Abstract
Background
Although current recommendations suggest that hip hemiarthroplasties performed for femoral neck fractures be implanted with bone cement, it is known to cause cardiorespiratory and hemodynamic reactions that in some patients can be fatal. Older patients may be at particular risk of this complication, but because of its relative infrequency, large studies—perhaps even larger than can be achieved in the context of single-country national registries—are needed to get reasonably precise estimates as to its frequency. Pooling results from national registries reporting on death within 48 hours of cement exposure in this setting may therefore be helpful.
Question/purpose
In a systematic review of studies based on large national registries, we asked: Does the risk of death within 48 hours of hip hemiarthroplasty differ between patients treated with cemented and cementless implants?
Methods
MEDLINE and Embase data sources were searched for cohort studies on patients with hip fractures treated with cement or cementless hip hemiprostheses based on results from national registries that tracked perioperative deaths within 48 hours of surgery, from 2010 or later (to include only studies that used contemporary cement techniques). We excluded registry research on elective THAs for other indications (such as degenerative joint disease), mixed populations (registries that combined patients having arthroplasty for fracture and for other diagnoses like osteoarthritis, such that we could not separate them), and overlapping data from the same registers (to avoid double and triple publications of similar data). Five studies met our inclusion criteria. The cohorts ranged from about 11,000 to about 25,000 patients. About 31% of the patients were in the cementless group. Two studies reported the age ranges of participating patients, and three studies communicated mean ages (which were 82 years for both sexes). Twice as many females as males were present in both the cemented and cementless group. When reported, more than 50% in both groups were in the American Society of Anesthesiologists physical status classification 3 or 4. Study quality was deemed good according to the Newcastle-Ottawa Scale. Publication bias was assessed using a funnel plot and the Egger test, and study heterogeneity was evaluated using the I2 heterogeneity statistic and Cochran Q heterogeneity test. There was some heterogeneity between the studies, with a Cochran Q statistics of 8.13 (degrees of freedom = 4; p = 0.08) and an I2 statistic of 50.8%. There was evidence for a small amount of publication bias (Egger test; p = 0.02). The pooled risk ratio (RR) from a random-effects model is presented with 95% confidence intervals. The primary endpoint was the occurrence of any fatalities within 48 hours of hip fracture treatment with cementless compared with cemented prostheses. We performed a sensitivity analysis to assess the needed association of a potential unmeasured or uncontrolled confounding, and we made an estimate of the amount of unmeasured confounding that would need to be present in order to change the direction of the result. We summarized this using a parameter known as the “E-value.” Based on that sensitivity analysis, we found it unlikely that an unmeasured hypothetical confounder could explain the significant association between cemented and cementless implants and risk of death within 48 hours of hip hemiarthroplasty.
Results
Compared with the cementless group, mortality was increased in the cemented group (RR 1.63 [95% CI 1.31 to 2.02]; p < 0.001). The number needed to harm from the pooled data was 1 of 183 operated patients; that is, for every 183 patients treated with cemented implants, one death would be expected.
Conclusion
Bone cement is associated with a higher risk of fatalities within 48 hours of surgery compared with cementless prostheses. However, numerous prior studies have found a higher risk of serious complications resulting in additional surgical procedures associated with cementless devices in this population; those complications, as well, may result in death. Based on our study alone, we cannot recommend cementless implants in this setting. Large, national registries should evaluate fixation choice in older patients with hip fractures, and those studies should consider both early death and the potential for later harms.
Level of Evidence
Level III, therapeutic study.
Introduction
Since the introduction of cemented hip prostheses in humans, studies have reported cardiorespiratory and vascular dysfunction that is closely linked to impaction of cement and the prosthesis, which is occasionally fatal [4, 7, 10, 12, 14, 16, 21, 24, 26, 27]. The highest mortality proportion, around 11%, was reported in 1989 by Duncan [10]. However, closer attention to perioperative monitoring, improved cementing techniques, systematic anticoagulation regimens, and better general health in the population have contributed to reduce the frequency of this complication [30]. Although current recommendations suggest that hip hemiarthroplasties performed for femoral neck fractures be implanted with bone cement [5], patients with comorbidities and increased age may still be at particular risk of this serious outcome [3, 20].
