Abstract
Introduction
Public health emergencies such as pandemics affect the health, safety, and well-being of both individuals and societies. Thus, this study aims to better understand the fear due to coronavirus disease (COVID) and associated levels of anxiety, depression, stress, and coping in the general public of India during the initial stage of the COVID-19 outbreak.
Materials and methods
This was a cross-sectional study to assess the psychological impact of COVID-19 and coping levels among the general population during the coronavirus pandemic’s initial phase. An online survey was conducted using a snowball sampling technique.
Results
A total of 489 people responded to the survey. The prevalence rates of depression, anxiety and stress were 27.2%, 21.5%, and 15.3% respectively. Female gender, age below 35 years, history of medical or psychiatric illness, and those who had personal contact with persons with COVID-19 were significantly associated with presence of depression, anxiety, and stress whereas spending more than 1 hour on COVID-19-related information was associated with significant stress.
Conclusion
This study concludes that the prevalence rates of psychological problems were high during the COVID-19 pandemic. These are directly related to the fear associated with COVID-19 but had an inverse relationship with the resilient coping levels.
Keywords: coronavirus, stress, depression, anxiety, fear, mental health, pandemic, covid-19
Introduction
Public health emergencies such as pandemics affect individuals’ and societies’ health, safety, and well-being. Hence, they affect not only physical health but also mental health intimately due to their unprecedented nature [1,2]. The World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak a global pandemic on March 11, 2020 [3]. The Indian government also acted swiftly, and the largest national lockdown in the world was imposed on 25th March for 21 days which was later extended to May 3, 2020, in response to the pandemic. Although the WHO praised this response as “tough and timely,”[4] the coronavirus itself has plunged the world into uncertainty and induced fear in the general public with people worrying about themselves or their loved ones contracting the virus. Mandatory contact tracing and restricted movement as a public health response also further contribute to the general population’s increased anxiety, guilt, and stigma [5].
Though lockdown is necessary to curb community spread and break the infection cycle, it can also affect people’s psychological health and generate much turmoil [6]. It is an unpleasant and unfamiliar experience with separation from loved ones, loneliness, loss of freedom, and boredom at times, causing a high prevalence of psychological symptoms of distress and disorder [7]. Previous research during the severe acute respiratory syndrome (SARS) epidemics has shown that poor coping mechanisms, a high degree of anxiety, pre-existing illness, and unverified information were risk factors in developing psychological problems [8,9].
In a recent meta-analysis, the prevalence rates of stress, anxiety, and depression due to the COVID-19 pandemic were 29.6, 31.9, and 33.7%, respectively, in the general population [10]. The prevalence rates of anxiety among the general population were also found to be more than three times higher during the COVID-19 pandemic compared to normal times [11]. Thus, this study aims to better understand the fear due to COVID and associated levels of anxiety, depression, stress, and coping in the general public of India during the initial stage of the COVID-19 outbreak.
Materials and methods
This was a cross-sectional study to assess the general public’s psychological response during the initial phase of the coronavirus pandemic, particularly the impact of lockdown and the beginning of the quarantine (April 12 to April 18, 2020). A snowball sampling technique was utilized to recruit the general public in India, and it was first distributed to college students through email and WhatsApp who were then asked to circulate it to others. The respondents completed the survey using an online survey platform (Google forms). Post-completion, participants with severe scores were advised to seek help along with listed mental health resources. Institutional ethics committee approval was obtained from Kamineni Hospitals on April 7, 2020 (Registration #: ECR/58/Inst/AP/2013/RR-19).
Sociodemographic details were collected such as age, sex, education, residential location, current living status, employment status, and medical/psychiatric illness. Respondents were also asked questions regarding time spent on coronavirus news (discussing/watching), source of information, contact history, and perceived risk of contracting the coronavirus.
The psychological impact of coronavirus was measured using the Depression, Anxiety, Stress Scale-21 (DASS-21), which is an easy-to-use instrument that has been used in research related to both COVID-19 as well as other infectious disease outbreaks multiple times [11-12]. The questionnaire was divided into three subscales: depression; anxiety; and stress. The total depression score was divided into normal (0-9), mild depression (10-13), moderate depression (14-20), severe depression (21-27), and extremely severe depression (28-42). The anxiety subscale score was divided into normal (0-7), mild anxiety (8-9), moderate anxiety (10-14), severe anxiety (15-19), and extremely severe anxiety (20-42). The stress subscale score was divided into normal (0-14), mild stress(15-18), moderate stress (19-25), severe stress (26-33), and extremely severe stress (34-42). This questionnaire has been provided in the Appendices Section.
