Abstract
Interventional therapy, which can prolong the survival of patients with liver cancer (LC), is an important means to treat the disease. During interventional therapy for LC, it is essential to make a targeted and detailed nursing plan to ameliorate the prognosis. The purpose of this study was to determine the application significance of personalized nursing in patients undergoing interventional therapy for LC. We retrospectively analyzed 136 patients with LC undergoing interventional therapy. Among them, 70 cases receiving personalized nursing were assigned to the observation group (OG), and the remaining 66 cases receiving routine nursing were the control group (CG). After nursing, sleep time of patients in the OG was significantly longer than that in CG. In addition, time to ambulation and hospital stay were shorter in the OG than in the CG. Furthermore, the OG exhibited significantly lower scores of visual analogue scale (VAS) and self-rating anxiety scale (SAS), as well as significantly reduced incidence of adverse reactions than the CG. Compared with the CG, the levels of serum alanine aminotransferase (AST), aspartate aminotransferase (ALT), and total bilirubin (TBIL) were significantly lower in the OG after nursing, while the level of albumin (ALB) was significantly increased. Moreover, patients in the OG showed significantly higher nursing satisfaction and quality of life scores than those in the CG. Therefore, personalized nursing has good prospects for usein interventional therapy for LC.
Keywords: Liver cancer, interventional therapy, personalized nursing, quality of life
Introduction
Liver cancer (LC), also known as hepatocellular carcinoma, is one of the main malignancies causing cancer death [1]. The early clinical presentations of LC are not obvious and non-specific, which results in most patients being diagnosed at middle and late stages [2]. Currently, surgical resection and liver transplantation are the mainstays of treatment for patients with early-stage LC, while interventional therapy is the main palliative treatment for those with advanced disease [3]. Interventional therapy for LC has been extensively applied in the clinic. It is minimally invasive, safe and has a low risk of complications, so it can prolong the overall survival of patients [4]. However, after treatment, patients often experience a series of adverse reactions such as nausea and vomiting, pain, and dysuria [5]. So, giving targeted nursing intervention to patients with LC undergoing interventional therapy is necessary.
The clinical routine nursing intervention lacks pertinence and overall planning, which leads to unsatisfactory clinical efficacy [6]; hence, it is not effective in reducing the incidence of adverse reactions and relieving pain of patients in cancer treatment [7]. Personalized nursing, on the other hand, is a targeted and patient-centered nursing model that combines the individual differences and nursing needs of patients according to the principles of nursing [8]. During the implementation of personalized nursing, corresponding adjustments can be made according to the actual situation to provide interactive and scientific nursing intervention for patients [9]. It has been previously reported that nurses who actively combined patient preferences with scientific and practical evidence succeeded in raising patients’ expectations and making informed decisions in personalized care [10]. Welch-Coltrane showed that by developing a personalized nursing plan for sickle cell disease patients, the hospitalization time was reduced by 1.23 days, the 7-day readmission rate by 34%, and the use of intravenous hydromorphone by 25%, thus reducing the economic burden on patients [11]. According to Tekin, it is very important to provide personalized care for patients undergoing orthopedic surgery to improve their satisfaction with nursing, and nurses should realize the importance of personalized care in clinical practice [12]. Thus, personalized nursing has a positive effect on patients in clinical practice.
At present, there is no research on the application of personalized nursing in interventional therapy of LC. Accordingly, this study, through the implementation of personalized care for LC patients undergoing interventional therapy, aimed to study the effect of this nursing model in patients with LC.
Materials and methods
The internal Medical Ethics Committee approved this research, and all the study participants were thoroughly informed and provided a written informed consent prior to enrollment. This retrospective analysis included 136 patients with LC who received interventional therapy in our hospital from September 2018 to March 2020. Inclusion criteria: all the enrolled patients met the diagnostic criteria of LC [13] and received interventional therapy in the Shanxi Provincial People’s Hospital, with complete case data and life expectancy >3 months. Exclusion criteria: patients with other malignant tumors, heart, kidney and other vital organ disorders or mental disorders were excluded.
