Abstract
Berberine is a natural alkaloid used to improve glycemia but displays poor bioavailability and increased rates of gastrointestinal distress at higher doses. Recently, dihydroberberine has been developed to combat these challenges. This study was designed to determine the rate and extent to which berberine appeared in human plasma after oral ingestion of a 500 mg dose of berberine (B500) or 100 mg and 200 mg doses of dihydroberberine (D100 and D200). In a randomized, double-blind, crossover fashion, five males (26 ± 2.6 years; 184.2 ± 11.6 cm; 91.8 ± 10.1 kg; 17.1 ± 3.5% fat) completed a four-dose supplementation protocol of placebo (PLA), B500, D100, and D200. The day prior to their scheduled visit, participants ingested three separate doses with breakfast, lunch, and dinner. Participants fasted overnight (8–10 h) and consumed their fourth dose with a standardized test meal (30 g glucose solution, 3 slices white bread) after arrival. Venous blood samples were collected 0, 20, 40, 60, 90, and 120 minutes (min) after ingestion and analyzed for BBR, glucose, and insulin. Peak concentration (CMax) and area under the curve (AUC) were calculated for all variables. Baseline berberine levels were different between groups (p = 0.006), with pairwise comparisons indicating that baseline levels of PLA and B500 were different than D100. Berberine CMax tended to be different (p = 0.06) between all conditions. Specifically, the observed CMax for D100 (3.76 ± 1.4 ng/mL) was different than PLA (0.22 ± 0.18 ng/mL, p = 0.005) and B500 (0.4 ± 0.17 ng/mL, p = 0.005). CMax for D200 (12.0 ± 10.1 ng/mL) tended (p = 0.06) to be different than B500. No difference in CMax was found between D100 and D200 (p = 0.11). Significant differences in berberine AUC were found between D100 (284.4 ± 115.9 ng/mL × 120 min) and PLA (20.2 ± 16.2 ng/mL × 120 min, p = 0.007) and between D100 and B500 (42.3 ± 17.6 ng/mL × 120 min, p = 0.04). Significant differences in D100 BBR AUC (284.4 ± 115.9 ng/mL×120 min) were found between PLA (20.2 ± 16.2 ng/mL × 120 min, p = 0.042) and B500 (42.3 ± 17.6 ng/mL × 120 min, p = 0.045). Berberine AUC values between D100 and D200 tended (p = 0.073) to be different. No significant differences in the levels of glucose (p = 0.97) and insulin (p = 0.24) were observed across the study protocol. These results provide preliminary evidence that four doses of a 100 mg dose of dihydroberberine and 200 mg dose of dihydroberberine produce significantly greater concentrations of plasma berberine across of two-hour measurement window when compared to a 500 mg dose of berberine or a placebo. The lack of observed changes in glucose and insulin were likely due to the short duration of supplementation and insulin responsive nature of study participants. Follow-up efficacy studies on glucose and insulin changes should be completed to assess the impact of berberine and dihydroberberine supplementation in overweight, glucose intolerant populations.
Keywords: absorption, safety, plants, glucose, insulin
1. Introduction
Berberine is an isoquinoline derivative alkaloid present in various parts (root, stem, fruit, bark) of multiple plants including, in particular, species found in the Coptis, Hydrastis, and Berberis genus [1]. Various animal and culture models have reported on the ability of berberine to exert lipid and glucose-lowering effects in addition to helping with weight loss and improving glucose tolerance [2,3]. For this reason, interest in berberine has suggested it may be beneficial in treating diabetes and obesity. While still being fully characterized, mechanistic actions of berberine consist of it reducing blood lipid levels via action on hepatocyte nuclear factor 1 alpha (HNF-1 alpha) and hepatic LDL receptors, intestinal absorption of cholesterol [4], and glucose levels while increasing insulin sensitivity.
Moreover, berberine is a known activator of AMP Kinase [1,5], which contributes to increases in fatty acid oxidation and a reduction of lipogenic gene expression.
Yin and colleagues [6] published results from two separate studies that both examined the impact of berberine at improving various biomarkers associated with glucose homeostasis. Throughout the first study, berberine (500 mg/dose, 3 doses/day) or metformin was administered over a 3-month period to 36 adults who were recently diagnosed with type 2 diabetes. Levels of hemoglobin A1C, fasting blood glucose, postprandial blood glucose, and triglycerides were all significantly improved in comparison to pre-treatment, and, importantly, the magnitude of changes was similar to what was observed with metformin. An additional investigation was reported where berberine was added to the established treatment plan 48 type 2 diabetes patients. Over a 13-week period, blood glucose (both fasting and postprandial), hemoglobin A1C, fasting, insulin, and HOMA-IR were all improved when berberine was added. These results align with the Perez-Rubio et al. [7] investigation that reported improvements in waist circumference, blood pressure, triglycerides, and area under the curve values for both glucose and insulin (after a 75-g glucose load over a two-hour period) in 24 patients with metabolic syndrome. In this study, berberine was randomly assigned in a double-blind, placebo-controlled fashion at a daily dosage of 1500 mg/day (500 mg/dose, 3 doses/day with meals) for three months. Similar outcomes using berberine have been reported by Rao et al. [8] after completing a randomized, open-label study on 41 diabetic patients where various indicators of glucose and insulin metabolism were improved over the three-month study period.
One challenge associated with oral ingestion of berberine has been its low bioavailability (<1%) reported in both animal [9,10] and human models largely due to poor intestinal absorption and high levels of first-pass removal in the intestines and liver [5]. To overcome this limitation, higher doses of berberine are commonly administered, which has led to a consistent reporting of gastrointestinal adverse events. For example, Yin et al. [6] reported that gastrointestinal adverse events were 34.5% during a 13-week study which provided berberine hydrochloride as a monotherapy or in combination with other treatments. Interestingly all adverse events were reported when berberine was combined with other treatments (metformin, insulin, etc.) and all incidents occurred during the first four weeks of treatment.
For this reason, alternative approaches have been explored to help improve its poor bioavailability. For example, techniques such as encapsulation [11,12], packaging with other nutrients and compounds [13], and spray drying [14] have all been reported on in the literature. In addition, the reduced derivative of berberine, dihydroberberine, has been suggested as a natural alternative to improve bioavailability [15]. Buchanan and investigators [16] examined the ability of transdermal application of dihydroberberine in 40 Sprague-Dawley rats to improve bioavailability, improve glucose homeostasis parameters, and reduce adverse events in comparison to oral berberine gavage and transdermal applications of berberine. Results from both acute and chronic (14 days) pharmacokinetic approaches indicated that transdermal dihydroberberine achieved higher bioavailability than both transdermal and oral berberine administration. Oral administration of dihydroberberine has yet to be reported in human literature, thus initial studies should provide some level of insight into its impact on absorption kinetics, preliminary safety indicators, and adverse events associated with its ingestion. Consequently, the purpose of this study was to conduct a randomized, double-blind, placebo-controlled investigation to examine the dose-dependent impact on absorption kinetics, clinical safety parameters, and adverse events of oral dihydroberberine ingestion in humans.
2. Methods
2.1. Overview of Research Design
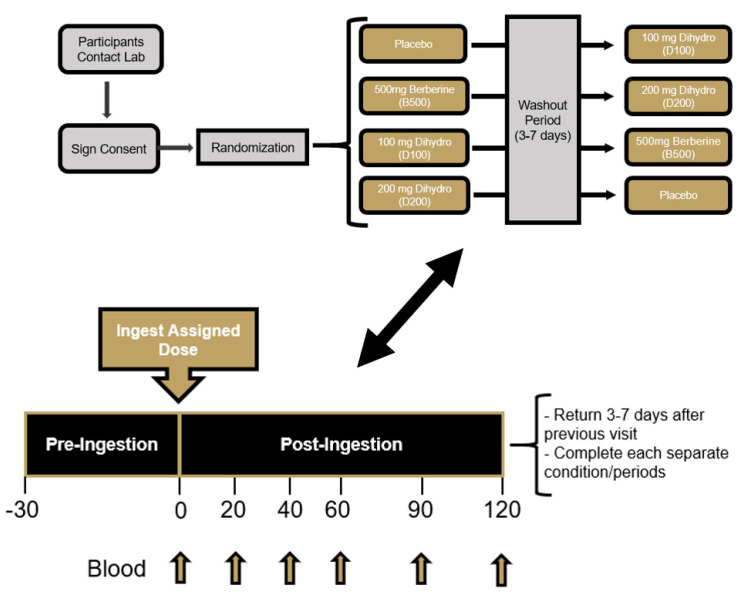
This study was completed using a randomized, double-blind, crossover study design. Prior to beginning, all participants signed an IRB-approved informed consent document (Lindenwood University: IRB-20-173, approval date: 22 June 2020) and completed a healthy history questionnaire to determine study eligibility. A power analysis was not computed as this study was considered a proof of concept, pilot investigation. This study protocol and design was retrospectively registered on Clinicaltrials.gov on 25 August 2021 as NCT05021341 (https://clinicaltrials.gov/ct2/show/NCT05021341 accessed on 24 December 2021). All four supplementation conditions were completed by each participant in a crossover fashion with a minimum washout of 72 h. For each supplementation condition, four total doses were consumed with three doses being consumed the day before testing (with breakfast, lunch, and dinner) and the fourth dose being consumed the morning of testing with a standardized test meal after observing an overnight (8 to 10 h) fast (Figure 1). Participants were scheduled to begin each visit at approximately the same times and reported to the laboratory between 600 and 1000 h. Using a randomized, double-blind, placebo-controlled fashion, study participants consumed either a placebo (resistance dextrin) (PLA), 500 mg of berberine (B500), 100 mg dihydroberberine (D100), or 200 mg dihydroberberine (D200). To minimize any order effects from testing, participants were randomized using an online randomization software program (www.random.org accessed on 1 July 2020). Upon arrival for each study visit, participants had their height, body mass, body composition, and hemodynamics (resting heart rate and blood pressure) measured along with an assessment of capillary glucose levels approximately 30 min prior to supplementation ingestion to evaluate fasting status. An indwelling catheter was then implanted into a forearm vein and flushed with saline to remain patent. The fourth and final dose of their assigned supplement was then consumed with 240 milliliters of cold tap water. After supplement ingestion, participants consumed a standardized test meal consisting of a 30-g glucose solution and four slices of white bread. Immediately after ingestion of the test meal, venous blood samples were collected 20, 40, 60, 90, and 120 min (Figure 2). Participants were provided 200 mL of cold water to ingest after each blood collection. Upon processing, all blood samples were stored at −80 °C. Throughout each visit, study participants were asked to report the occurrence of any adverse events (dizziness, headache, nausea, upset stomach, cramping, diarrhea, etc.) that occur throughout completion of the study protocol. All subsequent study visits were completed in an identical fashion and scheduled with at least 72 h between visits.
