Abstract
Objective:
To assess the three-dimensional (3D) skeletal response to a standardized 5 mm of rapid maxillary expansion (RME) in growing children (6–15 years) with maxillary width deficiency and crowding.
Materials and Methods:
A bonded appliance was used prior to the eruption of the maxillary first premolars (Mx4s), and a banded appliance was used thereafter. A consecutive sample of 89 patients (29 boys and 60 girls) from a large pediatric dentistry and orthodontics practice was divided into four groups: 1) 6–8 years old (n = 26), 2) 9–11 years old with unerupted Mx4s (n = 21), 3) 9–11 years with erupted Mx4s (n = 23), and 4) 12–15 years (n = 19). For all patients, the 3D evaluation of dental and skeletal effects was performed with cone-beam computed tomography (CBCT).
Results:
For both appliances in all patients, CBCT confirmed a triangular pattern of expansion in both the frontal and sagittal planes. Overall, both appliances produced significant maxillary expansion (>80% of the 5-mm activation), but older children showed a progressively more dental (less skeletal) response. Comparison of the two types of expanders in the crossover sample, children aged 9–11 years, showed that the bonded RME produced the most efficient skeletal expansion in the preadolescent sample. Increased maxillary width at the level of the zygomaticomaxillary suture was the best indicator for development of maxillary arch circumference.
Conclusion:
Development-dependent appliances (bonded RPE before Mx4s erupt, and a banded device thereafter) provided optimal RME treatment for all children from age 6–15 years.
Keywords: CBCT, RME, Bonded expander, Banded expander, Maxillary deficiency, Crowding
INTRODUCTION
Since rapid maxillary expansion (RME) was first introduced by Angell in 1860,1 the effects of RME on both skeletal and dental structures have been widely investigated.2–9 RME is usually used to correct cross-bite and to eliminate crowding by increasing the maxillary arch circumference, and it may improve nasal respiration.2,10–12 However, problems such as dental and/or alveolar tipping, periodontal (gingival) recession, dental extrusion, and anterior open-bite are common concerns.13–15
Traditionally, the effects of RME are evaluated using casts and/or two-dimensional (2D) radiographs, but reproducibility of 2D radiographs is problematic, and overlapping images are difficult to assess.16–18 Cone-beam computed tomography (CBCT) provides more accurate and reproducible imaging19,20 for assessing all craniofacial skeletal structures, including the circummaxillary sutures.21–23
Common RME appliances are the bonded (McNamara type)24–27 and the tooth banded (Hyrax type).28 Analysis of both casts and cephalometrics have been used to compare these two appliances.14,29,30 However, no studies have controlled for developmental timing of treatment to select the optimal appliance for each patient. Reportedly, RME in younger patients results in a greater orthopedic effect with less dental tipping,31,32 but there has been no direct comparison to older patients treated with the same standardized activation. There are no studies of consecutive patients sampled throughout the usual period of conservative treatment, which is from the early transitional to the early permanent dentition (age 6–15 years).
There are many 2D reports indicating a nonparallel, triangular expansion pattern: greater expansion in the anterior rather than the posterior dimension.19,20,33 However, there have been only a few studies that have focused on the effects of RME on craniofacial sutures by evaluating the frontal (coronal) dimension.34–37
Overall, the present literature review suggests the bonded appliance is the optimal appliance before the maxillary first premolars (Mx4s) erupt, and the banded expander is more desirable thereafter. The aim of this study is to quantitatively evaluate the efficiency of a standardized activation (5 mm) in a consecutive series of children (6–15 years) treated with a development-appropriate appliance.
MATERIALS AND METHODS
The consecutive sample was retrospectively drawn from all children age 6–15 years presenting for treatment at a large private practice providing both pediatric dentistry and orthodontics services. The study was approved by the institutional review board of Tohoku University #12–21. In the practice studied, patients 6–15 years of age with crowding (≤6 mm), associated with moderate maxillary constriction, are usually treated with 5 mm of rapid palatal expander (RPE). Inclusion criteria were: mixed or early permanent dentition, symmetric sagittal position of maxillary first molars, relatively modest constricted maxilla, insufficient maxillary arch circumference, and with or without cross-bite. Exclusion criteria were age >15 years, periodontal disease, previous orthodontic treatment, and congenital malformations. For all patients sampled, the average ANB was 4.5° ± 1.9°, and the average FMA was 29.7° ± 4.2°. Patients satisfying the inclusion and exclusion criteria were assigned to one of four RME treatment groups according to age and Mx4s development. To manage crowding without extractions, a standardized 5 mm of RPE was delivered with the development-appropriate (optimal) appliance. Thus, “optimal RME” was defined as a bonded expander prior to the eruption of the Mx4s and a banded one thereafter. The bonded appliance was a McNamara-type RME, and the banded appliance was a Hyrax-type RME (Figure 1).
