagnosis had been performed on plane radiographs. The orthodontist was absent during surgery in 11 patients. Nine canines had been exposed by open procedures. ICRR was not related to the severity of impaction. Its diagnosis was made on existing radiographs, new films, and/or new CBCT. The severity of the lesions was Class 3 or 4, and the teeth were finally extracted. Loss of anchorage characterized 11 patients. Apical resorption of the roots of adjacent teeth was diagnosed in 9 patients.
Conclusions:
ICRR is a frequently undiagnosed or unrecognized cause of failure of orthodontic resolution of impacted canines and should be distinguished from replacement resorption. CBCT should be used for its early detection and accurate assessment of potential damage to adjacent anchor teeth.
Keywords: Impacted canines, Invasive cervical root resorption, Failure, Ankylosis
INTRODUCTION
Orthodontic treatment is usually aimed at aligning erupted teeth, but in 1%–3% of patients, it also has to address impacted teeth.1,2 In these latter cases, it is necessary to combine surgery to uncover the impacted tooth with orthodontics to bring the buried teeth into their place in the arch.
Because of the complexity of the combined orthosurgical treatment modality, treatment for patients with impacted canines may sometimes fail.3,4 In an earlier article, an analysis of factors contributing to the failure of the response of impacted canines to orthodontic traction revealed that ankylosis was blamed as the etiologic factor in 32.4% of the patients.5 However, in that article, a thorough diagnosis using cone beam computerized tomography (CBCT) was not performed on all patients. Retrospective CBCT and histologic examination performed on a number of these extracted teeth revealed typical invasive cervical root resorption (ICRR) lesions in advanced stages.
ICRR is a rare, insidious, and aggressive form of external root resorption, also known as extracanal invasive resorption.6 Typically, it begins at a focal point on the surface of the root below the epithelial attachment in the clinical cervical area and progresses into dentine coronally, apically, and circumpulpally, halting only at the predentine layer surrounding the pulp. Typically, it does not involve the pulp until very advanced stages. Thus, extensive dentinal destruction can occur in the complete absence of untoward symptoms.7
The pathogenesis of ICRR is still unclear but has been attributed to injury to the cementum at the cementoenamel junction (CEJ), which exposes the underlying dentin.8,9 Microscopic analysis of the cervical region of teeth has shown frequent gaps in the cementum, which leave the underlying mineralized dentin exposed and vulnerable to osteoclastic root resorption.10 Exposed dentin has been reported to generate a host of molecular biological events involving cytokines, enzymes, and hormones, which attract clastic cells from the periodontal ligament that is responsible for the progressive hard tissue resorptive process.9,11,12
The aim of the present investigation was to raise the specter of ICRR as an unrecognized and/or undiagnosed etiologic factor in the failure of response of an impacted tooth to orthodontic traction.
MATERIALS AND METHODS
Institutional ethical board approval was granted to conduct this study. A case series of 14 healthy patients (7 females and 7 males, age 13–21 years) with 15 impacted maxillary canines was culled from a much larger group of patients5 who had been referred to two of the authors for second opinions after these teeth failed to respond to the treatment that had been provided by the referring orthodontist. All the referring orthodontists had more than 10 years of experience in orthodontic practice. The failed canines in these 14 patients were each retrospectively and serially diagnosed with ICRR (which was seen bilaterally in only one patient) by the present authors. The diagnosis of ICRR was made directly from existing radiographs, fresh plane films, and/or new CBCT. The typical radiolucent appearance of ICRR was seen in the cervical area of the teeth concerned (Figures 1 and 2).
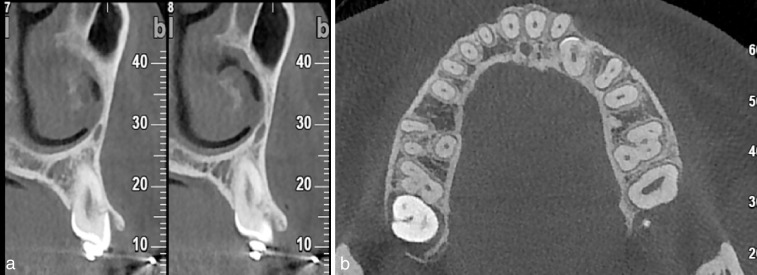
Figure 1.