Nursing methods
Sixty-six patients receiving routine nursing intervention were assigned into the control group (CG), and 70 patients receiving personalized nursing intervention were included into the observation group (OG).
Routine nursing
During treatment, the nursing staff closely monitored the vital signs of patients and immediately reported the abnormalities to the attending physician. In addition, medication was given to patients in strict accordance with the doctor’s orders, and adverse reactions were observed after medication.
Personalized nursing
Establishment of a dedicated nursing team: An experienced nurse was appointed as the leader of the nursing team, and a WeChat working group was established to send the patients’ medical records to the team members to formulate specific nursing measures.
Psychological care
Patients were provided with clean, sanitary and well-ventilated wards during nursing. The nursing staff maintained good communication with the patients and their families, created a relaxed and happy atmosphere for patients and build a harmonious and mutual trusting nurse-patient relationship. Advanced information about the interventional therapy was explained to patients and their families, so that patients could know their condition and face it with a optimistic attitude.
Intraoperative and postoperative care
The humidity and temperature of the operating room were adjusted preoperatively. The patient was comforted when wheeled to the operating room, and all vital signs were closely watched during surgery. Postoperatively, patients were told to stay in bed and reduce unnecessary visits. Within 2 h after surgery, the patient was closely observed to see if there was oozing blood, redness, swelling or exudation at the venipuncture site.
Dietary care
After surgery, patients were given liquid food, with less high sugar and high-lipid food as well as less gas-producing food such as soy products and milk; while spicy, fried, barbecued and other irritating food was strictly prohibited. When patients got better, they were allowed to eat semi-liquid food such as tofu, mince meat, and thick porridge. The amount of food was kept appropriate so that patients did not feel any abdominal distension.
Pain care
Patients’ attention was channeled by soothing music or mitigated by sedatives and analgesics if the pain was severe. In case of physiological pain, the patient was instructed to massage the temple with the thumb and fingertips in a spiral way for 5 min/time. During the massage, the patient’s complexion was observed and the patient was asked whether there was any discomfort. In addition, patients were instructed to do proper deep breathing exercises, and to contract and relax the muscles of the upper and lower limbs.
Post-discharge nursing guidance
After discharge, patients were provided with life guidance such as diet and activities through WeChat and telephone. In addition, another dedicated WeChat group was established, with doctors regularly answering questions online to understand the needs of patients and answer questions from patients and their families.
Outcome measures
(1) Clinical indicators were observed, including sleep time, ambulation time, and length of hospital stay. Before and after nursing (before discharge), liver function indexes such as aspartate aminotransferase (AST, Cat. No. E-BC-K235-M), alanine aminotransferase (ALT, Cat. No. E-BC-K236-M), albumin (ALB, Cat. No. E-BC-K057-M) and total bilirubin (TBIL, Cat. No. E-BC-K760-M) were detected using the colorimetric method, with kits all purchased from Elabscience Biotechnology Co., Ltd., Wuhan, China. Adverse reactions during care were recorded.
(2) Visual analogue scale (VAS) [14] was used to assess patients’ degree of pain at 12 h and 48 h after surgery, with scores ranging from 0 (painless) to 10 points (unbearable pain). The complexion of patients was scored according to the scoring scale, and scoring was in proportion to the severity of the pain. The anxiety of patients was evaluated using the self-rating anxiety scale (SAS) before and after nursing (before discharge) [15]. There are 20 questions in the scale, each scores 1-4 points, with a cut-off of 50 points. The score is proportional to the anxiety level of the patient.
(3) A self-made nursing satisfaction questionnaire [16] was utilized to investigate patients’ satisfaction with the nursing work, with a score <50 indicating unsatisfied, 50-69 indicating fair, 70-89 indicating satisfied, and ≥90 indicating very satisfied. Satisfaction rate = (satisfied + very satisfied) cases/total cases ×100%.
(4) Patients’ quality of life (QoL) before and after nursing (1 month after discharge) was evaluated using the European Organization for Research and Treatment of Cancer QOL Core Questionnaire 30 (EORTC QLQ-30) [17] from the following five domains: physical function, cognitive function, role function, emotional function, and social function. The higher the score, the better the QoL.
