Abstract
Background
The lockdown measure implemented to face the 2019 Coronavirus Disease (COVID-19) first wave deeply modified the lifestyle of the Italian population. Despite its efficacy in limiting the number of infections, forced home confinement was paralleled by sleep/wake cycle disruptions, psychological distress and maladaptive coping strategies (i.e., unhealthy behaviours, such as tobacco and alcohol consumption). Under these unprecedented stress conditions, we explored a possible association between poor sleep quality and increased likelihood of engaging in an unhealthy lifestyle.
Methods
A cross-sectional study was conducted by disseminating an online survey via social networks and e-mail. We collected information on demographics, COVID-19-related data, sleep quality, chronotype, circadian misalignment, and lifestyle before and during the lockdown (i.e., consumption of cigarettes, alcoholic beverages, coffee, hypnotics, comfort food and fresh food; practice of physical activity). A global healthiness score was computed to assess participants’ modifications in lifestyle since the beginning of the lockdown.
Results
1297 respondents were included in the study: 414 (31.9%) from Northern Italy, 723 (55.8%) from Central Italy, 160 (12.3%) from Southern Italy. The following variables were found to be significant predictors of the adoption of an unhealthy lifestyle since the beginning of the lockdown: poor sleep quality, high BMI and considering the measures adopted by the government to fight the pandemic as excessive. Living in Northern Italy, instead, was associated with healthier habits compared to living in Central Italy.
Conclusions
Poor sleepers may represent the share of the general population who paid the highest price for social isolation. Further investigations are required to explore the role of sleep quality assessment in the identification of individuals vulnerable to unhealthy behaviours under stressful conditions.
Keywords: COVID-19, Sleep quality, Lockdown, Healthy behaviours, Psychological well-being, Maladaptive coping
1. Background
On March 11th the World Health Organization declared the 2019 Coronavirus Disease (COVID-19) as a pandemic. Until then, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) identified in the Chinese city of Wuhan in December 2019 [1] had already officially infected 118.000 people across 114 countries [2]. On March 9th in Italy, 9172 people have been infected by the virus, 463 of which died (5% of total number of cases) and 733 (8%) were hospitalized in intensive care units [3]. On the same day the Italian Government implemented an unprecedented lockdown measure on the whole national territory to limit the spread of the disease. Italians were only allowed to leave their homes to satisfy essential needs (e.g., buying food or seeking medical help), or for other limited documented purposes. Only few working categories were granted permission to reach their workplace, while most of working activities were carried out from home [4]. This measure was effective in reducing the number of infections at the price of considerable, negative, socio-economic consequences. From 2019 to 2020, Italian GDP decreased by 8%, deficit/GDP ratio increased from 134.8% to 155.7%, unemployment raised from 10% to 11.6% of the workforce [5]. 51.5% of the Italian company owners declared that, in 2020, they might not have sufficient liquidity to cover the expenditure of the year [6].
Several studies demonstrated how sleep quality deteriorated during the COVID-19 pandemic in the general population in France [7], in Italy [8] and across the globe [9]. Home confinement may disrupt circadian regulation of sleep by reducing light exposure and activity levels during the day. The lack of social interactions, as well as the disruption of daily routine established by working schedule, may also contribute to the onset of sleep problems [10]. Moreover, both pandemic spread and the restrictions of freedom imposed by quarantine possibly generated deep anxious feelings that might have compromised sleep quality [11]. Finally, the negative impact of COVID-19 emergency on mental health is likely to increase the incidence of sleep disturbances, and vice-versa [[12], [13], [14]]. Sleep, indeed, is an important regulator of humans’ emotional functioning, and its role in emotion regulation might explain the association between sleep disorders and poor mental health [15,16], as well as its association with health-related habits [17]. Emotional dysregulation may contribute to the onset and maintenance of unhealthy lifestyle habits under stressful conditions, such as smoking or drinking alcohol [18,19]. Moreover, acute stress is also associated with an increase in coffee consumption, with potential negative consequences on cardiovascular health [20]. Stress may also exert a negative influence on eating behaviour [21]. A clinical trial showed that stressed emotional eaters are more likely to choose sweet high-fat foods and energy-dense foods as compared to both unstressed and unemotional eaters [22]. Some people also tend to increase high-calories comfort food intake when stressed, thereby increasing their risk of developing obesity [23]. It is therefore possible that the systematic adoption of unhealthy behaviours under stress conditions might lead to negative consequences on health both in the short term and in the long run.
It is likely that forced home confinement acted as a chronic stressor for the general population, favouring the spread of behaviours dangerous to health. Moreover, it is also likely that the lockdown might have impacted each person differently, grounded on their individual characteristics. In line with this hypothesis, results from the Italian population showed that cigarettes consumption globally increased, and that the growth in tobacco use was particularly pronounced in participants with higher psychological suffering and disturbed sleep [24].In parallel, a study conducted on Italian medical students showed that during the lockdown participants practiced less physical activity, especially when affected by sleep disturbances [25]. The increased prevalence in sleep disturbances is likely to explain the increased use of hypnotic drugs reported during the lockdown [26].
Forced home confinement also modified dietary habits. A decrease in fresh food intake and an increase in comfort food intake have been observed during the lockdown both in the US and in Italy [28,29]. The Italian general population registered a worsening in eating behaviour (e.g., in the frequency of snacking between meals), most apparent in participants with a high Body Mass Index (BMI) [30]. Therefore, it is possible that both disturbed sleep and high BMI might represent vulnerabilities in facing stress induced by COVID-19 emergency.
The aim of this study is to explore a possible association between poor sleep quality and unhealthy lifestyle in the Italian population during the lockdown. We hypothesized that poor sleepers represent the most vulnerable share of the general population whose lifestyle has been globally and negatively affected by the COVID-19 emergency.
2. Material and methods
2.1. Study design and participants
This study is part of a wider project named “RestAcasa”, aimed at exploring the routine habits and psychological well-being of the Italian population during the lockdown.
A web-based survey was disseminated by e-mail and through social networks (LinkedIn, Facebook, Instagram, WhatsApp) to conduct a cross-sectional study. Data were collected from April 29th to May 17th, when the Italian government granted a significant relaxation of the restrictive measures.
An informed consent was electronically obtained from each participant by ticking a mandatory box before answering the survey. Inclusion criteria were:
-
-
having attained the age of eighteen;
-
-
being fluent in the Italian language;
-
-
living in Italy while participating in the study.
The study was conducted in accordance with the declaration of Helsinki and received the approval of Bioethical Committee of the University of Pisa on April 28th, with protocol number 0040387/2020.
The survey consisted of a combination of validated questionnaires and ad hoc questions on demographics and COVID-19-related information. The average completion time was 40 minutes. Out of 1716 participants who started filling the questionnaire, 392 withdrew before ending, 25 were furtherly excluded because not resident in Italy during the lockdown, 2 were removed because they were duplicates and 1 because of the impossibility to properly interpret questionnaires’ answers. Data analyses were performed on a final sample of 1297 participants.
2.2. Materials
2.2.1. Demographics and COVID-19 related information
The questionnaire collected data on age, sex, height, weight, region of residence, level of education, occupation and included a section on pandemic-related data.
The level of education was explored through a multiple-choice question, with four possible answers:
-
-
Middle school degree
-
-
High school degree
-
-
Graduation
-
-
Post-graduation
Working condition was explored through a multiple-choice question, with three possible answers:
-
-
Working from home
-
-
Working at the workplace
-
-
Unemployed
The COVID-19 section assessed:
-
-
the perceived severity of the disease, evaluated on a 4-point Likert scale (“Very severe”, “Severe”, “Fairly severe”, “Not severe”) [31]. Only seven participants answered “Not severe”: data analysis was therefore performed considering participants who answered “Not severe” and “Fairly severe” as a single group;
-
-
the economic impact of the lockdown, which could be rated as “Positive”, “Negative”, or “Not significant”;
-
-
the perceived efficacy of the measures adopted by Italian government to face pandemic's spread, which could be rated as “Not effective”, “Effective” or “Excessive”.
2.2.2. Healthy behaviours
Participants were asked to report their levels of consumption of coffee, alcohol, cigarettes, hypnotics and their purchase habits for comfort food and fresh food products, both during and before the lockdown. Caffeine and tobacco use was reported by participants as the daily number of coffee drunk and cigarettes smoked both during and before the lockdown. Hypnotics consumption was instead evaluated in terms of weekly frequency of use (“Never”, “Less than once a week”, “Once a week”, “More than once a week”, “Every day”, “More than once a day”), including both medications available only by prescription and over-the-counter sleep aids. Comfort food and fresh food purchase, as well as alcohol consumption, were evaluated through a single item assessing modifications in these behaviours comparing the pre-lockdown and the lockdown period. A set of healthy behaviour-related variables was computed by comparing self-reported participants’ lifestyle during the lockdown to their lifestyle in the pre-lockdown period. The frequency of engaging in each behaviour might be decreased, unchanged or increased. Participants were also asked whether they practiced physical activity both during and before the lockdown. Questionnaire items exploring healthy behaviours are provided in Appendix 1.
