Abstract
Background
Information is routinely given to pregnant women, but information about caesarean birth may be inadequate.
Objectives
To examine the effectiveness of information about caesarean birth.
Search methods
We searched the Cochrane Pregnancy and Childbirth register, CENTRAL (26 November 2002), MEDLINE [online via PubMed 1966‐] and the Web of Science citation database [1995‐] (20 September 2002), and reference lists of relevant articles.
Selection criteria
Randomised controlled trials, non‐randomised clinical trials and controlled before‐and‐after studies of information given to pregnant women about caesarean birth.
Data collection and analysis
Two review authors independently assessed trial quality and extracted data. Missing and further data were sought from trial authors unsuccessfully. Analyses were based on 'intention to treat'. Relative risk and confidence intervals were calculated and reported.
Consumer reviewers commented on adequacy of information reported in each study.
Main results
Two randomised controlled trials involving 1451 women met the inclusion criteria. Both studies aimed to reduce caesarean births by encouraging women to attempt vaginal delivery. One used a program of prenatal education and support, and the other cognitive therapy to reduce fear. Results were not combined because of differences in the study populations. Non‐clinical outcomes were ascertained in both studies through questionnaires, but were subject to rates of loss to follow‐up exceeding 10%.
A number of important outcomes cannot be reported: knowledge or understanding; decisional conflict; and women's perceptions: of their ability to discuss care with clinicians or family/friends, of whether information needs were met, and of satisfaction with decision‐making.
Neither study assessed women's perception of participation in decision‐making about caesarean birth, but Fraser 1997, who examined the effect of study participation on decision making, found that women in the intervention group were more likely to consider that attempting vaginal birth was easier (51% compared to 28% in control group), or more difficult (10% compared to 6%). These results could be affected by the attrition rate of 11%, and are possibly subject to bias.
Neither intervention used in these trials made any difference to clinical outcomes. About 70% or more women attempted vaginal delivery in both trials, yet caesarean delivery rates exceeded 40%, at least 10% higher than was hoped. There was no significant difference between control and intervention groups for any of the outcomes measured: vaginal birth, elective/scheduled caesarean, and attempted vaginal delivery.
Outcome data, although similar for both groups, were not sufficient to compare maternal and neonatal morbidity or neonatal mortality.
There was no difference in the psychological outcomes for the intervention and control groups reported by either of the included trials.
Consumer reviewers said information for women considering a vaginal birth after caesarean (VBAC) should include: risks of VBAC and elective caesarean; warning signs in labour; philosophy and policies of hospital and staff; strategies to improve chances of success; and information about probability of success with specific care givers.
Authors' conclusions
Research has focussed on encouraging women to attempt vaginal delivery. Trials of interventions to encourage women to attempt vaginal birth showed no effect, but shortcomings in study design mean that the evidence is inconclusive.
Further research on this topic is urgently needed.
Plain language summary
Information to encourage pregnant women to attempt vaginal birth has not been shown to change caesarean birth rates
Caesarean births have become more common in many countries. Women need information to know what to expect after surgery and to help them make decisions. Women's choices are thought to contribute to the rise in caesarean births. Information given to pregnant women may affect their choices. Shortcomings in the included studies mean the evidence is inconclusive, although the trials found that information to encourage women to attempt vaginal birth did not affect caesarean birth rates. More research is urgently needed.
Background
Introduction
The purpose of this review is to examine the effectiveness of methods to inform pregnant women about caesarean birth, and to review the content of information given to women about caesarean birth.
Caesarean birth is a major health issue affecting the lives of many childbearing women. Caesarean delivery rates have risen steadily in the developed world since the 1970s. In some areas and among some populations caesarean deliveries represent a quarter or more of all births (Nassar 2001; Potter 2001; Thomas 2001).
Importance of health information
There is some evidence that information for health consumers can influence health outcomes. The provision of additional information affects the willingness of people to undergo hypothetical screening tests (Domenighetti 2000), and is associated with higher satisfaction without inducing anxiety (Garrud 2001). The information given to women considering, or being encouraged to consider, a caesarean birth, is a critical component of their care, and is the basis of informed consent and informed decision‐making.
There are two reasons for giving women evidence‐based information about caesarean section: (a) to help women understand their care needs when they undergo a caesarean section; and (b) to help women in decision‐making related to caesarean section.
Information about caesarean section
Information is routinely given to women to improve knowledge about what to expect and how to care for themselves after giving birth. However, knowledge of the extent of morbidities following caesarean birth may be lacking. One Australian study recommended that women be better informed about the likelihood of infection after a caesarean birth, after reporting overall infection rates of 17% one month after caesarean birth compared to 2.8% at the time of discharge from hospital (Creedy 2001). Other studies have found that caesarean birth has also been associated with higher levels of maternal rehospitalisation (Lydon‐Rochelle 2000; Thompson 2002). It is unclear whether health professionals or women know about these rates of infection and rehospitalisation, but without research to explain such findings fully three different conclusions could be drawn. First, there may be a general lack of awareness among health professionals of the extent of complications associated with caesarean birth. This raises questions about whether women are similarly ill informed. Alternatively, women may be appropriately informed about how to reduce poor outcomes but are failing to act on the information given to them. A third possibility is that the information given to women about what to expect post‐operatively may not be sufficient either to prepare them to care for themselves after surgery, or to reduce poor outcomes such as infection.
Availability of information is not the only problem for women considering caesarean birth. Caesarean birth itself comprises a number of care decisions (eg. type of anaesthesia, methods of wound repair, use of prophylactic therapies and care practices after surgery) (Hopkins 1999; Mangesi 2002; Smaill 2002; Wilkinson 2002; Bamigboye 2003) but in practice such choices may be limited or unavailable, or may not be made known to women if not thought appropriate. In an observational study of antenatal care, Stapleton (Stapleton 2002) witnessed most women tending to comply with the suggestions of health professionals. The latter guided women's decisions towards technological interventions by giving information that minimised risk for those interventions and emphasising the potential for harm without the intervention. In the context of a review of information provision it is appropriate to compare the information given to women about procedures and their choices, with the actual services made available to them.
Maternal preference for caesarean birth is thought to contribute to the rise in caesarean birth rates. British doctors reported to the National Sentinel Caesarean Section Audit that maternal request was the main reason for seven per cent of caesarean births (Thomas 2001) and interest in women's preference to deliver by caesarean section has prompted considerable study over the past decade (Mould 1996; Graham 1999; Quinlivan 1999; Turnbull 1999; Gamble 2000; Gamble 2001). On the other hand, a literature review of women's preferred mode of delivery (Gamble 2000) found that caesarean delivery was rarely requested by women (one per cent or less) in the absence of obstetric complications in either their current or previous pregnancies. Common sense argues that information must not only be available, but also of a good quality before women can make good choices. None of the ten studies in Gamble's literature review examined the quality of the information given to the women, although some assessed women's perceived level of knowledge (Gamble 2000).
Information for decision‐making
Information is the minimal requirement of a decision aid, or intervention designed to help people make health care choices. Decision aids generally combine the provision of information with at least one other component such as a values clarification exercise or guidance in decision‐making. A Cochrane review has found that decision aids improve knowledge of options and outcomes, lead to more realistic expectations, reduce the decisional conflict associated with people feeling uninformed, and stimulate an active role in decision‐making (O'Connor 2002). An Australian trial is underway, of a decision aid to help women who have previously undergone a caesarean to consider their options in a subsequent pregnancy (Shorten 2003).
Information may influence choices about care, but health decisions are complex and predicting the impact of providing health consumer information on the caesarean birth rate is difficult. While it would be unethical to manipulate health choices through the selective presentation of evidence, the impact of information‐based interventions needs to be monitored because shifts in health care patterns are important in health planning. Information about caesarean birth may also affect medico‐legal pressures, which are also believed to contribute to rising caesarean birth rates (Thomas 2001; Johanson 2002). Some doctors believe that pregnant women have unrealistic expectations which lead women to sue if the birth does not go as planned. In response, doctors practice 'defensively', that is, choose to intervene earlier and perform a caesarean delivery (Tito 1995). Information given to women has the potential to modify expectations and may influence outcomes.
Women's information needs
There is little research on what information women actually need or want to make decisions about caesarean birth, or how to care for themselves afterwards. In other aspects of maternity care however, there is a mismatch between women's experiences and what they want to know, and caregivers' beliefs about their information needs (Freda 1993; Zib 1999). For instance Zib et al. found that a wider range of symptoms were experienced by pregnant women than are mentioned in current obstetric texts, and presumably understood by caregivers. Freda et al. found significant differences between the topics of interest to pregnant women and the topics that those who provided their care thought would be of interest to them.
There is also variation in the quantity and type of information that individual consumers want, or need, to feel informed (Robinson 2001). While healthcare‐related information is needed for decision‐making, it is not the only criterion people use, because each person brings previous experiences, beliefs and values, fears and information from other sources (Callister 1995; Charles 1999). Women may rely on health professionals, partners, friends or family members to help make decisions about their health care; but exactly who is involved is likely to be subject to personal and cultural influences. However, in most countries, women retain legal autonomy in regard to decisions about their health care, so how women themselves are informed, and how they feel about decision‐making processes, are important factors in making decisions when considering caesarean birth.
Dimensions of information quality
The potential impact of variables on a study such as those described above make it desirable to assess the intervention, or information given, as well as the study design. The data checklist developed by the Cochrane Effective Practice and Organisation of Care Review Group (EPOC 1998) provided a valuable starting point for developing an approach to this. Thus the content of any information needs to be assessed to see what consideration has been given to the quality, or evidence base, of material included and the range of issues covered, in particular potential benefits and harms, and treatment options (Shepperd 1997; Coulter 1999).
Format also needs to be assessed because it may shape how effective information will be. Information is given to consumers in a variety of formats such as leaflets and videos. Its presentation, such as the sequence and the types of information presented together, can affect how information is received. The style, or how information is framed, and how risk data are presented are important. Other important factors are the language, such as the degree of certainty used, and the use of scales, graphics and explanations (Entwistle 1998; Coulter 1999; Edwards 2002).
