Abstract
Resistance to antifungal agents represents a major clinical challenge, leading to high morbidity and mortality rates, especially in immunocompromised patients. In this study, we screened soil bacterial isolates for the capability of producing metabolites with antifungal activities via the cross-streak and agar cup-plate methods. One isolate, coded S6, showed observable antifungal activity against Candida (C.) albicans ATCC 10231 and Aspergillus (A.) niger clinical isolate. This strain was identified using a combined approach of phenotypic and molecular techniques as Lysinibacillus sp. MK212927. The purified metabolite displayed fungicidal activity, reserved its activity in a relatively wide range of temperatures (up to 60 °C) and pH values (6–7.8) and was stable in the presence of various enzymes and detergents. As compared to fluconazole, miconazole and Lamisil, the minimum inhibitory concentration of the metabolite that showed 90% inhibition of the growth (MIC90) was equivalent to that of Lamisil, half of miconazole and one fourth of fluconazole. Using different spectroscopic techniques such as FTIR, UV spectroscopy, 1D NMR and 2D NMR techniques, the purified metabolite was identified as terbinafine, an allylamine antifungal agent. It is deemed necessary to note that this is the first report of terbinafine production by Lysinibacillus sp. MK212927, a fast-growing microbial source, with relatively high yield and that is subject to potential optimization for industrial production capabilities.
Keywords: antifungal, Lysinibacillus, terbinafine, bio-active metabolite, fungicidal, 2D NMR
1. Introduction
High levels of resistance to antifungal agents have been recently reported particularly among pathogenic Candida spp. [1] and Aspergillus spp. isolates [2,3]. These elevated resistance rates are responsible for a largely silent epidemic and aggravated the prognosis of fungal infections, especially in the immunocompromised patients, leading to high morbidity and mortality rates [4]. Candida spp., for example, can cause a wide spectrum of systemic and invasive infections [5]. Invasive candidiasis was reported to cause about 20% of the serious illness in Intensive Care Units (ICUs) [6]. HIV-positive populations mainly suffer from oropharyngeal candidiasis as an opportunistic infection, with 95% of them showing infection by C. albicans [7,8,9].
Terbinafine hydrochloride, which is (E)-N-Methyl-N-(l-Naphtylmethyl)-6,6-dimethylhept-2-ene-4-ynyl-l-amine, was reported first in the European patent No.24587, as a good antifungal agent used preferably against mycosis caused by dermatophyte on the skin and on nails. This compound was prepared in three different ways, according to the process disclosed in this patent [10]. In a later publication [11], the hydrochloride salt of the trans isomer of terbinafine was prepared from the mixture of Cis and Trans isomers by column chromatography on silica gel and salt formation of base by treatment with hydrochloric acid in ethanol followed by recrystallization. Another study included the synthesis of chiral derivatives of terbinafine; a series of allylamine compounds have been synthesized and evaluated for their antifungal activity towards Cryptococcus neoformans. All compounds were chiral derivatives of terbinafine, having additional substituents at the carbon connected to the central nitrogen atom [12]. The stereo-selective synthesis of terbinafine, bearing (E)-tert-butylenyne structural element as the side chain, has been performed and resulted in a good yield. This methodology avoids the use of toxic starting materials [13]. A three-step batch-flow hybrid process has been developed for an expeditious synthesis of the enynol key intermediate of antifungal terbinafine. This procedure involves consecutive organometallic steps without the need for any in-line purification, enabling safe and convenient scale-up [14]. Therapies of fungal infections have been restricted by the limited numbers, low safety profiles and emergence of resistance to currently used antifungal agents [15]. No doubt we are facing a serious public health problem, which highlights the crucial need for the discovery of new specific antifungal agents, preferably from natural resources, particularly those that have not been exploited yet [16], for instance, soil microbial communities, which have been reported to produce biologically active natural byproducts [17,18,19,20]. This study is concerned with Lysinibacillus sp., a Gram-positive, rod-shaped bacterium from the family Bacillaceae [21]. These microorganisms were previously considered as members of the genus Bacillus, but due to the new taxonomic classification they now belong to the genus Lysinibacillus [22].
Bioactive metabolites derived from the genus Bacillus have showed structural diversity and a wide spectrum of bioactivities such as antifungal, antibacterial, antitumor and antimycoplastic activities [23]. The known Bacillus spp. that produce antifungal antibiotics are B. subtilis, B. brevis, B. licheniformis, B. circulans and B. cereus [24]. Most of peptide antifungal agents such as bacillomycin, mycobacillin and fungistatin are able to target and disintegrate fungal cell walls [25,26]. A recent study showed that fengycin and iturin can be used for biological control of Mortierella and Myrothecium and Fusarium [27]. Additionally, iturin can be used for the management of infections caused by C. albicans and several other human important fungal pathogens [28]. Both B. subtilis and B. mojavensis have a potential of lipopeptides and cell-wall degrading enzymes production, which act as an alternative resource for control of C. albicans [29]. Another 7-amino-acid residue lipopeptide antibiotic produced by B. subtilis named Surfactin showed antifungal activity against Fusarium moniliforme [30]. Bacillus strains (CWSI-B1567 and CWSI-B1568) also secreted antifungal metabolites that inhibited the growth of C. albicans [23]. Tyrocidine and Gramicidin S are cyclic peptides produced by Brevibacillus brevis. The gramicidin S synthetase, a multifunctional enzyme complex, catalyzes Gramicidin S synthesis [31]. B. cereus and B. licheniformis, which excrete several antifungal compounds, mainly lipopeptides, have also been successfully tested against candidiasis [32]. B. cereus produces cispentacin, which is active on C. albicans both in vitro and in vivo in mice, and mycocerein, an iturin antifungal, which inhibits growth [33]. Members of the B. subtilis group were found to produce numerous highly active antifungal compounds, e.g., Subtilin, subsporins A–C, lipooligopeptides, rhizocticins A-D and phosphooligopeptides [34]. Moreover, they produce lipopeptide bacillomycins L and D; bacillopeptins; and rhizocticin A, a hydrophilic phosphonooligopeptide active against Candida spp. [35].
Several metabolites produced by Bacillus sp. have been previously explored, but the antifungal potential of Lysinibacillus is poorly reported in literature. Therefore, this study aimed to identify the promising antifungal activity of a Lysinibacillus isolate recovered from soil against A. niger clinical isolate and C. albicans standard strain ATCC 10231. Subsequent purification, characterization and structure elucidation of the respective metabolite were performed, emphasizing the advantages of soil microbes as natural producers of bioactive metabolites.
2. Results
2.1. Screening for the Production of Antifungal Metabolite(s)
Seventy-three bacterial colonies were isolated and screened using the cross-streak, agar cup-plate and dual-culture methods. Results showed that only three isolates (coded F1, S6 and F2) out of 73 (4.1%) isolates gave clear halos of inhibition against C. albicans ATCC 10231 and A. niger clinical isolate, indicating their antifungal activities (Figure S1). The isolate S6 showed maximum inhibition zone as compared to F1 and F2 and therefore was chosen for further study (Table S1).
2.2. Identification of the Isolate S6
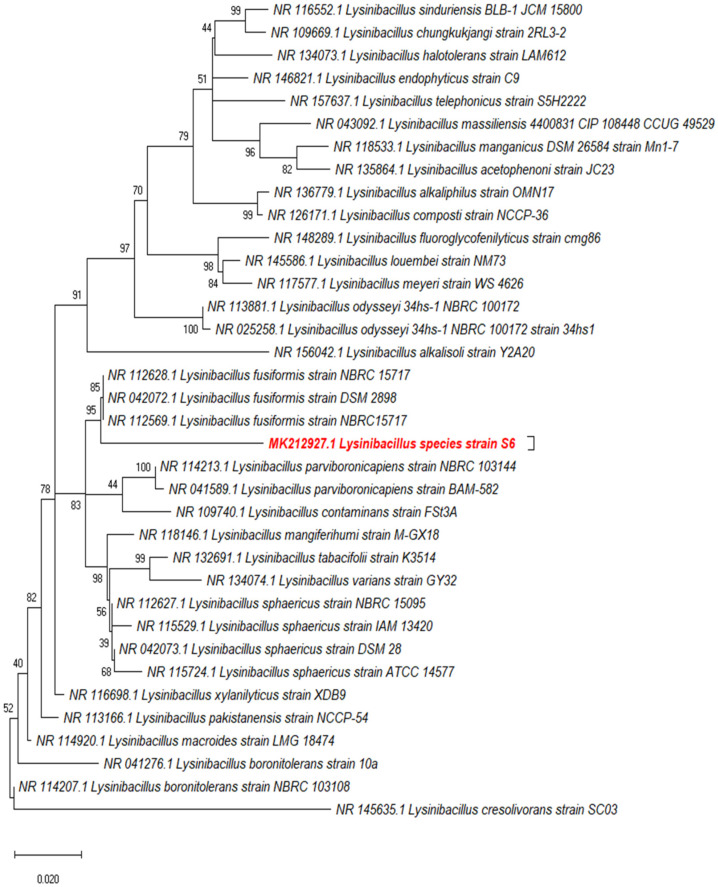
A phylogenetic tree of the 16S ribosomal RNA gene sequence was constructed using the MEGA X and showed that the S6 isolate clustered in close vicinity to Lysinibacillus (L.) fusiformis but occupied a separate sub-branch (Figure 1). Isolate S6 was spore-forming Gram positive rods, which gave positive for starch hydrolysis, catalase production and citrate utilization and negative for gelatin liquefaction, casein hydrolysis and urease production. According to the obtained results, isolate S6 was identified as Lysinibacillus isolate MK212927 (NCBI nucleotide accession code, MK212927.1) and deposited in the Culture Collection Ain Shams University CCASU-MK212927.
Figure 1.