A global score of healthiness was finally calculated by summing up the values assigned to the healthy behaviour-related variables, as it follows: 1 point for each increase in coffee, alcohol, cigarettes, hypnotics, comfort food consumption. Also, participants who stopped practicing physical activity during lockdown or decrease fresh food consumption scored 1 point. Healthiness score ranged from 0 (healthy lifestyle change) to 7 (unhealthy lifestyle change).
2.2.3. Sleep and chronobiological parameters
Sleep quality was assessed through the Pittsburgh Sleep Quality Index (PSQI). The 19-item questionnaire evaluates seven different dimensions of sleep (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications and daytime dysfunction). The global score is calculated by summing up each component's score. It can range from 0 to 21. The higher PSQI score, the worse the participants' sleep quality. A score greater than 5 conventionally identifies poor sleepers [32]. The Italian version of the questionnaire has been validated by Curcio and colleagues [33].
The reduced version of the Morningness/Eveningness Questionnaire (rMEQ) was used to assess participants’ chronotype. The 5-item questionnaire score ranges from 4 to 26, being a lower score indicative of a greater eveningness and a higher score of morningness [34,35]. The questionnaire was translated and adapted into Italian language by Natale and colleagues [36,37].
Circadian misalignment was assessed through a 7-item questionnaire asking:
-
-
the preferred time for sleep onset;
-
-
the preferred time for sleep offset;
-
-
the average sleep onset on working days;
-
-
the average sleep offset on working days;
-
-
the average sleep onset on free days;
-
-
the average sleep offset on free days;
-
-
the number of working days in a week.
The preferred sleep midpoint and the sleep midpoint during working days and free days were calculated by subtracting the sleep onset time from the sleep offset time and dividing by 2 as described elsewhere [38]. The average sleep midpoint was defined as the weighted mean of sleep midpoint during free days and sleep midpoint during working days [39]. Finally, the absolute value of the difference between the preferred sleep midpoint and the average sleep midpoint was used as a proxy for circadian misalignment.
2.2.4. Intensive care unit beds
The number of Intensive Care Unit (ICU) beds occupied by COVID-19 patients per 100.000 population of each Italian region was used as an index of both pandemic spread and workload of local health service. The data on the progress of the pandemic in Italy are freely available in an online repository updated daily since 2020 February 24th [3]. The number of COVID-19 patients currently in intensive care on April the 30th (the day after data collection start) was normalized by the number of inhabitants of each region reported the same day by the Italian Statistical Institute (ISTAT) [40].
2.3. Statistical analyses
Statistical analyses were performed using R 4.0.4. Mean and standard deviation described the distribution of quantitative variables, whereas frequencies and percentages were provided for the categorical ones. The Fisher test was run to compare health-related variables (i.e., cigarettes, alcohol, coffee, hypnotics, comfort food, fresh food consumption; physical exercise) distribution according to sex, level of education, working condition, perceived severity of COVID-19, perceived effectiveness of anti-COVID-19 measures, economic impact of the lockdown. The ANOVA test was used to compare age, BMI, sleep quality (PSQI), chronotype (rMEQ) and circadian misalignment among the groups identified by the health-related variables. To investigate more in detail the relationship between sleep quality and healthy behaviour, the post-hoc HSD Tukey test was used for pairwise comparisons. Eta squared (η2) was used to quantify the strength of the association between sleep and chronobiologic parameters (sleep quality, chronotype and circadian misalignment), on the one side, and healthy behaviours on the other side. A linear regression model was estimated to identify the possible predictors of the adoption of unhealthy lifestyle-related changes during the lockdown, considering as regressors: age, sex, BMI, education, region, working condition, ICU beds occupied by COVID-19 patients per 100.000 population, economic impact of the lockdown, perceived severity of COVID-19, perceived efficacy of the anti-COVID-19 measures, sleep quality, chronotype and circadian misalignment; and the global healthiness score as dependent variable. All statistical tests were two-sided, and the level of significance was set at 0.05.
3. Results
3.1. Descriptive statistics
The descriptive statistics of the sample are displayed in Table 1 . The average age was 39.17 years (±14.97) and the average BMI 23.6 kg/m2 (±3.86). 60.1% of participants declared they worked from home, while 16% were allowed to reach their workplace and 23.9% were unemployed. The sample was mainly composed of women (61.9%) and showed a high level of education (64.4% graduated or with a higher level of education). Most of participants lived in Central Italy (55.8%), 31.9% in Northern Italy and 12.3% in Southern Italy. Taken together these findings suggest that the sample is not representative of the Italian general population: in fact, on April 30th (the day after data collection started) females represented the 51.3% of the Italian population; 46.3% of the Italian population lived in Northern Italy, 19.8% in Central Italy, and 28.9% in Southern Italy; at the end of the second trimester of 2020, people with a Bachelor's degree or higher qualification represented the 15% of Italian people above 15 years [40]. While this may introduce bias, estimating an adjusted regression model, in which we incorporated potential predictors of the outcome, may improve the generalizability of our results and alleviate possible self-selection of the respondents.
Table 1.
Descriptive statistics.
| Age (years) | 39.17 (14.96) |
| Sex | |
| Females | 803 (61.9%) |
| Males | 494 (38.1%) |
| BMI (kg/m2) | 23.6 (3.86) |
| Education | |
| Middle school | 37 (2.9%) |
| High school | 424 (32.7%) |
| Graduation | 634 (48.8%) |
| Post-graduation | 202 (15.6%) |
| Region | |
| Northern Italy | 414 (31.9%) |
| Central Italy | 723 (55.8%) |
| Southern Italy | 160 (12.3%) |
| Working condition | |
| Home | 779 (60.1%) |
| Workplace | 208 (16%) |
| Unemployed | 310 (23.9%) |
| Severity of the disease | |
| Fairly severe | 80 (6.2%) |
| Severe | 724 (55.8%) |
| Very severe | 493 (38%) |
| Effectiveness of anti-COVID19 measures | |
| Not effective | 130 (10%) |
| Effective | 1082 (83.4%) |
| Excessive | 85 (6.6%) |
| Economic impact of the lockdown | |
| Negative | 767 (59.1%) |
| No impact | 468 (36.1%) |
| Positive | 62 (4.8%) |
| Sleep quality (PSQI) | 5.52 (3.2) |
| Chronotype (rMEQ) | 15.05 (3.74) |
| Circadian misalignment (hours) | 00:40 (00:38) |
Mean and standard deviation are reported for the quantitative variables, frequency and percentage for the categorical ones.
BMI: Body Mass Index.
PSQI: Pittsburgh Sleep Quality Index.
rMEQ: reduced Morningness/Eveningness Questionnaire.
Circadian misalignment was computed as the absolute value of the difference between the preferred midsleep point and the average midsleep point.
N = 1297.
With respect to pandemic-related variables, nearly all participants considered COVID-19 a severe or very severe disease (93.8%); 83.4% believed that the measure adopted by the Italian government to counteract the spread of the virus were effective (10% Not effective, 6.6% Excessive); and more than half of them reported that the lockdown had a negative impact on their financial situation (59.1%).
Regarding sleep and chronobiological parameters, participants’ sleep quality (PSQI) was poor on average (5.52 ± 3.2), while chronotype (rMEQ) distribution did not appear to be different from that reported by literature (29.7% morning types, 18.1% evening types) [41]. Data on circadian misalignment suggest that the preferred time window dedicated to sleep was on average delayed as compared to the actual one (00:40 ± 00:38).
3.2. Sleep quality, chronotype, circadian misalignment and healthy behaviours
Table 2 summarizes sleep and chronobiological parameters distribution according to the different lifestyle variables. To identify possible differences in sleep quality, chronotype and circadian misalignment among participants who increased, decreased or left unchanged their likelihood of engaging in each behaviour of interest during the lockdown, we performed the ANOVA test and computed the Eta squared coefficient (η2).
Table 2.