It is important to understand the context in which information about caesarean birth is given to pregnant women. Studies should report timeliness, or when information is given, when outcomes are measured, and whether information is given in stages or followed‐up. Despite a lack of work on this issue specific to the provision of information about caesarean birth, the timing of information is important in general studies (Butow 1998) and when measuring postnatal outcomes, for example the potential bias of the 'halo' effect, which follows the period immediately after birth when women are unwilling to be critical of their care (Brown 1993; Turnbull 1999).
Procedures used in caesarean birth are not uniform across health services, and health information for consumers has lacked consistency in content. Other issues such as who delivers the information and the timing of its delivery might also be relevant. It is also important to know who has taken part in research involving any information exchange, because of the influence they may have on the outcome.
Information for consumers should be acceptable and useful to them. In the absence of research on what consumers want to know about caesarean birth, it is important to know how information used in research has been produced to meet consumer needs. To achieve good outcomes, it is recommended that consumer needs form the basis of producing consumer information, and a key feature is the involvement of consumers (Coulter 1999; Silburn 2000).
Objectives
To examine the effectiveness of the provision of an information intervention for pregnant women about caesarean birth on health outcomes, knowledge, impact on decision‐making, information seeking and information needs.
To review the content of information interventions given to pregnant women about caesarean birth.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials, non‐randomised clinical trials and controlled before‐and‐after studies.
Types of participants
Pregnant women, including those with a specific indication for caesarean delivery or who have previously delivered by caesarean section.
Studies that include outcomes for others, such as partners and other family members, will be included where the outcomes for the women alone can be extracted. Outcomes for other participants are not included in this review, because whilst others play an important role in some cultures, they are outside the scope of this review. Not all women have partners or others active in decision‐making about their health care.
Studies that give information about caesarean birth to women planning pregnancy were excluded.
Types of interventions
Any intervention designed to inform women about caesarean birth, their choices for care, and the implications of treatment choices compared to usual care. The interventions might aim to improve information given to pregnant women or they might be interventions designed specifically for women considering caesarean birth or who have been advised to undergo caesarean delivery.
Types of outcome measures
(1) Knowledge or understanding (2) Decisional conflict (3) Women's perception of: (a) participation in decision‐making or 'active say' (b) ability to discuss care with clinicians or family/friends (c) whether information needs are met (d) satisfaction with decision‐making (4) Clinical outcomes (primary or secondary caesarean), mode of birth, maternal morbidities (eg. infection and incontinence) and neonatal morbidities (5) Psychological outcomes: eg. anxiety and sense of control
Search methods for identification of studies
We searched the Cochrane Pregnancy and Childbirth Review Group register of studies on 26 November 2002 (see 'Search strategies for the identification of studies section' within the editorial information about the Cochrane Pregnancy and Childbirth Group). We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library issue 4, 2002), using the terms 'exp cesarean section/(MeSH), and text words cesarean or caesarian' on 26 November 2002.
We searched MEDLINE [online via PubMed 1966‐ ] and the Web of Science citation database [electronic resource: Institute for Scientific Information; including Science Citation Index Expanded, Social Sciences Citation Index, Arts & Humanities Citation Index 1995‐ ], on 20 September 2002, using the following strategy: 1 randomized controlled trial.pt. 2 randomized controlled trials/ 3 controlled clinical trial.pt. 4 random allocation/ 5 double blind method/ 6 single‐blind method/ 7 or/1‐6 8 clinical trial.pt. 9 exp clinical trials/ 10 (clin$ adj25 trial$).tw. 11 ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).tw. 12 placebos/ 13 placebo$.tw. 14 random$.tw. 15 research design/ 16 or/8‐15 17 comparative study/ 18 exp evaluation studies/ 19 follow up studies/ 20 prospective studies/ 21 (control$ or prospectiv$ or volunteer$).tw. 22 (time adj series).tw. 23 (pre test or pretest or (post test or posttest)).tw. 24 or/17‐23 25 animal/ not (human/ and animal/) 26 7 or 16 or 24 27 26 not 25 28 exp cesarean section/ 29 27 and 28 30 (case adj conference$).tw. 31 (counseling or counselling).tw. 32 counseling/ 33 (group adj therap$).tw. 34 psychotherapy, group/ 35 family therapy/ 36 discussion$.tw. 37 (information or informing or informed or inform).tw. 38 patient education/ 39 (educational adj material$).tw. 40 self‐help groups/ 41 (support adj group$).tw. 42 (telling or disclosure).tw. 43 (leaflet$ or booklet$ or pamphlet$ or helpline or advice or advise$).tw. 44 (informed adj consent).tw. 45 (decision adj making).tw. 46 communicat$.tw. 47 patient participation/ 48 or/30‐47 49 29 and 48
We also checked the reference lists of relevant articles used in the background and identified by the search.
Data collection and analysis
Two review authors assessed the potential relevance of all abstracts identified from the electronic searches independently. Disagreement was resolved by discussion. Full publications were retrieved and assessed for inclusion by two review authors independently on the basis of assessment criteria for intervention and study quality set out in the protocol for this review. An assessment of consumer involvement and the potential for assessor bias were reported, but do not form the basis for exclusion. Disagreement was resolved by discussion.
Assessment of Study Quality
Two review authors independently screened studies identified by the search for inclusion. They were assessed for: (1) intervention quality (content, adequacy of content, format, context); (2) study design (randomised controlled trials, non‐randomised clinical trials and controlled before‐and‐after studies); (3) methodological quality (concealment, completeness of follow‐up, blinding of assessment of outcome or data collection and control site); (4) consumer involvement in information preparation; (5) clinician involvement in information preparation; (6) potential for assessor bias; (7) agreement with clinical protocols.
Discrepancies were resolved by discussion. Each of the full publications was screened for eligibility. Reasons for exclusion of studies are given in Characteristics of excluded studies.
(1) Intervention quality
Assessment of the intervention quality was done in two steps.
Step 1: Eligible studies were screened to see if the information intervention had been assessed using a validated instrument. If not, an assessment was made based on the criteria outlined in Step 2.
Step 2: Information interventions were assessed based on a) Content b) Format and c) Context as follows:
(a) Assessment of content based on: (i) Quality of information (evidence base); (ii) Potential outcomes ‐ benefits and harms (evidence base); (iii) Options ‐ alternatives (evidence base).
Adequacy of content graded as follows: (A) Quality of information, potential outcomes and options are all addressed in information content, with evidence base reported; (B) Unclear whether all issues addressed but evidence base reported; (C) All issues addressed in information content but evidence base unclear; (D) Not all issues addressed in information and evidence base unclear; (E) Unclear whether issues addressed in content and evidence base unclear.
Clarification was sought from study authors if necessary. Studies were excluded when final assessment of adequacy of content was graded as (D) or (E).
(b) Assessment of format based on: (i) Type ‐ eg. pamphlet, video, counselling; (ii) Information used alone or in conjunction with other forms of information; (iii) Language ‐ inclusion of comment/ description/ translation; (iv) Style ‐ perspective, framing.
Adequacy of reporting on format graded as follows: (A) Trialists reported type of format, whether information used alone or in conjunction with other forms of information, language and style; (B) Trialists reported at least three of these issues (type of format, whether information used alone or on conjunction with other forms of information, language and style); (C) Trialists reported at least two of these issues (type of format, whether information used alone or on conjunction with other forms of information, language and style); (D) Trialists reported at least one issue (type of format, whether information used alone or on conjunction with other forms of information, language or style); (E) Trialists do not report on type of format, whether information used alone or in conjunction with other forms of information, language or style.
Clarification was sought from study authors if necessary. Studies were excluded when final assessment of adequacy of format was graded as (E).
(c) Assessment of context based on: (i) Timeliness ‐ When information given ‐ eg. staging and follow‐up; (ii) Participants ‐ Information exchange participants: who gives information and who receives information ‐ population in statement; (iii) Process of information development.
Adequacy of reporting on context graded as follows: (A) Timeliness, participants and process of information development are all reported; (B) At least two issues reported; (C) At least one issue reported; (D) No issues reported.
Clarification was sought from study authors if necessary. Studies were excluded when final assessment of adequacy of context was graded as (C) or (D).
(2) Study design
Initial assessment ranked studies by their design. Studies other than randomised controlled trials, controlled clinical trials and controlled before‐and‐after studies were excluded.
Study design was graded as: (A) Randomised controlled trials; (B) Controlled clinical trials; (C) Controlled before‐and‐after studies; (D) Other study designs.
Studies assessed as (D) were excluded from the review. (3) Study Methodological Quality
The methodological quality of studies was assessed for inclusion based on factors relating to the study design.
The methodological quality of the included trials was assessed using the following criteria (Clarke 2000):
Randomised controlled trials (RCT)
(a) Adequacy of concealment of allocation to experimental or control groups was graded as: (A) if adequate; (B) if unclear; (C) if inadequate; (D) if it is not used. Clarification was sought from study authors if necessary. Studies were excluded when final assessment of adequacy of concealment was graded as (C) or (D).
In addition, quality scores were assigned to each trial for completeness of follow‐up and blinding of outcome assessment as follows:
(b) Completeness of follow‐up was graded as: (A) if < 3% of participants excluded; (B) if 3 to 9.9% of participants excluded; (C) if 10 to 19.9% of participants excluded; (D) if 20% or more excluded; (E) if completeness of follow‐up is unclear.
Clarification was sought from study authors if necessary. Studies were excluded when final assessment of adequacy of completeness of follow‐up was graded as (C), (D) or (E).
(c) Blinding of assessment of outcome was graded as: (A) if there is blinded outcome assessment; (B) if it is unblinded, but unlikely to be biased; (C) if there is a high likelihood of assessment bias; (D) if blinding of outcome assessment is unknown.