(A) Periapical and (B) panoramic views of a failed impacted canine, showing a distal cervical lesion that has mushroomed inward and extended into the crown.
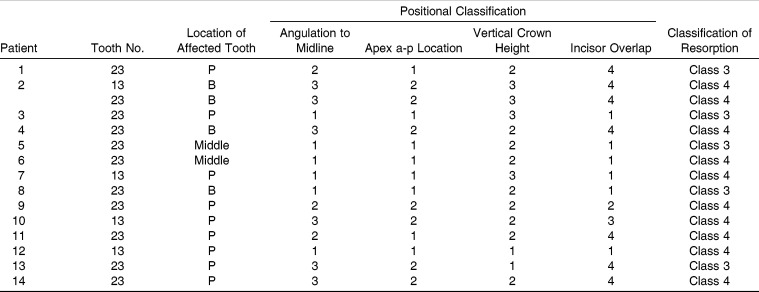
Figure 2.
Views from cone beam CT. (A) Transaxial view (vertical slice) through the impacted canine. (B) Axial view (horizontal slice) showing advanced Class 4 cervical root resorption.
Initial pretreatment radiographic records were available for all patients. For the purposes of the present study, each failed canine was considered an individual entity. The cases were taken consecutively within this referral system for inclusion in the investigative sample.
From the patient records, the following treatment details were gathered:
-
A. Details related to the impacted canine:
-
B. Details related to the initial condition, diagnosis, and treatment:
Original radiographic documentation initially used for diagnosis and treatment planning.
Duration of treatment between initiation of orthodontics and the realization of failure.
Method of surgical exposure (closed or open).
Orthodontist present or absent in the operating theater.
-
C. Details related to the diagnosis of failure:
Non-eruption, intrusion of adjacent teeth.
Radiographic documentation used for the diagnosis of failure.
Apical root resorption of anchor teeth.
D. Final outcome.
In addition, two examiners assessed blindly the presence or absence, the severity, and the location of ICRR on the plane film images and the corresponding reconstructed CBCT images in patients for whom both forms of imaging were available.
Statistical Analysis
The intraclass correlation test was used to assess intrarater reliability in assessing the positional classification and the extent of root resorption.
RESULTS
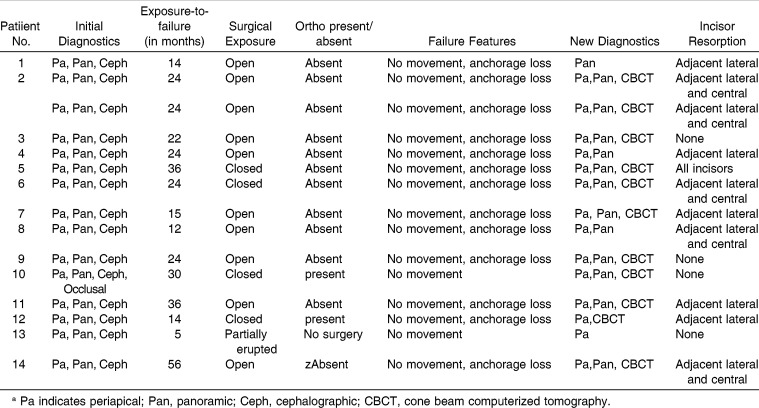
Table 1 shows that the initial location relative to the adjacent incisor varied considerably. Nine of the affected canines were palatally displaced, four were buccally displaced, and two were in the midalveolus. Six canines were normally angulated, and nine showed an exaggerated angulation to the midsagittal plane. The apex was normally positioned in the a-p plane for eight canines and above the first premolar in seven canines. In no patient was the apex more distally located. Most of the canines (n = 11) were relatively close to the occlusal plane. Eight canines showed an almost complete crown overlap of the adjacent incisor, while seven canines were situated in a normal a-p position. The extent of the resorptive lesion was classified as Class 3 in five teeth and Class 4 in the remaining 10. It is to be noted that a CBCT examination was not performed initially in any of the cases. The overall intrarater reliability for image assessment was excellent (r > .9).
Table 1.
