Abstract
Objective:
To evaluate the pharyngeal airway and maxillary sinus volume changes after mandibular setback surgery combined with maxillary advancement and/or impaction surgery.
Materials and Methods:
Seventeen Class III skeletal patients (11 females, 6 males) who required bimaxillary orthognathic surgery were selected. Volumetric measurements were performed using cone beam computed tomography (CBCT) scans preoperatively and 3.9 ± 0.87 months postoperatively. All the CBCT scans were assessed and analyzed using MIMICS 14.0 software. Preoperative and postoperative volumes of pharyngeal airway and maxillary sinuses and the relationship between the amounts of surgical movement of the jaws and the above volumes were statistically evaluated.
Results:
The pharyngeal airway area presented no significant change except for the lower and total pharyngeal airway volumes in males, in whom a significant decrease was observed (4196.27 ± 2061.11 mm3 and 3375.53 ± 3624.67 mm3, respectively). No significant change was observed in the minimal cross-sectional area of the pharyngeal airway. There was a significant decrease in the volume of the maxillary sinuses after the surgery by 3448.09 ± 3315.56 mm3. No correlation was found between the amount of skeletal movement and the change in the volume of pharyngeal airway or maxillary sinuses.
Conclusion:
There was a significant decrease only for lower and total pharyngeal airway volumes in males and a significant decrease in the volume of the maxillary sinuses.
Keywords: Pharyngeal airway, Maxillary sinus, Volume, Cone beam computed tomography, Class III bimaxillary surgery
INTRODUCTION
In patients with severe skeletal and dental dysplasia combined orthodontic-orthognathic surgical treatment offers a solution to the problem. For cases in which both mandible and maxilla are responsible for the Class III skeletal deformity, bimaxillary surgery is indicated.
A very important aspect of the surgical correction of a skeletally Class III relationship is that it causes changes in the position of the hyoid bone and the tongue. The posterior shift of the tongue base is associated with an increase in the contact length between the soft palate and the tongue. This change appears to push the soft palate posteriorly and to decrease the pharyngeal airway space (PAS).1
As a result of these changes in hard and soft tissues, it has been suggested2 that mandibular setback surgery produces a shift in oropharyngeal characteristics to a morphology commonly associated with sleep-disordered breathing, typified by obstructive sleep apnea (OSA). In bimaxillary surgery during which the maxilla is advanced, in addition to mandibular setback, this effect may be less pronounced, as shown by the conflicting results among the authors.3,4
It has also been noted5 that maxillary impaction surgery may influence the maxillary sinus. The superior positioning of the maxilla obtained by removal of bone in the vertical direction may result in a decrease in the maxillary sinus area. The clinical implications of such a decrease in sinus area are unknown.
In the past, the majority of research has measured airway and maxillary sinuses mainly in two dimensions; however, these structures are three dimensional. A new-generation dentofacial imaging system, namely, cone beam computed tomography (CBCT), was relatively recently introduced, contributing to the diagnosis and treatment planning related to maxillofacial deformities.
The purpose of the current pilot study was to evaluate—using CBCT—the pharyngeal airway and maxillary sinus volume changes following bimaxillary surgical treatment of Class III skeletal deformities. In addition, we also aimed to determine if a correlation exists between the amount of the surgical movement of the jaws and the amount of change in the volumes of the pharyngeal airway and maxillary sinus.
MATERIALS AND METHODS
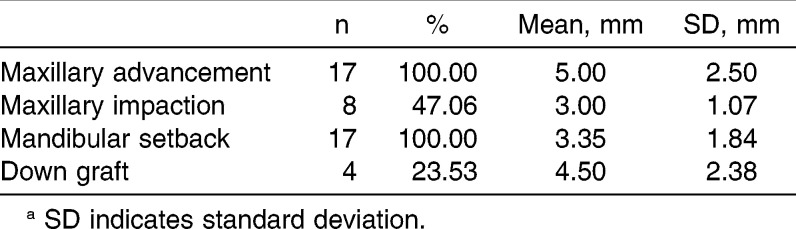
The sample for this study consisted of 17 patients who were under treatment for the combined orthodontic and surgical correction of their skeletal Class III malocclusion. The selection criteria according to which patients were selected were as follows: completed growth and development, Class III skeletal relationship scheduled to be treated by bimaxillary orthognathic surgery (mandibular setback combined with maxillary advancement, with or without maxillary impaction), lack of systemic disease, and lack of syndrome. All subjects were white and from the same geographic area. Our sample consisted of six male and 11 female patients with a mean age of 22.59 years. All 17 patients underwent mandibular setback and maxillary advancement, while eight patients underwent maxillary impaction in addition to maxillary advancement and mandibular setback. Four patients underwent mandibular setback, maxillary advancement, and maxillary down graft (Table 1).