Clarification was sought from study authors if necessary. Studies were excluded when final assessment of adequacy of blinding of assessment is graded as (C) or (D).
Non‐randomised clinical trial (CT)
(a) Quasi‐random allocation to experimental or control groups would have been graded as: (A) if definitely assigned prospectively; (B) if it is unclear whether assigned prospectively; (C) if it is not assigned prospectively.
Clarification would have been sought from study authors if necessary. If final assessment of adequacy of concealment was graded as (C), the study would have been excluded.
In addition, quality scores were to be assigned to each trial for completeness of follow‐up and blinding of outcome assessment as follows:
(b) Completeness of follow‐up would have been graded as: (A) if < 3% of participants are excluded; (B) if 3 to 9.9% of participants are excluded; (C) if 10 to 19.9% of participants are excluded; (D) if 20% or more are excluded; (E) if completeness of follow‐up is unclear.
Clarification would have been sought from study authors if necessary. If final assessment of completeness of follow‐up was graded as (C), (D) or (E), the study would have been excluded.
(c) Blinding of assessment of outcome would have been graded as: (A) if blinded outcome assessment; (B) if unblinded, but unlikely to be biased; (C) if there is a high likelihood of assessment bias; (D) if blinding of assessment bias is unknown.
Clarification would have been sought from study authors if necessary. If final assessment of blinding of assessment was graded as (C) or (D), the study would have been excluded.
Controlled before‐and‐after study
(a) Contemporaneous data collection would have been graded as: (A) if it is done for both pre and post intervention periods; (B) if it is unclear whether done for both pre and post intervention periods; (C) if it is not done for both pre and post intervention periods.
Clarification would have been sought from study authors if necessary. If final assessment of contemporaneous data collection was graded as (C), the study would have been excluded.
(b) Appropriate choice of control site would have been graded as: (A) if both study and control sites are comparable; (B) if it is unclear whether both study and control sites are comparable; (C) if study and control sites are not comparable.
Clarification would have been sought from study authors if necessary. If final assessment of choice of control site was graded as (C), the study would have been excluded.
In addition, quality scores were to be assigned to each trial for completeness of follow‐up and blinding of outcome assessment as follows:
(c) Completeness of follow‐up would have been graded as: (A) if < 3% of participants are excluded; (B) if 3 to 9.9% of participants are excluded; (C) if 10 to 19.9% of participants are excluded; (D) if 20% or more are excluded; (E) if completeness of follow‐up is unclear.
Clarification would have been sought from study authors if necessary. If final assessment of completeness of follow‐up was graded as (C), (D) or (E), the study would have been excluded.
(d) Blinding of assessment of outcome would have been graded as: (A) if blinded outcome assessment; (B) if unblinded, but unlikely to be biased; (C) if high likelihood of assessment bias; (D) if blinding of assessment cannot be ascertained.
Clarification would have been sought from study authors if necessary. If final assessment of contemporaneous data collection was graded as (C) or (D), the study would have been excluded.
The following criteria were reported but were not used as a basis of exclusion:
(4) Consumer involvement
Consumer involvement was graded as:
(A) if consumers were involved in the process of preparing consumer information; (B) if it is not clear if consumers were involved in the process of preparing consumer information; (C) if consumers were not involved in the process of preparing consumer information.
(5) Health professional involvement
Health professional involvement was graded as:
(A) if health professionals were directly involved in the process of preparing consumer information; (B) if it is not clear if health professionals were directly involved or if indirectly involved in the process of preparing consumer information; (C) if health professionals were not involved in the process of preparing consumer information. (6) Potential for assessor bias
Potential for assessor bias was graded as:
(A) if researcher not provider of information or clinical care; (B) if researcher not provider of clinical care; (C) if researcher not provider of information; (D) if it is unclear whether researcher is provider of information or clinical care; (E) if researcher provider of both information and clinical care.
(7) Agreement with clinical protocols
Agreement with clinical protocols was graded as: (A) if intervention is assessed as agreeing with relevant hospital clinical protocols; (B) if intervention is assessed as partially agreeing with relevant hospital clinical protocols; (C) if intervention is assessed as not agreeing with relevant hospital clinical protocols or if no assessment has been made.
Data collection and analysis
For included studies, two review authors extracted data independently. Discrepancies were resolved by discussion and consensus between review authors.
Missing and further data were sought from the trial authors unsuccessfully. These were necessary for subgroup analyses to assess the effect of parity, and previous caesarean delivery in clinical outcomes.
Outcomes subject to attrition bias are reported but not analysed further. There were insufficient studies included in the review to enable sub‐group analyses to assess the impact of the potential for assessor bias, and the effect of the purpose of the intervention, that is to educate, to aid decision‐making, etc.
Descriptive data collected included the authors, year of publication, setting, country, time span of the study, calculated sample size, number of study participants, description of study participants, number of participants analysed, timing of data collection, description of the intervention, eg. content and purpose (to educate, to aid decision‐making,etc), timing and frequency of intervention, proportion of sample with caesarean delivery, and report of follow‐up strategy.
Primary analyses were based on 'intention to treat' and were confined to study type, that is, results from different study designs were not combined. All the comparisons were analysed with both a fixed effect and random effects model and reported using a fixed effect approach.
It was intended that outcomes for continuous data measured in a standard way across studies, be reported by the weighted mean difference and confidence intervals (CIs). If studies were found to use different instruments to measure the same conceptual phenomenon (eg. satisfaction with decision‐making) it was intended that the standardised mean difference would be reported, with a rationale and cautious approach to combining results.
In studies that reported dichotomous data, the relative risk (RR) and CIs were calculated and reported. It was intended that the risk difference would be reported if appropriate. Where necessary, and possible, outcomes and 95% CIs were calculated from result data.
The described content of information in each study was collated, with the intention of sorting for its intended purpose for comparison. Experienced consumer reviewers in the Cochrane Pregnancy and Childbirth Review Group Consumer Panel commented on the adequacy of the information. Similarly members of the Pregnancy and Childbirth Consumer Panel provided feedback on the preliminary results of the review. A summary of the consumer feedback is included and was considered in the final analysis. It was intended to combine statistically the results of studies if appropriate, with the meta‐analytic technique dependent on the outcomes reported.
The RR and CIs were calculated and reported for dichotomous data.
Results
Description of studies
Results of the search
The search strategy yielded 279 studies, of which five studies were judged to be potentially relevant based on the abstracts. These five papers were assessed in detail. For details of the three excluded studies, see Characteristics of Excluded Studies table.
Included studies
Two studies, both randomised controlled trials, met the criteria for inclusion in the review.
Fraser 1997 was a multi‐centre trial in 12 North American hospitals involving 1275 pregnant women who had previously given birth by caesarean. It aimed to assess whether a prenatal education and support program promoting vaginal birth after caesarean delivery (VBAC), compared to providing a brief pamphlet, increases probability of vaginal birth for women with a previous caesarean section.
Saisto 2001 was based in a single centre in Finland and involved 176 pregnant women. It aimed to evaluate the effect of an intensive treatment, compared to conventional treatment, to reduce requests for caesarean birth among women who feared childbirth.
Participants
Fraser 1997 recruited pregnant women who had experienced a single previous low caesarean birth, identified through doctors' offices and hospital pre‐admission registries.
Saisto 2001 recruited women following referral to an outpatient clinic at a university teaching hospital. Women who were giving birth for the first time comprised about half of the study population. Participants were physically healthy women with a low obstetric risk diagnosed with a fear of childbirth by their responses to a 10‐item questionnaire. Fear was assessed on the basis of either five or more positive responses to any of the 10 items, or a positive response to one specific item "do you prefer a cesarean to an ordinary delivery?"
Both studies categorised women's motivation to achieve vaginal delivery. There was no comment on the validity and reliability of either assessment tool.
Fraser 1997 blocked and stratified randomisation according to women's motivation. This was assessed by responses on a visual analogue scale to the statement "I plan to attempt a vaginal delivery in this pregnancy".
Saisto 2001 used a less conventional approach and assessed motivation for treatment and confrontation of fears on the basis of the completion or otherwise of three voluntary questionnaires. Women who did not complete questionnaires were judged to have low motivation. We were unsuccessful in obtaining clarification from the researchers as to how women were classified who completed one or two of the three questionnaires. The questionnaires were designed to assess depression, anxiety and personal concerns in pregnancy, as well as satisfaction with childbirth after birth.
Intervention
(a) Purpose
The aim of both studies was to reduce caesarean birth rates. Fraser 1997 promoted vaginal birth after caesarean delivery and Saisto 2001 sought to reduce requests for caesarean delivery among pregnant women identified as having fear of vaginal birth.
(b) Content
Although the purpose of both studies was to reduce the caesarean birth rate, the information contained in the interventions was similar in only one topic, pain relief options in labour. Saisto 2001 covered this topic only in an optional appointment with a midwife, whereas Fraser 1997 gave women in the intervention group information about the pain relief options in labour available in their centre.
Fraser 1997 also gave all participants a pamphlet that included information that outlined the benefits of vaginal birth after caesarean section compared to those of repeat caesarean. Women in the intervention group also received information in face‐to‐face sessions with a research nurse and a resource person, the latter with personal experience of vaginal birth after caesarean delivery (VBAC). This information included: the probability of success of vaginal birth in their centre; available pain relief options in labour; alternative sterilisation options (if it was being considered); national consensus panel recommendations favouring vaginal birth; and identification and discussion of barriers to VBAC, including, when applicable, the views of the treating obstetrician.
Saisto 2001 involved all participants in two sessions at 24 and 36 weeks of pregnancy with an obstetrician trained in cognitive therapy and childbirth psychology to discuss feelings, experiences and misconceptions about childbirth and to "reformulate the problem". Women in the intervention group were given additional sessions, and were offered an optional session with a midwife to discuss practical information about pain relief and possible interventions. They were encouraged to visit the obstetric ward, and were given telephone access to the obstetrician and midwife throughout their pregnancy.