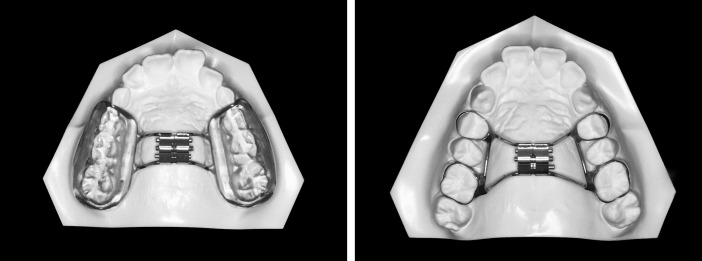
Figure 1.
Left: McNamara-type (bonded) appliance; right: Hyrax (banded) appliance.
A consecutive sample of 89 patients (29 boys and 60 girls with a mean age of 10 years 2 months ± 2 years 0 months) was divided into four groups: 1) 6–8 years (n = 26), 2) 9–11 years with insufficiently erupted Mx4s (n = 21), 3) 9–11 years with sufficiently erupted Mx4s (n = 23), and 4) 12–15 years (n = 19).
The expansion screw was turned .025 mm twice a day for 10 days or until 5 mm of activation was achieved. The postactivation retention time was 5 to 6 months; bone formation in the expanded midpalatal suture was confirmed with occlusal radiographs. A bi-helix appliance was used for all patients to expand the lower dental arch to maintain coordination of the arches.
The Alphard-3030 (Asahi Roentgen Ind Co Ltd, Kyoto, Japan) was used to obtain CBCT images before (T1) and after the retention period when the expander was removed (T2). The CT scans were performed at 80 Kv and 2mA, with a scan time of 17 seconds and voxel dimensions of 0.39 × 0.39 × 0.39 mm. The data for each patient were evaluated with stereotaxic three-dimensional (3D)-CT software produced by Imagnosis (Orlando, Fla). Both right and left inferior borders of the infraorbital foramina and the midpoint between right and left superior borders of the external auditory canals were used as reference points (Figure 2A). The plane constructed by these three reference points was used as a reference plane (Figure 2B). The coronal plane was through the cusp tip of the most anterior maxillary first molar, perpendicular to the FH and midsagittal planes. All measurements were performed by a single examiner (Dr Kanomi). As shown in Figure 3, distances were measured between the following bilateral structures:
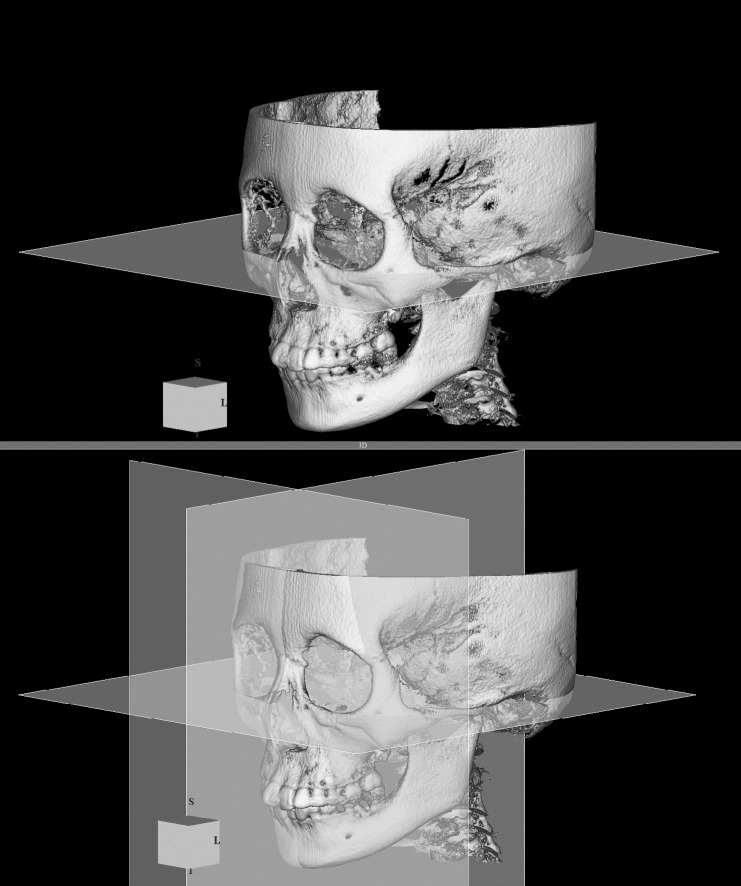
Figure 2.