Because of the relative infrequency of cardiorespiratory and hemodynamic reactions, large studies—perhaps even larger than can be achieved in the context of single-country national registries—are needed to get reasonably precise estimates of their frequency. Pooling results from studies on national registries reporting on death within 48 hours of cement exposure in this setting may therefore be helpful.
Thus, we performed a systematic review of studies on large national registries, and asked: Does the risk of death within 48 hours of hip hemiarthroplasty differ between patients treated with cemented and cementless implants?
Materials and Methods
Protocol, Registration, and Ethical Approval
This study was based on published data extracted from national registries on hip fracture patients. No formal ethical approval was requested, and this protocol was not preregistered.
Eligibility Criteria
Eligibility criteria were hip fracture patients treated with cemented or cementless hip hemiprostheses. Inclusion criteria were papers based on national registries that tracked perioperative deaths within 48 hours of surgery, from 2010 or later (to include only studies that used contemporary cement techniques). We excluded registry research about elective THA for other indications (such as degenerative joint disease), mixed populations (registries that combined patients having arthroplasty for fracture and for other diagnoses like osteoarthritis, such that we could not separate them), and overlapping data from the same registers (to avoid double and triple publications of similar data).
Information Sources and Search Strategy
We performed a systematic search in MEDLINE and Embase from their inception in 2010 to July 2, 2021. The main search terms were hip or femoral neck fracture, hemiarthroplasty, cemented prosthesis, cementless prosthesis, mortality, and intraoperative and perioperative period (Appendix 1; http://links.lww.com/CORR/A619). Controlled subject headings and free-text search terms were used in both electronic databases. The general searches were restricted to articles written in English. In addition, the reference lists of summarized articles were manually scrutinized by both reviewers (OED, AHP).
Study Selection and Characteristics
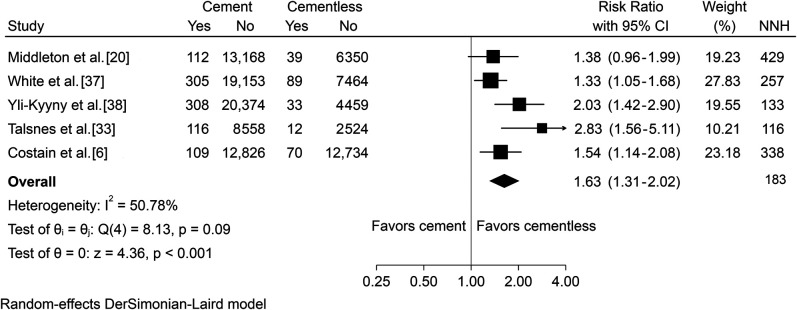
Initially, we identified 366 studies; 235 records remained after we removed duplicates. After we applied the inclusion and exclusion criteria, five studies were eligible for inclusion, with cohorts ranging from about 11,000 to 25,000 patients (Fig. 1) [6, 20, 33, 37, 38]. Two reviewers (OED, AHP) independently reviewed and assessed the eligibility according to the listed entry criteria.
Fig. 1.
The flow chart illustrates the number of the studies that were identified during the electronic search. After application of the inclusion criteria, five studies were feasible for statistical calculations.
About 31% of patients were in the cementless group. Two studies reported the age ranges of participating patients, three studies communicated mean ages (which were 82 years for both sexes), and about twice as many females as males were present in both the cemented and cementless groups. When reported, more than 50% were in the American Society of Anesthesiologists (ASA) physical status classification system 3 or 4 in both groups (Table 1).
Table 1.