(c) Implementation
The intervention used in both studies was the provision of additional face‐to‐face information and support.
Fraser 1997 provided the intervention as two separate face‐to‐face contacts, the first at the time of recruitment with a research nurse, prior to 28 weeks of pregnancy, and the second with the research nurse and the resource person, four to eight weeks later.
Saisto 2001 provided women in the intervention group with four additional 45‐minute appointments with the doctor at 28, 32, 37 and 38 weeks, and an optional 90‐minute appointment with a midwife at 37 weeks.
Both included studies were conducted in the 1990s over time spans of two and a half years (Fraser 1997) to almost three years (Saisto 2001).
(d) Informed consent
Informed consent was formally obtained and reported in both studies. However whilst Saisto 2001 assured women that completion of the questionnaires was voluntary, completion of questionnaires was taken as an indication of each woman's motivation to confront fears of childbirth.
Methods of analysis
Statistical analysis for the primary outcomes in both studies was based on an intention to treat approach.
There were additional post hoc analyses in both studies where outcomes were analysed based on the motivational strata into which women were classified. Fraser 1997 compared attempted vaginal delivery, vaginal delivery and scheduled caesarean delivery for women classified as having low motivation to achieve a vaginal birth with those with high motivation. Saisto 2001 compared requests for caesarean delivery and actual caesarean delivery amongst women who completed questionnaires, against those that did not. Requests for caesarean delivery among women who took up the optional midwifery appointment and those that did not were also compared. In addition, Saisto 2001 reported separately their analyses of two items in the Pregnancy Anxiety Scale (fear of pain in labour, and fear of the obstetrician's unfriendly behaviour). We unsuccessfully sought clarification as to how the trialists classified women who completed one or two of the three questionnaires.
Risk of bias in included studies
The methodological quality of included studies was assessed on aspects of the study design (allocation, follow‐up and blinding of assessment) and the information intervention (content, format and context). See Table 1.
1. Assessment of information intervention.
| Study | Description | Assessment | Preparation | Agreement | Assessor bias |
| Fraser 1997 | PURPOSE: to encourage women with previous caesarean to attempt VBAC All participants received a pamphlet that outlined the benefits of vaginal birth after caesarean section compared to repeat caesarean. Women in the intervention group also received national consensus panel recommendations favouring vaginal birth, information about the probability of success of vaginal birth in their centre, pain relief options in labour, alternative sterilisation options (if it was being considered), and identification and discussion of barriers to VBAC, including, when applicable, the views of the treating obstetrician. The program also included peer support from the resource person. | Not assessed with validated instrument. | Consumer involvement in preparing information: Resource person had personal experience of VBAC. Graded A. | No assessment of agreement with clinical protocols reported but intervention specifically addresses identification and discussion of barriers to VBAC including the views of the treating obstetrician. Graded C. | Researchers not providers of information or clinical care. Potential for conflict of interest graded A. |
| CONTENT: Quality of information, potential outcomes and options are all addressed in information content with evidence base reported. Content graded B. | Health professional involvement in preparing information: Research nurses chosen on basis of experience in prenatal instruction, directly involved. Graded A. | ||||
| FORMAT: Type, whether additional information used, language and style all reported. Verbal information based on model of health promotion‐disease prevention interventions in Green & Kreuter. Format graded A. | |||||
| CONTEXT: Timeliness, participants and process of information development are all reported. Context graded A. | |||||
| OVERALL grade: A | |||||
| Saisto 2001 | PURPOSE: to reduce number of requests for caesarean birth among women with fear of childbirth. The content comprised discussion of feelings, experiences and misconceptions. Women in the intervention group were also offered an optional session with a midwife to discuss practical information about pain relief and possible interventions, and were encouraged to visit the obstetric ward. They were also given telephone access to obstetrician and midwife throughout their pregnancy. | Not assessed with validated instrument. | Consumer involvement in preparing information: No information given about consumer involvement. Graded C. | No assessment evident but written information provided to women includes "alternative modes of pain relief available at our hospital". Graded C. | The researcher directly involved in the intervention and with measuring the primary outcome (request for caesarean delivery). No information about how this data were collected from control group. Graded E. |
| CONTENT: Potential outcomes and options addressed in content but evidence base unclear. Content graded C. | Health professional involvement in preparing information: Obstetrician provider of information about cognitive and behavioural exercises, midwife provider of practical information about pain relief and labour interventions. Graded A | ||||
| FORMAT: Type, whether additional information used, and style ("reformulation") all reported. Format graded B. | |||||
| CONTEXT: When information was given and who delivered and received it were reported. No information about process of development. Context graded B. | |||||
| OVERALL grade: C |
Study Design
Allocation
Fraser 1997 allocated women randomly to control and intervention groups using a centralised telephone answering service. Allocation to either group was blocked, and stratified by hospital and by woman's motivation to attempt vaginal birth.
Saisto 2001 allocated women to either control or intervention groups in balanced blocks of 20 using sealed opaque envelopes.
Follow‐up
In both studies complete data on clinical outcomes were extracted from medical records for all study participants. Data collected by questionnaire were less complete. Loss to follow‐up exceeded 10% in both studies.
Fraser 1997 had an 89% response to a single questionnaire to assess sense of control and effects of participation on decision‐making, distributed 12 to 72 hours after delivery.
Saisto 2001 had less than 80% response to each of three questionnaires, with less than 65% of study participants completing all questionnaires. There were two questionnaires in pregnancy, at 24 weeks (response rate 77.6% for the intervention group and 79.1% for the control group), and 36 weeks (69.4% and 62.6%). A postpartum questionnaire three months after birth was used to measure satisfaction with childbirth, but had a response of less than 70% (67.1% of the intervention group and 58.2% of the control group).
Blinding of assessment
Fraser 1997 reported that researchers did not have direct contact with women after recruitment, however research nurses who provided the intervention extracted data from medical records after hospital discharge. Predetermined criteria were defined for attempted vaginal delivery prior to data extraction.
Saisto 2001 did not blind assessment. The researcher assessed the primary outcome of request for caesarean birth at 38 weeks of pregnancy, as well as providing the intervention sessions.
Sample size calculations
Both studies reported sample size power calculations.
Fraser 1997 calculated that each arm of the study needed 649 women, with a total of 1298, to achieve a caesarean birth rate of 30% for the control group and RR for the verbal intervention group of 1.25 with 80% power.
Saisto 2001 calculated that, based on 90% power, each study arm needed 74 women, a total of 148, to detect a 50% reduction in a caesarean birth rate that had been identified in other studies comparing outcomes for women with a fear of childbirth. These studies included a descriptive study (Ryding 1993) and a case‐control study (Sjogren 1997), which found an initial request for caesarean birth of 68%.
Intervention quality
Neither study reported that they assessed the information used in the study with a validated tool, so criteria pre‐determined by review authors were used to assess the intervention. This assessment was based on three aspects of consumer health information: content, format and context. See Table 2.
2. Assessment of study design and methodological quality.
| Study | Design | Concealment | Follow‐up | Blinding |
| Fraser (1997) | Randomised controlled trial. Graded A | Used centralised telephone answering service. Graded A | For clinical outcomes <3% of participants excluded. Graded A. For sense of control 10% to 19.9% of participants excluded. Graded C | Although researchers were careful to restrict contact to pre‐randomisation period only, the research nurse who provided the intervention extracted data from medical records. Blinding graded B. |
| Saisto (2001) | Randomised controlled trial. Graded A | Randomly assigned to either intensive or conventional treatment groups "in balanced blocks of 20 by sealed opaque envelopes". Graded A. | Preference for delivery, mode of delivery, length of labour and pain relief in labour 100% follow‐up. Graded A. Depression, anxiety, concerns and satisfaction 20% or more. Graded D. | Not blinded for woman's preference for delivery as obstetrician responsible for providing intervention collected data at last antenatal visit. Graded B. |
Content
Content assessment was based three factors: the evidence base of the information provided; whether potential outcomes were included; and whether options were addressed.
Fraser 1997 reported that consensus panel recommendations and local centre data on vaginal birth after caesarean provided the basis for the information given to women. Although it was unclear whether potential harms were included in the information, alternatives in terms of pain relief and sterilisation were discussed.
Saisto 2001 based the intervention on psychotherapy, in the form of cognitive and behavioural exercises. Women were told about the pain relief alternatives available at the hospital, and about the pros and cons of vaginal and caesarean birth, but the evidence base, on which this information was based, was not reported.
Format
Both studies compared interventions that involved the provision of information through additional face‐to‐face contact and written material with control groups that received written material and standard treatment (Saisto 2001) or written material and standard antenatal care (Fraser 1997).
Both studies reported that those delivering the information had specific training prior to the commencement of the study.
Fraser 1997 based the intervention on a theoretical model of health promotion and focussed on each woman's needs.
Saisto 2001 used a conversational style and assisted women to review their experiences, feelings and misconceptions.
Context
The interventions used in both studies took place on more than one occasion and involved trained health professionals.
Fraser 1997 used research nurses experienced in antenatal education for both contacts and included a resource person selected for their communication skills and previous birth experiences in the second contact.
In Saisto 2001 an obstetrician who had completed courses in cognitive therapy and childbirth psychology provided the intervention in three additional 45‐minute antenatal appointments.
Other assessment criteria
Other aspects of the study were also graded in considering the quality of the study, although they were not used to exclude studies from the review. They were: consumer involvement and health professional involvement in the preparation of the information, potential for conflict of interest, and whether there had been an assessment of the agreement between clinical protocols and information given to study participants.
Consumer involvement in information preparation
In Fraser 1997 the intervention included contact with a resource person chosen for communication skills and personal experience of a vaginal birth after a caesarean delivery.
Saisto 2001 did not report any consumer input.
Health professional involvement in information preparation
Health professional involvement in the preparation of information was apparent in both studies.
in both contacts with the intervention group, Fraser 1997 involved research nurses with experience in antenatal education to give information and support.