CBCT image shows the three reference planes: axial, sagittal, and frontal (coronal), which correspond to the reference box that defines planes relative to superior (S), inferior (I), and lateral (L).
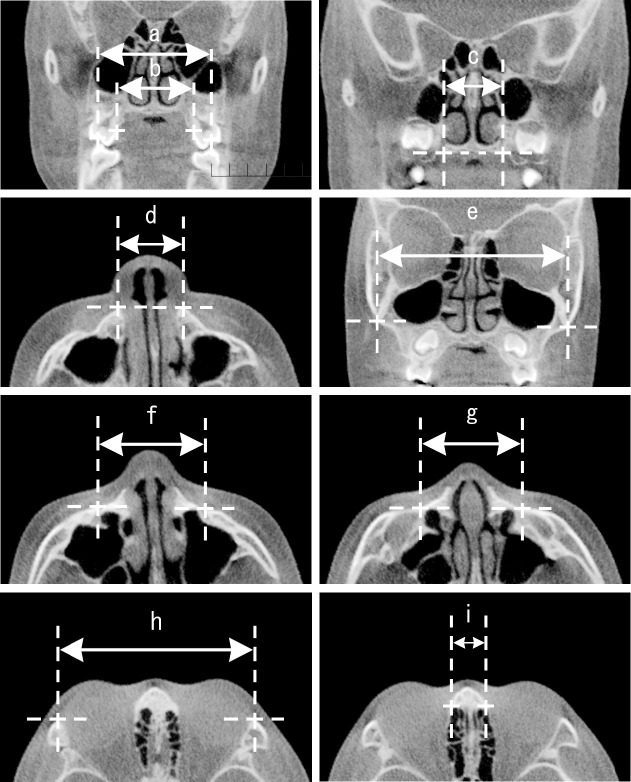
Figure 3.
Distance between bilateral landmarks: (a) maxillary first molar central pits, (b) palatal alveolar crests, (c) greater palatine foramena, (d) nasal width, (e) inferior margin zygomaticomaxillary suture, (f) infraorbital foramena, (g) superior margin zygomaticomaxillary suture, (h) the anterior border frontozygomatic suture, (i) and the lateral border frontomaxillary suture.
Upper maxillary first molar: central fossae
Palatal alveolar bone crests: adjacent to the maxillary first molar
Greater palatine foramen: distance between the foramina on a coronal slice
Nasal width: maximum dimension of the piriform aperture on the coronal image
Inferior margin of the zygomaticomaxillary suture: on the coronal image
Infraorbital foramens: on the axial image
Superior margin of the zygomaticomaxillary suture: on the axial image
Anterior border of the frontozygomatic suture: on the axial image
Lateral border of the frontomaxillary suture: on the axial image
Intraexaminer reliability was within +5% for all measurements as determined by data replications at least 2 weeks apart. Descriptive statistics including means and standard deviations were calculated for measurements for the changes from T1 to T2. Differences between variables in T1 and T2, as well as within groups, were assessed with the one-sample t-test. Student's and Welch's t-tests were used to compare between the different appliances. The level of significance was P < .05, and the power analysis exceeded 0.85. All statistical analysis was performed using the computer software Microsoft Excel 2010 (Microsoft, Redmond, Wash).
