A 70-year-old Japanese man who had Behçet disease (BD) with exacerbated skin ulcers was suspected of having vascular BD. He developed BD in his 30s and developed refractory skin ulcers in his lower limbs in his 40s. Because skin biopsy revealed nonspecific congestion, which is consistent with BD, infliximab (IFX) (400 mg) was administered 4 times. The skin ulcers were unchanged, but painful induration of the tongue appeared, and a tongue biopsy was performed (Fig. 1). Histopathologically, granulomas were found in the muscle layer (Fig. 2A). These granulomas with multinucleated giant cells involved small arteries (Figs. 2B–G). Congo red and amyloid A–positive eosinophilic material was observed in the center of the granuloma and blood vessel wall (Fig. 2G-I). He did not have M-proteinemia but had elevated serum amyloid A level. Although microorganisms were not detected (Fig. 2F), it was difficult to rule out infection, and we therefore discontinued IFX therapy. The tongue lesion disappeared 2 months after stopping IFX therapy.
FIGURE 1.

Tongue induration without ulcers.
FIGURE 2.
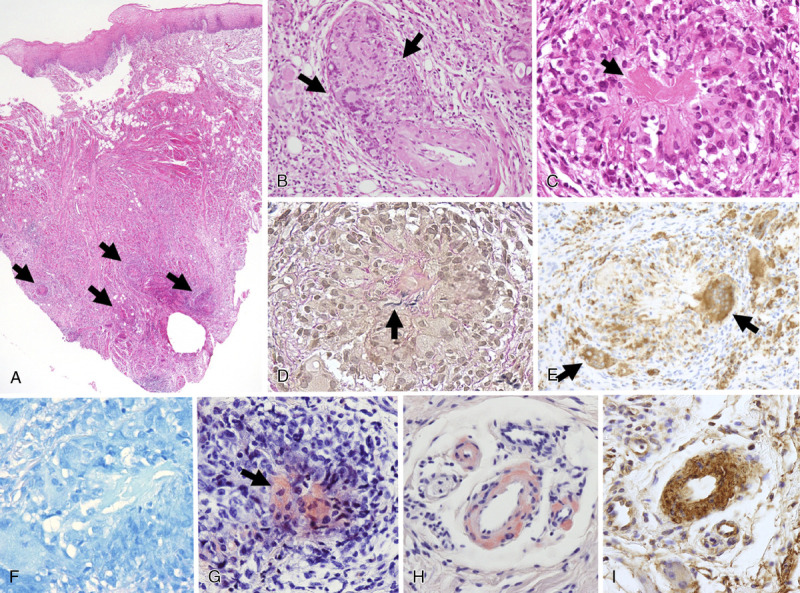
Histopathological findings of the tongue. A, Granulomatous inflammation (arrow) was found in the muscle layer (hematoxylin-eosin stain, original magnification ×2). B, Granulomas with multinucleated giant cells (arrow) were present along the small arteries (hematoxylin-eosin stain, original magnification ×20). C, Eosinophilic materials (arrow) were observed in the center of the granuloma (hematoxylin-eosin stain, original magnification ×20). D, Fragments of elastic fibers of the vascular wall (arrow) were observed at the center of the granuloma (Elastica–van Gieson stain, original magnification ×20). E, Multinucleated giant cells (arrow) were positive for CD68 by immunohistochemistry (PG-M1, original magnification ×20). F, Mycobacterium was not found in the granuloma (Ziehl-Neelsen stain, original magnification ×20). G and H, Eosinophilic materials found in the granuloma center (G, arrow) and blood vessel wall near the granuloma (H) were positive for Congo red (original magnification ×20). I, Eosinophilic materials on the vessel wall were positive for amyloid A by immunohistochemistry (original magnification ×20).
We presented a case of BD treated with IFX in which granulomatous vasculitis with AA amyloid deposits developed in the tongue. The tongue lesion developed 3 months after initiation of IFX therapy and improved promptly after discontinuation of the therapy, suggesting that vasculitis was induced by IFX.
The most common vasculitis caused by tumor necrosis factor (TNF) inhibitors is cutaneous leukocytoclastic vasculitis.1 There are also reports of granulomatous large vessel vasculitis such as Takayasu arteritis.2 Reports of TNF inhibitor–induced sarcoidosis indicate a link between TNF inhibitors and granulomatous inflammation.3 In the central nervous system, a relationship between vascular amyloid deposits and granulomatous vasculitis has been suggested.4 Tumor necrosis factor inhibitors may be associated with granulomatous vasculitis and amyloid A deposition in inflammatory foci.
Footnotes
This work was supported by a grant from the Ministry of Health, Labour, and Welfare of Japan for Japan Research Committee for Intractable Vasculitis (JPVAS, to A.I.).
The authors declare no conflict of interest.
Contributor Information
Sari Iwasaki, Email: sariwasaki@gmail.com.
Toshiyuki Watanabe, Email: nabe0727@med.hokudai.ac.jp.
Takahiro Tsuji, Email: tsuji.takahiro@gmail.com.
Takuya Otsuka, Email: xanavi.nismo.tune@gmail.com.
Keishi Makita, Email: keimak154@hotmail.co.jp.
Yuichiro Fukasawa, Email: yuichiro.fukasawa@doc.city.sapporo.jp.
Akihiro Ishizu, Email: aishizu@med.hokudai.ac.jp.
REFERENCES
- 1.Saint Marcoux B De Bandt M, CRI (Club Rhumatismes et Inflammation) . Vasculitides induced by TNFalpha antagonists: a study in 39 patients in France. Joint Bone Spine. 2006;73:710–713. [DOI] [PubMed] [Google Scholar]
- 2.Souabni L Ben Abdelghani K Jradi S, et al. Takayasu's arteritis occurring under TNF-α blockers: a new paradoxical effect? BMJ Case Rep. 2014;2014:bcr2014204226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vigne C Tebib JG Pacheco Y, et al. Sarcoidosis: an underestimated and potentially severe side effect of anti–TNF-alpha therapy. Joint Bone Spine. 2013;80:104–107. [DOI] [PubMed] [Google Scholar]
- 4.Ng DW Magaki S Terashima KH, et al. Amyloid-β–related angiitis: a report of 2 cases with unusual presentations. Hum Pathol. 2017;64:191–197. [DOI] [PubMed] [Google Scholar]