The fear of coronavirus disease-19 scale (FCoV-19s) consists of seven items and measures the fear of coronavirus disease with each statement on a 5-point scale from 1-Strongly disagree to 5-Strongly agree with subjects rating their agreement [13].
Coping and resilience were assessed using the 4-item Brief Resilient Coping Scale (BRCS). The scale was divided into low-resilient copers (4-13), medium-resilient copers (14-16 points), and high-resilient copers (17-20) [8].
The data collected was analyzed using SPSS 23.0 version (SPSS Inc., Chicago, IL, USA). Descriptive statistics were calculated for sociodemographic data and the study population’s prevalence of depression, anxiety, and stress levels. The chi-square test was used to find the association for categorical variables, and correlation statistics were used for continuous variables to find the strength of association. A p-value of less than 0.05 was considered statistically significant.
Results
During the study, a total of 489 responses were collected from 21 states in India. The sociodemographic profile of the sample revealed that 51.3 % of the subjects were males while the age distribution of respondents for 18-24 years was 31.5%, 25-35 years was 39.9%, 36-45 years was 10%, 45-60 years was 12.7%, and >60 years was 5.9%. About 60.9% were from non-medical backgrounds, 49.9% were single, but 82.6% lived with the family during the lockdown period. The study found that 33.6% of the subjects worked as part of the essential COVID-19 services during the lockdown, and 42.5% reported working from home. The primary source of information regarding COVID-19 during lockdown was news and social media in 62.2 % and 14.7% of the sample, respectively. During the lockdown, 41.9% of the individuals reported spending more than 1 hour on average on COVID-19 discussion/news/statistics, with 6.7% spending more than 4 hours. About 44.4% of the subjects reported their perceived level of risk for contracting the COVID-19 as low; however, 47.3% were extremely concerned that a family member might contract the COVID-19.
The psychological impact was assessed by using the DASS-21. Table 1 shows the prevalence rates of depression, anxiety, and stress with the levels of severity. The prevalence of depression, anxiety, and stress was found to be 27.2%, 21.5%, and 15.3% respectively. A total of 8.2% were considered to suffer from mild depression, 9.8% from moderate depression, 3.9% from severe, and the remaining 5.3% from extremely severe depression. Of the total sample, 3.7% were considered to suffer from mild anxiety, 9.0% from moderate anxiety, 3.1% from severe, and 5.7% from extremely severe anxiety. About 4.7% were considered to suffer from mild stress, 3.7% from moderate stress, 7% from severe to extremely severe stress levels. Resilience and coping were measured through the BRCS. About 39.1% of the respondents were low resilient copers while 37.8% and 23.1%, respectively, were medium- and high-resilient copers as shown in Table 1.
Table 1. Prevalence of Depression, Anxiety, Stress, and Resilient Coping.
| Parameter | n (489) | % |
| Depression screening | ||
| Score ≤ 9 (Not depressed) | 356 | 72.8 |
| Mild (10-13) | 40 | 8.2 |
| Moderate (14-20) | 48 | 9.8 |
| Severe (21-28) | 19 | 3.9 |
| Extremely severe (>28) | 26 | 5.3 |
| Anxiety screening | ||
| Score ≤7 (Not anxious) | 384 | 78.5 |
| Mild (8-9) | 18 | 3.7 |
| Moderate (10-14) | 44 | 9.0 |
| Severe (15-19) | 15 | 3.1 |
| Extremely severe (>20) | 28 | 5.7 |
| Stress screening | ||
| Score ≤14 (Not stressed ) | 414 | 84.7 |
| Mild (15-18) | 23 | 4.7 |
| Moderate (19-25) | 18 | 3.7 |
| Severe (26-33) | 21 | 4.3 |
| Extremely severe (>34) | 13 | 2.7 |
| Coping | ||
| Low resilient (4-13) | 191 | 39.1 |
| Medium resilient (14-16) | 185 | 37.8 |
| High resilient (17-20) | 113 | 23.1 |
| (Total number of participants=489) | ||
Table 2 shows the association of depression, anxiety, and stress levels with various social and demographic factors. It was found that female gender, age less than 35 years, history of medical or psychiatric illness, and those who had personal contact with persons with COVID-19 were significantly associated with the presence of depression, anxiety, and stress levels. Being single was significantly associated with stress and depression, whereas substance use and spending more than 1 hour on COVID-19-related information/news was associated with significant stress.