Saisto 2001 involved an obstetrician to give information about cognitive and behavioural exercises, and a midwife to provide practical information about pain relief and labour interventions, although the involvement of the midwife in the preparation of the information is not clear.
Potential for assessor bias
Criteria for determining potential assessor bias were based on the researcher's relationship with the delivery of the intervention and assessment of study outcomes.
In Fraser 1997, researchers involved in the analysis did not participate in the intervention or control groups, either in the provision of information or clinical care, apart from the pre‐randomisation procedures involved in informed consent and the distribution of the baseline questionnaire.
In Saisto 2001, the principal researcher was the obstetrician who provided the intervention and assessed the primary outcome of request for caesarean birth at 38 weeks for the intervention group. Details about the timing and assessor of this outcome are not clear for the control group.
Agreement with clinical protocols
Neither study reported that there had been an attempt to assess whether the information given to women was consistent with the clinical situation they may face.
Fraser 1997 provided women with data about the probability of achieving a vaginal birth after a previous caesarean delivery at the centre where they planned to deliver, and discussed barriers to a vaginal birth that included "the views of treating obstetrician".
Saisto 2001 provided women with pain relief options "available at our hospital".
Effects of interventions
Two randomised controlled trials involving 1451 women met the inclusion criteria of this review. Both studies aimed to reduce caesarean births by encouraging women to attempt vaginal delivery. One used a program of prenatal education and support, and the other cognitive therapy to reduce fear. Results were not combined because of differences in the study populations. All women in the Fraser 1997 trial had a previous caesarean delivery whereas participants in the Saisto 2001 trial included women who had not previously given birth.
Non‐clinical outcomes were ascertained in both studies through questionnaires and were subject to rates of loss to follow‐up exceeding 10%. A range of clinical outcomes, extracted from hospital records, was reported by both studies.
(1) Knowledge or understanding
Neither study measured women's levels of knowledge or understanding of caesarean birth.
(2) Decisional conflict
Neither study measured decisional conflict.
(3) Women's perceptions
(a) Women's perception of participation in decision‐making or 'active say' Neither study assessed women's perception of participation in decision‐making about their caesarean birth. However Fraser 1997 sought women's views of the effect of taking part in the study on the ease of decision‐making about delivery. Women in the control group were more likely to indicate that participation in the trial had no effect on decision‐making (67% compared to 38%). Women in the intervention group were more likely to consider the decision to attempt vaginal birth easier than those in the control group (51% compared to 28%) or more difficult (10% compared to 6%). These results were subject to an attrition rate of 11%, and may be subject to bias. (b) Women's perception of ability to discuss care with clinicians or family/friends Neither study examined women's perception of ability to discuss care with clinicians or family/friends.
(c) Women's perception of whether information needs were met Neither study examined women's perception of whether their information needs were met.
(d) Women's perception of satisfaction with decision‐making Neither study examined women's perception of their satisfaction with decision‐making.
(4) Clinical outcomes
(a) Mode of delivery Both studies reported the number of caesarean and vaginal deliveries among both intervention and control groups. Data also reported were the number of women attempting vaginal delivery, and requesting or scheduling a caesarean delivery.
(i) Caesarean delivery Over 40% of all women gave birth by caesarean section, and the rate of caesarean delivery was not affected by giving women information to encourage them to attempt vaginal birth.
Fraser 1997 calculated its sample size to detect a reduction in the caesarean section rate to 30% but about half of all participants in the Fraser 1997 study delivered by caesarean birth, 47.1% of the intervention group (302/641), and 51.1% of the control group (324/634). The difference is not statistically different (RR 0.92; 95% CI 0.82 to 1.03).
Saisto 2001 hoped to reduce the caesarean section rate by 50% but there was no significant difference between the two groups. The caesarean birth rate was 43.5% in the intervention group (37/85) and 48.4% in the control group (44/91) (RR 0.90; 95% CI 0.65 to 1.24).
(ii) Vaginal birth More than half the women gave birth vaginally and there was no significant difference between intervention and control groups.
In Fraser 1997 there was no statistically significant difference between the intervention group (339/641 or 52.9%) and the control group (310/634 or 48.9%) (RR 1.08; 95% CI 0.97 to 1.21).
Over half of the participants in Saisto 2001 gave birth vaginally, 56.5% of the intervention group (48/85) and 51.6% of the control group (47/91). This difference is not statistically significant (RR 1.09; 95% CI 0.83 to 1.44).
(iii) Elective/scheduled caesarean More than one in five women elected or scheduled a caesarean delivery with no difference between the intervention and control groups.
Over 20% of women in Fraser 1997 scheduled a caesarean delivery, 21.4% of the intervention group (137/641) and 23.7% of the control group (150/634). The difference is not statistically significant (RR 0.90; 95% CI 0.74 to 1.11).
In Saisto 2001 the proportion of women who chose caesarean for psychosocial reasons was 23.5% in the intervention group (20/85) and 28.6% in the control group (26/91). This is not a statistically significant difference (RR 0.82; 95% CI 0.50 to 1.36).
(iv) Attempted vaginal delivery Vaginal delivery was attempted by about 70% of women in both intervention and control groups.
Fraser 1997 set pre‐determined criteria for assessing attempted vaginal delivery from medical records. An 'attempt' included at least one of the following: a vaginal birth; caesarean birth preceded by at least four hours of labour in hospital; or caesarean birth with less than four hours of labour in hospital but where there was an urgent indication for caesarean delivery. About 70% of women in each group attempted vaginal delivery (72.5% of the intervention group (465/641) and 69.4% of the control group (440/634)). This difference is not statistically different (RR 1.05; 95% CI 0.97 to 1.12).
In the Saisto 2001 study, over 70% of participants chose vaginal delivery, 76.4% of the intervention group (65/85) and 71.4% of the control group (65/91) (RR 1.07; 95% CI 0.90 to 1.28).
Both studies analysed mode of delivery by women's motivation to deliver vaginally, but the assessment used by Saisto 2001 is dubious and there were no results for over 20% of the study sample. Fraser 1997 found a significant difference in the proportion that scheduled caesarean section in both treatment groups when comparing high to low motivation (intervention group 12% and control group 13% compared to 44% and 49% respectively). The intervention had no affect on this outcome.
(b) Maternal morbidity Fraser 1997 assessed maternal morbidity: uterine rupture, hysterectomy, and blood transfusion. Data were not sufficient to compare intervention and control groups. Outcomes for both groups were similar. In the intervention or verbal group 8/642 women experienced uterine rupture or dehiscence compared to 6/634 women in the control group. There were no hysterectomies in the intervention group and two in the control group. Two women in the intervention group, and three in the control group, had blood transfusions.
(c) Neonatal mortality and morbidity Fraser 1997 only reported neonatal mortality and two measures of neonatal morbidity: Apgar score less than 7 at 5 minutes, and admission to Neonatal Intensive Care Unit. Data were not sufficient to compare groups. There were six perinatal deaths, two in the intervention group and four in the control group.
(5) Psychological outcomes
(a) Anxiety Saisto 2001 measured anxiety twice during pregnancy (at 24 weeks and 36 weeks) using a Pregnancy Anxiety Scale. Results were reported only graphically although the study authors state that there was no statistical significance between the intervention and control groups. The attrition rate exceeded 30% for both groups.
(b) Sense of control Fraser 1997 measured women's sense of control over the birth experience with an 18‐item Birth Experience Rating Scale (a shortened version of the Labor Agency Scale) 12 to 72 hours after birth. Results were similar for both groups with no statistically significant difference between them. The loss to follow‐up was greater than 10%.
(c) Depression Saisto 2001 measured depression, using a revised version of Beck's Depression Inventory, in pregnancy and three months postpartum. There was no statistically significant difference between the intervention and control groups in the puerperium but these results were subject to considerable loss to follow‐up (greater than 30%). Depression after birth was highest amongst those with earlier depression at both 24 and 36 weeks.
(6) Other outcomes
Saisto 2001 assessed additional outcomes not identified in the protocol for this review: concerns (using a revised version of Personal Concerns Scale) at 24 weeks and 36 weeks in pregnancy (no statistically significant difference) and an 8‐item assessment of satisfaction with childbirth made three months postpartum (no statistically significant difference). Saisto 2001 also reported two items in the Pregnancy Anxiety Scale separately, however outcomes were missing on these items for over 20% of participants at 24 weeks, and 30% of participants at 36 weeks and at three months postpartum.
Saisto 2001 reported two outcomes for women who gave birth vaginally: duration of labour for women and pain relief used. The authors state that there was no significant difference between the duration of labour prior to emergency caesarean but do not show data. Labour was shorter for the intervention group compared to the control group but there was no difference in the use of epidural analgesia.
Comparison of the studies
The two studies included in this review had similar aims for giving women information about caesarean birth: to reduce the caesarean delivery rate. However, the content of the information given to women was common in relation to pain relief options only. Without further information from the study authors, the results could not be combined, because Fraser 1997 comprised women who had previously delivered by caesarean, whereas about half the women in Saisto 2001 were pregnant for the first time. Neither study found a statistically significant difference between intervention and control groups for their primary outcome of mode of birth (caesarean delivery, vaginal delivery, elective or scheduled caesarean delivery or attempted vaginal delivery). Attrition introduced potential bias for other outcomes.
Adequacy of content
The intended purpose of the information used in both studies was similar. Both sought to reduce the caesarean birth rate, either by increasing the proportion of women attempting vaginal births after a previous caesarean delivery (Fraser 1997), or by reducing requests for caesarean among women judged to have a fear of childbirth (Saisto 2001). Consumer reviewers in the Cochrane Pregnancy and Childbirth Review Group Consumer Panel reviewed the descriptions of the information content. Consumers felt that information for women considering a vaginal birth after caesarean (VBAC) should also include: the risks of VBAC and elective caesarean; warning signs to be aware of in labour; information about the philosophy and policies of the hospital and staff; strategies to improve chances of a successful VBAC; and information about the probability of success with specific care givers.