RESULTS
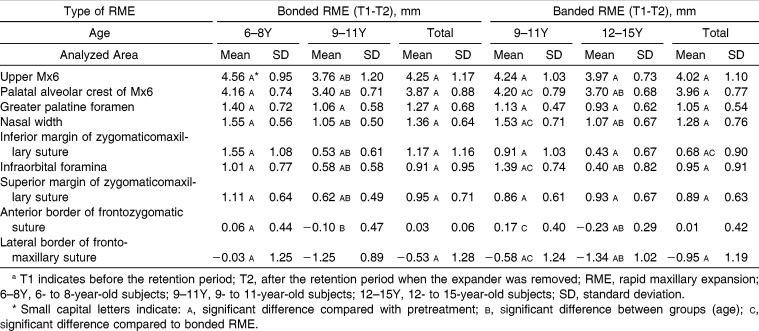
Overall, the results were consistent with 1) a triangular pattern of maxillary expansion in the frontal and sagittal planes, 2) an inverse relationship between age and the amount of skeletal expansion achieved, and 3) the banded appliance producing more efficient expansion in the 9- to 11-year-old patients. Both RME appliances produced statistically significant (P < .05) increases in all the landmarks measured, except for the anterior border of the frontozygomatic suture and the lateral border of the frontomaxillary suture. For patients treated with a bonded RME (6–8 vs 9–11 years), the younger patients experienced more expansion of all landmarks, except for the greater palatine foramen and the lateral border of the frontomaxillary suture. For patients treated with the bonded RME (9–11 vs 12–15 years), the older patients exhibited less expansion of all landmarks except the upper (Mx)6, greater palatine foramen, and both margins of the zygomaticomaxillary suture. Comparison of the bonded (McNamara-type) and banded (Hyrax-type) appliances in 9- to 11-year-old children demonstrated that the banded appliance produced significantly more expansion (greater interlandmark dimension) at the palatal alveolar crest of Mx6, nasal width, infraorbital foramina, and both borders of the frontomaxillary suture (Table 1).
Table 1.
Comparison Between T1 and T2 Relative to Age and Appliancea
DISCUSSION
All measurements were made after 5–6 months of postactivation retention to allow new bone to form and consolidate in the midpalatal suture.5,19 For the standardized 5-mm activation, the mean expansion between the Mx6s was approximately 4.3 mm (86%) for the bonded (McNamara-type) RME patients compared to 4.0 mm (80%) in the banded (Hyrax-type) groups (Table 1). This relatively efficient RME may reflect the concurrent expansion of the lower arch.38 The positioning of the upper molar cusp in the lower molar fossa may have minimized relapse of maxillary expansion.
This amount of expansion (Table 1) is similar to previous CBCT reports of a 3.6-mm increase36 and 4.8 mm37 of intermolar width. The effect of RME is not limited to the maxillary alveolar process but is also seen on adjacent structures, including the cranial and circummaxillary sutures.39 In the present study, RME had significant effects at the level of the zygomaticomaxillary suture and nasal bone, but not in the frontozygomatic and frontomaxillary sutures (triangular expansion pattern). Finite element analysis of the stress distribution with RME shows high tensile stress at the zygomaticomaxillary suture, except along its anteromedial surface.40 For this reason, the zygomaticomaxillary buttress is a primary osteotomy site in surgical expansion.41,42 Bell and Epker43 confirmed this surgical strategy based on skeletal resistance to expansion within the zygomaticomaxillary sutures. In the present study, significant expansion at the zygomaticomaxillary suture was seen in all groups, which may be the best indication for effective skeletal expansion to increase the circumferential arch length of the maxillary arch.
Overall, the expansion data (Table 1) are consistent with the well-known triangular pattern.2,16 The maxillary bones were displaced laterally, with the fulcrum located close to the area of the frontomaxillary suture, which tends to close slightly during maxillary expansion.2,34 Tipping movement is more likely to occur with increased resistance to expansion at the zygomatic buttress. This pattern of variable resistance results in a triangularly shaped expansion, especially in older patients. The present data (Table 1) are consistent with more parallel expansion in patients <8 years of age for bonded-type expanders that incorporate acrylic over the occlusal surface. These appliances are designed to provide more uniform expansion of the palate and to inhibit alveolar tipping.5,44
Compared to the slight negative expansion (constriction) of the frontomaxillary suture, noted for all groups in the present study (Table 1), Ghoneima et al.39 reported a small but significant increase (0.1 mm) in the width at the frontomaxillary suture with a bonded RME in a group of children with mean age of 12 years (range 8–15 years). However, the magnitude of the difference between the studies is small (∼1 mm), so it is relatively insignificant compared to the overall triangular pattern of expansion noted in both studies. Also, finite element analysis showed significantly lower stress in the frontal bone compared to other craniofacial regions.45 It is clear that the frontomaxillary suture expands little if any with RME, which is consistent with the triangular pattern of expansion with both banded and bonded RME appliances.