Molecular phylogenetic analysis of the query isolate (S6) using maximum likelihood method based on the Kimura 2-parameter model in MEGA X.
2.3. Extraction of the Antifungal Metabolite(s)
No precipitation of any peptides was seen in the culture supernatant using (NH₄)₂SO₄ at the stated conditions. Ethyl acetate was the optimum solvent for extraction, with a net weight yield of 1.07 g from 200 mL of clear supernatant, and resulted in inhibition zones of 26.6 mm and 24.3 mm against C. albicans standard strain and A. niger clinical isolate, respectively (Table S2).
2.4. Purification of the Bioactive Metabolite(s) by Silica Gel Column Chromatography
The solvent system consisting of hexane: ethyl acetate was used for extract fractionation (Table 1). About 136 fractions were collected and pooled into 21 pooled fractions (PFs) based on their TLC retardation factors. The fractions were checked by means of bioautography for their antifungal activities, where the PFs 6, 7 and 8 showed maximum antifungal activities (Figure S2). Other PFs showed either no or moderate activities. Elutes 43–47 forming the pooled fraction PF 6 showed the maximum antimycotic activity and were harvested using solvent system hexane: ethyl acetate with the ratio 75:25 (Table 1).
Table 1.
Fractionation of crude antifungal metabolite by Lysinibacillus isolate showing ratios of the solvent systems used, the retention factor(s), dry weight(s) and bioautography results.
| Pooled Fractions (PFs) | n-Hexane: Ethyl Acetate (EA) | Elutes Recovered | Retardation Factor (RF) | Dry Weight of Each PF (mg) | Mean Inhibition Zones (mm) ± SD |
|
|---|---|---|---|---|---|---|
| C. albicans | A. niger | |||||
| 1 | n-hexane 100% | 1–7 | 0.96 | 1.4 | - | - |
| 2 | 95:5 | 8–19 | 0.93 | 1.8 | - | - |
| 3 | 90:10 | 20–25 | 0.88 | 4.6 | 16 ± 0.25 | 14 ± 0.25 |
| 4 | 85:15 | 26–36 | 0.84 | 2 | 21 ± 0.45 | 20 ± 0.36 |
| 5 | 80:20 | 37–42 | 0.78 | 3.33 | 22 ± 0.36 | 14 ± 0.25 |
| 6 | 75:25 | 43–47 | 0.71 | 4.1 | 31 ± 0.58 | 29 ± 0.58 |
| 7 | 70:30 | 48–53 | 0.69 | 2.4 | 30 ± 0.36 | 27 ± 0.36 |
| 8 | 65:35 | 54–59 | 0.63 | 4.22 | 29 ± 0.58 | 28 ± 0.58 |
| 9 | 60:40 | 60–64 | 0.60 | 2.6 | 13 ± 0.25 | 15 ± 0.36 |
| 10 | 55:45 | 65–69 | 0.58 | 0.99 | - | - |
| 11 | 50:50 | 70–76 | 0.52 | 0.89 | - | - |
| 12 | 45:55 | 77–82 | 0.49 | 4 | - | - |
| 13 | 40:60 | 83–88 | 0.46 | 3.9 | - | - |
| 14 | 35:65 | 89–94 | 0.43 | 3.7 | 17 ± 0.45 | 19 ± 0.58 |
| 15 | 30:70 | 95–99 | 0.39 | 1.67 | 18 ± 0.45 | 15 ± 0.25 |
| 16 | 25:75 | 100–106 | 0.35 | 2.78 | 14 ± 0.36 | 16 ± 0.36 |
| 17 | 20:80 | 107–112 | 0.31 | 4.4 | 12 ± 0.25 | 11 ± 0.25 |
| 18 | 15:85 | 113–119 | 0.28 | 1.8 | 15 ± 0.45 | 17 ± 0.36 |
| 19 | 10:90 | 120–125 | 0.23 | 1.01 | 20 ± 0.36 | 18 ± 0.36 |
| 20 | 5:95 | 126–130 | 0.14 | 5.2 | 19 ± 0.45 | 20 ± 0.58 |
| 21 | EA 100% | 131–136 | 0.12 | 4.9 | 23 ± 0.58 | 21 ± 0.36 |
2.5. Correlation between the Metabolite(s) Concentration and Inhibition Zone Diameters Using Agar Well Diffusion
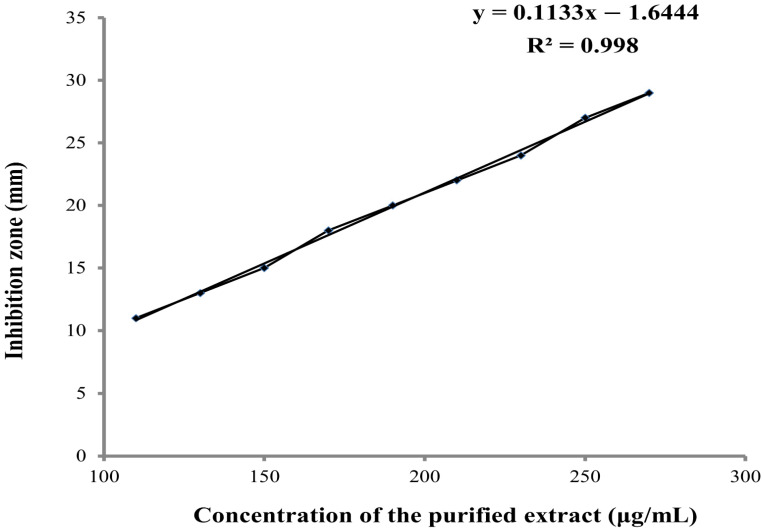
As shown in Figure 2, the increase in the concentrations of the purified antifungal compound was associated with a linear increase in the inhibition zones (mm) of the respective concentration.
Figure 2.
Linear relationship between different concentrations of the purified extract (µg/mL) and the inhibition zone diameter (mm).
2.6. Thermal, Enzymes, Detergents, and pH Stability of the Antifungal Metabolite
The compound was found to be a light brown amorphous solid. It was soluble in most organic solvents. As shown in Figure S3, the bioactive metabolite retained its activity up to 60 °C; however, reduced activity was observed as the temperature exceeded 70 °C, and its activity was lost after autoclaving for 15 min at 121 °C. On the contrary, the antifungal activity was preserved in the presence of proteinase-K, lysozyme and alpha-amylase. Similarly, the antifungal activity was not significantly affected by the presence of tween 20, 40, 80 nor SDS and cetrimide (Figure S3). It also reserved its activity over a wide pH range (6.0–7.8) (Figure S3). Moreover, the antifungal compound produced by Lysinibacillus isolate MK212927 was assayed for fungistatic or fungicidal mode of action. The fungus A. niger showed no regrowth after it had been transferred to a new SDA plate and monitored over 7 days. These results indicated that the metabolite produced has fungicidal activity.
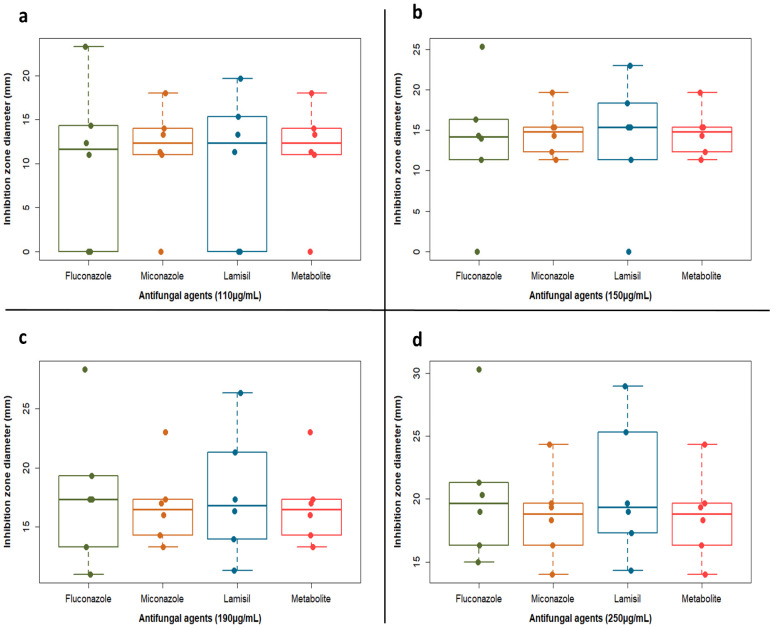
2.7. Evaluation of the Antifungal Activity of the Lysinibacillus Isolate MK212927 Metabolite Compared to the Commercially Available Antifungal Agents
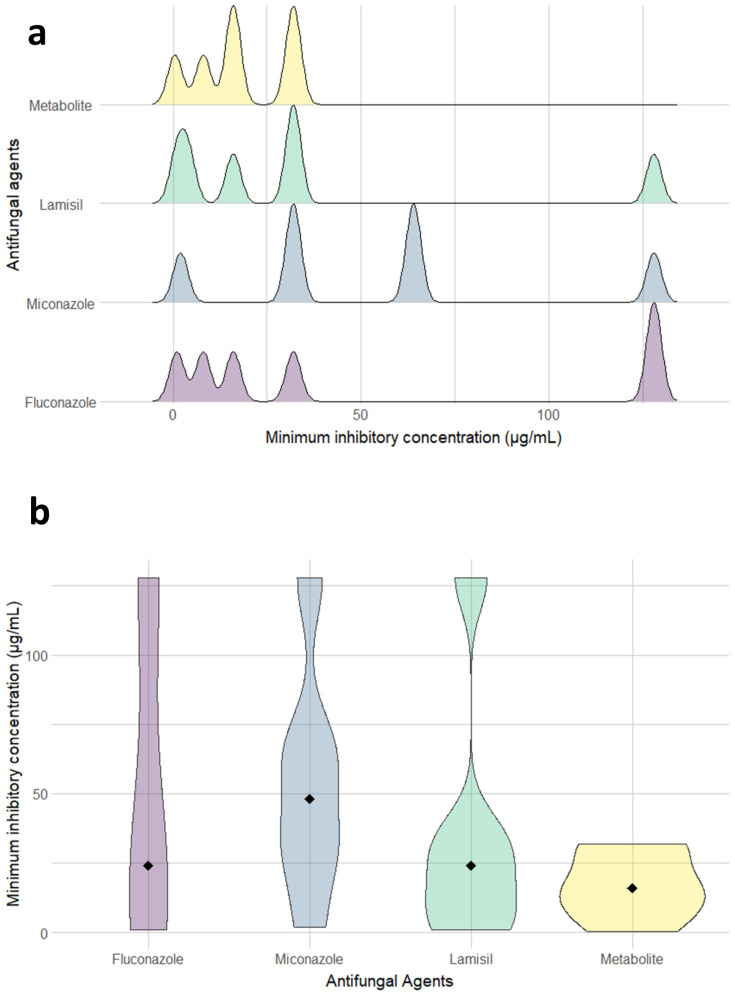
Table 2 illustrates the antifungal spectrum of three chosen antifungal agents and the purified metabolite at concentrations of 110, 150, 190 and 250 μg/mL against C. albicans clinical isolates. The purified metabolite showed comparable results to the chemical agents, with inhibition zones in the range of 11–25 mm as against 11–30, 11–25 and 11–29 mm zones of fluconazole, miconazole and Lamisil, respectively. Mostly, inhibition zones documented for the metabolite were less dispersed around the median and with very few outliers (Figure 3). Interestingly, the purified compound showed enhanced antifungal activity (i.e., inhibition zones between 11 and 12.5mm) against isolates 1 and 3 exhibiting resistance to fluconazole (i.e., no inhibition zones) at concentrations of 110 and 150 μg/mL. It is worth mentioning that MIC determination using broth microdilution method confirmed the promising inhibitory activity of the metabolite with results in the range of 0.5–32 μg/mL, while fluconazole, miconazole and Lamisil showed an extended range of MIC values reaching 128 μg/mL (Figure 4a and Table S3).