In response to the description of information used in the study involving women who were fearful of childbirth (Saisto 2001), consumers said information given to women should include: the evidence base of practical information about pain relief and interventions; the specific risks and benefits of vaginal and caesarean birth; and the options for pain relief in labour.
Consumers were concerned that information‐giving should be interactive, and that women should be able to get more information if wanted.
Discussion
Despite the large increase in caesarean births over the past thirty years, the broad scope of information given to women about caesarean birth, and the incorporation of both non‐randomised controlled trials and controlled before‐and‐after studies in this review's inclusion criteria, our search yielded only three studies that assessed the impact of providing pregnant women with some form of information about caesarean birth. All were randomised controlled trials and one (Greene 1989) was excluded from the review.
The two included studies, Fraser 1997 and Saisto 2001, limit this current review to information designed to encourage women to attempt a vaginal delivery. The role of women in the decision to deliver by caesarean is not clear, however, although maternal demand for caesarean delivery appears to be uncommon in the absence of known clinical factors (Gamble 2000). The studies used different approaches to influence women's decisions about caesarean birth, and provided different types of information, but inadequacies in both studies mean that the evidence of the effects of giving women information about caesarean birth is inconclusive.
Neither intervention used in these trials made any difference to clinical outcomes. About 70% or more women attempted vaginal delivery in both trials, yet caesarean delivery rates exceeded 40%, a rate that was 10% higher than was hoped. There was no significant difference between control and intervention groups for any of the outcomes measured.
This review is unable to report on a number of important outcomes because they were not included in either study: knowledge or understanding; decisional conflict; and women's perceptions of: their ability to discuss care with clinicians or family/friends, whether information needs are met; and satisfaction with decision‐making.
There was no difference in the psychological outcomes for the intervention and control groups reported by either of the included trials although over 10% of participants were not included in these assessments. Fraser 1997 reported on sense of control, and Saisto 2001 reported anxiety and depression.
There is considerable variability in the outcomes measured in decision‐making studies (O'Connor 2002) and Bekker 1999 argues that research in this area should be theory driven. However, neither Fraser 1997 nor Saisto 2001 were explicit about the theoretical relationship of their information‐based interventions and the hypotheses they tested.
Fraser 1997 used a program of face‐to‐face prenatal education. It is based on the assumption that information can influence behaviour. Yet there was no assessment of participant knowledge, either before or after the intervention, so the effectiveness of the intervention in increasing women's knowledge is not known.
Saisto 2001 looked at whether additional sessions with an obstetrician trained in cognitive therapy to address fear of childbirth reduced requests for caesarean birth. There was no assessment of the impact of these sessions on fear of childbirth.
Neither Fraser 1997 nor Saisto 2001 found a statistically significant difference between the intervention and control groups for any study outcome. Unfortunately, neither study measured outcomes that would have provided a direct assessment of the effectiveness of the interventions they used. This makes interpretation of the results difficult. The interventions may not have been effective, or they may have been poorly implemented, or the theoretical assumptions upon which the studies are based may not hold. That is, increasing knowledge or reducing fear may not influence health behaviour around caesarean birth.
There are methodological concerns with Saisto 2001. First, women were diagnosed with fear of childbirth using a 10‐item questionnaire that required at least five positive responses or a positive response to a statement expressing preference for caesarean delivery. However there was no attempt to assess the accuracy of this instrument as a diagnostic tool by comparing results with those from other instruments. Second, there was no evidence of any assessment of women's reasons for preferring a caesarean birth. Therefore we do not know if the women who indicated a preference for caesarean were influenced by their obstetric history. Third, assumptions about women's motivation for treatment and confrontation of fears were based on their completion or otherwise of voluntary questionnaires. It is not clear how motivation was assessed when one or two of the three questionnaires were completed. Finally the credibility of some calculations is uncertain. The sample size calculations are based on the assumption that increasing the number of cognitive therapy sessions in pregnancy could halve the caesarean birth rate. Results for non‐clinical outcomes are reported as statistically significant yet the standard error is greater than the magnitude of the results (Saisto 2001).
The excluded trial, Greene 1989, evaluated the impact of giving information to women undergoing caesarean delivery. It described the procedures and physical experience of caesarean delivery on maternal anxiety, physiological distress, knowledge and recovery. The trial was excluded because data were not reported in a form that could be extracted, completeness of follow‐up could not be confirmed, and pre‐determined criteria for assessing the quality of the intervention were not met. Nevertheless this study reveals potential for further work in this area.
Research into the impact of strategies to inform women about caesarean birth has focussed on encouraging women to attempt vaginal delivery. Trials of interventions to encourage women to attempt vaginal birth were inconclusive, but both trials were flawed in design. Neither study included in this review showed that the type of information they provided to women affected outcomes, nor did they include outcomes to test their theoretical assumptions. These shortcomings mean that the evidence about the impact of these strategies is inconclusive.
This review is unable to report on a range of important outcomes.Further research on this topic is urgently needed.
Authors' conclusions
Implications for practice.
This systematic review provides no evidence for the withdrawal of routine information provision to women, for and about caesarean birth.
Implications for research.
Future research should consider the information needed by women who give birth by caesarean birth, how it could improve their experiences and outcomes, and what to expect after a caesarean birth.
Further research is needed on women's information needs when they are considering caesarean delivery as an option. Such research should consider the theoretical assumptions on which the intervention is based when considering the outcomes to be measured, and take into account women's views in the development of information for women.
What's new
| Date | Event | Description |
|---|---|---|
| 16 February 2011 | Amended | Information about the plans for the update of this review have been added to Published notes. |
History
Protocol first published: Issue 4, 2002 Review first published: Issue 1, 2004
| Date | Event | Description |
|---|---|---|
| 27 March 2008 | Amended | Converted to new review format. |
| 30 August 2003 | New citation required and conclusions have changed | Substantive amendment |
Notes
This review is being updated by two new reviews: 'Interventions for supporting women with decisions about a first caesarean delivery' and 'Interventions for supporting women with decisions about vaginal birth after caesarean delivery'. When the new reviews have been published, this review will be withdrawn.
Acknowledgements
We are grateful to Sophie Hill and other editors of the Cochrane Consumers and Communication Review Group, Review Group Coordinator Megan Prictor, anonymous external peer reviewers for the Review Group, Judy Stoelwinder for her expertise and assistance with the search strategy, Lynn Hampson and Anne Robinson for their help in conducting the searches, and participants in the Consumer Panel of the Cochrane Pregnancy and Childbirth Review Group: Susan Hodges, Henci Goer, Brigid Cumming, Kay Coppa and Cynthia Clarkson.
Data and analyses
Comparison 1. Verbal information plus pamphlet versus pamphlet only.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Caesarean delivery | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2 Vaginal birth | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Elective/scheduled caesarean | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Attempted vaginal delivery | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
1.1. Analysis.
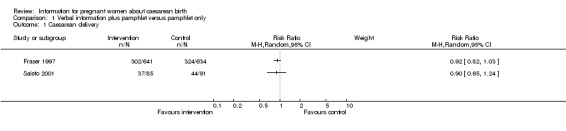
Comparison 1 Verbal information plus pamphlet versus pamphlet only, Outcome 1 Caesarean delivery.
1.2. Analysis.
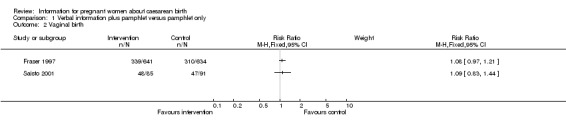
Comparison 1 Verbal information plus pamphlet versus pamphlet only, Outcome 2 Vaginal birth.
1.3. Analysis.
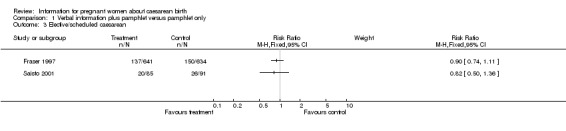
Comparison 1 Verbal information plus pamphlet versus pamphlet only, Outcome 3 Elective/scheduled caesarean.
1.4. Analysis.
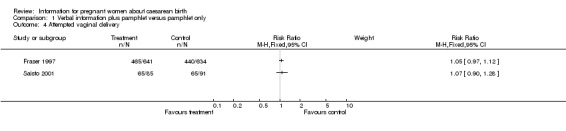
Comparison 1 Verbal information plus pamphlet versus pamphlet only, Outcome 4 Attempted vaginal delivery.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Fraser 1997.