Sample Description
The initial radiographic imaging included plane radiographs only, usually a panoramic view and cephalometric film, together with a variable number of periapical and other views (Table 2).
Table 2.
Factors Related to Orthodontic Treatment and to Diagnosis of ICRR
Open surgical exposure was performed in nine patients (10 canines) while four patients (four canines) were treated using a closed procedure. In one patient (patient 13) the affected tooth had spontaneously partially erupted at the beginning of orthodontic treatment and no surgery was needed. The orthodontist was present at the surgical exposure for two patients only (Table 2); thus, in cases where closed procedures were performed, the attachment on the impacted canine was bonded by the surgeon.
A fully bracketed fixed appliance with a passive heavy stainless steel main archwire provided the anchor base in each patient in the sample. Traction was applied with the use of elastic chains or thread, between attachments on the teeth direct to the labial archwire, except in those patients where two directions of traction were indicated. The mean duration of treatment, from initiation to realization of failure, was 24 ± 12 months.
Failure was determined on the basis of nonmovement of the target teeth. Obvious signs of anchorage loss (intrusion and tipping of adjacent teeth with creation of lateral/anterior open bite) were seen in 12 patients (13 teeth).
Resorption of the roots of adjacent lateral incisors was diagnosed in six patients (six teeth), and resorption of both lateral and central incisors was seen in five patients (12 teeth) (Table 2).
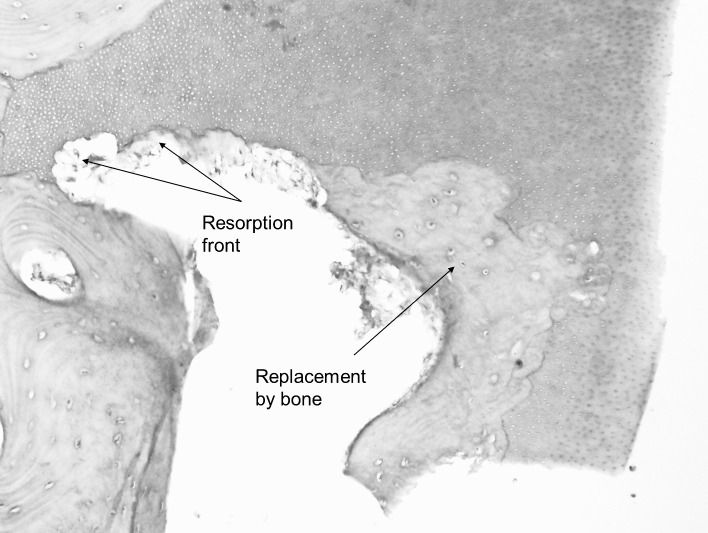
Imaging of ICRR and root resorption of adjacent teeth included preexisting initial radiographs, fresh plane films prescribed by the referring practitioner during the treatment in all patients, and CBCT prescribed by the authors in 12 patients (Table 2). Postextraction histologic examination was carried out in two patients and showed areas of replacement of tooth structure by bonelike calcified tissue (Figure 3). The final outcome for each of the ICRR-affected teeth was extraction.
Figure 3.
Histologic section of an extracted canine with ICRR. Arrows show extensive resorption lacunae and areas of bone deposition in the CEJ area.
DISCUSSION
ICRR has been the subject of discussion in the endodontic and traumatology literature over the past three decades. Although Heithersay6 reported that previous orthodontics was the main single predisposing factor for ICRR, its relevance has been almost entirely overlooked by orthodontists. In relation to impacted teeth, a search of the orthodontic literature lacks any reference to the condition, apart from a published opinion that presented no supportive evidence or illustrative example.14
Exposure and application of directional traction to an impacted maxillary canine is a routine and largely successful undertaking. In patients in which the impacted tooth does not respond, the practitioner assumes that the tooth is ankylosed.4 This empirical clinical diagnosis implies the presence of replacement resorption, which cannot always be confirmed radiographically, nor can it be confirmed histologically unless the tooth is extracted. Therefore, the diagnosis of ankylosis relies only on typical clinical features.
The evidence presented here shows that the differential diagnosis of ankylosis needs to include ICRR, as the patients display the following common clinical signs:
The impacted tooth does not respond to orthodontic traction.