Table 1.
Amounts of Surgical Movement of the Jawsa
Informed consent forms were signed by all patients or their parents, and this project was approved by the local institutional ethical committee. All patients were referred for preoperative CBCT evaluation within a period of 1 week before surgery (T1). All of the postsurgical CBCT scans were obtained during a period of 10–22 weeks postoperatively (T2). The average interval period between the surgery and the second scan was 3.90 ± 0.87 months. All of the scans were acquired with the patient sitting upright with the Frankfort horizontal plane parallel to the floor, at maximum intercuspation. The patient's head position was adjusted with the help of two laser beams, one parallel to the floor, coinciding with the Frankfort horizontal plane, and with one vertical beam passing through the patient's facial midline. The patients were asked not to swallow and not to move their heads or tongues during exposure.
The technical properties of the cone beam machine (Iluma Imtec, 3M, St Paul, Minn) we used are as follows: focal spot: 0.3 mm × 0.3 mm; X-ray tube working with 120 KV; X-ray tube current: 1–4 mA; detector size: 19.5 cm × 24.5 cm; scanning with 360° rotation; radiation: 555 microsieverts maximum; scanning time, 40 seconds maximum and 7.8 seconds minimum; field of view or imaging area: 14.2 cm × 21.1 cm; voxel size: 0.0936 mm; and gray scale: 14 bit. The data obtained from CT images were transferred to a network computer workstation, where volumetric changes of the pharyngeal airway and maxillary sinuses were measured using MIMICS 14.0 software (Materialise Europe, World Headquarters, Leuven, Belgium).
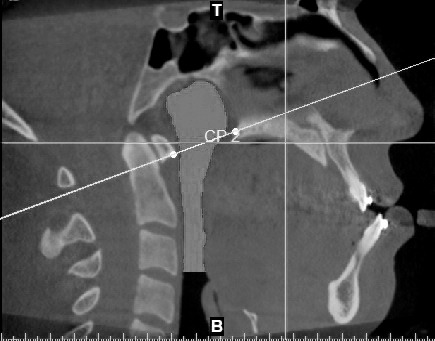
All CBCT scans were processed and analyzed by the same operator. The method that was applied involved the following steps: initially, on the sagittal view the slice for which all of the borders of the pharyngeal airway were clearly defined was selected (Figure 1). Thresholding was applied with a minimum limit of −1024 Hounsfield Units (HU) and a maximum of −526 HU. The pharyngeal airway was cropped, according to the following borders: The anterior border was defined by a vertical plane passing through PNS. The superior border was the roof of the pharynx. The posterior border was the posterior pharyngeal wall. The inferior border was a horizontal plane passing from the most anterior and inferior point of the third vertebra (Figure 2). Then, the connection with the outer air was cropped slice by slice (Figure 3).
Figure 1.
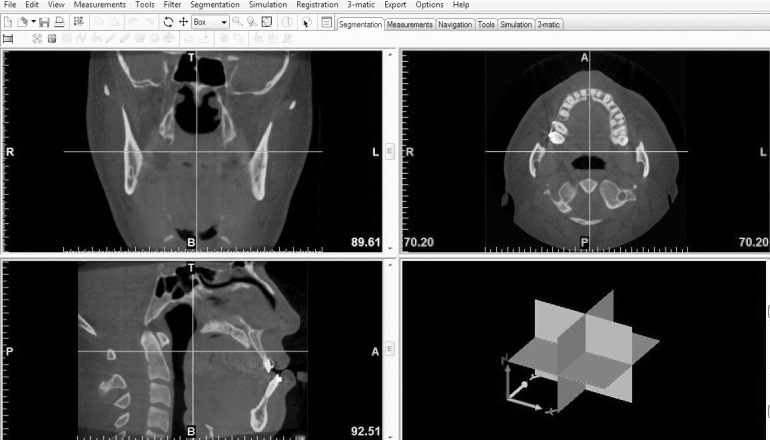
Image before thresholding.