Table 2. Association of Depression, Anxiety, and Stress as per DASS-21 in Relation To Various Sociodemographic Parameters.
DASS-21: Depression, Anxiety, Stress Scale-21
| Stress | Depression | Anxiety | ||||||||||||||
| Yes | No | p-value | Yes | No | p-value | Yes | No | p-value | ||||||||
| Gender | Male | 23 | 30.7% | 228 | 55.1% | <0.001 | 55 | 41.4% | 196 | 55.1% | 0.007 | 39 | 37.1% | 212 | 55.2% | <0.001 |
| Female | 52 | 69.3% | 186 | 44.9% | 78 | 58.6% | 160 | 44.9% | 66 | 62.9% | 172 | 44.8% | ||||
| Age | <35 years | 64 | 85.3% | 285 | 68.8% | 0.003 | 105 | 78.9% | 244 | 68.5% | 0.023 | 85 | 81.0% | 264 | 68.8% | 0.014 |
| 35 years and above | 11 | 14.7% | 129 | 31.2% | 28 | 21.1% | 112 | 31.5% | 20 | 19.0% | 120 | 31.3% | ||||
| Marital status | Single | 46 | 61.3% | 198 | 47.8% | 0.031 | 77 | 57.9% | 167 | 46.9% | 0.031 | 59 | 56.2% | 185 | 48.2% | 0.146 |
| Married | 29 | 38.7% | 216 | 52.2% | 56 | 42.1% | 189 | 53.1% | 46 | 43.8% | 199 | 51.8% | ||||
| Lockdown status | Living Alone—Solitary | 13 | 17.3% | 72 | 17.4% | 0.99 | 27 | 20.3% | 58 | 16.3% | 0.298 | 16 | 15.2% | 69 | 18.0% | 0.513 |
| Living with family/ Significant other | 62 | 82.7% | 342 | 82.6% | 106 | 79.7% | 298 | 83.7% | 89 | 84.8% | 315 | 82.0% | ||||
| work/study from home | Yes | 39 | 52.0% | 169 | 40.8% | 0.072 | 61 | 45.9% | 147 | 41.3% | 0.363 | 46 | 43.8% | 162 | 42.2% | 0.766 |
| No | 36 | 48.0% | 245 | 59.2% | 72 | 54.1% | 209 | 58.7% | 59 | 56.2% | 222 | 57.8% | ||||
| Essential services | Yes | 18 | 24.0% | 145 | 35.0% | 0.062 | 42 | 31.6% | 121 | 34.0% | 0.615 | 38 | 36.2% | 125 | 32.6% | 0.483 |
| No | 57 | 76.0% | 269 | 65.0% | 91 | 68.4% | 235 | 66.0% | 67 | 63.8% | 259 | 67.4% | ||||
| Past medical/psychiatric history | Yes | 28 | 37.3% | 56 | 13.5% | <0.001 | 45 | 33.8% | 39 | 11.0% | <0.001 | 32 | 30.5% | 52 | 13.5% | <0.001 |
| No | 47 | 62.7% | 358 | 86.5% | 88 | 66.2% | 317 | 89.0% | 73 | 69.5% | 332 | 86.5% | ||||
| Substance use | Yes | 20 | 26.7% | 72 | 17.4% | 0.059 | 28 | 21.1% | 64 | 18.0% | 0.439 | 26 | 24.8% | 66 | 17.2% | 0.078 |
| No | 55 | 73.3% | 342 | 82.6% | 105 | 78.9% | 292 | 82.0% | 79 | 75.2% | 318 | 82.8% | ||||
| Time spent | <1 hour | 35 | 46.7% | 249 | 60.1% | 0.03 | 70 | 52.6% | 214 | 60.1% | 0.136 | 55 | 52.4% | 229 | 59.6% | 0.182 |
| 1 hour and above | 40 | 53.3% | 165 | 39.9% | 63 | 47.4% | 142 | 39.9% | 50 | 47.6% | 155 | 40.4% | ||||