Study characteristics of patients treated with cemented or cementless implants for femoral neck fractures
| Cemented | Cementless | ||||||||||||
| Author | Country | Time span | NOS for assessing qualitya | Number | Age, years | Female, % | ASA 3-4, % | Dementia, % | Number | Age, years | Female, % | ASA 3-4, % | Dementia, % |
| Costain et al. 2011 [6] | Australia | 2009 | Selection: **** Comparability: * Outcome: *** |
12,935 | Younger than 70: 13% 71-80: 32% > 80: 55% |
74 | 12,804 | Younger than 70: 7% 71-80: 26% > 80: 67% |
74 | ||||
| Yli-Kyyny et al. 2014 [38] | Finland | 1999 -2009 | Selection: **** Comparability: * Outcome: *** |
20,682 | 81 | 73.8 | 20.4 | 4492 | 81 | 73.8 | 23.8 | ||
| Middleton et al. 2014 [20] | UK | 2002-2011 | Selection: **** Comparability: * Outcome: *** |
13,280 | 6389 | ||||||||
| Talsnes et al. 2013 [33] | Norway | 2005-2010 | Selection: **** Comparability: * Outcome: *** |
8674 | 83 | 74.6 | 56 | 25.5 | 2536 | 83.3 | 73.9 | 56 | 28.5 |
| White et al. 2014 [37] | UK | 2012 | Selection: **** Comparability: * Outcome: *** |
19,458 | 68.5 | 7353 | 73.3 | ||||||
aA study can be awarded a maximum of one star for each numbered item within the Selection and Outcome categories (minimum score is no stars and maximum score is four stars); a maximum of two stars can be given for Comparability; ASA = American Society of Anesthesiologists physical status classification system; NOS = Newcastle-Ottawa Scale for assessing the quality of nonrandomized studies in meta-analyses.
Data Collection Process
Primary outcomes of our meta-analysis were to investigate any difference in death within 48 hours of hip hemiarthroplasty between patients treated with cemented and cementless implants as well as the number needed to harm in the individual studies and the pooled analysis. We assessed study characteristics by examining the data extraction and baseline characteristics, and study quality was evaluated using the Newcastle-Ottawa Scale.
Risk of Bias
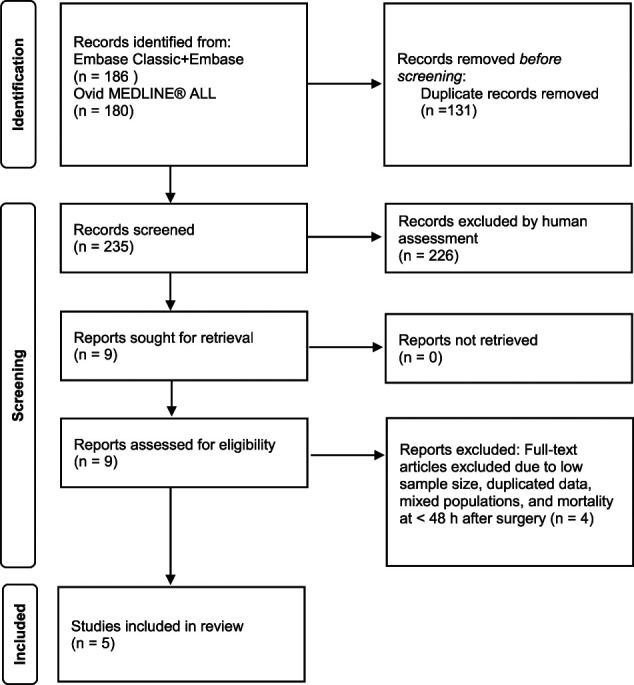
We assessed publication bias using a funnel plot (Fig. 2) and an Egger test (a linear regression of the intervention effect estimates on their standard errors weighted by their inverse variance). Study heterogeneity was evaluated using the I2 heterogeneity statistic (percentage of the variability in effect estimates that is due to heterogeneity) and Cochran Q heterogeneity test. There was some heterogeneity between the studies, with a Cochran Q statistic of 8.13 (degrees of freedom = 4; p = 0.08) and an I2 statistic of 50.8%, and indication of publication bias (Egger test; p = 0.02).