Figure 2.
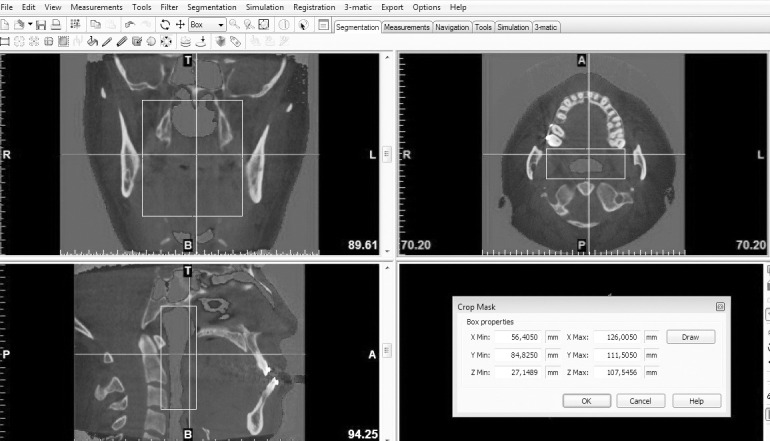
The pharyngeal airway, cropped. The defined borders are clearly seen in the sagittal view.
Figure 3.
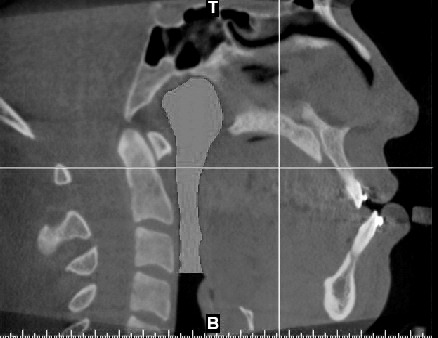
Sagittal view. The connections of the pharyngeal airway with the external air are removed.
The structures that failed to connect with the outer airway were separated, and the three-dimensional image of the pharyngeal airway was constructed and calculated. The three-dimensional image of the pharyngeal airway was divided into upper and lower parts by a plane drawn from PNS to the most anterior and inferior point of the first vertebrae (Figure 4). The volumes of upper, lower, and total pharyngeal airway were calculated (Figure 5). In addition, the smallest cross-sectional airway area was measured in each CT.
Figure 4.
Sagittal view. The plane that divides the pharyngeal airway into upper and lower compartments is visible.
Figure 5.
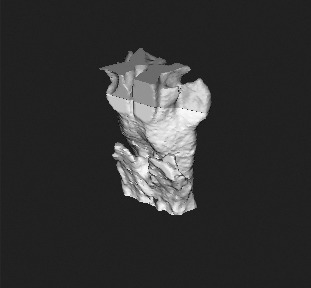
Three-dimensional model of the pharyngeal airway (lateral view).
For the assessment of maxillary sinus volumes the coronal image was selected. The same thresholding limits were applied as in the pharyngeal airway assessment, and the sinuses were cropped in the slice in which their widest size was apparent (Figure 6). Cropping was also done in axial and sagittal views. Any connection with the outer air was eliminated; three-dimensional images of the left and right sinus were constructed, and their volumes were calculated (Figures 7 and 8).
Figure 6.
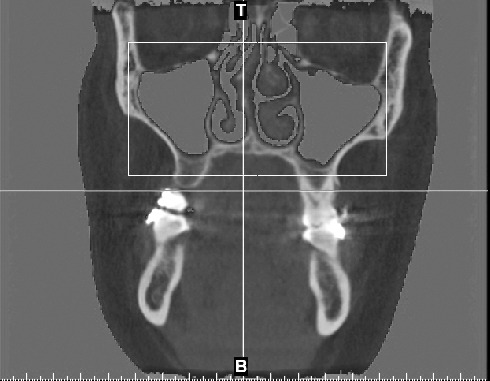
Maxillary sinuses, cropped.