Table 2.
In vitro susceptibilities of six C. albicans isolates to fluconazole, miconazole, Lamisil, and the antifungal metabolite determined by agar well diffusion method.
| C. albicans Isolate | Inhibition Zone Diameter (mm) ± SD | |||
|---|---|---|---|---|
| 110 µg/mL | 150 µg/mL | 190 µg/mL | 250 µg/mL | |
| Fluconazole | ||||
| 1 | 0 | 0 | 11 ± 0.33 | 15 ± 0.26 |
| 2 | 12 ± 0.58 | 14 ± 0.26 | 17 ± 0.33 | 20 ± 0.33 |
| 3 | 0 | 11 ± 0.33 | 13 ± 0.33 | 16 ± 0.58 |
| 4 | 11 ± 0.25 | 14 ± 0.25 | 17 ± 0.58 | 19 ± 0.33 |
| 5 | 23 ± 0.58 | 25 ± 0.58 | 28 ± 0.58 | 30 ± 0.33 |
| 6 | 14 ± 0.58 | 16 ± 0.58 | 19 ± 0.58 | 21 ± 0.58 |
| Miconazole | ||||
| 1 | 0 | 11 ± 0.33 | 14 ± 0.33 | 16 ± 0.33 |
| 2 | 13 ± 0.33 | 15 ± 0.33 | 17 ± 0.33 | 19 ± 0.67 |
| 3 | 11 ± 0.33 | 12 ± 0.46 | 13 ± 0.33 | 14 ± 0.26 |
| 4 | 11. ± 0.33 | 14 ± 0.36 | 16 ± 0.33 | 18 ± 0.33 |
| 5 | 18 ± 0.33 | 19 ± 0.67 | 23 ± 0.26 | 24 ± 0.33 |
| 6 | 14 ± 0.46 | 15. ± 0.33 | 17 ± 0.33 | 19 ± 0.33 |
| Lamisil | ||||
| 1 | 0 | 11 ± 0.33 | 14 ± 0.26 | 17 ± 0.33 |
| 2 | 11 ± 0.33 | 15 ± 0.33 | 16 ± 0.58 | 19. ± 0.67 |
| 3 | 0 | 0 | 11 ± 0.33 | 14 ± 0.58 |
| 4 | 15 ± 0.33 | 18 ± 0.5 | 21 ± 0.33 | 25 ± 0.58 |
| 5 | 19 ± 0.67 | 23 ± 0.33 | 26 ± 0.33 | 29 ± 0.6 |
| 6 | 13 ± 0.33 | 15 ± 0.33 | 17 ± 0.33 | 19 ± 0.6 |
| Antifungal metabolite | ||||
| 1 | 0 | 11 ± 0.33 | 14 ± 0.33 | 16 ± 0.33 |
| 2 | 13 ± 0.33 | 15 ± 0.66 | 17 ± 0.33 | 19 ± 0.69 |
| 3 | 11 ± 0.33 | 12 ± 0.33 | 13 ± 0.33 | 14 ± 0.45 |
| 4 | 11 ± 0.33 | 14 ± 0.33 | 16 ± 0.2 | 18 ± 0.33 |
| 5 | 18 ± 0.6 | 19 ± 0.67 | 23 ± 0.3 | 24 ± 0.33 |
| 6 | 14 ± 0.6 | 15 ± 0.33 | 17 ± 0.3 | 19 ± 0.67 |
Figure 3.
Boxplots showing inhibition zone diameter (mm) vs. antifungal agents (fluconazole, miconazole, Lamisil and the active metabolite) at different concentrations: (a) 110 µg/mL, (b) 150 µg/mL, (c) 190 µg/mL and (d) 250 µg/mL. Dots representing each sample were overlaid to show the actual variability and distribution of the data. Plot was created by R (“ggplot2”) package.
Figure 4.
(a) Ridgeline plots showing the distribution of minimum inhibitory concentrations (µg/mL) for fluconazole, miconazole, Lamisil and the metabolite against six isolates of C. albicans. Area under the ridgeline is plotted after calculation of density estimates from the provided data. Plot was created by R (“gg ridges”) package. (b) Violin plots representing the kernel probability density of C. albicans isolates at different values of the minimum inhibitory concentrations (µg/mL) for fluconazole, miconazole, Lamisil and the metabolite. The filled black diamond signifies the MIC median value allowing better assessment of the data obtained from different antifungals. Plot was created by R (“ggplot2”) package.
The metabolite had a median MIC value of 16, which was one third that recorded by miconazole and slightly less than that recorded by Lamisil and fluconazole (Figure 4b and Table 3). Next, we used Kruskal–Wallis One Way Analysis of Variance to test the differences between the effects of the tested antifungal agents. Despite the trend of discrepancies in the recorded medians among the tested antifungals, these differences did not reach statistical significance (p-value = 0.427); this could be due to the low number of isolates in each group. However, the metabolite displayed MIC90 32 μg/mL, which was equipotent to Lamisil, 2-fold more potent than MN and 4-fold the potency of fluconazole (Table 3). Of note, the results also emphasized the improved activity against the two isolates displaying resistance to fluconazole, miconazole and Lamisil according to the interpretive guidelines of CLSI for in vitro susceptibility of Candida spp.
Table 3.
In vitro susceptibilities of six C. albicans isolates to fluconazole, miconazole, Lamisil, and the antifungal metabolite determined by broth microdilution.
| Antifungal Product | Susceptibility (μg/mL) | |||
|---|---|---|---|---|
| Range | Median c | MIC50 a | MIC90 b | |
| Fluconazole | 1–128 | 24 | 16 | 128 |
| Miconazole | 2–128 | 48 | 32 | 64 |
| Lamisil | 1–128 | 24 | 16 | 32 |
| Antifungal metabolite | 0.5–32 | 16 | 16 | 32 |
a,b 50% and 90%, MICs at which 50 and 90% of isolates are inhibited, respectively; c in calculation of the median values, MICs of >64 μg/mL were classed as 128 μg/mL.
2.8. Spectral Analyses of the Purified Antifungal Compound
The ultraviolet (UV) absorption spectrum showed a maximum absorption peak (λ max) at 219 nm (Figure S4). The FTIR chart showed no absorption peaks between 3100 and 3500 cm−1 nor between 1630 and 1820 cm−1, which indicated that the compound had no OH stretch nor carbonyl groups, respectively. On the other hand it exhibited an absorption at 3000–3100 cm−1 characteristic of the (SP2-1s)=C-H bonds in aromatic rings. In addition, aromatic rings showed absorption in the region 690–900 cm−1 because of the out plane C-H bending. Besides, the compound showed several absorptions between 1450 and 1600 cm−1 owing to C=C stretching in the aromatic ring. In the double bond region, a strong peak at 1600 cm−1 denoted the presence of an alkene (Figure S4). The obtained results were in accordance with those of the standard terbinafine (Figure S4).