Statistical methods
GraphPad 6.0 and SPSS 17.0 were used for data analysis. Categorical variables were expressed as cases/percentage [n (%)] and analyzed using χ2 test; Continuous variables were recorded as mean ± SD, and the difference between two groups were analyzed using t test while that within the group before and after nursing by paired t test. P<0.05 indicated that a difference was statistically significant.
Results
Patient clinical data
We collected the clinical data of all the participants (Table 1). The statistical analysis revealed no evident difference in clinical data such as gender, age, disease type, course of disease, tumor diameter, intraoperative blood loss, operation time, hepatic portal occlusion time, and marital status between the two groups (P>0.05).
Table 1.
Clinical data of patients in the control group and observation group
| Classification | Control group (n=66) | Observation group (n=70) | t/χ2 | P |
|---|---|---|---|---|
| Gender | 0.666 | 0.414 | ||
| Female | 51 (77.27) | 58 (82.86) | ||
| Male | 15 (22.73) | 12 (17.14) | ||
| Age (years) | 48.91±3.89 | 48.36±5.63 | 0.661 | 0.510 |
| Disease type | 0.708 | 0.400 | ||
| Primary liver cancer | 53 (80.30) | 60 (85.71) | ||
| Secondary liver cancer | 13 (19.70) | 10 (14.29) | ||
| Course of disease (year) | 2.09±0.38 | 2.16±0.26 | 1.235 | 0.219 |
| Tumor diameter (cm) | 5.91±1.85 | 6.04±1.90 | 0.415 | 0.679 |
| Intraoperative blood loss (mL) | 323.86±62.97 | 330.86±46.08 | 0.742 | 0.459 |
| Operation time (min) | 127.45±29.41 | 132.20±36.88 | 0.827 | 0.410 |
| Occlusion time of hepatic portal (min) | 20.31±6.26 | 19.47±6.84 | 0.217 | 0.829 |
| Marital status | 0.365 | 0.546 | ||
| Married | 58 (87.88) | 59 (84.29) | ||
| Single or widowed | 8 (12.12) | 11 (15.71) | ||
| Education level | 0.555 | 0.456 | ||
| College and below | 40 (60.61) | 38 (54.29) | ||
| Bachelor degree or above | 26 (39.39) | 32 (45.71) | ||
| Provider payments | 0.064 | 0.800 | ||
| Self-paying | 4 (6.06) | 5 (7.14) | ||
| Insurance | 62 (93.94) | 65 (92.86) |
Clinical indicators in the two groups
We observed the clinical indicators in the two groups. As shown in Table 2, after the implementation of personalized nursing, the sleep time of patients in the OG was significantly longer than that in the CG, and the time to ambulation and hospital stay were shorter than those in the CG (P<0.05).
Table 2.
Clinical indicators in the control group and observation group
| Clinical indicators | Control group (n=66) | Observation group (n=70) | t | P |
|---|---|---|---|---|
| Sleep time (h) | 6.05±0.43 | 7.36±0.39 | 18.630 | <0.001 |
| Early ambulation (h) | 50.75±18.02 | 40.88±11.54 | 3.827 | <0.001 |
| Hospital stay (d) | 8.37±1.53 | 6.84±1.29 | 6.318 | <0.001 |
Pain score and anxiety degree in two groups
There was no significant difference in the VAS score between the two groups at 12 h postoperatively (Figure 1A) (P>0.05); 48 h after surgery, the VAS score decreased obviously in both groups, and the score in the OG was significantly lower than that in the CG (P<0.05). The SAS (Figure 1B) score differed insignificantly between CG and OG before nursing (P>0.05), but was reduced in both groups after nursing, with a lower level in the OG compared with the CG (P<0.05).
Figure 1.