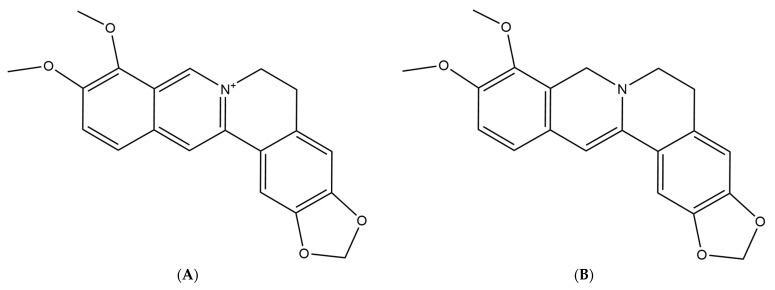
Figure 1.
(A) Chemical structure of berberine. (B) Chemical structure of dihydroberberine.
Figure 2.
Overview of research design.
2.2. Study Participants
Prior to participation, all recruited individuals provided signed informed consent using an IRB-approved consent form (Lindenwood University: IRB-20-173, approval date: 22 June 2020). Five healthy males (26.0 ± 2.6 years, 184.2 ± 11.6 cm, 91.8 ± 10.1 kg, 17.1 ± 3.5% fat) successfully completed all study visits (see Table 1 for full participant characteristics). Inclusion criteria included age (18–45 years), healthy and free of disease (as reported by the health screening questionnaire), and physically active (reported at least 30 min of moderate exercise three days a week). Any individual diagnosed with or being treated for cardiac, respiratory, circulatory, musculoskeletal, metabolic, obesity (defined as body mass index > 30 kg/m2 and body fat greater than 30%), immune, autoimmune, psychiatric, hematological, neurological, or endocrinological disorder or disease were not allowed to participate in the current study. Any participant taking any dietary supplement besides a multi-vitamin/mineral or a protein supplement were required to abstain from consuming any further doses for 30 days prior to beginning the study protocol.
Table 1.
Baseline age, gender, height (cm), weight (kg), body mass index, % fat, heart rate, systolic blood pressure, diastolic blood press, energy, carbohydrates, proteins, and fat intake.
| Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|
| Age | 26.0 | 2.6 | 23 | 30 |
| Height (cm) | 184.2 | 11.6 | 171 | 202 |
| Weight (kg) | 91.8 | 10.1 | 82.4 | 108.5 |
| Body mass index (kg/m2) | 27.1 | 3.9 | 22.6 | 33.1 |
| % fat | 17.1 | 3.5 | 12.5 | 20.9 |
| Heart rate (beats/minute) | 61.0 | 12.0 | 41 | 70 |
| Systolic blood pressure (mm Hg) | 122.3 | 11.4 | 111 | 138 |
| Diastolic blood pressure (mm Hg) | 72.4 | 8.8 | 64 | 70 |
| Energy intake (kcals/day) | 2433 | 810 | 1503 | 3695 |
| Carbohydrate intake (grams/day) | 217 | 62 | 144 | 312 |
| Protein intake (grams/day) | 121 | 34 | 66 | 153 |
| Fat intake (grams/day) | 112 | 45 | 75 | 186 |
2.3. Supplementation Protocol
Using a randomized, double-blind, placebo-controlled fashion, study participants consumed either a placebo (resistance dextrin) (PLA), 500 mg of berberine (B500), 100 mg dihydroberberine (D100), or 200 mg dihydroberberine (D200). The dihydroberberine was manufactured by NNB Nutrition (Nanjing, China) and is marketed as Glucovantage®. Berberine (≥99%) was extracted from Berberis Aristata in the hydrochloride form and was used as raw material. Dihydroberberine was obtained by a patented preparation method (CN108997332A). Neither molecule contains any crystalline water. Study participants supplemented consumed four total doses prior to having the absorption kinetics determined. This regimen started the morning before their scheduled visit with participants consuming one dose each with breakfast, lunch, and dinner. In addition to consuming with a meal, all doses were consumed with at least eight fluid ounces of cold tap water. Participants were then required to follow an overnight fast (approximately 8 to 10 h). Upon arrival, capillary glucose levels were determined from a finger-stick blood sample and a handheld glucose monitor (CVS Health Advanced Glucose Monitor, Agamatrix, Inc., Salem, NH, USA). After fasting status was confirmed, the fourth and final dose of their assigned supplement was consumed in front of a study team member with approximately eight fluid ounces of cold tap water. A catheter was then inserted into a forearm vein and approximately 30 min after consuming their final dose a standardized test meal was ingested which consisted of four slices of white bread (approximately 264 kcals, 3.2 g of fat, 50.6 g of carbohydrates and 7.6 g of protein) and 30 g of glucose powder that was mixed with approximately 8–12 fluid ounces of water. The test meal was ingested within five minutes. The ingestion of the test meal was considered to be the 0-min time point and all subsequent measurements occurred as outlined.
All participants were required to complete a supplementation log to document when each dose was consumed. No doses were reported being missed by any participant throughout the study protocol. All study materials were prepared into gelatin capsules of identical size, color, shape, and transparency. All doses were prepared into a single capsule which required each participant to consume a single capsule for each required dose. A resistant dextrin was used as the placebo. All doses were placed into individually labeled bags for each condition for each participant throughout the entire study protocol.
2.4. Procedures
2.4.1. Baseline Demographics and Hemodynamics
During the initial visit, after providing written consent, participants were instructed to rest quietly for approximately 10 min before measuring resting heart rate and blood pressure. Resting heart rate was measured by palpating the radial artery for a period of 60 s. While still resting, blood pressure (Omron BP785, Omron Corporation, Kyoto, Japan) measurements were taken before participants resumed normal activity. Participants then had their body mass determined (Tanita BWB-627A, Tokyo, Japan) and recorded to the nearest ±0.1 kg upon arrival prior to each study visit. All recorded body masses were compared to ensure the participant was weight stable. Any participant whose body mass changed by more than 2% between consecutive study visits was excluded from participation. Following body mass measurements, height was measured using a standard wall-mounted stadiometer (Tanita, HR-200, Tokyo, Japan) and recorded to the nearest ±0.5 cm (cm). Fat and fat-free mass was determined using a bioelectrical impedance analyzer (InBody 570, Beverly Hills, CA, USA). Participants were required to observe an overnight fast to ensure an accurate determination of body composition. Body composition analysis occurred between 600 and 1000 h by trained research personnel. All assessments were completed according to device specifications.
2.4.2. Dietary Monitoring
Prior to their baseline visit, study participants completed a hand-written four-day food record (three weekdays and one weekend day). The four-day food log was provided to allow participants to replicate their diets. In addition to the four-day food log, participants were instructed on how to complete the ASA24 online dietary assessment tool (https://epi.grants.cancer.gov/asa24/ accessed on 23 December 2021), for determination of baseline caloric and macronutrient intake. From this information, study participants were asked to replicate their dietary intake prior to each subsequent testing visit. Study participants reported 100% compliance to this protocol.