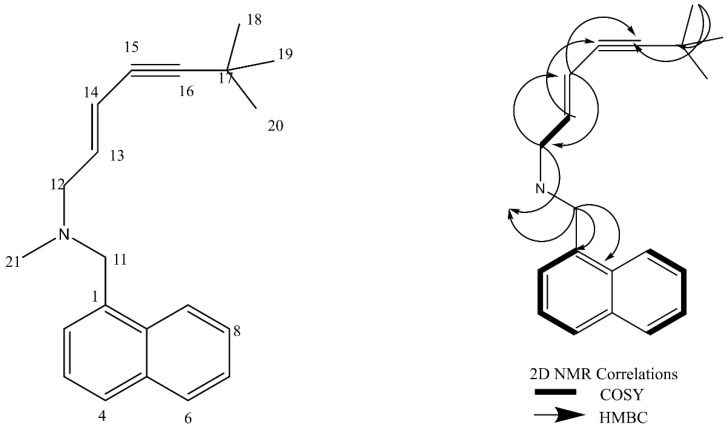
Results of extensive 1D and 2D NMR experiments are listed in Table 4. The chemical structure of the active metabolite produced by Lysinibacillus isolate MK212927 based on the spectral data showing 1H NMR,13C NMR signals assignments and 2D NMR (COSY, HMBC) correlations is delineated in Figure 5. Careful analysis of the generated spectra (Figures S5 and S6) showed great resemblance to those reported in the literature for the potent antifungal drug terbinafine (Lamisil)® [36]. Terbinafine is a synthetic allylamine; however, we report a new microbial producer of this highly active antifungal compound.
Table 4.
1H NMR and 13C NMR data of the pure metabolite in ppm (multiplicity, J in Hz) a.
| Position | δH (MeOD, 400 MHz, J in Hz) | δC (MeOD, 100 MHz) |
|---|---|---|
| 1 | - | 132.1 (C) |
| 2 | 7.54 (m) | 125.9 (CH) |
| 3 | 7.64 (m) | 126.6 (CH) |
| 4 | 8.2 (m) | 123.4 (CH) |
| 5 | - | 134 (C) |
| 6 | 7.54 (m) | 126.1 (CH) |
| 7 | 7.93 (m) | 128.7 (CH) |
| 8 | 7.93 (m) | 129.7 (CH) |
| 9 | 7.64 (m) | 129.6 (CH) |
| 10 | - | 131.9 (C) |
| 11 | 4.4 (s) | 56.8 (C) |
| 12 | 3.6 (d, 7) | 58.2 (CH2) |
| 13 | 5.9 (d, 15.9) | 118.2 (CH) |
| 14 | 6.1 (m) | 131.7 (CH) |
| 15 | - | 76.6 (C) |
| 16 | - | 100.1 (C) |
| 17 | - | 27.6 (C) |
| 18–20 | 1.23 (s) | 29.9 (CH3) |
| 21 (N-CH3) | 2.52 (s) | 39.9 (CH3) |
a Assignments were done based on COSY, HSQC and HMBC experiments.
Figure 5.
Chemical structure of the active metabolite produced by Lysinibacillus isolate MK212927 based on the spectral data showing 1H NMR,13C NMR signals assignments and 2D NMR (COSY, HMBC) correlations.
3. Discussion
In this study, a total of 105 soil samples were gathered from various regions in Egypt and were processed for the isolation of bacterial strains showing inhibitory effect against two clinically relevant human fungal pathogens. Cross-streak and agar cup-plate methods were used to verify the production of the antifungal metabolite. Both methods confirmed that isolate S6 strongly inhibited the growth of fungal target pathogens. This Gram-positive isolate was identified as Lysinibacillus sp. MK212927 based on biochemical tests and 16S ribosomal RNA sequence (NCBI GenBank accession number: MK212927.1). Previous studies reported that the genus Lysinibacillus can produce valuable bioactive agents [37,38,39], while Ahmad and colleagues [40] described the antibacterial nature of the cell-free supernatant of a certain Lysinibacillus isolate. In another study, the species Lysinibacillus fusiformis were found to produce potential antifungal metabolites against certain fungi causing plant diseases [41]. However, comparison of the obtained cultural, biochemical and molecular characteristics, from the nucleotide DNA sequences of the 16S ribosomal RNA of our Lysinibacillus isolate MK212927 to those of the related Lysinibacillus sp. [22], indicated that our isolate was different from these previously reported Lysinibacillus spp. This species difference was also confirmed by using molecular phylogenetic analysis of our isolate using maximum likelihood method based on the Kimura 2-parameter model in MEGA X software. Our data supported these studies, demonstrating the potent antifungal properties of the metabolite produced by our Lysinibacillus isolate MK212927.1. Additionally, we have described for the first time the significant inhibitory effect of this antifungal metabolite against clinical isolates of the human pathogenic fungi C. albicans and A. niger. The optimized factors affecting the production of this metabolite were reported in our previous study [42].
The present investigation correspondingly defines the nature of the metabolite produced by Lysinibacillus isolate to elucidate its structure and demonstrate the effect of different factors on its activity. As a start, tests performed indicated that the anti-fungal metabolite was not proteinaceous in nature. Eight organic solvents were used to extract the active metabolite. The maximum yield (1.07 g/200 mL) was obtained by using ethyl acetate. This is in accordance with many reports where most of the antifungal metabolites are extracted with ethyl acetate [43,44]. Next, we purified the compound from the culture extract of Lysinibacillus isolate MK212927.1 using silica gel column chromatography techniques. Silica gel could tightly attach with high polar compound; therefore, low polar compounds were eluted from column before high polar compounds, which were sequentially eluted by increasing polarity of developing solvent [45]. Fractions 43–47 were the most bioactive ones, with confirmed antifungal activity verified by bioautography against C. albicans. A linear relationship was observed between the inhibition zones and the concentration of the purified extract; both increased proportionally.
Generally, secondary bacterial metabolites are stable because they are end products and not subject to alteration by the producing microorganisms. On that account, we subjected our bioactive metabolite to stability studies by examining the influence of various factors (temperature, pH, detergents and enzymes) on its antifungal activity. The metabolite was moderately thermostable, with the highest activity recorded at 30 and 40 °C, but totally lost its activity when autoclaved. It retained its maximum activity around neutral pH; this is in accordance with the properties of a previously reported antifungal metabolite produced by Bacillus spp. [46]. Moreover, the metabolite reserved its antifungal activity regardless of the employed enzymes and detergents, which highlights advantageous features at the industrial level.
Next, we compared the activity of commonly used antifungals to the purified metabolite. Intriguingly, the metabolite exhibited analogous activity to all the chemical agents and even superior outcome in some cases. In comparison to the tested antifungal agents, the minimum inhibitory concentration of the antifungal compound that inhibited 90% of the growth (MIC90) was equivalent to that of Lamisil, half of miconazole and one fourth of fluconazole. Even though fluconazole is the most common treatment of Candida spp. infections, resistant strains have emerged due to its repeated use [47]. An additional advantage of the metabolite was the enhanced effect against C. albicans clinical isolates resistant to the tested agents, fluconazole, miconazole and Lamisil. Antifungal compounds usually exhibit either a fungistatic or fungicidal mode of action in preventing fungal growth. Fungicidal compounds kill fungal cells, hence, no rejuvenation occurs after the compound is removed. On the contrary, fungistatic agents are characterized by reversible growth inhibition, where fungal cells continue to grow upon elimination of the antifungal agent [48]. In this study, plating of the fungi taken from the dual assay plate did not show any resumed growth. This indicated fungicidal effect of the compound produced by Lysinibacillus isolate MK212927.1. Furthermore, meta-analysis studies on the pharmacotherapy of invasive candidiasis detected higher therapeutic success rates among patients treated with fungicidal therapy when compared to fungistatic therapy [49,50]. Spectral analyses, including IR, 1D-NMR and 2D-NMR experiments (COSY, HSQC and HMBC), have been used in attempt to elucidate the structure of the compound. The data provided by these analyses confirmed the structure to be identical with that of terbinafine [51,52].
Terbinafine was discovered in 1983 and approved in 1996 in the US as the first oral allylamine antifungal agent [53]. Terbinafine inhibits ergosterol synthesis, an essential component of the fungal cytoplasmic membrane, by inhibiting the fungal cell membrane synthesis pathway through inhibition of squalene monooxygenase (squalene 2, 3-epoxidase) enzyme [54]. Since its approval, terbinafine has demonstrated high cure rates and well-established safety record. In contrast to azoles, terbinafine does not inhibit CYP3A4 isoenzyme during its metabolism and thus drug–drug interactions are low. This advantage enables the use of terbinafine for patients who are likely to be receiving concomitant medication, including antidiabetic and antihypertensive drugs [55]. Terbinafine is synthetically developed by Novartis under the trade name Lamisil®. Hence, the significance of this study remains that it reports the use of a new microbial process to produce terbinafine. Drugs produced by microbial processes surpass chemically produced ones in terms of their high specificity range and being easily produced from renewable carbon sources [56]. Recently, Abdel-Kader and Muharram obtained terbinafine from the culture media of Streptomyces spp. KHF12 isolated from a soil sample collected from Adilamm, KSA [57]. In our study, we used Lysinibacillus spp., a bacterium that passes through exponential phase during 3 to 10 h of growth and enters into stationary phase after 12 h of incubation, while typical Streptomyces colonies can be selected after 7 days [58]. Thus, our strain shows enhanced kinetics of terbinafine production that could be further optimized for industrial purposes.
4. Materials and Methods
4.1. Soil Sampling and Isolation of Bacterial Isolates
A total of 105 samples from soil were randomly gathered from various agricultural regions in Egypt over six months. An open-end soil borer was used to take samples from a depth of 10–20 cm then placed in tightly closed polyethylene plastic bags and stored at 4 °C for further processing. Briefly, 1 g of each soil sample was transferred into 100-mL normal saline, heated for 30–60 min at 80–100 °C to eliminate the non-spore-forming bacteria. Samples were then allowed to settle, and 100 μL of the supernatant was inoculated on yeast malt extract agar, starch casein agar, nutrient agar, trypticase soy agar and Sabouraud’s dextrose agar (SDA) and incubated for 1 week at temperatures of 28 °C and 37 °C [59]. The isolated colonies were then picked up, propagated on the same culture media, and preserved at 4 °C for later assays.