Fig. 2.
A funnel plot with the effect of the treatment, that is, the log risk ratios from the individual studies in each study (horizontal axis) is plotted against the study precision, as measured by the standard error of the log risk ratio (vertical axis). The dotted lines show pseudo-95% confidence interval lines.
Synthesis of Results and Primary Study Outcomes
Because of the heterogeneity between studies, a random-effects model (DerSimonian-Laird estimator) was deemed appropriate, using the risk ratio (RR) with 95% confidence intervals as the effect measure from each study and in the pooled analysis. Our primary endpoint was the occurrence of any fatalities within 48 hours of hip fracture treatment with cementless compared with cemented prostheses. The number needed to harm, that is, the inverse of the perioperative risk difference, was calculated from each individual study and from the pooled data. The number needed to harm estimates the required number of patients treated with cemented arthroplasty to attribute one perioperative death in relation to a scenario with cementless-only treatment. The meta-analysis was conducted with the meta command in Stata version 16 (StataCorp).
Sensitivity Analysis
A sensitivity analysis was conducted to assess how robust the association was to potential unmeasured or uncontrolled confounding by estimating the “E-value,” a sensitivity measure developed for observational research that is defined as the minimum strength of association that an unmeasured confounder would need to have with both the treatment and the outcome to fully explain a treatment-outcome association [35].
Data on the baseline characteristics of the cement and cementless groups were too scarce to control for measured confounders by stratified or meta-regression (Table 1). We therefore conducted a sensitivity analysis by estimating the “E-value” [35]. The E-value for the lower confidence interval limit was 1.95; that is, an unmeasured confounder would have needed to have a risk ratio of 1.95 with both the exposure (cemented or cementless) and outcome (death within 48 hours) to explain the reported significant association between cemented and cementless implants and risk of death within 48 hours of hip hemiarthroplasty. To fully explain the observed treatment-outcome association—that is, an unmeasured confounder being large enough to change the pooled risk ratio to 1.0—its association would need to have a risk ratio of 2.64.
Results
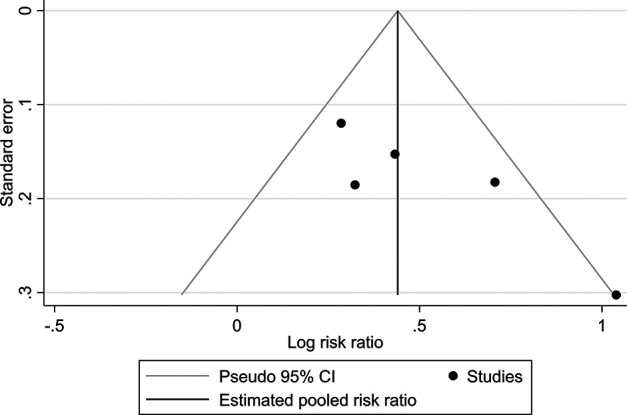
Mortality was greater in the cemented group than it was in the cementless group (pooled risk ratio 1.63 [95% CI 1.31 to 2.02]; p < 0.001). The number needed to harm in the individual studies varied from 1 extra death attributed to cementation per 116 patients [33] to 1 in 429 patients [20]. The pooled analysis showed one death in 183 operated patients in the cemented group compared with the cementless category (Fig. 3).
Fig. 3.
The forest plot shows risk ratios for any mortality within 48 hours after surgery. Risk ratios less than 1.0 favor cemented implants, and those greater than 1.0 favor cementless installed prostheses. Horizontal lines give 95% confidence intervals; NNH = number needed to harm, that is, the number of patients operated on with cemented prostheses to experience one death attributed to cemented treatment in each study and the pooled data; I2 = I-squared statistics (heterogeneity); Q = Cochran Q heterogeneity statistic (with degrees of freedom (df) and p value).