2.4.3. Venous Blood Collection and Processing
To confirm a fasting state prior to catheter insertion and supplement administration, capillary blood was collected from a finger on their non-dominant hand. The collected blood was analyzed using a hand-held glucose analyzer (CVS Health Advanced Glucose Monitor, Agamatrix, Inc., Salem, NH, USA). Fasting was confirmed if glucose was <110 mg/dL. Within each supplementation condition, study participants had their venous blood collected on six different occasions: 0, 20, 40, 60, 90, and 120 min after ingestion of their assigned study agent. Blood was collected via a forearm vein using standard phlebotomy techniques into serum and ethylenediaminetetraacetic acid EDTA-coated Vacutainer™ tubes. To establish safety, whole blood samples were collected into EDTA and serum tubes for assessment of complete blood count and comprehensive metabolic count, respectively. Blood samples collected into EDTA were gently inverted ten times while blood samples collected into serum tubes were gently inverted ten times and allowed to clot at room temperature. For same day analysis, these samples were placed into a chilled container and sent to a commercial diagnostic laboratory (Quest Diagnostics). Plasma samples used for berberine determination were collected into EDTA tubes, gently inverted ten times and centrifuged at 3000 revolutions per minute (rpm) (MegaFuge XFR, Thermo Fisher Scientific, Waltham, MA, USA) at 4 °C for 20 min. After centrifugation, 400 μL aliquots of plasma were removed and frozen at −80 °C within four hours of collection.
2.4.4. Complete Blood Count
To assess adverse events reported in response to the assigned supplementation, whole blood samples were collected in EDTA tubes and analyzed at a commercial diagnostic laboratory (Quest Diagnostics) for changes in red blood cell count, white blood cell count, platelet count, hemoglobin, hematocrit, red blood cell dimension width (RDW), mean corpuscle volume (MCV), mean corpuscle hemoglobin (MCH), mean corpuscle hemoglobin content (MCHC), neutrophil % and cell count, lymphocytes % and cell count, monocytes % and cell count, eosinophils % and cell count, and basophils % and cell count (granulocytes → neutrophils, eosinophils, basophils). Complete blood counts were only assessed at the 0 and 120-min time points.
2.4.5. Comprehensive Metabolic Panel
To assess adverse events in response to the assigned supplementation, serum samples were assayed at a commercial diagnostic laboratory (Quest Diagnostics) for a comprehensive metabolic panel (albumin, albumin/globulin ratio (calculated), alkaline phosphatase, ALT, AST, BUN/creatinine ratio (calculated), calcium, carbon dioxide, chloride, creatinine with estimated GFR, globulin, glucose, potassium, sodium, total bilirubin, total protein, and urea nitrogen). Comprehensive metabolic panels were only assessed at the 0 and 120-min time points.
2.4.6. Glucose and Insulin Determination
Each plasma sample was analyzed in duplicate for glucose and insulin concentration. Plasma glucose was analyzed at a commercial diagnostic laboratory (Quest Diagnostics) using automated clinical analyzers while insulin concentrations were assessed using a standard ELISA technique (DRG International, EIA2935, Springfield, NJ, USA). Briefly, all standards, samples, and controls were analyzed in duplicate across a range of 1.76–100 μIU/mL. Plate to plate controls were employed between all analyzed plates and exhibited a 6.3% coefficient of variation between the plates.
2.4.7. Plasma Berberine Determination
Berberine analysis was performed in plasma samples by Heartland Assays (Iowa State University Research Park, Ames, IA, USA) using coupled liquid chromatography-mass spectrometry-mass spectrometry technology (LC-MS-MS) following the procedures of Buchanan et al. [16]. Briefly, BBR and d6-BBR (Sigma-Aldrich, St. Louis, MO, USA and Toronto Research Chemicals, Toronto, Canada, respectively) standards were prepared using gravimetric determination and were dissolved in 50:50 methanol: water. As previously published, plasma samples and controls were removed from freezer storage and allowed to thaw at room temperature. An amount of 100 µL of plasma was transferred to a 13 × 100 glass test tube followed by the addition of 15.0 µL of d6-BBR internal standard (ISTD, 0.5 ng/µL). Next, samples were treated with 400 µL of acetonitrile containing 3% acetic acid, vortexed and centrifuged. The supernatant was transferred to 12 × 75 glass test tube and dried in a vacuum dryer. A standard curve (0.3–1000.0 ng/mL) was prepared and dried. Samples, controls, and standard curve were reconstituted in 50 µL of LC/MS/MS organic and 50 µL aqueous mobile phase solutions (Mobile phase B, LCMS-grade methanol and Mobile phase A, LCMS-grade water, both containing 0.2% formic acid and 0.1% 10 M ammonium formate solution) vortexed and transferred into LC/MS/MS vials. Chromatographic separation of BBR and d6-BBR was conducted on an Agilent Poroshell C18 column (2.1 × 50 mm, 2.7 µm) using an Agilent 6460 triple quadrupole LC/MS/MS system (Santa Clara, CA, USA). The initial gradient conditions were 45% B from 0 to 2 min and advanced to 95% B over 1 min with a flow rate of 0.40 mL/minute. BBR and d6-BBR data were collected using the Multiple Reaction Monitoring (MRM) mode with Mass Hunter acquisition software (Agilent, Santa Clara, CA, USA). The MRM pairs used for BBR were 337.1 → 322.1 and 337.1 → 293.1 and 343.1 → 325.2 and 343.1 → 307.1 for d6-BBR. Mass Hunter Quantitation software was used to quantitate the unknown plasma samples based on best fit standard curves. Quality control samples were run at two levels in each assay (4.0 and 100.0 ng/mL). Average recovery was 102% and ranged from 95% to 108%. The average accuracy (bias from nominal) was 1.0%. The average precision (CV) was 2.1% and 1.5% for intra- and inter-assay precision, respectively.
2.5. Statistical Analysis
The primary outcome for this study protocol was berberine AUC while secondary outcomes were considered to the maximum berberine concentration (CMax) as well as the AUC and CMax for glucose and insulin. Area under the curve (AUC) for berberine, glucose, and insulin were calculated using the trapezoidal method (Equation (1)), where C0 is the unknown concentration at the first time point of interest, C1 is the unknown concentration at the second time point of interest, and Time1–0 is the total time interval between the two time points when the unknown was measured. These individual AUC values for each time interval were then summed to determine the total AUC for berberine, glucose, and insulin (Equation (2)).
| (1) |
| (2) |
All analyses were completed using Microsoft Excel and the Statistical Package for the Social Sciences (v26; SPSS Inc., Chicago, IL, USA) while provided figures were developed using GraphPad (La Jolla, CA, USA). For all dependent measures, descriptive statistics are presented herein as mean ± standard deviations. Before any statistical tests were completed, normality was assessed using a Shapiro-Wilk test for all dependent variables. All non-normal data were transformed using natural logarithms, cubed, and then square root transformation approaches and was retested for normality. Data were then analyzed using both parametric and non-parametric approaches. In all such situations, the final statistical decision was identical whether parametric or non-parametric approaches were completed. All reported p-values are computed using parametric approaches. Blood markers were analyzed with a mixed factorial ANOVA, and if a significant interaction was observed then follow-up simple effects testing was performed using a repeated measures ANOVA followed by post-hoc testing consisting of paired samples t-tests. Body mass, blood pressure, AUC, and CMax variables were analyzed with a repeated measures ANOVA followed by post-hoc testing consisting of paired samples t-tests. For all statistical tests, data were considered statistically significant when the probability of type I error was 0.05 or less. Trends were highlighted and discussed when p-values were between 0.05 and 0.10.
3. Results
3.1. Pre-Supplementation Status
Table 2 outlines the pre-supplementation values for body mass and hemodynamics. Body mass was significantly different between groups (p = 0.045), and post-hoc testing revealed differences between PLA (90.6 ± 10.1 kg) and D200 (91.4 ± 9.7 kg). Resting heart rate (p = 0.21), systolic blood pressure (p = 0.07), and diastolic blood pressure (p = 0.87) were not different.
Table 2.
Baseline body mass, hemodynamic, glucose, insulin, and berberine.
| Raw Data | Group | Pre | p-Value |
|---|---|---|---|
| Body Mass (kg) | PLA | 90.6 ± 10.1 ‡ | 0.043 |
| D100 | 91.6 ± 10.3 | ||
| D200 | 91.4 ± 9.7 | ||
| B500 | 90.8 ± 10.0 | ||
| Resting Heart Rate (beats/minute) | PLA | 64 ± 10 | 0.21 |
| D100 | 62 ± 6 | ||
| D200 | 60 ± 5 | ||
| B500 | 57 ± 9 | ||
| Systolic Blood Pressure (mm Hg) | PLA | 120 ± 8 | 0.07 |
| D100 | 115 ± 10 | ||
| D200 | 118 ± 11 | ||
| B500 | 124 ± 10 | ||
| Diastolic Blood Pressure (mm Hg) | PLA | 72 ± 5 | 0.87 |
| D100 | 70 ± 5 | ||
| D200 | 70 ± 10 | ||
| B500 | 72 ± 7 | ||
| Glucose (mg/dL) | PLA | 91.8 ± 7.6 | 0.59 |
| D100 | 92.0 ± 8.5 | ||
| D200 | 90.6 ± 3.4 | ||
| B500 | 89.8 ± 1.8 | ||
| Berberine (ng/mL) | PLA | 0.14 ± 0.09 †,‡ | 0.006 |
| D100 | 2.60 ± 1.06 | ||
| D200 | 4.54 ± 2.24 | ||
| B500 | 0.30 ± 0.12 †,‡ | ||
| Insulin (μIU/mL) | PLA | 15.4 ± 5.4 | 0.20 |
| D100 | 16.7 ± 9.1 | ||
| D200 | 14.8 ± 4.4 | ||
| B500 | 18.4 ± 6.3 |
† = Different than D100 (p < 0.05); ‡ = Different than D200 (p < 0.05).