4.2. Screening for Production of Metabolites with Antifungal Activity
For the detection of diffusible antifungal metabolites, cross-streak method was used against C. albicans ATCC 10231. The screened isolate was streaked as a dense line in the center of the agar plate, and the C. albicans strain was streaked at right angle near the periphery of the plate. After incubation at 28 °C for 48 h, we recorded the size of inhibition zones [58,60]. Screening for the antifungal activity was also carried out using the dual-culture method against the mold A. niger clinical isolate recovered from Kasr Al-Ainy Hospital, Cairo university, Egypt (the ethical committee Nr. ENERC-ASU-230 at faculty of pharmacy and the hospital Ethics Committee have approved the study). Study protocols and experiments included agreed with international declarations for biomedical research ethics, relevant regulations, and guidelines. First, A. niger clinical isolate was cultured on SDA medium form 5 days to 1 week at 28 °C; then, a small block from the proliferated culture was centrally placed on another SDA plate. Then, a loopful of 24-h-old, screened isolate was cultured as a wide band approximately 3 cm away from the block of mycelia at two opposite margins. Plates cultured with fungus without any bacteria were served as control [61]. Finally, after 1 week incubation at 28 °C, the inhibition of fungal growth was calculated as the zone between the margins of streaked bacteria and the mycelia of the fungus [62].
Isolates that showed preliminary antifungal activity were selected for confirmatory testing by the agar cup-plate method [63]. In brief, the isolates were inoculated in 100 mL of culture media under shaking conditions at 37 °C. After 24 h, the resulting culture broths were filtered then centrifuged at 6000 rpm for 15 min (Hettich Zentrifugen EBA 12, Tuttlingen, Germany) and the supernatants were examined for their antimycotic activity against C. albicans standard strain ATCC 10,231 (OD=0.5 McFarland standard at 530 nm). The plates were incubated at 28 °C, and the inhibition zones were measured after 24 h. Each experiment was performed in triplicate, and mean values of the inhibition zones diameters were recorded [64,65,66].
Ultimately, the bacterial isolate with the highest antimycotic activity was inoculated into TSB and incubated under shaking conditions (250 rpm) overnight at 37 °C. After that, centrifugation of 1 mL aliquots of these cultures was carried for 10 min at 10.000 rpm using a micro centrifuge (Hettich Zentrifugen EBA 12, Tuttlingen, Germany) in Eppendorf tubes. The obtained bacterial pellets were resuspended into 1 mL aliquots of glycerol stock medium. The Eppendorf tubes were then kept at −80 °C for long-term preservation of bacteria.
4.3. Identification of the Selected Isolate
The isolate showing the highest antifungal activity was identified using microscopical, biochemical and molecular approaches; 16S ribosomal RNA gene amplification and sequencing [67]. Staden package program was used to perform DNA analysis and sequence assembly (http://staden.sourceforge.net/ (accessed on 30 November 2021). The bioedit 7.2 software was used to get a consensus sequence of the 16S ribosomal RNA (https://bioedit.software.informer.com/7.2/ (accessed on 30 November 2021)), and by using BLASTn (Basic Local Alignment Search Tool of nucleotides) it was blasted in the GenBank database (http://blast.ncbi.nlm.nih.gov/Blast.cgi (accessed on 30 November 2021)). The homology percentage between the submitted sequence and the sequence in the data base was demonstrated. MEGA X software served to get the evolutionary analyses [68]. Alignment of the 16S rRNA sequence of each strain was done using MUSCLE against representative nucleotide sequences obtained from GenBank. Moreover, phylogenetic analyses were carried out through likelihood method based on the Kimura 2-parameter model with 1000 replicates bootstrap analysis [69]. The 16S ribosomal RNA sequence was deposited in the NCBI (accession number, MK212927), and the bacterial strain was deposited in the Culture Collection Ain Shams University (CCASU) belonging to WDCM (the World Data Centre for Microorganisms) (strain number, CCASU-MK212927).
4.4. Production of the Antifungal Metabolite(s)
A loopful from the selected bacterial culture (24 h old) was transferred to 50 mL trypticase soy broth (TSB) to prepare the seed culture and incubated for 15–18 h at 30 °C under shaking conditions (250 rpm). About 1 mL of the obtained culture was withdrawn to a micro centrifuge tube and then underwent centrifugation for at 16,000 rpm for 10 min (Centurion Scientific-K240R), rinsed with 1 mL sterile normal saline, and then transferred to 30 mL of the basal production medium. The basal production medium was prepared according to Singh et al. [41]. After inoculation by 1 mL of seed culture (final count of 1 × 107 cfu/mL), the production flasks were incubated at 150 rpm and 30 °C.
4.5. Extraction of the Antifungal Metabolite(s)
The resulting culture broth from the production process was centrifuged for 30 min at 10,000; then, the resulting supernatant was harvested, filtered and stored at 4 °C for further assay [43,45]. Initially, to inspect peptide nature of the metabolite, (NH4)2SO4 (608 g/L) was added to the culture supernatant, kept overnight at 4 °C under shaking conditions, and monitored for peptide precipitation, if any [41].
For the extraction process, equal volumes of different solvents such as ethyl acetate (EA), chloroform, methanol, n-butanol, hexane, ethanol and diethyl ether were used [70]. Afterwards, the obtained extract was concentrated to dryness under reduced pressure at 45 °C using rotary evaporator (Staurt RE300, Warwickshire, UK) [45]. The antimycotic activities of the extracts were tested by using agar cup-plate method, and negative controls were prepared using the respective solvents [70,71]. The organic solvent that gave superior extraction evidenced by enhanced zone of inhibition was selected for further extraction procedures [43].
4.6. Thin Layer Chromatography (TLC) Analysis
TLC was the method of choice for the separation of the bioactive compound into its components. The crude EA extract was spotted on silica TLC plate and developed in different solvent systems: EA 1:9 hexane (v/v), EA 1:9 diethyl ether (v/v), methanol 1:9 EA (v/v), EA 1:9 chloroform (v/v), n-butanol 1:9 EA (v/v) and EA 1:9 dichloromethane (v/v). The separated metabolite(s) were then examined under UV lamp (UVitec®) at 254 nm and 365 nm and confirmed by the formation of localized brown spots after subjecting the TLC plates to iodine vapors in a fuming hood [45]. The solvent system that showed improved resolution of the spots was used at different ratios for the gradient elution of the compound.
4.7. Purification of the Bioactive Metabolite(s) through Activity Guided Fractionation
The dry mass of EA crude extract was adsorbed on a small amount of column grade silica gel, 60–120 mesh size (Merck, Germany). The silica gel column (3.5 × 80 cm) was first eluted with 100% n-hexane, and then we used linear gradients of n-hexane and ethyl acetate, increasing the polarity of the solvents. Fractions (each of 15 mL) were collected at regular intervals (1 mL/min flow rate) [70]. The fractions were loaded separately on silica TLC plates, developed with the same solvent system, and those exhibiting the same retardation factor (RF) values were pooled together [45]. The pooled fractions (PF) were concentrated using rotary evaporator at 45 °C; then, bioautography method was used to check their antifungal activity against test organism C. albicans ATCC 10231 [45]. The inhibitory zone resulting from bioautography method was visible after incubation at 28 °C for 1 day [72]. Fractions showing significant and potent antimycotic activity were re-purified as mentioned before; then, TLC plates were used to check their purity and were designated for further characterization [73].
4.8. Correlation between the Metabolite Concentration and Diameter of Inhibition Zone Using Agar Well Diffusion
The most active purified fraction of the metabolite obtained above was diluted in DMSO to achieve concentrations of 110, 130, 150, 170, 190, 210, 230, 250 and 270 μg/mL, and 200 µL of each concentration were added in separate cups in SDA plates inoculated with C. albicans ATCC 10231. After 24 h incubation at 28 °C for, the diameters of the inhibition zones were recorded and plotted against the corresponding concentrations.
4.9. Effect of Heat, pH, Detergents and Enzymes on Stability and Activity of the Antifungal Compound
To demonstrate the stability of the antifungal metabolite at different temperatures, 7 screw capped ampoules, each with 100 μg/mL of the metabolite, were kept in a water bath at temperatures 30, 40, 50, 60, 70 and 80 °C for 1 h, and the last ampoule was subjected to autoclaving temperature (121 °C for 15 min) [73]. Correspondingly, the effect of pH on stability of the metabolite was concluded through mixing 100 μg of the compound with 1 mL of 0.1 M phosphate buffer of different pH values (5.7–8.0) and then incubated at 30 °C for 1 h. Susceptibility of the antifungal metabolite to denaturation by various detergents, including tween 20, tween 40, tween 80, sodium dodecyl sulphate (SDS) and cetrimide, was also tested. Detergents were dissolved in distilled water at concentration of 0.01 g/mL. One hundred µL of the antifungal solution (100 μg/mL) was mixed with 10 mL of detergent and incubated at 30 °C for 6 h. The antifungal solution without any detergents served as control [74]. Similarly, we explored the effect of proteinase K, lysozyme and alpha amylase (Sigma-Aldrich, Cairo, Egypt) on the metabolite. All the enzymes were dissolved in distilled water at concentration 1 mg/mL, and 100 μL of the antifungal solution was mixed with 10 mL enzyme and incubated at 30 °C for 3 h. The antifungal solution without any enzymes acted as control [74]. The residual antifungal activities of the metabolite after heat, pH, detergents and enzyme treatments were determined by the agar cup-plate method using 100 µL of the antifungal compound per well [73]. Each experiment was performed in triplicate, and the mean values of the inhibition zones were recorded.
4.10. Investigation for Fungicidal and/or Fungistatic Mode of Action
A single 10-mm culture plug was taken from the edges of the inhibition zones of the Lysinibacillus isolate against the fungus A. niger and transferred to a fresh SDA plate, which was consequently incubated for a week at 28 °C [75,76]. Throughout the incubation period, growth or lack of growth of A. niger was examined. Regrowth was suggestive of fungistatic activity and absence of growth denoted fungicidal properties of the metabolite produced by Lysinibacillus isolate.