Discussion
Implanting hip prostheses with bone cement in patients with femoral neck fractures may cause cardiorespiratory and hemodynamic reactions that can be fatal. But because this complication is rare, large studies are needed to get reasonably precise estimates as to its frequency. Pooling results from studies on national registries reporting on death within 48 hours of cement exposure in this setting may be helpful. We therefore performed a meta-analysis of data from large, national registries [6, 20, 33, 37, 38] to ascertain whether the risk of death within 48 hours of hip hemiarthroplasty differed between patients treated with cemented and cementless implants. The most important finding was that cementation was associated with increased risk of perioperative death compared to cementless prostheses.
Limitations
This study has some important limitations. The most important limitation of this study is that we evaluated only one single endpoint: death within 48 hours. The choice of implant fixation, cemented or cementless, has implications that extend far beyond that point; considerable research has found that patients with hip fractures who receive cementless implants are at substantially increased risk of periprosthetic fracture and revision surgery, which also may lead to death [17]. Some research suggests no difference in mortality at one year between patients treated with cemented and cementless fixation [36], or even a lower risk of death at one year with cemented fixation [29].
Another important limitation is that we were unable to control for confounding variables, such as medical comorbidities, patient age, ASA score, practice setting, or surgeon volume, in this meta-analysis. However, baseline characteristics of the groups were comparable, and a sensitivity analysis found it unlikely that an unmeasured hypothetical confounding could explain away the reported significant finding. Thus, to the best of our knowledge, the association between risk of death within 48 hours of hip hemiarthroplasty and patients treated with cemented and cementless implants seems robust. Unfortunately, only the Norwegian and UK register-based studies presented ASA scores. In our previous study, we found that the number needed to harm due to cementation increased from 1 of 116 in the general hip fracture population to 1 of 33 in patients with preoperative symptomatic comorbidity (ASA 3-4) [33]. In the UK study, they noted that a greater proportion of patients receiving cementless prostheses were of poorer physiological status (ASA 3-5) than those receiving cemented prostheses. In spite of this, mortality within 24 hours of surgery was higher in those who received cemented prostheses compared with those who received cementless implants. The mortality rose from 0.6% in ASA class 1 to 35.9% in those with an ASA score of 5 [37]. None of the three remaining national cohorts presented ASA scores and uniform baseline characteristics that made it possible to control or adjust for confounders by stratified analysis or meta-regression. Consequently, we were not able to present ASA data on each study or in our pooled data. In the Scottish study, they also noted that uncemented fixation was more often used in patients with comorbidities [20]. Despite this, day 0 mortality was higher in patients with cemented prostheses compared with those with a cementless hemiarthroplasty, equivalent to one extra death per 424 procedures. By day 1 it was 1 of 338, and the cumulative rate continued to be higher on days 2 and 3. The authors also showed that the general mortality increased from 60 to 90 years of age [20]. Although we are not able to present pooled data in our calculations, it seems from the referenced studies that patients with comorbidities, older age, and cemented prostheses might be more susceptible to perioperative death than those who receive cementless implants. Based on the sensitivity analysis “E-value,” we find it unlikely that an unmeasured confounding could be present to explain the specific treatment-outcome association.
Another limitation is that our study was based on data from large, national registries rather than on randomized controlled trials (RCTs). Clinical trials in this area tend to focus on long-term outcomes [1, 2, 8, 9, 11, 13, 15, 22, 23, 25, 31, 32, 34], and they are underpowered to investigate perioperative deaths [32]. Although meta-analyzing them would offset the problem of insufficient power, we opted not to because the number of perioperative deaths in those studies—which tend to enroll dozens or hundreds of patients overall, at most—was very small and would not have changed the outcomes here, given that our study populations ranged from approximately 11,000 to 25,000 patients. In addition, combining RCTs with registry data would make pooling data—a key strength of our study—inappropriate, given the dissimilarities in study design between RCTs and large registry studies.