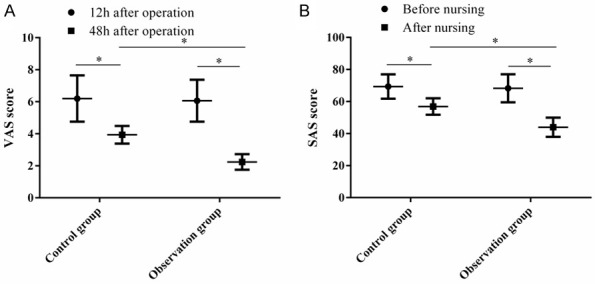
VAS and SAS scores of patients in the control group and observation group. The VAS (A) and SAS (B) scores of patients in the two groups were significantly lower than those before nursing, and the two scores in the observation group were significantly lower than those of the control group. Note: Paired t-test statistics showed that compared with the VAS score 12 hours after operation or before nursing, *P<0.05; t-test statistics showed that compared with the control group after nursing, *P<0.05.
Change in liver function indexes in two groups
We observed the changes of liver function indexes AST (Figure 2A), ALT (Figure 2B), ALB (Figure 2C) and TBIL (Figure 2D) in two groups. No significant differences were observed in the above parameters between CG and OG before nursing (P>0.05). After nursing, serum AST, ALT, and TBIL decreased while ALB increased in both groups (P<0.05), and the improvement of these liver function indexes was more significant in the OG compared with the CG (P<0.05).
Figure 2.
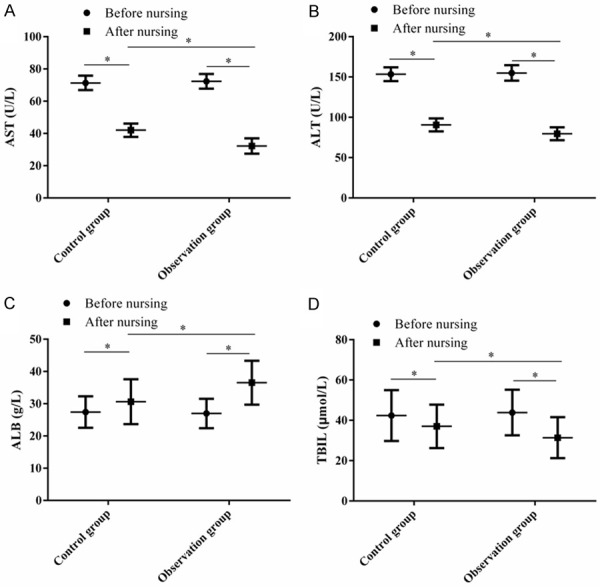
Changes in liver function indexes of patients in the control group and observation group. There was no significant difference in serum AST (A), ALT (B), ALB (C), or TBIL (D) levels between the two groups before nursing. After nursing, serum AST, ALT, and TBIL levels decreased significantly while ALB increased significantly, and these liver function indexes in the observation group were significantly better than those of the control group. Note: Paired t-test statistics showed that compared with the level before nursing, *P<0.05; t-test statistics showed that compared with the control group after nursing, *P<0.05.
Incidence of adverse reactions in two groups
During nursing, 12 cases of nausea and vomiting, 9 cases of abdominal distension and constipation, 13 cases of throat discomfort, and 2 cases of gastrointestinal bleeding were found in the CG. In the OG, nausea and vomiting occurred in 5 cases, abdominal distension and constipation in 7 cases, throat discomfort in 7 cases, and gastrointestinal bleeding in 1 case. Although there was no evident difference in each adverse reaction (P>0.05), the total incidence of adverse reactions in the OG was significantly lower than that in the CG (P<0.05, Table 3).
Table 3.