The adjacent teeth show typical signs of loss of anchorage, that is, tipping toward the impacted tooth and intrusion with creation of open bite.
However the diagnosis may differ insofar as the following characteristics are concerned:
ICRR does not eliminate the physiologic mobility of a normal tooth and, in the earlier stages, it lacks the metallic sound on percussion that is typical of an ankylosed tooth. The exception is in relation to the more advanced cases, where hard tissue may penetrate the area, showing extensive replacement of tooth structure by bonelike calcified tissue (Figure 3).7
ICRR-related replacement resorption is site specific, in contrast to the trauma or age-related replacement resorption, which may affect a large area of the root.
Surgical luxation and immediate reapplication of the traction force may be prescribed for an ankylosed tooth but is inappropriate in the case of ICRR, unless the resorptive tissue is removed.9
The present sample was, of necessity, small because of the relative rarity of the condition, but it is also the first reported case series of ICRR affecting impacted canines. Awareness of the condition by orthodontists is of paramount importance as ICRR begins and progresses asymptomatically, rapidly destroying the root of the tooth and extending into the crown, where it undermines the enamel. Because the ability to restore the affected teeth and to maintain them as integral parts of the dentition depends to a large extent on the amount of residual unaffected hard tissue, early diagnosis is vital. Treatment of early incipient ICRR lesions in erupted teeth is possible and includes exposure of the resorption lacunae with removal of the dentinoclastic material and granulation soft tissue. This needs to be followed by elimination of the defect with restorative materials and then by orthodontic extrusion to elevate the healthy dentinal margins to form a gingival pocket of manageable depth.5,15,16 Endodontic therapy may then be indicated electively for reasons of retention of a permanent restoration of the tooth. For unerupted teeth, effective treatment depends on ease of access.
The diagnosis in the present sample was established very late, and extraction was the final outcome in all cases. The missed diagnosis was partially due to lack of awareness of ICCR by the treating practitioners but also to the exclusive use of plane radiographs as the imaging tool. Conventional radiographs yield limited information because of the two-dimensional nature of images, geometric distortion, and anatomical noise.17,18 In cases of displaced teeth, superimposition of anatomical structures and roots of adjacent teeth make the diagnosis of incipient lesions at the cervical area practically impossible. The only imaging tool that may provide an absolute diagnosis of the existence, location, and extent of an ICRR lesion in its early stages is CBCT. Its sensitivity and specificity is significantly higher than that of conventional plane radiographs 18 and permits the extent and depth of root resorption to be accurately distinguished and defined.19
The teeth included in this sample represent the sum total of the ICRR affected maxillary canine cases referred to or treated by the authors. It should be clearly understood that the claim is not made that all cases with ICRR will fail to respond. This study does not discount the possibility that some ICRR-affected impacted teeth may be successfully treated by routine orthodontic traction. Given that all patients in the sample exhibited Class 3 or 4 degrees of severity, one may be permitted to speculate that perhaps Class 1 and 2 patients may be treated successfully by orthodontic traction. Whether this is because the defect that is produced in the periodontal ligament is below a certain critical size or whether bone has not yet secondarily been deposited in the lesion remains to be determined.
Treatment difficulty and duration have been associated with the degree of deviation of the canine from its normal position13,20–22 and the possibility that perhaps the occurrence of ICRR might be similarly linked to complex movements and force levels; duration was therefore investigated. The results show that in all four parameters that described the location of the canines in the present study, the initiation of ICRR showed no affinity to those that were severely displaced in preference to those in which the location was close to normal.
Most of the canines in this study were exposed by an open surgical approach in the absence of the orthodontist. In such circumstances, the surgeon is much more likely to err on the side of wider exposure in order to be able to place a surgical pack and maintain a wound opened for later attachment bonding.5 This approach could potentially cause mechanical damage to the CEJ area and may predispose it to the initiation of ICRR, as suggested by Heithersay.6 If bonding is performed during the surgical exposure, accidental leakage of orthophosphoric acid into the CEJ area might conceivably generate an ICRR lesion.23
Failure to recognize that a tooth has not responded to the frequently renewed forces may typically result in the continuous application of heavier and heavier orthodontic forces by the orthodontist. Heavy extrusive forces cause more significant root resorption than light forces.24,25 Furthermore, during tipping movements most of the force concentrates at the cervical region.26,27 Chan and Darendeliler24 showed that the cervical region had eight times more root resorption in the heavy-force group compared with the light-force group, while the other regions did not seem to have significant differences in the force levels. Furthermore, regions under compression had more root resorption than regions under tension, and there was more resorption in regions under heavy compression than in regions under light compression.