Mean and standard deviation of sleep and chronobiological parameters in the whole sample and according to the pre-lockdown vs lockdown lifestyle changes.
| Sleep Quality | Chronotype | Circadian misalignment | ||
|---|---|---|---|---|
| Physical activity (n = 1297) | Did not stop (n = 1079) | 5.43 (3.11) | 15 (3.69) | 00:40 (00:38) |
| Stopped (n = 218) | 5.95 (3.60) | 15.2 (3.97) | 00:39 (00:40) | |
| η2 | 0.0037 | 0.00015 | 0.0000024 | |
| p value | 0.029∗ | 0.66 | 0.96 | |
| Coffee consumption (n = 1297) | Decreased (n = 448) | 5.4 (3.09) | 14.3 (3.69) | 00:44 (00:41) |
| Unchanged (n = 703) | 5.45 (3.23) | 15.6 (3.62) | 00:36 (00:35) | |
| Increase (n = 146) | 6.25 (3.3) | 14.6 (3.99) | 00:43 (00:42) | |
| η2 | 0.0066 | 0.029 | 0.0087 | |
| p value | 0.014∗ | <0.001∗ | 0.004∗ | |
| Cigarette consumption (n = 1297) | Decreased (n = 139) | 5.84 (3.18) | 13.2 (3.76) | 00:55 (00:48) |
| Unchanged (n = 1054) | 5.37 (3.19) | 15.4 (3.64) | 00:36 (00:35) | |
| Increase (n = 104) | 6.59 (3.18) | 14.1 (3.89) | 00:52 (00:46) | |
| η2 | 0.012 | 0.037 | 0.031 | |
| p value | <0.001∗ | <0.001∗ | <0.001∗ | |
| Alcohol consumption (n = 1297) | Decreased (n = 441) | 5.49 (3.18) | 14.3 (3.76) | 00:47 (00:42) |
| Unchanged (n = 690) | 5.29 (3.13) | 15.7 (3.56) | 00:38 (00:38) | |
| Increase (n = 166) | 6.56 (3.37) | 14.3 (3.88) | 00:48 (00:43) | |
| η2 | 0.016 | 0.036 | 0:38 | |
| p value | <0.001∗ | <0.001∗ | 0.02∗ | |
| Hypnotics consumption (n = 1297) | Decreased (n = 54) | 5.7 (2.46) | 15.3 (4.1) | 00:41 (00:39) |
| Unchanged (n = 1140) | 5.24 (3.06) | 15.1 (3.73) | 00:34 (00:35) | |
| Increase (n = 103) | 8.58 (3.48) | 14.1 (3.59) | 00:44 (00.43) | |
| η2 | 0.08 | 0.0051 | 0.08 | |
| p value | <0.001∗ | 0.037∗ | 0.003∗ | |
| Comfort food purchase (n = 1109) | Decreased (n = 290) | 5.75 (3.44) | 15.3 (3.76) | 00:35 (00:33) |
| Unchanged (n = 538) | 5.24 (3.16) | 15.2 (3.57) | 00:37 (00:38) | |
| Increased (n = 281) | 5.84 (3.11) | 14.5 (3.85) | 00:44 (00:40) | |
| η2 | 0.0075 | 0.0077 | 0.010 | |
| p value | 0.016∗ | 0.014∗ | 0.006∗ | |
| Fresh products purchase (n = 1109) | Decreased (n = 199) | 5.99 (3.6) | 15.1 (3.67) | 00:35 (00:33) |
| Unchanged (n = 560) | 5.32 (3.2) | 15.2 (3.8) | 00:37 (00:38) | |
| Increase (n = 350) | 5.58 (3.04) | 14.7 (3.55) | 00:44 (00:40) | |
| η2 | 0.0059 | 0.0036 | 0.0093 | |
| p value | 0.038∗ | 0.135 | 0.006∗ |
Sleep quality was measured through the Pittsburgh Sleep Quality Index (PSQI).
Chronotype was measured through the reduced version of the Morningness/Eveningness Questionnaire (rMEQ).
Circadian misalignment was computed as the absolute value of the difference between preferred midsleep point and average midsleep point.
∗Level of significance set at 0.05.
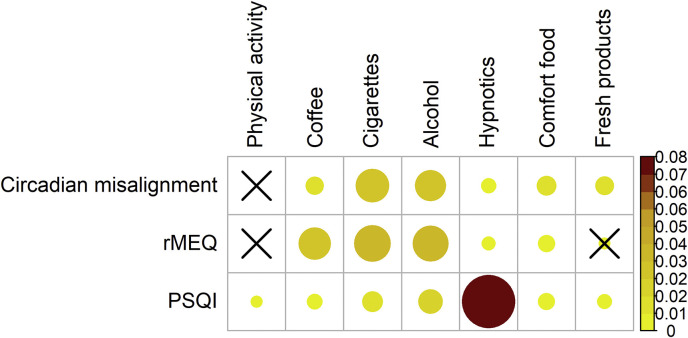
Overall, both sleep and circadian parameters were significantly associated with a change in most of the behaviours taken into account (Fig. 1 ). Sleep quality was significantly associated with each health-related variable; chronotype with each healthy behaviour change with the exclusion of physical activity and fresh food purchase; circadian misalignment with each variable except for physical activity. According to standard criteria used to interpret η2 value (η2 = 0.01, small effect size; η2 = 0.06, medium effect size, η2 = 0.14 large effect size) [42], almost all the effect sizes of the associations between sleep and chronobiological parameters and health-related variables are small. The association between sleep quality and hypnotics use, instead, showed a medium effect size.
Fig. 1.
Effect size of the comparisons between sleep quality (PSQI) and chronobiological metrics (rMEQ and circadian misalignment, rows) and healthy behaviours (columns). Effect size is represented by eta squared (η2) and its value is directly proportional to both size and colour intensity of the circles. “X” stands for non-significant associations. rMEQ stands for “reduced Morningness/Eveningness Questionnaire”. PSQI stands for “Pittsburgh Sleep Quality Index”.
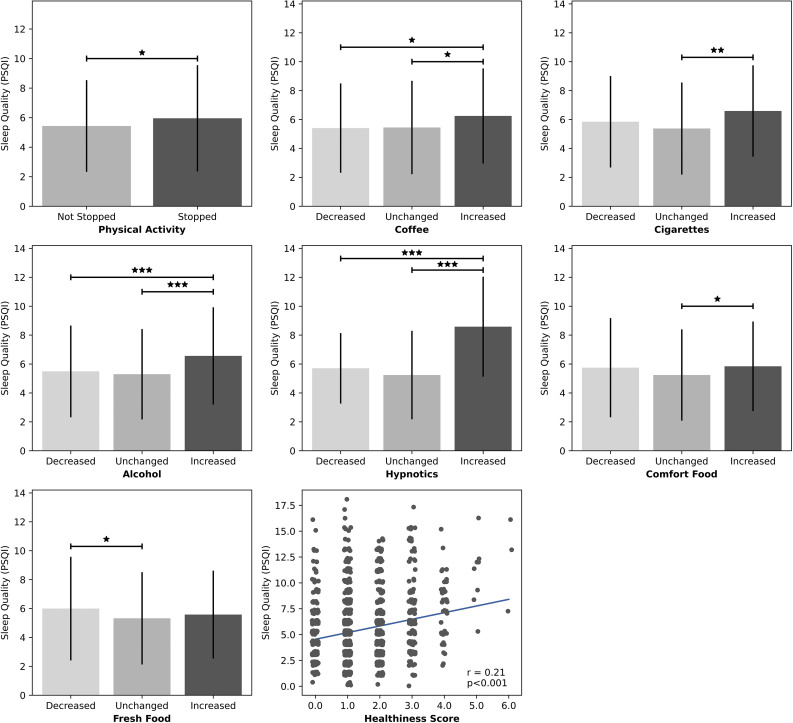
PSQI score was consistently higher in participants who reported to adopt an unhealthier lifestyle since the beginning of the lockdown across all behaviours as compared to people who did not change their habits or even improved their behaviours (Fig. 2 ). To verify the hypothesized association between poor sleep quality and unhealthy lifestyle change, we ran the Tukey HSD test to compare the mean PSQI score of the groups identified by each health-related variable. We found that sleep quality was significantly lower in participants who adopted a less healthy behaviour. Moreover, PSQI score was positively and significantly correlated with the global healthiness score (Pearson test; r = 0.21, p < 0.001), so that the worse participants slept, the more their lifestyle became unhealthy.
Fig. 2.
PSQI score distribution across different healthy behaviours and healthiness score. Sleep quality (PSQI score) is consistently poorer (higher) in participants who adopted an unhealthier lifestyle since the beginning of the lockdown as compared to people who did not change their habits or improved their behaviours. As expected, PSQI score (poor sleep quality) also significantly and positively correlates with the global healthiness score (adoption of unhealthier lifestyle). Significance code: ∗ < 0.05; ∗∗ < 0.01; ∗∗∗ < 0.001.