Death within 48 Hours of Surgery
The five registry studies we included, which come from five different countries, all showed higher perioperative mortality in patients with femoral neck fractures treated with cement-sealed prostheses versus those receiving cementless implants [6, 20, 33, 37, 38]. Because we did not rely on RCTs but rather on observational research, our findings cannot prove a cause-effect relationship. However, given what is known about the cardiovascular pathophysiology associated with cement-related complications [24], we believe it is likely that cement use contributed to these deaths. But based on the scientific underlying knowledge summarized above and in our study, which showed perioperative mortalities related to cemented implants [28], it is most likely that our finding is valid. However, it is well-known that cemented prostheses have a lower rate of periprosthetic fractures than cementless prostheses, and that they have a favorable long-term functional outcome, and several large, national registry studies as well as randomized trials have found that cemented femoral implants have a lower revision risk after hip fracture surgery [11, 25, 29, 31]. The excess risk of periprosthetic fracture and revision surgery associated with cementless femoral implants in this setting [17], which also may lead to death, must be balanced against our finding of an increased risk of early death associated with cemented implants [33]. Future registry-based efforts that weigh the risk of early death associated with cement against the harms over the longer term associated with cementless implants are needed to answer this important question.
The published small RCTs were designed to assess long-term outcomes and show an almost equal longstanding death rate in hip fracture patients treated with cemented or cementless prostheses [1, 11, 17-19, 23, 25, 31]. Despite the lack of perioperative fatalities as a primary endpoint in the RCTs, systematic reviews have based their short-term surgically related death reports on these trials. These sporadic reported deaths and lack of statistical differences related to the implants have supported the idea that all patients with hip fractures may benefit from cemented prostheses [1, 17-19]. That said, there is also strong evidence of harm associated with use of cementless implants in this setting, both in the form of periprosthetic fractures and excess major revision procedures [17]. We hope that national registry studies will focus attention on balancing what may be excess early harm associated with cemented against later harm associated with cementless implants so that we can answer this question more definitively as soon as possible.
Conclusion
Laboratory and clinical studies on bone cement have identified mechanical and chemical reactions that may trigger fatalities. However, such events are rare and large numbers of patients are needed to study this condition; randomized trials are too small to do so adequately. Our analysis of five large studies drawn from nationwide registers found that cemented fixation was associated with an increased risk of perioperative death compared with cementless fixation. However, we acknowledge that numerous prior studies have found a higher risk of serious complications resulting in additional surgical procedures associated with cementless devices in this population [5, 17, 36]; those complications, as well, may result in death. Based on our study alone, we cannot recommend cementless implants in this setting. Large, national registries should evaluate fixation choice in older patients with hip fractures, and those studies should consider both early death and the potential for later harms.
Supplementary Material
Acknowledgment
We thank Hilde Irene Flaatten MSc, medical librarian at the University of Oslo Library of Medicine and Science, who handled the electronic search string.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval was not sought for this study.
This work was performed at Centre of Medical Science, Education and Innovation, Innlandet Hospital Trust, Brumunddal, Norway.