3.2. Protocol Compliance
Compliance to the supplementation regimen was 100% with all participants reporting that all supplements were ingested as instructed with the final dose being ingested in front of investigators. All study participants were asked to record their food and fluid intake for two days. Compliance was reported at 87.5% as one participant did not record their food and fluid intake on one of the days. Dietary intake is provided in Table 1.
3.3. Adverse Events
A total of 11 adverse events were reported throughout the study protocol by two or 40% of the study participants. The largest number of adverse events (n = 6) were reported in D100, n = 3 were reported in PLA, n = 1 for D200, and n = 1 for B500. All but one reported adverse event (10/11 or 90.9%) was deemed by study participants to be mild in severity and one being moderate severity (See Table 3).
Table 3.
Adverse event table.
| PLA | D100 | D200 | B500 | |
|---|---|---|---|---|
| n | 5 | 5 | 5 | 5 |
| # of AE’s Reported | ||||
| Mild | 3 | 5 | 1 | 1 |
| Moderate | 0 | 1 | 0 | 0 |
| Severe | 0 | 0 | 0 | 0 |
| Adverse Events Breakdown | ||||
| Gastrointestinal | ||||
| Diarrhea | 0 | 0 | 0 | 0 |
| Nausea | 0 | 2 | 0 | 0 |
| Upset stomach | 0 | 0 | 1 | 0 |
| Stomach cramping | 2 | 0 | 0 | 0 |
| Pain | ||||
| Headache | 0 | 2 | 0 | 1 |
| Cardiovascular | ||||
| Abnormal heart rhythm | 1 | 0 | 0 | 0 |
| Dizziness | 0 | 2 | 0 | 0 |
| Constitutional Symptoms | ||||
| Nervousness | 0 | 0 | 0 | 0 |
| Blurred vision | 0 | 0 | 0 | 0 |
| Summary | ||||
| Total Adverse Events | 3 | 6 | 1 | 1 |
| # of Subjects Reporting AE | 2 | 2 | 1 | 1 |
| % of Subjects Reporting AE | 40% | 40% | 20% | 20% |
PLA = Placebo; D100 = 100 mg dose of dihydroberberine; D200 = 200 mg dose of dihydroberberine; B500 = 500 mg dose of berberine.
3.4. Berberine
Berberine data were not-normally distributed. The data were transformed using the aforementioned methods and reassessed for normality, which was unable to be achieved due to two high values in the D200 condition at the 60-min timepoint. Subsequently, all berberine data were analyzed using parametric approaches. A significant group x time interaction was revealed for berberine (p = 0.05). Simple main effects tests revealed no changes over time within each condition (p > 0.05), but significant changes between conditions at the following time points: baseline (p = 0.006), 20-min (p < 0.001), and 40-min (p = 0.039). At baseline, both D100 (2.60 ± 1.06 ng/mL) and D200 (4.54 ± 2.24 ng/mL) conditions had higher berberine values compared to placebo (0.14 ± 0.09 ng/mL; D100, p = 0.007; D200, p = 0.011) and B500 (0.30 ± 0.12 ng/mL; D100, p = 0.006; D200, p = 0.013). At the 20-min time point, both D100 (3.00 ± 1.85 ng/mL) and D200 (6.06 ± 2.50 ng/mL) conditions had higher berberine values compared to placebo (0.18 ± 0.18 ng/mL; D100, p = 0.030; D200, p = 0.005) and B500 (0.32 ± 0.20 ng/mL; D100, p = 0.008; D200, p = 0.029), but D200 had higher berberine values compared to D100 (p = 0.050). Lastly, at 40 min both D100 (2.32 ± 1.27 ng/mL) and D200 (6.90 ± 4.94 ng/mL) conditions had higher berberine values compared to placebo (0.20 ± 0.14 ng/mL; D100, p = 0.018; D200, p = 0.037) and B500 (0.36 ± 0.15 ng/mL; D100, p = 0.022; D200, p = 0.040), but D200 had higher berberine values compared to D100 (p = 0.050). There was a significant main effect for condition (p = 0.04), but no significant main effect for time (p = 0.18) was observed.
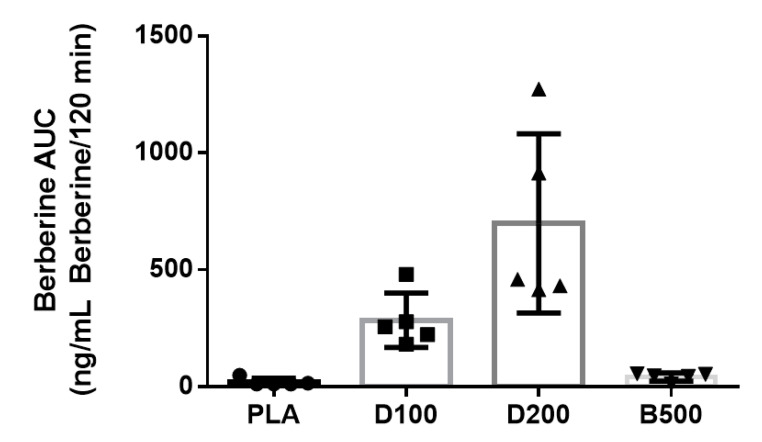
Berberine AUC values (Figure 3) were significantly difference between conditions (p = 0.045). Follow-up analysis indicated that higher berberine AUC values were identified in D200 (929 ± 694 ng/mL berberine/120 min) when compared to PLA (20.2 ± 16.2 ng/mL Berberine/120 min, p = 0.042) and B500 (42.3 ± 17.5 ng/mL Berberine/120 min, p = 0.045). Significantly higher berberine AUC values were identified for D100 (284.2 ± 115.9 ng/mL Berberine/120 min) when compared to placebo (20.2 ± 16.2 ng/mL Berberine/120 min, p = 0.007) and B500 (42.3 ± 17.5 ng/mL Berberine/120 min, p = 0.007). Berberine AUC values between D100 (284.2 ± 115.9) and D200 (929 ± 694 ng/mL Berberine/120 min) approached statistical significance (p = 0.07). Berberine AUC values between PLA (20.2 ± 16.2 ng/mL Berberine/120 min) and B500 (42.3 ± 17.5 ng/mL Berberine/120 min) tended (p = 0.096) to be different. Berberine CMax values tended to be different between conditions (p = 0.064). Further, differences in CMax between D100 and PLA were significant p = 0.005) while differences between PLA and D200 (p = 0.06) as well as PLA and B500 (p = 0.09) tended to be different.
Figure 3.
Individual and aggregated mean values for berberine AUC by condition.
Each individual symbol represents the individual AUC response for one study participant. For all graphs below, n = 5 participants completed each condition. PLA = Placebo; D100 = 100 mg dose of dihydroberberine; D200 = 200 mg dose of dihydroberberine; B500 = 500 mg dose of berberine. Data are presented as mean ± SD.
3.5. Glucose
There was no significant group x time interaction (p = 0.97) for glucose measures. However, a significant time effect (p < 0.001) was observed where glucose concentrations were significantly elevated at the 40-min timepoint (129.25 ± 27.43 mg/dL) compared to the baseline timepoint (91.05 ± 5.61 mg/dL, p < 0.022). Furthermore, both the 20-min timepoint (119.5 ± 21.27 mg/dL) and the 40-min timepoint (129.25 ± 27.43 mg/dL) had elevated glucose concentrations compared to the 90-min timepoint (85.40 ± 18.15 mg/dL; 20 min, p = 0.045; 40 min, p = 0.007), and the 120-min timepoint (69.6 ± 10.19 mg/dL; 20 min, p = 0.044; 40 min, p < 0.001). The 60-min timepoint (105.45 ± 23.55 mg/dL) had elevated glucose concentrations compared to the 120-min timepoint (69.60 ± 13.59 mg/dL, p = 0.033). Both AUC and CMax values were calculated for all four conditions. Oneway ANOVA indicated no significant differences were observed for AUC (p = 0.92) and CMax (p = 0.77) values (See Table 4 and Table 5).
Table 4.