3.3. Demographics, COVID-19 related data and healthy behaviours
Table 3a, Table 3ba and 3b summarizes demographic and pandemic-related characteristics of the sample according to lifestyle changes. 16.8% of participants declared to have stopped practicing physical activity; 11.3% to have increased coffee consumption; 8% to have increased cigarettes consumption; 12.8% to have increased alcohol consumption; 7.9% to have increased the use of hypnotics; 25.3% to have increased the purchase of comfort food and 17.9% to have instead decreased the purchase of fresh food products.
Table 3a.
Socio-demographics characteristics of the sample according to the pre-lockdown vs lockdown lifestyle changes.
| Age (years) | Sex |
BMI (kg/m2) | Education |
Working condition |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Females | Males | Middle school | High school | Graduation | Post-graduation | Home | Workplace | Unemployed | ||||
| Physical activity (n = 1297) | Did not stop (n = 1079) |
38.4 (14.8) | 684 (85.2%) | 395 (80%) | 23.4 (3.89) | 28 (75.7%) | 348 (82.1%) | 535 (84.4%) | 167 (83.1%) | 656 (84.2%) | 171 (82.2%) | 252 (81.3%) |
| Stopped (n = 218) | 43.2 (15.2) | 119 (14.8%) | 99 (20%) | 24.4 (3.51) | 9 (24.3%) | 76 (17.9%) | 99 (15.6%) |
34 (16.9%) |
123 (15.8%) | 37 (17.8%) |
58 (18.7%) |
|
| p value | <0.001∗ | 0.018∗ | <0.001∗ | 0.312 | 0.443 | |||||||
| Coffee consumption (n = 1297) | Decreased (n = 448) | 36 (13.4) | 278 (34.6%) | 170 (34.5%) | 23.4 (3.69) | 14 (37.9%) | 130 (30.7%) | 234 (36.9%) | 69 (34.3%) |
293 (37.6%) | 61 (29.3%) |
94 (30.3%) |
| Unchanged (n = 703) | 41.4 (15.6) | 438 (54.5%) | 265 (53.6%) | 23.7 (3.9) | 20 (54%) | 236 (55.7%) | 340 (53.6%) | 107 (53.2%) | 395 (50.7%) | 121 (58.2%) | 187 (60.3%) |
|
| Increased (n = 146) | 37.7 (14.5) | 87 (10.9%) | 59 (11.9%) | 23.8 (4.14) | 3 (8.1%) | 58 (13.6%) | 60 (9.5%) |
25 (12.5%) |
91 (11.7%) | 26 (12.5%) |
29 (9.4%) |
|
| p value | <0.001∗ | 0.828 | 0.31 | 0.525 | 0.024∗ | |||||||
| Cigarettes consumption (n = 1297) | Decreased (n = 139) | 29.6 (10.5) | 82 (10.2%) | 57 (11.5%) | 22.8 (3.45) | 5 (13.5%) | 58 (13.7%) | 63 (9.9%) |
12 (6%) |
88 (11.3%) | 18 (8.7%) |
33 (10.7%) |
| Unchanged (n = 1054) | 40.6 (15.1) | 657 (81.8%) | 397 (80.4%) | 23.7 (3.9) | 28 (75.7%) | 322 (75.9%) | 522 (82.3%) | 182 (89.6%) | 635 (81.5%) | 170 (81.7%) | 249 (80.3%) |
|
| Increased (n = 104) | 37.3 (13.8) | 64 (8%) |
40 (8.1%) | 23.2 (3.83) | 4 (10.8%) | 44 (10.4%) | 49 (7.8%) |
7 (3.4%) |
56 (7.2%) | 20 (9.6%) |
28 (9%) |
|
| p value | <0.001∗ | 0.73 | 0.02∗ | <0.001∗ | 0.572 | |||||||
| Alcohol consumption (n = 1297) | Decreased (n = 441) | 33 (13.3) | 270 (33.6%) | 171 (34.6%) | 23 (3.61) | 17 (46%) | 162 (38.2%) | 215 (33.9%) | 47 (23.4%) |
287 (36.8%) | 51 (24.6%) |
103 (33.2%) |
| Unchanged (n = 690) | 43.2 (15.2) | 446 (55.5%) | 244 (49.4%) | 23.9 (4) |
15 (40.5%) | 223 (52.6%) | 329 (51.9%) | 122 (60.7%) | 390 (50.1%) | 128 (61.5%) | 172 (55.5%) |
|
| Increased (n = 166) | 39 (12.2) | 87 (10.8%) | 79 (16%) | 23.6 (3.74) | 5 (13.5%) | 39 (9.2%) | 90 (14.2%) |
32 (15.9%) |
102 (13.1%) | 29 (13.9%) |
35 (11.3%) |
|
| p value | <0.001∗ | 0.014∗ | 0.001∗ | <0.001∗ | 0.011∗ | |||||||
| Hypnotics consumption (n = 1297) | Decreased (n = 54) | 34.3 (13.1) | 39 (4.9%) | 15 (3%) |
22.1 (2.91) | 3 (8.1%) | 15 (3.5%) | 29 (4.6%) |
7 (3.4%) |
39 (5%) |
5 (2.4%) |
10 (3.2%) |
| Unchanged (n = 1140) | 39.7 (15.1) | 691 (86.1%) | 449 (90.9%) | 23.6 (3.89) | 33 (89.2%) | 373 (88%) | 557 (87.9%) | 176 (87.6%) | 679 (87.2%) | 183 (88%) |
278 (89.7%) |
|
| Increased (n = 103) | 35.4 (12.8) | 73 (9%) |
30 (6.1%) | 23.7 (3.79) | 1 (2.7%) | 36 (8.5%) | 48 (7.6%) |
18 (9%) |
61 (7.8%) | 20 (9.6%) |
22 (7.1%) |
|
| p value | 0.001∗ | 0.035∗ | 0.01∗ | 0.849 | 0.345 | |||||||
| Comfort food purchase (n = 1109) | Decreased (n = 290) | 40.6 (16) | 185 (26.8%) | 105 (25.1%) | 23.6 (3.98) | 10 (37%) | 99 (28.3%) | 140 (25.3%) | 41 (23%) |
169 (25.7%) | 56 (29.2%) |
65 (25.1%) |
| Unchanged (n = 538) | 40.4 (14.9) | 331 (48%) | 207 (49.4%) | 23.5 (3.86) | 14 (51.9%) | 161 (46%) | 276 (49.9%) | 87 (48.9%) |
313 (47.6%) | 92 (47.9%) |
133 (51.4%) |
|
| Increased (n = 281) | 36.9 (12.7) | 174 (25.2%) | 107 (25.5%) | 23.7 (4.02) | 3 (11.1%) | 90 (25.7%) | 137 (24.8%) | 50 (28.1%) |
176 (26.7%) | 44 (22.9%) |
61 (23.6%) |
|
| p value | 0.002∗ | 0.813 | 0.76 | 0.189 | 0.621 | |||||||
| Fresh products purchase (n = 1109) | Decreased (n = 199) | 39.2 (14.2) | 126 (18.3%) | 73 (17.4%) | 23.5 (3.82) | 3 (11.1%) | 61 (17.4%) | 103 (18.7%) | 32 (18%) |
121 (18.4%) | 38 (19.8%) |
40 (15.4%) |
| Unchanged (n = 560) | 40.2 (15.5) | 346 (50.1%) | 214 (51.1%) | 23.9 (4.24) | 17 (63%) | 192 (54.9%) | 264 (47.7%) | 87 (48.9%) |
322 (48.9%) | 99 (51.6%) |
139 (53.7%) |
|
| Increased (n = 350) | 38.9 (13.9) | 218 (40.6%) | 132 (31.5%) | 23.1 (3.38) | 7 (25.9%) | 97 (27.7%) | 186 (33.6%) | 59 (33.1%) |
215 (32.7%) | 55 (28.6%) |
80 (30.9%) |
|
| p value | 0.39 | 0.931 | 0.007∗ | 0.115 | 0.555 | |||||||
∗Level of significance set at 0.05.
Mean and standard deviation are reported for quantitative variables, frequency and percentage for categorical ones.
BMI: Body Mass Index.
Table 3b.