Adverse reactions of patients in the control group and observation group
| Adverse reactions | Control group (n=66) | Observation group (n=70) | χ2 | P |
|---|---|---|---|---|
| Nausea and vomiting | 12 (18.18) | 5 (7.14) | 3.785 | 0.052 |
| Abdominal distension and constipation | 9 (13.64) | 7 (10.00) | 0.432 | 0.511 |
| Throat discomfort | 13 (19.70) | 7 (10.00) | 2.547 | 0.111 |
| Gastrointestinal bleeding | 2 (3.03) | 1 (1.43) | 0.404 | 0.525 |
| Total incidence (%) | 54.55 | 28.57 | 9.462 | 0.002 |
Nursing satisfaction in two groups
The self-made nursing satisfaction questionnaire was used to investigate the nursing service satisfaction of patients. After nursing, 7 patients felt dissatisfied, 5 felt fair, 33 felt satisfied, and 21 felt very satisfied, with an overall nursing satisfaction rate of 81.82%. In the OG, 1 patient was dissatisfied with the nursing service, 3 patients felt it was fair, 28 patients were satisfied, and 38 patients were very satisfied, with an overall nursing satisfaction rate of 94.29%. The results indicate that the nursing satisfaction of patients in OG was significantly higher than that in CG (P<0.05, Table 4).
Table 4.
Nursing satisfaction of patients in the control group and observation group
| Nursing satisfaction | Control group (n=66) | Observation group (n=70) | χ2 | P |
|---|---|---|---|---|
| Dissatisfied | 7 (10.61) | 1 (1.43) | 5.087 | 0.024 |
| Fair | 5 (7.58) | 3 (4.29) | ||
| Satisfied | 33 (50.00) | 28 (40.00) | ||
| Very satisfied | 21 (31.82) | 38 (54.29) | ||
| Satisfaction (%) | 81.82 | 94.29 |
QoL of patients in two groups
We applied EORTC QLQ-30 to evaluate the life quality of patients before and after nursing. No distinct differences were observed in scores of physical function (Figure 3A), cognitive function (Figure 3B), role function (Figure 3C), em=otional function (Figure 3D) and social function (Figure 3E) between the CG and OG (P>0.05). After nursing, the above scores increased significantly in both groups (P<0.05), with higher scores in the OG (P<0.05).
Figure 3.
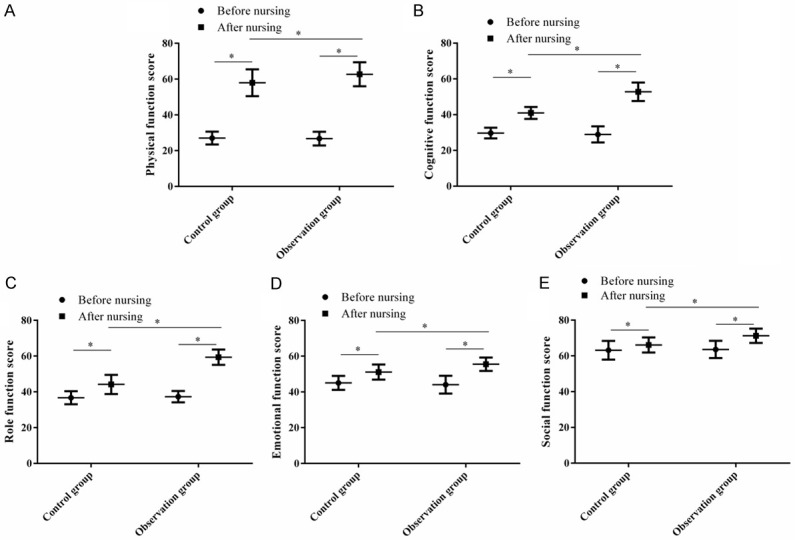
Changes in patients’ quality of life in the control group and observation group. After nursing, the scores of physical function (A), cognitive function (B), role function (C), emotional function (D), and social function (E) of patients in the two groups improved significantly compared with those before nursing, and the scores in the observation group were significantly better than those of the control group. Note: Paired t-test statistics showed that compared with the level before nursing, *P<0.05; t-test statistics showed that compared with the control group after nursing, *P<0.05.
Discussion
Clinically, interventional therapy for liver cancer (LC) has the advantage of small trauma and a simple operation, but it does cause postoperative pain, psychological disorders, and adverse reactions [18]. Therefore, giving appropriate nursing care to LC patients undergoing interventional therapy is necessary.