Berberine (ng/mL), glucose (mg/dL), and insulin (μIU/mL) data.
| Berberine (ng/mL) | 0 min | 20 min | 40 min | 60 min | 90 min | 120 min | p | |
|---|---|---|---|---|---|---|---|---|
| PLA | 0.14 ± 0.09 | 0.18 ± 0.18 | 0.20 ± 0.14 | 0.16 ± 0.13 | 0.16 ± 0.13 | 0.16 ± 0.13 | Group | 0.002 |
| B500 | 0.30 ± 0.12 | 0.32 ± 0.20 | 0.36 ± 0.15 | 0.38 ± 0.16 | 0.39 ± 0.16 | 0.32 ± 0.13 | Time | 0.18 |
| D100 | 2.6 ± 1.1 †,‡ | 3.0 ± 1.9 †,‡ | 2.3 ± 1.3 †,‡ | 2.5 ± 1.0 | 2.1 ± 0.8 | 1.9 ± 0.9 | G x T | 0.050 |
| D200 | 4.5 ± 2.2 †,‡ | 6.1 ± 2.5 †,‡,* | 6.9 ± 4.9 †,‡,* | 11.4 ± 10.7 | 7.8 ± 6.5 | 7.2 ± 6.5 | ||
| Glucose (mg/dL) | 0 min | 20 min | 40 min | 60 min | 90 min | 120 min | p | |
| PLA | 91.8 ± 7.6 | 120.4 ± 25.4 | 129.6 ± 33.0 | 102.8 ± 27.6 | 92.0 ± 23.9 | 63.4 ± 9.3 | Group | 0.92 |
| B500 | 89.8 ± 1.8 | 116.4 ± 30.1 | 125.6 ± 35.7 | 101.8 ± 30.9 | 84.0 ± 25.1 | 73.0 ± 13.7 | Time | <0.001 |
| D100 | 92.0 ± 8.5 | 121.8 ± 20.9 | 126.8 ± 24.5 | 106.4 ± 14.9 | 81.2 ± 10.1 | 69.4 ± 7.9 | G x T | 0.97 |
| D200 | 90.6 ± 3.4 | 119.2 ± 11.8 | 135.0 ± 23.3 | 110.8 ± 25.2 | 84.4 ± 13.4 | 72.6 ± 21.6 | ||
|
Insulin
(μIU/mL) |
0 min | 20 min | 40 min | 60 min | 90 min | 120 min | p | |
| PLA | 15.4 ± 5.4 | 47.9 ± 31.3 | 106.9 ± 26.8 | 85.0 ± 21.0 | 78.5 ± 23.5 | 35.4 ± 19.2 | Group | 0.43 |
| B500 | 18.4 ± 6.3 | 38.4 ± 26.9 | 87.1 ± 24.5 | 78.1 ± 23.0 | 58.0 ± 23.5 | 58.0 ± 23.5 | Time | <0.001 |
| D100 | 16.7 ± 9.1 | 47.2 ± 17.6 | 93.0 ± 35.2 | 84.5 ± 33.2 | 60.9 ± 23.1 | 34.6 ± 14.8 | G x T | 0.10 |
| D200 | 14.8 ± 4.4 | 69.6 ± 28.6 | 85.0 ± 9.0 | 83.9 ± 27.4 | 78.9 ± 12.6 | 53.3 ± 29.6 |
† = Different than placebo (p < 0.05); ‡ = Different than B500 (p < 0.05); * = Different than D100 (p < 0.05).
Table 5.
Area under the curve (AUC) and concentration max (CMax) for berberine, insulin, and glucose.
| Berberine | AUC (ng/mL × 120 min) |
CMax (ng/mL) |
|---|---|---|
| PLA | 20.2 ± 16.2 | 0.22 ± 0.18 |
| B500 | 42.3 ± 17.6 | 0.40 ± 0.17 |
| D100 | 284.2 ± 115.9 | 3.8 ± 1.4 |
| D200 | 929 ± 694 | 12.0 ± 10.1 |
| p | 0.045 | 0.06 |
| Insulin |
AUC
(μIU/mL × 120 min) |
CMax
(μIU/mL) |
| PLA | 8260 ± 420 | 110.6 ± 24.3 |
| B500 | 7429 ± 1519 | 99.1 ± 6.6 |
| D100 | 8502 ± 717 | 107.2 ± 21.4 |
| D200 | 7242 ± 1263 | 98.1 ± 3.4 |
| p | 0.22 | 0.36 |
| Glucose |
AUC
(mg/dL × 120 min) |
CMax
(mg/dL) |
| PLA | 12,199 ± 1602 | 146.2 ± 13.9 |
| B500 | 12,029 ± 194 | 139.4 ± 32.8 |
| D100 | 12,381 ± 1128 | 140.8 ± 8.8 |
| D200 | 11,898 ± 2058 | 139.0 ± 16.6 |
| p | 0.92 | 0.77 |
3.6. Insulin
There was no significant group x time interaction (p = 0.095) for insulin measures. A significant time effect (p < 0.001) was observed where insulin concentrations were significantly elevated at 20 min (50.8 ± 20.7 µIU/mL, p = 0.02), 40 min (93.0 ± 18.2 µIU/mL, p = 0.02, and 60 min (82.9 ± 13.6 µIU/mL, p = 0.003) in comparison to baseline (16.3 ± 6.1 µIU/mL). Additionally, insulin concentrations were significantly higher at 40 min (93.0 ± 18.2 µIU/mL) and 60 min (82.9 ± 13.6 µIU/mL) compared to 20 min (50.8 ± 20.7 µIU/mL; 40 min, p = 0.002; 60 min, p = 0.018) and 120 min (45.1 ± 24.5 µIU/mL; 40 min, p = 0.002; 60 min, p = 0.013). No significant condition effect (p > 0.05) was identified. No significant differences were observed for AUC (p = 0.22) and CMax (p = 0.36) insulin values (See Table 4 and Table 5).
3.7. Whole Blood and Serum Markers
Complete blood count analysis was completed on collected whole-blood samples to assess safety and presence of any adverse responses to supplementation. As seen in Table 6, absolute lymphocytes analysis revealed a significant main effect of condition (p = 0.011) where D100 had elevated concentrations compared to D200 (p = 0.032) but were in clinically accepted norms. Absolute monocytes analysis revealed a significant group × time interaction (p = 0.047) and follow-up simple main effects testing revealed significant changes over time within the Placebo (p = 0.042) and D100 (p = 0.029) conditions. Specifically, at 120 min within the Placebo and D100 conditions absolute monocytes were higher than baseline albeit they were within clinically accepted norms. Furthermore, no significant changes between conditions were revealed at any time point for absolute monocytes (p > 0.05). All other variables for complete blood count did not change over time, between conditions, or reveal any interactions (p > 0.05).
Table 6.
Complete blood count.