Region of residence and pandemic-related variables according to the pre-lockdown vs lockdown lifestyle changes.
| Region |
Severity of the disease |
Effectiveness of anti-COVID19 measures |
Economic impact of the lockdown |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Northern Italy | Central Italy | Southern Italy | Fairly severe | Severe | Very severe | Not effective | Effective | Excessive | Negative | No impact | Positive | ||
| Physical activity (n = 1297) | Did not stop (n = 1079) |
361 (87.2%) | 591 (81.7%) | 127 (79.4%) | 62 (77.5%) | 604 (83.4%) | 413 (83.8%) | 110 (84.6%) | 907 (83.8%) | 62 (72.9%) |
644 (84%) | 379 (84.8%) | 56 (90.3%) |
| Stopped (n = 218) | 53 (12.8%) |
132 (18.3%) | 33 (20.6%) |
18 (22.5%) | 120 (16.6%) | 80 (16.2%) | 20 (15.4%) | 175 (16.2%) | 23 (27.1%) |
123 (16%) | 89 (15.2%) | 6 (9.7%) |
|
| p value | 0.021∗ | 0.358 | 0.041∗ | 0.124 | |||||||||
| Coffee consumption (n = 1297) | Decreased (n = 448) | 159 (38.4%) | 233 (32.2%) | 56 (35%) |
25 (31.2%) | 249 (34.4%) | 174 (35.3%) | 55 (42.3%) | 358 (33.1%) | 35 (41.2%) |
275 (35.9%) | 149 (31.8%) | 24 (38.7%) |
| Unchanged (n = 703) | 214 (51.7%) | 403 (55.7%) | 86 (53.8%) |
42 (52.5%) | 402 (55.5%) | 259 (52.3%) | 63 (48.4%) | 601 (55.5%) | 39 (45.9%) |
404 (56.7%) | 272 (58.1%) | 27 (43.5%) | |
| Increased (n = 146) | 41 (9.9%) |
87 (12.1%) | 18 (11.2%) |
13 (16.3%) | 73 (10.1%) | 60 (12.2%) | 12 (9.3%) | 123 (11.4%) | 11 (12.9%) |
88 (7.4%) |
47 (10.1%) | 11 (17.8%) | |
| p value | 0.313 | 0.413 | 0.137 | 0.104 | |||||||||
| Cigarettes consumption (n = 1297) | Decreased (n = 139) | 39 (9.4%) |
69 (9.5%) | 31 (19.4%) |
11 (13.7%) | 85 (11.7%) | 43 (8.7%) | 13 (10%) |
119 (11%) | 7 (8.2%) |
82 (10.7%) | 49 (10.5%) | 8 (12.9%) |
| Unchanged (n = 1054) | 345 (83.3%) | 594 (82.2%) | 115 (71.9%) | 59 (73.8%) | 577 (79.7%) | 418 (84.8%) | 108 (83.1%) | 879 (81.2%) | 67 (78.8%) |
620 (80.8%) | 389 (83.1%) | 45 (72.6%) | |
| Increased (n = 104) | 30 (7.2%) |
60 (8.3%) | 14 (8.7%) |
10 (12.5%) | 62 (8.6%) | 32 (6.5%) | 9 (6.9%) |
84 (7.8%) | 11 (13%) |
65 (8.5%) | 30 (6.4%) | 9 (14.5%) | |
| p value | 0.008∗ | 0.066 | 0.505 | 0.188 | |||||||||
| Alcohol consumption (n = 1297) | Decreased (n = 441) | 141 (34.1%) | 226 (31.2%) | 74 (46.3%) |
29 (36.3%) | 256 (35.4%) | 156 (31.7%) | 39 (30%) |
377 (34.8%) | 25 (29.4%) |
254 (33.1%) | 159 (34%) | 28 (45.2%) |
| Unchanged (n = 690) | 220 (53.1%) | 389 (53.8%) | 81 (50.6%) |
36 (45%) | 368 (50.8%) | 286 (58%) | 65 (50%) |
583 (53.9%) | 42 (49.4%) |
407 (53%) | 264 (56.4%) | 19 (30.6%) | |
| Increased (n = 166) | 53 (12.8%) |
108 (15%) | 5 (3.1%) |
15 (18.7%) | 100 (13.8%) | 51 (10.3%) | 26 (20%) |
122 (11.3%) | 18 (21.2%) |
106 (13.9%) | 45 (9.6%) | 15 (24.2%) | |
| p value | <0.001∗ | 0.033∗ | 0.011∗ | <0.001∗ | |||||||||
| Hypnotics consumption (n = 1297) | Decreased (n = 54) | 20 (4.8%) |
26 (3.6%) | 8 (5%) |
2 (2.4%) |
25 (3.5%) | 27 (5.5%) | 6 (4.6%) |
44 (4.1%) | 4 (4.7%) |
32 (4.2%) | 16 (3.4%) | 6 (9.7%) |
| Unchanged (n = 1140) | 374 (90.4%) | 632 (87.4%) | 134 (83.8%) | 71 (88.8%) | 641 (88.5%) | 428 (86.8%) | 110 (84.6%) | 957 (88,4%) | 73 (85.9%) |
668 (87.1%) | 419 (89.5%) | 53 (85.5%) | |
| Increased (n = 103) | 20 (4.8%) |
65 (9%) |
18 (11.2%) |
7 (8.8%) |
58 (8%) |
38 (7.7%) | 14 (10.8%) | 81 (7.5%) | 8 (9.4%) |
67 (8.7%) | 33 (7.1%) | 3 (4.8%) |
|
| p value | 0.027∗ | 0.485 | 0.597 | 0.162 | |||||||||
| Comfort food purchase (n = 1109) | Decreased (n = 290) | 87 (24.3%) |
154 (24.3%) | 49 (41.5%) |
16 (23.5%) | 156 (25%) | 118 (28.4%) | 29 (25.7%) | 234 (25.4%) | 27 (36%) |
174 (26%) | 100 (25.8%) | 16 (30.2%) |
| Unchanged (n = 538) | 189 (52.8%) | 310 (49%) | 39 (33.1%) |
34 (50%) |
304 (48.6%) | 200 (48,1%) | 50 (44.2%) | 461 (50.1%) | 27 (36%) |
319 (47.7%) | 197 (50.9%) | 22 (41.5%) | |
| Increased (n = 281) | 82 (22.9%) | 169 (26.7%) | 30 (25.4%) |
18 (26.5%) | 165 (26.4%) | 98 (23.6%) | 34 (30.1%) | 226 (24.5%) | 21 (28%) |
176 (26.3%) | 90 (23.3%) | 15 (28.3%) | |
| p value | 0.001∗ | 0.706 | 0.097 | 0.621 | |||||||||
| Fresh products purchase (n = 1109) | Decreased (n = 199) | 50 (14%) |
125 (19.7%) | 24 (20.4%) |
7 (10.3%) | 111 (17.8%) | 81 (19.5%) | 20 (17.7%) | 166 (18%) | 13 (17.3%) |
118 (17.6%) | 70 (18.1%) | 11 (20.8%) |
| Unchanged (n = 560) | 179 (50%) |
321 (50.7%) | 60 (50.8%) |
41 (60.3%) | 310 (49.6%) | 209 (50.2%) | 52 (46%) |
470 (51%) | 38 (50.7%) |
348 (52%) | 189 (48.8%) | 23 (43.4%) | |
| Increased (n = 350) | 129 (36%) |
187 (19.6%) | 34 (28.8%) |
20 (29.4%) | 204 (32.6%) | 126 (30.3%) | 41 (36.3%) | 285 (29.7%) | 24 (32%) |
203 (30.4%) | 128 (33.1%) | 19 (35.8%) | |
| p value | 0.084 | 0.323 | 0.838 | 0.668 | |||||||||
∗Level of significance set at 0.05.
Frequency and percentage are reported for categorical variables.
The Fisher and ANOVA test were used to compare socio-demographic and COVID-related variables distribution among the different groups identified through behavioural changes. The number of significant associations per independent variable varied from one (perceived severity of COVID-19, economic impact of the lockdown) to five (BMI, Region) or six (Age) out of seven. Each independent variable was significantly associated with at least one behaviour of interest. Results suggest that socio-demographic and COVID-related variables may have influenced participants’ lifestyle during the lockdown. The regression model estimated to assess the impact of sleep-related parameters on health-related variables was therefore adjusted for all these covariates.
3.4. Predictors of the global healthiness score
To disentangle the effect of demographics, COVID-19-related data, sleep quality (PSQI), chronotype and circadian misalignment on the propensity to adopt an unhealthy lifestyle since the beginning of the lockdown, a linear regression model was estimated considering the global healthiness score as dependent variable and the following predictors as independent variables: age, sex, BMI, education, region, working condition, perceived severity of COVID-19, perceived efficacy of the anti-COVID-19 measures, economic impact of the lockdown, ICU beds occupied by COVID-19 patients per 100.000 population, PSQI score, rMEQ score and circadian misalignment.