| Methods | Multi‐centre randomised controlled trial to assess whether a prenatal education and support program promoting vaginal birth after caesarean delivery (VBAC) compared to a brief pamphlet increases probability of vaginal birth for women with a previous caesarean section. Women were identified through doctors' offices and hospital pre‐admission registries and randomly allocated to pamphlet (control), or program (intervention) group, by centralised telephone answering service blocked and stratified by hospital and woman's motivation to attempt VBAC. Follow‐up: Data extracted from medical records were complete (attempt at VBAC, mode of delivery, maternal morbidity, neonatal mortality and morbidity) for all participants. Data from the postnatal questionnaire was collected for 1135 women (89%) (women's sense of control and influence of study participation on ease of decision‐making). Blinding: Research nurse extracted data from hospital records after discharge. Informed consent: Yes. Time span of study: April 1992 to November 1994. Calculated sample size: 649 per group, 1298 total. Number approached: Not reported. Number of study participants: 1301 women randomised. Analysis on 1275 women. Number excluded after randomisation: 26 (1 randomised in error, 6 miscarried, 3 pregnancies terminated, 2 delivered before 24 weeks gestation, 1 withdrawal due to language difficulties, and 13 lost to follow up). Timing and frequency of intervention: First contact with nurse only, at randomisation (< 28 weeks). Second contact with nurse and resource person 4 to 8 weeks later. Analysis by intention to treat: Yes. Baseline assessment at randomisation: Questionnaire with 10.0cm visual analogue scale to indicate agreement or disagreement with statement "I plan to attempt a vaginal delivery in this pregnancy". Follow up assessment: Questionnaire 12 to 72 hours after delivery. Analysis: Effects of verbal program on rates of vaginal delivery and attempted vaginal delivery expressed as relative risks. Differences in mean scores on Birth Experience Rating Scale compared. Post hoc: Analysis of attempted vaginal delivery, vaginal delivery and scheduled caesarean birth by motivational strata. |
|
| Participants | Country: Canada and USA. Setting: 12 hospitals (11 Canadian and 1 USA) Description: Inclusion: Pregnant women with single previous low caesarean birth with gestational age <28 weeks at time of recruitment , with sufficient knowledge of English or French to complete questionnaire, and planning to give birth in a participating hospital. Exclusion: women with previous VBAC, classic caesarean or myomectomy scar, or known multiple pregnancy. N= 1275 Number program group: 641 Number pamphlet group: 634 Recruitment: Potential participants identified through doctors' offices and hospital pre‐admission registers. |
|
| Interventions | Purpose of intervention: to promote vaginal delivery after caesarean birth Control group ‐ Pamphlet group: received a brief pamphlet that outlined benefits of VBAC over elective repeat caesarean. Intervention group ‐ Program group: given same pamphlet and also offered a prenatal education and support program in the form of two contacts with a research nurse experienced in prenatal instruction and a resource person skilled in communication who had personal experience of VBAC. First contact with the nurse was at time of randomisation (that is before 28 weeks gestation). Second contact was with nurse and resource person 4 to 8 weeks later. Content of information: Pamphlet ‐ benefits of vaginal birth after caesarean section compared to repeat caesarean. Program ‐ assessment of motivation and perceptions of key people, including spouse and treating obstetrician. Consensus panel recommendations favouring vaginal birth; probability of success of vaginal birth in her centre; pain relief options in labour; alternative sterilisation options (if under consideration); identification of barriers to VBAC, including, when applicable, views of treating obstetrician. Program was individualized to the woman's situation and included peer support from the resource person. |
|
| Outcomes | Primary outcome: proportion of women achieving VBAC [from hospital records after discharge from hospital]. Proportion attempting VBAC defined as having met at least one of the following criteria: (a) vaginal delivery, (b) caesarean birth preceded by 4 or more hours of labour in hospital, (c) caesarean birth preceded by < 4 hours of labour in hospital but where there was an urgent indication of delivery [data from hospital records after discharge]. Maternal morbidity (uterine rupture or dehiscence, hysterectomy or blood transfusion) [from hospital records after discharge] neonatal mortality, neonatal morbidity (Apgar <7 at 5 minutes, and admission to NICU) [from hospital records after discharge]. Women's sense of control over birth experience [18 item Birth Experience Rating Scale, a shortened version of the Labor Agency Scale]. Women's views of effect of participation on ease of decision to attempt VBAC or choose elective delivery [post‐partum questionnaire distributed 12 to 72 hours after delivery]. |
|
| Notes | Program intervention comprised verbal information and support based on model of Green and Kreuter of health promotion‐disease prevention interventions. Green LW, Kreuter MW. Health promotion and planning: an educational and environmental approach. 2nd ed. Mountain View City (CA): Mayfield, 1991: 150‐87. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Saisto 2001.
| Methods | Randomised controlled trial to evaluate intensive treatment (intervention) group compared to conventional treatment (control) group to reduce requests for caesarean birth. Pregnant women randomly assigned to either
intensive (intervention) or conventional (control) treatment groups in balanced blocks of 20 by sealed opaque envelopes. Women were recruited at their first appointment following referral to an outpatient clinic at university teaching hospital after diagnosis of fear of vaginal delivery by a specific questionnaire. Allocation by sealed opaque envelopes. Follow‐up: Data extracted from medical records were complete (request for caesarean, mode of delivery, duration of labour and pain relief). Antenatal questionnaires at 24 and 36 weeks completed by 138 women (78.4%) and 116 (65.9%) respectively. Postnatal questionnaire completed by 110 women (62.5%). Assessor not blinded to woman's preference for delivery. Informed consent: Yes. Time span of study: August 1996 to July 1999. Calculated sample size: 74 per group. 148 total. Number approached: 176. Number of study participants: 176. Analysis on 176 women. 112 (64%) completed all 3 questionnaires. Number excluded: None. Timing and frequency of intervention: At 28, 32, 37 and 38 weeks of pregnancy. Analysis by intention to treat: Yes. Baseline assessment: Questionnaire at 24 weeks measuring anxiety, depression and concerns. Follow up assessment: Questionnaire 3 months after delivery. Post hoc analysis: Comparison of requests for caesareans and caesarean delivery by parity and non‐compliance (to complete questionnaire), and for caesarean request for women in intervention group who accepted the offer to visit with midwife compared to those who did not. Analysis of two items in Pregnancy Anxiety Scale was also reported: Q4 fear of pain in labour and Q9 fear of the obstetrician's unfriendly behaviour. |
|
| Participants | Country: Finland. Setting: outpatient clinic at university hospital. Description: Inclusion: Physically healthy pregnant women with low obstetric risk with a diagnosis of fear of childbirth by a 10‐item questionnaire based on either five or more positive responses or positive response to one item "do you prefer a cesarean to an ordinary delivery?" Exclusion: Contraindication to vaginal delivery at time of randomisation (two previous caesareans or vertical incision in previous caesarean). N= 176 (90 primiparous, 86 parous). Intervention group: 85 (44 primiparous). Control group: 91 (46 primiparous). Post hoc: Women who did not complete voluntary questionnaires, or who did not take up offer of visit with midwife were compared to those that did. Completion or otherwise of questionnaire was considered to be indication of motivation for treatment and confrontation of her fears. |
|
| Interventions | Purpose of intervention: to reduce requests for caesarean birth Control group: conventional treatment comprising standard information provision at 24 weeks about pros and cons of vaginal delivery versus caesarean and pain relief available in hospital, and 45 minute appointment with obstetrician trained in cognitive therapy and childbirth psychology at 24 weeks and 36 weeks. Intervention group: Intensive group received three additional 45 minute appointments with obstetrician with training in cognitive therapy and childbirth psychology to discuss feelings, experiences and misconceptions plus option of 90 minute appointment with midwife to discuss practical information about pain relief and possible interventions, encouragement to visit obstetric ward and telephone access to obstetrician and midwife. |
|
| Outcomes | Requests for caesarean delivery (women asked at 38 weeks pregnancy at last prenatal visit). Mode of delivery, duration of labour and pain relief (from medical records). Anxiety using Pregnancy Anxiety Scale (at 24 weeks and 36 weeks pregnancy). Depression (using revised version of Beck's Depression Inventory at 24 weeks and 36 weeks pregnancy) and Concerns (using revised version of Personal Concerns Scale at 24 weeks and 36 weeks pregnancy). Postnatal questionnaire was "similar to those used in pregnancy" but combined with obstetric data and eight questions about satisfaction with childbirth (positive or painful experience, sufficient pain relief, support from partner and staff, feeling safe, ability to influence treatment). Post hoc: Analysis of two items in Pregnancy Anxiety Scale was reported: Q4 fear of pain in labour and Q9 fear of the obstetrician's unfriendly behaviour. |
|
| Notes | All data available on request for caesarean, and data from hospital records. All questionnaires not completed by nearly 40% of women. Frequency of mention of birth‐related concerns was reported for first questionnaire but change over pregnancy was reported only graphically. Change in anxiety for both groups was reported to be not statistically significant but data were reported graphically only. Mean score of experience of childbirth was reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Fawcett 1993 | There was no random or quasi‐random allocation to intervention or control groups. Approximately one half of the control treatment group were recruited retrospectively. All other study participants were recruited prospectively. Attrition resulted in more than 20% of participants being lost to follow up. |
| Greene 1989 | This randomised controlled trial was excluded because data were not reported in a form that could be extracted, and completeness of follow‐up could not be confirmed. Pre‐determined criteria for assessing the quality of the intervention were not met. The evidence base, potential harms and benefits, and options were not addressed in the information given to the women in the study. The study evaluated the impact of giving women sensory information about caesarean birth on their prenatal maternal anxiety and on their recovery after a caesarean birth. |
| Kropp 1989 | There was no randomisation or control group. Sixty‐one pregnant women whose babies were in a breech position completed questionnaires about the information they were given, their satisfaction with it and the influence of their doctor on the decision, for either external version (41) or elective caesarean (20). |
Differences between protocol and review
The title of the protocol for this review was "Information for women about caesarean birth".
Contributions of authors
DH conceived and designed the review.
DH JW and HR all contributed to the preparation of the protocol. DH prepared the first draft of the protocol and incorporated additional input from JW and HR. All approved the protocol for submission.
DH and JW extracted data for the review. DH prepared the review with additional input from JW.