4.11. Evaluation of the Antifungal Activity of the Metabolite
We compared the efficacy of the metabolite to three antifungal products commonly used for treatment of Candida spp. infections, including fluconazole (Epico Pharmaceuticals Co., Ramadan City, Egypt), miconazole (Medical Union Pharmaceuticals, Nasr City, Egypt) and Lamisil (Novartis Pharmaceuticals, Cairo, Egypt). All tested agents were prepared at concentrations of 110, 150, 190 and 250 µg/mL in DMSO, and the respective solvent alone was used as control in the agar well diffusion method. We employed six clinical isolates of C. albicans with variable susceptibility profiles as our target organisms. The reported results are the mean values of three replicates ± standard deviation.
4.12. Minimal Inhibitory Concentration (MIC) Determination
The MIC values for the purified metabolite, fluconazole, miconazole and Lamisil were determined using different concentrations (0.125, 0.25, 0.5, 1, 2, 4, 8, 16, 32, 64 and 128 µg/mL) and following the Clinical and Laboratory Standards Institute (CLSI, 2018) protocol M27-A3 for fungi [77].
4.13. Spectral Analyses of the Antifungal Compound Assay
Ultraviolet (UV) spectrum was recorded on Shimadzu UV-1800 spectrophotometer, 1mg of sample was dissolved in 10 mL dimethylsulfoxide (DMSO) and the spectra were recorded at 200–400 nm range. Fourier transform infrared spectrum (FTIR) was determined by Bruker® Optik GmbH, Germany in the range 400–4000 cm−1 by using methanol as the medium for the preparation of the sample. 1H NMR and 13C NMR spectra were measured in methanol on Bruker® Avance III HD (400 MHz) spectrometer, Germany, equipped with a 5mm broad-band multinuclear (PABBO) probe. The chemical shifts were reported in parts per million (ppm) relative to TMS (δ0.0) used as internal standard. Two-dimensional (2D) NMR analyses, 1H-1H Correlation Spectroscopy (COSY), heteronuclear single quantum coherence (HSQC) and 1H-13C heteronuclear Multiple Bond Correlation Spectroscopy (HMBC) were also carried out on Bruker® Avance III HD (400 MHz) spectrometer. All spectroscopic measurements were performed at Drug Discovery and Development Research Center at Faculty of Pharmacy, Ain Shams University, Abbassia, Cairo, Egypt.
4.14. Statistical Analysis
All experiments were carried out in triplicate, and the data were expressed as the mean ± SD. Statistical analysis was conducted using R statistical platform (https://www.r-project.org (accessed on 30 November 2021)). Among R-packages used in data analysis and visualization are readxl, ggridges and boxplot. Kruskal–Wallis one-way analysis of variance on ranks was used to test the significance among different groups. p-value < 0.05 was considered to indicate statistically significant differences.
5. Conclusions
In this study, we describe the isolation and purification of terbinafine from a new fast-growing microbial source, Lysinibacillus sp. MK212927, recovered from Egyptian soil. This highlights the role of microbial communities recovered from soil as an abundant resource of antifungal agents required to overcome the currently emerging fungal resistance. It is deemed necessary to note that this is the first report of terbinafine production by Lysinibacillus sp. MK212927, a fast-growing microbial source, with relatively high yield and subject to potential optimization for industrial production capabilities.
Acknowledgments
Authors extend their gratefulness to Microbiology and Immunology Department, Faculty of Pharmacy, Ain Shams University, and Ahram Canadian University (ACU) Cairo, Egypt for their great help and support regarding the current study. Authors also acknowledge Taif University, Taif, Saudi Arabia for funding current work by Taif University Researchers Supporting Project number (TURSP—2020/116) at Taif University.
Supplementary Materials
The following are available online. Table S1: Screening for the antifungal activity of the metabolites produced by isolates S6, F1 and F2, Table S2: The yield of different solvent extracts obtained from Lysinibacillus isolate and the corresponding inhibition zones against C. albicans and A. niger, Table S3: Distribution of MIC for fluconazole, miconazole, lamisil and the antifungal metabolite against six isolates of C. albicans, Figure S1: Dual-culture technique showing inhibitory effect of Lysinibacillus (S6) against A. niger. Left plate shows clear zone between the edges of fungal mycelia and bacterial colonies. Right plate Control plate without tested bacteria, Figure S2: Bioautography method used to determine the antifungal activity of the pooled fractions obtained from column chromatography against C. albicans. Left plate highlights the zone of inhibition caused by the fractions with the most potent antifungal activity. Right plate shows no inhibitory effect of purified fractions, Figure S3: The effect of different (a) temperatures, (b) pH, (c) detergents, and enzymes on the stability of the purified antifungal metabolite of Lysinibacillus isolate, Figure S4: (a) UV and (b) FTIR spectra of the purified antifungal compound of Lysinibacillus isolate, Figure S5 (a) 1HNMR and (b) 13C NMR spectra of the purified antifungal compound of Lysinibacillus isolate, Figure S6: 2D NMR spectra of the purified antifungal compound of Lysinibacillus isolate (A) HMBC spectrum, (B) HSQC spectrum and (C) COSY spectrum.
Author Contributions
Study conception and design: S.E.E.-S., N.A.A., H.-E.H.O., G.S.E.-H., A.E.A. and K.M.A. Acquisition of data: S.E.E.-S., N.A.A., H.-E.H.O., G.S.E.-H., A.E.A. and K.M.A. Analysis and interpretation of data: N.A.A., G.S.E.-H., A.E.A. and K.M.A. Drafting of manuscript: S.E.E.-S., N.A.A. and G.S.E.-H., Critical revision: N.A.A., H.-E.H.O., G.S.E.-H., A.E.A. and K.M.A. funding acquisition: S.E.E.-S., H.-E.H.O. and K.M.A. All authors have read and agreed to the published version of the manuscript.
Funding
The current work was funded by Taif University Researchers Supporting Project number (TURSP—2020/116), Taif University, Taif, Saudi Arabia.
Data Availability Statement
All data are included within the manuscript and supplementary file.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of the compounds of this study are available from the authors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fuller J., Dingle T.C., Bull A., Shokoples S., Laverdière M., Baxter M.R., Adam H.J., Karlowsky J.A., Zhanel G.G. Species distribution and antifungal susceptibility of invasive Candida isolates from Canadian hospitals: Results of the CANWARD 2011–16 study. J. Antimicrob. Chemother. 2019;74:iv48–iv54. doi: 10.1093/jac/dkz287. [DOI] [PubMed] [Google Scholar]
- 2.Shishodia S.K., Tiwari S., Shankar J. Resistance mechanism and proteins in Aspergillus species against antifungal agents. Mycology. 2019;10:151–165. doi: 10.1080/21501203.2019.1574927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pérez-Cantero A., López-Fernández L., Guarro J., Capilla J. Azole resistance mechanisms in Aspergillus: Update and recent advances. Int. J. Antimicrob. Agents. 2020;55:105807. doi: 10.1016/j.ijantimicag.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 4.Pfavayi L.T., Denning D.W., Baker S., Sibanda E.N., Mutapi F. Determining the burden of fungal infections in Zimbabwe. Sci. Rep. 2021;11:13240. doi: 10.1038/s41598-021-92605-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lass-Flörl C., Samardzic E., Knoll M. Serology anno 2021–fungal infections: From invasive to chronic. Clin. Microbiol. Infect. 2021;27:1230–1241. doi: 10.1016/j.cmi.2021.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Lamoth F., Lockhart S.R., Berkow E.L., Calandra T. Changes in the epidemiological landscape of invasive candidiasis. J. Antimicrob. Chemother. 2018;73:i4–i13. doi: 10.1093/jac/dkx444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt-Westhausen A.M., Priepke F., Bergmann F.J., Reichart P.A. Decline in the rate of oral opportunistic infections following introduction of highly active antiretroviral therapy. J. Oral Pathol. Med. 2000;29:336–341. doi: 10.1034/j.1600-0714.2000.290708.x. [DOI] [PubMed] [Google Scholar]
- 8.Oliscovicz N., Pomarico L., de Araújo Castro G.F., Souza I.P. Effect of highly active antiretroviral therapy use on oral manifestations in pediatric patients infected with HIV. Indian J. Dent. Res. 2015;26:200–204. doi: 10.4103/0970-9290.159169. [DOI] [PubMed] [Google Scholar]
- 9.Quindos G., Gil-Alonso S., Marcos-Arias C., Sevillano E., Mateo E., Jauregizar N., Eraso E. Therapeutic tools for oral candidiasis: Current and new antifungal drugs. Med. Oral Patol. Oral Cir. Bucal. 2019;24:e172–e180. doi: 10.4317/medoral.22978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bod P., Terdy L., Trischler F., Fekecs E., Demeter M., Lauko A., Domany G., Komlosi G.S., Varga K. Process for Preparing a Substituted Allylamine Derivative and the Salts Thereof. Google Patents US20030028032A1. 2004. [(accessed on 4 December 2021)]. Available online: https://patents.google.com/patent/US20030028032A1/en.