Figure 7.
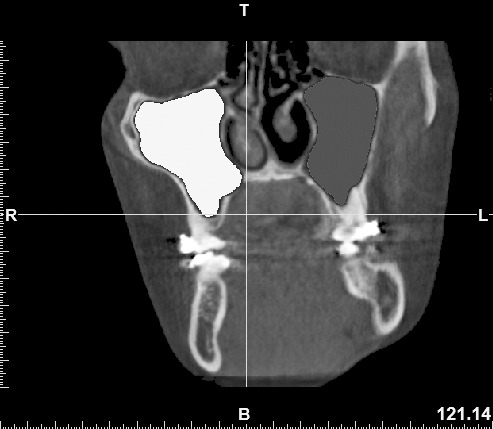
Maxillary sinuses, coronal view. The isolated maxillary sinuses are clearly visible.
Figure 8.
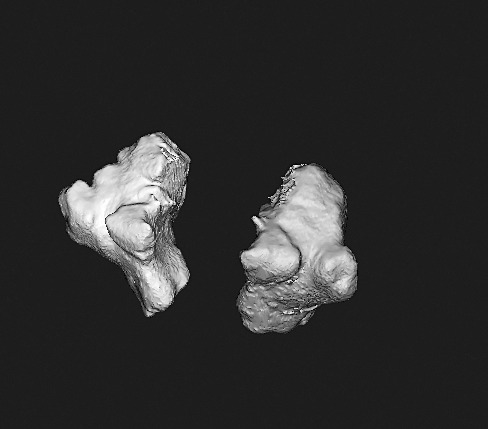
Three-dimensional image of the maxillary sinuses.
In cases in which polyps were observed inside the cavities of the maxillary sinuses, these polyps were included in the mask of the isolated sinus, since they were occupying space that should normally be occupied by air.
Means and standard deviations for all parameters were calculated. The initial values of all the parameters related to pharyngeal and sinus dimensions were evaluated for gender differences using the Mann-Whitney U-test. There was no statistically significant difference between the two genders except for the parameters of LPA and TPA. For these parameters, preoperative and postoperative comparisons were made separately in males and females using the Wilcoxon test. For the rest of the parameters, all of the comparisons were made in the whole sample using a paired-samples t-test. The amounts of mandibular setback in female and male patients were compared with the Mann-Whitney U-test as well. Pearson's correlation was used to determine if a relationship existed between the amount of the surgical movement and the volumetric changes observed between the time points. For reliability testing, 10 patients were randomly selected and all of the parameters were remeasured. The intraclass correlation coefficient was used in order to determine the reliability of the measurements.
RESULTS
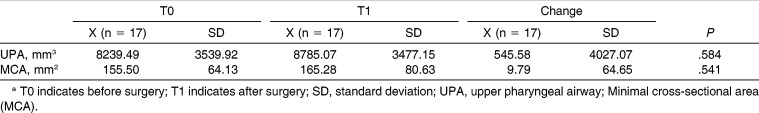
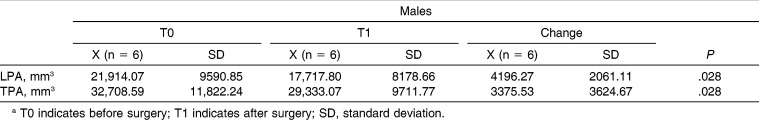
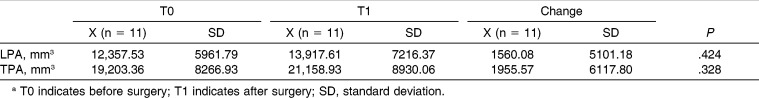
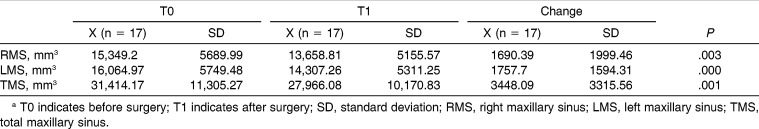
There was a high agreement between the duplicate measurements conducted by the same examiner. The intraclass correlation coefficient of all the measurements for 10 randomly selected cases showed a high rate of consonance between measurements. The upper pharyngeal airway volume increased by 545.58 ± 4027.07 mm3, on average, and this increase was not statistically significant (P = .584) (Table 2). Furthermore, the minimal cross-sectional area of the pharyngeal airway presented an average increase of 9.79 ± 64.65 mm2, which was not statistically significant (P = .541). There is a significant decrease of 4196.27 ± 2061.11 mm3 in the lower pharyngeal airway in males (P = .028), while the total pharyngeal airway reduced by 3375.53 ± 3624.67 mm3 postsurgically (Table 3). This decrease was statistically significant (P = .028). In females, there was an increase in lower pharyngeal airway volume of 1560.08 ± 5101.18 mm3, which was not significant (P = .424), while the total pharyngeal airway volume presented an increase of 1955.57 ± 6117.80 mm3, on average, which was not statistically significant (P = .328) (Table 4). The data show that the right maxillary sinus volume was reduced by 1690.39 ± 1999.46 mm3 and that this change was statistically significant (P = .003). There was a statistically significant (P = .000) average decrease of 1757.7 ± 1594.31 mm3 in the left maxillary sinus volume. The volume of the total maxillary sinuses reduced significantly, by 3448.09 ± 3315.56 mm3 (P = .001) (Table 5).
Table 2.
Changes of the Pharyngeal Airway After the Surgerya