Generally speaking, conventional nursing lacks the corresponding standardization and planning, and mainly implements the nursing plan according to the doctor’s advice [19]. Personalized nursing, on the other hand, seeks to develop a reasonable and scientific nursing plan by combining with the actual situation of patients, so that patients can receive more systematic nursing services [20]. During the interventional therapy for LC, the pain symptoms of patients are relatively obvious, coupled with a series of gastrointestinal adverse reactions after treatment, which will affect the recovery of patients [21]. In addition, patients are susceptible to negative moods such as tension, irritability, and anxiety as their mentality will change with the worsening pain [22]. In view of this, we gave patients psychological intervention and pain management. The results showed that personalized nursing validly mitigated the pain and anxiety of patients. In addition, compared with the CG, the sleep time of patients in the OG was significantly longer, and the time to ambulation and the length of hospital stay were significantly shorter. The research of Miladinia indicated that slow stroke back massage can reduce the progressive sleep disorders, pain, and fatigue and improve the sleep quality of patients with acute leukemia [23]. Based on this, we carried out music relaxation, massage, and appropriate exercise instruction in pain management, which also contributed to the pain relief in patients.
After interventional therapy, patients have to stay in bed under the conditions of fasting and water-deprivation, so the nursing time is relatively long [24]. In view of the adverse events that frequently occur after interventional therapy, we gave preventive nursing care to patients and adjusted the diet plan reasonably. Hence, the total incidence of adverse reactions decreased significantly and the liver function of patients recovered faster following personalized nursing. Similarly, Gou reported that the application of comprehensive nursing care for patients with liver cirrhosis and LC during interventional therapy can significantly improve patient satisfaction, QoL, and the survival rate, and reduce the incidence of postoperative complications [25]. The reason may be that in the process of personalized care for LC patients undergoing interventional therapy, timely psychological assessment and intervention can eliminate the negative impact caused by patients’ bad emotions and increase their confidence in treatment. In addition, the diet and pain management implemented under personalized nursing can facilitate the physical recovery of patients, reduce adverse reactions, and promote the improvement of liver function. The difference is that comprehensive nursing, with nursing procedures at its core, is a new nursing model that combines the advantages of group nursing and primary care, which is different from the concept of personalized nursing [26]. According to Li, most patients with LC are in the advanced stages, and for them, the QoL is as important as the survival time [27]. QoL is a multi-dimensional and multifaceted measure, which has been regarded as the primary endpoint of cancer medical management and high-quality nursing [28]. In the present study, we provided patients with nursing support and life guidance, which contributed to the improved life quality of patients after personalized nursing. A nursing satisfaction survey was conducted when patients were discharged from hospital. It showed that the patients were generally satisfied with the personalized nursing model, which was helpful for its application and popularization in the clinic.
Although we have confirmed the application prospects of personalized nursing in interventional therapy for LC, there are still some shortcomings in the research. First, the survival rate of patients after nursing was not observed. Second, as a personalized nursing model puts high requirements on a nursing staff’s professional skills, it requires systematic training to achieve the effect, and how to train nurses will be the focus of the next stage of research. Third, further investigation is warranted to confirm whether personalized nursing is applicable to other cancers. All these needs will be addressed by further study.
In conclusion, personalized nursing can mitigate pain and anxiety, reduce the incidence of adverse reactions, and improve patients’ liver function and QoL.
Disclosure of conflict of interest
None.