- 11.Stuetz A., Petranyi G. Synthesis and antifungal activity of (E)-N-(6,6-dimethyl-2-hepten-4-ynyl)-N-methyl-1-naphthalenemethanamine (SF 86-327) and related allylamine derivatives with enhanced oral activity. J. Med. Chem. 1984;27:1539–1543. doi: 10.1021/jm00378a003. [DOI] [PubMed] [Google Scholar]
- 12.Fuglseth E., Otterholt E., Høgmoen H., Sundby E., Charnock C., Hoff B.H. Chiral derivatives of Butenafine and Terbinafine: Synthesis and antifungal activity. Tetrahedron. 2009;65:9807–9813. doi: 10.1016/j.tet.2009.09.067. [DOI] [Google Scholar]
- 13.Gupta B., Ravindra Babu B., Gyanda K., Panda S.S., Jain S.C. Stereoselective methodology for the synthesis of an antifungal allylamine: Terbinafine. Lett. Org. Chem. 2014;11:141–144. doi: 10.2174/15701786113106660078. [DOI] [Google Scholar]
- 14.Hergert T., Mátravölgyi B., Örkényi R., Éles J., Faigl F. Multistep batch-flow hybrid synthesis of a terbinafine precursor. J. Flow Chem. 2021;2021:1–7. doi: 10.1007/s41981-021-00188-9. [DOI] [Google Scholar]
- 15.Da Matta D., Souza A., Colombo A. Revisiting species distribution and antifungal susceptibility of Candida bloodstream isolates from Latin American medical centers. J. Fungi. 2017;3:24. doi: 10.3390/jof3020024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah A.M., Rasool S., Majeed A., Mushtaq S., Khan M.H., Hussain A., Shah A., Hassan Q.P. Reappraisal of actinomycetes for novel bioactive metabolites. Ann. Phytomed. 2017;6:13–19. doi: 10.21276/ap.2017.6.1.3. [DOI] [Google Scholar]
- 17.Monciardini P., Iorio M., Maffioli S., Sosio M., Donadio S. Discovering new bioactive molecules from microbial sources. Microb. Biotechnol. 2014;7:209–220. doi: 10.1111/1751-7915.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Milshteyn A., Schneider J.S., Brady S.F. Mining the metabiome: Identifying novel natural products from microbial communities. Chem. Biol. 2014;21:1211–1223. doi: 10.1016/j.chembiol.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charlop-Powers Z., Owen J.G., Reddy B.V.B., Ternei M.A., Brady S.F. Chemical-biogeographic survey of secondary metabolism in soil. Proc. Natl. Acad. Sci. USA. 2014;111:3757–3762. doi: 10.1073/pnas.1318021111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El-Sayed S.E., Abdelaziz N.A., El-Housseiny G.S., Aboshanab K.M. Octadecyl 3-(3, 5-di-tert-butyl-4-hydroxyphenyl) propanoate, an antifungal metabolite of Alcaligenes faecalis strain MT332429 optimized through response surface methodology. Appl. Microbiol. Biotechnol. 2020;104:10755–10768. doi: 10.1007/s00253-020-10962-9. [DOI] [PubMed] [Google Scholar]
- 21.Nam Y.-D., Seo M.-J., Lim S.-I., Lee S.-Y. Genome sequence of Lysinibacillus boronitolerans F1182, isolated from a traditional Korean fermented soybean product. J. Bacteriol. 2012;194:5988. doi: 10.1128/JB.01485-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmed I., Yokota A., Yamazoe A., Fujiwara T. Proposal of Lysinibacillus boronitolerans gen. nov. sp. nov., and transfer of Bacillus fusiformis to Lysinibacillus fusiformis comb. nov. and Bacillus sphaericus to Lysinibacillus sphaericus comb. nov. Int. J. Syst. Evol. Microbiol. 2007;57:1117–1125. doi: 10.1099/ijs.0.63867-0. [DOI] [PubMed] [Google Scholar]
- 23.Liu X., Ma Z., Zhang J., Yang L. Antifungal Compounds against Candida Infections from Traditional Chinese Medicine. Biomed. Res. Int. 2017;2017:4614183. doi: 10.1155/2017/4614183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yilmaz M., Soran H., Beyatli Y. Antimicrobial activities of some Bacillus spp. strains isolated from the soil. Microbiol. Res. 2006;161:127–131. doi: 10.1016/j.micres.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Caulier S., Nannan C., Gillis A., Licciardi F., Bragard C., Mahillon J. Overview of the antimicrobial compounds produced by members of the Bacillus subtilis group. Front. Microbiol. 2019;10:302. doi: 10.3389/fmicb.2019.00302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jin P., Wang H., Tan Z., Xuan Z., Dahar G.Y., Li Q.X., Miao W., Liu W. Antifungal mechanism of bacillomycin D from Bacillus velezensis HN-2 against Colletotrichum gloeosporioides Penz. Pestic. Biochem. Physiol. 2020;163:102–107. doi: 10.1016/j.pestbp.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 27.Xiao J., Guo X., Qiao X., Zhang X., Chen X., Zhang D. Activity of fengycin and iturin A isolated from Bacillus subtilis Z-14 on Gaeumannomyces graminis var. tritici and soil microbial diversity. Front. Microbiol. 2021;12:682437. doi: 10.3389/fmicb.2021.682437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lei S., Zhao H., Pang B., Qu R., Lian Z., Jiang C., Shao D., Huang Q., Jin M., Shi J. Capability of iturin from Bacillus subtilis to inhibit Candida albicans in vitro and in vivo. Appl. Microbiol. Biotechnol. 2019;103:4377–4392. doi: 10.1007/s00253-019-09805-z. [DOI] [PubMed] [Google Scholar]
- 29.Ypucef-Ali M., Chaouche N.K., Dehimat L., Bataiche I., Mounira K., Cawoy H.E., Thonart P. Antifungal activity and bioactive compounds produced by Bacillus mojavensis and Bacillus subtilis. Afr. J. Microbiol. Res. 2014;8:476–484. [Google Scholar]
- 30.Jiang J., Gao L., Bie X., Lu Z., Liu H., Zhang C., Lu F., Zhao H. Identification of novel surfactin derivatives from NRPS modification of Bacillus subtilis and its antifungal activity against Fusarium moniliforme. BMC Microbiol. 2016;16:31. doi: 10.1186/s12866-016-0645-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sumi C.D., Yang B.W., Yeo I.-C., Hahm Y.T. Antimicrobial peptides of the genus Bacillus: A new era for antibiotics. Can. J. Microbiol. 2015;61:93–103. doi: 10.1139/cjm-2014-0613. [DOI] [PubMed] [Google Scholar]
- 32.Awais M., Shah A.A., Hameed A., Hasan F. Isolation, identification and optimization of bacitracin produced by Bacillus sp. Pak. J. Bot. 2007;39:1303. [Google Scholar]
- 33.Mikkola R. Ph.D. Thesis. Universitatis Helsingiensis in Viikki; Helsinki, Finland: 2006. [(accessed on 4 December 2021)]. Food and Indoor Air Isolated Bacillus Non-Protein Toxins: Structures, Physico-Chemical Properties and Mechanisms of Effects on Eukaryotic Cells. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.407.3810&rep=rep1&type=pdf. [Google Scholar]
- 34.Devi S., Kiesewalter H.T., Kovács R., Frisvad J.C., Weber T., Larsen T.O., Kovács Á.T., Ding L. Depiction of secondary metabolites and antifungal activity of Bacillus velezensis DTU001. Synth. Syst. Biotechnol. 2019;4:142–149. doi: 10.1016/j.synbio.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang X., Zhao D., Shen L., Jing C., Zhang C. Application and Mechanisms of Bacillus subtilis in Biological Control of Plant Disease. In: Meena V., editor. Role of Rhizospheric Microbes in Soil. Springer; Singapore: 2018. [DOI] [Google Scholar]
- 36.Hossain A.S.M., Sil B.C., Iliopoulos F., Lever R., Hadgraft J., Lane M.E. Preparation, Characterisation, and Topical Delivery of Terbinafine. Pharmaceutics. 2019;11:548. doi: 10.3390/pharmaceutics11100548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Singh M., Kumar A., Singh R., Pandey K.D. Endophytic bacteria: A new source of bioactive compounds. 3 Biotech. 2017;7:315. doi: 10.1007/s13205-017-0942-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahendran S., Vijayabaskar P., Saravanan S., An K., Shankar T. Structural characterization and biological activity of exopolysaccharide from Lysinibacillus fusiformis. Afr. J. Microbiol. Res. 2013;7:4666–4676. [Google Scholar]
- 39.Naureen Z., Rehman N.U., Hussain H., Hussain J., Gilani S.A., Al Housni S.K., Mabood F., Khan A.L., Farooq S., Abbas G. Exploring the potentials of Lysinibacillus sphaericus ZA9 for plant growth promotion and biocontrol activities against phytopathogenic fungi. Front. Microbiol. 2017;8:1477. doi: 10.3389/fmicb.2017.01477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahmad V., Iqbal A.N., Haseeb M., Khan M.S. Antimicrobial potential of bacteriocin producing Lysinibacillus jx416856 against foodborne bacterial and fungal pathogens, isolated from fruits and vegetable waste. Anaerobe. 2014;27:87–95. doi: 10.1016/j.anaerobe.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 41.Singh R.K., Kumar D.P., Solanki M.K., Singh P., Srivastva A.K., Kumar S., Kashyap P.L., Saxena A.K., Singhal P.K., Arora D.K. Optimization of media components for chitinase production by chickpea rhizosphere associated Lysinibacillus fusiformis B-CM18. J. Basic Microbiol. 2013;53:451–460. doi: 10.1002/jobm.201100590. [DOI] [PubMed] [Google Scholar]