As shown in Table 4 , PSQI score, BMI, region of residence and perceived efficacy of the anti-COVID-19 measures significantly predict the global healthiness score. Poor sleepers, participants with higher BMI and those who considered anti-COVID19 measures as excessive adopted an unhealthier lifestyle during the lockdown compared to the pre-lockdown period; also, participants who spent the lockdown in Northern Italy adopted a healthier lifestyle when compared to residents of Central Italy.
Table 4.
Linear regression model testing the impact of sleep, chronobiology, demographics and COVID-19-related data on the global healthiness score.
| Estimate | Standard error | p value | ||
|---|---|---|---|---|
| Intercept | 0.55 | 0.34 | 0.011∗ | |
| Circadian misalignment (fraction of day) | 0.77 | 1.26 | 0.54 | |
| Sleep quality (PSQI) | 0.070 | 0.010 | <0.001∗∗ | |
| Chronotype (rMEQ) | −0.012 | 0.0092 | 0.20 | |
| Age (years) | −0.0012 | 0.0026 | 0.65 | |
| Sex | Female | |||
| Male | 0.13 | 0.070 | 0.059 | |
| BMI (kg/m2) | 0.017 | 0.0088 | 0.049∗ | |
| Education | Middle school | |||
| High school | 0.17 | 0.21 | 0.43 | |
| Graduation | 0.11 | 0.21 | 0.61 | |
| Post-graduation | 0.20 | 0.22 | 0.37 | |
| Region | Central Italy | |||
| Northern Italy | −0.27 | 0.072 | <0.001∗∗ | |
| Southern Italy | −0.048 | 0.13 | 0.72 | |
| Working condition | Unemployed | |||
| Home | 0.083 | 0.080 | 0.31 | |
| Workplace | 0.12 | 0.10 | 0.24 | |
| Economic impact of the lockdown | Not significant | |||
| Negative | 0.12 | 0.067 | 0.085 | |
| Positive | 0.23 | 0.15 | 0.13 | |
| Severity perception of COVID-19 | Severe | |||
| Very severe | 0.014 | 0.069 | 0.84 | |
| Fairly severe | 0.13 | 0.14 | 0.34 | |
| Perceived efficacy of anti-pandemic measures | Effective | |||
| Excessive | 0.31 | 0.13 | 0.018∗ | |
| Not effective | −0.021 | 0.11 | 0.84 | |
| ICU beds per 100.000 population (COVID-19 patients) | 0.03 | 0.03 | 0.32 |
Significance codes: ∗< 0.05, ∗∗< 0.001.
Multiple R2 = 0.087, Adjusted R2 = 0.070.
N = 1109.
In reporting the statistics of categorical regressors, blank rows represent the references for comparisons.
4. Discussion
In the present study, we explored whether sleep-related variables were possibly associated with a change in lifestyle habits during the lockdown in Italy. Specifically, we considered human behaviours that may be negatively influenced by experiencing a chronic stress condition, resulting in a negative impact on health. We assumed that forced home confinement, combined with the uncertainty related to the pandemic spread all over the world, acted as a chronic stressor for the general population. Moreover, we hypothesized that sleep disruption, due to its crucial role in emotional regulation, might influence the propensity to adopt unhealthy lifestyles during the lockdown. Our results support the hypothesis that poor sleep quality is associated to the adoption of an unhealthy lifestyle. Also, in line with the literature, people with higher BMI and those who considered the measures implemented to face COVID-19 spread as excessive reported a shift towards unhealthier habits compared to the period before the lockdown. In parallel, participants who lived in Northern Italy adopted a healthier lifestyle as compared to participants who lived in Central Italy.
As COVID-19 spread and the related restrictive measures reshaped everyone's routine, we aimed, for the first time, at identifying individual characteristics that may lead to the adoption of unhealthy habits under this unprecedented stress condition. Indeed, the impact of the lockdown measures on psychological well-being has been highly heterogeneous, and it did not negatively affect mental health uniformly across different studies and populations [43]. This result is mirrored by available data on lifestyle habits during the first-wave lockdown. The average tobacco consumption, for example, is inconsistently reported as increased in the general population [44]: however, its growth was documented in the subpopulation of poor sleepers [24]. In parallel, food choices even improved in a sample of individuals with high food literacy [45], becoming instead particularly unhealthy in participants with a high BMI [30]. Regarding the Italian national context, our data on tobacco consumption (increased in 8% of the sample) are in line with those of Carreras et al. [24], who reported that 9% of Italians relapsed or started smoking, or increased smoking intensity. The same is true for alcoholic beverages consumption, which increased in the 12.8% of our sample and 10.1% of the sample of Scarmozzino et al. [28]. In the same study, it is also reported that 23.5% of Italian participants increased the consumption of salty and sweet snacks, similarly to our results on comfort food purchase (25.3% of participants increased). However, only 8.7% of Scarmozzino et al. sample decreased the consumption of fresh food as compared to the 17.9% of our study. Unlike ours, Scarmozzino et al. sample was mainly from Northern Italy: this could explain the discrepancies between the findings of the two studies in terms of fresh food consumption. It is in fact likely that residents of Northern Italy had easier access to food delivery systems. This point will be discussed later in this section.
We noticed that, in line with previous studies conducted in Italy during the lockdown [11,46], in our sample people slept worse as compared to reference values reported for the Italian population [33]. According to our results, poor sleepers are more prone to adopt an unhealthy lifestyle during the lockdown as compared to good sleepers. One possible explanation is that poor sleep quality might determine an emotional dysregulation [15], which in turn can engage people in following maladaptive coping strategies under stress condition [18]. The importance of a good sleep quality in granting adequate resilience levels during the first lockdown in Italy supports this hypothesis [47].
Conversely, increased consumption of caffeine, alcohol or nicotine have been associated with a worsening in sleep quality [48]. Based on the current results, it is not possible to draw definitive conclusions on the causal path that links poor sleep quality and unhealthy lifestyle. Nevertheless, we should not overlook the risk of a vicious circle where disturbed sleep leads to maladaptive coping and vice-versa, ultimately leading participants to poor psychic and physical health.
A second post-pandemic evaluation of sleep quality and habits in this sample would help shedding light on the relationship between sleep and lifestyle.
A higher Body Mass Index emerged as a significant predictor of an unhealthy lifestyle. This is in line with a previous study on Italian population during the lockdown [30], which yet only focused on eating habits. As suggested by the authors of another study on quarantine-related routine changes [49], a high BMI might be the result of habitual coping strategies that may be accountable for weight gain, such as drinking alcohol or eating high-calories comfort food.
Also, considering excessive the measures implemented by Italian government to fight the pandemic significantly predict a reduced lifestyle healthiness. Since the lockdown itself is a countermeasure for infection spread, we may conclude that participants who perceived quarantine as particularly stressful manifest the reduced tolerance to home confinement also by carrying out unhealthy coping strategies.
Finally, spending the lockdown in Northern Italy predicted a lower risk of adopting unhealthy behaviours as compared to living in Central Italy. These findings may appear counterintuitive, considered that Northern Italy was one of the epicentres of COVID-19 first wave [50]. Moreover, previous studies reported a poorer sleep quality in inhabitants of Northern Italy, as well as a higher psychological burden compared to inhabitants of other Italian regions [11]. Introducing the concept of “functional fear” might help interpret this result. “Functional fear” refers to negative emotions (i.e., fear and anxiety) that may motivate the avoidance of risky behaviours. This conceptual framework has been recently applied to COVID-19 pandemic, suggesting that, in some individuals, worry might have a beneficial impact on the adherence to the public health recommendations [51,52]. We can speculate that the fear of contracting COVID-19 has been highly prevalent in regions with a high number of infections, such as Northern Italy. We can also hypothesize that Northern Italy participants’ opting for a healthier lifestyle might also have been motivated by moderate levels of fear and anxiety secondary to local circulation of the virus. Future studies are needed to demonstrate an association between the adoption of COVID-19 prevention behaviours and healthier lifestyle.
Moreover, the different spatial distribution of the delivery systems on the Italian territory, might have make it easier for residents of Northern Italy to access services of general interest (such as fresh food home delivery).
The novelty of our study is twofold:
-
-
highlighting the relationship between sleep quality and global healthiness changes by gathering information on different lifestyle aspects at once;
-
-
identifying clusters of participants on which quarantine, as well as other potential chronic stressors, may impact most negatively.