| Variable Name | Group | Pre | Post | Group (G) (p) |
Time (T) (p) |
G x T (p) |
|---|---|---|---|---|---|---|
| White Blood Cell Count (103 × cells/μL) | PLA | 5.6 ± 1.0 | 5.7 ± 1.3 | 0.74 | 0.45 | 0.20 |
| D100 | 5.7 ± 1.1 | 5.9 ± 1.3 | ||||
| D200 | 6.6 ± 2.4 | 6.2 ± 2.1 | ||||
| B500 | 5.8 ± 1.2 | 5.3 ± 1.2 | ||||
| Red Blood Cell Count (103 × cells/μL) | PLA | 4.8 ± 0.2 | 4.8 ± 0.1 | 0.10 | 0.54 | 0.30 |
| D100 | 4.7 ±0.3 | 4.7 ± 0.3 | ||||
| D200 | 4.7 ± 0.3 | 4.7 ± 0.2 | ||||
| B500 | 5.0 ± 0.3 | 4.8 ± 0.4 | ||||
| Hemoglobin (g/dL) | PLA | 14.8 ± 0.5 | 14.8 ± 0.7 | 0.15 | 0.47 | 0.20 |
| D100 | 14.3 ± 0.4 | 14.5 ± 0.5 | ||||
| D200 | 14.3 ± 0.6 | 14.2 ± 0.4 | ||||
| B500 | 15.2 ± 1.0 | 14.8 ± 0.8 | ||||
| Hematocrit (%) | PLA | 43.2 ± 0.8 | 43.4 ± 1.4 | 0.20 | 0.73 | 0.19 |
| D100 | 42.2 ± 0.7 | 42.6 ± 1.4 | ||||
| D200 | 42.1 ± 1.3 | 42.0 ± 0.4 | ||||
| B500 | 44.6 ± 2.8 | 43.7 ± 3.0 | ||||
| Mean Corpuscular Volume | PLA | 89.4 ± 3.5 | 90.2 ± 3.8 | 0.87 | 0.44 | 0.71 |
| D100 | 90.1 ±4.7 | 90.0 ± 4.3 | ||||
| D200 | 90.4 ± 3.2 | 90.4 ± 3.8 | ||||
| B500 | 90.2 ± 2.8 | 90.5 ± 3.7 | ||||
| Mean Corpuscular Hemoglobin | PLA | 30.6 ± 1.6 | 30.7 ± 1.5 | 0.86 | 0.88 | 0.81 |
| D100 | 30.6 ± 1.6 | 30.5 ± 1.6 | ||||
| D200 | 30.7 ± 1.3 | 30.6 ± 1.6 | ||||
| B500 | 30.6 ± 1.6 | 30.7 ± 1.4 | ||||
| Mean Corpuscular Hemoglobin Content | PLA | 34.2 ± 0.6 | 34.1 ± 0.8 | 0.91 | 0.43 | 0.93 |
| D100 | 34.0 ± 0.6 | 34.0 ± 0.5 | ||||
| D200 | 34.0 ± 0.8 | 33.8 ± 0.7 | ||||
| B500 | 34.0 ± 0.9 | 33.9 ± 0.7 | ||||
| Red Cell Distribution Width (%) | PLA | 12.1 ± 0.4 | 12.0 ± 0.5 | 0.93 | 0.08 | 0.55 |
| D100 | 12.1 ± 0.4 | 12.0 ± 0.5 | ||||
| D200 | 12.1 ±0.4 | 12.1 ± 0.4 | ||||
| B500 | 12.0 ± 0.4 | 12.0 ± 0.4 | ||||
| Platelet Count | PLA | 242.2 ± 32.6 | 239.0 ± 37.3 | 0.85 | 0.91 | 0.55 |
| D100 | 243.4 ± 26.7 | 250.2 ± 26.5 | ||||
| D200 | 242.8 ± 23.9 | 242.0 ± 19.1 | ||||
| B500 | 247.4 ± 36.1 | 245.8 ± 30.9 | ||||
| Abs Neutrophils (cells/uL) | PLA | 2790 ± 1318 | 3046 ± 1295 | 0.45 | 0.88 | 0.38 |
| D100 | 2902 ± 719 | 2962 ± 949 | ||||
| D200 | 3926 ± 2324 | 3723 ± 2020 | ||||
| B500 | 2743 ± 737 | 2675 ± 702 | ||||
| Abs Lymphocytes (cells/uL) | PLA | 1893 ± 435 | 1805 ± 297 | 0.01 | 0.31 | 0.28 |
| D100 | 2068 ± 719 | 2173 ± 253 | ||||
| D200 | 1852 ± 528 | 1721 ± 149 | ||||
| B500 | 2268 ± 524 | 1899 ± 423 | ||||
| Abs Monocytes (cells/μL) | PLA | 477 ± 134 | 549 ± 168 | 0.92 | 0.04 | 0.007 |
| D100 | 494 ± 159 | 597 ± 225 | ||||
| D200 | 549 ± 152 | 504 ± 96 | ||||
| B500 | 545 ± 178 | 530 ± 205 | ||||
| Abs Eosinophils (cells/μL) | PLA | 218 ± 162 | 214 ± 162 | 0.17 | 0.09 | 0.62 |
| D100 | 179 ± 116 | 165 ± 96 | ||||
| D200 | 225 ± 148 | 188 ± 106 | ||||
| B500 | 183 ± 119 | 179 ± 161 | ||||
| Abs Basophils (cells/μL) | PLA | 42.8 ± 12.4 | 45.6 ± 10.9 | 0.47 | 0.94 | 0.67 |
| D100 | 38.4 ± 7.6 | 43.8 ± 12.2 | ||||
| D200 | 49.0 ± 18.5 | 44.6 ± 9.3 | ||||
| B500 | 41.2 ± 20.7 | 36.8 ± 11.6 | ||||
| Neutrophils (%) | PLA | 52.1 ± 13.2 | 52.2 ± 11.7 | 0.24 | 0.42 | 0.29 |
| D100 | 50.7 ± 7.3 | 49.1 ± 6.7 | ||||
| D200 | 56.7 ±14.4 | 57.3 ± 12.0 | ||||
| B500 | 47.5 ± 7.9 | 50.4 ± 7.8 | ||||
| Lymphocytes (%) | PLA | 34.7 ± 9.9 | 33.1 ± 7.8 | 0.17 | 0.26 | 0.32 |
| D100 | 36.7 ± 6.2 | 37.4 ± 5.2 | ||||
| D200 | 30.0 ± 9.5 | 29.8 ± 7.6 | ||||
| B500 | 39.5 ± 7.1 | 36.0 ± 4.7 | ||||
| Monocytes (%) | PLA | 8.5 ± 2.1 | 10.0 ± 3.1 | 0.12 | 0.15 | 0.60 |
| D100 | 9.0 ± 1.1 | 10.0 ± 2.9 | ||||
| D200 | 8.9 ± 2.7 | 8.8 ± 2.7 | ||||
| B500 | 9.3 ± 1.8 | 9.8 ± 2.4 | ||||
| Eosinophils (%) | PLA | 4.0 ± 3.0 | 3.9 ± 3.1 | 0.30 | 0.25 | 0.72 |
| D100 | 3.0 ± 1.4 | 2.7 ± 1.3 | ||||
| D200 | 3.6 ± 2.8 | 3.3 ± 2.5 | ||||
| B500 | 3.0 ± 1.5 | 3.1 ± 2.3 | ||||
| Basophils (%) | PLA | 0.8 ± 0.3 | 0.8 ± 0.3 | 0.37 | 0.43 | 0.95 |
| D100 | 0.7 ± 0.1 | 0.8 ± 0.3 | ||||
| D200 | 0.8 ± 0.3 | 0.8 ± 0.3 | ||||
| B500 | 0.7 ± 0.2 | 0.7 ± 0.2 |
Comprehensive metabolic panels were analyzed in collected serum samples. As seen in Table 7, analysis revealed significant main effects of time for glucose (p = 0.024), sodium (p < 0.001), potassium (p = 0.007), and chloride (p = 0.024) and these changes were within clinically accepted norms. A significant group × time interaction was revealed for creatinine (p = 0.008), and follow-up simple main effects testing revealed significant changes over time within the D100 (p = 0.031) and D200 (p = 0.030) conditions. Within the D100 condition at 120 min, creatinine measures were higher than baseline, and within the D200 condition, baseline measures were higher than 120 min, however, these measures are within clinically accepted norms. Additionally, there were significant creatinine differences between conditions at baseline (p = 0.039) and 120 min (p = 0.009) measures. At baseline, D200 (p = 0.030) and B500 (p = 0.016) conditions had higher creatinine measures compared to D100 and these differences were within clinically accepted norms. Lastly, a significant main effect of condition was observed for creatinine measures (p = 0.040) where D100 was higher than placebo (p = 0.035) but was within clinically accepted norms.
Table 7.
Comprehensive metabolic panel.