References
- 1.Zhu Y, Tang H, Zhang L, Gong L, Wu G, Ni J, Tang X. Suppression of miR-21-3p enhances TRAIL-mediated apoptosis in liver cancer stem cells by suppressing the PI3K/Akt/Bad cascade via regulating PTEN. Cancer Manag Res. 2019;11:955–968. doi: 10.2147/CMAR.S183328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Z, Lu J, Zeng G, Pang J, Zheng X, Feng J, Zhang J. MiR-129-5p inhibits liver cancer growth by targeting calcium calmodulin-dependent protein kinase IV (CAMK4) Cell Death Dis. 2019;10:789. doi: 10.1038/s41419-019-1923-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao W, Qiu L, Liu H, Xu Y, Zhan M, Zhang W, Xin Y, He X, Yang X, Bai J, Xiao J, Guan Y, Li Q, Chang L, Yi X, Li Y, Chen X, Lu L. Circulating tumor DNA as a potential prognostic and predictive biomarker during interventional therapy of unresectable primary liver cancer. J Gastrointest Oncol. 2020;11:1065–1077. doi: 10.21037/jgo-20-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Si MB, Yan PJ, Hao XY, Du ZY, Tian HW, Yang J, Han CW, Yang KH, Guo TK. Efficacy and safety of radiofrequency ablation versus minimally invasive liver surgery for small hepatocellular carcinoma: a systematic review and meta-analysis. Surg Endosc. 2019;33:2419–2429. doi: 10.1007/s00464-019-06784-0. [DOI] [PubMed] [Google Scholar]
- 5.Guo L, Ren H, Pu L, Zhu X, Liu Y, Ma X. The prognostic value of inflammation factors in hepatocellular carcinoma patients with hepatic artery interventional treatments: a retrospective study. Cancer Manag Res. 2020;12:7173–7188. doi: 10.2147/CMAR.S257934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li W, Gao J, Wei S, Wang D. Application values of clinical nursing pathway in patients with acute cerebral hemorrhage. Exp Ther Med. 2016;11:490–494. doi: 10.3892/etm.2015.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhuang Y, Pan Z, Li M, Liu Z, Zhang Y, Huang Q. The effect of evidence-based nursing program of progressive functional exercise of affected limbs on patients with breast cancer-related lymphoedema. Am J Transl Res. 2021;13:3626–3633. [PMC free article] [PubMed] [Google Scholar]
- 8.Hendriks J, Andreae C, Agren S, Eriksson H, Hjelm C, Walfridsson U, Ski CF, Thylen I, Jaarsma T. Cardiac disease and stroke: practical implications for personalised care in cardiac-stroke patients. A state of the art review supported by the Association of Cardiovascular Nursing and Allied Professions. Eur J Cardiovasc Nurs. 2020;19:495–504. doi: 10.1177/1474515119895734. [DOI] [PubMed] [Google Scholar]
- 9.Glasper A. Strategies to ensure that all patients have a personalised nursing care plan. Br J Nurs. 2020;29:62–63. doi: 10.12968/bjon.2020.29.1.62. [DOI] [PubMed] [Google Scholar]
- 10.den Hertog R, Niessen T. Taking into account patient preferences in personalised care: blending types of nursing knowledge in evidence-based practice. J Clin Nurs. 2021;30:1904–1915. doi: 10.1111/jocn.15743. [DOI] [PubMed] [Google Scholar]
- 11.Welch-Coltrane JL, Wachnik AA, Adams MCB, Avants CR, Blumstein HA, Brooks AK, Farland AM, Johnson JB, Pariyadath M, Summers EC, Hurley RW. Implementation of individualized pain care plans decreases length of stay and hospital admission rates for high utilizing adults with sickle cell disease. Pain Med. 2021;22:1743–1752. doi: 10.1093/pm/pnab092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tekin F, Findik UY. Level of perception of individualized care and satisfaction with nursing in orthopaedic surgery patients. Orthop Nurs. 2015;34:371–374. doi: 10.1097/NOR.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 13.Rastogi A. Changing role of histopathology in the diagnosis and management of hepatocellular carcinoma. World J Gastroenterol. 2018;24:4000–4013. doi: 10.3748/wjg.v24.i35.4000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ma J, Wang F, Zhang W, Wang L, Yang X, Qian Y, Huang J, Wang J, Yang J. Percutaneous cryoablation for the treatment of liver cancer at special sites: an assessment of efficacy and safety. Quant Imaging Med Surg. 2019;9:1948–1957. doi: 10.21037/qims.2019.11.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yue T, Li Q, Wang R, Liu Z, Guo M, Bai F, Zhang Z, Wang W, Cheng Y, Wang H. Comparison of hospital anxiety and depression scale (HADS) and Zung self-rating anxiety/depression scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology. 2020;236:170–178. doi: 10.1159/000498848. [DOI] [PubMed] [Google Scholar]