References
- 1.Azegami S, Gurusamy KS, Parker MJ. Cemented versus uncemented hemiarthroplasty for hip fractures: a systematic review of randomised controlled trials. Hip Int. 2011;21:509-517. [DOI] [PubMed] [Google Scholar]
- 2.Barenius B, Inngul C, Alagic Z, Enocson A. A randomized controlled trial of cemented versus cementless arthroplasty in patients with a displaced femoral neck fracture: a four-year follow-up. Bone Joint J. 2018;100-B:1087-1093. [DOI] [PubMed] [Google Scholar]
- 3.Bhattacharyya T, Iorio R, Healy WL. Rate of and risk factors for acute inpatient mortality after orthopaedic surgery. J Bone Joint Surg Am. 2002;84:562-572. [DOI] [PubMed] [Google Scholar]
- 4.Byrick RJ, Mullen JB, Mazer CD, Guest CB. Transpulmonary systemic fat embolism. Studies in mongrel dogs after cemented arthroplasty. Am J Respir Crit Care Med. 1994;150:1416-1422. [DOI] [PubMed] [Google Scholar]
- 5.Cornell CN. Guest editorial: An appeal for evidenced-based care and adoption of best practices in the management of displaced femoral neck fractures. Clin Orthop Relat Res. 2019;477:913-916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costain DJ, Whitehouse SL, Pratt NL, Graves SE, Ryan P, Crawford RW. Perioperative mortality after hemiarthroplasty related to fixation method. Acta Orthop. 2011;82:275-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dahl OE, Pripp AH. Letter to the Editor: Cemented or uncemented hemiarthroplasty for femoral neck fracture? Data from the Norwegian Hip Fracture Register. Clin Orthop Relat Res. 2020;478:685-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deangelis JP, Ademi A, Staff I, Lewis CG. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a prospective randomized trial with early follow-up. J Orthop Trauma. 2012;26:135-140. [DOI] [PubMed] [Google Scholar]
- 9.Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986;1:21-28. [DOI] [PubMed] [Google Scholar]
- 10.Duncan JA. Intra-operative collapse or death related to the use of acrylic cement in hip surgery. Anaesthesia. 1989;44:149-153. [DOI] [PubMed] [Google Scholar]
- 11.Emery RJ, Broughton NS, Desai K, Bulstrode CJ, Thomas TL. Bipolar hemiarthroplasty for subcapital fracture of the femoral neck. A prospective randomised trial of cemented Thompson and uncemented Moore stems. J Bone Joint Surg Br. 1991;73:322-324. [DOI] [PubMed] [Google Scholar]
- 12.Fallon KM, Fuller JG, Morley-Forster P. Fat embolization and fatal cardiac arrest during hip arthroplasty with methylmethacrylate. Can J Anaesth. 2001;48:626-629. [DOI] [PubMed] [Google Scholar]
- 13.Figved W, Opland V, Frihagen F, Jervidalo T, Madsen JE, Nordsletten L. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop Relat Res. 2009;467:2426-2435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hossain M, Andrew JG. Is there a difference in perioperative mortality between cemented and uncemented implants in hip fracture surgery? Injury. 2012;43:2161-2164. [DOI] [PubMed] [Google Scholar]
- 15.Lamade WR, Friedl W, Schmid B, Meeder PJ. Bone cement implantation syndrome. A prospective randomised trial for use of antihistamine blockade. Arch Orthop Trauma Surg. 1995;114:335-339. [DOI] [PubMed] [Google Scholar]
- 16.Lennox IA, McLauchlan J. Comparing the mortality and morbidity of cemented and uncemented hemiarthroplasties. Injury. 1993;24:185-186. [DOI] [PubMed] [Google Scholar]
- 17.Lin FF, Chen YF, Chen B, Lin CH, Zheng K. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a meta-analysis of randomized controlled trails. Medicine (Baltimore). 2019;98:e14634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu B, Li A, Wang J, et al. Cemented versus uncemented hemiarthroplasty for elderly patients with displaced fracture of the femoral neck: a PRISMA-compliant meta-analysis of randomized controlled trial. Medicine (Baltimore). 2020;99:e21731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luo X, He S, Li Z, Huang D. Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop Trauma Surg. 2012;132:455-463. [DOI] [PubMed] [Google Scholar]
- 20.Middleton RG, Uzoigwe CE, Young PS, Smith R, Gosal HS, Holt G. Peri-operative mortality after hemiarthroplasty for fracture of the hip: does cement make a difference? Bone Joint J. 2014;96-B:1185-1191. [DOI] [PubMed] [Google Scholar]