Heithersay6 speculated that excessive orthodontic forces at the cervical region of the tooth might result in tissue necrosis adjacent to exposed root dentin. This might result in mononuclear precursor cells being stimulated to differentiate into odontoclasts, which are attracted to and resorb the exposed root dentin.
Heavy forces also cause loss of anchorage (intrusion) and significant root resorption of the adjacent anchorage teeth. It is again reasonable to speculate that in the present context and in light of the excessively long periods of traction of the canines in the present sample (average of 24 ± 12 months), intrusion caused by the reactive forces is the likely cause of this arguably iatrogenic, apical root resorption of the anchor teeth.
CONCLUSIONS
ICRR is an overlooked cause of failure of orthodontic resolution of impacted canines.
If no movement of the impacted canine is observed, a CBCT should be considered to check for ICRR and assess damage of adjacent teeth.
Early diagnosis is critical if the implications of ICRR are to be overcome.
ACKNOWLEDGMENTS
The authors express their gratitude to the referring orthodontists for their candor in supplying details of the treatment provided and for their concern for the welfare of their patients.
REFERENCES
- 1.Dachi SF, Howell FV. A survey of 3,874 routine full-mouth radiographs. I. A study of retained roots and teeth. Oral Surg Oral Med Oral Pathol. 1961;14:916–924. doi: 10.1016/0030-4220(61)90003-2. [DOI] [PubMed] [Google Scholar]
- 2.Brin I, Becker A, Shalhav M. Position of the maxillary permanent canine in relation to anomalous or missing lateral incisors: a population study. Eur J Orthod. 1986;8:12–16. doi: 10.1093/ejo/8.1.12. [DOI] [PubMed] [Google Scholar]
- 3.Becker A, Chaushu S. Success rate and duration of orthodontic treatment for adult patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2003;124:509–514. doi: 10.1016/s0889-5406(03)00578-x. [DOI] [PubMed] [Google Scholar]
- 4.Becker A, Chaushu G, Chaushu S. Analysis of failure in the treatment of impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2010;137:743–754. doi: 10.1016/j.ajodo.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 5.Becker A. The Orthodontic Treatment of Impacted Teeth 3rd ed. Oxford: Wiley-Blackwell; 2012. [Google Scholar]
- 6.Heithersay GS. Invasive cervical resorption: an analysis of potential predisposing factors. Quintessence Int. 1999;30:83–95. [PubMed] [Google Scholar]
- 7.Heithersay GS. Clinical, radiologic, and histopathologic features of invasive cervical resorption. Quintessence Int. 1999;30:27–37. [PubMed] [Google Scholar]
- 8.Brosjo M, Anderssen K, Berg JO, Lindskog S. An experimental model for cervical resorption in monkeys. Endod Dent Traumatol. 1990;6:118–120. doi: 10.1111/j.1600-9657.1990.tb00405.x. [DOI] [PubMed] [Google Scholar]
- 9.Patel S, Kanagasingam S, Pitt Ford T. External cervical resorption: a review. J Endod. 2009;35:616–625. doi: 10.1016/j.joen.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 10.Neuvald L, Consolaro A. Cementoenamel junction: microscopic analysis and external cervical resorption. J Endod. 2000;26:503–508. doi: 10.1097/00004770-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Ramos Sde P, Ortolan GO, Dos Santos LM, et al. Anti-dentine antibodies with root resorption during orthodontic treatment. Eur J Orthod. 2011;33:584–591. doi: 10.1093/ejo/cjq145. [DOI] [PubMed] [Google Scholar]