Table 3.
Lower Pharyngeal Airway (LPA) and Total Pharyngeal Airway (TPA) Changes in Malesa
Table 4.
Lower Pharyngeal Airway (LPA) and Total Pharyngeal Airway (TPA) Changes in Femalesa
Table 5.
Volumetric Changes of Maxillary Sinusesa
There was no significant correlation between the volumetric change of the total pharyngeal airway and the maxillary impaction, maxillary advancement, and mandibular setback amounts (r = 0.232, P = 0.580; r = 0.234, P = .348; and r = 0.288, P = .262, respectively). No significant correlation was found between the volumetric change of the upper pharyngeal airway and the amount of maxillary impaction and maxillary advancement (r = 0.166, P = .695 and r = 0.106, P = .686, respectively), either. The lower pharyngeal airway change showed no correlation with maxillary impaction, maxillary advancement, and mandibular setback amounts (r = 0.222, P = .597; r = 0.244, P = .345; and r = 0.307, P = .231, respectively), and the total volumetric change of the maxillary sinuses also showed no correlation with the amounts of maxillary impaction and maxillary advancement (r = 0.253, P = .545 and r = 0.217, P = .403, respectively).
DISCUSSION
The positional changes resulting from the movements of the jaws have been shown to be responsible for airway narrowing6 and to be associated with sleep-related breathing disorders, such as OSA.2 Conversely, it has been reported that there is no decrease of the upper airway with bimaxillary correction of Class III malocclusion3 and that pharyngeal airway volumes are increased as a result of the surgery.7
In the present study the average interval between the surgery and the second CBCT scan was 3.90 ± 0.87 months. This interval was chosen in order to avoid the postsurgical tissue swelling as well as inflammation of the tongue, uvula, and hypopharynx that may occur immediately after surgery, thereby leading to biased results. Additionally, in order to be able to assess the immediate changes induced by surgery, before any significant relapse or remodeling could occur, no scan was taken after a period of 6 months after surgery. Gu et al.8 stated that the maximum forward relapse of the pogonion (Pg) occurred mainly within 6 months after the surgery. A possible limitation in our study may be the fact that there is no evaluation in the long term in order to assess the stability of the postoperative results. However, current regulations of the local ethical committee do not encourage repeated scanning of patients for research purposes.
Most of the previous studies dealing with the influence of orthognathic surgery on pharyngeal airway and maxillary sinus volume have been conducted on lateral cephalometric film,3,9 which does not give an accurate indication of the complexity of these structures or of their true size.
We chose to conduct our study using CBCT because of its advantages over the Multi-sllice-CT scans (MS-CT), the most important being their lower radiation dose, reduced artifact, and lower costs. With CBCT, it was possible to perform the scanning with the patients sitting upright, which is a benefit, since the supine position used in MS-CT imaging causes significant morphologic changes of the airway because gravity affects the soft tissues surrounding the oropharyngeal cavity.