| Personal contact | Yes | 11 | 14.7% | 26 | 6.3% | 0.012 | 16 | 12.0% | 21 | 5.9% | 0.023 | 13 | 12.4% | 24 | 6.3% | 0.035 |
| No | 64 | 85.3% | 388 | 93.7% | 117 | 88.0% | 335 | 94.1% | 92 | 87.6% | 360 | 93.8% | ||||
| Perceived level of risk | Low | 35 | 46.7% | 182 | 44.0% | 0.173 | 53 | 39.8% | 164 | 46.1% | 0.358 | 41 | 39.0% | 176 | 45.8% | 0.463 |
| Medium | 29 | 38.7% | 132 | 31.9% | 50 | 37.6% | 111 | 31.2% | 38 | 36.2% | 123 | 32.0% | ||||
| High | 11 | 14.7% | 100 | 24.2% | 30 | 22.6% | 81 | 22.8% | 26 | 24.8% | 85 | 22.1% | ||||
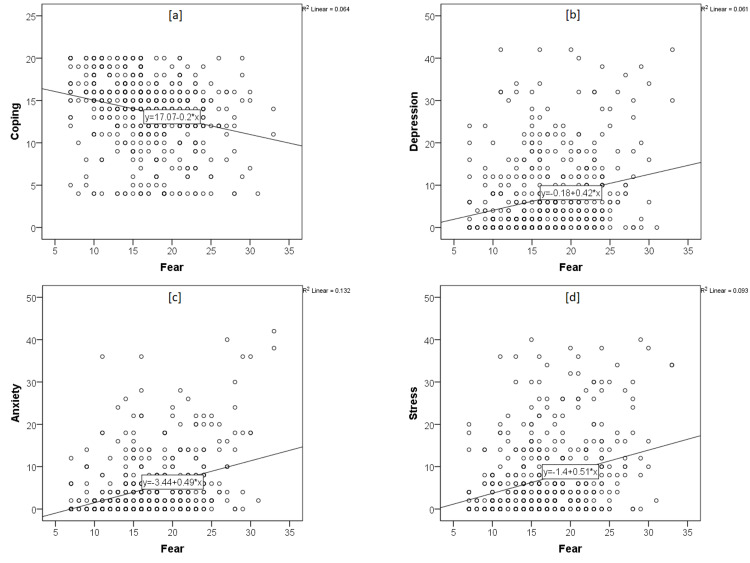
The scatter plot (Figure 1) shows the correlation statistics, and there was a positive correlation between scores of FCoV-19s and the scores of DASS-21 subscales of anxiety (r=0.364, p<0.01), depression (r=0.247, p<0.01), and stress(r=0.306, p<0.01). Meanwhile, the scores of BCRS had a negative correlation with scores of FCoV-19s (r=−0.253, p<0.01), as well as depression (r=−0.107, p<0.05), anxiety (r=−0.102, p<0.05), and stress (r=−0.91, p<0.05) subscales of DASS-21. There was also a significant positive correlation between depression and anxiety (r=−0.773, p<0.01) and stress subscale scores (r=0.859, p<0.01) (Table 3).
Table 3. Pearson’s Correlation of the Fear, Coping, and DASS-21.
**Correlation is significant at 0.01 level (two-tailed).
*Correlation is significant at 0.05 level (two-tailed).
| Fear | Coping | Depression | Anxiety | Stress | |
| Coping | -0.253** | 1 | -0.107* | -0.102* | -0.091* |
Figure 1. The scatter plots of correlation statistics between DASS-21, FCoV-19S, and BRCS scores.
DASS: Depression, Anxiety, Stress Scale; FCoV-19: Fear of COVID-19 Scale; BRCS: Brief Resilient Coping Scale
Discussion
Our research findings are consistent with other studies in the literature showing that COVID-19 has a significant impact on mental health. The prevalence of depression, anxiety, and stress was 27.2%, 21.5%, and 15.3%, respectively, and this is almost similar but relatively low compared to a recent meta-analysis by Salari et al. (2020) and a cross-sectional survey by Turna et al. (2021) of 632 individuals [10,14]. The prevalence rates of anxiety, depression, and stress levels during the COVID-19 pandemic in the general population sample of other countries also showed similar rates [15-19].