- 16.Fu S, Han H, Fan C, Jiang Y. Clinical nursing pathway improves the nursing satisfaction in patients with acute cerebral hemorrhage: a randomized controlled trial protocol. Medicine (Baltimore) 2020;99:e22989. doi: 10.1097/MD.0000000000022989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirchner T, Marquardt S, Werncke T, Kirstein MM, Brunkhorst T, Wacker F, Vogel A, Rodt T. Comparison of health-related quality of life after transarterial chemoembolization and transarterial radioembolization in patients with unresectable hepatocellular carcinoma. Abdom Radiol (NY) 2019;44:1554–1561. doi: 10.1007/s00261-018-1802-y. [DOI] [PubMed] [Google Scholar]
- 18.Wang J, Yan C, Fu A. A randomized clinical trial of comprehensive education and care program compared to basic care for reducing anxiety and depression and improving quality of life and survival in patients with hepatocellular carcinoma who underwent surgery. Medicine (Baltimore) 2019;98:e17552. doi: 10.1097/MD.0000000000017552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu X, Zhang P, Guo C, Xu J, Hu M. Effect of rehabilitation therapy and nursing intervention on postoperative recovery of patients with hypertensive intracerebral hemorrhage. Exp Ther Med. 2019;17:4598–4604. doi: 10.3892/etm.2019.7486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mello M. Practising personalised care. Br J Nurs. 2020;29:82. doi: 10.12968/bjon.2020.29.2.82. [DOI] [PubMed] [Google Scholar]
- 21.Zong DW, Guo CY, Cheng HT, Hu HT, Xiao JC, Li HL. Influence of lactulose on interventional therapy for HCC patients with hepatocirrhosis and hypersplenism. Asian Pac J Trop Med. 2016;9:193–196. doi: 10.1016/j.apjtm.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Lee HH, Chiu CC, Lin JJ, Wang JJ, Lee KT, Sun DP, Shi HY. Impact of preoperative anxiety and depression on quality of life before and after resection of hepatocellular carcinoma. J Affect Disord. 2019;246:361–367. doi: 10.1016/j.jad.2018.12.085. [DOI] [PubMed] [Google Scholar]
- 23.Miladinia M, Baraz S, Shariati A, Malehi AS. Effects of slow-stroke back massage on symptom cluster in adult patients with acute leukemia: supportive care in cancer nursing. Cancer Nurs. 2017;40:31–38. doi: 10.1097/NCC.0000000000000353. [DOI] [PubMed] [Google Scholar]
- 24.Li Z, Wang C, Li J, Liu Z, Jiao D, Han X. MR-guided microwave ablation of hepatocellular carcinoma (HCC): is general anesthesia more effective than local anesthesia? BMC Cancer. 2021;21:562. doi: 10.1186/s12885-021-08298-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gou Y, Yi J, Jiang M, Cao C. Analysis on effects of comprehensive nursing care applied in interventional therapy for patients with liver cirrhosis and liver cancer. Iran J Public Health. 2019;48:494–500. [PMC free article] [PubMed] [Google Scholar]
- 26.Cumbie SA, Conley VM, Burman ME. Advanced practice nursing model for comprehensive care with chronic illness: model for promoting process engagement. ANS Adv Nurs Sci. 2004;27:70–80. doi: 10.1097/00012272-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Li L, Yeo W. Value of quality of life analysis in liver cancer: a clinician’s perspective. World J Hepatol. 2017;9:867–883. doi: 10.4254/wjh.v9.i20.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yan B, Yang LM, Hao LP, Yang C, Quan L, Wang LH, Wu Z, Li XP, Gao YT, Sun Q, Yuan JM. Determinants of quality of life for breast cancer patients in Shanghai, China. PLoS One. 2016;11:e0153714. doi: 10.1371/journal.pone.0153714. [DOI] [PMC free article] [PubMed] [Google Scholar]