After all of the data were concentrated, MIMICS 14.0 software was incorporated in order to process the CBCT images and to calculate the volume of the pharyngeal airway and maxillary sinuses. The pharyngeal airway was defined according to the specific borders described previously, which were formed after evaluation and modification of the borders defined in other similar studies.10,11 In the present study the pharyngeal airway was divided into upper and lower parts according to the method described by Grauer et al.11
It has been shown that anatomically the sizes of the pharyngeal airway and maxillary sinus may differ between males and females.11 For this reason, in the present study, the initial values of the variables were compared between males and females. A statistically significant difference was found only for the parameters of lower and total pharyngeal airway. For those two variables we performed separate statistics, dividing the sample according to the gender.
In an effort to find an explanation for this difference in LPA and TPA volume changes between males and females, the mean setback amounts of males and females were compared to see if the males had a significantly greater amount of setback than females. However, there was no significant difference between the setback amounts for males and females.
In a CT-based study, Degerliyurt et al.12 found that after bimaxillary surgery, only midsagittal anteroposterior dimensions were significantly decreased at the level of the soft palate and the base of the tongue for males and females. In our study, however, we observed a significant decrease only in the male group for the lower and total pharyngeal airway volumes.
Recently, Hong et al.13 conducted a study that consisted of preoperative and postoperative CBCT scans of 21 skeletal Class III patients who were assigned to either mandibular setback surgery or bimaxillary surgery. They reported that the pharyngeal airway showed significant narrowing after mandibular setback and bimaxillary surgery. However, the amount of narrowing was smaller in patients undergoing bimaxillary surgery than in patients undergoing mandibular setback surgery. They also found that the amount of change in the anteroposterior dimension and cross-sectional area on the posterior nasal spine plane and the length of the pharyngeal airway presented significant differences between the two groups.
The study of Hong et al.13 includes a larger group divided into two subgroups depending on the type of surgery. In our study, however, all of the patients in the group underwent bimaxillary surgery. The results of the study of Hong et al.13 are in agreement with the results of the male subgroup in the present study.
As far as the maxillary sinuses are concerned, there are very few studies related to their size in general, and to our knowledge, no CBCT study has been conducted concerning their volume changes after maxillary osteotomies.
Halawa5 studied the maxillary sinus size before and after Le Fort I impaction surgery on the basis of lateral cephalometric radiographs of 36 patients obtained before and after the surgery. Additionally, for 12 patients, lateral cephalometric films were also taken, on average 15 months after surgery. They concluded that maxillary sinus area decreased significantly by 1.69 cm2 ± 1.07 cm2 after surgery, followed by an increase of 0.52 cm2 ± 0.53 cm2 during the average postsurgical period of 15 months. The use of lateral cephalometric radiographs in Halawa's study results in a limitation for that investigation, since three-dimensional structures were being assessed by a two-dimensional method. Additionally, in a lateral cephalometric radiograph the left and right sinuses are superimposed, making the evaluation of the sinus dimensions more inaccurate. According to our CBCT-based study, there was a significant decrease in the total volume of the maxillary sinus by 3448.09 mm3 ± 3315.56 mm3, as observed in the whole sample. It would be recommended, however, that researchers further investigate if in our sample this reduction in the maxillary sinus volume was permanent or if there was an increase in the long term, as reported by Halawa.5 Another interesting topic for research could be the clinical implications of this reduction in maxillary sinus size, if there are any.
Finally, the results of the present pilot study indicated that there was no correlation between the amount of surgical movement and the volumetric changes observed. Conversely, Tselnik and Pogrel14 found a strong correlation between the amount of mandibular setback and the decrease in PAS area. Furthermore, Jakobsone et al.15 suggested that clinically significant maxillary advancement of ≥2 mm causes a significant increase in the airway dimensions at the nasopharyngeal level.
It is evident that a prospective study conducted on a larger and more uniform sample would provide more definitive answers to the questions addressed in this study.
CONCLUSIONS
There is no significant change in the volume of pharyngeal airway after bimaxillary surgery for correction of Class III skeletal relationship, except for the lower and total pharyngeal airway volumes in males.