The female gender was significantly associated with stress, depression, and anxiety (p<0.05). This is similar to studies worldwide where gender differences have been noted with an increased biological sensitivity of women to stress [18,20,21]. Moreover, most women faced the responsibility of being the family’s main caregiver with the added burden of child-rearing, domestic work without additional help during the lockdown, making them more vulnerable to higher levels of anxiety and depression [17]. The higher FCoV-19s scores in females than males in the current study might have contributed to the high psychological impact of COVID-19 in females.
Age less than 35 years was also significantly associated with stress, anxiety, and depression consistent with previous studies. This could be attributed to a multitude of reasons, including uncertainty regarding future and career, boredom and frustration due to lockdown, and increased exposure to social media during the pandemic. Additional history of previous medical and psychiatric illness was also significantly associated with stress, anxiety, and depression. This echoes current literature and has been explained by the possibility that those with pre-existing conditions are at increased risk for psychological distress [16,22,23]. Moreover, these individuals also seem to evaluate themselves as more vulnerable to any new infections [21]. Those employed in essential services had lower DASS item scores than the rest of the study population. One possible explanation could be the absolute necessity and utility of their services to maintain health and welfare, leading to quick adaptation to the pandemic. Moreover, feeling useful and being occupied with work may also distract from pandemic-related negative thoughts and worries. This is also explained by the significantly higher mean scores of resilient coping in people working in essential services than non-essential services. Interestingly, lockdown status and working from home independently did not have any bearing on the DASS items scores. In the current study, married people had significantly lower scores of stress and depression, suggesting that marriage might act as a buffer and additional support to help combat stress.
The finding that the time spent over information about COVID-19 for more than 1 hour was associated with significant stress, anxiety, and depression is consistent with previous studies [17,18] as the excess time spent results in excess and/or repetitive exposure to misinformation and online health or COVID-19-related health search. Increased usage of online searches for medical information and the ensuing anxiety known as cyberchondria is considered as an independent risk factor for increased anxiety levels in the setting of COVID-19 [24-26].
The mean score of FCoV-19s was 16.8 (SD=5.27), which was slightly lower than other studies such as Doshi et al.’s [20] and another study by Giordani et al. [27], which reported 18.00 (SD=5.68) and 19.8 (SD=5.3), respectively. The lower score could be attributed to the difference in the pandemic stages, with India still in its initial phase. There was a significant positive correlation between depression and anxiety (ρ=−0.773, p<0.01) and stress (ρ=0.859, p<0.01). This could be due to similar pathophysiology and similarity of the items in the questionnaire. Furthermore, both anxiety and depression are often comorbid and interrelated to ongoing stress levels and the degree of strength of the stressor.
Finally, our results indicated that higher coping and resilience scores were associated with reduced FCoV-19s and DASS scale scores. This finding helps corroborate existing literature’s evidence that coping plays a vital role in protecting and improving mental health in individuals facing health-related stress [28-30]. However, only 23.1% of our population met the criteria for high resilience copers. In comparison, 39.1 % and 37.8 had low- and medium-resilient coping, resulting in relatively higher rates of stress, anxiety, and depression in the current study.
There were limitations to the study. First, the study was conducted online and was a cross-sectional study. The small sample size and snowball sampling technique employed meant that the sample size could not be generalized to the general population and there was a risk of low external validity. The psychiatric diagnosis was based on screening instruments rather than a clinical diagnostic interview. Unfortunately, due to the study design, retesting and follow-up are not possible. A longitudinal study is warranted to understand the long-term effects of the pandemic.
Conclusions
Our findings suggest that the COVID-19 pandemic and ensuing lockdown have led to a significant increase in psychological problems in the Indian general population. The Indian population must be granted access to timely mental health care, including psychotherapy and medication. Moreover, the research suggests that most of the study population has inadequate (low to medium) coping skills; hence, it is essential that we implement community-based strategies focusing on enhancing coping and caretaking behaviors to increase resilience. Proper implementation and access to telepsychiatry, an underutilized tool, can help individuals avail mental health services without the fear associated with in-person consultation during this COVID-19 crisis.
Appendices
Table 4. Semi-structured Questionnaire: DASS-21, FCOV 19, and BRCS scales used for the study.