Our results, indeed, suggest that poor sleepers could be those participants who paid the highest price for forced home confinement. If this pattern of reaction (i.e., increasing cigarettes and alcohol consumption, stop practicing physical exercise, etc.) would be systematically applied to every stressful condition, it could explain, at least partially, some of the negative consequences associated with poor sleep quality, such as cardiovascular diseases [53] or metabolic disorders [54,55].
This study has some important limitations that should be highlighted. The cross-sectional design makes it impossible to draw conclusions on causality. Moreover, results must be confirmed by studies involving objective (e.g., wrist actigraphy) and not only subjective sleep measures, although the use of self-report instruments is the only who could grant social distancing, allowing us to conduct a study without violating quarantine rules.
The limited predictive power of the model suggests that could be other predictors of the healthiness score not measured in the current study (e.g., the personal history of mental disorder, that may act as a risk factor for a worse response to stress conditions). However, sleep quality can be easily targeted by a preventive treatment which can reduce the impact on health of behavioural maladaptive coping strategies. Finally, some of the items used to explore health-related variables do not allow a direct estimate of participants’ likelihood of engaging in the behaviour of interest before the lockdown and during the lockdown. This might represent a limitation as no conclusion can be drawn in terms of magnitude of change.
5. Conclusion
During the lockdown in Italy, poor sleep quality was associated with the adoption of unhealthy lifestyles.
Sleep quality assessment might help identify people who could frequently react to stressful events by engaging in unhealthy behaviours. Large-scale interventions for good sleep quality promotion might contribute to better manage prolonged stressful situations, and ultimately improve people's health.
Public health interventions focused on the improvement of the well-being during COVID-19 pandemic, should also take into account lifestyle behavioural dimension, which can be negatively affected by stressful conditions, particularly in participants with poor sleep quality.
Credit author statement
Simone Bruno: Conceptualization, Methodology, Formal analysis, Writing – Original Draft, Writing – Review and Editing, Investigation.
Andrea Bazzani: Conceptualization, Methodology, Investigation, Writing – Review and Editing.
Sara Marantonio: Conceptualization, Methodology, Investigation, Writing – Original Draft, Writing – Review and Editing.
Francy Cruz-Sanabria: Formal Analysis, Writing – Review and Editing, Visualization.
Davide Benedetti: Formal analysis, Writing – Review and Editing, Visualization.
Paolo Frumento: Formal analysis, Writing – Review and Editing, Supervision.
Giuseppe Turchetti: Conceptualization, Methodology, Investigation, Writing – Review and Editing, Supervision.
Ugo Faraguna: Conceptualization, Methodology, Investigation, Writing – Review and Editing, Supervision.
Acknowledgement
The authors would like to thank Gianni Andreozzi, Emanuele Bombardini, Virginia Casigliani, Serena Ceccanti, Antonio Falco, Federico Ferri, Valentina Lorenzoni and Leopoldo Trieste for their support in survey design and data collection.
The present study was supported by a grant from the Arpa Foundation, Pisa, Italy (Sonnolab Grant to Ugo Faraguna); Italian Ministry of Health Grant RC2019 to U.F.
Footnotes
Ugo Faraguna is co-founder and president of sleepActa S.r.l, a spin-off company of the University of Pisa operating in the field of sleep medicine. All other authors declare no competing interest.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2022.01.002.
Appendix
In the Appendix, the English translation and the original Italian version of the questionnaire item exploring health-related variables are provided.
English translation
- 1) Before the lockdown, did you regularly take medicines to help you sleep?
- -No
- -Less than once a week
- -Once a week
- -More than once a week
- -Every day
- -More than once a day
- 2) How often do you take them now in a week?
- -I don't take them
- -Less than once a week
- -Once a week
- -More than once a week
- -Every day
- -More than once a day
- 3) Since the beginning of the lockdown, your consumption of alcoholic beverages is:
- -Decreased
- -Unchanged
- -Increased
- 4) Before the lockdown, how many cigarettes did you usually smoke per day?
- -I did not smoke
- -1–20 (multiple choice)
- -More than 20
- 5) Since the beginning of the lockdown, how many cigarettes do you smoke per day?
- -I do not smoke
- -1–20 (multiple choice)
- -More than 20
- 6) Before the lockdown, how many coffees did you usually drink per day?
- -I did not drink coffee usually
- -Less than once a day
- -1
- -2
- -3
- -4
- -5
- -More than 5
- 7) Since the beginning of the lockdown, how many coffees do you drink per day?
- -I do not drink coffee usually
- -Less than once a day
- -1
- -2
- -3
- -4
- -5
- -More than 5
- 8) Since the beginning of the lockdown, how often did you buy comfort food (e.g., pizza, chocolate, chips, candy)?
- -Less than before
- -As before
- -More than before
- 9) Compared to before the lockdown, how has your weekly purchase of fresh products (e.g., fruit and vegetables) changed?
- -Definitely decreased
- -Reduced
- -Unchanged
- -Increased
- -Definitively increased
- 10) Before the lockdown, did you regularly practice physical activity?
- -Yes
- -No
- 11) Since the beginning of the lockdown, do you regularly practice physical activity?
- -Yes
- -No
Original (Italian) version.
- 1) Prima del lockdown facevi uso di sostanze per facilitare il sonno?
- -No
- -Meno di una volta alla settimana
- -Una volta alla settimana
- -Più di una volta a settimana
- -Tutti i giorni
- -Più volte al giorno
- 2) Con quale frequenza le utilizzi adesso?
- -Non le utilizzo
- -Meno di una volta alla settimana
- -Una volta alla settimana
- -Più di una volta a settimana
- -Tutti i giorni
- -Più volte al giorno
- 3) Dall'inizio del lockdown, il tuo consumo di bevande alcoliche è:
- -Diminuito
- -Invariato
- -Aumentato
- 4) Abitualmente, quante sigarette fumavi al giorno prima del lockdown?
- -Non fumavo
- -1–20 (scelta multipla)
- -Più di 20
- 5) Quante sigarette fumi al giorno dall'inizio del lockdown?
- -Non fumo
- -1–20 (scelta multipla)
- -Più di 20
- 6) Abitualmente, quanti caffè bevevi al giorno prima del lockdown?
- -Non bevevo caffè abitualmente
- -Meno di uno al giorno
- -1
- -2
- -3
- -4
- -5
- -Più di 5
- 7) Quanti caffè bevi al giorno dall'inizio del lockdown?
- -Non bevo caffè abitualmente
- -Meno di uno al giorno
- -1
- -2
- -3
- -4
- -5
- -Più di 5
- 8) Dall'inizio del lockdown, quanto spesso hai acquistato generi di conforto (Es. pizza, cioccolata, patatine, dolciumi, ecc.)?
- -Meno di prima
- -Come prima
- -Più di prima
- 9) Rispetto a prima del lockdown, quanto acquisti settimanalmente prodotti freschi (es. frutta e verdura)?
- -Decisamente meno
- -Di meno
- -Come prima
- -Di più
- -Decisamente di più
- 10) Prima del lockdown, praticavi regolarmente attività fisica?
- -Sì
- -No
- 11) In questo periodo di lockdown, stai praticando regolarmente attività fisica?
- -Sì
- -No
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
References
- 1.WHO. Data as reported by: 20 January 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4 (accessed August 5, 2021).
- 2.WHO Director-General’s opening remarks at the media briefing on COVID-19. 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Google Scholar]
- 3.COVID-19/dati-regioni at master · pcm-dpc/COVID-19 · GitHub https://github.com/pcm-dpc/COVID-19/tree/master/dati-regioni (accessed August 5, 2021).
- 4.Decreto del Presidente del Consiglio dei Ministri 9 marzo 2020. https://www.gazzettaufficiale.it/eli/id/2020/03/09/20A01558/sg (accessed August 5, 2021).
- 5.Documento di Economia e Finanza sezione III: Programma Nazionale di Riforma, Ministero dell'Economia e delle Finanze, http://www.dt.mef.gov.it/modules/documenti_it/analisi_progammazione/documenti_programmatici/def_2020/DEF_2020_Programma_Nazionale_di_Riforma.pdf (accessed October 21, 2021).
- 6.Rapporto Annuale 2020: La situazione del Paese, ISTAT, https://www.istat.it/storage/rapporto-annuale/2020/Rapportoannuale2020.pdf (accessed October 21, 2021).