| Variable Name | Group | Pre | Post | Group (G) (p) |
Time (T) (p) |
G x T (p) |
|---|---|---|---|---|---|---|
| Glucose (mg/dL) | PLA | 90.6 ± 5.3 | 65.6 ± 11.0 | 0.66 | 0.02 | 0.17 |
| D100 | 92.0 ± 5.7 | 68.8 ± 10.0 | ||||
| D200 | 81.2 ± 13.6 | 73.2 ± 20.1 | ||||
| B500 | 89.2 ± 4.2 | 73.8 ± 15.4 | ||||
| Blood Urea Nitrogen (g/dL) | PLA | 16.2 ± 2.3 | 15.6 ± 2.3 | 0.14 | 0.11 | 0.46 |
| D100 | 13.8 ± 1.5 | 13.8 ± 1.3 | ||||
| D200 | 15.4 ± 1.9 | 14.8 ± 2.2 | ||||
| B500 | 15.8 ± 2.2 | 15.2 ± 2.5 | ||||
| Creatinine (mg/dL) | PLA | 1.0 ± 0.1 | 1.0 ± 0.1 | 0.04 | 0.55 | 0.008 |
| D100 | 0.9 ± 0.1 | 1.0 ± 0.1 | ||||
| D200 | 1.0 ± 0.1 | 0.9 ± 0.1 | ||||
| B500 | 1.0 ± 0.1 | 0.9 ± 0.1 | ||||
| Glomerular Filtrate Rate | PLA | 107.2 ± 12.0 | 102.2 ± 12.8 | 0.03 | 0.30 | 0.02 |
| D100 | 115.6 ± 8.4 | 109.4 ± 8.8 | ||||
| D200 | 106.2 ± 13.0 | 111.0 ± 11.9 | ||||
| B500 | 106.6 ± 13.3 | 109.2 ±12.8 | ||||
| Sodium (mM) | PLA | 137 ± 1 | 139 ± 2 | 0.20 | <0.001 | 0.82 |
| D100 | 136 ± 2 | 139 ± 2 | ||||
| D200 | 135 ± 2 | 137 ± 2 | ||||
| B500 | 136 ± 2 | 138 ± 3 | ||||
| Potassium (mM) | PLA | 4.3 ± 0.2 | 4.0 ± 0.1 | 0.36 | 0.007 | 0.90 |
| D100 | 4.2 ± 0.2 | 3.9 ± 0.2 | ||||
| D200 | 4.3 ± 0.2 | 4.0 ± 0.2 | ||||
| B500 | 4.2 ± 0.3 | 3.9 ± 0.2 | ||||
| Chloride (mM) | PLA | 102 ± 2 | 102 ± 1 | 0.45 | 0.02 | 0.18 |
| D100 | 103 ± 2 | 103 ± 2 | ||||
| D200 | 101 ± 2 | 103 ± 2 | ||||
| B500 | 101 ± 3 | 103 ± 2 | ||||
| Carbon Dioxide (mM) | PLA | 25 ± 2 | 26 ± 3 | 0.62 | 0.16 | 0.78 |
| D100 | 25 ± 1 | 26 ± 1 | ||||
| D200 | 26 ± 1 | 27 ± 2 | ||||
| B500 | 25 ± 1 | 26 ± 3 | ||||
| Calcium (mg/dL) | PLA | 9.3 ± 0.4 | 9.7 ± 0.2 | 0.26 | 0.12 | 0.049 |
| D100 | 9.4 ± 0.2 | 9.5 ± 0.3 | ||||
| D200 | 9.3 ± 0.5 | 9.4 ± 0.3 | ||||
| B500 | 9.5 ± 0.3 | 9.5 ± 0.3 | ||||
| Total Protein (g/dL) | PLA | 6.8 ± 0.4 | 6.9 ± 0.3 | 0.94 | 0.74 | 0.22 |
| D100 | 6.8 ± 0.3 | 6.9 ± 0.3 | ||||
| D200 | 6.8 ± 0.6 | 6.8 ± 0.4 | ||||
| B500 | 7.0 ± 0.5 | 6.8 ± 0.5 | ||||
| Albumin (g/dL) | PLA | 4.6 ± 0.2 | 4.5 ± 0.1 | 0.42 | 0.38 | 0.80 |
| D100 | 4.5 ± 0.1 | 4.4 ± 0.2 | ||||
| D200 | 4.5 ± 0.2 | 4.4 ± 0.0 | ||||
| B500 | 4.6 ± 0.1 | 4.5 ± 0.1 | ||||
| Globulin (g/dL) | PLA | 2.2 ± 0.3 | 2.3 ± 0.3 | 0.62 | 0.26 | 0.17 |
| D100 | 2.3 ± 0.3 | 2.4 ± 0.3 | ||||
| D200 | 2.4 ± 0.4 | 2.4 ± 0.3 | ||||
| B500 | 2.4 ± 0.4 | 2.3 ± 0.5 | ||||
| Alb/Glob Ratio | PLA | 2.1 ± 0.2 | 2.0 ± 0.2 | 0.37 | 0.11 | 0.28 |
| D100 | 2.0 ± 0.3 | 1.8 ± 0.3 | ||||
| D200 | 1.9 ± 0.3 | 1.9 ± 0.3 | ||||
| B500 | 1.9 ± 0.3 | 2.0 ± 0.4 | ||||
| Total Bilirubin (mg/dL) | PLA | 0.9 ± 0.3 | 0.8 ± 0.3 | 0.52 | 0.14 | 0.37 |
| D100 | 0.8 ± 0.3 | 0.8 ± 0.3 | ||||
| D200 | 0.9 ± 0.4 | 0.8 ± 0.3 | ||||
| B500 | 1.0 ± 0.4 | 0.9 ± 0.4 | ||||
| Alkaline Phosphatase (U/L) | PLA | 53 ± 10 | 51 ± 10 | 0.13 | 0.16 | 0.45 |
| D100 | 51 ± 11 | 52 ± 10 | ||||
| D200 | 51 ± 13 | 50 ± 10 | ||||
| B500 | 54 ± 12 | 53 ± 13 | ||||
| AST (U/L) | PLA | 22 ± 5 | 22 ± 5 | 0.22 | 0.18 | 0.55 |
| D100 | 24 ± 7 | 24 ± 7 | ||||
| D200 | 24 ± 6 | 23 ± 5 | ||||
| B500 | 20 ± 3 | 20 ± 3 | ||||
| ALT (U/L) | PLA | 19 ± 6 | 19 ± 5 | 0.93 | 1.00 | 0.60 |
| D100 | 19 ± 7 | 20 ± 7 | ||||
| D200 | 19 ± 4 | 18 ± 3 | ||||
| B500 | 18 ± 6 | 18 ± 5 |
A significant group x time interaction was revealed for globular filtration rate (p = 0.016) and follow-up simple main effects testing revealed significant changes over time within the D100 (p = 0.047) and D200 (p = 0.037) conditions. Within the D100 condition, baseline globular filtration rate measures were higher than 120 min, and within the D200 condition 120 min measures were higher than baseline, however, these measures are within clinically accepted norms. Additionally, follow-up simple main effects testing from the interaction revealed significant differences between conditions for globular filtration rate measures at baseline (p = 0.050) and 120 min (p = 0.005). At baseline, globular filtration rate measures were higher in D100 compared to D200 (p = 0.048) and B500 (p = 0.038), which were within clinically accepted norms. At 120 min, globular filtration rate measures were higher in D200 (p = 0.024), D100 (p = 0.024), and B500 (p = 0.047) compared to placebo and were within clinically accepted norms. Lastly, a significant main effect of condition was observed for globular filtration rate measures (p = 0.033) where D100 was higher than placebo (p = 0.028) but was within clinically accepted norms.
A significant group x time interaction was revealed for calcium (p = 0.049) and follow-up simple main effects testing revealed significant changes over time within the placebo condition (p = 0.009), the levels of which were higher at 120 min compared to baseline, but within clinically accepted norms. Furthermore, a follow-up simple main effects revealed significant differences between conditions for calcium measures at 120 min (p = 0.030) where placebo was higher than D200 (p = 0.040) and all measures were within clinically accepted norms. All other variables for the comprehensive metabolic panel did not change over time, between conditions, or reveal any interactions (p > 0.05).
4. Discussion
The intent of this project was to evaluate the observed differences in plasma berberine concentrations after oral ingestion of two doses (100 mg [D100] and 200 mg [D200], respectively) of dihydroberberine and one dose (500 mg) of berberine (B500). Findings from this pilot approach revealed that area under the curve calculations for berberine were significantly greater when either dose of dihydroberberine was ingested in comparison to the values observed for berberine and placebo (PLA). In addition, peak berberine concentrations (CMax) tended to be different between all conditions. Specifically, the 100 mg dose of dihydroberberine was significantly greater than peak values observed in PLA and B500 while peak concentrations for the 200 mg dose of dihydroberberine tended to be different than what was observed in the berberine group.
Of the available human research that has explored efficacy and safety of oral berberine ingestion, the majority of these studies have employed a dosing regimen that consists of two to three daily doses with meals (to reduce incidence of gastrointestinal complications) at a dosage of 500 mg per dose. For example, Perez-Rubio et al. [7] had 24 metabolic syndrome patients randomly ingest, in a double-blind, placebo-controlled fashion, three daily doses of 500 mg/dose (total daily dosage of 1500 mg/day) for three months. Similarly, Yin et al. [6] also randomly assigned type 2 diabetes patients to ingest three daily 500 mg doses for a total of 13 weeks. Finally, Zhang et al. [17] randomly assigned 116 individuals diagnosed with type 2 diabetes to consume two 500 mg daily doses (1000 mg total) over a 3-month period. While results of these studies outline efficacy outcomes in various clinical populations, very limited human data are available that has outlined the absorption pattern and plasma kinetics after oral berberine ingestion. In this respect, it has been previously reported that oral bioavailability of berberine is extremely low (<1%) in both animal [9,10] and human models largely due to poor intestinal absorption and high levels of first-pass removal in the intestines and liver [5]. This has led to the identification of various strategies to increase bioavailability, including administration of dihydroberberine. Currently, no human research has appeared in the peer-reviewed literature that has examined oral ingestion of dihydroberberine. Towards this end, Buchanan et al. [16] compared the pharmacokinetics associated with transdermal administration of berberine and dihydroberberine in Sprague-Dawley rats. Using this model and over an 8-h period, transdermal application of dihydroberberine resulted in greater AUC values than what was observed for both transdermal and oral administration of berberine. Moreover, transdermal delivery of berberine resulted in greater AUC values than what was observed for oral administration, further highlighting the poor bioavailability of oral berberine ingestion.
Other highlights from the present study include the statistically significant higher outcomes at baseline (after three doses, but prior to the 4th dose in the present study) in D100 and D200 when compared to PLA and B500. When viewed in comparison to PLA, this outcome was not surprising and some might deem it expected considering that dihydroberberine was administered, however, the finding of greater levels in comparison to berberine seemingly speaks to the ability of dihydroberberine to maintain berberine levels in the blood better than oral berberine ingestion. Whether or not these increases in plasma berberine translate beyond one day or measurement or improvements in efficacy outcomes commonly associated with berberine supplementation cannot be determined from this project. In this respect, more research is certainly needed with dihydroberberine to determine how well the greater plasma berberine levels improve dyslipidemia and glucose and insulin homeostasis as commonly reported in the literature.