- 21.Modig J, Olerud S, Malmberg P, Busch C. Medullary fat embolization during total hip replacement surgery: a preliminary report. Injury. 1973;5:161-164. [DOI] [PubMed] [Google Scholar]
- 22.Moerman S, Mathijssen NMC, Niesten DD, et al. More complications in uncemented compared to cemented hemiarthroplasty for displaced femoral neck fractures: a randomized controlled trial of 201 patients, with one year follow-up. BMC Musculoskelet Disord. 2017;18:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Movrin I. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a randomized controlled trial with two years follow-up. Acta Orthop Traumatol Turc. 2020;54:83-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olsen F, Kotyra M, Houltz E, Ricksten SE. Bone cement implantation syndrome in cemented hemiarthroplasty for femoral neck fracture: incidence, risk factors, and effect on outcome. Br J Anaesth. 2014;113:800-806. [DOI] [PubMed] [Google Scholar]
- 25.Parker MI, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: a randomised controlled trial in 400 patients. J Bone Joint Surg Br. 2010;92:116-122. [DOI] [PubMed] [Google Scholar]
- 26.Parvizi J, Holiday AD, Ereth MH, Lewallen DG. The Frank Stinchfield Award. Sudden death during primary hip arthroplasty. Clin Orthop Relat Res. 1999;369:39-48. [DOI] [PubMed] [Google Scholar]
- 27.Patterson BM, Healey JH, Cornell CN, Sharrock NE. Cardiac arrest during hip arthroplasty with a cemented long-stem component. A report of seven cases. J Bone Joint Surg Am. 1991;73:271-277. [PubMed] [Google Scholar]
- 28.Pripp AH, Talsnes O, Reikeras O, Engesaeter LB, Dahl OE. The proportion of perioperative mortalities attributed to cemented implantation in hip fracture patients treated by hemiarthroplasty. Hip Int. 2014;24:363-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Richardson CG, Lethbridge LN, Dunbar MJ. Increased mortality with the use of cementless fixation for femoral neck fractures: analysis of 5883 hip arthroplasty cases. J Arthroplasty. 2020;35:3627-3630. [DOI] [PubMed] [Google Scholar]
- 30.Rutter PD, Panesar SS, Darzi A, Donaldson LJ. What is the risk of death or severe harm due to bone cement implantation syndrome among patients undergoing hip hemiarthroplasty for fractured neck of femur? A patient safety surveillance study. BMJ Open. 2014;4:e004853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sonne-Holm S, Walter S, Jensen JS. Moore hemi-arthroplasty with and without bone cement in femoral neck fractures. A clinical controlled trial. Acta Orthop Scand. 1982;53:953-956. [DOI] [PubMed] [Google Scholar]
- 32.Talsnes O, Hjelmstedt F, Pripp AH, Reikeras O, Dahl OE. No difference in mortality between cemented and uncemented hemiprosthesis for elderly patients with cervical hip fracture. A prospective randomized study on 334 patients over 75 years. Arch Orthop Trauma Surg. 2013;133:805-809. [DOI] [PubMed] [Google Scholar]
- 33.Talsnes O, Vinje T, Gjertsen JE, et al. Perioperative mortality in hip fracture patients treated with cemented and uncemented hemiprosthesis: a register study of 11,210 patients. Int Orthop. 2013;37:1135-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am. 2012;94:577-583. [DOI] [PubMed] [Google Scholar]
- 35.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167:268-274. [DOI] [PubMed] [Google Scholar]
- 36.Veldman HD, Heyligers IC, Grimm B, Boymans TA. Cemented versus cementless hemiarthroplasty for a displaced fracture of the femoral neck: a systematic review and meta-analysis of current generation hip stems. Bone Joint J. 2017;99-B:421-431. [DOI] [PubMed] [Google Scholar]
- 37.White SM, Moppett IK, Griffiths R. Outcome by mode of anaesthesia for hip fracture surgery. An observational audit of 65 535 patients in a national dataset. Anaesthesia. 2014;69:224-230. [DOI] [PubMed] [Google Scholar]
- 38.Yli-Kyyny T, Sund R, Heinanen M, Venesmaa P, Kroger H. Cemented or uncemented hemiarthroplasty for the treatment of femoral neck fractures? Acta Orthop. 2014;85:49-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.