RME is known to affect nasal aperture width,2,20 which is consistent with finite element modeling.40 Previous CBCT studies reported that RME produced a 1.6-mm increase in the width of the nasal floor; this is comparable to 1.3 - 1.4 mm of expansion for bonded and banded RME, respectively (Table 1). In 9- to 11-year-old patients, the banded appliance produced ∼0.5 mm more nasal floor expansion than the bonded appliance.
Sari et al.46 found no significant difference in the amount of expansion between the mixed and permanent dentition using a bonded RME device. However, that data is difficult to compare to the current results because of the variable age of the patients and lack of a standardized expansion protocol. The present study demonstrated that the bonded appliance is superior for younger children (<9 years) and that the banded RME is more effective for older children, once the Mx4s have erupted. In the Hyrax group (Table 1), more expansion was seen in the 9- to 11-year-old group (4.2 mm) compared to that in the 12- to 15-year-old (3.7 mm) group at the palatal alveolar crest, nasal width, and infraorbital foramina. The only direct comparison between the appliances was for 9- to 11-year-old patients. The banded appliance consistently produced ∼0.5 mm more dental and skeletal expansion. These small changes were significant but may not be clinically relevant. Overall, the efficiency of expansion was inversely related to age, as previously reported.31
CONCLUSIONS
RME is an effective treatment option for all growing patients, but expansion efficiency (skeletal effect) is inversely related to age.
Zygomaticomaxillary sutural expansion appears to be the best indicator for development of maxillary arch circumference.
CBCT is an important 3D diagnostic tool for managing crowding due to maxillary deficiencies.
REFERENCES
- 1.Angell EH. Treatment of irregularities of the permanent or adult tooth. Dent Cosmos. 1860;1:540–544. [Google Scholar]
- 2.Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the mid palatal suture. Angle Orthod. 1961;31:73–89. [Google Scholar]
- 3.Haas AJ. The treatment of maxillary deficiency by opening the mid-palatal suture. Angle Orthod. 1965;65:200–217. doi: 10.1043/0003-3219(1965)035<0200:TTOMDB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Haas AJ. Palatal expansion: just the beginning of dentofacial orthopedics. Am J Orthod. 1970;57:219–255. doi: 10.1016/0002-9416(70)90241-1. [DOI] [PubMed] [Google Scholar]
- 5.Haas AJ. Long-term posttreatment evaluation of rapid palatal expansion. Angle Orthod. 1980;50:189–217. doi: 10.1043/0003-3219(1980)050<0189:LPEORP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Isaacson RJ, Wood JL, Ingram AH. Forces produced by rapid maxillary expansion. Part I. Design of the force measuring system. Angle Orthod. 1964;34:256–260. [Google Scholar]
- 7.Isaacson RJ, Ingram AH. Forces produced by rapid maxillary expansion. Part II. Forces present during treatment. Angle Orthod. 1964;34:261–269. doi: 10.1043/0003-3219(1965)035<0178:FPBRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Starnbach H, Bayne D, Cleall J, Subtelny JD. Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod. 1966;36:152–164. doi: 10.1043/0003-3219(1966)036<0152:FADCRF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Chung CH, Font B. Skeletal and dental changes in the sagittal, vertical, and transverse dimensions after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2004;126:569–575. doi: 10.1016/j.ajodo.2003.10.035. [DOI] [PubMed] [Google Scholar]
- 10.Hershey HG, Stewart BL, Warren DW. Changes in nasal airway resistance associated with rapid maxillary expansion. Am J Orthod. 1976;69:274–284. doi: 10.1016/0002-9416(76)90076-2. [DOI] [PubMed] [Google Scholar]
- 11.Hartgerink DV, Vig PS, Abbott DW. The effect of rapid maxillary expansion on nasal airway resistance. Am J Orthod Dentofacial Orthop. 1987;92:381–389. doi: 10.1016/0889-5406(87)90258-7. [DOI] [PubMed] [Google Scholar]
- 12.Warren DW, Hairfield WM, Seaton DL, Hinton VA. The relationship between nasal airway cross-sectional area and nasal resistance. Am J Orthod Dentofacial Orthop. 1987;92:390–395. doi: 10.1016/0889-5406(87)90259-9. [DOI] [PubMed] [Google Scholar]