- 12.Iqbal MK. Clinical and scanning electron microscopic features of invasive cervical resorption in a maxillary molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e49–e54. doi: 10.1016/j.tripleo.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 13.Stivaros N, Mandall NA. Radiographic factors affecting the management of impacted upper permanent canines. J Orthod. 2000;27:169–173. doi: 10.1093/ortho/27.2.169. [DOI] [PubMed] [Google Scholar]
- 14.Consolaro A. Orthodontic traction: possible consequences for maxillary canines and adjacent teeth. Part 1. Dent Press J Orthod. 2010;15:15–23. [Google Scholar]
- 15.Bergmans L, Van Cleynenbreugel J, Verbeken E, et al. Cervical external root resorption in vital teeth. J Clin Periodontol. 2002;29:580–585. doi: 10.1034/j.1600-051x.2002.290615.x. [DOI] [PubMed] [Google Scholar]
- 16.Smidt A, Nuni E, Keinan D. Invasive cervical root resorption: treatment rationale with an interdisciplinary approach. J Endod. 2007;33:1383–1387. doi: 10.1016/j.joen.2007.07.036. [DOI] [PubMed] [Google Scholar]
- 17.Patel S, Dawood A, Whaites E, Pitt Ford T. New dimensions in endodontic imaging: part 1. Conventional and alternative radiographic systems. Int Endod J. 2009;42:447–562. doi: 10.1111/j.1365-2591.2008.01530.x. [DOI] [PubMed] [Google Scholar]
- 18.Patel S. New dimensions in endodontic imaging: Part 2. Cone beam computed tomography. Int Endod J. 2009;42:463–475. doi: 10.1111/j.1365-2591.2008.01531.x. [DOI] [PubMed] [Google Scholar]
- 19.Becker A, Chaushu S, Casap-Caspi N. Cone-beam computed tomography and the orthosurgical management of impacted teeth. J Am Dent Assoc. 2010;141(suppl 3):14S–18S. doi: 10.14219/jada.archive.2010.0360. [DOI] [PubMed] [Google Scholar]
- 20.Zuccati G, Ghobadlu J, Nieri M, Clauser C. Factors associated with the duration of forced eruption of impacted maxillary canines: a retrospective study. Am J Orthod Dentofacial Orthop. 2006;130:349–356. doi: 10.1016/j.ajodo.2004.12.028. [DOI] [PubMed] [Google Scholar]
- 21.Crescini A, Nieri M, Buti J, Baccetti T, Pini Prato GP. Orthodontic and periodontal outcomes of treated impacted maxillary canines. Angle Orthod. 2007;77:571–577. doi: 10.2319/080406-318.1. [DOI] [PubMed] [Google Scholar]
- 22.Stewart JA, Heo G, Glover KE, et al. Factors that relate to treatment duration for patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2001;119:216–225. doi: 10.1067/mod.2001.110989. [DOI] [PubMed] [Google Scholar]
- 23.Blomlof J, Lindskog S. Periodontal tissue-vitality after different etching modalities. J Clin Periodontol. 1995;22:464–468. [PubMed] [Google Scholar]
- 24.Chan E, Darendeliler MA. Physical properties of root cementum: part 7. Extent of root resorption under areas of compression and tension. Am J Orthod Dentofacial Orthop. 2006;129:504–510. doi: 10.1016/j.ajodo.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 25.Montenegro VC, Jones A, Petocz P, Gonzales C, Darendeliler MA. Physical properties of root cementum: Part 22. Root resorption after the application of light and heavy extrusive orthodontic forces: a microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2012;141:e1–e9. doi: 10.1016/j.ajodo.2011.06.032. [DOI] [PubMed] [Google Scholar]
- 26.McGuinness N, Wilson AN, Jones M, Middleton J, Robertson NR. Stresses induced by edgewise appliances in the periodontal ligament–a finite element study. Angle Orthod. 1992;62:15–22. doi: 10.1043/0003-3219(1992)062<0015:SIBEAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Tanne K, Sakuda M, Burstone CJ. Three-dimensional finite element analysis for stress in the periodontal tissue by orthodontic forces. Am J Orthod Dentofacial Orthop. 1987;92:499–505. doi: 10.1016/0889-5406(87)90232-0. [DOI] [PubMed] [Google Scholar]