BRCS- Brief Resilient Coping Scale8
DASS-21 - Depression and Anxiety Stress Scale12
FCoV 19- Fear of COVID 19 Scale13
| Q. No | Item | Response ✓ | |||||||||||
| 1 | Gender | Male | |||||||||||
| Female | |||||||||||||
| 2 | Age | 18-24 years | |||||||||||
| 25-35 years | |||||||||||||
| 36-45 years | |||||||||||||
| 46-60 years | |||||||||||||
| >60 years | |||||||||||||
| 3 | City (Residence at present) | ||||||||||||
| 4 | Education | ||||||||||||
| 5 | Marital status | Single | |||||||||||
| Married | |||||||||||||
| Widow/Widower | |||||||||||||
| 6 | What is your current living status in this period of lockdown? | Living alone | |||||||||||
| Living with significant other | |||||||||||||
| 7 | Profession | ||||||||||||
| 8 | Are you working at present in any of the following essential COVID-19 services? | Healthcare | |||||||||||
| Police | |||||||||||||
| Sanitization services | |||||||||||||
| Government public administrative services | |||||||||||||
| Banking, electricity, postal department | |||||||||||||
| Other | |||||||||||||
| No, not working | |||||||||||||
| 9 | Do you need to work from home or attend classes online (students) during lockdown period? | Yes | |||||||||||
| No | |||||||||||||
| 10 | Medical Illness/Psychiatric illness? If yes, specify | Yes | |||||||||||
| No | |||||||||||||
| Specify, if yes | |||||||||||||
| 11 | Do you use/ consume alcohol/tobacco/cannabis? | Yes | |||||||||||
| No | |||||||||||||
| 12 | What is your source of information regarding COVID-19? | News | |||||||||||
| Social media | |||||||||||||
| Journals/publications | |||||||||||||
| Friends/relatives/neighbors | |||||||||||||
| Healthcare professionals | |||||||||||||
| Other | |||||||||||||
| 13 | How much time do you spend on average on coronavirus news/statistics? (Watching/Reading/Forwarding/Discussing) | <1 hour | |||||||||||
| 1-3 hours | |||||||||||||
| 4-7 hours | |||||||||||||
| > 7 hours | |||||||||||||
| 14 | Do you personally know anyone who has been infected by the coronavirus? | Yes | |||||||||||
| No | |||||||||||||
| 15 | How do you rate your level of risk for contracting (catching) the coronavirus (COVID-19)? | High | |||||||||||
| Medium | |||||||||||||
| Low | |||||||||||||
| 16 | How concerned are you that a family member will contract the coronavirus ? | Extremely concerned | |||||||||||
| Somewhat concerned | |||||||||||||
| Not concerned at all | |||||||||||||
| Rate your agreement from (1)- Strongly disagree to (5) -Strongly agree | |||||||||||||
| 17 | I am most afraid of COVID-19 | 1 | 2 | 3 | 4 | 5 | |||||||
| 18 | It makes me uncomfortable to think about COVID-19 | 1 | 2 | 3 | 4 | 5 | |||||||
| 19 | My hands become clammy when I think about COVID-19 | 1 | 2 | 3 | 4 | 5 | |||||||
| 20 | I am afraid of losing my life because of COVID-19 | 1 | 2 | 3 | 4 | 5 | |||||||
| 21 | When watching news and stories about COVID-19 on social media, I become nervous or anxious | 1 | 2 | 3 | 4 | 5 | |||||||
| 22 | I cannot sleep because I'm worrying about getting COVID-19 | 1 | 2 | 3 | 4 | 5 | |||||||
| 23 | My heart races or palpitates when I think about getting COVID-19 | 1 | 2 | 3 | 4 | 5 | |||||||
| Rate your agreement from (0)- Did not apply to me at all, (1)- Applied to me to some degree, (2)- Applied to me to a considerable degree, (3)- Applied to me very much | |||||||||||||
| 24 | I found it hard to wind down | 0 | 1 | 2 | 3 | ||||||||
| 25 | I was aware of dryness of mouth | 0 | 1 | 2 | 3 | ||||||||
| 26 | I couldn't seem to experience any positive feeling at all | 0 | 1 | 2 | 3 | ||||||||
| 27 | I experienced breathing difficulty (especially rapid breathing, breathlessness in the absence of physical exertion) | 0 | 1 | 2 | 3 | ||||||||
| 28 | I found it difficult to work up the initiative to do things | 0 | 1 | 2 | 3 | ||||||||
| 29 | I tended to over-react to situations | 0 | 1 | 2 | 3 | ||||||||
| 30 | I experienced trembling (e.g., in the hands) | 0 | 1 | 2 | 3 | ||||||||