- 13.Rungcharassaeng K, Caruso JM, Kan JY, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428.e1–e8. doi: 10.1016/j.ajodo.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 14.Asanza S, Cisneros GJ, Nieberg LG. Comparison of Hyrax and bonded expansion appliances. Angle Orthod. 1997;67:15–22. doi: 10.1043/0003-3219(1997)067<0015:COHABE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Sun Z, Smith T, Kortam S, Kim DG, Tee BC, Fields H. Effect of bone thickness on alveolar bone-height measurements from cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2011;139:e117–e127. doi: 10.1016/j.ajodo.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 16.da Silva Filho OG, Montes LA, Torelly LF. Rapid maxillary expansion in the deciduous and mixed dentition evaluated through posteroanterior cephalometric analysis. Am J Orthod Dentofacial Orthop. 1995;107:268–275. doi: 10.1016/s0889-5406(95)70142-7. [DOI] [PubMed] [Google Scholar]
- 17.Braun S, Bottrel JA, Lee KG, Lunazzi JJ, Legan HL. The biomechanics of rapid maxillary sutural expansion. Am J Orthod Dentofacial Orthop. 2000;118:257–261. doi: 10.1067/mod.2000.108254. [DOI] [PubMed] [Google Scholar]
- 18.Cross DL, McDonald JP. Effect of rapid maxillary expansion on skeletal, dental, and nasal structures: a postero-anterior cephalometric study. Eur J Orthod. 2000;22:519–28. doi: 10.1093/ejo/22.5.519. [DOI] [PubMed] [Google Scholar]
- 19.Lione R, Ballanti F, Franchi L, Baccetti T, Cozza P. Treatment and posttreatment skeletal effects of rapid maxillary expansion studied with low-dose computed tomography in growing subjects. Am J Orthod Dentofacial Orthop. 2008;134:389–392. doi: 10.1016/j.ajodo.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 20.Garrett BJ, Caruso JM, Rungcharassaeng K, Farrage JR, Kim JS, Taylor GD. Skeletal effects to the maxilla after rapid maxillary expansion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2008;134:8–9. doi: 10.1016/j.ajodo.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 21.Davis WM, Kronman JH. Anatomical changes induced by splitting of the midpalatal suture. Angle Orthod. 1969;39:126–132. doi: 10.1043/0003-3219(1969)039<0126:ACIBSO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Timms DJ. A study of basal movement with rapid maxillary expansion. Am J Orthod. 1980;77:500–507. doi: 10.1016/0002-9416(80)90129-3. [DOI] [PubMed] [Google Scholar]
- 23.Wagemans PA, van de Velde JP, Kuijpers-Jagtman AM. Sutures and forces: a review. Am J Orthod Dentofacial Orthop. 1988;94:129–141. doi: 10.1016/0889-5406(88)90361-7. [DOI] [PubMed] [Google Scholar]
- 24.Sarver DM, Johnston MW. Skeletal changes in vertical and anterior displacement of the maxilla with bonded rapid palatal expansion appliances. Am J Orthod Dentofacial Orthop. 1989;95:462–466. doi: 10.1016/0889-5406(89)90409-5. [DOI] [PubMed] [Google Scholar]
- 25.Memikoglu TU, Işeri H. Effects of a bonded rapid maxillary expansion appliance during orthodontic treatment. Angle Orthod. 1999;69:251–256. doi: 10.1043/0003-3219(1999)069<0251:EOABRM>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.McNamara JA, Jr, Sigler LM, Franchi L, Guest SS, Baccetti T. Changes in occlusal relationships in mixed dentition patients treated with rapid maxillary expansion. A prospective clinical study. Angle Orthod. 2010;80:230–238. doi: 10.2319/040309-192.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guest SS, McNamara JA, Jr, Baccetti T, Franchi L. Improving Class II malocclusion as a side-effect of rapid maxillary expansion: a prospective clinical study. Am J Orthod Dentofacial Orthop. 2010;138:582–591. doi: 10.1016/j.ajodo.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 28.Garib DG, Henriques JF, Janson G, Freitas MR, Coelho RA. Rapid maxillary expansion—tooth tissue-borne versus tooth-borne expanders: a computed tomography evaluation of dentoskeletal effects. Angle Orthod. 2005;75:548–557. doi: 10.1043/0003-3219(2005)75[548:RMETVT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Reed N, Ghosh J, Nanda RS. Comparison of treatment outcomes with banded and bonded RPE appliances. Am J Orthod Dentofacial Orthop. 1999;116:31–40. doi: 10.1016/s0889-5406(99)70300-8. [DOI] [PubMed] [Google Scholar]