However, there was a significant decrease observed in the total volume of the maxillary sinuses.
There was also no correlation between the amount of surgical movement and the change in the volume of the pharyngeal airway or the volume of the maxillary sinuses.
REFERENCES
- 1.Muto T, Yamazaki A, Takeda S, Sato Y. Effect of bilateral sagittal split ramus osteotomy setback on the soft palate and pharyngeal airway space. Int J Oral Maxillofac Surg. 2008;37:419–423. doi: 10.1016/j.ijom.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 2.Riley RW, Powell NB, Guilleminault C, Ware W. Obstructive sleep apnea syndrome following surgery for mandibular prognathism. J Oral Maxillofac Surg. 1987;45:450–452. doi: 10.1016/0278-2391(87)90016-4. [DOI] [PubMed] [Google Scholar]
- 3.Chen F, Terada K, Hua Y, Saito I. Effects of bimaxillary surgery and mandibular setback surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. Am J Orthod Dentofacial Orthop. 2007;131:372–377. doi: 10.1016/j.ajodo.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 4.Degerliyurt K, Ueki K, Hashiba Y, Marukawa K, Nakagawa K, Yamamoto E. A comparative CT evaluation of pharyngeal airway changes in Class III patients receiving bimaxillary surgery or mandibular setback surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:495–502. doi: 10.1016/j.tripleo.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Halawa AE. Radiologic Evaluation of the Maxillary Sinus Size Before and After Le Fort I Impaction Surgery [doctorate thesis] 2005. Marmara University, Istanbul, Turkey. [Google Scholar]
- 6.Katakura N, Umino M, Kubota Y. Morphologic airway changes after mandibular setback osteotomy for prognathism with and without cleft palate. Anesth Pain Control Dent. 1993;2:22–26. [PubMed] [Google Scholar]
- 7.Pereira-Filho VA, Castro-Silva LM, de Moraes M, Gabrielli MF, Campos JA, Juergens P. Cephalometric evaluation of pharyngeal airway space changes in Class III patients undergoing orthognathic surgery. J Oral Maxillofac Surg. 2011;69:409–415. doi: 10.1016/j.joms.2011.02.132. [DOI] [PubMed] [Google Scholar]
- 8.Gu G, Gu G, Nagata J, et al. Hyoid position, pharyngeal airway and head posture in relation to relapse after the mandibular setback in skeletal Class III. Clin Orthod. 2000;3:67–77. [PubMed] [Google Scholar]
- 9.Chen F, Terada K, Hanada K, Saito I. Predicting the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2005;63:1509–1514. doi: 10.1016/j.joms.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 10.Burgess BL. Pharyngeal Airway Volume Following Maxillomandibular Advancement Surgery Utilizing Cone Beam Computed Tomography [master's thesis] 2008. Saint Louis, MO: University of Saint Louis; [Google Scholar]
- 11.Grauer D, Cevidanes LS, Styner MA, Ackerman JL, Proffit WR. Pharyngeal airway volume and shape from cone-beam computed tomography: relationship to facial morphology. Am J Orthod Dentofacial Orthop. 2009;136:805–814. doi: 10.1016/j.ajodo.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Degerliyurt K, Ueki K, Hashiba Y, et al. The effect of mandibular setback or two-jaws surgery on pharyngeal airway among different genders. Int J Oral Maxillofac Surg. 2009;6:647–652. doi: 10.1016/j.ijom.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 13.Hong J, Park Y, Kim Y, Hong S, Oh K. Three-dimensional changes in pharyngeal airway in skeletal Class III patients undergoing orthognathic surgery. J Oral Maxillofac Surg. 2011;69:401–408. doi: 10.1016/j.joms.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 14.Tselnik M, Pogrel MA. Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2000;58:282–285. doi: 10.1016/s0278-2391(00)90053-3. [DOI] [PubMed] [Google Scholar]
- 15.Jakobsone G, Stenvik A, Espeland L. The effect of maxillary advancement and impaction on the upper airway after bimaxillary surgery to correct Class III malocclusion. Am J Orthod Dentofacial Orthop. 2011;139:369–376. doi: 10.1016/j.ajodo.2010.07.022. [DOI] [PubMed] [Google Scholar]