| 31 | I was worried about situations in which I might panic and make a fool of myself | 0 | 1 | 2 | 3 | ||||||||
| 32 | I felt that I was using a lot of nervous energy | 0 | 1 | 2 | 3 | ||||||||
| 33 | I felt that I had nothing to look forward to | 0 | 1 | 2 | 3 | ||||||||
| 34 | I found myself getting agitated | 0 | 1 | 2 | 3 | ||||||||
| 35 | I found it difficult to relax | 0 | 1 | 2 | 3 | ||||||||
| 36 | I felt down-hearted and blue | 0 | 1 | 2 | 3 | ||||||||
| 37 | I felt intolerant of anything that kept me from getting on with what I was doing | 0 | 1 | 2 | 3 | ||||||||
| 38 | I felt I was close to panic | 0 | 1 | 2 | 3 | ||||||||
| 39 | I was unable to become enthusiastic about anything | 0 | 1 | 2 | 3 | ||||||||
| 40 | I felt I wasn't worth much as a person | 0 | 1 | 2 | 3 | ||||||||
| 41 | I felt that I was rather touchy | 0 | 1 | 2 | 3 | ||||||||
| 42 | I was aware of the action of my heart in the absence of physical exertion (sense of heart rate increase, heart missing a beat) | 0 | 1 | 2 | 3 | ||||||||
| 43 | I felt scared without any good reason | 0 | 1 | 2 | 3 | ||||||||
| 44 | I felt that life was meaningless | 0 | 1 | 2 | 3 | ||||||||
| Rate your agreement from (1)-Does not describe me, (2)- Does not describe me, (3)- Neutral, (4)- Describes me, (5)- Describes me very well. | |||||||||||||
| 45 | I look for creative ways to alter difficult situations | 1 | 2 | 3 | 4 | 5 | |||||||
| 46 | Regardless of what happens to me, I believe I can control my reaction to it | 1 | 2 | 3 | 4 | 5 | |||||||
| 47 | I believe I can grow in positive ways by dealing with difficult situations | 1 | 2 | 3 | 4 | 5 | |||||||
| 48 | I actively look for ways to replace the losses I encounter in life | 1 | 2 | 3 | 4 | 5 | |||||||
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Kamineni Hospitals issued approval ECR/58/Inst/AP/2013/RR-19
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.COVID-19 and lockdown: a study on the impact on mental health. Kazmi SSH, Hasan DK, Talib S, et al. https://ssrn.com/abstract=3577515 Social Science Research Network. 2020 [Google Scholar]
- 2.COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. Elhai JD, Yang H, McKay D, Asmundson GJ. J Affect Disord. 2020;274:576–582. doi: 10.1016/j.jad.2020.05.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO declares COVID-19 a pandemic. Cucinotta D, Vanelli M. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.India under COVID-19 lockdown. The Lancet. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30938-7/fulltext. Lancet. 2020;395:1315. doi: 10.1016/S0140-6736(20)30938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Ng CH. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.COVID 19: Impact of lock-down on mental health and tips to overcome. Hiremath P, Suhas Kowshik CS, Manjunath M, Shettar M. Asian J Psychiatr. 2020;51:102088. doi: 10.1016/j.ajp.2020.102088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rapid review the psychological impact of quarantine and how to reduce it: rapid review of the evidence. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(20)30460-8.pdf. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The development and psychometric evaluation of the Brief Resilient Coping Scale. Sinclair VG, Wallston KA. Assessment. 2004;11:94–101. doi: 10.1177/1073191103258144. [DOI] [PubMed] [Google Scholar]
- 9.Consuming information related to COVID-19 on social media among older adults and its association with anxiety, social trust in information, and COVID-safe behaviors: cross-sectional telephone survey. Wong FH, Liu T, Leung DK, et al. J Med Internet Res. 2021;23:0. doi: 10.2196/26570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Salari N, Hosseinian-Far A, Jalali R, et al. Global Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prevalence of anxiety in the COVID-19 pandemic: an updated meta-analysis of community-based studies. Santabárbara J, Lasheras I, Lipnicki DM, et al. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110207. doi: 10.1016/j.pnpbp.2020.110207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lovibond SH, Lovibond PF. Sydney N.S.W.: Psychology Foundation of Australia. Sydney: Psychology Foundation of Australia; 1995. Manual for the Depression Anxiety Stress Scales (2nd Ed.) [Google Scholar]