- 42.El-Sayed S.E., El-Housseiny G.S., Abdelaziz N.A., El-Ansary M.R., Aboshanab K.M. Optimized Production of the Allylamine Antifungal “Terbinafine” by Lysinibacillus Isolate MK212927 Using Response Surface Methodology. Infect. Drug Resist. 2020;13:3613. doi: 10.2147/IDR.S267590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Parthasarathi S., Sathya S., Bupesh G., Manikandan M., Kim C., Manikandan T., Balakrishnan K. Isolation, Characterization and Extraction of antimicrobial compound from marine actinomycete Streptomyces hygroscopicus BDUS 49. Res. J. Biotechnol. 2012;8:3. [Google Scholar]
- 44.Thangadurai D., Murthy K., Prasad P., Pullaiah T. Antimicrobial screening of Decalepis hamiltonii wight and arn.(Asclepiadaceae) root extracts against food-related microorganisms. J. Food Saf. 2004;24:239–245. doi: 10.1111/j.1745-4565.2004.00537.x. [DOI] [Google Scholar]
- 45.Chawawisit K., Bhoopong P., Phupong W., Lertcanawanichakul M. 2,4-Di-tert-butylphenol, the bioactive compound produced by Streptomyces sp. KB1. J. Appl. Pharm. Sci. 2015;5:007–012. [Google Scholar]
- 46.Motta A., Brandelli A. Characterization of an antibacterial peptide produced by Brevibacterium linens. J. Appl. Microbiol. 2002;92:63–70. doi: 10.1046/j.1365-2672.2002.01490.x. [DOI] [PubMed] [Google Scholar]
- 47.Morschhäuser J. The development of fluconazole resistance in Candida albicans—An example of microevolution of a fungal pathogen. J. Microbiol. 2016;54:192–201. doi: 10.1007/s12275-016-5628-4. [DOI] [PubMed] [Google Scholar]
- 48.Ali G.S., El-Sayed A.S., Patel J.S., Green K.B., Ali M., Brennan M., Norman D. Ex Vivo Application of Secreted Metabolites Produced by Soil-Inhabiting Bacillus spp. Efficiently Controls Foliar Diseases Caused by Alternaria spp. Appl. Environ. Microbiol. 2016;82:478–490. doi: 10.1128/AEM.02662-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kumar A., Zarychanski R., Pisipati A., Kumar A., Kethireddy S., Bow E.J. Fungicidal versus fungistatic therapy of invasive Candida infection in non-neutropenic adults: A meta-analysis. Mycology. 2018;9:116–128. doi: 10.1080/21501203.2017.1421592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gupta A.K., Drummond-Main C. Meta-analysis of randomized, controlled trials comparing particular doses of griseofulvin and terbinafine for the treatment of tinea capitis. Pediatr. Dermatol. 2013;30:1–6. doi: 10.1111/j.1525-1470.2012.01866.x. [DOI] [PubMed] [Google Scholar]
- 51.Muharram M., Abdel-Kader M. Taxonomic characterization and chemical study of the antifungal constituents of Streptomyces sp. KH-F12. J. Biol. Sci. 2014;14:403–413. doi: 10.3923/jbs.2014.403.413. [DOI] [Google Scholar]
- 52.Kind T., Fiehn O. Advances in structure elucidation of small molecules using mass spectrometry. Bioanal. Rev. 2010;2:23–60. doi: 10.1007/s12566-010-0015-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Abdel-Rahman S.M., Nahata M.C. Oral terbinafine: A new antifungal agent. Ann. Pharmacother. 1997;31:445–456. doi: 10.1177/106002809703100412. [DOI] [PubMed] [Google Scholar]
- 54.Maxfield L., Preuss C.V., Bermudez R. Terbinafine. StatPearls Publishing; Treasure Island, FL, USA: 2021. [(accessed on 4 December 2021)]. Available online: https://www.ncbi.nlm.nih.gov/books/NBK545218/ [PubMed] [Google Scholar]
- 55.Elewski B., Tavakkol A. Safety and tolerability of oral antifungal agents in the treatment of fungal nail disease: A proven reality. Ther. Clin. Risk Manag. 2005;1:299. [PMC free article] [PubMed] [Google Scholar]
- 56.Chubukov V., Mukhopadhyay A., Petzold C.J., Keasling J.D., Martín H.G. Synthetic and systems biology for microbial production of commodity chemicals. NPJ Syst. Biol. Appl. 2016;2:16009. doi: 10.1038/npjsba.2016.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abdel-Kader M.S., Muharram M.M. New microbial source of the antifungal allylamine “Terbinafine”. Saudi Pharm. J. 2017;25:440–442. doi: 10.1016/j.jsps.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hossain N., Rahman M. Antagonistic activity of antibiotic producing Streptomyces sp. against fish and human pathogenic bacteria. Braz. Arch. Biol. Technol. 2014;57:233–237. doi: 10.1590/S1516-89132014000200011. [DOI] [Google Scholar]
- 59.Rahman M.A., Islam M.Z., Islam M.A. Antibacterial activities of actinomycete isolates collected from soils of rajshahi, bangladesh. Biotechnol. Res. Int. 2011;2011:857925. doi: 10.4061/2011/857925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Peela S., Kurada V.B., Terli R. Studies on antagonistic marine actinomycetes from the Bay of Bengal. World J. Microbiol. Biotechnol. 2005;21:583–585. doi: 10.1007/s11274-004-3493-5. [DOI] [Google Scholar]
- 61.Tiru M., Muleta D., Bercha G., Adugna G. Antagonistic effect of rhizobacteria against coffee wilt disease caused by Gibberella xylarioides. Asian J. Plant Pathol. 2013;7:109–122. doi: 10.3923/ajppaj.2013.109.122. [DOI] [Google Scholar]
- 62.Montealegre J.R., Reyes R., Pérez L.M., Herrera R., Silva P., Besoain X. Selection of bioantagonistic bacteria to be used in biological control of Rhizoctonia solani in tomato. Electron. J. Biotechnnol. 2003;6:115–127. doi: 10.2225/vol6-issue2-fulltext-8. [DOI] [Google Scholar]
- 63.Magaldi S., Mata-Essayag S., Hartung de Capriles C., Perez C., Colella M.T., Olaizola C., Ontiveros Y. Well diffusion for antifungal susceptibility testing. Int. J. Infect. Dis. 2004;8:39–45. doi: 10.1016/j.ijid.2003.03.002. [DOI] [PubMed] [Google Scholar]
- 64.Wiegand I., Hilpert K., Hancock R.E. Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat. Protoc. 2008;3:163. doi: 10.1038/nprot.2007.521. [DOI] [PubMed] [Google Scholar]
- 65.Bundale S., Begde D., Nashikkar N., Kadam T., Upadhyay A. Isolation of aromatic polyketide producing soil Streptomyces using combinatorial screening strategies. Open Access Libr. J. 2014;1:1–16. doi: 10.4236/oalib.preprints.1200010. [DOI] [Google Scholar]
- 66.Rojas J.J., Ochoa V.J., Ocampo S.A., Muñoz J.F. Screening for antimicrobial activity of ten medicinal plants used in Colombian folkloric medicine: A possible alternative in the treatment of non-nosocomial infections. BMC Complement. Altern. Med. 2006;6:2. doi: 10.1186/1472-6882-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moreno-Arribas M.V., Polo M.C. Occurrence of lactic acid bacteria and biogenic amines in biologically aged wines. Food Microbiol. 2008;25:875–881. doi: 10.1016/j.fm.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 68.Kumar S., Stecher G., Li M., Knyaz C., Tamura K. MEGA X: Molecular Evolutionary Genetics Analysis across Computing Platforms. Mol. Biol. Evol. 2018;35:1547–1549. doi: 10.1093/molbev/msy096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kimura M. A simple method for estimating evolutionary rates of base substitutions through comparative studies of nucleotide sequences. J. Mol. Evol. 1980;16:111–120. doi: 10.1007/BF01731581. [DOI] [PubMed] [Google Scholar]
- 70.Bhosale H., Kadam T., Mirajgave R., Holkar S. Optimization and characterization of antifungal metabolite from a soil actinomycete Streptomyces indiaensis SRT1. Indian J. Biotechnol. 2018;17:261–271. [Google Scholar]
- 71.Kumar P.S., Duraipandiyan V., Ignacimuthu S. Isolation, screening and partial purification of antimicrobial antibiotics from soil Streptomyces sp. SCA 7. Kaohsiung J. Med. Sci. 2014;30:435–446. doi: 10.1016/j.kjms.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Balouiri M., Bouhdid S., Harki E., Sadiki M., Ouedrhiri W., Ibnsouda S.K. Antifungal activity of Bacillus spp. isolated from Calotropis procera AIT. Rhizosphere against Candida albicans. Asian J. Pham. Clin. Res. 2015;8:213–217. [Google Scholar]
- 73.Augustine S., Bhavsar S., Kapadnis B. A non-polyene antifungal antibiotic from Streptomyces albidoflavus PU 23. J. Biosci. 2005;30:201–211. doi: 10.1007/BF02703700. [DOI] [PubMed] [Google Scholar]
- 74.Munimbazi C., Bullerman L. Isolation and partial characterization of antifungal metabolites of Bacillus pumilus. J. Appl. Microbiol. 1998;84:959–968. doi: 10.1046/j.1365-2672.1998.00431.x. [DOI] [PubMed] [Google Scholar]
- 75.Shahidi Bonjar G., Rashid Farrokhi P., Aghighi S., Shahidi Bonjar L., Aghelizadeh A. Antifungal characterization of actinomycetes isolated from Kerman, Iran and their future prospects in biological control strategies in greenhouse and field conditions. Plant Pathol. J. 2005;4:78–84. [Google Scholar]
- 76.Navi S., Rajasab A., Yang X. In Vitro evaluation of commercial fungicides against some of the major soil borne pathogens of soybean. J. Plant Pathol. Microbiol. 2016;7:340–347. doi: 10.4172/2157-7471.1000340. [DOI] [Google Scholar]
- 77.CLSI . Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts, Approved Standard. 2nd ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2008. [(accessed on 4 December 2021)]. Available online: https://clsi.org/media/1897/m27ed4_sample.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are included within the manuscript and supplementary file.