A key limitation with the present study is the sample size on this project. While the fully randomized, crossover, double-blind, and placebo-controlled approach was a sound approach for this pilot assessment, it is readily acknowledged by the authors that more study participants are needed on future studies to continue to establish the safety and efficacy of berberine and dihydroberberine. Further to the point and beyond just having a low sample size, one needs to closely consider our plasma berberine data as two participants in the D200 at the 60-min time point exhibited high values, which nearly achieved traditional definitions of being a statistical outlier (>±3 of standardized residual estimates). When combined with the low sample size, these data exerted substantial impact on the distribution of these data. As such, traditional approaches to transforming the data were unsuccessful at achieving normality and all data were subsequently analyzed using a parametric approach. Furthermore, all analysis was also completed using an intent-to-treat approach with those values removed and the high values replaced with the previous data point and no meaningful differences were noted in the outcomes of the project. Another limitation might be considered to be the small number of doses ingested prior to assessing the absorption kinetics. This was an a priori consideration as our primary focus for this pilot project was to assess and compare the absorption kinetics of two different doses of oral dihydroberberine in comparison to oral ingestion of berberine and placebo.
5. Conclusions
In conclusion, results from this study represent what we believe are the first data in humans to evaluate the absorption kinetics of berberine and two doses of dihydroberberine. Results from this study demonstrate that dihydroberberine, irrespective of what dose is delivered, achieves greater area under the curve as well as peak berberine concentrations when compared to oral ingestion of berberine or placebo. Since berberine use has traditionally spanned several months to establish the observed efficacy outcomes known for berberine (improved glucose and insulin homeostasis and lipid parameters), several follow-up approaches are recommended. First, can the increased levels of berberine seen from dihydroberberine ingestion usher in faster improvements in outcomes of interest. In a similar vein, are the outcomes improved as a result of dihydroberberine ingestion in comparison to berberine ingestion.
Acknowledgments
The authors like to thank the participants for their dedication to completing this study protocol. Additionally, the authors would like to thank Kate Tessmer, Associate Dean of the School of Science, Technology, and Health at Lindenwood University for her assistance with blinding the supplements.
Author Contributions
Designed study: C.M.K.; data collection: J.M.M., A.M.H., K.M.R. and R.A.S.; analyzed data: P.W.M.; prepared initial draft: C.M.K., A.M.H., J.M.M. and P.W.M.; approved final version: all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by NNB Nutrition.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Lindenwood University: IRB-20-173, approval date: 22 June 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data and/or statistical analyses are available upon request on a case-by-case basis for non-commercial scientific inquiry and/or educational use.
Conflicts of Interest
C.M.K. serves as a paid advisor for NNB Nutrition. A conflict-of-interest management plan was filed and approved by the Lindenwood University IRB prior to commencing any data collection. As part of this plan, C.M.K. was not involved in any part of the consenting, randomization, or data collection process. All statistical analysis performed by C.M.K. was done while data was still blinded and all analysis and interpretation was confirmed by P.W.M. As such, P.W.M. and C.M.K. prepared all statistical analysis and interpretation. All other authors declare that they have no competing interests.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liu C.S., Zheng Y.R., Zhang Y.F., Long X.Y. Research progress on berberine with a special focus on its oral bioavailability. Fitoterapia. 2016;109:274–282. doi: 10.1016/j.fitote.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Imenshahidi M., Hosseinzadeh H. Berberine and barberry (Berberis vulgaris): A clinical review. Phytother. Res. 2019;33:504–523. doi: 10.1002/ptr.6252. [DOI] [PubMed] [Google Scholar]
- 3.Lee Y.S., Kim W.S., Kim K.H., Yoon M.J., Cho H.J., Shen Y., Ye J.M., Lee C.H., Oh W.K., Kim C.T., et al. Berberine, a natural plant product, activates AMP-activated protein kinase with beneficial metabolic effects in diabetic and insulin-resistant states. Diabetes. 2006;55:2256–2264. doi: 10.2337/db06-0006. [DOI] [PubMed] [Google Scholar]
- 4.Li X.Y., Zhao Z.X., Huang M., Feng R., He C.Y., Ma C., Luo S.H., Fu J., Wen B.Y., Ren L., et al. Effect of Berberine on promoting the excretion of cholesterol in high-fat diet-induced hyperlipidemic hamsters. J. Transl. Med. 2015;13:278. doi: 10.1186/s12967-015-0629-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim W.S., Lee Y.S., Cha S.H., Jeong H.W., Choe S.S., Lee M.R., Oh G.T., Park H.S., Lee K.U., Lane M.D., et al. Berberine improves lipid dysregulation in obesity by controlling central and peripheral AMPK activity. Am. J. Physiol. Endocrinol. Metab. 2009;296:E812–E819. doi: 10.1152/ajpendo.90710.2008. [DOI] [PubMed] [Google Scholar]
- 6.Yin J., Xing H., Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metab. Clin. Exp. 2008;57:712–717. doi: 10.1016/j.metabol.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perez-Rubio K.G., Gonzalez-Ortiz M., Martinez-Abundis E., Robles-Cervantes J.A., Espinel-Bermudez M.C. Effect of berberine administration on metabolic syndrome, insulin sensitivity, and insulin secretion. Metab. Syndr. Relat. Disord. 2013;11:366–369. doi: 10.1089/met.2012.0183. [DOI] [PubMed] [Google Scholar]
- 8.Rao A. Efficacy of berberine hydrochloride on biochemical parameters in Indian type 2 diabetes patients. Endocr. Pract. 2017;23:18A. [Google Scholar]
- 9.Chen W., Miao Y.Q., Fan D.J., Yang S.S., Lin X., Meng L.K., Tang X. Bioavailability study of berberine and the enhancing effects of TPGS on intestinal absorption in rats. AAPS PharmSciTech. 2011;12:705–711. doi: 10.1208/s12249-011-9632-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Y.T., Hao H.P., Xie H.G., Lai L., Wang Q., Liu C.X., Wang G.J. Extensive intestinal first-pass elimination and predominant hepatic distribution of berberine explain its low plasma levels in rats. Drug Metab. Dispos. 2010;38:1779–1784. doi: 10.1124/dmd.110.033936. [DOI] [PubMed] [Google Scholar]
- 11.Zhou Y., Liu S., Ming J., Li Y., Deng M., He B. Sustained release effects of berberine-loaded chitosan microspheres on in vitro chondrocyte culture. Drug Dev. Ind. Pharm. 2017;43:1703–1714. doi: 10.1080/03639045.2017.1339076. [DOI] [PubMed] [Google Scholar]
- 12.Yu F., Ao M., Zheng X., Li N., Xia J., Li Y., Li D., Hou Z., Qi Z., Chen X.D. PEG-lipid-PLGA hybrid nanoparticles loaded with berberine-phospholipid complex to facilitate the oral delivery efficiency. Drug Deliv. 2017;24:825–833. doi: 10.1080/10717544.2017.1321062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Pierro F., Putignano P., Villanova N., Montesi L., Moscatiello S., Marchesini G. Preliminary study about the possible glycemic clinical advantage in using a fixed combination of Berberis aristata and Silybum marianum standardized extracts versus only Berberis aristata in patients with type 2 diabetes. Clin. Pharmacol. 2013;5:167–174. doi: 10.2147/CPAA.S54308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Godugu C., Patel A.R., Doddapaneni R., Somagoni J., Singh M. Approaches to improve the oral bioavailability and effects of novel anticancer drugs berberine and betulinic acid. PLoS ONE. 2014;9:e89919. doi: 10.1371/journal.pone.0089919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan L., Wang Y., Ai G., Luo C., Chen H., Li C., Zeng H., Xie J., Chen J., Su Z. Dihydroberberine, a hydrogenated derivative of berberine firstly identified in Phellodendri Chinese Cortex, exerts anti-inflammatory effect via dual modulation of NF-κB and MAPK signaling pathways. Int. Immunopharmacol. 2019;75:105802. doi: 10.1016/j.intimp.2019.105802. [DOI] [PubMed] [Google Scholar]
- 16.Buchanan B., Meng Q., Poulin M.M., Zuccolo J., Azike C.G., Gabriele J., Baranowski D.C. Comparative pharmacokinetics and safety assessment of transdermal berberine and dihydroberberine. PLoS ONE. 2018;13:e0194979. doi: 10.1371/journal.pone.0194979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Y., Li X., Zou D., Liu W., Yang J., Zhu N., Huo L., Wang M., Hong J., Wu P., et al. Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. J. Clin. Endocrinol. Metab. 2008;93:2559–2565. doi: 10.1210/jc.2007-2404. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and/or statistical analyses are available upon request on a case-by-case basis for non-commercial scientific inquiry and/or educational use.