- 30.Kiliç N, Kiki A, Oktay H. A comparison of dentoalveolar inclination treated by two palatal expanders. Eur J Orthod. 2008;30:67–72. doi: 10.1093/ejo/cjm099. [DOI] [PubMed] [Google Scholar]
- 31.Baccetti T, Franchi L, Cameron CG, McNamara JA., Jr Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71:343–350. doi: 10.1043/0003-3219(2001)071<0343:TTFRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Geran RG, McNamara JA, Jr, Baccetti T, Franchi L, Shapiro LM. A prospective long-term study on the effects of rapid maxillary expansion in the early mixed dentition. Am J Orthod Dentofacial Orthop. 2006;129:631–640. doi: 10.1016/j.ajodo.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 33.Bishara SE, Staley RN. Maxillary expansion: clinical implications. Am J Orthod Dentofacial Orthop. 1987;91:3–14. doi: 10.1016/0889-5406(87)90202-2. [DOI] [PubMed] [Google Scholar]
- 34.Wertz RA. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970;58:41–66. doi: 10.1016/0002-9416(70)90127-2. [DOI] [PubMed] [Google Scholar]
- 35.Kartalian A, Gohl E, Adamian M, Enciso R. Cone-beam computerized tomography evaluation of the maxillary dentoskeletal complex after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2010;138:486–492. doi: 10.1016/j.ajodo.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 36.Ballanti F, Lione R, Fanucci E, Franchi L, Baccetti T, Cozza P. Immediate and post-retention effects of rapid maxillary expansion investigated by computed tomography in growing patients. Angle Orthod. 2009;79:24–29. doi: 10.2319/012008-35.1. [DOI] [PubMed] [Google Scholar]
- 37.Phatouros A, Goonewardene MS. Morphologic changes of the palate after rapid maxillary expansion: a 3-dimensional computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2008;134:117–124. doi: 10.1016/j.ajodo.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 38.Sandstrom RA, Klapper L, Papaconstantinou S. Expansion of the lower arch concurrent with rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 1988;94:296–302. doi: 10.1016/0889-5406(88)90054-6. [DOI] [PubMed] [Google Scholar]
- 39.Ghoneima A, Abdel-Fattah E, Hartsfield J, El-Bedwehi A, Kamel A, Kula K. Effects of rapid maxillary expansion on the cranial and circummaxillary sutures. Am J Orthod Dentofacial Orthop. 2011;140:510–519. doi: 10.1016/j.ajodo.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gautam P, Valiathan A, Adhikari R. Stress and displacement patterns in the craniofacial skeleton with rapid maxillary expansion: a finite element method study. Am J Orthod Dentofacial Orthop. 2007;132:5.e1–e11. doi: 10.1016/j.ajodo.2006.09.044. [DOI] [PubMed] [Google Scholar]
- 41.Kennedy JW, III, Bell WH, Kimbrough OL, James WB. Osteotomy as an adjunct to rapid maxillary expansion. Am J Orthod. 1976;70:123–137. doi: 10.1016/s0002-9416(76)90313-4. [DOI] [PubMed] [Google Scholar]
- 42.Lehman JA, Jr, Haas AJ. Surgical-orthodontic correction of transverse maxillary deficiency. Clin Plast Surg. 1989;16:749–755. [PubMed] [Google Scholar]
- 43.Bell WH, Epker BN. Surgical-orthodontic expansion of the maxilla. Am J Orthod. 1976;70:517–528. doi: 10.1016/0002-9416(76)90276-1. [DOI] [PubMed] [Google Scholar]
- 44.Oliveira NL, Da Silveira AC, Kusnoto B, Viana G. Three-dimensional assessment of morphologic changes of the maxilla: a comparison of 2 kinds of palatal expanders. Am J Orthod Dentofacial Orthop. 2004;126:354–362. doi: 10.1016/j.ajodo.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 45.Holberg C, Rudzki-Janson I. Stresses at the cranial base induced by rapid maxillary expansion. Angle Orthod. 2006;76:543–550. doi: 10.1043/0003-3219(2006)076[0543:SATCBI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 46.Sari Z, Uysal T, Usumez S, Basciftci FA. Rapid maxillary expansion. Is it better in the mixed or in the permanent dentition. Angle Orthod. 2003;73:654–661. doi: 10.1043/0003-3219(2003)073<0654:RMEIIB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]