Sources of support
Internal sources
No sources of support supplied
External sources
Bursary, Cochrane Consumers and Communication Review Group, La Trobe University, Australia.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Fraser 1997 {published data only}
- Fraser W, Maunsell E, Hodnett E, Moutquin JM. Randomized controlled trial of a prenatal vaginal birth after cesarean section education and support program. American Journal of Gynecology and Obstetrics 1994;176(2):419‐25. [DOI] [PubMed] [Google Scholar]
Saisto 2001 {published data only}
- Saisto T, Salmela‐Aro K, Nurmi JE, Kononen T, Halmesmaki E. A randomized controlled trial of intervention in fear of childbirth. Obstetrics & Gynecology 2001;98(5):820‐6. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Fawcett 1993 {published data only}
- Fawcett J, Pollio N, Tully A, Baron M, Henklein JC, Jones RC. Effects of information on adaption to cesarean birth. Nursing Research 1993;42(1):49‐53. [PubMed] [Google Scholar]
Greene 1989 {published data only}
- Greene PG, Zeichner A, Roberts NL, Callahan EJ, Granados JL. Preparation for cesarean delivery: a multicomponent analysis of treatment outcome. Journal of Consulting & Clinical Psychology 1989;57:484‐7. [DOI] [PubMed] [Google Scholar]
Kropp 1989 {published data only}
- Kropp S, Schmidt S, Saling E. Influences on decisions of pregnant patients with breech presentation for external fetal version or cesarean section ‐ information status and anxiety pattern [Einflusse auf Entscheidungen von Schwangeren mit BEL zur ausseren Wendung oder zur Schnittentbindung‐Aufklarungsstatus and Angstmuster.]. Zeitschrift fur Geburtshilfe und Perinatologie 1989;193(2):84‐91. [PubMed] [Google Scholar]
Additional references
Bamigboye 2003
- Bamigboye AA, Hofmeyr GJ. Closure versus non‐closure of the peritoneum at caesarean section. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD000163] [DOI] [PubMed] [Google Scholar]
Bekker 1999
- Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al. Informed decision making: an annotated bibliography and systematic review. Health Technology Assessment 1999;3(1):1‐156. [PubMed] [Google Scholar]
Brown 1993
- Brown S, Lumley J. Antenatal care: a case of the inverse care law?. Australian Journal of Public Health 1993;17(2):95‐103. [DOI] [PubMed] [Google Scholar]
Butow 1998
- Butow P, Brindle E, McConnell D, Boakes R, Tattersall M. Information booklets about cancer: factors influencing patient satisfaction and utilization. Patient Education and Counseling 1998;33(2):129‐41. [DOI] [PubMed] [Google Scholar]
Callister 1995
- Callister LC. Beliefs and perceptions of childbearing women choosing different primary health care providers. Clinical Nursing Research 1995;4(2):168‐80. [DOI] [PubMed] [Google Scholar]
Charles 1999
- Charles C, Gafni A, Whelan T. Decision‐making in the physician‐patient encounter: revisiting the shared treatment decision‐making model. Social Science & Medicine 1999;49(5):651‐61. [DOI] [PubMed] [Google Scholar]
Clarke 2000 [Computer program]
- Clarke M, Oxman AD, editors. Cochrane Reviewers’ Handbook 4.1 [updated June 2000]. In: Review Manager (RevMan). Version 4.1. Oxford: The Cochrane Collaboration, 2000.
Coulter 1999
- Coulter A, Entwistle V, Gilbert D. Sharing decisions with patients: is the information good enough?. British Medical Journal 1999;318(7179):318‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Creedy 2001
- Creedy DK, Noy DL. Postdischarge surveillance after cesarean section. Birth 2001;28(4):264‐9. [DOI] [PubMed] [Google Scholar]
Domenighetti 2000
- Domenighetti G, Grilli R, Maggi JR. Does provision of an evidence‐based information change public willingness to accept screening tests?. Health Expectations 2000;3(2):145‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edwards 2002
- Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ 2002;324(7341):827‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Entwistle 1998
- Entwistle VA, Sheldon TA, Sowden A, Watt IS. Evidence‐informed patient choice: practical issues of involving patients in decisions about health care technologies. International Journal of Technology Assessment in Health Care 1998;14(2):212‐25. [DOI] [PubMed] [Google Scholar]
EPOC 1998
- Effective Practice and Organisation of Care Collaborative Review Group. The Data Collection Checklist. Revised by Claire Allen, 1998.
Freda 1993
- Freda MC, Andersen HF, Damus K, Merkatz IR. What pregnant women want to know: a comparison of client and provider perceptions. Journal of Obstetric, Gynecologic, & Neonatal Nursing 1993;22(3):237‐44. [DOI] [PubMed] [Google Scholar]
Gamble 2000
- Gamble JA, Creedy DK. Women's request for a cesarean section: a critique of the literature. Birth 2000;27(4):256‐63. [DOI] [PubMed] [Google Scholar]
Gamble 2001
- Gamble JA, Creedy DK. Women's preference for a cesarean section: incidence and associated factors. Birth 2001;28(2):101‐10. [DOI] [PubMed] [Google Scholar]
Garrud 2001
- Garrud P, Wood M, Stainsby L. Impact of risk information in a patient education leaflet. Patient Education and Counseling 2001;43(3):301‐4. [DOI] [PubMed] [Google Scholar]
Graham 1999
- Graham WJ, Hundley V, McCheyne AL, Hall MH, Gurney E, Milne J. An investigation of women's involvement in the decision to deliver by caesarean section. British Journal of Obstetrics and Gynaecology 1999;106(3):213‐20. [DOI] [PubMed] [Google Scholar]
Hopkins 1999
- Hopkins L, Smaill F. Antibiotic prophylaxis regimens and drugs for cesarean section. Cochrane Database of Systematic Reviews 1999, Issue 2. [DOI: 10.1002/14651858.CD001136] [DOI] [PubMed] [Google Scholar]
Johanson 2002
- Johanson R, Newburn M, McFarlane A. Has the medicalisation of childbirth gone too far?. BMJ 2002;324(7342):892‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lydon‐Rochelle 2000
- Lydon‐Rochelle M, Holt VL, Martin DP, Easterling TR. Association between method of delivery and maternal rehospitalization. JAMA 2000;283(18):2411‐6. [DOI] [PubMed] [Google Scholar]
Mangesi 2002
- Mangesi L, Hofmeyr GJ. Early compared with delayed oral fluids and food after caesarean section. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD003516] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mould 1996
- Mould TA, Chong S, Spencer JA, Gallivan S. Women's involvement with the decision preceding their caesarean section and their degree of satisfaction. British Journal of Obstetrics and Gynaecology 1996;103(11):1074‐7. [DOI] [PubMed] [Google Scholar]
Nassar 2001
- Nassar N, Sullivan EA. Australia's Mothers and Babies 1999. Sydney: AIHW National Perinatal Statistics Unit (Perinatal Statistics Series No. 11), 2001. [Google Scholar]
O'Connor 2002
- O'Connor AM, Stacey D, Rovner D, Holmes‐Rovner M, Tetroe J, Llewellyn‐Thomas H, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD001431] [DOI] [PubMed] [Google Scholar]
Potter 2001
- Potter JE, Berquo E, Perpetuo IHO, Leal OF, Hopkins K, Souza MR, et al. Unwanted caesarean sections among public and private patients in Brazil: prospective study. BMJ 2001;323(7322):1155‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Quinlivan 1999
- Quinlivan JA, Petersen RW, Nichols CN. Patient preference the leading indication for elective caesarean section in public patients ‐ results of a 2‐year prospective audit in a teaching hospital. Australian and New Zealand Journal of Obstetrics and Gynaecology 1999;39(2):207‐14. [DOI] [PubMed] [Google Scholar]
Robinson 2001
- Robinson A, Thomson R. Variability in patient preferences for participating in medical decision making: implication for the use of decision support tools. Quality in Health Care 2001;10(Suppl 1):i34‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryding 1993
- Ryding EL. Investigation of 33 women who demanded a cesarean section for personal reasons. Acta Obstetricia et Gynecologica Scandinavica 1993;72(4):280‐5. [DOI] [PubMed] [Google Scholar]
Shepperd 1997
- Shepperd S. DISCERN: an instrument for judging the quality of written consumer information on treatment choices. Oxford: University of Oxford, 1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shorten 2003
- Shorten A, Chamberlain M, Shorten B, Kariminia A. Making choices for childbirth: development and testing of a decision‐aid for women who have experienced previous caesarean. Patient Education and Counseling 2003;52(3):307‐13. [DOI: 10.1016/S0738-3991(03)00106-X] [DOI] [PubMed] [Google Scholar]
Silburn 2000
- Silburn K. Communicating with consumers: good practice guide to providing information. Melbourne: Department of Human Services, 2000. [Google Scholar]
Sjogren 1997
- Sjogren B, Thomassen P. Obstetric outcome in 100 women with severe anxiety over childbirth. Acta Obstetricia et Gynecologica Scandinavica 1997;76(10):948‐52. [DOI] [PubMed] [Google Scholar]
Smaill 2002
- Smaill F, Hofmeyr GJ. Antibiotic prophylaxis for cesarean section (Cochrane Review). Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD000933] [DOI] [PubMed] [Google Scholar]
Stapleton 2002
- Stapleton H, Kirkham M, Thomas G. Qualitative study of evidence based leaflets in maternity care. British Medical Journal 2002;324:639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2001
- Thomas J, Paranjothy S, Royal College of Obstetricians and Gynaecologists Clinical Effectiveness Support Unit. National Sentinel Caesarean Section Audit Report. RCOG Press, 2001. [Google Scholar]
Thompson 2002
- Thompson J, Roberts CL, Currie M, Ellwood DA. Prevalence and persistence of health problems after childbrith: associations with parity and method of birth. Birth 2002;29(2):83‐94. [DOI] [PubMed] [Google Scholar]
Tito 1995
- Commonwealth Department of Human Services and Health. Review of professional indemnity arrangements for health care professionals (Tito F, chair). Compensation and professional indemnity in health care: a final report. Canberra: Australian Government Publishing Service, 1995. [Google Scholar]
Turnbull 1999
- Turnbull DA, Wilkinson C, Yaser A, Carty V, Svigos JM, Robinson JS. Women's role and satisfaction in the decision to have a caesarian section. Medical Journal of Australia 1999;170(12):580‐3. [DOI] [PubMed] [Google Scholar]
Wilkinson 2002
- Wilkinson C, Enkin MW. Absorbable staples for uterine incision at caesarean section. Cochrane Database of Systematic Reviews 1996, Issue 1. [DOI: 10.1002/14651858.CD000005] [DOI] [PubMed] [Google Scholar]
Zib 1999
- Zib M, Lim L, Walters WA. Symptoms during normal pregnancy: a prospective controlled study. Australian and New Zealand Journal of Obstetrics and Gynaecology 1999;39(4):401‐10. [DOI] [PubMed] [Google Scholar]