- 7.Bertrand L., Schröder C., Bourgin P., et al. Sleep and circadian rhythm characteristics in individuals from the general population during the French COVID-19 full lockdown. J Sleep Res. 2021 doi: 10.1111/JSR.13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franceschini C., Musetti A., Zenesini C., et al. Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy. Front Psychol. 2020;11:1–15. doi: 10.3389/fpsyg.2020.574475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jahrami H., BaHammam A.S., Bragazzi N.L., et al. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17 doi: 10.5664/JCSM.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altena E., Baglioni C., Espie C.A., et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020;29 doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 11.Casagrande M., Favieri F., Tambelli R., et al. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75 doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alvaro P.K., Roberts R.M., Harris J.K. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36 doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gualano M.R., lo Moro G., Voglino G., et al. Effects of COVID-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baglioni C., Nanovska S., Regen W., et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142:969–990. doi: 10.1037/bul0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palmer C.A., Alfano C.A. Sleep and emotion regulation: an organizing, integrative review. Sleep Med Rev. 2017;31 doi: 10.1016/j.smrv.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Avvenuti G., Bertelloni D., Lettieri G., et al. Emotion regulation failures are preceded by local increases in sleep-like activity. J Cognit Neurosci. 2021:1–15. doi: 10.1162/jocn_a_01753. [DOI] [PubMed] [Google Scholar]
- 17.Garbarino S., Nobili L. Springer; Milano: 2014. Lifestyle and habits. Sleepiness and human impact assessment; pp. 95–103. [DOI] [Google Scholar]
- 18.Kun B., Demetrovics Z. Emotional intelligence and addictions: a systematic review. Subst Use Misuse. 2010;45 doi: 10.3109/10826080903567855. [DOI] [PubMed] [Google Scholar]
- 19.Leventhal A.M., Zvolensky M.J. Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychol Bull. 2015;141 doi: 10.1037/bul0000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mattioli A.V., Bonatti S., Zennaro M., et al. The relationship between personality, socio-economic factors, acute life stress and the development, spontaneous conversion and recurrences of acute lone atrial fibrillation. Europace. 2005;7 doi: 10.1016/j.eupc.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 21.Leng G., Adan R.A.H., Belot M., et al. The determinants of food choice. Proc Nutr Soc. 2017;76 doi: 10.1017/S002966511600286X. [DOI] [PubMed] [Google Scholar]
- 22.Oliver G., Wardle J., Gibson E.L. Stress and food choice: a laboratory study. Psychosom Med. 2000;62 doi: 10.1097/00006842-200011000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Dallman M.F., Pecoraro N., Akana S.F., et al. vol. 100. ” Proceedings of the National Academy of Sciences of the United States of America; 2003. (Chronic stress and obesity: a new view of “comfort food). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carreras G., Lugo A., Stival C., et al. Impact of COVID-19 lockdown on smoking consumption in a large representative sample of Italian adults. Tobac Control. 2021;29 doi: 10.1136/tobaccocontrol-2020-056440. :tobaccocontrol-2020-056440. [DOI] [PubMed] [Google Scholar]
- 25.Luciano F., Cenacchi V., Vegro V., et al. COVID-19 lockdown: physical activity, sedentary behaviour and sleep in Italian medicine students. Eur J Sport Sci. 2021;21(10):1459–1468. doi: 10.1080/17461391.2020.1842910. [DOI] [PubMed] [Google Scholar]
- 26.Beck F., Léger D., Fressard L., et al. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J Sleep Res. 2021;30 doi: 10.1111/jsr.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scarmozzino F., Visioli F. Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. 2020;9 doi: 10.3390/foods9050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mitchell E.S., Yang Q., Behr H., et al. Adherence to healthy food choices during the COVID-19 pandemic in a U.S. population attempting to lose weight. Nutr Metabol Cardiovasc Dis. 2021;31 doi: 10.1016/j.numecd.2021.03.009. [DOI] [PubMed] [Google Scholar]
- 30.Maffoni S., Brazzo S., de Giuseppe R., et al. Lifestyle changes and body mass index during COVID-19 pandemic lockdown: an Italian online-survey. Nutrients. 2021;13 doi: 10.3390/nu13041117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peng E.Y.C., Lee M.B., Tsai S.T., et al. Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. J Formos Med Assoc. 2010;109:524–532. doi: 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buysse D.J., Reynolds C.F., Monk T.H., et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989;28 doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 33.Curcio G., Tempesta D., Scarlata S., et al. Validity of the Italian version of the Pittsburgh sleep quality index (PSQI) Neurol Sci. 2013;34 doi: 10.1007/s10072-012-1085-y. [DOI] [PubMed] [Google Scholar]
- 34.Adan A., Almirall H. Horne & Östberg morningness-eveningness questionnaire: a reduced scale. Pers Indiv Differ. 1991;12 doi: 10.1016/0191-8869(91)90110-W. [DOI] [Google Scholar]
- 35.Horne J.A., Ostberg O. A self assessment questionnaire to determine Morningness Eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 36.Natale V. Validazione di una scala ridotta di Mattutinità (rMEQ) = Validation of a reduced version of the Morningness-Eveningness Questionnaire (rMEQ) Giunti Organizzazioni Speciali. 1999:229. [Google Scholar]
- 37.Natale V., Esposito M.J., Martoni M., et al. Validity of the reduced version of the morningness-eveningness questionnaire. Sleep Biol Rhythm. 2006;4 doi: 10.1111/j.1479-8425.2006.00192.x. [DOI] [Google Scholar]
- 38.Roenneberg T., Wirz-Justice A., Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythm. 2003;18 doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- 39.Veronda A.C., Allison K.C., Crosby R.D., et al. Development, validation and reliability of the chrononutrition profile - questionnaire. Chronobiol Int. 2020;37 doi: 10.1080/07420528.2019.1692349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.ISTAT. Popolazione residente - bilacio: dati mensili http://dati.istat.it/Index.aspx?DataSetCode=DCIS_POPRES1 (accessed August 5, 2021).
- 41.Adan A., Natale V. Gender differences in morningness-eveningness preference. Chronobiol Int. 2002;19:709–720. doi: 10.1081/CBI-120005390. [DOI] [PubMed] [Google Scholar]
- 42.Cohen J. Elsevier; 1977. Statistical power analysis for the behavioral sciences. [DOI] [Google Scholar]
- 43.Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51 doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bommelé J., Hopman P., Walters B.H., et al. The double-edged relationship between COVID-19 stress and smoking: implications for smoking cessation. Tob Induc Dis. 2020;18 doi: 10.18332/TID/125580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Celorio-Sardà R., Comas-Basté O., Latorre-Moratalla M.L., et al. Effect of covid-19 lockdown on dietary habits and lifestyle of food science students and professionals from Spain. Nutrients. 2021;13 doi: 10.3390/nu13051494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cellini N., Conte F., de Rosa O., et al. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2021;77 doi: 10.1016/j.sleep.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bazzani A., Bruno S., Frumento P., et al. Sleep quality mediates the effect of chronotype on resilience in the time of COVID-19. Chronobiol Int. 2021:38. doi: 10.1080/07420528.2021.1895199. [DOI] [PubMed] [Google Scholar]
- 48.Hoefelmann L.P., Lopes A. da S., Silva KS da, et al. Lifestyle, self-reported morbidities, and poor sleep quality among Brazilian workers. Sleep Med. 2012;13 doi: 10.1016/j.sleep.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 49.Coulthard H., Sharps M., Cunliffe L., et al. Eating in the lockdown during the Covid 19 pandemic; self-reported changes in eating behaviour, and associations with BMI, eating style, coping and health anxiety. Appetite. 2021;161 doi: 10.1016/j.appet.2020.105082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Istituto Superiore di Sanità . 2020. Sorveglianza integrata Covid-19 in italia.https://www.epicentro.iss.it/coronavirus/bollettino/Infografica_29aprile%20ITA.pdf [Google Scholar]
- 51.Solymosi R., Jackson J., Pósch K., et al. Functional and dysfunctional fear of COVID-19: a classification scheme. Crime Science. 2021;10:1–23. doi: 10.1186/S40163-020-00137-2. 2021 10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harper C.A., Satchell L.P., Fido D., et al. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addiction. 2020 2020:1–14. doi: 10.1007/S11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hoevenaar-Blom M.P., Spijkerman A.M.W., Kromhout D., et al. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep. 2011;34 doi: 10.5665/sleep.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fatima Y., Doi S.A.R., Mamun A.A. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17 doi: 10.1111/obr.12444. [DOI] [PubMed] [Google Scholar]
- 55.Lee S.W.H., Ng K.Y., Chin W.K. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: a systematic review and meta-analysis. Sleep Med Rev. 2017;31:91–101. doi: 10.1016/j.smrv.2016.02.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1