- 13.The fear of COVID-19 scale: development and initial validation. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anxiety, depression and stress during the COVID-19 pandemic: results from a cross-sectional survey. Turna J, Zhang J, Lamberti N, et al. J Psychiatr Res. 2021;137:96–103. doi: 10.1016/j.jpsychires.2021.02.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Dawel A, Shou Y, Smithson M, et al. Front Psychiatry. 2020;11:1–8. doi: 10.3389/fpsyt.2020.579985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. Compr Psychiatry. 2020;102:152192. doi: 10.1016/j.comppsych.2020.152192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Front Psychol. 2020;11:1–23. doi: 10.3389/fpsyg.2020.01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Psychological impacts of the COVID-19 pandemic on the public in Egypt. Arafa A, Mohamed A, Saleh L, Senosy S. Community Ment Health J. 2021;57:64–69. doi: 10.1007/s10597-020-00701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Depression and anxiety in Hong Kong during COVID-19. Choi EP, Hui BP, Wan EY. https://doi.org/10.3390/ijerph17103740. Int J Environ Res Public Health. 2020;17:3740. doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Assessing coronavirus fear in Indian population using the fear of COVID-19 scale. Doshi D, Karunakar P, Sukhabogi JR, Prasanna JS, Mahajan SV. Int J Ment Health Addict. 2021;19:2383–2391. doi: 10.1007/s11469-020-00332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, Roma P. https://doi.org/10.3390/ijerph17093165. Int J Environ Res Public Health. 2020;17:3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reported symptoms before and one year after hysterectomy in African American and white women. Moorman PG, Schildkraut JM, Myers ER, Wang F. https://doi.org/10.1089/jwh.2010.2543. J Women's Health. 2011;20:1035–1042. doi: 10.1089/jwh.2010.2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anxious temperament and cyberchondria as mediated by fear of COVID-19 infection: a cross-sectional study. Oniszczenko W. https://doi.org/10.1371/journal.pone.0255750. PLoS ONE. 2021;16:0. doi: 10.1371/journal.pone.0255750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The mediating effect of the cyberchondria and anxiety sensitivity in the association between problematic internet use, metacognition beliefs, and fear of COVID-19 among Iranian online population. Seyed Hashemi SG, Hosseinnezhad S, Dini S, Griffiths MD, Lin CY, Pakpour AH. Heliyon. 2020;6:0. doi: 10.1016/j.heliyon.2020.e05135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cyberchondria in the age of COVID-19. Jokic-Begic N, Lauri Korajlija A, Mikac U. https://doi.org/10.1371/journal.pone.0243704. PLoS ONE. 2020;15:0. doi: 10.1371/journal.pone.0243704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fear of COVID-19 scale: assessing fear of the coronavirus pandemic in Brazil. Giordani RC, Zanoni da Silva M, Muhl C, Giolo SR. J Health Psychol. 2020:1–12. doi: 10.1177/1359105320982035. [DOI] [PubMed] [Google Scholar]
- 28.Coping with diabetes in adulthood: a meta-analysis. Duangdao KM, Roesch SC. https://doi.org/10.1007/s10865-008-9155-6. J Behav Med. 2008;31:291–300. doi: 10.1007/s10865-008-9155-6. [DOI] [PubMed] [Google Scholar]
- 29.Coping with prostate cancer: a meta-analytic review. Roesch SC, Adams L, Hines A, et al. https://doi.org/10.1007/s10865-005-4664-z. J Behav Med. 2005;28:281–293. doi: 10.1007/s10865-005-4664-z. [DOI] [PubMed] [Google Scholar]
- 30.Coping and adjustment in children with cancer: a meta-analytic study. Aldridge AA, Roesch SC. https://doi.org/10.1007/s10865-006-9087-y. J Behav Med. 2007;30:115–129. doi: 10.1007/s10865-006-9087-y. [DOI] [PubMed] [Google Scholar]